Case report
A 67-year-old male had been suffering from recurrent
lower urinary tract infections for 5 years. The major
manifestations were urgency and urinary frequency, lower abdominal
and perineal pain, and occasionally hematuria. The patient's
self-administered antibiotics improved his symptoms, but these
symptoms often occured repeatedly. The patient also previously had
hypospadias, and >40 years ago, he had received hypospadias
repair and cystostomy. The patient had not received any treatment
for his left cryptorchidism, azoospermia or infertility.
On digital rectal examination, prostate palpation
was not obvious, a stony hard mass was present at the distal end
and it was not possible to assess the boundaries. Scars from the
previous surgery for hypospadias and vesicostomy were present. The
right testicle was atrophic and had an empty left hemiscrotum. No
abnormalities were observed in body temperature on admission,
routine blood tests, biochemical tests and electrocardiogram.
Parathyroid hormone levels, prostate-specific antigen, coagulation
function, androgen levels and cytological results, as well as renal
and liver function, were normal and hepatitis tests were negative.
The prostate-specific antigen level was 0.01 ng/ml. The patient's
blood type was B and RH positive. Urinalysis revealed a leukocyte
count of 12.83 per high-power field (HPF), an erythrocyte count of
7.09 per HPF and a squamous cell count of 12.66 per HPF. The urine
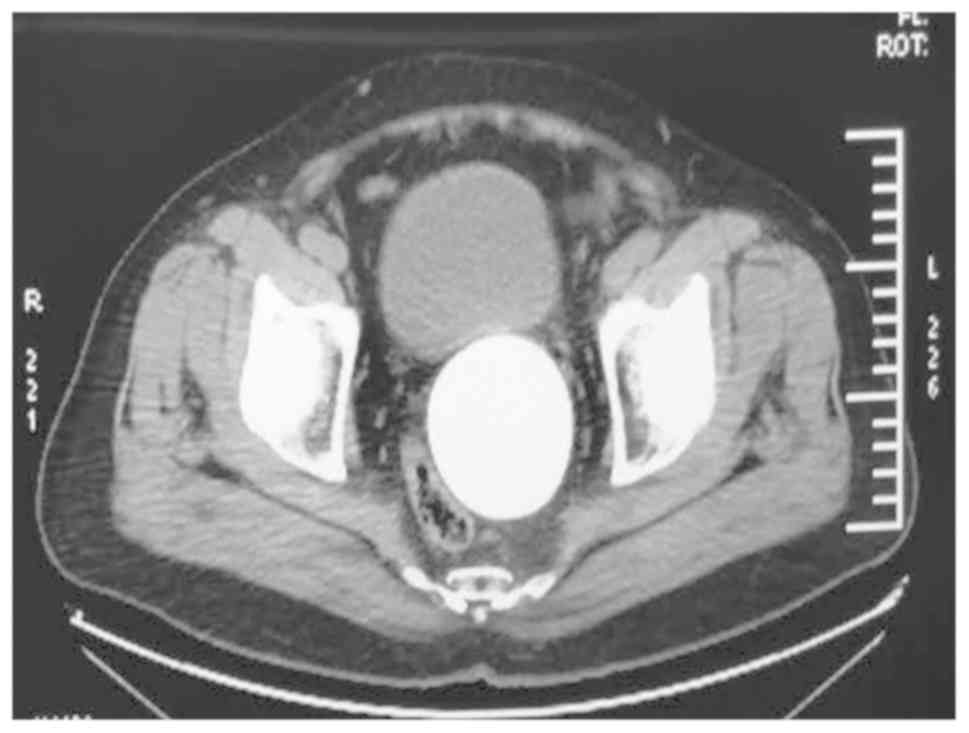
culture results indicated an Escherichia coli infection. An X-ray
of the pelvis displayed a large calcific density in the pelvic
cavity (Fig. 1). CT revealed a large
round dense shadow with a clear boundary that appeared between the
bladder and rectum, which was 10.4 cm in diameter and a CT value of
~792.9 HU. The bladder, rectum and sigmoid colon were obviously
compressed and displaced (Fig. 2).
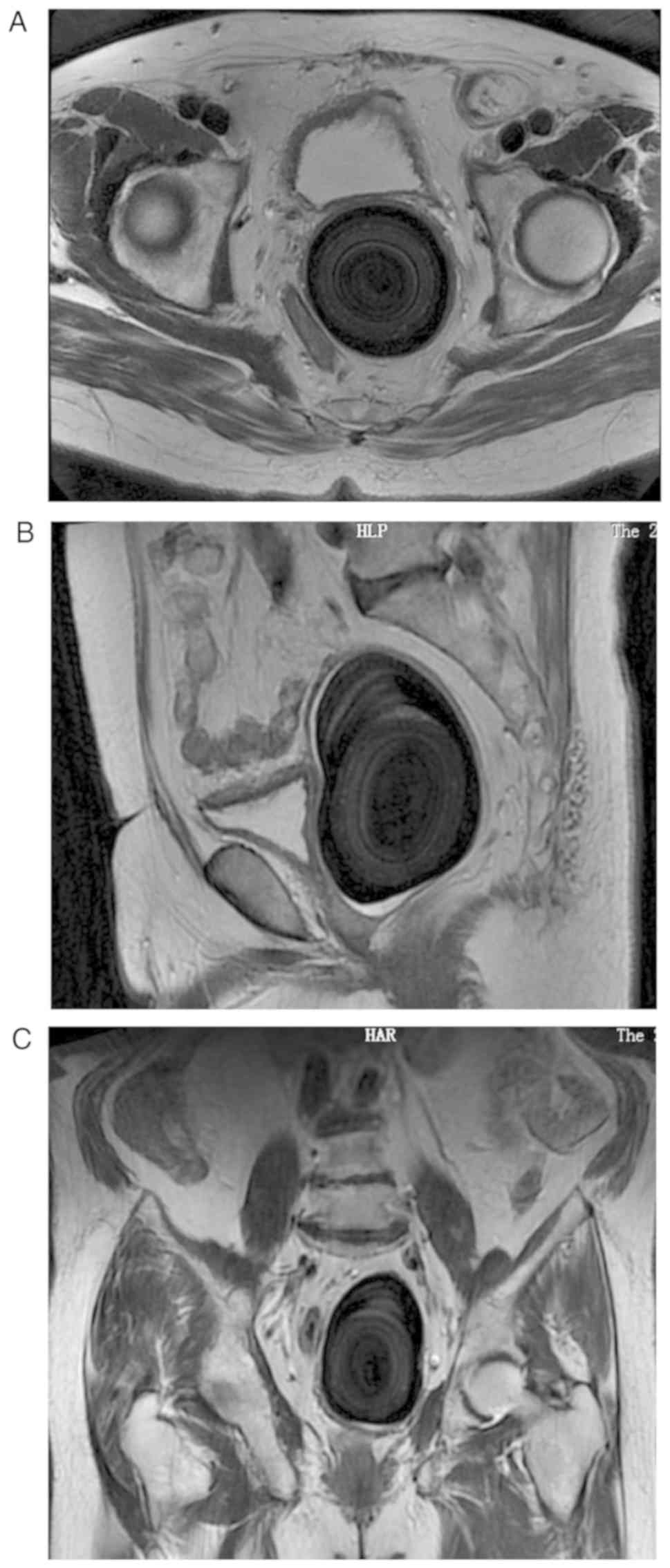
MRI of the pelvis indicated a large abnormal signal that was
visible between the bladder and the rectum, and the lesion was
dominated by extremely low signals. The inside of the stone
appeared as a concentric ring shape with a slightly higher signal
(Fig. 3).
The urinary infection was controlled using suitable
antibiotics. An endoscopic examination was performed before the
removal of the calculus to further confirm the diagnosis of SVC.
Due to urethral stricture, urethral dilatation was performed
intra-operatively by using a 24 French (Fr) urethral sound, and
subsequently, a 8.5/9.8 Fr rigid ureteroscope was successfully
placed under guidance. It was observed that the anterior
hypospadias repair had healed to leave a stenosis scar and the
seminal hillock was obviously expanded. However, it was not
possible to place the ureteroscope into the seminal vesicle around
the giant calculus. The diagnosis of SVC was further confirmed.
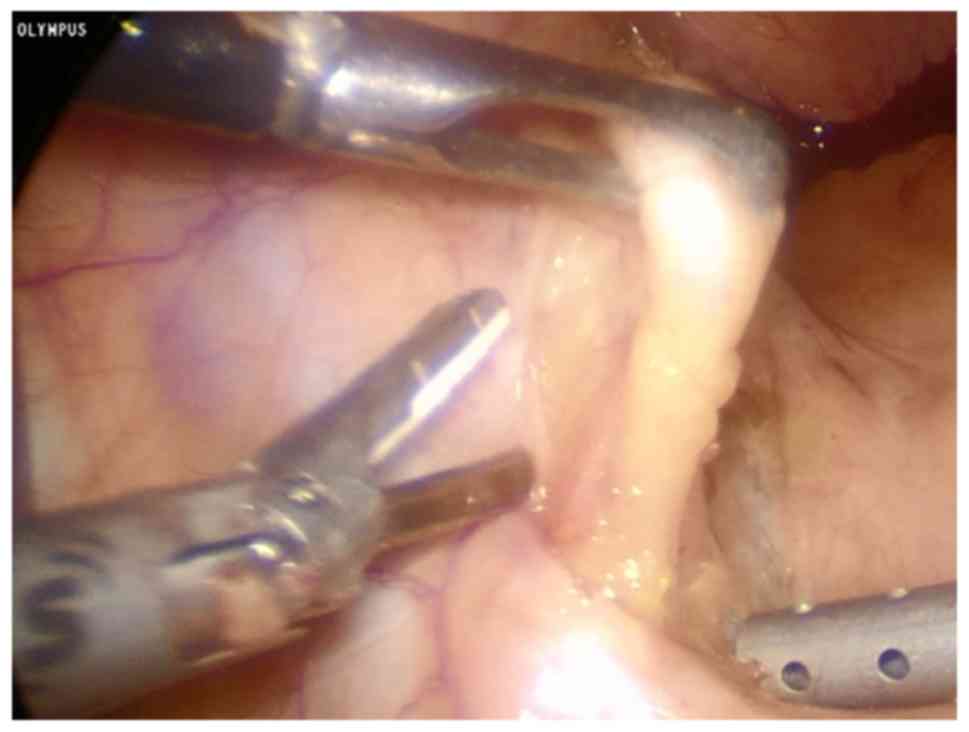
Considering the size of the calculus, laparoscopic
surgery was selected for removal of the calculus. The easily
identifiable vas deferens was used as a guide for seminal vesicle
resection (Fig. 4). It was observed
that the left seminal vesicle was significantly enlarged. The
bottom of the seminal vesicle was dissected by using an ultrasonic
knife and the calculus was then removed and placed in a specimen
bag. The inner wall of the seminal vesicle was smooth and the
opening of the seminal vesicle was clearly visible. The dilated
seminal vesicle wall was dissected and almost completely excised.
Serious adhesions were observed between the seminal vesicle wall
and the pelvic tissue. The remaining vesicle was closed with a
continuous locking suture. Upon examination of the left groin area,
the inguinal hernia was not obvious and no cryptorchid tissue was
observed. The calculus and dilated wall were removed through the
expanded umbilical incision. The calculus was light brown-colored,
had a round and smooth appearance, measured roughly 10.4×6.0×6.9 cm
(Fig. 5). Pathological analysis
indicated that the cystic wall consisted of proliferating fiber
smooth muscle vascular tissue. The covered mucosa was a
proliferating squamous epithelium with hyperkeratosis with massive
chronic inflammatory cell infiltration.
The patient recovered well without any complaints or
complications. The transurethral catheter was removed after 3 days
and was discharged on post-operative day 5. The patient was
regularly followed up and the symptoms were obviously improved
compared with those prior to the surgery.
Discussion
The first case of SVC was reported in 1928, and
since then, only a few clinically reported cases have been
described (1). The definite
mechanisms of the formation of SVC remain elusive; however, it
usually occurs in patients with infection, urinary tract
obstruction, anatomic anomaly, seminal vesicle cysts or reflux
(2). In addition, 16.2% of patients
with hemospermia have SVC (3).
Although certain patients are asymptomatic, frequent lower urinary
tract infections, haematospermia and ejaculatory pain, perineum or
testicular pain are common (4).
Furthermore, a series of lower urinary tract symptoms have been
associated with frequency and urgency to urinate, dysuria and
urinary tract infections (1,4). The most common symptom/complaint of a
patient seeking medical care is hematospermia and ejaculation pain,
and this may subside if left untreated. The patient of the present
study had a history of numerous years of recurrent urinary tract
infections. The major symptoms included urgency and increased
frequency of urination, lower abdominal and perineal pain and
occasionally hematuria. The patient's self-administered antibiotics
improved his symptoms, which may in part be the reason why he did
not seek hospital care for treatment previously.
The diagnosis of SVC usually involves a combination
of clinical symptoms, rectal digital examination and X-rays
(5). MRI are more sensitive compared
with transrectal ultrasound and CT in the diagnosis of SVC
(6,7). SVC frequently requires surgical
treatment. In previous case reports, transurethral, suprapubic,
transrectal or perineal procedures were applied for the treatment
of stones (8). For large calculus,
open supra-pubic incision and cystotomy is usually selected
(9). Transurethral seminal
vesiculoscopy and laparoscopic approach are currently in use as
effective treatments for SVC. Table
I lists the characteristics and treatments of certain typical
cases that have been reported in the English literature.
 | Table I.Characteristics and treatment of some
significant SVC cases reported in the English literature. |
Table I.
Characteristics and treatment of some
significant SVC cases reported in the English literature.
| Author, year | Country | Age | Clinical
symptoms | Diagnostic
modality | Clinical
diagnosis | Size (cm) | Outcome | (Refs.) |
|---|
| Li et al,
1991 | China | 53 | Perineal
discomfort | X-ray | Multiple stones | 3.2×2.8×2.2
2.5×2.0×0.7 | Transrectal removal
of calculus | (14) |
| Wilkinson, 1993 | UK | 10 | Dysuria and
frequency | X-ray and CT | SVC | N.S. | Fruitless
cystolithotomy followed by seminal vesiculotomy | (15) |
| Carachi and Gobara,
1997 | UK | 7 | Recurent
epididymo-orchitis | X-ray and CT | SVC | 1.0×0.5 | Extraperitoneal
extraction of calculus | (16) |
| Kilciler et
al, 2002 | Turkey | 35 | Perineal and
testicular pain | X-ray and TRUS | SVC | N.S. | Seminal vesiculotomy
to remove the calculi | (17) |
| Kilciler et
al, 2002 | Turkey | 40 | Terminal pain on
urination and hemospermia | X-ray and TRUS | Multiple stones | Max1.2 | Perineal approach for
removal of calculus | (17) |
| Namjoshi, 2002 | UK | 82 | Frequency of
urine | X-ray and CT | Bilateral seminal
vesicle calculus | R3.5×3.5×5.0
L3.0×2.0×4.5 | N.S. | (18) |
| Ozgok et al,
2005 | Turkey | 31 | Perineal pain and
painful ejaculation | X-ray | Multiple stones | N.S. | Seminal vesicle
endoscopic calculi removal | (11) |
| Modi, 2006 | India | 53 | Urinarytract
infection and dysuria | X-ray and TRUS | Multiple stones | N.S. | TRU-SVS and pneumatic
lithotripsy of calculi | (19) |
| Cuda et al,
2006 | USA | 25 | Painful
ejaculation | TRUS | SVC | N.S. | TRU-SVS and laser
lithotripsy of calculi | (7) |
| Singh and Ansari,
2006 | India | 35 | Frequency of urine
and dysuria, lower abdominal pain | X-ray | Bilateral seminal
vesicle calculus | 4.0×3.0 | The patient declined
to seminal vesiculectomy | (5) |
| Han et al,
2008 | China | 62 | Hemospermia, painful
ejaculation and perineal pain | X-ray and CT | Calculus within a
seminal vesicle cyst | 1.2×1.0 | Transperitoneal
laparoscopic vesciculotomy for calculus | (20) |
| Yun et al,
2008 | Korea | 20 | Small volume
ejaculate | X-ray and
urethrography and CT | SVC | 6.0×3.5×3.5 | Transperitoneal
laparoscopic stone removal | (21) |
| Hadidi et al,
2011 | Jordan | 29 | Lower urinary tract
infections and painful ejaculation | X-ray and CT and
MRI | Bilateral seminal
vesicle calculus | 7.0×4.0×3.5 | Transurethral
excision + Open surgical removal of calculus | (9) |
| Lee et al,
2014 | China | 51 | Hemospermia and
perineal discomfort | TRUS | SVC | N.S. | TRU-SVS and laser
fragmentation of calculi | (2) |
| Present study | China | 67 | Lower urinary tract
infections, perineal discomfort, and painful ejaculation | X-ray and CT and
MRI | SVC | 10.4×6.0×6.9 stone
removal | Transperitoneal
laparoscopic |
|
The first seminal vesiculoscopy was reported in 1996
(10) and the first endoscopic
lithotripsy was reported in 2005 (11). Subsequent studies have suggested that
transurethral seminal vesiculoscopy is relatively simple to
perform, is associated with a rapid post-operative recovery, to
have fewer complications than transurethral resection of
ejaculatory ducts and to preserve the normal structure of seminal
vesicles and ejaculatory ducts in the treatment of seminal vesicle
disease (12). It is particularly
advantageous when dealing with small stones of seminal vesicles.
Transperitoneal laparoscopy is considered a safe and thorough
treatment for large stones (1). To
the best of our knowledge, the SVC of the present case is the
largest reported in the English literature and laparoscopic surgery
was selected for treatment. The patient was 67 years old,
infertile, had low requirements for sexual and reproductive
functions and decided not to retain the seminal vesicle at the
pre-operative consultation
This patient had a history of hypospadias,
cryptorchidism, and azoospermic, and a similar medical history was
observed in another case (9). Both
of them were infertile. There is currently no clear evidence of an
association between SVC and hypospadias (9). Hypoplasia, agenesis and congenital
cysts of the seminal vesicles have been suggested to be linked to
cryptorchidism (13). Anomalies of
the seminal vesicles can affect patients of any age, especially
after sexual maturity it become more obvious (9). Based on the current health awareness of
the general population and medical improvements, the number of
patients with SVC will increase; however, large seminal calculi may
be difficult to detect. The patient of the present study was not
the first case of large SVC accompanied with hypospadias and
cryptorchidism reported. Further research is warranted to determine
whether there may be a link with chromosome variations.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
HH conceived and supervised the study. HY, YW and JG
acquired the data. PW, XJ and DT retrieved and reviewed the
literature, analyzed the results and critically revised the
manuscript for intellectual content. HY drafted the manuscript. HH
and HY prepared figures and tables. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the Department of Urology, The Second Hospital of
Tianjin Medical University (Tianjin, China).
Patient consent for publication
Informed consent for publication was obtained from
the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Christodoulidou M, Parnham A and Nigam R:
Diagnosis and management of symptomatic seminal vesicle calculi.
Scand J Urol. 51:1–8. 2017.PubMed/NCBI
|
|
2
|
Lee TH, Juan YS, Jang MY, Wang HS and Shen
JT, Lee TH, Juan YS, Jang MY, Wang HS and Shen JT: Successful
seminal vesiculoscopic lithotripsy of seminal vesicle stone: A case
report and literature review. Urolog Sci. 25:134–146. 2014.
View Article : Google Scholar
|
|
3
|
Yang SC, Rha KH, Byon SK and Kim JH:
Transutricular seminal vesiculoscopy. J Endourol. 16:343–345. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Corriere JN Jr: Painful ejaculation due to
seminal vesicle calculi. J Urol. 157:6261997. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Singh I and Ansari M: Idiopathic bilateral
giant seminal vesicle calculi and calcification of the male
ejaculatory system: Current review of diagnosis and management.
Indian J Surg. 68:38–40. 2006.
|
|
6
|
Cho IR, Lee MS, Rha KH, Hong SJ, Park SS
and Kim MJ: Magnetic resonance imaging in hemospermia. J Urol.
157:258–262. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cuda SP, Brand TC, Thibault GP and Stack
RS: Case report: Endoscopic laser lithotripsy of seminal-vesicle
stones. J Endourol. 20:916–918. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schwartz BF: Stones of the urethra,
prostate, seminal vesicle, bladder, and encrusted foreign
bodiesUrinary Stone Disease. Stoller ML and Meng MV: Humana Press;
New Jersey: pp. 661–681. 2007, View Article : Google Scholar
|
|
9
|
Hadidi M, Hadidy A, Alrabadi AF,
Ahdul-Wahab AD and Murshidi MM: Bilateral very large calcium
oxalate stones in the seminal vesicles: Case report and literature
review. Urol Res. 39:509–513. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shimada M and Yoshida H: Ex vivo ultrathin
endoscopy of the seminal vesicles. J Urol. 156:1388–1390. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ozgok Y, Kilciler M, Aydur E, Saglam M,
Irkilata HC and Erduran D: Endoscopic seminal vesicle stone
removal. Urology. 65:5912005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Han CH, Liang Q, Dong BZ, Hao L, Fan T,
Zhang JJ, Zhang WD, Chen B, Qiu XZ, Zhou XJ and Pei CS: The
transurethral seminal vesiculoscopy in the diagnosis and treatment
of the seminal vesicle disease. Cell Biochem Biophys. 66:851–853.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
King BF, Hattery RR, Lieber MM, Williamson
B Jr, Hartman GW and Berquist TH: Seminal vesicle imaging.
Radiographics: A review publication of the Radiological Society of
North America, Inc. 9:653–676. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Li YK: Diagnosis and management of large
seminal vesicle stones. Br J Urol. 68:322–323. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wilkinson AG: Case report: Calculus in the
seminal vesicle. Pediatr Radiol. 23:3271993. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Carachi R and Gobara D: Recurrent
epididymo-orchitis in a child secondary to a stone in the seminal
vesicle. Br J Urol. 79:9971997. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kilciler M, Saglam M, Ozgok Y, Somuncu I,
Erduran D and Harmankaya C: Giant seminal vesicle stones. Report of
two cases. Urol Int. 69:250–251. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Namjoshi SP: Large bilateral star-shaped
calculi in the seminal vesicles. J Postgrad Med. 48:122–123.
2002.PubMed/NCBI
|
|
19
|
Modi PR: Case report: Endoscopic
management of seminal vesicle stones with cutaneous fistula. J
Endourol. 20:432–435. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Han P, Yang YR, Zhang XY and Wei Q:
Laparoscopic treatment of a calcium fluorophosphate stone within a
seminal vesicle cyst. Asian J Androl. 10:337–340. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yun SJ, Kim TH, Kwon WA, Kim YJ, Lee SC
and Kim WJ: A large stone in the dilated left seminal vesicle:
Laparoscopic removal and partial seminal vesiculectomy. Korean J
Urol. 49:656–658. 2008. View Article : Google Scholar
|