Introduction
Silicone oils are constituted of a linear chain of
siloxane repeat units (-Si-O) and are considered to be an ideal
substitute material for the vitreous. Silicone oil has been widely
used in complex vitreoretinal surgery since Cibis et al
(1) first demonstrated the
intravitreal use of silicone oil in 1962, and is an important
auxiliary tool in complex vitreoretinal surgery. The common
indications for silicone oil tamponade (SOT) are proliferative
vitreoretinopathy, severe diabetic retinopathy, large retinal
tears, viral retinitis and ocular trauma (2,3). The
success rate of vitreoretinal surgery has markedly increased since
the introduction of SOT and the range of applications has expanded
to the treatment of macular holes in highly myopic eyes (4), chronic and persistent macular holes,
colobomatous retinal detachment (5)
and chronic uveitis with hypotony (6). However, the long-term use of
intraocular SOT is thought to cause complications, including
cataracts, keratopathy and glaucoma. Therefore, silicone oil is
commonly used in temporary intraocular tamponade and is recommended
to be removed as soon as possible (7). However, there is no consensus on when
to remove the silicone oil and most surgeons do so between 3 and 6
months to avoid alleged late complications, including optic atrophy
from glaucoma or tissue impregnation (8).
Optical coherence tomography angiography (OCTA) is a
novel non-invasive vascular imaging technique used to display
retinal and choroidal blood vessels, providing a novel method for
the assessment of associated vascular diseases (9,10).
Intraocular silicone oil has been commonly used as a vitreous
substitute for >5 decades. However, whether silicone oil is
toxic to the retinal vasculature and whether the compressing effect
of silicone oil decreases retinal thickness has remained to be
elucidated. To address these questions, the association between
silicone oil treatment and the condition of the retinal vessels was
explored using OCTA. In addition, retinal thickness was evaluated
in patients with SOT using OCT.
Materials and methods
Study participants
The present study retrospectively analyzed the
results of 23 patients with complex vitreoretinal disease, reported
at Zhongshan Ophthalmic Center (Sun Yat-sen University, Guangzhou,
China) between July 2016 and September 2017, and a single eye was
assessed in each participant. These patients had previously
received pars plana vitrectomy, laser coagulation and SOT, had used
perfluorocarbon liquids where necessary (SOT group) and had all
received OCTA examinations ~1 and 3 months into the follow-up
period. Furthermore, 20 patients were included who had received SOT
between January 2016 and April 2017, had required silicone oil
removal (SOR group), and who had received an OCTA examination ~1
week previously, as well as 3 months after SOR. Patients with
glaucoma, keratopathy, severe cataracts, a re-detached retina,
diabetes or any other severe systemic diseases were excluded from
the study. All patients underwent comprehensive ocular
examinations, including best-corrected visual acuity, intraocular
pressure, slit lamp biomicroscopy and dilated fundus examinations.
OCT and OCTA images with correct segmentation and without macular
edema and artifacts were included, and those with incorrect
segmentation, masking, black bands, bright lines and distorted
stripes following en face OCTA were excluded. The study was
performed in accordance with the Declaration of Helsinki and with
the approval of the Ethics Committee of Zhongshan Ophthalmic Center
(Guangzhou, China). Informed surgical consent was obtained from
each participant.
OCTA
OCT and OCTA were performed using a spectral domain
system (RTVue-XR Avanti; Optovue), a device with a high speed of
70,000 axial scans per second, using a light source with a
wavelength of 840 nm and with an axial resolution of 5 µm. The
AngioVue OCTA system is based on a split-spectrum amplitude
decorrelation angiography algorithm, using blood flow as an
intrinsic contrast (11). In the
present study, each patient underwent cross-line, retina map and
angio-retinal scanning. All procedures were performed using
RTVue-XR Avanti software (version 2016.2.0.35; Optovue), where the
vessel output of the OCTA algorithm is an image of the retinal and
choroidal vasculature, which may be segmented into four zones: The
superficial capillary plexus, deep capillary plexus, outer retina
and choroid (12).
Assessment of the foveal avascular
zone (FAZ) area and retinal vasculature
In the present study, 3×3-mm macular OCTA scans were
acquired. The FAZ area, foveal and parafoveal vessel densities of
the retinal vasculature, which incorporates the superficial
capillary plexus (SCP) and deep capillary plexus (DCP), were
evaluated using the integrated analytics software of the AngioVue
device. The foveal area was defined as a circle with a 1-mm
diameter, centered on the fovea; the parafoveal area was defined as
an annulus with an outer diameter of 3 mm and an inner diameter of
1 mm centered on the fovea. Furthermore, the parafovea was divided
into four parts: Tempo, superior, nasal and inferior. The foveal
and parafoveal vessel densities were defined as the percentage area
occupied by vessels in the corresponding segmented areas.
Retinal thickness
Retinal thickness was determined using the retinal
map protocol, which calculates the full and inner retinal
thickness. The full retinal thickness was defined as the distance
between the internal limiting membrane and the center of the
retinal pigment epithelial cell (RPE), and the inner retinal
thickness, between the internal limiting membrane and the outer
boundary of the inner plexiform layer. The full and inner retinal
thicknesses of the foveal and parafoveal areas were automatically
calculated using the system's software and were defined as the mean
thicknesses of each area (13).
Statistical analysis
Statistical analyses were performed using SPSS
software version 13 (SPSS Inc.). A paired t-test was used to
compare the capillary vessel densities, FAZ area and retinal
thickness between the baseline and follow-up measurements. The
statistical analyses were two-tailed and P<0.05 was considered
to indicate a statistically significant difference.
Results
Demographic and clinical features
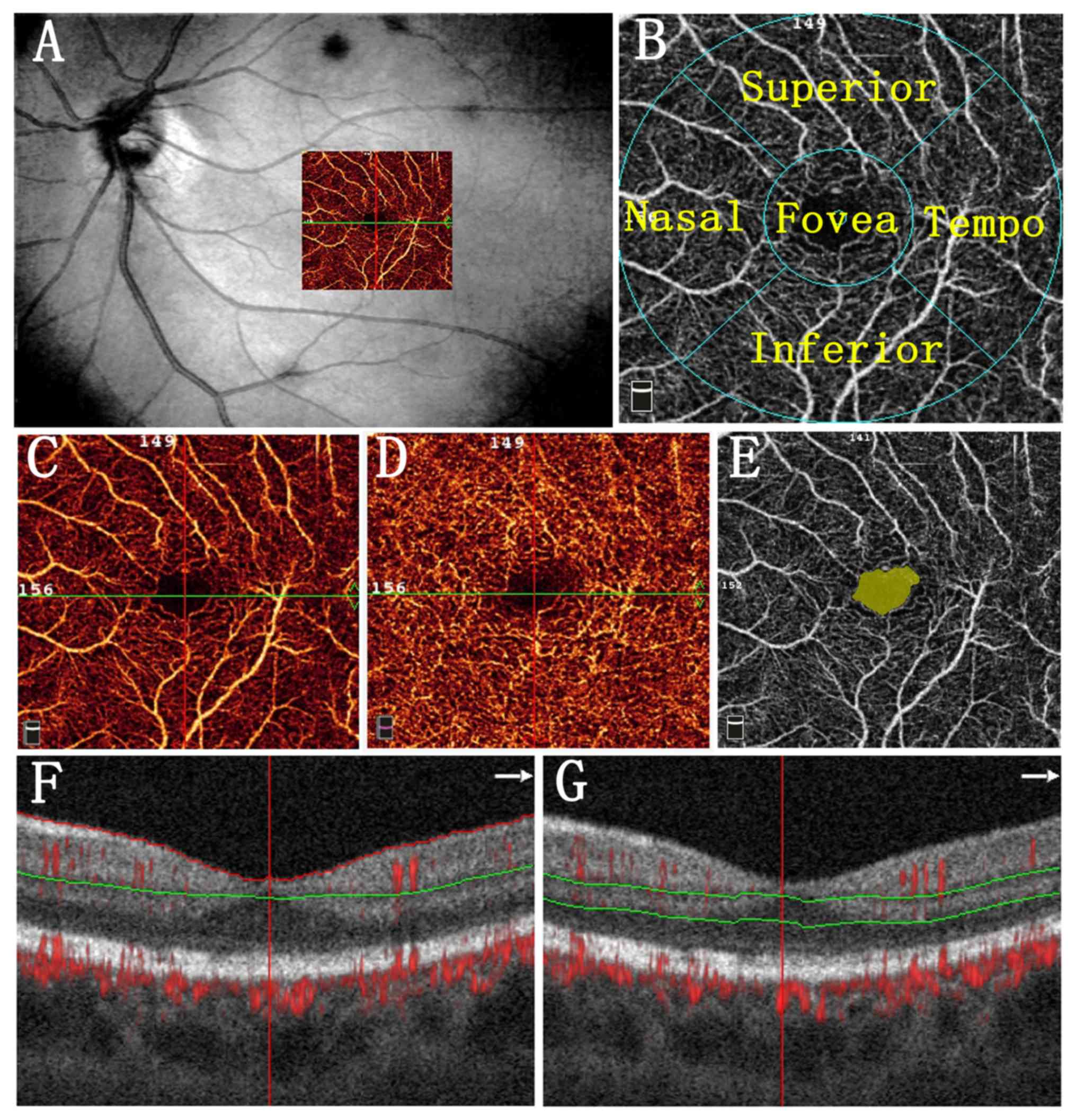
A total of 23 patients who underwent vitreoretinal
surgery with SOT were recruited. The participants in the SOT group
included 17 males and 6 females, and a single eye was assessed in
each participant; the mean age was 46.57±15.64 years (range, 14–67
years). In addition, 20 patients were recruited in the SOR group.
Participants in the SOR group included 15 males and 5 females, with
a mean age of 47.00±16.68 years (range, 8–68 years). The mean
duration of SOT in the SOT group was 5.56±2.17 months. The
demographic and clinical features of the subjects are listed in
Tables I and SI, and representative images of the
retinal capillary density measurement and FAZ area are provided in
Fig. 1.
 | Table I.Demographic data and clinical
characteristics of the subjects. |
Table I.
Demographic data and clinical
characteristics of the subjects.
| Variable | SOT (n=23) | SOR (n=20) |
|---|
| Age (years) | 46.57±15.64 | 47.00±16.68 |
| Pre-operative
BCVA | 0.12±0.21 | 0.08±0.07 |
| Final BCVA | 0.18±0.22 | 0.13±0.16 |
| Eyes with macular-off
RRD | 22 (95.65) | 20 (100) |
| Duration of silicone
oil application (months) | 5.56±2.17 | 7.35±3.07 |
Macular capillary vessel density and
thickness
In reference to the 3×3-mm macular OCTA images, the
mean capillary density of the SCP and DCP, FAZ area and full
retinal thickness remained at a stable level in the SOT (P>0.05)
and SOR (P>0.05) groups. The inferior inner retinal thickness
remained unchanged, whereas the parafoveal (P=0.008), superior-hemi
(P=0.007), temporal (P=0.015), superior (P=0.028) and nasal
(P=0.002) inner retinal thickness was decreased in the SOT group.
Furthermore, the inner retinal thickness was unaltered in the SOR
group (P>0.05; Tables
II–V).
 | Table II.Vessel density of SCP, DCP and area of
FAZ in eyes with silicone oil tamponade. |
Table II.
Vessel density of SCP, DCP and area of
FAZ in eyes with silicone oil tamponade.
| Item | 1st follow-up | 2nd follow-up | P-value |
|---|
| Vessel density of
SCP |
|
Whole | 45.24±4.65 | 43.08±6.22 | 0.15 |
|
Fovea | 24.12±6.43 | 21.94±9.84 | 0.15 |
|
Parafovea | 47.60±5.33 | 45.68±6.97 | 0.24 |
|
Superior-hemi | 47.68±5.55 | 45.96±7.32 | 0.31 |
|
Inferior-hemi | 47.52±5.48 | 45.46±6.88 | 0.22 |
|
Tempo | 46.36±5.73 | 44.79±8.08 | 0.43 |
|
Superior | 47.88±6.28 | 46.37±6.93 | 0.38 |
|
Nasal | 48.39±4.96 | 45.59±7.49 | 0.09 |
|
Inferior | 47.80±6.04 | 46.00±6.57 | 0.27 |
| Vessel density of
DCP |
|
Whole | 49.28±7.10 | 49.87±6.80 | 0.57 |
|
Fovea | 29.15±6.44 | 28.45±7.93 | 0.70 |
|
Parafovea | 51.66±8.11 | 52.44±7.45 | 0.46 |
|
Superior-hemi | 52.39±7.95 | 52.78±7.76 | 0.76 |
|
Inferior-hemi | 50.48±8.36 | 51.67±7.18 | 0.27 |
|
Tempo | 50.61±8.53 | 51.05±7.21 | 0.75 |
|
Superior | 52.98±8.85 | 53.85±8.42 | 0.56 |
|
Nasal | 52.30±7.66 | 52.66±7.65 | 0.79 |
|
Inferior | 50.75±8.98 | 53.55±10.62 | 0.16 |
| FAZ | 0.45±0.26 | 0.45±0.22 | 0.99 |
 | Table V.Retinal thickness in eyes with
silicone oil removal. |
Table V.
Retinal thickness in eyes with
silicone oil removal.
| Item | Pre-Op | Post-Op | P-value |
|---|
| Full retinal
thickness |
|
Fovea | 245.0±47.53 | 247.3±50.92 | 0.70 |
|
Parafovea | 302.7±43.19 | 308.3±44.26 | 0.15 |
|
Superior-hemi | 315.9±72.99 | 320.9±71.75 | 0.33 |
|
Inferior-hemi | 289.3±31.34 | 295.6±37.46 | 0.07 |
|
Tempo | 280.3±50.14 | 286.5±53.52 | 0.11 |
|
Superior | 333.5±89.96 | 334.3±82.47 | 0.90 |
|
Nasal | 311.8±55.77 | 318.9±50.78 | 0.18 |
|
Inferior | 289.7±35.83 | 295.7±41.43 | 0.08 |
| Inner retinal
thickness |
|
Fovea | 71.85±21.50 | 72.60±19.62 | 0.88 |
|
Parafovea | 103.0±14.13 | 105.5±17.25 | 0.40 |
|
Superior-hemi | 104.6±15.83 | 107.8±18.26 | 0.38 |
|
Inferior-hemi | 101.4±15.89 | 103.5±17.83 | 0.48 |
|
Tempo | 96.15±21.12 | 98.80±20.36 | 0.35 |
|
Superior | 106.5±17.98 | 109.7±20.42 | 0.44 |
|
Nasal | 107.0±16.42 | 109.9±18.69 | 0.46 |
|
Inferior | 102.2±17.61 | 103.9±19.83 | 0.61 |
Discussion
In the present study, OCT and OCTA were used to
evaluate the FAZ area, the vessel density of the retinal capillary
plexuses and the retinal thickness in the eyes of patients with
SOT. The results indicated that the FAZ area, SCP and DCP vessel
densities and the full retinal thickness were not altered by SOT or
following SOR. The inner retinal thickness remained stable prior to
and after SOR. However, the parafoveal, temporal, superior and
nasal inner retinal thickness decreased during the SOT period.
Silicone oil has been commonly used to treat complex
cases of vitreoretinal disease. However, opinions on the retinal
effects of silicone oil are inconsistent. A previous study of 500
patients indicated no evidence of toxicity to the retina associated
with the use of silicone oil, even in a number of cases that were
monitored for up to 8 years (14).
However, Ma et al (15)
reported that for the use of silicone oil for periods of <9
months, silicone oil vesicles were observed only on the surface of
the retina, whereas after 9 months, these vesicles began to enter
the sensory layer of the retina. Furthermore, the use of SOT for
>9 months causes alterations to retinal saturation and narrowing
of retinal arterioles, which may further interfere with oxygen
metabolism in the retina; no such changes were observed within a
tamponade period of ≤9 months (16).
In addition, to the best of our knowledge, no
previous studies have addressed the effects of silicone oil on
retinal vessel density in patients. In the present study, a
non-invasive OCTA technique was adopted to detect macular capillary
changes in the eyes of patients with SOT, and no obvious changes in
vessel density in SCP and DCP during SOT or following SOR were
identified. This indicated that silicone oil had no effect on the
retinal vasculature when used for <6 months, suggesting that it
has no significant toxic effect on the retinal vasculature.
Furthermore, the present results were consistent with those of Yang
et al (17), which
demonstrated that SOT in rabbit eyes may not cause any pathological
changes in the retinal vascular or retinal hypoxia over a period of
6 months.
However, the present results appear to contradict
those of previous studies. Kubicka-Trzaska et al (18) assessed macular microcirculatory blood
flow using Doppler laser scanning to demonstrate that silicone oil
may negatively impact the retinal microcirculation as early as 1
month after surgery. In addition, Effert et al (19) measured the arteriovenous passage
times of silicone-oil-filled eyes using a laser scan ophthalmoscope
and reported a prolongation of the arteriovenous passage time in
the silicone-oil-filled eye as compared with that in the
contralateral eye. The above study concluded that silicone oil may
have a negative long-term effect on retinal microcirculation.
However, the two studies mentioned above included a subject group
with unilateral macular-on complex rhegmatogenous retinal
detachment (RRD) and a set of normal contralateral eyes as the
control, which were not directly comparable. As RRD itself may
damage the retinal microcirculation, it was unreasonable to suggest
that silicone oil directly caused a reduction in the macular
microcirculation. In addition, the study focused on retinal blood
flow but not vessel density.
It is known that silicone oil has lower specific
gravity than the aqueous phase of the vitreous; thus, silicone oil
exerts pressure on the retina in the sitting, lateral and prone
positions. Whether this effect affects retinal thickness in the
long-term has so far remained elusive. The present results
demonstrated that, the inferior inner retinal thickness remained
unchanged, whilst the parafoveal, temporal, superior and nasal
inner retinal thickness were decreased in eyes with SOT, which
implies that silicone oil may compress the inner retina and
decrease the inner retinal thickness. However, this requires
further investigation.
As the present study had a retrospective design, not
all patients regularly visited our hospital following surgery.
Thus, the present study was limited to a relatively small number of
subjects. Therefore, 23 patients in the SOT group and 20 in the SOR
group were assessed separately, rather than as a single group of
patients who underwent SOT and subsequent SOR. However, further
prospective studies with a larger sample size should be
performed.
In conclusion, the present results demonstrate that
the use of silicone oil for <6 months has no significant effect
on macular capillary vessel density. However, reduced inner retinal
thickness in eyes with SOT was also demonstrated. Therefore, it is
recommended that silicone oil is removed as soon as possible once
the ocular disease is stable. Whether silicone oil irreversibly
affects retinal thickness requires assessment in a prospective
study with an increased sample size.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The current study was supported by the National
Natural Science Foundation of China (grant no. 81700817).
Availability of data and materials
The datasets used and/or analyzed in the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
WX drafted the manuscript. ZZ, LZ and RL acquired
the data. SZ was responsible for the treatment of the patients. WX,
YW and WC analyzed the data and revised the manuscript. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Zhongshan Ophthalmic Center (Guangzhou, China). Informed consent
was obtained from each participant.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cibis PA, Becker B, Okun E and Canaan S:
The use of liquid silicone in retinal detachment surgery. Arch
Ophthalmol. 68:590–599. 1962. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pastor JC: Proliferative
vitreoretinopathy: An overview. Surv Ophthalmol. 43:3–18. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Azen SP, Scott IU, Flynn HJ Jr, Lai MY,
Topping TM, Benati L, Trask DK and Rogus LA: Silicone oil in the
repair of complex retinal detachments. A prospective observational
multicenter study. Ophthalmology. 105:1587–1597. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ortisi E, Avitabile T and Bonfiglio V:
Surgical management of retinal detachment because of macular hole
in highly myopic eyes. Retina. 32:1704–1718. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wei Y, Li Y and Chen F: Vitrectomy
treatment of retinal detachments related to choroidal coloboma
involving the disk. Retina. 34:1091–1095. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kapur R, Birnbaum AD, Goldstein DA,
Tessler HH, Shapiro MJ, Ulanski LJ and Blair MP: Treating
uveitis-associated hypotony with pars plana vitrectomy and silicone
oil injection. Retina. 30:140–145. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Toklu Y, Cakmak HB, Ergun SB, Yorgun MA
and Simsek S: Time course of silicone oil emulsification. Retina.
32:2039–2044. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kampik A and Gandorfer A: Silicone oil
removal strategies. Semin Ophthalmol. 15:88–91. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jia Y, Morrison JC, Tokayer J, Tan O,
Lombardi L, Baumann B, Lu CD, Choi W, Fujimoto JG and Huang D:
Quantitative OCT angiography of optic nerve head blood flow. Biomed
Opt Express. 3:3127–3137. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jia Y, Bailey ST, Wilson DJ, Tan O, Klein
ML, Flaxel CJ, Potsaid B, Liu JJ, Lu CD, Kraus MF, et al:
Quantitative optical coherence tomography angiography of choroidal
neovascularization in age-related macular degeneration.
Ophthalmology. 21:1435–1444. 2014. View Article : Google Scholar
|
|
11
|
Jia Y, Tan O, Tokayer J, Potsaid B, Wang
Y, Liu JJ, Kraus MF, Subhash H, Fujimoto JG, Hornegger J and Huang
D: Split-spectrum amplitude-decorrelation angiography with optical
coherence tomography. Opt Express. 20:4710–4725. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Koustenis A Jr, Harris A, Gross J,
Januleviciene I, Shah A and Siesky B: Optical coherence tomography
angiography: An overview of the technology and an assessment of
applications for clinical research. Brit J Ophthalmol. 101:16–20.
2017. View Article : Google Scholar
|
|
13
|
Yu J, Xiao K, Huang J, Sun X and Jiang C:
Reduced retinal vessel density in obstructive sleep apnea syndrome
patients: An optical coherence tomography angiography study. Invest
Ophth Vis Sci. 58:3506–3512. 2017. View Article : Google Scholar
|
|
14
|
Lucke K and Laqua H: Visual outcome after
silicon oil surgery. Fortschr Ophthalmol. 88:603–607. 1991.(In
German). PubMed/NCBI
|
|
15
|
Gisbert R, Ulrich S and Alexander AB:
Pathological changes of occular tissue after solicone oil filling.
Chin J Ocular Fundus Dis. 35–37. 1999.
|
|
16
|
Lou B, Yuan Z, He L, Lin L, Gao Q and Lin
X: The changes of retinal saturation after long-term tamponade with
silicone oil. Biomed Res Int. 2015:7138282015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yang W, Yuan Y, Zong Y, Huang Z, Mai S, Li
Y, Qian X, Liu Y and Gao Q: Preliminary study on retinal vascular
and oxygen-related changes after long-term silicone oil and
foldable capsular vitreous body tamponade. Sci Rep. 4:52722014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kubicka-Trzaska A, Kobylarz J and
Romanowska-Dixon B: Macular microcirculation blood flow after pars
plana vitrectomy with silicone oil tamponade. Klin Oczna.
113:146–148. 2011.PubMed/NCBI
|
|
19
|
Effert R, Wolf S, Arend O, Schulte K and
Reim M: Retinal hemodynamics after pars plana vitrectomy with
silicone oil tamponade. Ger J Ophthalmol. 3:65–67. 1994.PubMed/NCBI
|