Introduction
Developmental dysplasia of the hip (DDH) is a
congenital or developmental deformation or misalignment of the hip
joint, and is one of the most common congenital defects in the
newborns, which significantly impairs skeletal development in
children (1). DDH has become one of
the most common types of skeletal congenital anomaly and affects 1
in 1,000 live births in China (2).
It has been indicated that DDH may be influenced by environmental
and genetic factors and the incidence in females is five times that
in males (3). Surgical management is
the most common treatment for DDH of severities ranging from a mild
form of acetabular dysplasia to a moderate form of subluxation of
the hips (4). A systematic review
demonstrated that the incidence of avascular necrosis was frequent
following medial open reduction in pediatric patients with DDH
(5).
At present, surgery is the most commonly used
treatment for DDH, and the success depends on the accuracy of the
pelvic osteotomy (6). The 3D
printing technique has been applied in orthopedics research on
trauma, tumor, joint replacement and pedicle screw fixation
(7,8). Zheng et al (9) suggested that a 3D-printed navigation
template in proximal femoral osteotomy simplifies surgery and
improves the precision for older pediatric patients with DDH. In
addition, Wu et al (10)
indicated that the 3D printing technique provides virtual
pre-operative planning prior to reconstruction of old pelvic
injuries. Zengy et al (11)
suggested that the 3D reconstruction technique may restore the true
acetabular morphology and allows for quantitative analysis of DDH
patients. Of note, a pilot study demonstrated the potential
application of the rapid prototyping pelvic model for patients with
DDH, which facilitates arthroplasty planning and surgical
procedures due to better planning and improved orientation
(12).
To explore the value of the 3D printing technique in
the surgical management and strategy of rehabilitation therapy for
DDH, a 3D-printed pelvis model was used as an adjuvant protocol for
the DDH surgery, and 3D reconstruction, reverse engineering and
rapid prototyping were employed. The present study indicated that
osteotomy simulation using the 3D-printed pelvis model contributes
to the surgical management and strategy of individualized operative
treatment of DDH using osteotomy simulation.
Materials and methods
Subjects
A total of 56 patients (28 females and 28 males)
with DDH were recruited at the Affiliated Hongqi Hospital of
Mudanjiang Medical University between May 2014 and July 2017. The
mean age of the patients was 17.5 years (range, 12.0–19.5 years).
DDH was diagnosed by computed tomography (CT) imaging examination
and all subjects had unilateral or bilateral DDH. The severity of
DDH was defined according to three grades: Instability, subluxation
and dislocation, as previously described (13). None of the patients had any history
or symptoms of DDH and patients with any systemic syndrome were
excluded from the study.
Processing of 3D-printed pelvis
model
The 3D printing experiments were performed using a
self-developed selective laser melting machine, DiMetal-100 (South
China University of Technology). The 3D-printed pelvis model was
directed by a scanning galvanometer according to a previous study
(14).
The settings for the procedure were as follows:
Scanning speed, 30–3,000 mm/sec; thickness of layer, 20–120 µm;
focusing spot diameter, 80 µm. The largest size of the part
produced was 100×100×120 mm.
Surgical reconstruction guided by a
3D-printed pelvis model
The osteotomy surgery was performed with the
guidance of the 3D-printed pelvis model and the final reduction was
pre-assessed to obtain the best-fit position for each DDH patient.
The surgery was first simulated using a 3D-printed pelvis model. By
using the virtual skeletal model, the optimal osteotomy position
and angle were determined to achieve the best wedge resection
geometry during osteotomy surgery.
Pelvic osteotomy
All operations were planned with the 3D model and
performed using pelvic osteotomy as described previously (15). In brief, the hip joint of patients
was approached superficially between the sartorius and tensor
fascia lata and the deep dissection was between the hip abductors
and rectus. The anteromedial capsule was adequately incised and the
hip was identified; the ligamentum teres was cut and traced to the
acetabulum. Soft-tissue release was applied in all hips; the hip
was abducted and adducted, and the zone of abduction and adduction
in which the femoral head remains reduced in the acetabulum was
determined. The orientation of the osteotomy was marked on the
lateral cortex of the ilium and a straight 0.5-inch osteotome was
used to perform the bone cut. A guide wire was inserted under
fluoroscopic control at the most cephalad point of the curvilinear
marking line, which was used to ensure that the osteotomy
terminated at the appropriate level just above the horizontal limb
of the triradiate cartilage. The osteotomy site was kept open by
inserting two correctly sized bone grafts and fixed with metallic
internal fixation. After the insertion of femoral and acetabular
components, computed tomography was performed to evaluate the
efficacy of surgery.
Evaluation
The bone and model measurements were compared to
assess the accuracy of the osteotomies guided by the 3D printed
model or CT-based model. Surgical time, post-operative recovery
time, hospital stay and an inflammation-based prognostic score were
recorded for all patients (16). CT
examination was performed three days after the osteotomy surgery.
Hip function was assessed using the Majeed score (17). The accuracy of the internal fixation
was determined from the post-operative CT. The patients' hip joints
were classified according to Tonnis measurements of the acetabula
angles into 4 grades using International Hip Dysplasia Institute
classification system as described previously (18). The detailed summary scores and the
visual analog scale of satisfaction mean score were recorded in
patients as described previously (19). The evaluations and follow-up (24
months) were performed by the same three independent doctors.
Statistical analysis
Values are expressed as the mean ± standard
deviation and statistical analyses were performed using SPSS
version 19.0 software (IBM Corp.). Student's t-test was used to
compare the measurements made on the 3D printed models to those
from the 3D-CT based pelvis model. P<0.05 was considered to
indicate statistical significance.
Results
Patient characteristics
A total of 56 DDH patients (28 female, 28 male) were
included in the present study. DDH was located on the right hip in
36 cases and on the left in 20 cases. The mean follow-up time was
24 months. A total of 18 DDH patients (8 female, 10 male) were
treated by surgery planned by using the 3D-printed pelvis model and
38 DDH patients (20 female, 18 male) received surgery planned by
using 3D-CT. All patients were randomly recruited and voluntarily
received 3D-printed pelvis model or 3D-CT. The baseline
characteristics of the DDH patients are summarized in Table I. Regarding the different severities
of DDH (instability, subluxation and dislocation), the percentage
of male and female patients was not significantly different between
the two groups.
 | Table I.Characteristics of patients with
developmental dysplasia of the hip. |
Table I.
Characteristics of patients with
developmental dysplasia of the hip.
| Characteristic | 3D-CT | 3D-printed pelvis
model | P-value |
|---|
| Total number | 38 (67.9) | 18 (32.1) | 0.026 |
| Sex |
|
|
|
|
Female | 20 (52.6) | 8 (44.4) | 0.054 |
| Male | 18 (47.4) | 10 (55.6) | 0.068 |
| Side affected |
|
|
|
|
Right | 28 (73.7) | 8 (44.4) | 0.022 |
| Left | 10 (26.3) | 10 (55.6) | 0.034 |
| Age (years) | 32±4 | 36±5 | 0.68 |
| Severity of
dysplasia |
|
|
|
|
Instability | 10 (26.3) | 5 (27.8) | 0.46 |
|
Subluxation | 15 (39.5) | 7 (38.9) | 0.52 |
|
Dislocation | 13 (34.2) | 6 (33.3) | 0.76 |
| Follow-up
(months) | 24 | 24 | – |
Efficacy
The efficacy of the 3D-printed pelvis model was
investigated in the 56 DDH patients (n=18 in the 3D-printed pelvis
model group; n=38 in the 3D-CT group). The success rate of surgery
(at month 3) in those DDH patients pre-evaluated with the
3D-printed pelvis model (94.2%) was significantly higher than that
in the patients pre-evaluated by 3D-CT (82.4%). Use of the
3D-printed pelvis model decreased the surgery time (surgery +
3D-printed pelvis model, 4.8 h; surgery + 3D-CT, 6.2 h) and
shortened the post-operative recovery time for DDH patients
compared with that in the surgery + 3D-CT group. In addition, the
3D-printed pelvis model significantly reduced total redislocations
and redislocations detected after discharge for DDH patients
(Table II).
 | Table II.Efficacy of 3D-printed pelvis model
for patients with developmental dysplasia of the hip. |
Table II.
Efficacy of 3D-printed pelvis model
for patients with developmental dysplasia of the hip.
| Item | 3D-CT | 3D-printed pelvis
model | P-value |
|---|
| Success rate (%) | 82.4 | 94.2 | 0.040 |
| Surgery time (h) | 6.2±1.5 | 4.8±2.0 | 0.026 |
| Post-operative
recovery time (days) | 28.5±7.0 | 21.0±5.0 | 0.036 |
| Total
redislocations | 5 (17.8) | 3 (7.9) | 0.0053 |
| Redislocations
detected after discharge | 4 (10.5) | 2 (5.6) | 0.038 |
Recovery
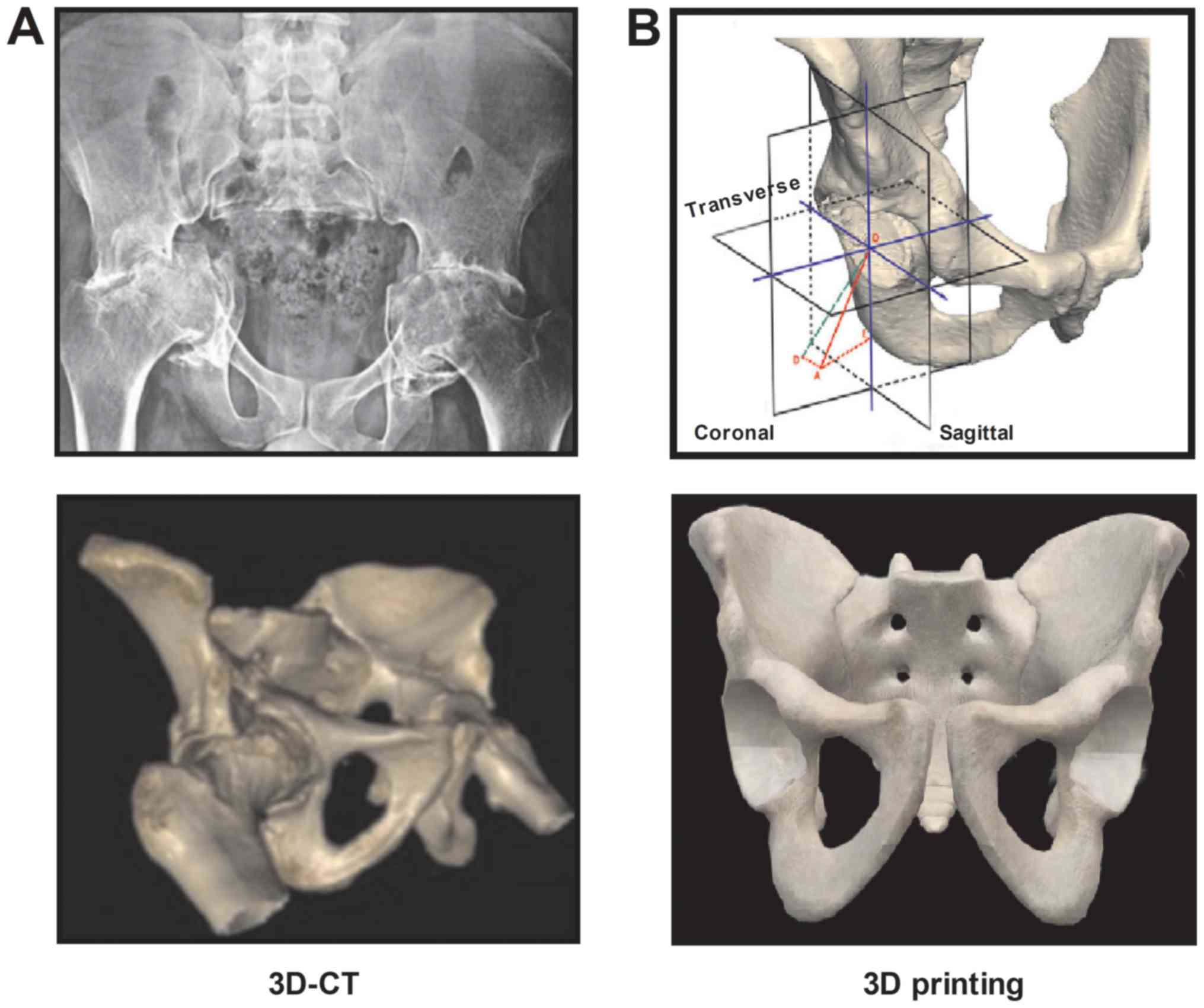
Representative images of the 3D-CT and 3D-printed
pelvis model were provided in Fig.
1. The present results revealed that use of the 3D-printed
pelvis model allowed for more rapid recovery of the DDH patients.
The time of hospital stay and inflammation score were decreased in
the surgery + 3D-printed pelvis model group compared with those in
the surgery + 3D-CT group. Furthermore, few DDH patients with
osteotomy simulation using the 3D-printed pelvis model or 3D-CT had
delayed incision healing, wound infection or nonunion. The overall
Majeed score demonstrated an similar between the surgery +
3D-printed pelvis model group and the surgery + 3D-CT groups
(Table III).
 | Table III.Efficacy of 3D-printed pelvis model
for post-operative parameters in patients with developmental
dysplasia of the hip. |
Table III.
Efficacy of 3D-printed pelvis model
for post-operative parameters in patients with developmental
dysplasia of the hip.
| Item | 3D-CT | 3D-printed pelvis
model | P-value |
|---|
| Hospital stay
(days) | 28.0±6.0 | 23.5±4.5 | 0.035 |
| Inflammation
score | 6.0±2.0 | 4.0±2.0 | 0.044 |
| Delayed incision
healing | 2 (7.1) | 2 (7.1) | >0.05 |
| Wound infection | 1 (3.6) | 1 (3.6) | >0.05 |
| Nonunion | 1 (3.6) | 1 (3.6) | >0.05 |
| Majeed score | 72±10 | 70±15 | >0.05 |
Outcomes
The detailed summary scores and the visual analog
scale of satisfaction mean score are provided in Table IV. The scores for the pelvis and the
spine tests for the 3D-CT group were significantly lower than those
for the 3D-printed pelvis model group (P<0.01). However, no
significant differences were observed in the scores for the upper
limb test or the lower limb test (P=0.64 and P=0.72, respectively).
The visual analog scale of satisfaction mean score was 7.49±1.38
and 5.80±1.30 in 3D-printed pelvis model group and 3D-CT group,
respectively (P<0.01).
 | Table IV.Comparison of summary scores
(coordination score and visual analog scale of satisfaction score)
between the 3D-CT and 3D-printed pelvis model groups. |
Table IV.
Comparison of summary scores
(coordination score and visual analog scale of satisfaction score)
between the 3D-CT and 3D-printed pelvis model groups.
| Parameter | 3D-CT | 3D-printed pelvis
model | P-value |
|---|
| Upper limb
coordination score | 7.01±1.56 | 7.12±1.38 | 0.64 |
| Lower limb
coordination score | 7.52±1.69 | 7.40±1.46 | 0.72 |
| Pelvis coordination
score | 4.64±1.52 | 6.80±1.52 | <0.01 |
| Visual analog scale
of satisfaction | 5.36±1.21 | 7.58±1.46 | <0.01 |
The pre- and post-operative acetabular index and
center edge angle were compared between the two groups of patients.
There was no significant difference in the pre-operative acetabular
index (38.5±10.5 vs. 40.6±12.6°) and center edge angle (14.2±6.8
vs. 13.5±7.5°) between the 3D-printed pelvis model group and the
3D-CT group. As indicated in Table
V, none of the patients in the two groups presented with any
hip deformities or torticollis. The average acetabula index at
month 3 was 22.6±4.2 and 24.3±4.8° in the surgery + 3D-printed
pelvis model group and the surgery + 3D-CT group, respectively
(P<0.05). The average center edge angle was 27.5±5.6 and
24.4±6.0° in the surgery + 3D-printed pelvis model group and the
surgery + 3D-CT group, respectively (Table V). DDH patients in the surgery +
3D-printed pelvis model group had a better radiographic acetabular
index and center edge angle than those in the surgery + 3D-CT
group.
 | Table V.Pre- and post-operative acetabular
index and center edge angle (°) for patients with developmental
dysplasia of the hip. |
Table V.
Pre- and post-operative acetabular
index and center edge angle (°) for patients with developmental
dysplasia of the hip.
| Time-point/angle
type | 3D-CT | 3D-printed pelvis
model |
|---|
| Prior to the
operation |
|
|
|
Acetabular index angle | 38.5±10.5 | 40.6±12.6 |
| Center
edge angle | 14.2±6.8 | 13.5±7.5 |
| Post-operation (3
months) |
|
|
|
Acetabular index angle | 22.6±4.2 |
24.3±4.8a |
| Center
edge angle | 27.5±5.6 |
24.4±6.0a |
Discussion
With the development of 3D printing technology, its
application in life science is increasing and it is becoming an
important tool in medical treatments (20). A previous study has indicated that
putting 3D modeling and 3D printing into practice is beneficial for
virtual surgery and pre-operative planning to reconstruct complex
post-traumatic skeletal deformities and defects (21). In the present study, the auxiliary
efficacy of a 3D-printed pelvis model combined with surgery was
investigated in a total of 38 DDH patients with 3D-CT planning (18
DDH patients) as a control. The results indicated that the
3D-printed pelvis model comprising 3D reconstruction, reverse
engineering and rapid prototyping is beneficial for osteotomy
simulation in patients with DDH.
A previous study reported on the efficacy of 3D
printing simulated operation and the associated improvement in the
accuracy and safety of minimally invasive surgery through a small
incision lateral to the rectus abdominis for pelvic fracture
(22). Xiao et al (23) demonstrated that 3D printing
technology increased the predictability, feasibility and
reliability of simultaneous mandibular contour osteoplasty and
orthognathic surgery. The present study indicated that a 3D-printed
pelvis model improved the accuracy of pelvic osteotomy, and also
decreased the surgery time and post-operative inflammation compared
to 3D-CT-based surgery for patients with DDH. In a previous study,
dimensional evaluation of patient-specific 3D printing using
calcium phosphate cement provided a good degree of fitting and
accuracy for craniofacial bone reconstruction (24). In the present study, the 3D-printed
pelvis model was able to accurately represent the morphology and
various angles of the pelvis using osteotomy simulation.
Furthermore, through the use of rapid prototyping, 3D printing
models have been used in orthopaedic surgery, which offers surgeons
a number of advantages when treating complex fractures (14). The present study indicated that use
of the 3D-printed pelvis model increased the accuracy of the
surgery and decreased the time of surgery, which led to a higher
success rate of the operation and shorter post-operative recovery
time for DDH patients.
The acetabula index is considered the most reliable
radiographic measure to evaluate the development of DDH (25). The average acetabular index was
significantly improved in patients with DDH receiving 3D-printed
pelvis model-based surgery compared with those treated by
3D-CT-based surgery with an upper limit of normal of <30°.
Radiological post-operative assessment of the center edge angle
remains the primary factor influencing normal hip development and
is required to optimize the development of the hip with the minimum
number of operations (26). In the
present study, the center edge angle was markedly improved in the
3D-printed pelvis model-based surgery group compared with that in
the 3D-CT-based surgery group. Good follow-up results were
achieved, with no evidence of loosening of the acetabular
components, or any type of hip deformity or torticollis.
The limitation of the study is that it was a
retrospective preliminary study, and the number of patients was
relatively small in both the 3D-printed pelvis model and 3D-CT
groups. In addition, the follow-up for all DDH patients was
relatively short. Furthermore, the data of the present study were
from a single medical center and the full post-operative
radiological information was not available for all patients. Future
studies should include a large number of patients with DDH and also
evaluate the cost of treatment of this disease between the
3D-printed pelvis model and the 3D-CT group.
In conclusion, in the present study, the potential
application of the 3D-printed pelvis model for DDH was
investigated. The results indicated that the 3D-printed pelvis
model may serve as an important tool for the individualized
treatment of DDH patients. Further research is required to validate
the application of the 3D-printed pelvis model for DDH therapy.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KXL, ZTL, and YBM performed the experiments,
analyzed the data and conducted the statistical analysis. HYL
designed the experiments, wrote the original manuscript and revised
the manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Mudanjiang Medical University (Mudanjiang). Written
informed consent was obtained from all participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Toma P, Valle M, Rossi U and Brunenghi GM:
Paediatric hip-ultrasound screening for developmental dysplasia of
the hip: A review. Eur J Ultrasound. 14:45–55. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yang S and Cui Q: Total hip arthroplasty
in developmental dysplasia of the hip: Review of anatomy,
techniques and outcomes. World J Orthop. 3:42–48. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Rhodes AM and Clarke NM: A review of
environmental factors implicated in human developmental dysplasia
of the hip. J Child Orthop. 8:375–379. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Canavese F, Vargas-Barreto B, Kaelin A and
de Coulon G: Onset of developmental dysplasia of the hip during
clubfoot treatment: Report of two cases and review of patients with
both deformities followed at a single institution. J Pediatric
Orthop B. 20:152–156. 2011. View Article : Google Scholar
|
|
5
|
Gardner RO, Bradley CS, Howard A,
Narayanan UG, Wedge JH and Kelley SP: The incidence of avascular
necrosis and the radiographic outcome following medial open
reduction in children with developmental dysplasia of the hip: A
systematic review. Bone Joint J. 96-B:279–286. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Di Mascio L, Carey-Smith R and Tucker K:
Open reduction of developmental hip dysplasia using a medial
approach: A review of 24 hips. Acta Orthop Belg. 74:343–348.
2008.PubMed/NCBI
|
|
7
|
Eley KA, Watt-Smith SR and Golding SJ:
‘Black Bone’ MRI: A novel imaging technique for 3D printing.
Dentomaxillofac Radiol. 46:201604072017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhou Z, Buchanan F, Mitchell C and Dunne
N: Printability of calcium phosphate: Calcium sulfate powders for
the application of tissue engineered bone scaffolds using the 3D
printing technique. Mater Sci Eng C Mater Biol Appl. 38:1–10. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zheng P, Xu P, Yao Q, Tang K and Lou Y:
3D-printed navigation template in proximal femoral osteotomy for
older children with developmental dysplasia of the hip. Sci Rep.
7:449932017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wu XB, Wang JQ, Zhao CP, Sun X, Shi Y,
Zhang ZA, Li YN and Wang MY: Printed three-dimensional anatomic
templates for virtual preoperative planning before reconstruction
of old pelvic injuries: Initial results. Chin Med J (Engl).
128:477–482. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zengy Y, Min L, Lai OJ, Shen B, Yang J,
Zhou ZK, Kang PD and Pei FX: Acetabular morphological analysis in
patients with high dislocated DDH using three-dimensional surface
reconstruction technique. Sichuan Da Xue Xue Bao Yi Xue Ban.
46:296–300. 2015.(In Chinese). PubMed/NCBI
|
|
12
|
Xu J, Li D, Ma RF, Barden B and Ding Y:
Application of rapid prototyping pelvic model for patients with DDH
to facilitate arthroplasty planning: A pilot study. J Arthroplasty.
30:1963–1970. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dai J, Shi D, Zhu P, Qin J, Ni H, Xu Y,
Yao C, Zhu L, Zhu H, Zhao B, et al: Association of a single
nucleotide polymorphism in growth differentiate factor 5 with
congenital dysplasia of the hip: A case-control study. Arthritis
Res Ther. 10:R1262008. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Upex P, Jouffroy P and Riouallon G:
Application of 3D printing for treating fractures of both columns
of the acetabulum: Benefit of pre-contouring plates on the mirrored
healthy pelvis. Orthop Traumatol Surg Res. 103:331–334. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tuhanioglu U, Cicek H, Ogur HU,
Seyfettinoglu F and Kapukaya A: Evaluation of late redislocation in
patients who underwent open reduction and pelvic osteotomy as
treament for developmental dysplasia of the hip. Hip Int.
28:309–314. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Watt DG, McSorley ST, Park JH, Horgan PG
and McMillan DC: A postoperative systemic inflammation score
predicts short- and long-term outcomes in patients undergoing
surgery for colorectal cancer. Ann Surg Oncol. 24:1100–1109. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bajada S and Mohanty K: Psychometric
properties including reliability, validity and responsiveness of
the Majeed pelvic score in patients with chronic sacroiliac joint
pain. Eur Spine J. 25:1939–1944. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Miao M, Cai H, Hu L and Wang Z:
Retrospective observational study comparing the international hip
dysplasia institute classification with the Tonnis classification
of developmental dysplasia of the hip. Medicine (Baltimore).
96:e59022017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chandrasekaran S, Gui C, Walsh JP, Lodhia
P, Suarez-Ahedo C and Domb BG: Correlation between Changes in
visual analog scale and patient-reported outcome scores and patient
satisfaction after hip arthroscopic surgery. Orthop J Sports Med.
5:23259671177247722017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lee N: The lancet technology: 3D printing
for instruments, models, and organs? Lancet. 388:13682016.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tetsworth K, Block S and Glatt V: Putting
3D modelling and 3D printing into practice: Virtual surgery and
preoperative planning to reconstruct complex post-traumatic
skeletal deformities and defects. SICOT J. 3:162017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zeng CJ, Tan XY, Huang HJ, Huang WQ, Li T,
Jin DD, Zhang GD and Huang WH: Clincial effect of 3D
printing-assisted minimal invasive surgery through a small incision
lateral to the rectus abdominis for pelvic fracture. Nan Fang Yi Ke
Da Xue Xue Bao. 36:220–225. 2016.(In Chinese). PubMed/NCBI
|
|
23
|
Xiao Y, Sun X, Wang L, Zhang Y, Chen K and
Wu G: The application of 3D printing technology for simultaneous
orthognathic surgery and mandibular contour osteoplasty in the
treatment of craniofacial deformities. Aesthetic Plast Surg.
41:1413–1424. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bertol LS, Schabbach R and Dos Santos LAL:
Dimensional evaluation of patient-specific 3D printing using
calcium phosphate cement for craniofacial bone reconstruction. J
Biomater Appl. 31:799–806. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Nie Y, Wang H, Huang Z, Shen B, Kraus VB
and Zhou Z: Radiographic underestimation of in vivo cup coverage
provided by total Hip arthroplasty for dysplasia. Orthopedics.
41:e46–e51. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Murphy RF and Kim YJ: Surgical Management
of pediatric developmental dysplasia of the Hip. J Am Acad Orthop
Surg. 24:615–624. 2016. View Article : Google Scholar : PubMed/NCBI
|