Introduction
Among the refractive surgery treatments,
laser-mediated corneal epithelial removal, known as transepithelial
photorefractive keratectomy (TransPRK), was performed in the 1990s
(1). Since then, the epithelium has
been removed using excimer laser photo therapeutic keratectomy
followed by refractive ablation of the stroma (two-step approach).
The two-step technique was not widely used due to the long
intervention time, the uneven epithelial removal and treatment
inaccuracy (2,3).
More recently, with the development of the newer
generation of faster lasers and improved ablation algorithms, a
single-step treatment TransPRK was developed on the Schwind Amaris
platform (Schwind eye-tech-solutions GmbH). This one-step approach
allows for simultaneous ablation of the epithelium and the stroma
with little trauma to the eye. Studies using high-frequency digital
ultrasonography have demonstrated that the corneal epithelium does
not have a uniform thickness (4).
The single-step ablation profile was generated from the literature
targets of 55 µm centrally and 65 µm peripherally, using
theoretical simulations for the scope of ablation optical zone (OZ)
(2).
Several studies have determined increased
higher-order wavefront aberrations (HOAs) after corneal refractive
surgery, including PRK (5–7). However, to date, only a few studies
have reported on HOAs associated with single-step TransPRK in
myopia. Adib-Moghaddam et al (8) indicated that corneal spherical, coma
and trefoil aberrations were significantly improved at 18 months
after single-step TransPRK. Other studies comparing TransPRK with
alcohol-assisted PRK indicated that the differences between the
pre- and post-operative HOAs of the same type of surgery were not
significant (9,10). The present study evaluated the
changes of corneal HOAs after TransPRK in myopia and the
association between post-operative changes in HOAs and
pre-operative mean spherical equivalent refraction (MSER),
astigmatism and central corneal ablation depth (CCAD). HOAs in the
eye are closely linked to visual quality after refractive surgery.
The present study investigated the changes in post-operative
corneal HOAs and the correlation between changes in HOA and the
pre-operative diopter (D). It is important to predict
post-operative corneal HOA changes and visual quality.
Materials and methods
Patient population and study
design
The present retrospective study included 80 eyes of
80 patients with myopia who underwent single-step TransPRK between
June 2015 and July 2017 at the Department of Ophthalmology of
Peking University International Hospital (Beijing, China).
The inclusion criteria were as follows: Age >18
years, primary myopia with astigmatism no higher than 3 D, stable
refraction for at least 12 months, discontinued contact lens use
for at least 2–4 weeks (depending on the type of lens) prior to the
surgery, corrected distance visual acuity (CDVA) of 20/25 or
better. Exclusion criteria were abnormal or keratoconic topography,
post-operative corneal bed thickness of <325 µm, dry eye and
other types of diagnosed ocular disease, a history of ocular trauma
and pregnancy.
Pre-operative examination
Pre-operative examination included uncorrected
distance visual acuity (UDVA), CDVA, manifest and cycloplegic
refraction, intraocular pressure, slit lamp biomicroscopy, corneal
topography, dilated fundus evaluation and ultrasound corneal
pachymetry.
Wavefront measurement
Wavefront errors in each eye were measured
pre-operatively and at 1 year after single-step TransPRK using a
rotating Scheimpflug Camera (Pentacam Scheimpflug topography;
Oculus). Patients with no haze and without dry eye were recruited
for the study and the examined eye was selected at random. The
examination was performed in a dark room (11,12).
HOAs with a 6.0-mm analysis diameter were calculated separately for
the anterior and posterior corneal surfaces and for the total
cornea. The root-mean-square (µm) of coma (Z31), trefoil
(Z33) and spherical aberration (Z40) were
analyzed, as they are clinically significant in terms of visual
performance (7). The values of each
HOA (coma, trefoil, spherical and total HOA) were determined at the
post- and pre-operative stage.
Surgical technique
All surgeries were performed using an Amaris 500E
excimer laser platform (Schwind eye-tech-solutions GmbH) with its
integrated ORK-CAM software. The epithelium and stroma were ablated
in a single step. For each treatment, the epithelial thickness
profile was 55 µm centrally and 65 µm peripherally based on
population statistics. The ablation plan provides an even
application of laser energy on the surface of the entire cornea and
the OZ diameter was 6.30 mm.
After the surgery, the cornea was irrigated with a
cooled balanced salt solution and a bandage contact lens was
applied.
Post-operative medication and
protocol
After the surgery, the patients were instructed to
use 0.5% levofloxacin (Cravit; Santen, Inc.) four times daily for
one week, 0.1% fluorometholone drops (Allergan, Inc.) four times
daily (tapered over 12 weeks) and preservative-free artificial
tears four times daily for six months. The contact lens was removed
two to three days after the surgery when corneal
re-epithelialization was completed.
Statistical analysis
Statistical analysis was performed using SPSS 19.0
(IBM Corp.). To assess changes in the parameters following surgery,
Student's t-test was used to compare pre-operative and
post-operative mean values. The change in HOA was calculated as the
difference between the post- and pre-operative value. The
correlation between the changes in HOA and pre-operative MSER, mean
astigmatism and CCAD were tested by calculating the Pearson
correlation coefficient. P<0.05 was considered to indicate a
statistically significant difference.
Results
Patient characteristics
The demographic data of the patients of the present
study are listed in Table I.
Table II provides a comparative
analysis of refractive components (sphere, cylinder, SE refraction)
and LogMAR visual acuities prior to and at 1 year after
surgery.
 | Table I.Demographic data for the cohort of 80
eyes. |
Table I.
Demographic data for the cohort of 80
eyes.
| Parameter | Mean ± SD | Range |
|---|
| Age (y) | 28.9±5.5 | 18–37 |
| Sex |
|
|
| Male | 30.5±6.6 | 18–37 |
|
Female | 28.2±5.0 | 19–37 |
| Number (n) |
|
|
| Male | 11 |
|
|
Female | 29 |
|
 | Table II.Summary of the data of the cohort at
the pre-operative stage and at 1 year post-operatively (n=80). |
Table II.
Summary of the data of the cohort at
the pre-operative stage and at 1 year post-operatively (n=80).
| Parameter | Pre-operation | 1 Year
post-operatively | P-value |
|---|
| Sphere (D) |
|
| <0.001 |
| Mean ±
SD | −3.96±1.22 | 0.21±0.48 |
|
|
Range | −6.75, −0.50 | −1.25, 1.25 |
|
| Cylinder (D) |
|
| <0.001 |
| Mean ±
SD | −0.59±0.54 | −0.29±0.25 |
|
|
Range | −2.00, 0.00 | −1.00, 0.50 |
|
| SER (D) |
|
| <0.001 |
| Mean ±
SD | −4.19±1.35 | 0.05±0.46 |
|
|
Range | −7.15, −0.50 | −1.38, 1.00 |
|
| UCVA (logMAR) |
|
| <0.001 |
| Mean ±
SD | 0.97±0.26 | −0.10±0.08 |
|
|
Range | 0.40, 1.50 | −0.20, 0.10 |
|
| CDVA (logMAR) |
|
|
|
| Mean ±
SD | −0.10±0.08 | −0.14±0.07 | <0.001 |
|
Range | −0.20, 0.00 | −0.20, 0.00 |
|
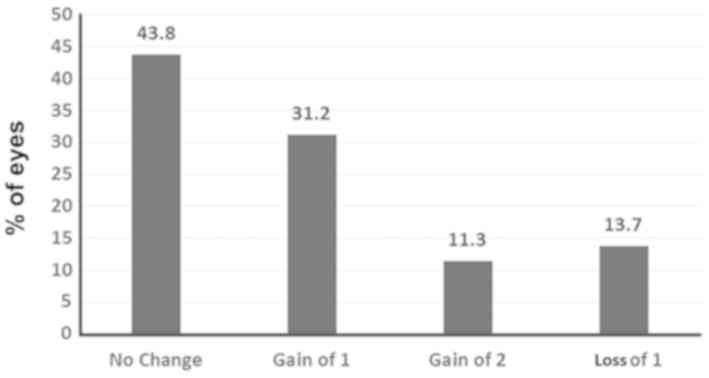
CDVA and UDVA
Fig. 1 presents the
percentage change in CDVA. The CDVA was increased post-operatively
(P<0.001) in a certain proportion of eyes and remained the same
in 43.8% of the eyes. A total of 31.7% of eyes gained one Snellen
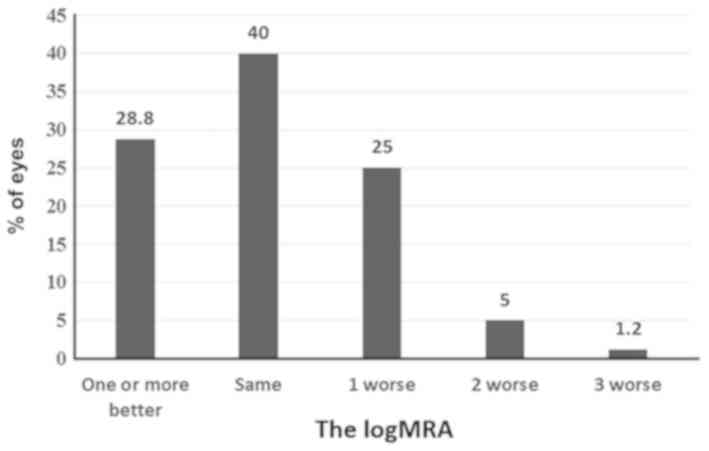
line of CDVA and no eye lost ≥2 lines of CDVA. Fig. 2 provides the difference between
post-operative UDVA and pre-operative CDVA. The post-operative UDVA
was the same or superior compared with the pre-operative CDVA in
~69% of the eyes.
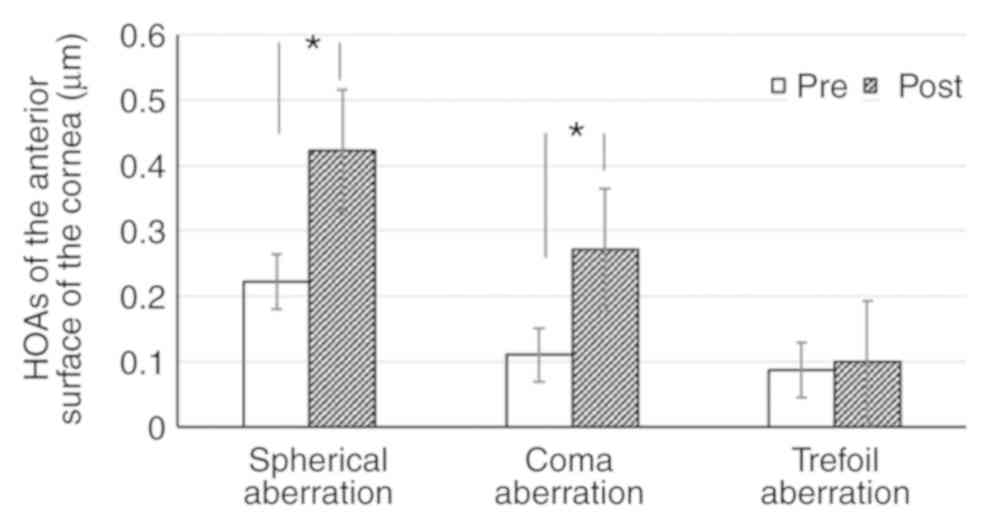
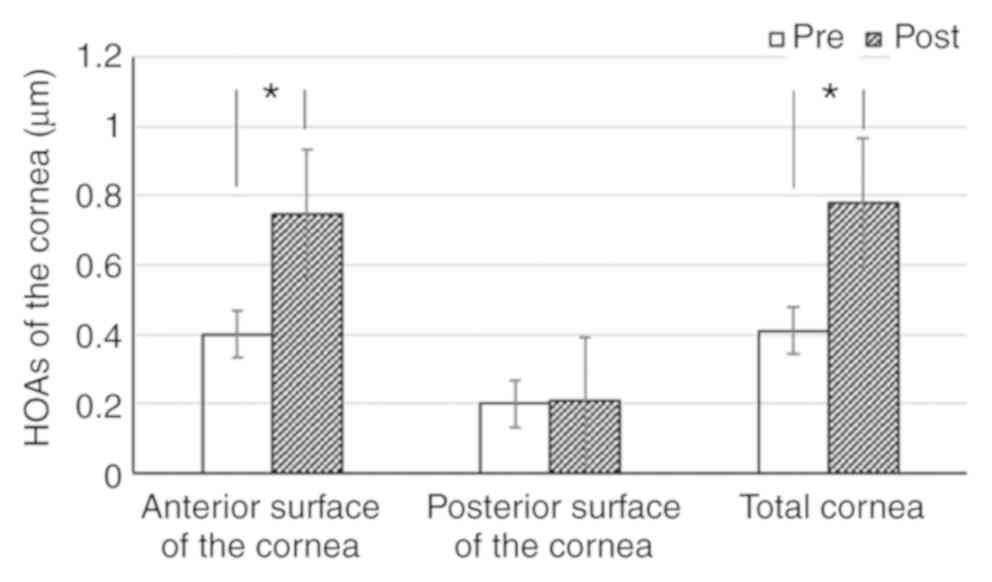
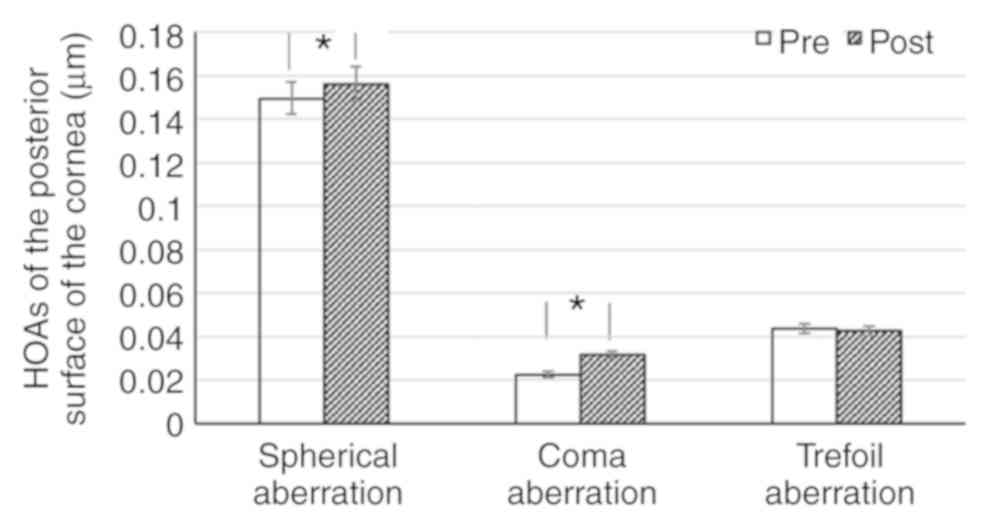
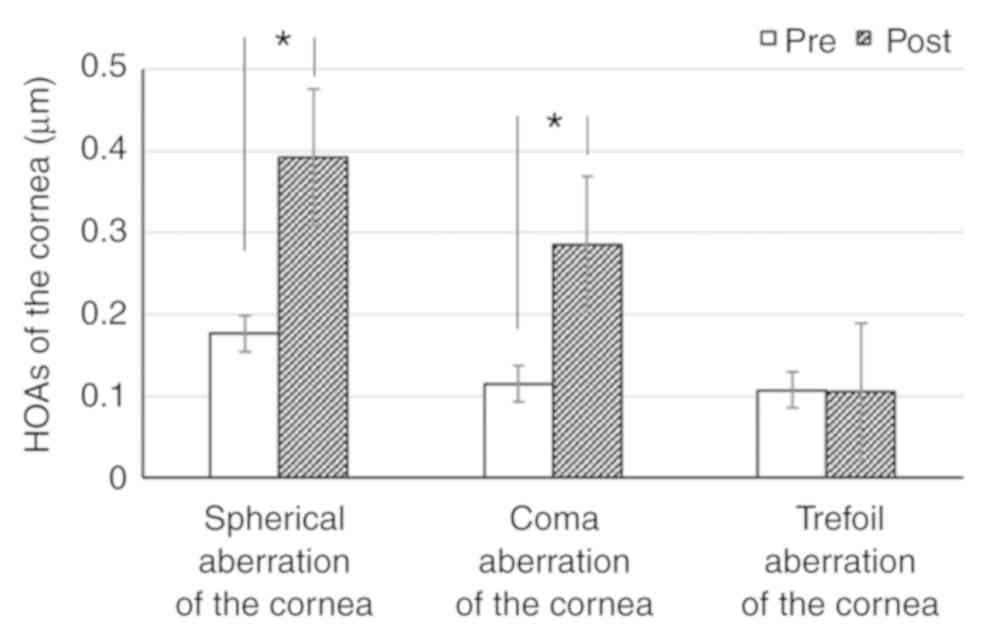
Changes in HOAs
Table III and
Figs. 3–6 present the changes in HOAs of the cornea.
Compared with the pre-operative values, the spherical and coma
aberration of the anterior (Fig. 3),
posterior (Fig. 4) and total cornea
(Fig. 5) were significantly
increased post-operatively (P<0.001). By contrast, the trefoil
was not significantly affected (P=0.262, 0.805 and 0.936,
respectively). The total HOAs of the anterior surface and total
cornea were significantly increased (P<0.001); however, the
posterior surface of the cornea was not significantly changed
(P=0.303; Fig. 6).
 | Table III.Changes in HOAs of the cornea. |
Table III.
Changes in HOAs of the cornea.
| A, Anterior |
|---|
|
|---|
| Measured outcome | Spherical
aberration | Coma | Trefoil | HOA
root-mean-square |
|---|
| Pre-operative | 0.22±0.08 | 0.11±0.08 | 0.09±0.07 | 0.40±0.09 |
| Post-operative | 0.42±0.19 | 0.27±0.21 | 0.10±0.07 | 0.75±0.25 |
| P-value | <0.001 | <0.001 | 0.262 | <0.001 |
|
| B,
Posterior |
|
| Measured
outcome | Spherical
aberration | Coma | Trefoil | HOA
root-mean-square |
|
| Pre-operative | 0.15±0.03 | 0.02±0.02 | 0.04±0.04 | 0.20±0.04 |
| Post-operative | 0.16±0.03 | 0.03±0.03 | 0.04±0.03 | 0.21±0.06 |
| P-value | <0.001 | <0.001 | 0.805 | 0.303 |
|
| C, Total |
|
| Measured
outcome | Spherical
aberration | Coma | Trefoil | HOA
root-mean-square |
|
| Pre-operative | 0.18±0.08 | 0.11±0.10 | 0.11±0.08 | 0.41±0.012 |
| Post-operative | 0.39±0.20 | 0.29±0.22 | 0.11±0.08 | 0.78±0.26 |
| P-value | <0.001 | <0.001 | 0.936 | <0.001 |
Correlations
The correlations between changes in the HOA of the
anterior cornea and pre-operative MSER, mean astigmatism and CCAD
are presented in Table IV.
Significant correlations of the pre-operative MSER, astigmatism and
CCAD with the change of coma aberration (r=0.268, P=0.016; r=0.260,
P=0.02; r=0.323, P=0.004, respectively) and HOA (r=0.554,
P<0.001; r=0.312, P=0.005; r=0.583, P<0.001, respectively) of
the anterior cornea were determined. The change in spherical
aberration of the anterior cornea was significantly correlated with
pre-operative MSER (r=0.462, P<0.001) and CCAD (r=0.510,
P<0.001), but not with astigmatism (P=0.09). However, the change
in trefoil was only significantly correlated with pre-operative
astigmatism (r=−0.279, P=0.012).
 | Table IV.Pearson correlation analysis between
changes in HOA of the anterior cornea and pre-operative MSER,
astigmatism and CCAD. |
Table IV.
Pearson correlation analysis between
changes in HOA of the anterior cornea and pre-operative MSER,
astigmatism and CCAD.
|
| Spherical
aberration (post-pre) | Coma aberration
(post-pre) | Trefoil aberration
(post-pre) | HOA (post-pre) |
|---|
|
|
|
|
|
|
|---|
| Parameter | R | P-value | R | P-value | R | P-value | R | P-value |
|---|
| MSER | 0.462 | <0.001 | 0.268 | 0.016 | 0.087 | 0.442 | 0.554 | <0.001 |
| Astigmatism | 0.191 | 0.090 | 0.260 | 0.020 | −0.279 | 0.012 | 0.312 | 0.005 |
| CCAD | 0.510 | <0.001 | 0.323 | 0.004 | 0.014 | 0.901 | 0.583 | <0.001 |
Discussion
The present study revealed a significant improvement
in SE, astigmatism, UDVA and CDVA in eyes with myopia after
one-step TransPRK. Of note, ~96% eyes had a UDVA of 20/20 or
better, with >95% treated eyes within ±1.00D of the intended
target refraction and no eye lost two or more Snellen lines of
CDVA. It was demonstrated that one-step TransPRK was able to
correct myopia effectively. Previous clinical studies also
confirmed the efficacy and safety of one-step TransPRK in the
correction of myopia (8,9,13,14).
One other study proved that HOA values of the
anterior surface were significantly higher compared with the HOA
values of the total cornea (5).
According to the pre-operative analysis of wavefront aberration in
the present study, the spherical aberration of the anterior corneal
surface proved to be significantly higher compared with the
spherical aberration of the total cornea. This suggested that the
posterior corneal surface may have a compensatory role in the
balance of spherical aberration in myopic eyes. Pentacam is a
commonly used multi-function instrument for analyzing corneal
topography in patients at the pre-operative stage. It may also be
used to analyze HOAs of patients' corneas. The use of Pentacam to
analyze the HOAs of the patients prior to and after surgery is of
clinical guiding significance.
In the present study, the spherical and coma
aberration of the anterior, posterior and total cornea were
significantly increased post-operatively. Compared with the
pre-operative values, the trefoil aberration was not significantly
affected, nor were the HOAs of the posterior corneal surface.
Induced HOAs after one-step TransPRK may be attributed to various
factors. A certain extent of decentration during keratorefractive
surgery, fluctuations in accommodation and changes of tear film
after surgery have been reported in the induction of HOAs (7,15). By
using very high-frequency digital ultrasonography, Reinstein et
al (4) determined that the
corneal epithelium was thicker inferiorly than superiorly and
thicker nasally than temporally. Unequal pre-operative epithelial
thickness may potentially be a source of HOAs. Another factor for
the increase of HOAs may be the changes in epithelial thickness
after surgery. Hou et al (16) assessed the characteristics of
epithelial thickening, indicating that the epithelium was thicker
inferiorly than superiorly and temporally than nasally after
TransPRK. Following PRK, Chen et al (17) observed a maximum amount of epithelial
thickening temporally.
The present study analyzed the correlation between
changes in corneal HOAs and pre-operative diopter and depth of cut,
which is significant to predict the changes in post-operative
corneal HOAs. The increase in HOAs of the anterior cornea was
linearly correlated with the pre-operative MSER, the mean
astigmatism and the CCAD. Pre-operative astigmatism was
significantly associated with the post-operative increases in
trefoil aberration but not with spherical aberration. According to
these results, the diopter of myopia and the ablation depth should
be considered as important factors for increased HOAs. In patients
with a higher MSER prior to surgery, the chances of increased HOAs
after surgery are increased. This may be one of the factors
affecting the visual quality following myopia surgery. The
biomechanical response of the cornea tissue may be changed after
the surgery, which may then induce HOAs to a certain extent.
Astigmatism may have an increased effect on the trefoil. In
patients with high astigmatism refraction, the trefoil should be
monitored post-operatively.
In conclusion, the present study demonstrated the
effectiveness of TransPRK for the treatment of myopia. The total
HOAs of the anterior surface of the cornea and further aberrations,
including spherical and coma aberrations, were increased
post-operatively. The increased HOAs were linearly correlated with
the degree of pre-operative myopia and CCAD. The increase in the
trefoil was only significantly correlated with the degree of
pre-operative astigmatism. There is a requirement for further study
of the predictability of the treatment algorithm used in one-step
TransPRK.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LX performed the study, participated in the design,
drafted the manuscript, revised the manuscript and gave final
approval of the version for publication.
Ethics approval and consent to
participate
The study was performed in accordance with the
Declaration of Helsinki and was approved by the Ethics Committee of
the Peking University International Hospital (Beijing, China).
Patients included in the present study had complete clinical data
and cooperated with the medical staff to complete the relevant
medical treatment. Written informed consent was obtained from the
patients and/or their guardians.
Patient consent for publication
Not applicable.
Competing interests
The author declared that he has no competing
interests.
References
|
1
|
Clinch TE, Moshirfar M, Weis JR, Ahn CS,
Hutchinson CB and Jeffrey JH: Comparison of mechanical and
transepithelial debridement during photorefractive keratectomy.
Ophthalmology. 106:483–489. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Arba Mosquera S and Awwad ST: Theoretical
analyses of the refractive implications of transepithelial PRK
ablations. Br J Ophthalmol. 97:905–911. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ghadhfan F, Al-Rajhi A and Wagoner MD:
Laser in situ keratomileusis versus surface ablation: Visual
outcomes and complications. J Cataract Refract Surg. 33:2041–2048.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Reinstein DZ, Archer TJ, Gobbe M,
Silverman RH and Coleman DJ: Epithelial thickness in the normal
cornea: Three-dimensional display with Artemis very high-frequency
digital ultrasound. J Refract Surg. 24:571–581. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Juhasz E, Kranitz K, Sandor GL, Gyenes A,
Toth G and Nagy ZZ: Wavefront properties of the anterior and
posterior corneal surface after photorefractive keratectomy.
Cornea. 3:172–176. 2014. View Article : Google Scholar
|
|
6
|
Serrao S, Lombardo G, Ducoli P and
Lombardo M: Long-term corneal wavefront aberration variations after
photorefractive keratectomy for myopia and myopic astigmatism. J
Cataract Refract Surg. 37:1655–1666. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lee SB, Hwang BS and Lee J: Effects of
decentration of photorefractive keratectomy on the induction of
higher orderwavefront aberrations. J Refract Surg. 26:731–743.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Adib-Moghaddam S, Soleyman-Jahi S,
Salmanian B, Omidvari AH, Adili-Aghdam F, Noorizadeh F and Eslani
M: Single-step transepithelial photorefractive keratectomy in
myopia and astigmatism: 18-month follow-up. J Cataract Refract
Surg. 42:1570–1578. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kaluzny BJ, Cieslinska I, Mosquera SA and
Verma S: Single-step transepithelial PRK vs Alcohol-assisted PRK in
myopia and compound myopic astigmatism correction. Medicine
(Baltimore). 95:e19932016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Aslanides IM, Padroni S, Arba Mosquera S,
Ioannides A and Mukherjee A: Comparison of single-step reverse
transepithelial all-surface laser ablation (ASLA) to
alcohol-assisted photorefractive keratectomy. Clin Ophthalmol.
6:973–980. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Miháltz K, Kovács I, Takács A and Nagy ZZ:
Evaluation of keratometric, pachymetric, and elevation parameters
of keratoconic cornea with pentacam. Cornea. 28:976–980. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bastawrous A, Silvester A and Batterbury
M: Laser refractive eye surgery. BMJ. 342:d23452011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Aslanides IM, Georgoudis PN, Selimis VD
and Mukherjee AN1: Single-step transepithelial ASLA (SCHWIND) with
mitomycin-C for the correction of high myopia: Long term follow-up.
Clin Ophthalmol. 9:33–41. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Luger MH, Ewering T and Arba-Mosquera S:
Myopia correction with transepithelial photorefractive keratectomy
versus femtosecond assisted laser in situ keratomileusis: One-year
case-matched analysis. J Cataract Refract Surg. 42:1579–1587. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Artal P, Chen L, Fernández EJ, Singer B,
Manzanera S and Williams DR: Adaptive optics for vision: The eye's
adaptation to point spread function. J Refract Surg. 19
(Suppl):S585–S587. 2003.PubMed/NCBI
|
|
16
|
Hou J, Wang Y, Lei Y, Zheng X and Zhang Y:
Corneal epithelial remodeling and its effect on corneal asphericity
after transepithelial photorefractive keratectomy for myopia. J
Ophthalmol. 2016:85823622016.PubMed/NCBI
|
|
17
|
Chen X, Stojanovic A, Liu Y, Chen Y, Zhou
Y and Utheim TP: Postoperative changes in corneal epithelial and
stromal thickness profiles after photorefractive keratectomy in
treatment of myopia. J Refract Surg. 31:446–453. 2015. View Article : Google Scholar : PubMed/NCBI
|