Introduction
Epstein-Barr virus (EBV), which is carried in
>95% of the population worldwide, is a human γ-1 herpes virus
(1). This virus is the cause of a
range of lymphoid and epithelial malignancies and autoimmune
diseases (2,3). EBV usually infects B cells in
oropharyngeal lymphoid tissues and then establishes a persistent
infection in the circulating memory B cells (4,5). EBV
infection may lead to downregulation of the expression of most of
the viral genes with the ability to evade the host's immune
response (6).
Infectious mononucleosis (IM) is a typical form of
primary EBV infection. It usually affects pediatric, adolescent and
young adult patients. It is characterized by fever, pharyngitis,
lymphadenopathy and hepatosplenomegaly. Local or generalized rash
usually occurs during the onset or end of the disease and lasts for
1–6 days (7,8). IM frequently manifests as
hepatosplenomegaly and the enlargement of the spleen is highly
correlated with the platelet count (PLT) in the peripheral blood.
The mean platelet volume (MPV), as an indicator of platelets, is a
simple biomarker of inflammation and is increased in cardiovascular
diseases, peripheral diseases and diabetes mellitus (9–11).
Hepatic dysfunction is common in IM patients. Numerous studies have
indicated that elevation of alanine aminotransferase (ALT),
aspartate aminotransferase (AST) and γ-glutamyl transferase (GGT)
was more common than elevation of bilirubin (12).
Although the MPV/PLT ratio is known to be a useful
index for the diagnosis of numerous diseases in adult patients
(13,14), its utility in pediatric patients with
IM has remained elusive. The aim of the present study was to
investigate the ability of MPV/PLT to detect IM in pediatric
patients. The correlation between MPV/PLT and liver function
indices was also determined. To the best of our knowledge, the
present study was the first to perform this assessment.
Materials and methods
Patients
The present prospective study was performed at the
Children's Hospital of Zhejiang University School of Medicine
(Hangzhou, China). A total of 141 patients (sex, 54 males and 83
females; mean age, 4.9±3.0 years; age range, 0.8–16.6 years) with a
confirmed diagnosis of IM and a normal control cohort consisting of
146 healthy participants (sex, 69 males and 77 females; mean age,
5.2±3.0 years; age range, 0.3–16.3 years) were enrolled. In Western
developed countries, the diagnostic criteria are as follows
(15): i) Clinical triad: Fever,
angina, lymphadenopathy; ii) peripheral blood lymphocyte ratio
≥0.50 and atypical lymphocyte ratio ≥0.10; iii) serum heterophilic
agglutination antibody-positive. However, the diagnostic criteria
for the aforementioned standard adaptation population was composed
of IM cases of 10–30 years of age. China is a developing country
and the peak age of IM is during childhood (<18 years old)
(16). Referring to previous studies
(17,18), the following criteria were used to
diagnose IM in the present study: i) 3 of the following clinical
symptoms: Fever, angina, large cervical lymph nodes, hepatomegaly,
splenomegaly; ii) serological evidence of primary EBV infection,
meeting any of the following two standards: a) Positivity for
anti-EBV-capsid antigen (CA)-IgM and anti-EBV-CA-IgG antibodies; b)
negativity for anti-EBV-CA-lgM but positivity for anti-EBV-CA-IgG
antibody, which is a low-affinity antibody. Those patients meeting
the two criteria described above were diagnosed with IM. The
participants selected for the present study met the diagnostic
criteria aforementioned. Healthy participants were those who
visited the hospital for a general health examination and with
excluded inflammatory diseases based on WBC and hypersensitive
C-reactive protein measurements. The present study was approved by
the medical ethics committee of the Children's Hospital of Zhejiang
University School of Medicine (Hangzhou, China). Written informed
consent was obtained from the guardians on behalf of the
participants of the study.
Blood and liver function
examination
Routine complete blood count (CBC) of peripheral
blood from all participants was performed using the BC-5380
instrument (Mindray Medical International Ltd) and liver function
parameters were detected on an AU5800 (Beckman Coulter). All
reagents for testing were the original reagents of the
instruments.
Statistical analysis
The Kolmogorov-Smirnov normality test was used to
determine if the data is normally distributed. The Mann-Whitney
U-test was used to compare differences in non-parametric variables
(non-normally distributed data). Categorical variables were
presented as a proportion and analyzed with the Chi-squared test.
Continuous data were analyzed using Student's t-test. Values were
expressed as n (%), the mean ± standard deviation or median
(interquartile range). Spearman correlation analysis was used for
grading variable data, whereas Pearson correlation analysis was
used for continuous variable data. For the prediction of IM based
on platelet indices, logistic regression analysis was used to
determine odds ratios (OR) with 95% CI. Receiver operating
characteristic (ROC) curve analysis was used to assess the
diagnostic accuracy of MPV/PLT for IM. All statistical analyses
were performed using SPSS version 22.0 (IBM Corp.). P<0.05 was
considered to indicate statistical significance.
Results
Characteristics of IM patients and
controls
In the IM group, a total of 91.5% of the 141
pediatric patients had fever, 85.8% had angina, 92.9% had cervical
lymphadenopathy, 71.6% had liver enlargement and 65.2% had
splenomegaly. Furthermore, 61.7% were positive for EBV-CA-IgM
antibody and 97.9% were positive for EBV-CA-IgG antibody.
Apart from age and gender for which no statistical
significance were found between the IM and control groups, it was
observed that WBC, ALT, AST, GGT, uric acid (UA) and triglycerides
(TG) were significantly higher in the IM patients compared with in
the healthy controls (P<0.001; Table
I). However, RBC, hemoglobin (HB), urea and total cholesterol
(TC) were significantly reduced (P<0.001; Table I). The four platelet indices, PLT,
platelet distribution width (PDW), MPV and MPV/PLT, exhibited
statistically significant differences between the two groups (PLT,
P<0.001; PDW, P=0.035; MPV, P<0.001; MPV/PLT, P<0.001;
Table I).
 | Table I.Baseline characteristics of pediatric
patients with IM and controls. |
Table I.
Baseline characteristics of pediatric
patients with IM and controls.
| Characteristic | IM group (n=141) | Normal range | Control group
(n=146) | P-value |
|---|
| Male gender | 54
(38.3) | – | 69
(47.3) | 0.125 |
| Age (years) | 4.9±3.0
(0.8–16.6) | – | 5.2±3.0
(0.3–16.3) | 0.334 |
| WBC
(109/l) |
15.06±6.40 |
4.0–12.0 |
7.19±1.47 | 0.000 |
| RBC
(1012/l) |
4.37±0.33 | 3.50–5.50 |
4.52±0.36 | <0.001 |
| HB (g/l) | 119.7±9.2 | 110–155 | 125.0±8.4 | <0.001 |
| ALT (U/l) | 79.0
(36.0–178.5) | <50 | 13.0
(11.0–16.0) | <0.001 |
| AST (U/l) | 69.5
(45.0–116.3) | 15–60 | 31.0
(27.0–35.3) | <0.001 |
| GGT (U/l) | 52.5
(16.0–106.3) | 8–57 | 11.0
(10.0–13.0) | <0.001 |
| CREA (µmol/l) | 46.0 (41.0–51.0) | 15–77 | 46.0
(40.0–52.3) | 0.922 |
| Urea (µmol/l) | 2.95 (2.47–3.55) | 1.79–6.43 | 4.14
(3.64–4.90) | <0.001 |
| UA (µmol/l) | 304 (254–364) | 155–357 | 257 (228–296) | <0.001 |
| TC (mmol/l) |
3.19±0.72 | 3.00–5.70 |
4.28±0.95 | <0.001 |
| TG (mmol/l) |
1.87±0.84 | <1.70 |
1.07±0.86 | <0.001 |
| PLT
(109/l) | 208.4±73.0 | 100–400 | 308.4±81.2 | <0.001 |
| MPV (fl) |
9.73±1.25 |
6.5–11.5 |
8.39±1.00 | <0.001 |
| PDW (%) | 15.37±1.44 |
0.0–20.0 | 15.65±0.64 | 0.035 |
| MPV/PLT (%) |
5.43±2.66 | – |
2.95±1.06 | <0.001 |
Predictive value of platelet indices
in IM patients
Regression analysis was used to analyze the
predictive value of the four indices of platelets in the disease
group. For regression analysis, three models were built (Table II). Using Model 1 without any
correction factors, all four indices were statistically significant
predictors of IM within the 95% CI (P<0.05). Following
adjustment for age and gender in Model 2, the four indices remained
statistically significant in the 95% CI (P<0.05). However, based
on Model 2, after WBC, RBC, HB, ALT, AST, GGT, UA, urea, creatinine
(CREA), TC and TG were adjusted in Model 3, MPV and PDW were no
longer statistically significant (PDW, P=0.350; MPV, P=0.353),
while PLT and MPV/PLT remained significant predictors of IM
(P=0.005 and 0.006, respectively; Table
II).
 | Table II.Logistic regression analysis for
platelet indices to distinguish pediatric patients with infectious
mononucleosis from healthy controls. |
Table II.
Logistic regression analysis for
platelet indices to distinguish pediatric patients with infectious
mononucleosis from healthy controls.
|
| Model 1 | Model 2 | Model 3 |
|---|
|
|
|
|
|
|---|
| Variable | OR (95%CI) | P-value | OR (95%CI) | P-value | OR (95%CI) | P-value |
|---|
| PLT
(109/l) | 0.982
(0.977–0.986) | <0.001 | 0.981
(0.976–0.985) | <0.001 | 0.976
(0.959–0.993) | 0.005 |
| MPV (fl) | 2.938
(2.212–3.902) | <0.001 | 3.225
(2.381–4.368) | <0.001 | 1.425
(0.675–3.006) | 0.353 |
| PDW (%) | 0.782
(0.617–0.989) | 0.040 | 0.778
(0.614–0.984) | 0.036 | 0.693
(0.322–1.493) | 0.350 |
| MPV/PLT (%) | 2.997
(2.268–3.961) | <0.001 | 3.297
(2.448–4.442) | <0.001 | 3.224
(1.396–7.447) | 0.006 |
Correlation of MPV/PLT with laboratory
parameters in IM and healthy control groups
In the IM group, age, WBC, ALT, AST, GGT, CREA and
UA were positively correlated with MPV/PLT, while RBC, HB, urea, TC
and TG were negatively correlated with MPV/PLT. The correlation of
MPV/PLT with ALT, AST, GGT, CREA, UA and TC was statistically
significant (P≤0.01). Regarding the correlation between MPV/PLT (%)
and other variables in healthy controls, only age, creatinine and
WBC were statistically significant (P<0.05). Of note, the
correlation between MPV/PLT and liver function indices in the IM
patients was statistically significant (ALT, P=0.005; AST, P=0.010;
GGT, P=0.004). The details are provided in Table III.
 | Table III.Correlation between mean platelet
volume-to-platelets ratio (%) and other variables in pediatric
patients with IM and controls. |
Table III.
Correlation between mean platelet
volume-to-platelets ratio (%) and other variables in pediatric
patients with IM and controls.
|
| IM group
(n=141) | Control group
(n=146) |
|---|
|
|
|
|
|---|
| Variable | r | P-value | r | P-value |
|---|
| Age (years) | 0.125 | 0.140 | 0.247 | 0.003 |
| WBC
(109/l) | 0.013 | 0.877 | −0.174 | 0.036 |
| RBC
(1012/l) | −0.137 | 0.106 | −0.047 | 0.574 |
| HB (g/l) | −0.109 | 0.200 | 0.054 | 0.517 |
| ALT
(U/l)a | 0.235 | 0.005 | −0.048 | 0.574 |
| AST
(U/l)a | 0.216 | 0.010 | −0.152 | 0.071 |
| GGT
(U/l)a | 0.244 | 0.004 | −0.133 | 0.114 |
| CREA
(µmol/l)a | 0.292 | <0.001 | 0.202 | 0.016 |
| Urea
(µmol/l)a | −0.039 | 0.653 | 0.113 | 0.182 |
| UA
(µmol/l)a | 0.271 | 0.001 | 0.100 | 0.237 |
| TC (mmol/l) | −0.300 | <0.001 | −0.095 | 0.261 |
| TG (mmol/l) | −0.131 | 0.123 | −0.048 | 0.570 |
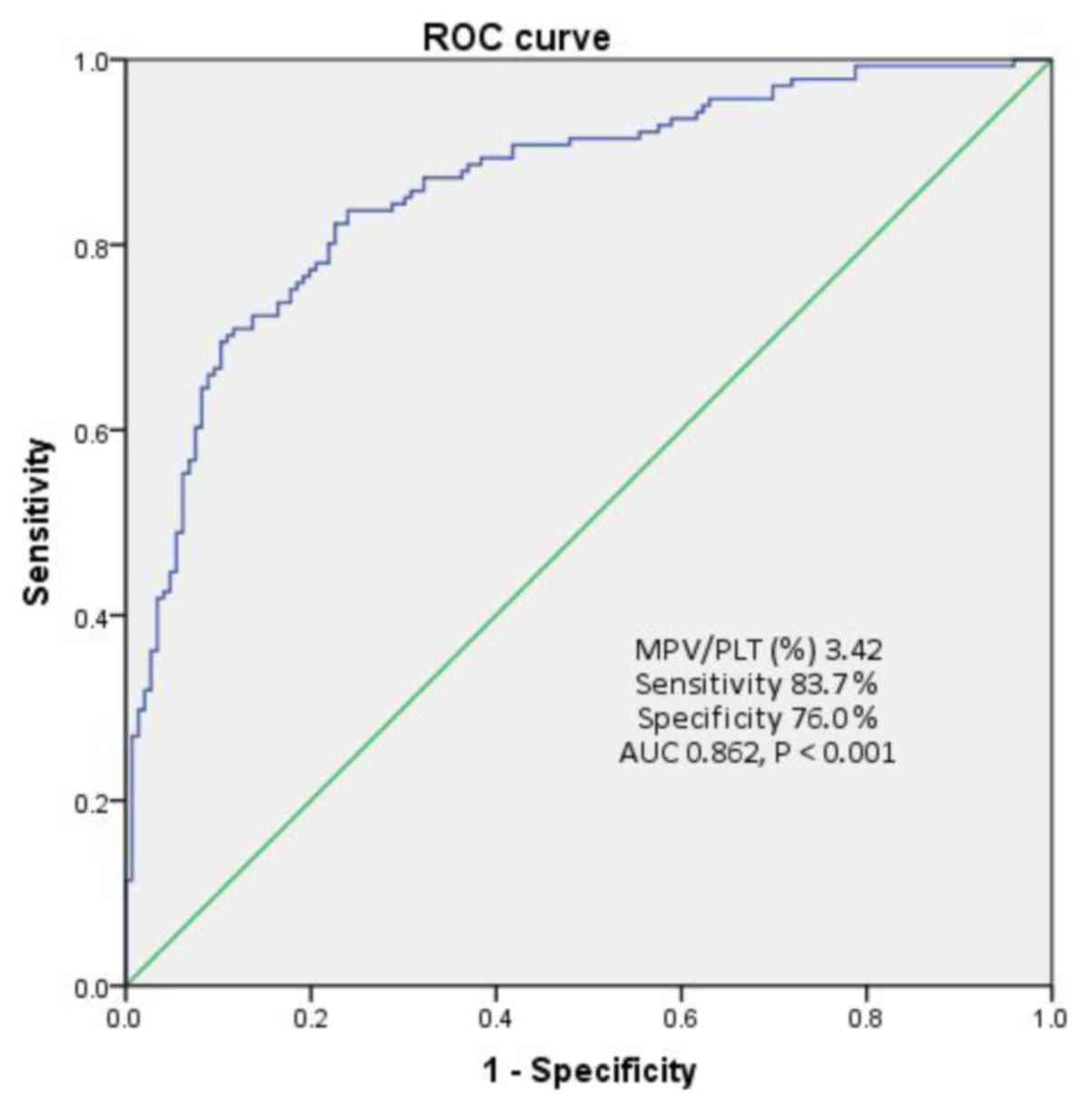
Diagnostic accuracy of MPV/PLT in
IM
As indicated above, it was possible to distinguish
pediatric patients with IM from healthy controls based on the
MPV/PLT. ROC curve analysis was therefore used to evaluate the
diagnostic sensitivity and specificity of MPV/PLT for pediatric IM
(Fig. 1). When the cut-off value for
MPV/PLT was set at 3.42%, the sensitivity was 83.7%, the
specificity was 76% with an area under the curve calculated to be
0.862.
Discussion
EBV has a high prevalence worldwide (19). In industrialized countries, it is
estimated that >50% of the population under the age of 5 years
have been infected with EBV (20).
Most individuals infected with EBV are either asymptomatic or have
mild symptoms; however, certain patients develop IM, particularly
during childhood.
Numerous studies have investigated the association
between certain diseases and readily available parameters from CBC
data, including the neutrophil-to-lymphocyte ratio,
monocyte-to-lymphocyte ratio, PLT-to-lymphocyte ratio and MPV/PLT
(15,16,21,22).
MPV, PDW and PLT are three general indicators of platelets. Studies
have suggested that a high MPV may be associated with an increased
risk of vascular complications (23,24).
MPV mainly reflects the proliferation, metabolism
and platelet production of megakaryocytes in the bone marrow. In
addition, it reflects the survival time of platelets in the
circulation. When the function of myeloproliferation is normal, the
decrease in the number of platelets stimulates the production of
large-volume platelets by megakaryocytes, resulting in an increase
in MPV (25). Thrombocytopenia in
aplastic anemia or acute leukemia is caused by bone marrow damage
and as a result, the MPV is reduced. Idiopathic thrombocytopenic
purpura (ITP), also known as primary or immune thrombocytopenic
purpura, is an autoimmune disease, and most pediatric patients
affected have a history of viral infections (e.g., viral upper
respiratory tract infection, rubella or chickenpox) (26). Thrombocytopenia occurs 1–3 weeks
after viral infection, indicating that it is not a virus that
directly destroys platelets. Intravascular platelet destruction may
be another mechanism for thrombocytopenia in pediatric patients
with ITP (26).
The present study indicated that in pediatric
patients with IM, the MPV was higher than that in the control group
and the difference was statistically significant (P<0.01). IM
patients frequently have splenomegaly, while the spleen has a close
association with platelets in peripheral blood. Thus, PDW and PLT
were examined in the present study. Of note, the disease group had
a higher MPV and a lower PDW (P<0.01). As the MPV was relatively
higher and the PLT was lower in IM patients, the MPV/PLT ratio was
introduced to observe the difference between the two groups. As
expected, the MPV/PLT ratio in IM patients was significantly higher
than that in the controls (P<0.01). ITP has a good bone marrow
compensatory function and PLT feedback activates megakaryocytes,
resulting in an increase in platelet volume. Increased MPV and
thrombocytopenia lead to an increase in MPV/PLT; however, this
occurs one to three weeks after viral infection.
IM usually unfolds as a benign clinical process but
serious complications may occur. Hepatic failure has been reported
in patients with IM (27,28). ALT, AST and GGT are the three
transferases with the highest clinical relevance and primary
indices of liver function. GGT is widely used as a marker of
excessive alcohol intake in patients with alcoholic liver disease
(29). In addition, serum GGT levels
are frequently increased in patients with non-alcoholic fatty liver
disease (30). As GGT is a
manifestation of liver injury, the present study aimed to predict
liver damage in the early stage of IM.
In the clinic, anti-viral therapy is generally
applied in pediatric IM complicated with liver function damage.
Early prediction and intervention of liver function damage in
children is necessary. In order to study the diagnostic value of
each indicator, regression analysis was used in the present study
to assess various indicators. After adjustment for other variables,
only PLT and MPV/PLT were obtained as diagnostic indices
independent of other clinical indices (P<0.01). It was indicated
that MPV/PLT had a higher predictive value for IM than PLT alone
(MPV/PLT, 95% CI=1.396–7.447 and OR=3.224; PLT alone, 95%
CI=0.959–0.993 and OR=0.976). Although 0.976 appears to be an
insufficient OR, MPV/PLT was significantly superior in predicting
disease compared with PLT.
The present study indicated that the liver function
indices of pediatric patients with IM were significantly higher
than those of the control group. Sampling of liver biopsies from
patients with IM may explain the cause of the increased transferase
levels (31). Of note, liver biopsy
places high emotional and physical burden on children. In the
present study, MPV/PLT was indicated to be an independent
diagnostic factor for IM, which also had a significant positive
correlation with liver function indicators. Although MPV/PLT had a
significantly correlated with creatinine (P<0.001) in a positive
manner, it is a renal index which can be investigated further in
future research. At the same time, the ROC curve analysis for
MPV/PLT to predict IM had high sensitivity and specificity
(sensitivity, 83.7%; specificity, 76%).
CBC is an examination that is routinely performed
for almost all diseases. The present study indicated that the
MPV/PLT ratio has a certain diagnostic value for pediatric IM. At
the same time, it was revealed that if the MPV/PLT ratio is
increased, liver function damage is more likely to occur. MPV/PLT
may be a novel indicator for the diagnosis of pediatric IM and
indirectly predict damage of liver function.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
XCH and PFX designed the current study and were
major contributors in writing the manuscript. XZD, YXL and JFZ were
responsible for the collection and analysis of data. HX performed
the statistics of the data and gave final approval of the
manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the medical ethics
committee of the Children's Hospital of Zhejiang University School
of Medicine (Hangzhou, China). Written informed consent was
obtained from the guardians on behalf of the participants of the
present study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Young LS and Rickinson AB: Epstein-Barr
virus: 40 years on. Nat Rev Cancer. 4:757–768. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Posnett DN: Herpesviruses and
autoimmunity. Curr Opin Investig Drugs. 9:505–514. 2008.PubMed/NCBI
|
|
3
|
Salvetti M, Giovannoni G and Aloisi F:
Epstein-Barr virus and multiple sclerosis. Curr Opin Neurol.
22:201–206. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Babcock GJ, Decker LL, Volk M and
Thorley-Lawson DA: EBV persistence in memory B cells in vivo.
Immunity. 9:395–404. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rickinson AB, Long HM, Palendira U, Munz C
and Hislop AD: Cellular immune controls over Epstein-Barr virus
infection: New lessons from the clinic and the laboratory. Trends
Immunol. 35:159–169. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kurth J, Spieker T, Wustrow J, Strickler
GJ, Hansmann LM, Rajewsky K and Küppers R: EBV-infected B cells in
infectious mononucleosis: Viral strategies for spreading in the B
cell compartment and establishing latency. Immunity. 13:485–495.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hall LD, Eminger LA, Hesterman KS and
Heymann WR: Epstein-Barr virus: Dermatologic associations and
implications: Part I. Mucocutaneous manifestations of Epstein-Barr
virus and nonmalignant disorders. J Am Acad Dermatol. 72:1–19.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Di Lernia V and Mansouri Y: Epstein-Barr
virus and skin manifestations in childhood. Int J Dermatol.
52:1177–1184. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Berger JS, Eraso LH, Sha D and Mohler ER
III: Mean platelet volume and prevalence of peripheral artery
disease, the National Health and Nutrition Examination Survey,
1999–2004. Atherosclerosis. 213:586–591. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Abalı G, Akpınar O and Söylemez N:
Correlation of the coronary severity scores and mean platelet
volume in diabetes mellitus. Adv Ther. 31:140–148. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sansanayudh N, Numthavaj P, Muntham D,
Yamwong S, McEvoy M, Attia J, Sritara P and Thakkinstian A:
Prognostic effect of mean platelet volume in patients with coronary
artery disease. A systematic review and meta-analysis. Thromb
Haemost. 114:1299–1309. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yang SI, Geong JH and Kim JY: Clinical
characteristics of primary Epstein Barr virus hepatitis with
elevation of alkaline phosphatase and γ-glutamyltransferase in
children. Yonsei Med J. 55:107–112. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Golwala ZM, Shah H, Gupta N, Sreenivas V
and Puliyel JM: Mean platelet volume (MPV), platelet distribution
width (PDW), platelet count and plateletcrit (PCT) as predictors of
in-hospital paediatric mortality: A case-control Study. Afr Health
Sci. 16:356–362. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Loonen AJ, de Jager CP, Tosserams J,
Kusters R, Hilbink M, Wever PC and van den Brule AJ: Biomarkers and
molecular analysis to improve bloodstream infection diagnostics in
an emergency care unit. PLoS One. 9:e873152014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Naess A, Nilssen SS, Mo R, Eide GE and
Sjursen H: Role of neutrophil to lymphocyte and monocyte to
lymphocyte ratios in the diagnosis of bacterial infection in
patients with fever. Infection. 45:299–307. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zheng CF, Liu WY, Zeng FF, Zheng MH, Shi
HY, Zhou Y and Pan JY: Prognostic value of platelet-to-lymphocyte
ratios among critically ill patients with acute kidney injury.
Critical Care. 21:2382017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chan CW, Chiang AK, Chan KH and Lau AS:
Epstein- Barr-virus-associated infectious mononucleosis in Chinese
children. Pediatr Infect Dis J. 22:974–978. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Taai MH, Hsu CY, Yen MH, Yan DC, Chiu CH,
Huang YC, Lin SJ and Lin TY: Epstein-Barr-virus-associated
infectious mononucleosis and risk factor analysis for complications
hospitalized children. J Microbio Immunol Infect. 38:255–261.
2005.
|
|
19
|
Hislop AD, Taylor GS, Sauce D and
Rickinson AB: Cellular responses to viral infection in humans:
Lessons from Epstein-Barr virus. Annu Rev Immunol. 25:587–617.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Luzuriaga K and Sullivan JL: Infectious
mononucleosis. N Engl J Med. 362:1993–2000. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Liu X, Shen Y, Wang H, Ge Q, Fei A and Pan
S: Prognostic significance of neutrophil-to-lymphocyte ratio in
patients with sepsis: A prospective observational study. Mediators
Inflamm 2016:. 191254:2016.
|
|
22
|
Oh GH, Chung SP, Park YS, Hong JH, Lee HS,
Chung HS, You JS, Park JW and Park I: Mean platelet volume to
platelet count ratio as a promising predictor of early mortality in
severe sepsis. Shock. 47:323–330. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ulutas KT, Dokuyucu R, Sefil F, Yengil E,
Sumbul AT, Rizaoglu H, Ustun I, Yula E, Sabuncu T and Gokce C:
Evaluation of mean platelet volume in patients with type 2 diabetes
mellitus and blood glucose regulation: A marker for
atherosclerosis? Int J Clin Exp Med. 7:955–961. 2014.PubMed/NCBI
|
|
24
|
Kodiatte TA, Manikyam UK, Rao SB, Jagadish
TM, Reddy M, Lingaiah HK and Lakshmaiah V: Mean platelet volume in
type 2 diabetes mellitus. J Lab Physicians. 4:5–9. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
O Malley T, Langhome P, Elton RA and
Stewart C: Platelet size in stroke patients. Stroke. 26:995–999.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gao Ju and Luo Chunhua: The pathogenesis
and diagnosis of autoimmune thrombocytopenic purpura progress in
governance. Chin J Prac Pediatrics. 18:772003.
|
|
27
|
Harries JT and Ferguson AW: Fatal
infectious mononucleosis with liver failure in two sisters. Arch
Dis Child. 43:480–485. 1968. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
McMahon JM, Elliott CW and Green RC:
Infectious mononucleosis complicated by hepatic coma. Am J
Gastroenterol. 51:200–207. 1969.PubMed/NCBI
|
|
29
|
Rosalki SB and Rau D: Serum-glutamyl
transpeptidase activity in alcoholism. Clin Chim Acta. 39:41–47.
1972. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Banderas DZ, Escobedo J, Gonzalez E,
Liceaga MG, Ramírez JC and Castro MG: γ-Glutamyl transferase: A
marker of nonalcoholic fatty liver disease in patients with the
metabolic syndrome. Eur J Gastroenterol Hepatol. 24:805–810. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wadsworth RC and Keil PG: Biopsy of the
liver in infectious mononucleosis. Am J Pathol. 28:1003–1025.
1952.PubMed/NCBI
|