Introduction
With the aging of the population, spinal stenosis
with degenerative lumbar spondylolisthesis (DLS) in elderly
patients has become an increasingly common condition (1). Neurogenic claudication and
radiculopathy are the most common symptoms of spinal stenosis
(2). Surgery may be offered to
patients who are symptomatic and fail to respond to non-operative
treatment measures, including physical therapy and epidural steroid
injections. Patients are frequently treated using a decompression
operation of neural structures. However, the management of these
patients remains controversial (1).
Several surgical methods have been used for the management of DLS,
including decompression without fusion, posterolateral in
situ fusion, posterolateral instrumented fusion with pedicle
screws, anterior lumbar interbody fusion, posterolateral
instrumented fusion with pedicle screws plus interbody fusion and
dynamic stabilization (3). In recent
years, various studies have assessed the efficacy of decompression
alone vs. decompression with fusion for this condition, but the
results were conflicting (3–7). The focus of controversy was whether the
addition of fusion added benefit to decompression for patients with
either grade I or II spondylolisthesis spondylolisthesis.
Increasing evidence has demonstrated that in the management of DLS
associated with spinal stenosis, additional fusion may not yield
any clinical improvement over treatment with decompression alone
(5–7).
Minimally invasive decompression, which involves a
small incision, causes significantly less tissue disruption than
open surgery and provides greater patient satisfaction, and is
increasingly and more frequently used for DLS (8). Certain studies have indicated that
microendoscopic laminotomy is also an effective procedure for the
treatment of patients with DLS (8,9).
Minimally invasive decompression may prevent post-operative
instability and lead to the preservation of stabilizing structures,
avoiding the requirement for fusion. Therefore, minimally invasive
decompression procedures have been attracting attention in cases of
radiating pain-dominant DLS that is associated with spinal stenosis
without severe segmental instability (9).
In recent years, percutaneous endoscopic discectomy
has been confirmed as an ultra-minimally invasive option for the
treatment of lumbar herniated discs (10). Compared with microendoscopic
discectomy, percutaneous transforaminal endoscopic discectomy may
lead to an increased recovery time and result in an improved
clinical outcome (11). Furthermore,
a number of studies have demonstrated that percutaneous endoscopic
decompression under local anesthesia may also be an efficient
alternative to conventional open lumbar decompression surgery for
the treatment of lumbar stenosis in elderly patients, while
administration of general anesthesia may potentially be a
considerable hazard (12,13). In the present study, it was
hypothesized that the percutaneous transforaminal endoscopic
decompression (PTED) procedure may be effective in cases of
radicular pain-dominant DLS, which is associated with spinal
stenosis, without any obvious segmental instability. The purpose of
the present study was to determine the efficacy of PTED by
evaluating the clinical outcome of a group of patients with
DLS.
Materials and methods
Patients
The present investigation was a retrospective cohort
study, which was approved by the Ethics Committee of Renji Hospital
(Shanghai, China) and aimed to evaluate the outcome of PTED
treatment in elderly patients with lumbar spinal stenosis
associated with DLS. A total of 750 patients with spinal diseases
were treated at the Department of Spine Surgery of Renji Hospital
(Shanghai, China) between November 2015 and November 2016; 56
patients with DLS were identified and 18 patients with DLS and
spinal stenosis aged >65 years, with comorbidities, were
included. X-ray was used to diagnose DLS and CT and MRI were used
to indicate the compression position. Radiographic instability was
determined using flexion-extension radiographs. Patients who had
previous lumbar surgeries, trauma, tumors or infection were
excluded. The demographic characteristics, radiographic and
clinical outcomes and surgery were recorded, and the following
inclusion and exclusion criteria were selected with reference to a
previous study (14): i) Low-grade
(Meyerding grades I and II) DLS; ii) no obvious radiographic lumbar
intervertebral instability; iii) symptoms of unilateral radicular
leg pain with no or mild back pain; iv) failure of conservative
therapies at >3 months; and v) elderly patients with potentially
considerable hazards for general anesthesia due to severe
comorbidities, including heart failure, diabetes mellitus, coronary
insufficiency and respiratory failure. Patients enrolled in the
present study were excluded according to the following criteria: i)
Lumbar spine pathologic conditions, including trauma, tumor or
infection; ii) significant facet effusions indicated during MRI
(determined as the largest distance between the apparent articular
surfaces); and iii) a history of lumbar surgery. A total of 18
patients were successfully included in the current study (average
age, 71.2 years; age range, 66–85 years; 10 females and 8
males).
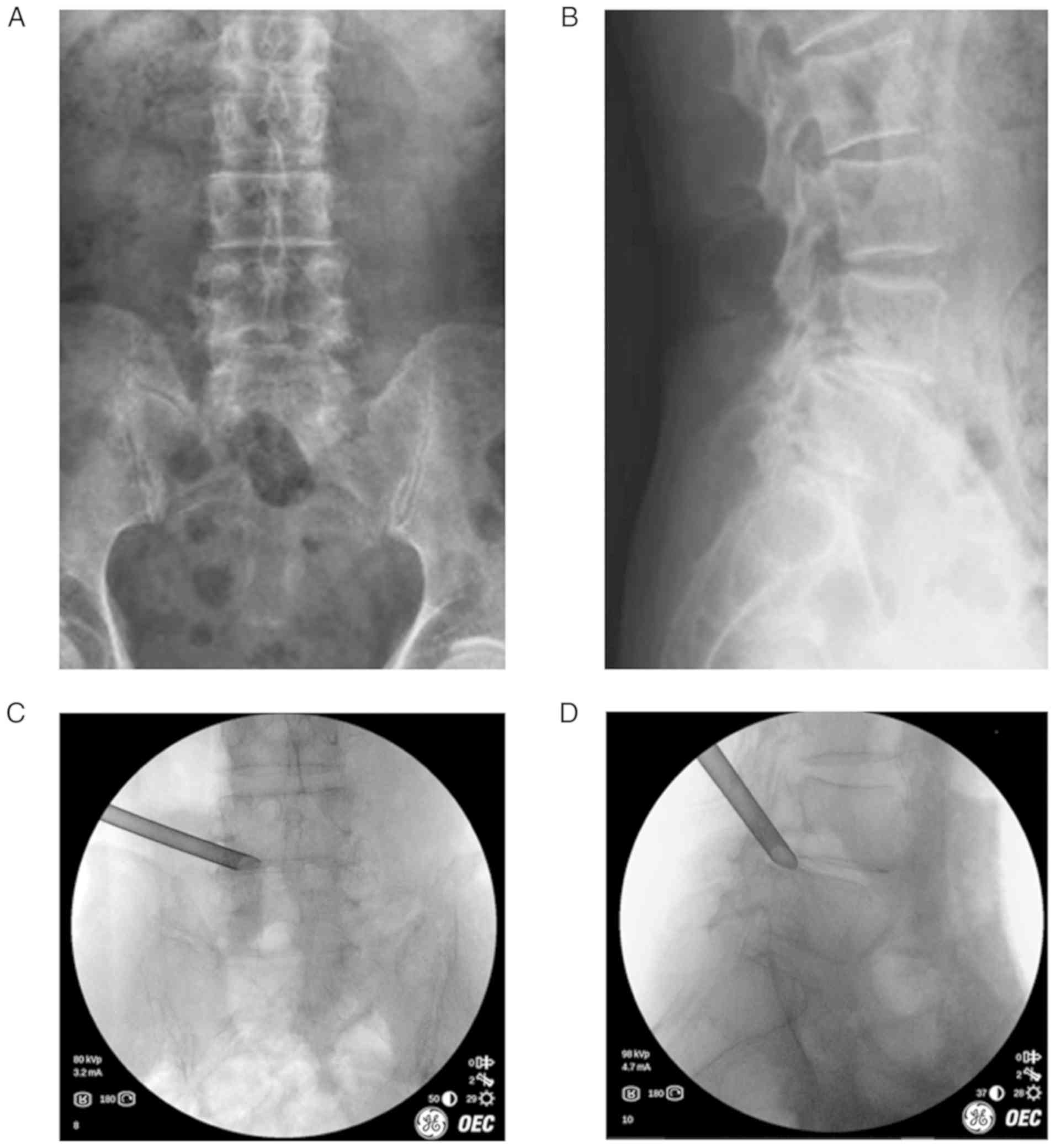
Surgical technique
All patients underwent PTED procedures. All
operations were completed by one surgeon with >5 years of
surgical experience. The procedures were performed using a PTED
system (TESSYS®; Joimax Co.). Patients were placed in
the prone position on a radiolucent table for standard
anteroposterior and lateral radiographs to be obtained during
intra-operative fluoroscopy. The level of the responsible segment
was subsequently determined using C-arm fluoroscopy. The skin entry
point was superior to the iliac crest and 9–13 cm lateral from the
midline, depending on the patient's waist size. Following surface
anesthesia with 1% lidocaine, needle entry tract anesthesia was
performed using a 18-gauge spinal needle with 8–10 ml 1% lidocaine.
The facet joint was anaesthetized using 1% lidocaine when the
needle was engaged with the superior articular processes, and a
guide wire was placed into the needle. A 7-mm cut was created via
the entry point of the guide wire. The sequential dilators were
used to establish a muscle gap approach and bone drills were used
to enlarge the foraminal area by removing bone from the anterior
lateral portion of the upper articular process. Finally, the
working cannula was placed along the guide wire (Fig. 1). The endoscopic system combined with
a 0.9% saline rinsing bag was placed into the working cannula.
Nerve decompression was then performed using this system. The
hypertrophic ligament flavum, perineural scar and extruded disc
material were removed with different instruments, including a
radiofrequency knife, punch forceps and nucleus forceps. In order
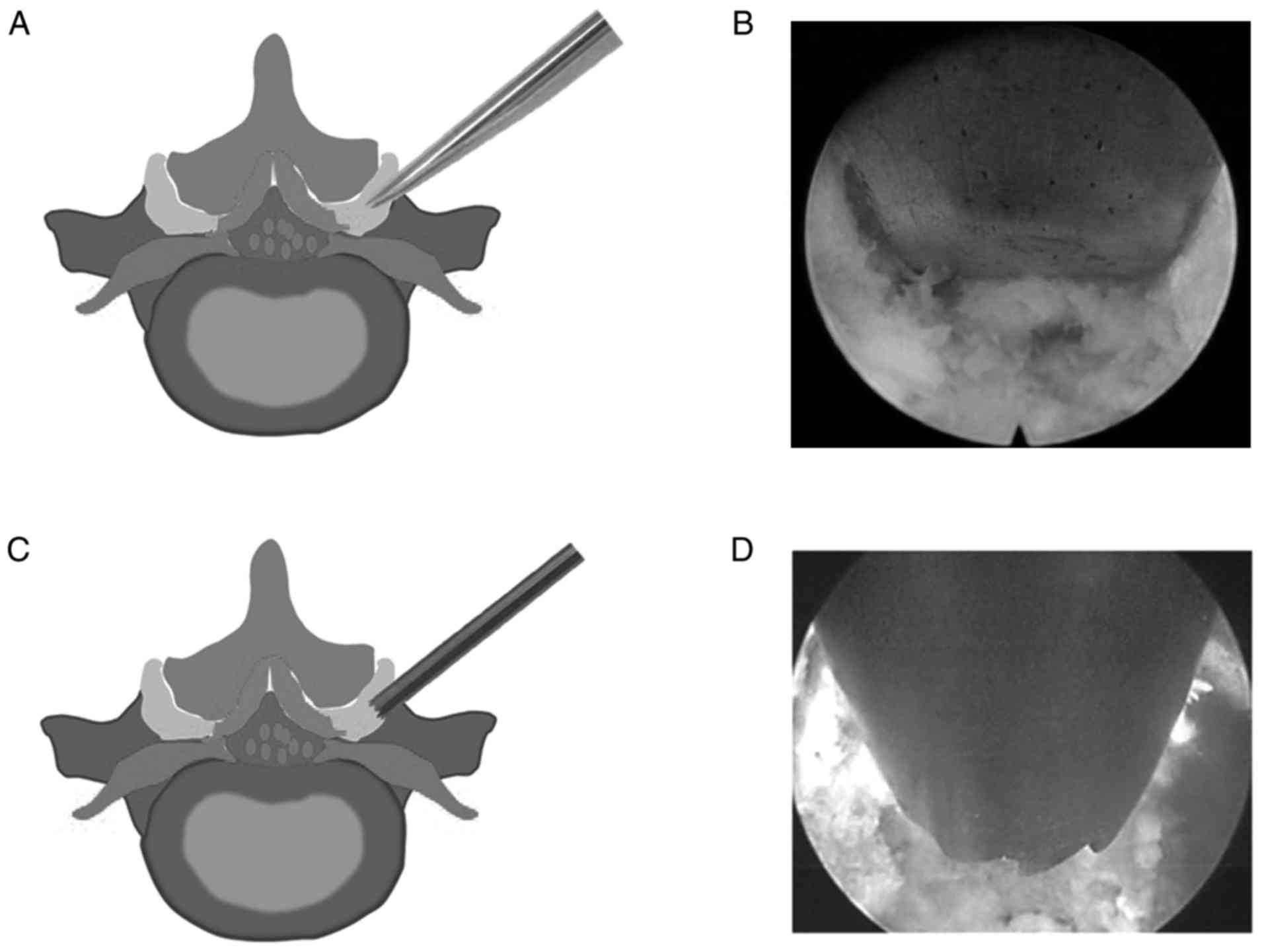
to obtain adequate nerve decompression, foraminoplasty was
performed using an endoscopic chisel (Fig. 2A and B) or endoscopic trephine
(Fig. 2C and D) to remove
hypertrophied superior articular processes. Completely decompressed
nerve roots were easily moved and pulsations were indicated to be
consistent with the heart rate. Bleeding was stopped by squeezing
the rinsing bag or using a bipolar coagulator. After adequate
hemostasis, the endoscopic system was removed and the incision was
sutured. At 2 h after surgery, patients were allowed to move when
no complications occurred.
Outcome assessment
Imaging methods, including X-ray, CT and MRI, were
used to determine radiological outcomes. The improvement in walking
distance prior to and after the operation was rated using three
different degrees (worse, no change or better). The average visual
analogue scale (VAS) score (15),
Oswestry Disability Index (ODI) (16) and modified MacNab criteria (17) were determined as the clinical
outcomes. The data were obtained using patient questionnaires. All
variables were collected at 1 and 3 months following surgery and at
a mean follow-up of 27.7 months. Nerve decompression was
demonstrated on radiographic imaging examination. For all patients,
the percentage slip was measured from the lateral radiographs of
the lumbar spine. The sliding distance was determined as the
distance between the trailing edge of the vertebral body, below the
sliding vertebra, and the parallel line extending through the
posterior border of the vertebra, and this was defined as b. The
percentage slip was defined as the ratio of b to the front and back
dimensions of the sliding vertebral body (a): % of slip=(b/a)
×100%.
Statistical analysis
Statistical analysis was performed using one-way
analysis of variance or a paired t-test with SPSS 19.0 (IBM Corp.)
to compare the differences in the mean of the outcome scores prior
to and after surgery. The Bonferroni test was used for post-hoc
comparison. P<0.05 was considered to indicate statistical
significance.
Results
Demographic characteristics and
outcomes
Demographic characteristics of the patients and some
peri-operative and post-surgical parameters are listed in Table I. The mean body mass index was
24.1±3.0 kg/m2. The prevalence of comorbidities among
the patients was as follows: Hypertension (61.1%); diabetes
mellitus (27.8%); heart disease (38.9%); cerebrovascular infarction
(11.1%); respiratory diseases (16.7%); renal/ureteral disease
(16.7%); and peripheral vascular disease (11.1%).
 | Table I.Demographics of the cohort of the
present study (n=18). |
Table I.
Demographics of the cohort of the
present study (n=18).
| Parameter | Value |
|---|
| Age (years) | 71.2 (66–85) |
| Female sex | 10 (55.6) |
| Duration of symptoms
(months) | 5.3 (3–12) |
| Levels involved |
|
| L4-5 | 12 (66.7) |
|
L5-S1 | 6 (33.3) |
| Number of levels
operated |
|
| One
level | 18 (100) |
| Two
level | 0 (0) |
|
Spondylolisthesis |
|
| Meyerding
grade I | 13 (72.2) |
| Meyerding
grade II | 5 (27.8) |
| Body mass
index | 24.1 (27.1–21.1) |
| Prevalence of
comorbidities |
|
|
Hypertension | 61.1% |
|
Diabetes mellitus | 27.8% |
| Heart
disease | 38.9% |
|
Cerebrovascular
infarction | 11.1% |
|
Respiratory diseases | 16.7% |
|
Renal/ureteral disease | 16.7% |
|
Peripheral vascular
disease | 11.1% |
|
Follow-up (months) | 27.7 (24–33) |
| Blood
loss (ml) | 12.8 (10–25) |
|
Duration of surgery (min) | 90.6 (50–120) |
|
Hospital stay (days) | 1.4 (1–5) |
Clinical outcomes
Modified MacNab criteria were applied in the present
study to evaluate the outcomes (Table
II). The good-to-excellent rate was 83.3%. A total of 2
patients rated their outcome as fair and 1 patient as poor until
three months of the follow-up and this patient underwent subsequent
micro-decompression surgery for correction.
 | Table II.Outcomes according to the modified
MacNab criteria. |
Table II.
Outcomes according to the modified
MacNab criteria.
| Outcome | Description | n (%) |
|---|
| Excellent | Complete relief of
symptoms | 10 (55.6) |
| Good | Marked improvement
but occasional pain | 5 (27.8) |
| Fair | Improved functional
capacity and the need for pain medications | 2 (11.1) |
| Poor | Unimproved symptoms
or worsening | 1 (5.6) |
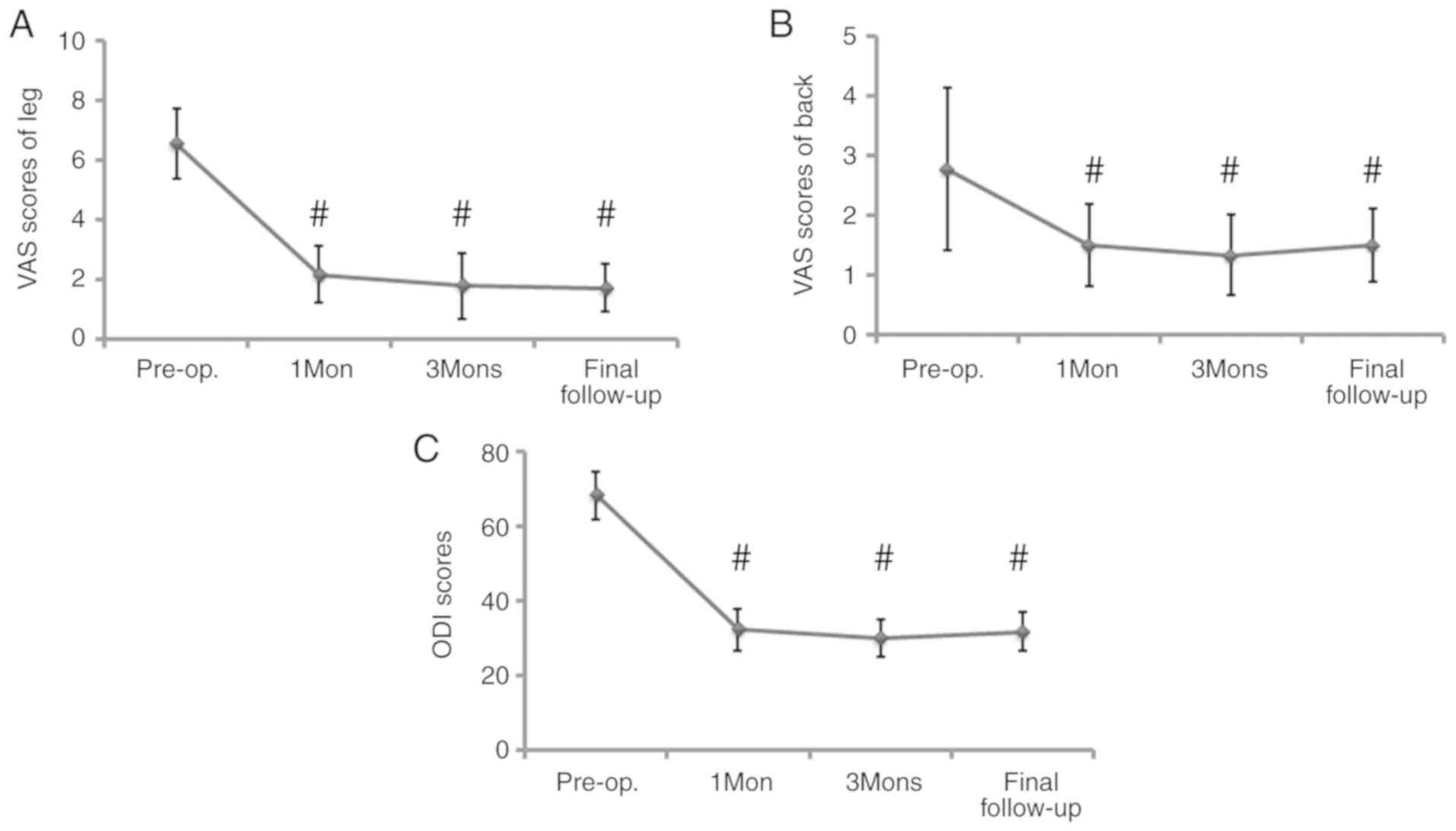
The mean pre-operative ODI was 68.2±6.5 and the VAS
pain score of the leg and back were 6.6±1.2 and 2.8±1.4,
respectively (Fig. 3). Improved
outcomes were reported by patients post-operatively (32.3±5.6,
2.2±0.9, 1.5±0.7 at 1 month; 29.9±5.0, 1.8±1.1, 1.3±0.7 at 3
months; and 31.7±5.2, 1.7±0.8, 1.5±0.6 at the latest follow-up
(Fig. 3). A significant improvement
was observed at 1 month, 3 months and at the latest follow-up in
the ODI and VAS score for the leg (P<0.01), and in the VAS score
for the back (P<0.05; Fig. 3).
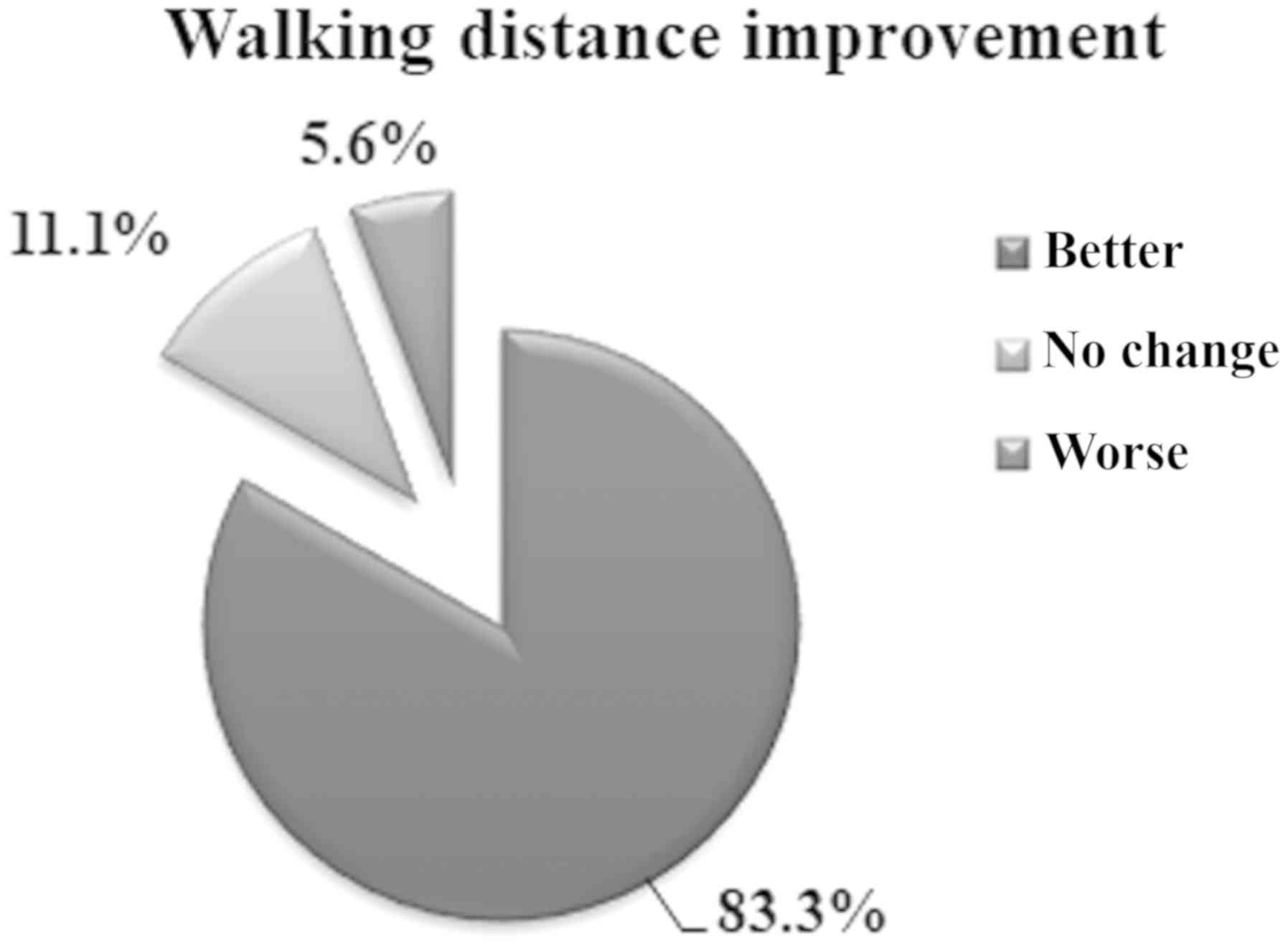
The patients' estimated walking distance increased and an
improvement was reported in 83.3% of cases, and only 5.6% of
patients complained of worsening (Fig.
4).
Radiological outcomes
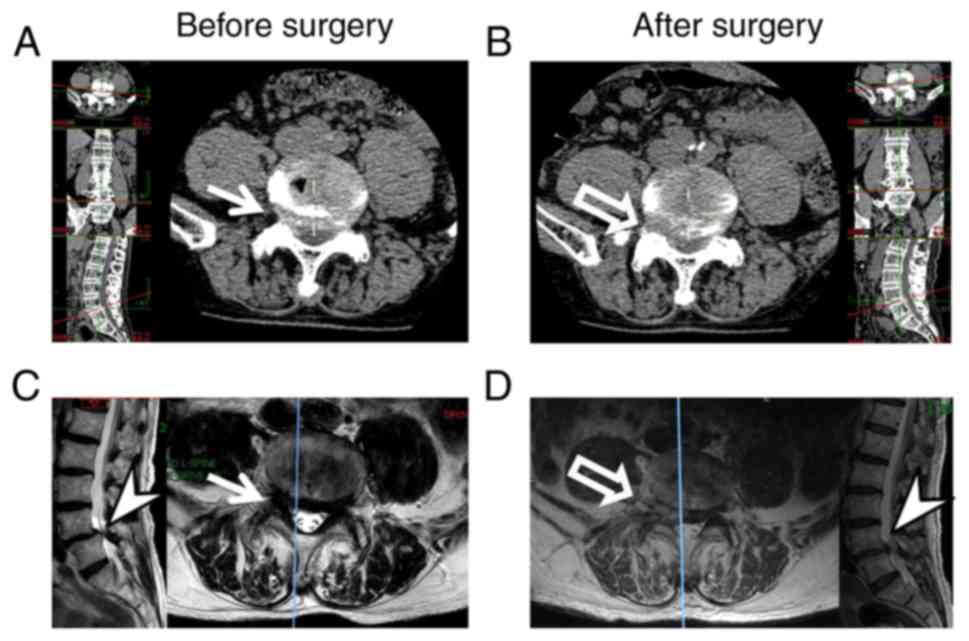
Following surgery, CT and MRI images were evaluated
for the assessment of decompression. Fig. 5 represents the case of an 81-year-old
male patient exhibiting right leg-dominant symptoms with DLS and
spinal stenosis. The pre- and post-surgery images were captured and
compared. CT scans and MRI images demonstrated that right foramina
stenosis and nerve compression were present (Fig. 5A and C), and following surgery, the
removal of the thickened ligaments and the osteophyte of the facet
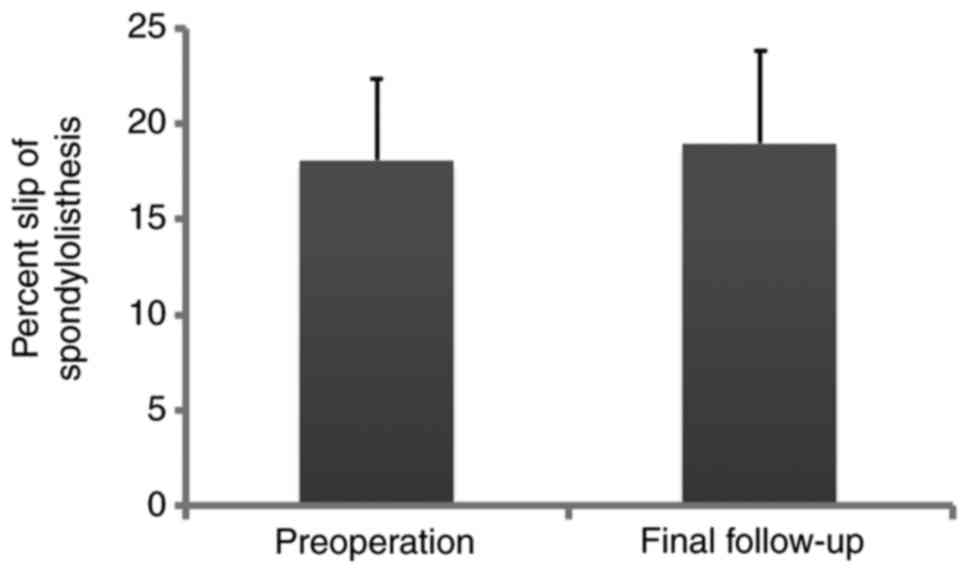
joints pressing on the nerve was evidenced (Fig. 5B and D). As presented in Fig. 6, the average percent slippage was
18.1±4.3% prior to surgery and 18.9±4.8% at the final follow-up. No
statistically significant differences were observed between the
percentage of lumbar spondylolisthesis prior to surgery and at the
end of follow-up (P>0.05).
Complications and recurrence
Complications occurred in 3 patients. A total of 2
small dural tears were detected intra-operatively, which were not
repaired at the time of surgery. No permanent neurological sequelae
were indicated during the follow-up period of these 2 patients. A
single patient with sciatica exhibited sciatica-associated symptoms
for three months following surgery. Non-surgical treatment failed
and this patient underwent micro-decompression surgery. At the
final follow-up, the patient's symptoms of sciatica were relieved.
No post-operative major complications, including neuro-vascular
injury, cauda equina injury or surgical wound infection were
recorded.
Discussion
The use of percutaneous transforaminal endoscopic
techniques is popular in the treatment of patients with lumbar
degenerative diseases (10). DLS
associated with spinal stenosis is a common clinical condition that
significantly contributes to pain and disability, particularly in
the elderly (1). However, few
studies have assessed the application of transforaminal endoscopic
techniques in the treatment of this condition (18,19). The
present retrospective indicated that a cohort of elderly patients
with DLS experienced symptom relief following PTED surgery. The
data of ≥2 years of follow-up demonstrated that transforaminal
endoscopic decompression under local anesthesia is a feasible and
safe procedure, and this technique may provide an alternative
treatment option for a proportion of elderly patients exhibiting
DLS with spinal stenosis.
Open surgery with general anesthesia for the lumbar
spine remains challenging. Multiple factors, including old age,
osteoporosis and other unfavorable factors, may lead to a poor
clinical outcome (20). Furthermore,
residual axial lower back pain and adjacent-segment degeneration
after instrument implantation are commonly indicated in a number of
patients (21). The operation
procedure for DLS may be divided into simple decompression or
decompression combined with fixation (10). The argument for the treatment of DLS
is that arthrodesis is used to enhance the stability of the spine
and avoid the progression of spondylolisthesis. However,
spondylolisthesis has been indicated to rarely progress in adults
(22). Recent studies have
demonstrated that the additional fusion may not yield obvious
clinical improvements over decompression alone, particularly when
minimally invasive decompression is used (1,9). The
extent of resection of the articular joint or ligamentous elements
exhibits a strong influence on the degree of spinal instability
(23). Transforaminal endoscopic
techniques may preserve the biomechanical structure of the surgical
segment and this is improved compared with traditional open
surgery. Therefore, transforaminal endoscopic techniques exert a
minimal impact on spinal stability.
Microendoscopic discectomy (MED) is a reliable
technique for the treatment of DLS (24). During MED, the dorsal ligamentum
flavum and part of the lamina are removed to enlarge the volume of
the spinal canal. In the transforaminal endoscopic decompression
procedure, decompression was achieved via local excision of the
ligamentum flavum and ventral superior articular processes. The
transforaminal endoscopic procedure may preserve the intact
structure of the facet joint capsule. PTED preserves more
structures and MED is able to provide more volume for the spinal
cord and nerve roots involved. Jang et al (25) retrospectively reviewed 21 patients
who underwent MED for spinal stenosis associated with DLS, and the
ODI score was demonstrated to improve from 59.5 to 26.2 at a
minimum follow-up of 3 years. Kelleher et al (26) collected the data of 25 patients with
DLS who reported radicular leg pain without severe back pain and
obvious spinal instability. In that study, following MED surgery,
the ODI score indicated a 48.8% improvement and 77.8% of patients
were satisfied with this surgical treatment at the final follow-up.
In the present study, similar functional improvement was achieved
compared with the outcome of MED reported in the the aforementioned
studies. The mean decrease in the ODI was 36.5 and the mean
decrease of the VAS score of the leg was 5.4 in the present study.
Clinical observations demonstrated that the PTE procedure has a
number of advantages over MED, including decreased incision length,
hospital stay, surgical time, blood loss and muscle damage.
Compared with the MED technique, PTED is associated with a more
rapid recovery and provides improved clinical outcomes for patients
(11,25). However, comparison of the long-term
clinical outcomes between PTED and MED is required in future
studies.
The transforaminal endoscopic procedure may be used
to treat nerve root compression caused by a herniated disc.
However, in DLS, the surgeon should ensure that the ventral and
dorsal nerves are completely decompressed. In the present study,
the dorsal approach decompression procedure was performed using an
endoscopic chisel or trephine to remove hypertrophied superior
articular processes. The intervertebral foramen was then enlarged
under endoscopy to provide a sufficient space for the surgical
procedure. Consequently, it was possible to fully resect the target
hypertrophied ligament flavum. Due to a small space between the
ligamentum flavum and the underlying dural sac, the surgeon should
avoid aggressive manipulation of the dura mater or nerve root
injury. The ventral approach was always performed after the
completion of posterior decompression. To obtain ventral
decompression, a working cannula should be retreated to make its
transition from the dorsal side to the ventral side safe. The
conditions of central stenosis, lateral recess stenosis and
combined stenosis were included in the present cohort. The majority
of patients with DLS are generally associated with lateral recess
stenosis, which is usually caused by a herniated disc, ligamentum
flavum hypertrophy and/or joint capsule hypertrophy (27). With the accumulation of experience,
percutaneous transforaminal endoscopic techniques may be performed
safely, with decreased blood loss and and decreased complication
rates of dural tears and wound infection. The majority of dural
tears are small and do not require repair during surgery. Revision
decompression was required in 5.6% of patients of the present
study, which is similar to the rates in other open surgery studies
(5,28).
The transforaminal and interlaminar approach are two
common operative procedures used in full endoscopic lumbar spine
surgery treatment. The interlaminar approach was initially
developed due to the pelvis, particularly at the L5/S1 level,
obstructing the established working cannular (29,30). In
the present study, all patients with L5/S1-level spondylolisthesis
were operated using the transforaminal approach. The interlaminar
approach provided an advantage in dorsal decompression. However,
extensive exposure of the dural sac may increase the risk of dural
sac injury. Furthermore, general anesthesia is required, as local
anesthesia is not sufficient during this operation due to dural sac
irritation (31). The interlaminar
approach has been indicated to be suitable for the decompression of
central stenosis combined with or without lateral recess stenosis,
and the transforaminal procedure is applied to lateral and/or
foraminal stenosis. However, these indications may change with the
development of surgical instruments and surgeons should use the
technique they are familiar with to achieve reliable clinical
results. Although patients treated with the transforaminal or
interlaminar approach exhibit good short-term clinical outcomes,
long-term follow-up is required to determine whether these outcomes
deteriorate.
In the present study, all samples were collected
from a single research center and the sample size was small, which
may reduce the statistical power of the results and limit the
scientific value of the conclusions drawn. The statistical power of
the present study was calculated for all comparisons. Power
analysis validated the results of ODI, VAS of the leg and back pain
scores between the pre-operative baseline and post-operative month
1 and 3, as well as the final follow-up with >98% certainty.
However, the power for comparison of the percentage of lumbar
spondylolisthesis between the pre-operative baseline and at the end
of the follow-up period was <70%. The results of the comparison
between the percentage of lumbar spondylolisthesis prior to surgery
and at the final follow-up may have been partly affected by the
small sample size. A study assessing a larger sample size should be
performed in the future. The present study was also a retrospective
study based on electronic records. Although the information
regarding the comorbidities of the patients was provided, data on
the severity grading of their pathologies were not obtained. In
addition, PTED techniques continue to evolve, and although patients
treated with such methods exhibit good short-term clinical
outcomes, long-term follow-up is required to determine whether any
deterioration occurs.
In conclusion, the present preliminary study
demonstrated that PTED alone is a feasible and safe procedure for
the treatment of leg-dominant symptoms in elderly patients with
lumbar spinal stenosis that is associated with DLS. No significant
difference was indicated in the percentage of slippage between the
pre-operative stage and the end of the follow-up. The rate of
post-surgical revision was low, with 5.6% of patients requiring a
subsequent micro-decompression surgery at a mean follow-up of 27.7
months. PTED under local anesthesia may also be an efficient
alternative to conventional open lumbar decompression surgery for
the treatment of elderly patients. However, PTED techniques
continue to evolve and the efficacy of this technique requires to
be further evaluated by a long-term follow-up study.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Natural
Science Foundation of China (grant nos. 81772292 and 81270027) and
by the Medico-Engineering cooperation Fund of Shanghai Jiao Tong
University (grant nos. YG2012MS25 and YG2016MS54).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XFL designed the study and drafted the manuscript.
LYJ and XXS recruited the patients and analyzed the data. ZDL and
XJS analyzed the data. KW and HXS collected and analyzed the pre-,
intra- and post-operative data. All authors reviewed and approved
the final manuscript.
Ethics approval and consent to
participate
Ethics approval was obtained from the Ethics
Committee of Renji Hospital (Shanghai, China). All patients
provided written informed consent.
Patient consent for publication
All patients provided consent for publication of
their data and images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Scholler K, Alimi M, Cong GT, Christos P
and Hartl R: Lumbar spinal stenosis associated with degenerative
lumbar spondylolisthesis: A systematic review and meta-analysis of
secondary fusion rates following open vs minimally invasive
decompression. Neurosurgery. 80:355–367. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Resnick DK, Watters WC III, Sharan A,
Mummaneni PV, Dailey AT, Wang JC, Choudhri TF, Eck J, Ghogawala Z,
Groff MW, et al: Guideline update for the performance of fusion
procedures for degenerative disease of the lumbar spine. Part 9:
Lumbar fusion for stenosis with spondylolisthesis. J Neurosurg
Spine. 21:54–61. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Austevoll IM, Gjestad R, Brox JI, Solberg
TK, Storheim K, Rekeland F, Hermansen E, Indrekvam K and Hellum C:
The effectiveness of decompression alone compared with additional
fusion for lumbar spinal stenosis with degenerative
spondylolisthesis: A pragmatic comparative non-inferiority
observational study from the norwegian registry for spine surgery.
Eur Spine J. 26:404–413. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ghogawala Z, Dziura J, Butler WE, Dai F,
Terrin N, Magge SN, Coumans JV, Harrington JF, Amin-Hanjani S,
Schwartz JS, et al: Laminectomy plus fusion versus laminectomy
alone for lumbar spondylolisthesis. N Engl J Med. 374:1424–1434.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ahmad S, Hamad A, Bhalla A, Turner S,
Balain B and Jaffray D: The outcome of decompression alone for
lumbar spinal stenosis with degenerative spondylolisthesis. Eur
Spine J. 26:414–419. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Inose H, Kato T, Yuasa M, Yamada T,
Maehara H, Hirai T, Yoshii T, Kawabata S and Okawa A: Comparison of
decompression, decompression plus fusion, and decompression plus
stabilization for degenerative spondylolisthesis: A prospective,
randomized study. Clin Spine surg. 31:E347–E352. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chang W, Yuwen P, Zhu Y, Wei N, Feng C,
Zhang Y and Chen W: Effectiveness of decompression alone versus
decompression plus fusion for lumbar spinal stenosis: A systematic
review and meta-analysis. Arch Orthop Trauma Surg. 137:637–650.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Alimi M, Hofstetter CP, Pyo SY, Paulo D
and Hartl R: Minimally invasive laminectomy for lumbar spinal
stenosis in patients with and without preoperative
spondylolisthesis: Clinical outcome and reoperation rates. J
Neurosurg Spine. 22:339–352. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Minamide A, Yoshida M, Simpson AK,
Nakagawa Y, Iwasaki H, Tsutsui S, Takami M, Hashizume H, Yukawa Y
and Yamada H: Minimally invasive spinal decompression for
degenerative lumbar spondylolisthesis and stenosis maintains
stability and may avoid the need for fusion. Bone Joint J.
100-B:499–506. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Allen RT and Garfin SR: The economics of
minimally invasive spine surgery: The value perspective. Spine
(Phila Pa 1976). 35 (26 Suppl):S375–S382. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu X, Yuan S, Tian Y, Wang L, Gong L,
Zheng Y and Li J: Comparison of percutaneous endoscopic
transforaminal discectomy, microendoscopic discectomy, and
microdiscectomy for symptomatic lumbar disc herniation: Minimum
2-year follow-up results. J Neurosurg Spine. 28:317–325. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ahn Y, Oh HK, Kim H, Lee SH and Lee HN:
Percutaneous endoscopic lumbar foraminotomy: An advanced surgical
technique and clinical outcomes. Neurosurgery. 75:124–133,
Discussion 132–133. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shin SH, Bae JS, Lee SH, Keum HJ, Kim HJ
and Jang WS: Transforaminal endoscopic decompression for lumbar
spinal stenosis: A novel surgical technique and clinical outcomes.
World Neurosurg. 114:e873–e882. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Li XF, Jin LY, Lv ZD, Su XJ, Wang K, Song
XX and Shen HX: Endoscopic ventral decompression for spinal
stenosis with degenerative spondylolisthesis by partially removing
posterosuperior margin underneath the slipping vertebral body:
Technical note and outcome evaluation. World Neurosurg.
126:e517–e525. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Downie WW, Leatham PA, Rhind VM, Pickup ME
and Wright V: The visual analogue scale in the assessment of grip
strength. Ann Rheum Dis. 37:382–384. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Daltroy LH, Cats-Baril WL, Katz JN, Fossel
AH and Liang MH: The North American spine society lumbar spine
outcome assessment Instrument: Reliability and validity tests.
Spine (Phila Pa 1976). 21:741–749. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Macnab I: Negative disc exploration. An
analysis of the causes of nerve-root involvement in sixty-eight
patients. J Bone Joint Surg Am. 53:891–903. 1971. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jasper GP, Francisco GM and Telfeian AE:
Transforaminal endoscopic discectomy with foraminoplasty for the
treatment of spondylolisthesis. Pain Physician. 17:E703–E708.
2014.PubMed/NCBI
|
|
19
|
Jasper GP, Francisco GM, Aghion D and
Telfeian AE: Technical considerations in transforaminal endoscopic
discectomy with foraminoplasty for the treatment of
spondylolisthesis: Case report. Clin Neurol Neurosurg. 119:84–87.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kim CH, Chung CK, Choi Y, Kim MJ, Kim MJ,
Shin S, Yang SH, Hwang SH, Kim DH, Park SB and Lee JH: increased
proportion of fusion surgery for degenerative lumbar
spondylolisthesis and changes in reoperation rate: A nationwide
cohort study with a minimum 5-year follow-Up. Spine (Phila Pa
1976). 44:346–354. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hsieh MK, Kao FC, Chen WJ, Chen IJ and
Wang SF: The influence of spinopelvic parameters on
adjacent-segment degeneration after short spinal fusion for
degenerative spondylolisthesis. J Neurosurg Spine. 29:407–413.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Winter RB: The natural history of
spondylolysis and spondylolisthesis. J Bone Joint Surg Am.
67:8231985. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zander T, Rohlmann A, Klockner C and
Bergmann G: Influence of graded facetectomy and laminectomy on
spinal biomechanics. Eur Spine J. 12:427–434. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ikuta K, Tono O and Oga M: Clinical
outcome of microendoscopic posterior decompression for spinal
stenosis associated with degenerative spondylolisthesis-minimum
2-year outcome of 37 patients. Minim Invasive Neurosurg.
51:267–271. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Jang JW, Park JH, Hyun SJ and Rhim SC:
Clinical outcomes and radiologic changes after microsurgical
bilateral decompression by a unilateral approach in patients with
lumbar spinal stenosis and grade I degenerative spondylolisthesis
with a minimum 3-year follow-up. Clin Spine Surg. 29:268–271. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kelleher MO, Timlin M, Persaud O and
Rampersaud YR: Success and failure of minimally invasive
decompression for focal lumbar spinal stenosis in patients with and
without deformity. Spine (Phila Pa 1976). 35:E981–E987. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Dijkerman ML, Overdevest GM, Moojen WA and
Vleggeert-Lankamp CLA: Decompression with or without concomitant
fusion in lumbar stenosis due to degenerative spondylolisthesis: A
systematic review. Eur Spine J. 27:1629–1643. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen Z, Zhang L, Dong J, Xie P, Liu B,
Wang Q, Chen R, Feng F, Yang B, Shu T, et al: Percutaneous
transforaminal endoscopic discectomy compared with microendoscopic
discectomy for lumbar disc herniation: 1-year results of an ongoing
randomized controlled trial. J Neurosurg Spine. 28:300–310. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Forsth P, Michaelsson K and Sanden B: Does
fusion improve the outcome after decompressive surgery for lumbar
spinal stenosis?: A two-year follow-up study involving 5390
patients. Bone Joint J. 95-B:960–965. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ruetten S, Komp M and Godolias G: A New
full-endoscopic technique for the interlaminar operation of lumbar
disc herniations using 6-mm endoscopes: Prospective 2-year results
of 331 patients. Minim Invasive Neurosurg. 49:80–87. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Nie H, Zeng J, Song Y, Chen G, Wang X, Li
Z, Jiang H and Kong Q: Percutaneous endoscopic lumbar discectomy
for L5-S1 disc herniation via an interlaminar approach versus a
transforaminal approach: A prospective randomized controlled study
with 2-year follow up. Spine (Phila Pa 1976). 41 (Suppl
19):B30–B37. 2016. View Article : Google Scholar : PubMed/NCBI
|