Introduction
Metabolic syndrome (MetS) is a clinical syndrome
characterized by several associated risk factors for cardiovascular
diseases and diabetes, including obesity, hypertension, elevated
blood glucose and dyslipidemia (1).
Epidemiological data suggest that in Chinese populations, the
prevalence of MetS has exhibited a rapid increase in recent years
(2). Preventing MetS by controlling
relevant risk factors is a crucial and urgent task for the National
Health Commission of the People's Republic of China.
Sleep deficiency has become prevalent in modern
society, and it has been proven that chronic sleep deprivation may
interrupt numerous essential homeostatic mechanisms. Various
studies have demonstrated that short sleep duration is associated
with the prevalence of various cardiovascular and metabolic
diseases, including hypertension, coronary heart disease and
diabetes (3–5). However, as to the potential association
of sleep duration and the prevalence of MetS, no consistent
conclusion has been reached so far. Certain previous studies have
reported a U-shaped association between sleep duration and MetS
(6,7). However, this conflicted with other
studies, which demonstrated that a short rather than long sleep
duration was associated with a higher risk of MetS (3,8). In
addition, certain studies indicated that individuals with long
sleep duration were predisposed to MetS (9,10). To
date, the potential association of sleep duration with the
prevalence of MetS has remained to be clarified.
However, the evaluation of sleep has qualitative and
quantitative aspects. Perhaps it is not comprehensive to measure
sleep by sleep duration only. Recently, the role of sleep quality
in the development of cardiometabolic diseases has raised concern
among cardiologists (11). Certain
studies have demonstrated that poor sleep quality may contribute to
the development of MetS (12,13).
Furthermore, certain studies have attempted to explore the
interactive effects of sleep duration and sleep quality on certain
components of MetS, including abnormal glucose control and high
blood pressure, and an additive effect of insufficient sleep
duration and quality was identified (14,15). It
is therefore necessary to elucidate the potential association of
sleep duration with the prevalence of MetS while including the
possible confounding effect of sleep quality.
The present cross-sectional survey aimed to explore
the potential association of self-reported sleep duration and
quality with the prevalence of MetS in adult Chinese males. In
addition, the separate and combined effects of sleep duration and
sleep quality on the prevalence of MetS were analyzed.
Materials and methods
Study design and population
This study was designed as a cross-sectional study.
A total of 6,120 participants aged >18 years residing in the
Fangezhuang, Tangshan, Lvjiatuo and Qianjiaying communities of
Tangshan city located in North China were enrolled in the study
between September 2013 and December 2013, and the data was
collected and analyzed at Kailuan General Hospital (Tangshan,
Hebei, China). Participants with obstructive sleep apnea syndrome
(OSAS), restless legs syndrome (RLS) or snoring were excluded due
to their complex mechanistic association with hypertension, which
was difficult to measure and control. Most participants were
employees of the Kailuan Group, a large-scale comprehensive
enterprise that mainly manages coal products, where female
employees make up a small proportion. Only 571 female participants
were initially enrolled and the sample size was too small to be
analyzed to accomplish the aim of the study; therefore, only the
results of the association of sleep with MetS in male participants
are included. All study protocols were approved by the Ethics
Committee of Kailuan General Hospital [Tangshan, Hebei, China;
approval reference no. 2013(5)] and written informed consent was
obtained from all study participants.
Anthropometric measurements
Anthropometric measurements were performed on
participants wearing light clothes but no shoes. The waist
circumference was measured with participants standing up straight
at the navel level as participants exhaled lightly. Body height was
measured to the nearest 0.1 cm and weight was measured to the
nearest 0.1 kg. Using a calibrated standard mercury
sphygmomanometer (Yuyue Medical Equipment & Supply Co., Ltd.),
blood pressure was measured twice in a sitting position and the
mean reading was recorded. If the difference between two readings
was >5 mmHg, a third reading was taken and the mean of the three
readings was used.
Blood test
Participants were requested to fast overnight prior
to the collection of a venous blood sample. Serum was prepared by
centrifuging the blood at 500 × g for 10 min at 4°C within 4 h of
collection. Serum triglyceride, high-density lipoprotein
cholesterol (HDL-C) and fasting blood glucose were measured using
an automatic biochemical analyzer (Hitachi 717; Hitachi).
Questionnaire survey
All participants were subjected to a structured
questionnaire including age, history of diagnosed hypertension and
type 2 diabetes and/or receiving of hypertension and diabetes
medication, smoking status, drinking status, educational level,
physical activity, sleep duration and sleep quality. Details
regarding the definition as well as the classification of certain
items listed above were identical to those of a previous study by
our group (14). Sleep duration was
evaluated based on self-reported average sleep duration in the past
month, which precluded the time spent awake in bed. Sleep duration
was categorized into 5 groups, ‘<6’, ‘6’, ‘7’, ‘8’ and ‘>8
h’, as stated in the questionnaire. Sleep quality was assessed
using the standard Pittsburgh Sleep Quality Index (PSQI; Table SI) (16). The PSQI is a 19-item self-reporting
measure of sleep quality over the past month and contains 7
component scales: Sleep quality, sleep latency, sleep duration,
sleep efficiency, sleep disturbances, use of sleep medication and
daytime dysfunction. The global PSQI score may vary within a range
of 0–21. In the present study, sleep quality of participants was
classified into four groups: ‘Very good’ (PSQI of <3), ‘good’
(PSQI of 3 to <6), ‘poor’ (PSQI of 6 to <9) and ‘very poor’
(PSQI ≥9). In addition, the General Anxiety Disorder-7 (GAD-7) and
Patient Health Questionnaire-9 (PHQ-9) scales were used to evaluate
the anxiety and depression status of participants, respectively.
GAD-7 is a seven-question inventory for self-assessment and is one
of the most common instruments for measuring severity of anxiety
(17). PHQ-9 is a widely used
nine-question inventory for the self-assessment of depression
(18).
Definition of MetS
According to the definition of MetS issued in the
Dyslipidemia Prevention and Cure Guidelines of China in 2007
(19), MetS was diagnosed when any
three or more of the following five risk factors were present: i)
Abdominal obesity: Waist circumference ≥90 cm for males, ≥85 cm for
females; ii) elevated blood glucose: Fasting blood glucose ≥6.l
mmol/l or 2-h post-prandial plasma glucose ≥7.8 mmol/l and/or with
diagnosed diabetes and current use of anti-diabetic therapy; iii)
hypertension: Blood pressure ≥130/85 mmHg and/or with diagnosed
hypertension and iv) fasting HDL-C<l.04 mmol/l.
Statistical analysis
In the present study, continuous variables were
expressed as mean ± SE and compared using one-way analysis of
variance followed by Dunnett's post-hoc test. Categorical variables
were expressed as n (%) and compared using the χ2 test.
Cochran-Armitage tests were used to test the association between
the prevalence of MetS and sleep duration/quality. The potential
correlation between sleep duration and sleep quality with the
prevalence of MetS was explored by logistic regression analysis
with or without adjustment for plausible confounders, including
age, smoking status, drinking status, physical activity,
educational level, and anxiety and depression scores. Furthermore,
to investigate the interactive association of sleep duration and
sleep quality with the prevalence of MetS, participants were
divided into groups according to different combinations of sleep
duration and sleep quality. Odds ratios (ORs) and 95% CIs of each
group were calculated using multiple logistic regression analysis,
with the group with a sleep duration of 7 h and very good sleep
quality used as the reference. For all comparisons, the level of
statistical significance was set at P<0.05 (two-sided). SPSS
19.0 (IBM Corp.) was used for all statistical analyses.
Results
Basic characteristics
Of the 6,120 initially enrolled participants, 351
(5.7%) were diagnosed with OSAS, 43 (0.7%) with RLS, 1,011 (16.5%)
reported snoring and the 571 females (9.3%) were excluded. The
remaining 4,144 males were included into the final analysis.
Participants with <6, 6, 7, 8 and >8 h of sleep accounted for
8.6% (n=356), 24.6% (n=1,021), 34.9% (n=1,446), 26.1% (n=1,082) and
5.8% (n=239) of the cohort, respectively. With regard to sleep
quality, the participants with sleep quality rated as very good,
good, poor and very poor accounted for 57.2% (n=2,369), 27.7%
(n=1,146), 11.3% (n=468) and 4.6% (n=191) of the cohort,
respectively (Tables I and II).
 | Table I.Basic characteristics of adult Chinese
male participants according to sleep duration. |
Table I.
Basic characteristics of adult Chinese
male participants according to sleep duration.
|
| Sleep duration
(h) |
|---|
|
|
|
|---|
| Item | <6 (n=356) | 6 (n=1,021) | 7 (n=1,446) | 8 (n=1,082) | >8 (n=239) | Total (n=4,144) | P-value |
|---|
| Age (years) | 47.91±0.37 | 46.84±0.23 | 46.92±0.18 | 46.98±0.41 | 47.47±0.42 | 47.04±0.14 | 0.33 |
| WC (cm) | 91.73±6.02 | 88.71±4.11 | 88.78±4.10 | 89.03±4.37 | 91.27±5.68 | 88.94±4.21) | <0.01 |
| BMI
(kg/m2) | 25.45±0.19 | 25.17±0.11 | 25.44±0.10 | 25.19±0.10 | 25.05±0.19 | 25.28±0.06 | 0.16 |
| SBP (mmHg) | 130.61±0.71 | 129.79±0.47 | 129.96±0.38 | 129.62±0.44 | 131.84±0.81 | 130.02±0.22 | 0.18 |
| DBP (mmHg) | 85.87±0.47 | 85.9±0.31 | 85.80±0.25 | 85.71±0.30 | 86.86±0.55 | 85.88±0.15 | 0.50 |
| TG (mmol/l) | 2.03±0.12 | 1.95±0.03 | 1.84±0.06 | 1.89±0.07 | 1.95±0.12 | 1.90±0.04 | 0.07 |
| HDL-C (mmol/l) | 1.33±0.02 | 1.34±0.02 | 1.34±0.01 | 1.35±0.01 | 1.37±0.02 | 1.33±0.01 | 0.53 |
| FBG (mmol/l) | 5.57±0.08 | 5.41±0.05 | 5.43±0.0 | 5.5±0.05 | 5.29±0.07 | 5.45±0.02 | 0.08 |
| Previous
hypertension | 72 (20.2) | 157 (15.4) | 201 (13.9) | 120 (11.1) | 34 (14.3) | 584 (14.1) | <0.01 |
| Previous
diabetes | 52 (14.6) | 85 (8.3) | 103 (7.1) | 80 (7.4) | 24 (10.2) | 344 (8.3) | <0.01 |
| GAD-7 score | 4.40±0.28 | 3.35±0.15 | 1.63±0.08 | 1.51±0.09 | 1.93±0.30 | 2.27±0.06 | <0.01 |
| PHQ-9 score | 5.06±0.32 | 3.29±0.16 | 2.02±0.10 | 1.63±0.10 | 2.25±0.32 | 2.48±0.07 | <0.01 |
| Current
smoking | 215 (60.5) | 611 (59.8) | 781 (54.0) | 576 (53.2) | 133 (55.8) | 2316 (55.9) | <0.01 |
| Current
drinking | 115 (32.2) | 289 (28.3) | 320 (22.1) | 285 (26.2) | 62 (25.9) | 1071 (25.8) | <0.01 |
| Active exercise
habit | 109 (30.6) | 311 (30.5) | 508 (35.1) | 392 (36.2) | 59 (24.6) | 1379 (33.3) | <0.01 |
| High level of
education | 140 (39.4) | 415 (40.6) | 450 (31.1) | 413 (38.2) | 92 (38.7) | 1510 (36.4) | <0.01 |
 | Table II.Basic characteristics of adult
Chinese male participants according to sleep quality. |
Table II.
Basic characteristics of adult
Chinese male participants according to sleep quality.
|
| Sleep quality |
|---|
|
|
|
|---|
| Item | Very good
(n=2,369) | Good (n=1,146) | Poor (n=468) | Very poor
(n=191) | Total
(n=4,144) | P-value |
|---|
| Age (years) |
47.20±0.14 |
46.38±0.40 |
47.48±0.36 |
47.34±0.52 |
47.01±0.14 | 0.06 |
| WC (cm) |
88.72±4.19 |
89.21±4.11 |
90.41±5.13 |
92.01±5.73 |
88.94±4.21 | <0.01 |
| BMI
(kg/m2) |
25.26±0.08 |
25.33±0.11 |
25.41±0.18 |
25.01±0.23 |
25.29±0.06 | 0.58 |
| SBP (mmHg) | 130.53±0.30 | 129.16±0.42 |
130.16±0.69 | 128.32±1.04 | 130.01±0.23 | 0.02 |
| DBP (mmHg) |
86.24±0.20 |
85.32±0.28 |
85.69±0.48 | 85.38±0.7 |
85.89±0.15 | 0.05 |
| TC (mmol/l) |
2.02±0.03 |
1.94±0.09 |
1.89±0.12 |
2.01±0.12 |
1.90±0.04 | 0.09 |
| HDL-C (mmol/l) |
1.36±0.03 |
1.29±0.02 |
1.26±0.02 |
1.27±0.03 |
1.34±0.02 | 0.19 |
| FBG (mmol/l) |
5.47±0.03 |
5.44±0.05 |
5.38±0.06 |
5.42±0.10 |
5.45±0.02 | 0.68 |
| Previous
hypertension | 296
(12.5) | 170 (14.8) | 74 (15.8) | 44 (23.0) | 584
(14.1) | <0.01 |
| Previous
diabetes | 173
(7.3) | 93 (8.1) | 48 (10.3) | 30 (15.7) | 344
(8.3) | <0.01 |
| GAD-7 score |
1.15±0.06 |
3.06±0.12 |
4.54±0.26 |
6.4±0.43 |
2.27±0.06 | <0.01 |
| PHQ-9 score |
1.21±0.06 |
3.54±0.13 |
4.60±0.26 |
7.9±0.53 |
2.48±0.07 | <0.01 |
| Current
smoking | 1,279 (54.0) | 662 (57.8) | 256 (54.7) | 119 (62.2) | 2,316 (55.9) | 0.04 |
| Current
drinking | 572
(24.1) | 289 (25.2) | 132 (28.3) | 78
(40.8) | 1,071 (25.8) | <0.01 |
| Active exercise
habit | 785
(33.1) | 416 (36.3) | 126 (26.9) | 52
(27.2) | 1,379 (33.3) | <0.01 |
| High level of
education | 811
(34.2) | 452 (39.4) | 162 (34.7) | 85
(44.4) | 1,510 (36.4) | <0.01 |
Prevalence of MetS
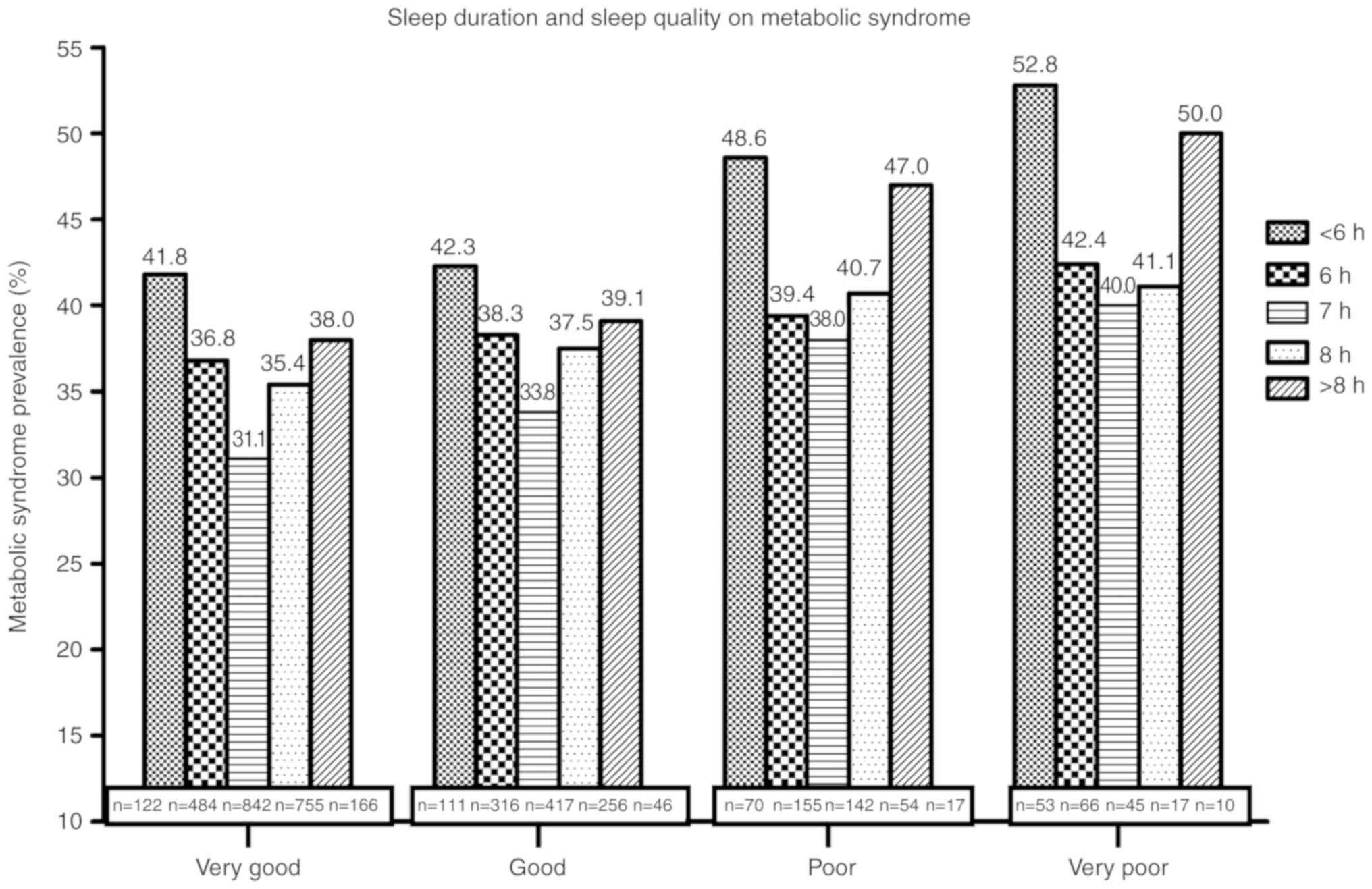
The prevalence of MetS in participants with
different sleep duration or quality is provided in Fig. 1. The participants with a sleep
duration of 7 h and sleep quality rated as very good had the lowest
prevalence of MetS. Compared to participants with a sleep duration
of 7 h, those with a shorter and longer sleep duration were
indicated to have a higher prevalence of MetS, and a U-shaped
association between sleep duration and the prevalence of MetS was
observed. This trend was statistically significant (P<0.05). As
for sleep quality, participants with poorer sleep quality were
observed to have a higher prevalence of MetS as compared with those
with very good sleep quality (P<0.05).
Association of sleep duration or sleep
quality with the prevalence of MetS
Multivariate logistic regression analysis was used
to explore the potential association of sleep duration or sleep
quality with the prevalence of MetS. After adjustment for age,
smoking, drinking, exercise, education level, anxiety scores and
depression scores, compared with participants with 7 h of sleep,
the ORs and 95% Cis for MetS of those with <6, 6, 8 and >8 h
of sleep were 1.57 (95% CI, 1.26–1.95), 1.26 (95% CI, 1.14–1.39),
1.21 (95% CI, 1.11–1.32) and 1.32 (95% CI, 1.06–1.65),
respectively. Furthermore, compared with the group with very good
sleep quality, the ORs and 95% CIs for MetS in patients with good,
poor and very poor sleep quality were 1.12 (95% CI, 1.01–1.23),
1.20 (95% CI, 1.02–1.40) and 1.51 (95% CI, 1.21–1.88), respectively
(Table III).
 | Table III.Logistic regression analysis of the
influence of sleep duration and sleep quality on the prevalence of
metabolic syndrome in adult Chinese males. |
Table III.
Logistic regression analysis of the
influence of sleep duration and sleep quality on the prevalence of
metabolic syndrome in adult Chinese males.
| A, Influence of
sleep duration |
|---|
|
|---|
| Sleep duration
(h) | n | Unadjusted OR
(95%CI) | P-value | Adjusted OR
(95%CI)a | P-value |
|---|
| <6 | 356 | 1.55
(1.23–1.92) | – | 1.57
(1.26–1.95) | – |
| 6 | 1,021 | 1.23
(1.12–1.36) | <0.00 | 1.26
(1.14–1.39) | <0.00 |
| 7 | 1,446 | Reference | – | Reference | – |
| 8 | 1,082 | 1.24
(1.13–1.35) | <0.00 | 1.21
(1.11–1.32) | <0.00 |
| >8 | 239 | 1.29
(1.03–1.60) | P-value | 1.32
(1.06–1.65) | P-value |
|
| B, Influence of
sleep quality |
|
| Sleep duration
(h) | n | Unadjusted OR
(95%CI) | P-value | Adjusted OR
(95%CI)a | P-value |
|
| Very good | 2,369 | Reference | – | Reference | – |
| Good | 1,146 | 1.15
(1.02–1.30) | <0.00 | 1.12
(1.01–1.23) | <0.00 |
| Poor | 438 | 1.21
(1.03–1.42) | <0.00 | 1.20
(1.02–1.40) | <0.00 |
| Very poor | 191 | 1.53
(1.23–1.92) | <0.00 | 1.51
(1.21–1.88) | <0.00 |
Association of combined sleep duration
and sleep quality with the prevalence of MetS
The association of the combined effects of sleep
duration and quality on MetS was analyzed by univariate and
multivariate logistic regression analysis (Table IV). Compared with participants with
7 h sleep duration and very good sleep quality (used as the
reference), those in all other groups were observed to have a
higher prevalence of MetS after adjusting for potential confounding
factors. The ORs as well as their 95% CIs for each group are stated
below, indicating an obvious additive effect of inadequate sleep
duration and quality on the prevalence of MetS: Sleep duration of
<6 h combined with any sleep quality [1.52 (1.23–1.88) for very
good; 1.64 (1.30–1.86) for good; 2.25 (1.60–3.03) for poor and very
poor], sleep duration of 6 h combined with any sleep quality [1.24
(1.14–1.36) for very good; 1.33 (1.13–1.52) for good; 1.49
(1.21–1.67) for poor and very poor], 7 h sleep duration combined
with any sleep quality [1.17 (1.05–1.31) for good; 1.34 (1.09–1.63)
for poor and very poor], sleep duration of 8 h combined with any
sleep quality [1.25 (1.12–1.39) for very good; 1.30 (1.15–1.46) for
good; 1.52 (1.22–1.93) for poor and very poor], and sleep duration
of >8 h combined with any sleep quality [1.37 (1.11–1.67) for
very good; 1.39 (1.13–1.73) for good; 2.03 (1.45–2.86) for poor and
very poor].
 | Table IV.Logistic regression analysis of the
influence of different combinations of sleep duration and quality
on the prevalence of metabolic syndrome in adult Chinese males. |
Table IV.
Logistic regression analysis of the
influence of different combinations of sleep duration and quality
on the prevalence of metabolic syndrome in adult Chinese males.
| A, Unadjusted
analysis |
|---|
|
|---|
|
|
Sleep
duration (h) |
|---|
|
|
|
|---|
|
| <6 | 6 | 7 | 8 | >8 |
|---|
|
|
|
|
|
|
|
|---|
| Sleep quality | n | OR (95% CI) | n | OR (95% CI) | n | OR (95% CI) | n | OR (95% CI) | n | OR (95% CI) |
|---|
| Very good | 122 | 1.54
(1.25–1.90)b | 484 | 1.27
(1.16–1.39)b | 842 | Reference | 755 | 1.23
(0.11–1.38)d | 166 | 1.34
(1.10–1.63)c |
| Good | 111 | 1.62
(1.28–1.84)b | 316 | 1.36
(1.15–1.55)b | 417 | 1.16
(1.05–1.30)c | 256 | 1.32
(1.17–1.50)b | 46 | 1.41
(1.14–1.75)b |
| Poor and very
poor | 123 | 2.21
(1.62–3.06)b | 221 | 1.47
(1.20–1.65)b | 187 | 1.38
(1.13–1.68)b | 71 | 1.50
(1.21–1.90)b | 27 | 1.98
(1.40–2.78)b |
|
| B, Adjusted
analysisa |
|
| Sleep
quality | n | OR (95%
CI) | n | OR (95%
CI) | n | OR (95%
CI) | n | OR (95%
CI) | n | OR (95%
CI) |
|
| Very good | 122 | 1.52
(1.23–1.88)b | 484 | 1.24
(1.14–1.36)b | 842 | Reference | 755 | 1.25
(1.12–1.39)b | 166 | 1.37
(1.11–1.67)c |
| Good | 111 | 1.64
(1.30–1.86)b | 316 | 1.33
(1.13–1.52)c | 417 | 1.17
(1.05–1.31)c | 256 | 1.30
(1.15–1.46)b | 46 | 1.39
(1.13–1.73)c |
| Poor and very
poor | 123 | 2.25
(1.60–3.03)b | 221 | 1.49
(1.21–1.67)b | 187 | 1.34
(1.09–1.63)c | 71 | 1.52
(1.22–1.93)b | 27 | 2.03
(1.45–2.86)b |
Discussion
In the present study on adult Chinese males, a
U-shaped association between sleep duration and the prevalence of
MetS was observed and it was also noted that poor sleep quality was
associated with a high prevalence of MetS. Furthermore, the
combined effects of sleep duration and sleep quality on the
prevalence of MetS in the study population were explored and the
results indicated an additive effect of inadequate sleep duration
and sleep quality on the prevalence of MetS.
A U-shaped association between sleep duration and
MetS was observed in the present study. This result was consistent
with those of previous studies (6,7).
However, the studies of Wu et al (3) and Najafian et al (20), which indicated that a short rather
than long sleep duration increased the risk of MetS, were not in
accordance with the present results. Apart from differences in age,
ethnicity and basic characteristics, negligence of the confounding
effect of sleep quality is one of the important potential reasons
for the conflicting results mentioned above. Sleep has quantitative
as well as qualitative aspects. Sleep duration is not the only
criterion for determining the presence of sleep deficiency.
Therefore, it may not be sufficient to evaluate sleep only based on
sleep duration, which was performed in most previous studies on the
potential association between sleep and the prevalence of MetS
(3,6–10).
Failure to assess sleep comprehensively may be the most important
reason for the conflicting results among those previous
studies.
The present study indicated that poor sleep quality
was associated with MetS, which was consistent with the results of
previous studies (12,13). Kazman et al (21) also assessed the sleep quality by
using the PSQI, but failed to observe an association between poor
sleep quality and the prevalence of MetS among African Americans.
Sociodemographic factors, health behaviors and socioeconomic status
have already been proven to be linked to MetS and sleep (3,10,22,23).
However, health-associated behaviors (e.g., smoking, drinking and
exercise) and socioeconomic status were not considered and adjusted
for in the study by Kazman et al (21), which may explain the discrepancies
between the previous study by Kazman et al and the present
study. It has been reported that poor mental health status,
including depression or anxiety, may increase the risk of MetS
(24,25), and sleep disorders are also
frequently concomitant in patients with depression and anxiety
(26). Therefore, whether poor
mental and emotional health are independent risk factors of MetS or
whether sleep disorders mediate the association of mental/emotional
health with the development of MetS has not been confirmed.
However, this was neglected in most previous studies. In the
present study, the depression and anxiety status of all
participants was evaluated by using the PHQ-9 and GAD-7 scales and
adjustment for these parameters was included in the logistic
regression analysis for the influence of sleep on MetS.
As mentioned above, it is preferable to consider and
measure sleep duration as well as quality when exploring the
potential association of sleep with MetS. To elucidate the exact
effect of combined sleep duration and quality on MetS, the
influence of different combinations of sleep duration and sleep
quality on the prevalence of MetS was investigated in the present
study. The results suggest that in spite of long sleep duration,
such as 8 h or more, there was still a high prevalence of MetS in
those participants with poor sleep quality, suggesting that sleep
duration and sleep quality had a combined effect on the prevalence
of MetS. Evaluation of sleep based on either sleep quality or
quantity on its own may inevitably lead to bias of the results,
which should be considered in future studies on the link between
sleep and diseases.
The mechanisms underlying the association between
sleep and MetS remain to be fully elucidated. It has been indicated
that short sleep duration affects the levels of endocrine hormones,
including leptin and ghrelin, finally resulting in increased
appetite and obesity (27). A recent
study performed on Chinese children suggested a strong link between
short sleep duration and adverse adipokine secretion patterns
(28). Lusardi et al
(29) reported that sleep
deprivation was associated with sympathetic hyperactivity and
elevated blood pressure. Insulin resistance, which is a key factor
in the development of MetS, was also suggested to be associated
with short sleep duration (30).
Furthermore, long sleep duration was observed to increase the risk
of MetS components. Long sleep duration may be associated with
obesity due to a decline in activity levels and energy consumption
(7). It was also reported that
people getting a sufficient sleep duration had lower levels of
inflammation and oxidative stress and higher levels of
anti-oxidants compared with short or long sleepers (31). From the above, it is obvious that
further studies are required to elucidate the potential link
between sleep disorders and MetS.
The present study has several limitations. First of
all, it was difficult to assess the causal association between
sleep status and the prevalence of MetS due to the cross-sectional
design of the study. It is likely that sleep disorders are
associated with an increased risk of MetS, considering the fact
that certain cohort studies have confirmed that sleep disorders
area major cause of hypertension and diabetes, which are components
of MetS (5,32). Furthermore, self-reported sleep
duration may not represent real sleep duration. However, Signal
et al (33) indicated that
self-reported sleep duration was close to the polysomnography
result. In addition, the 2-h post-prandial blood glucose of the
enrolled participants was not measured in the present study due to
limited time and funding. This may have led to underestimation of
the number of participants with impaired glucose metabolism,
considering the fact that a sizeable proportion of the Chinese
diabetic population presents with normal fasting blood glucose
(34).
Despite the limitations mentioned above, the present
study indicated a U-shaped association between sleep duration and
MetS and indicated that poor sleep quality was associated with an
elevated prevalence of MetS in male Chinese adults. Furthermore,
the study also revealed that inadequate sleep duration and sleep
quality have an additive effect on the prevalence of MetS, which
was the most important result. This indicated that sleep duration
as well as quality should be measured to avoid a biased result when
exploring the potential association of sleep with cardiometabolic
diseases.
Supplementary Material
Supporting Data
Acknowledgements
The authors thank the staff of Kailuan Study for
their efforts in data collection. Additionally, the authors express
their gratitude to Mrs. Mele Vaikoloa Fonua, Graduate College of
Chongqing Medical University, China, for her work to improve the
language and style of the manuscript.
Funding
This study was funded by grants from the 12th
Five-Year Science and Technology Support Program of the Ministry of
Science and Technology of China (grant no. 2013BAI06B02).
Availability of data and materials
The datasets generated and/or analyzed during the
current study are not publicly available due to the present study
being one part of the 12th Five-Year Science and Technology Support
Program of the Ministry of Science and Technology of China (grant
no. 2013BAI06B02) which has not finished officially. As such, the
relevant raw data can not be made freely available to any
researchers at this current time. However, any researchers who wish
to use them for non-commercial purposes whilst preserving the
necessary confidentiality can contact the corresponding author and
the data are available from the corresponding author on reasonable
request.
Authors' contributions
DH and HX developed the idea for the study and
carried out the design with all co-authors. KL is responsible for
the recruitment and follow-up of study participants as well as data
collection. JC carried out the analysis. YZ participated in the
analysis and drafted the manuscript which was revised by all
authors. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
All study protocols were approved by the Ethics
Committee of Kailuan General Hospital (Tangshan, Hebei, China).
Written informed consent for publication was obtained from all
study participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mamcarz A, Podolec P, Kopeć G, Czarnecka
D, Rynkiewicz A, Stańczyk J, Undas A, Godycki-Cwirko M, Kozek E,
Pajak A, et al: Polish forum for prevention guidelines on metabolic
syndrome. Kardiol Pol. 68:121–124. 2010.PubMed/NCBI
|
|
2
|
Shen J, Goyal A and Sperling L: The
emerging epidemic of obesity, diabetes, and the metabolic syndrome
in china. Cardiol Res Pract. 2012:1786752012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wu MC, Yang YC, Wu JS, Wang RH, Lu FH and
Chang CJ: Short sleep duration associated with a higher prevalence
of metabolic syndrome in an apparently healthy population. Prev
Med. 55:305–309. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Katano S, Nakamura Y, Nakamura A, Murakami
Y, Tanaka T, Takebayashi T, Okayama A, Miura K, Okamura T and
Ueshima H; HIPOP-OHP Research Group, : Relationship between sleep
duration and clustering of metabolic syndrome diagnostic
components. Diabetes Metab Syndr Obes. 4:119–125. 2011.PubMed/NCBI
|
|
5
|
Gangwisch JE, Heymsfield SB, Boden-Albala
B, Buijs RM, Kreier F, Pickering TG, Rundle AG, Zammit GK and
Malaspina D: Short sleep duration as a risk factor for
hypertension: Analyses of the first National Health and Nutrition
Examination Survey. Hypertension. 47:833–839. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ju SY and Choi WS: Sleep duration and
metabolic syndrome in adult populations: A meta-analysis of
observational studies. Nutr Diabetes. 3:e652013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Choi KM, Lee JS, Park HS, Baik SH, Choi DS
and Kim SM: Relationship between sleep duration and the metabolic
syndrome: Korean National Health and Nutrition Survey 2001. Int J
Obes (Lond). 32:1091–1097. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Xi B, He D, Zhang M, Xue J and Zhou D:
Short sleep duration predicts risk of metabolic syndrome: A
systematic review and meta-analysis. Sleep Med Rev. 18:293–297.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Arora T, Jiang CQ, Thomas GN, Lam KB,
Zhang WS, Cheng KK, Lam TH and Taheri S: Self-reported long total
sleep duration is associated with metabolic syndrome: The Guangzhou
Biobank Cohort Study. Diabetes Care. 34:2317–2319. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Santos AC, Ebrahim S and Barros H: Alcohol
intake, smoking, sleeping hours, physical activity and the
metabolic syndrome. Prev Med. 44:328–334. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Basnet S, Merikanto I, Lahti T, Männistö
S, Laatikainen T, Vartiainen E and Partonen T: Associations of
common chronic non-communicable diseases and medical conditions
with sleep-related problems in a population-based health
examination study. Sleep Sci. 9:249–254. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Okubo N, Matsuzaka M, Takahashi I, Sawada
K, Sato S, Akimoto N, Umeda T and Nakaji S; Hirosaki University
Graduate School of Medicine, : Relationship between self-reported
sleep quality and metabolic syndrome in general population. BMC
Public Health. 14:5622014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hung HC, Yang YC, Ou HY, Wu JS, Lu FH and
Chang CJ: The association between self-reported sleep quality and
metabolic syndrome. PLoS One. 8:e543042013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lu K, Chen J, Wu S, Chen J and Hu D:
Interaction of sleep duration and sleep quality on hypertension
prevalence in adult Chinese males. J Epidemiol. 25:415–422. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lou P, Chen P, Zhang L, Zhang P, Chang G,
Zhang N, Li T and Qiao C: Interaction of sleep quality and sleep
duration on impaired fasting glucose: A population-based
cross-sectional survey in China. BMJ Open. 4:e0044362014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Buysse DJ, Reynolds CF III, Monk TH,
Berman SR and Kupfer DJ: The pittsburgh sleep quality index: A new
instrument for psychiatric practice and research. Psychiatry Res.
28:193–213. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Donker T, van Straten A, Marks I and
Cuijpers P: Quick and easy self-rating of Generalized Anxiety
Disorder: Validity of the Dutch web-based GAD-7, GAD-2 and GAD-SI.
Psychiatry Res. 188:58–64. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhang Y, Ting R, Lam M, Lam J, Nan H,
Yeung R, Yang W, Ji L, Weng J, Wing YK, et al: Measuring depressive
symptoms using the Patient Health Questionnaire-9 in Hong Kong
Chinese subjects with type 2 diabetes. J Affect Disord.
151:660–666. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Weng J, Ji L, Jia W, Lu J, Zhou Z, Zou D,
Zhu D, Chen L, Chen L, Guo L, et al: Standards of care for type 2
diabetes in China. Diabetes Metab Res Rev. 32:442–458. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Najafian J, Toghianifar N, Mohammadifard N
and Nouri F: Association between sleep duration and metabolic
syndrome in a population-based study: Isfahan healthy heart
program. J Res Med Sci. 16:801–806. 2011.PubMed/NCBI
|
|
21
|
Kazman JB, Abraham PA, Zeno SA, Poth M and
Deuster PA: Self-reported sleep impairment and the metabolic
syndrome among African Americans. Ethn Dis. 22:410–415.
2012.PubMed/NCBI
|
|
22
|
Zuo HJ, Yao CH, Hu YS and Kong LZ:
Relations between smoking, alcohol intake, physical activity,
sleeping hours and the metabolic syndrome in Chinese male aged
18–45 years old. Zhonghua Liu Xing Bing Xue Za Zhi. 32:235–238.
2011.(In Chinese). PubMed/NCBI
|
|
23
|
Bidulescu A, Din-Dzietham R, Coverson DL,
Chen Z, Meng YX, Buxbaum SG, Gibbons GH and Welch VL: Interaction
of sleep quality and psychosocial stress on obesity in African
Americans: The Cardiovascular Health Epidemiology Study (CHES). BMC
Public Health. 10:5812010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bonnet F: Associations between anxiety,
depression, and the metabolic syndrome. Biol Psychiatry.
62:1251–1257. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kahl KG, Schweiger U, Correll C, Müller C,
Busch ML, Bauer M and Schwarz P: Depression, anxiety disorders, and
metabolic syndrome in a population at risk for type 2 diabetes
mellitus. Brain Behav. 5:e003062015. View
Article : Google Scholar : PubMed/NCBI
|
|
26
|
Nyer M, Farabaugh A, Fehling K, Soskin D,
Holt D, Papakostas GI, Pedrelli P, Fava M, Pisoni A, Vitolo O and
Mischoulon D: Relationship between sleep disturbance and
depression, anxiety, and functioning in college students. Depress
Anxiety. 30:873–880. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
27
|
Taheri S, Lin L, Austin D, Young T and
Mignot E: Short sleep duration is associated with reduced leptin,
elevated ghrelin, and increased body mass index. PLoS Med.
1:210–217. 2004. View Article : Google Scholar
|
|
28
|
Li L, Fu J, Yu XT, Li G, Xu L, Yin J,
Cheng H, Hou D, Zhao X, Gao S, et al: Sleep duration and
cardiometabolic risk among chinese school-aged children: Do
adipokines play a mediating role? Sleep. 40:2017. View Article : Google Scholar
|
|
29
|
Lusardi P, Zoppi A, Preti P, Pesce RM,
Piazza E and Fogari R: Effects of insufficient sleep on blood
pressure in hypertensive patients: A 24-h study. Am J Hypertens.
12:63–68. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Stamatakis KA and Punjabi NM: Effects of
sleep fragmentation on glucose metabolism in normal subjects.
Chest. 137:95–101. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kanagasabai T and Ardern CI: Contribution
of inflammation, oxidative stress, and antioxidants to the
relationship between sleep duration and cardiometabolic health.
Sleep. 38:1905–1912. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Knutson KL, Wu D, Patel SR, Loredo JS,
Redline S, Cai J, Gallo LC, Mossavar-Rahmani Y, Ramos AR, Teng Y,
et al: Association between sleep timing, obesity, diabetes: The
Hispanic Community Health Study/Study of Latinos (HCHS/SOL) cohort
study: Sleep timing, obesity, and diabetes. Sleep. 40:2017.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Signal TL, Gale J and Gander PH: Sleep
measurement in flight crew: Comparing actigraphic and subjective
estimates to polysomnography. Aviat Space Environ Med.
76:1058–1063. 2005.PubMed/NCBI
|
|
34
|
Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J,
Shan Z, Liu J, Tian H, Ji Q, et al: Prevalence of diabetes among
men and women in China. N Engl J Med. 362:1090–1101. 2010.
View Article : Google Scholar : PubMed/NCBI
|