Introduction
Incidence of type 2 diabetes mellitus (T2DM) has
been rising each year due to trends in population aging. It has
been estimated that by 2040, there will be 615 million people
suffering from T2DM (1). Meanwhile,
morbidity of cognitive impairment (CI) increases as patients age.
Some studies have documented that the incidence rate of CI is 5–10%
in patients over 65 years old and 20–50% in patients over 85 years,
with a higher prevalence in women than in men (2). Stroke is believed to be the second
biggest factor in inducing CI (3).
There have been studies revealing that T2DM is one of the common
risk factors in causing stoke and CI. Thus patients with T2DM are
more likely to have cognitive dysfunction after a stroke (4–6).
Regarding the pathogenesis, it has been reported
that T2DM and CI share common lesion characteristics including Aβ
gathering, decreased ability in regulating protein phosphorylation,
and participation of chronic inflammatory factors; moreover,
insulin resistance and damage to insulin signal transmission are
also common pathological bases in the occurrence of both diseases
(7,8). Glucagon-like peptide-1 (GLP-1) is an
endogenous incretin. It can promote the release of insulin from
islet cell and keep the glucose content at a relatively stable
level in the body (9). Some recent
studies have demonstrated that GLP-1 can not only affect pancreatic
islet function but also display neurotransmitter-like and neuron
growth factor-like properties (10).
GLP-1 agents, such as liraglutide and exenatide, have been
demonstrated to be able to mitigate neurodegeneration in
Alzheimer's disease (AD) and decrease memory and learning
disabilities when used in the rat model of AD (11,12).
However, some studies have found that GLP-1 gets readily hydrolyzed
by dipeptidyl peptidase-4 (DPP-4) in the body, causing loss of
activity and function. DPP-4 inhibitors including sitagliptin,
vildagliptin, and linagliptin reduce sugar level mainly through
inhibiting GLP-1 hydrolysis (13).
Currently, studies regarding the improvement of cognitive ability
by DPP-4 were primarily carried out among patients with AD, whereas
studies performed in patients with T2DM combined with post-stroke
mild cognitive impairment (MCI) were few (14,15).
Therefore, in the present study, we used DPP-4 inhibitor in
treating elderly patients with T2DM combined with post-stroke MCI
and investigated its effect on patients' blood sugar level and
cognitive ability.
Materials and methods
Patient characteristics
The present study was approved by the Ethics
Committee of Heilongjiang Provincial Hospital, (Harbin, China) and
informed consent was obtained from all individuals included in this
study. Sixty patients treated in the department of neurology in
Heilongjiang Provincial Hospital between January 2017 and June 2018
for T2DM combined with post-stroke CI were selected and randomized
into a study group (treated with DPP-4 inhibitor) and a control
group (treated with sulfonylurea) of 30 patients each. All patients
were aged above 65 years.
Inclusion criteria were as follows: i) Patients who
met the diagnostic criteria for T2DM (16); ii) patients who met the diagnostic
criteria for post-stroke CI after assessment of cognitive ability
and the condition was stabilized after treatment (17); iii) patients who met the following
four criteria for MCI: a) patients with a score of ≥24 points in
Mini-Mental State Examination (MMSE, 19 items, total score of 30
points); b) patients with a score of <26 points in Montreal
Cognitive Assessment (MoCA) if they had over 12 years of education
(one point was added to the MoCA score if patients did not have
over 12 years of education); c) patients were reported by
themselves or their family members to have hypomnesia; d) activity
of daily living score <26 points (18); iv) patients had diabetes before
stroke occurrence, and the antidiabetic drugs patients received
were sulfonylurea and metformin instead of DPP-4 inhibitor.
Exclusion criteria were: i) Patients who were
allergic to DPP inhibitor; ii) patients who had histories of
craniocerebral trauma, epilepsy, and cerebrovascular disease; iii)
patients who would not cooperate with cognitive testing; iv)
patients who were taking glucocorticoid which would affect blood
sugar level; v) patients who had cardiopulmonary insufficiency; vi)
patients who had malignant tumors; vii) patients who had mental
illness which would affect cognition.
Methods
According to a random number table, patients in the
study were assigned to either a study group or a control group of
30 patients each. In the study group, patients received oral
administration of 100 mg sitagliptin (Merck Sharp & Dohme,
Ltd., registration number for imported medicine: H20090834), a
DPP-4 inhibitor, one time per day and one pill each time;
meanwhile, patients in the control group received sulfonylurea. If
the blood sugar level was not lowered effectively, regular insulin
would be administered temporarily to control the sugar content.
Efficacy was evaluated at six months after treatment.
Outcome measures
Main outcome measures were: i) fasting blood glucose
(FBG), 2-hour postprandial blood glucose (2hPG), and hemoglobin A1c
(HbA1c) values before and six months after treatment; FBG and 2hPG
were measured using Accu-Chek Performa blood glucose meter (Roche),
while HbA1c was measured using DCA 2000 analyzer (Bayer); ii) MMSE
and MoCA scores before and six months after treatment for cognitive
evaluation.
Secondary outcome measures included C-reactive
protein (CRP), tumor necrosis factor (TNF)-α, interleukin (IL)-6,
and Aβ1–40 and Aβ1–42 values. Two tubes of venous blood (5 ml each)
were collected from each patient at 8′clock in the morning before
and six months after treatment. The blood samples were placed in
sterile EDTA tubes and kept in a fridge at 4°C for 15 min.
Afterward, samples were centrifuged at 1,500 × g at 4°C for 30 min
to separate serum from plasma. The plasma was incubated with
phosphate buffered saline containing 40 µl protease inhibitor at
−80°C. Levels of CRP, TNF-α, and IL-6 in serum were measured using
immunoturbidimetry, while values of Aβ1–40 and Aβ1–42 in plasma
were measured using ELISA.
Statistical analysis
SPSS 17.0 software was applied for statistical
analysis. Continuous variables are expressed as mean ± SD. t-test
was performed if there were normal distribution and homogeneity of
variance; comparison between two groups was conducted by
independent-samples t-test; before versus after comparison within
the group was performed by paired t-test; quartile was presented,
and Wilcoxon rank-sum test was conducted if there were no normal
distribution and homogeneity of variance. Pearson's Chi-squared
test was performed for count data. P<0.05 was considered to
indicate a statistically significant difference.
Results
Patient characteristics
There were no intergroup differences in sex, age,
education background, body mass index, and comorbidities so that
the results were comparable (all P>0.05, Table I).
 | Table I.Patient characteristics and baseline
data. |
Table I.
Patient characteristics and baseline
data.
|
Characteristics | Study group
(n=30) | Control group
(n=30) | χ2/t
value | P-value |
|---|
| Sex
(male:female) | 17:13 | 14:16 | 0.601 | 0.438 |
| Age (years) | 68.5±7.1 | 67.4±5.9 | 0.692 | 0.492 |
| Education
(year) | 12.5±3.8 | 11.9±4.0 | 0.627 | 0.533 |
| Body mass index
(kg/m2) | 25.71±3.76 | 25.59±4.28 | 0.110 | 0.913 |
| Diabetes
duration |
8.17±3.05 |
8.97±2.65 | 0.534 | 0.128 |
| Stroke type |
|
| 0.268 | 0.605 |
|
Ischemic stroke | 15 | 17 |
|
|
|
Hemorrhagic stroke | 15 | 13 |
|
|
| Comorbidity |
|
|
|
|
|
Hyperlipemia |
|
| 0.067 | 0.759 |
|
Yes | 17 | 16 |
|
|
|
No | 13 | 14 |
|
|
|
Hypertension |
|
| 0.635 | 0.426 |
|
Yes | 20 | 17 |
|
|
|
No | 10 | 13 |
|
|
|
Coronary heart disease |
|
| 0.287 | 0.592 |
|
Yes | 10 | 12 |
|
|
|
No | 20 | 18 |
|
|
|
Obesity |
|
| 0.635 | 0.426 |
|
Yes | 10 | 13 |
|
|
|
No | 20 | 17 |
|
|
|
Hyperhomocysteinemia |
|
| 0.373 | 0.542 |
|
Yes | 22 | 24 |
|
|
|
No | 8 | 6 |
|
|
|
Hyperuricemia |
|
| 0.693 | 0.405 |
|
Yes | 19 | 22 |
|
|
|
No | 11 | 8 |
|
|
Sugar blood content before and after
treatment in the two groups
No intergroup differences were found in FBG, 2hPG,
and HbA1c in the two groups before and after treatment (all
P>0.05). Compared with the pretreatment values, these markers
improved significantly six months after treatment (all P<0.05)
(Table II).
 | Table II.Sugar blood content before and after
treatment in the two groups. |
Table II.
Sugar blood content before and after
treatment in the two groups.
| Sugar blood
content | Study group Before
treatment | Control group
Before treatment | t value | P-value | Study group After
treatment | Control group After
treatment | t value | P-value |
|---|
| FBG (mmol/l) |
9.51±1.24 |
9.29±1.32 | 0.666 | 0.508 |
7.19±1.81a |
7.17±1.77a | 0.050 | 0.960 |
| 2hPG (mmol/l) | 16.89±3.77 | 16.70±4.69 | 0.170 | 0.866 |
10.47±3.80a |
10.56±2.59a | 0.103 | 0.918 |
| HbA1c (%) |
8.56±1.25 |
8.86±3.17 | 0.471 | 0.640 |
6.97±1.25a |
7.35±2.48a | 0.749 | 0.457 |
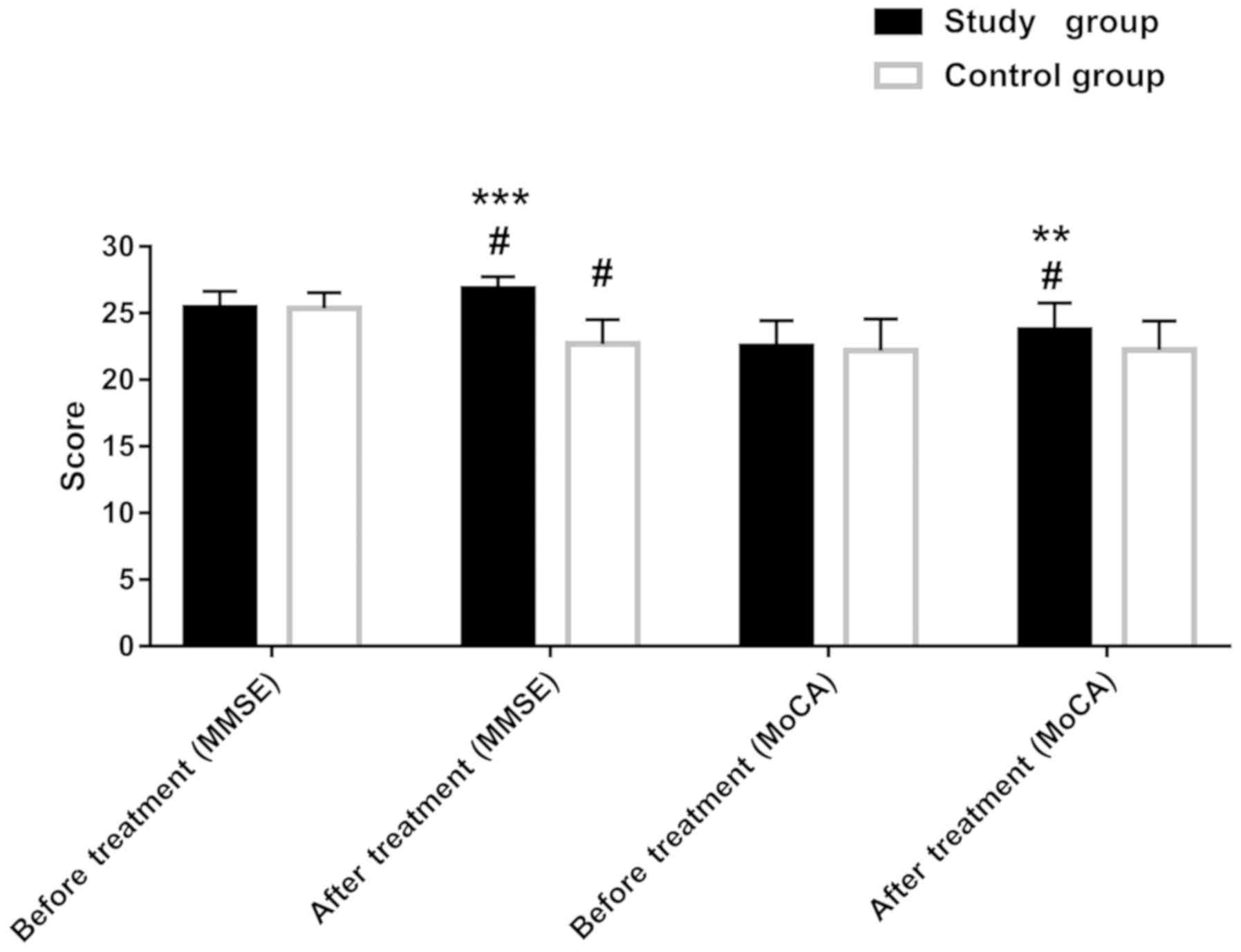
Cognitive ability before and after
treatment in the two groups
No intergroup differences were found in MMSE and
MoCA scores in the two groups before treatment (both P>0.05).
However, at six months after treatment, the MMSE and MoCA scores in
the study group improved significantly compared with the
pretreatment scores (both P<0.05). In the control group, the
MMSE score was lower than that before the treatment (P<0.05).
Differences were observed between the two groups regarding these
scores after treatment (both P<0.01). (Table III and Fig. 1).
 | Table III.Score of cognitive ability before and
after treatment in the two groups. |
Table III.
Score of cognitive ability before and
after treatment in the two groups.
| Scores | Study group Before
treatment | Control group
Before treatment | t value | P-value | Study group After
treatment | Control group After
treatment | t value | P-value |
|---|
| MMSE | 25.42±1.22 | 25.37±1.16 | 0.108 | 0.914 |
26.83±0.91a |
22.70±1.80a | 11.201 | <0.001 |
| MoCA | 22.50±1.94 | 22.20±2.35 | 0.538 | 0.592 |
23.73±2.03a | 22.23±2.18 |
2.759 | 0.008 |
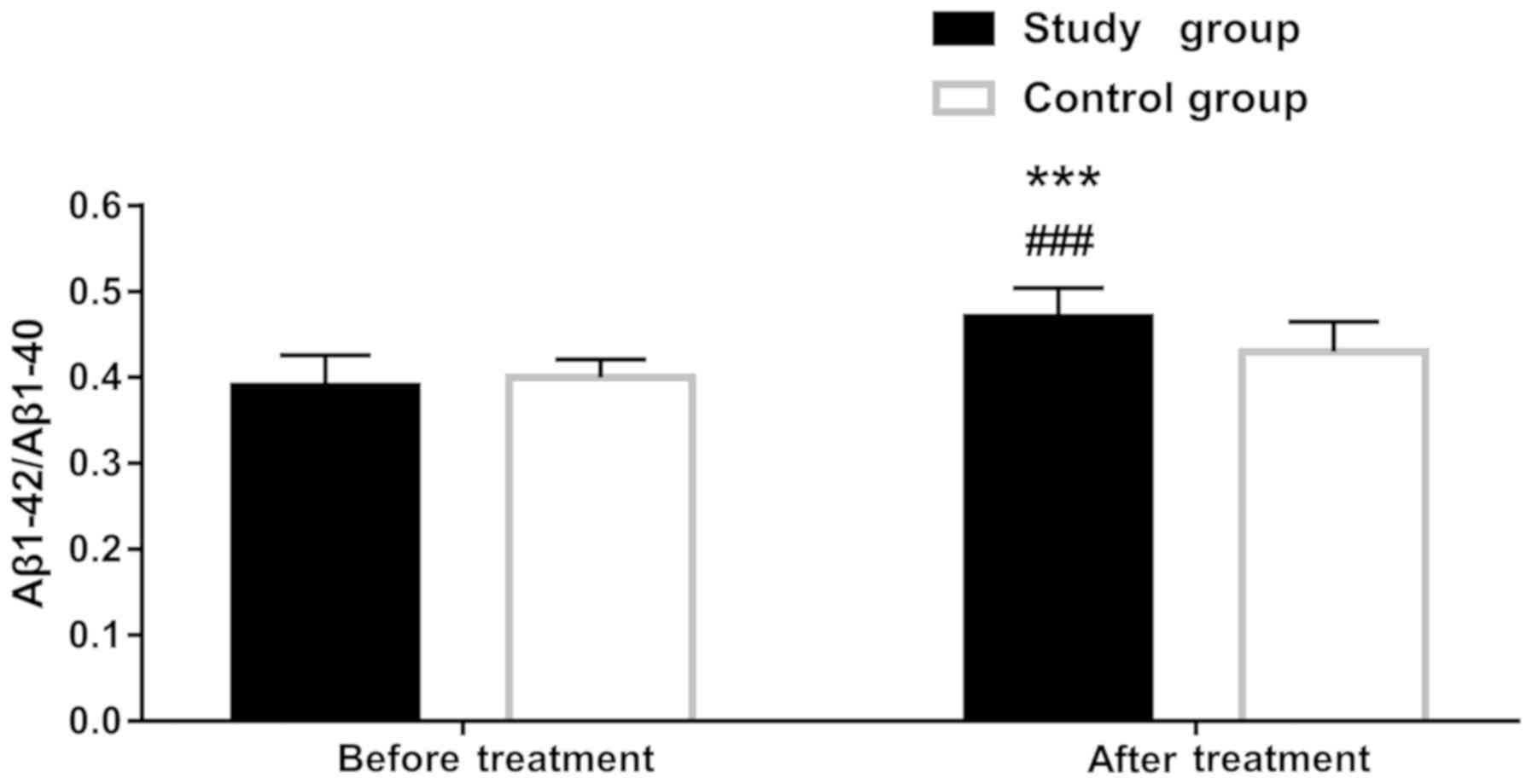
Aβ1-42, Aβ1-40, and Aβ1-42/Aβ1–40 levels in plasma
before and after treatment in the two groups. There were no
intergroup differences in Aβ1-42, Aβ1-40, and Aβ1-42/Aβ1–40 levels
before treatment (all P>0.05). However, at six months after
treatment, the value of Aβ1-42/Aβ1–40 improved significantly in the
study group (P<0.001), whereas the levels of the other two
markers were similar to those before treatment (both P>0.05).
Aβ1-42/Aβ1–40 value differed between the two groups after treatment
(P<0.05) (Table IV and Fig. 2).
 | Table IV.Aβ1-42, Aβ1-40, and Aβ1-42/Aβ1–40
levels in plasma before and after treatment in the two groups. |
Table IV.
Aβ1-42, Aβ1-40, and Aβ1-42/Aβ1–40
levels in plasma before and after treatment in the two groups.
| Markers | Study group Before
treatment | Control group
Before treatment | t value | P-value | Study group After
treatment | Control group After
treatment | t value | P-value |
|---|
| Aβ1–42 (ng/l) | 18.37±5.08 | 17.73±4.64 | 0.504 | 0.616 | 19.03±3.17 | 19.40±5.05 | 0.337 | 0.737 |
| Aβ1–40 (ng/l) | 46.50±11.19 | 43.80±9.98 | 0.987 | 0.328 | 41.03±9.18 | 44.97±10.83 | 1.517 | 0.135 |
| Aβ1-42/Aβ1–40 | 0.39±0.04 |
0.40±0.02 | 1.445 | 0.154 |
0.47±0.03a | 0.43±0.04 | 4.649 | <0.001 |
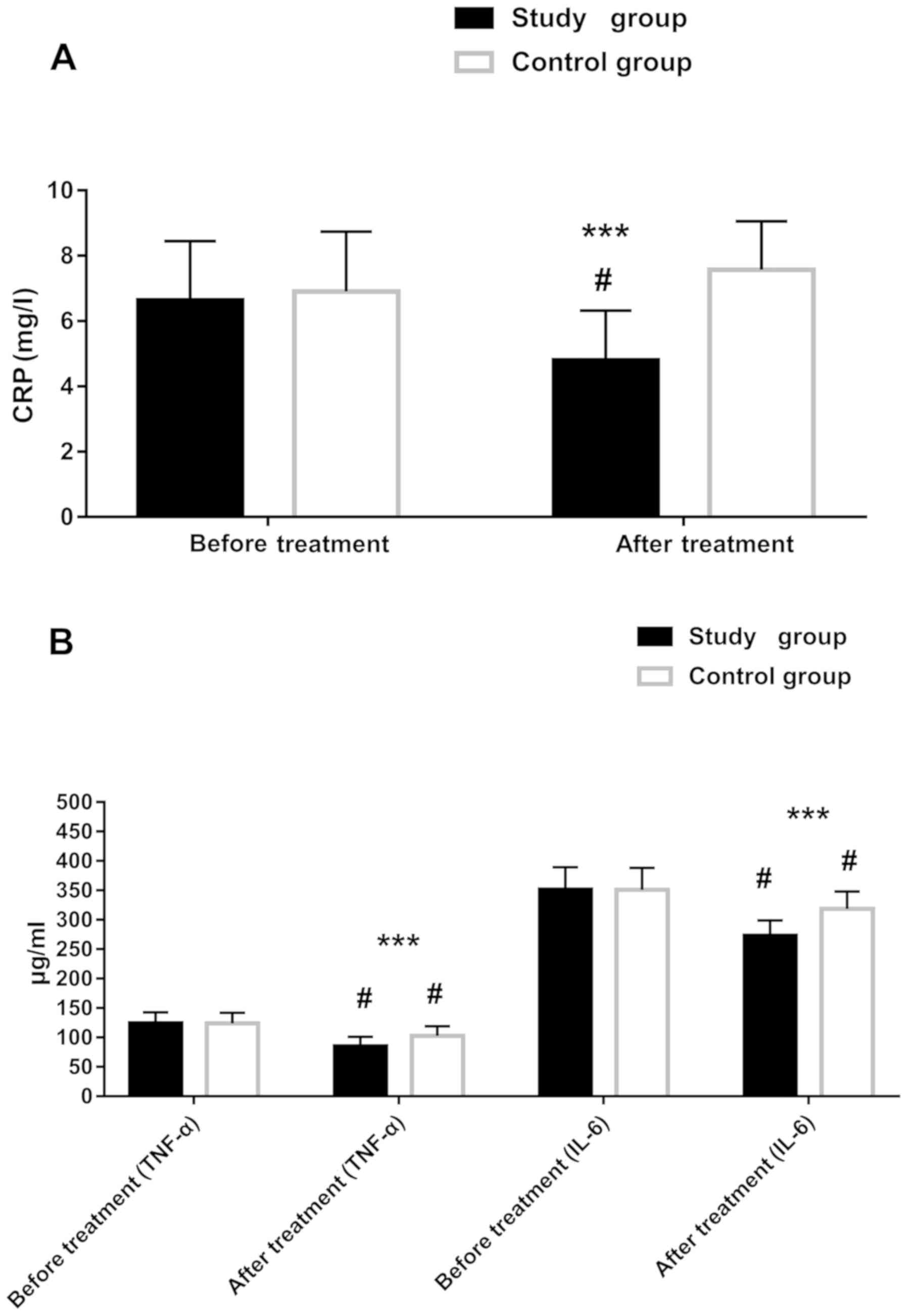
CRP, TNF-α, and IL-6 levels before and
after treatment in the two groups
There were no intergroup differences in CRP, TNF-α,
and IL-6 before treatment (all P>0.05). However, at six months
after treatment, the levels of these markers improved greatly in
the study group (all P<0.05). The control group had improved
levels of TNF-α and IL-6 after treatment (both P<0.05).
Intergroup differences were observed in the three markers after
treatment, and the reductions in the study group were greater (all
P<0.05) (Table V and Fig. 3).
 | Table V.CRP, TNF-α, and IL-6 levels before
and after treatment in the two groups. |
Table V.
CRP, TNF-α, and IL-6 levels before
and after treatment in the two groups.
| Factors | Study group Before
treatment | Control group
Before treatment | t value | P-value | Study group After
treatment | Control group After
treatment | t value | P-value |
|---|
| CRP (mg/l) | 6.64±1.81 | 6.90±1.84 | 0.917 | 0.363 |
4.80±1.52a | 7.57±1.48 | 7.153 | <0.001 |
| TNF-α (µg/ml) | 124.51±18.22 | 123.80±17.87 | 0.154 | 0.878 |
85.01±15.90a |
102.66±16.12a | 4.269 | <0.001 |
| IL-6 (µg/ml) | 351.37±37.86 | 351.00±37.32 | 0.038 | 0.969 |
273.27±25.64a |
318.34±29.73a | 6.287 | <0.001 |
Discussion
Some clinical studies have displayed that elderly
patients with T2DM are more likely to have CI, and the occurrence
is often unnoticeable. The condition may be mild cognitive
dysfunction in the beginning but turns to dementia as it
progresses.
Pathogenesis of the disease may be associated with
various factors, including Aβ gathering, chronic inflammation, and
age, making CI more easily developed in elderly patients with T2DM;
moreover, the occurrence of CI is closely correlated with glucose
variability (19). Some researchers
have reported that CI is more likely to occur in T2DM patients with
long-term insulin resistance and hyperinsulinemia, and T2DM is
regarded as a risk factor of CI. Furthermore, patients with T2DM
and CI often have brain insulin resistance (20). Studies on stroke have indicated that
in patients who had a stroke, the injury to neurovascular unit due
to cerebra hypoxia-ischemia can impair cognitive ability (21,22).
Other studies have exhibited that DPP-4 inhibitor not only has
better blood sugar lowering effect versus other hypoglycemic agents
but also attenuates CI induced by AD (23–26). In
the present study, we compared the efficacy of DPP-4 inhibitor
sitagliptin with that of sulfonylurea in the treatment and observed
that the two agents performed similarly in lowering blood sugar
content. However, in terms of improving cognitive ability, the
study group given DPP-4 inhibitor exhibited better MMSE and MoCA
scores than the control group, which aligns with the studies
above.
It has been demonstrated that Aβ gathering,
decreased ability in regulating protein phosphorylation, and the
participation of chronic inflammatory factors are common lesion
characteristics in both T2DM and CI (27). Regarding the mechanism of improving
cognitive ability, we studied the Aβ gathering and chronic
inflammatory factors. Some researchers have reported increased Aβ
expressions in cerebral cortex and hippocampus of mice with
diabetes, whereas using DPP-4 inhibitor decreases Aβ expression
levels in these two areas (27).
Another study has documented a reduction in Aβ expression in the
cerebrospinal fluid of AD patients (28). However, it is not easy to perform a
cerebrospinal fluid test during an early diagnosis of CI.
Therefore, clinical studies were performed to find more
easy-to-measure biomarkers in blood. Some studies on Aβ1–40 and
Aβ1–42 have observed different expression changes including rising,
no-change, and reduction in these two markers in plasma of patients
with MCI (29–31). Moreover, the ratio of Aβ1–42 to
Aβ1–40 has been found to decrease in patients with MCI, and the
ratio reduces even much more in patients with AD (31). The high blood sugar content in T2DM
can induce an immuno-inflammatory response. It has been revealed
that levels of CRP, TNF-α, and IL-6 can all elevate in T2DM
patients (32). Inflammatory factors
also exist in patients with CI. Some studies have reported elevated
levels of various inflammatory factors in CI patients, leading to
neuroinflammation. Due to inflammatory response, microglia and
astrocyte can be excessively activated and produce toxic substances
that damage neurons, thereby causing neuron denaturalization and
apoptosis (33). IL-6 is a type of
inflammatory factor. Previous studies reported that IL-6 expression
could begin to increase in plasma during the early stage of AD
(34). However, another study
reported no difference in IL-6 expression in serum between patients
with MCI and normal people (35).
CRP, a marker commonly used in clinic, is a protein synthesized in
liver mediated by inflammatory factors such as IL-6 (36). In the present study, we compared the
study group with the control group and found no intergroup
differences in Aβ1–40 and Aβ1–42 in plasma before and after
treatment in patients. After treatment, the study group had a
significantly higher ratio of Aβ1–42 to Aβ1–40 than the control
group. Moreover, no intergroup differences were observed in CRP,
TNF-α, and IL-6 levels before treatment, whereas these values were
much lower in the study group than in the control group after
treatment. These results align with previous findings.
There were still some limitations in the study. The
sample size was small, requiring a study with a larger sample size
in the future. Also, the study period was relatively short, and the
study was affected by several external factors including area of
infarction or bleeding, the difference in the treatment plan for
infarction and bleeding, and recovery duration. Therefore, a longer
follow-up will be needed in future studies.
In conclusion, using DPP-4 inhibitor in treating
elderly patients with T2DM combined with post-stroke MCI can
decrease blood sugar level and improve cognitive ability. The
mechanism may be associated with the improvement of Aβ gathering
and reduction in the inflammatory response in the body.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JX recorded and compared sugar blood content and
wrote the manuscript. CW and CP conceived and designed the study.
CP and HX were responsible for the collection and analysis of the
experimental data. LX and XC interpreted the data and drafted the
manuscript. XW and NW were responsible for the comparison of CRP,
TNF-α and IL-6, and revised the manuscript critically for important
intellectual content. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Heilongjiang Provincial Hospital (Harbin, China). Patients who
participated in this research had complete clinical data. Signed
written informed consents were obtained from the patients and/or
guardians.
Patient consent for publication
Not applicable.
Conflict of interest
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
DPP-4
|
dipeptidyl peptidase-4
|
|
T2DM
|
type 2 diabetes mellitus
|
|
MCI
|
mild cognitive impairment
|
|
CI
|
cognitive impairment
|
|
GLP-1
|
glucagon-like peptide-1
|
|
AD
|
Alzheimer's disease
|
|
MCI
|
mild cognitive impairment
|
|
MMSE
|
Mini-Mental State Examination
|
|
FBG
|
fasting blood glucose
|
|
2hPG
|
2-hour postprandial blood glucose
|
|
HbA1c
|
hemoglobin A1c
|
|
CRP
|
C-reactive protein
|
|
TNF
|
tumor necrosis factor
|
|
IL
|
interleukin
|
|
MoCA
|
Montreal Cognitive Assessment
|
References
|
1
|
Zaccardi F, Webb DR, Yates T and Davies
MJ: Pathophysiology of type 1 and type 2 diabetes mellitus: A
90-year perspective. Postgrad Med J. 92:63–69. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Weuve J, Hebert LE, Scherr PA and Evans
DA: Prevalence of Alzheimer disease in US states. Epidemiology.
26:e4–e6. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cumming TB, Marshall RS and Lazar RM:
Stroke, cognitive deficits, and rehabilitation: still an incomplete
picture. Int J Stroke. 8:38–45. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kosaraju J, Gali CC, Khatwal RB, Dubala A,
Chinni S, Holsinger RM, Madhunapantula VS, Muthureddy Nataraj SK
and Basavan D: Saxagliptin: A dipeptidyl peptidase-4 inhibitor
ameliorates streptozotocin induced Alzheimer's disease.
Neuropharmacology. 72:291–300. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Le Couteur DG, Wahl D and Naismith SL:
Comorbidity and vascular cognitive impairment-no dementia (VCI-ND).
Age Ageing. 46:705–707. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shi D, Chen X and Li Z: Diagnostic test
accuracy of the Montreal Cognitive Assessment in the detection of
post-stroke cognitive impairment under different stages and
cutoffs: a systematic review and meta-analysis. Neurol Sci.
39:705–716. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kosaraju J, Murthy V, Khatwal RB, Dubala
A, Chinni S, Muthureddy Nataraj SK and Basavan D: Vildagliptin: An
anti-diabetes agent ameliorates cognitive deficits and pathology
observed in streptozotocin-induced Alzheimer's disease. J Pharm
Pharmacol. 65:1773–1784. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kornelius E, Lin CL, Chang HH, Li HH,
Huang WN, Yang YS, Lu YL, Peng CH and Huang CN: DPP-4 Inhibitor
linagliptin attenuates Aβ-induced cytotoxicity through activation
of AMPK in neuronal cells. CNS Neurosci Ther. 21:549–557. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Graaf C, Donnelly D, Wootten D, Lau J,
Sexton PM, Miller LJ, Ahn JM, Liao J, Fletcher MM, Yang D, et al:
Glucagon-like peptide-1 and its class B G protein-coupled
receptors: A long march to therapeutic successes. Pharmacol Rev.
68:954–1013. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tramutola A, Arena A, Cini C, Butterfield
DA and Barone E: Modulation of GLP-1 signaling as a novel
therapeutic approach in the treatment of Alzheimer's disease
pathology. Expert Rev Neurother. 17:59–75. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hansen HH, Barkholt P, Fabricius K,
Jelsing J, Terwel D, Pyke C, Knudsen LB and Vrang N: The GLP-1
receptor agonist liraglutide reduces pathology-specific tau
phosphorylation and improves motor function in a transgenic
hTauP301L mouse model of tauopathy. Brain Res. 1634:158–170. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Candeias EM, Sebastião IC, Cardoso SM,
Correia SC, Carvalho CI, Plácido AI, Santos MS, Oliveira CR,
Moreira PI and Duarte AI: Gut-brain connection: The neuroprotective
effects of the anti-diabetic drug liraglutide. World J Diabetes.
6:807–827. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang X, Wang L, Jiang R, Xu Y, Zhao X and
Li Y: Exendin-4 antagonizes Aβ1-42-induced attenuation of spatial
learning and memory ability. Exp Ther Med. 12:2885–2892. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Isik AT, Soysal P, Yay A and Usarel C: The
effects of sitagliptin, a DPP-4 inhibitor, on cognitive functions
in elderly diabetic patients with or without Alzheimer's disease.
Diabetes Res Clin Pract. 123:192–198. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yin Y, Gao D, Wang Y, Wang ZH, Wang X, Ye
J, Wu D, Fang L, Pi G, Yang Y, et al: Tau accumulation induces
synaptic impairment and memory deficit by calcineurin-mediated
inactivation of nuclear CaMKIV/CREB signaling. Proc Natl Acad Sci
USA. 113:E3773–E3781. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ogedengbe S, Ezeani IU and Aihanuwa E:
Comparison of clinical and biochemical variables in type 2 diabetes
mellitus patients and their first-degree relatives with metabolic
syndrome in Benin City, Nigeria: A cross sectional case controlled
study. Endocr Regul. 50:32–40. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Blum S, Luchsinger JA, Manly JJ, Schupf N,
Stern Y, Brown TR, DeCarli C, Small SA, Mayeux R and Brickman AM:
Memory after silent stroke: hippocampus and infarcts both matter.
Neurology. 78:38–46. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ciesielska N, Sokołowski R, Mazur E,
Podhorecka M, Polak-Szabela A and Kędziora-Kornatowska K: Is the
Montreal Cognitive Assessment (MoCA) test better suited than the
Mini-Mental State Examination (MMSE) in mild cognitive impairment
(MCI) detection among people aged over 60? Meta-analysis. Psychiatr
Pol. 50:1039–1052. 2016.(In Polish). View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rizzo MR, Marfella R, Barbieri M, Boccardi
V, Vestini F, Lettieri B, Canonico S and Paolisso G: Relationships
between daily acute glucose fluctuations and cognitive performance
among aged type 2 diabetic patients. Diabetes Care. 33:2169–2174.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Watson GS and Craft S: Modulation of
memory by insulin and glucose: Neuropsychological observations in
Alzheimer's disease. Eur J Pharmacol. 490:97–113. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zheng G, Zheng Y, Xiong Z, Ye B, Tao J and
Chen L: Effect of Baduanjin exercise on cognitive function in
patients with post-stroke cognitive impairment: Study protocol for
a randomised controlled trial. BMJ Open. 8:e0209542018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Rosenberg GA: Extracellular matrix
inflammation in vascular cognitive impairment and dementia. Clin
Sci (Lond). 131:425–437. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhou JB, Bai L, Wang Y and Yang JK: The
benefits and risks of DPP4-inhibitors vs. sulfonylureas for
patients with type 2 diabetes: Accumulated evidence from randomised
controlled trial. Int J Clin Pract. 70:132–141. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Loh HH, Yee A, Loh HS, Sukor N and
Kamaruddin NA: Comparative studies of dipeptidyl peptidase 4
inhibitor vs sulphonylurea among Muslim Type 2 diabetes patients
who fast in the month of Ramadan: A systematic review and
meta-analysis. Prim Care Diabetes. 10:210–219. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bekiari E, Rizava C, Athanasiadou E,
Papatheodorou K, Liakos A, Karagiannis T, Mainou M, Rika M, Boura P
and Tsapas A: Systematic review and meta-analysis of vildagliptin
for treatment of type 2 diabetes. Endocrine. 52:458–480. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xi YD, Zhang DD, Ding J, Yu HL, Yuan LH,
Ma WW, Han J and Xiao R: Genistein inhibits Aβ25-35-induced
synaptic toxicity and regulates CaMKII/CREB pathway in SH-SY5Y
cells. Cell Mol Neurobiol. 36:1151–1159. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kosaraju J, Holsinger RMD, Guo L and Tam
KY: Linagliptin, a dipeptidyl peptidase-4 inhibitor, mitigates
cognitive deficits and pathology in the 3×Tg-AD mouse model of
Alzheimer's disease. Mol Neurobiol. 54:6074–6084. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
de Leon MJ, Pirraglia E, Osorio RS,
Glodzik L, Saint-Louis L, Kim HJ, Fortea J, Fossati S, Laska E,
Siegel C, et al Alzheimer's Disease Neuroimaging Initiative;
National Alzheimer's Coordinating Center, : The nonlinear
relationship between cerebrospinal fluid Aβ42 and tau in
preclinical Alzheimer's disease. PLoS One. 13:e01912402018.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mayeux R, Honig LS, Tang MX, Manly J,
Stern Y, Schupf N and Mehta PD: Plasma A[beta]40 and A[beta]42 and
Alzheimer's disease: Relation to age, mortality, and risk.
Neurology. 61:1185–1190. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Rembach A, Faux NG, Watt AD, Pertile KK,
Rumble RL, Trounson BO, Fowler CJ, Roberts BR, Perez KA, Li QX, et
al AIBL research group, : Changes in plasma amyloid beta in a
longitudinal study of aging and Alzheimer's disease. Alzheimers
Dement. 10:53–61. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Janelidze S, Stomrud E, Palmqvist S,
Zetterberg H, van Westen D, Jeromin A, Song L, Hanlon D, Tan Hehir
CA, Baker D, et al: Plasma β-amyloid in Alzheimer's disease and
vascular disease. Sci Rep. 6:268012016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ebtehaj S, Gruppen EG, Parvizi M, Tietge
UJF and Dullaart RPF: The anti-inflammatory function of HDL is
impaired in type 2 diabetes: Role of hyperglycemia, paraoxonase-1
and low grade inflammation. Cardiovasc Diabetol. 16:1322017.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Prati F, Bartolini M, Simoni E, De Simone
A, Pinto A, Andrisano V and Bolognesi ML: Quinones bearing
non-steroidal anti-inflammatory fragments as multitarget ligands
for Alzheimer's disease. Bioorg Med Chem Lett. 23:6254–6258. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Mun MJ, Kim JH, Choi JY and Jang WC:
Genetic polymorphisms of interleukin genes and the risk of
Alzheimer's disease: An update meta-analysis. Meta Gene. 8:1–10.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kim YS, Lee KJ and Kim H: Serum tumour
necrosis factor-α and interleukin-6 levels in Alzheimer's disease
and mild cognitive impairment. Psychogeriatrics. 17:224–230. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhang Q, Qian G and Ding Z: Xuemaitong
granules attenuate carotid atherosclerosis by decreasing the
expression of CD14+CD16+ monocytes, IL-6,
TNF-α, and hsCRP. Genet Mol Res. 13:7519–7527. 2014. View Article : Google Scholar : PubMed/NCBI
|