Introduction
High arterial stiffness is known to be a risk
factor, as well as a prognostic marker for cardiovascular disease
(CVD) (1). Endothelial dysfunction
plays a key role in arterial stiffness by reducing the endothelial
properties of vasodilatation, accelerating the proinflammatory and
prothrombotic properties (2).
Endothelial dysfunction is an early event in patients with CVD and
is considered as one of the several potential contributors to
plaque destabilization (3).
A number of non-invasive techniques are available to
assess the endothelial function and arterial stiffness of the
peripheral vasculature, such as brachial artery flow-mediated
vasodilatation (bFMD), pulse wave velocity (PWV) and cardio-ankle
vascular index (CAVI) (4,5). These non-invasive methods were widely
used clinically to predict the risk of subclinical atherosclerosis
in individuals who are at a high risk of CVD (6). CAVI is an inexpensive, non-invasive,
office-based method which is used to evaluate arterial stiffness in
the aorta, femoral artery and tibial artery, which reflects the
degree of cardiovascular disease (1,7). The
advantage to CAVI is that it is not affected by blood pressure (BP)
and the measurements are automatic via validated software (6,8,9).
Our group has demonstrated the cardioprotective
effects of AGE by decreasing atherosclerotic plaque progression in
patients with type 2 diabetes (10)
and improving endothelial function (11,12).
Endothelial dysfunction plays a critical role in the pathogenesis
of micro- and macrovascular diseases in patients with type 2
diabetes (13). Annual screening is
recommended for diabetic patients for the early detection of micro-
and macrovascular complications. This study investigated the
effects of AGE in individuals with type 2 diabetes on vascular
elasticity and endothelial function, which was measured by CAVI,
over a period of 3 months.
Patients and methods
Study population and
randomization
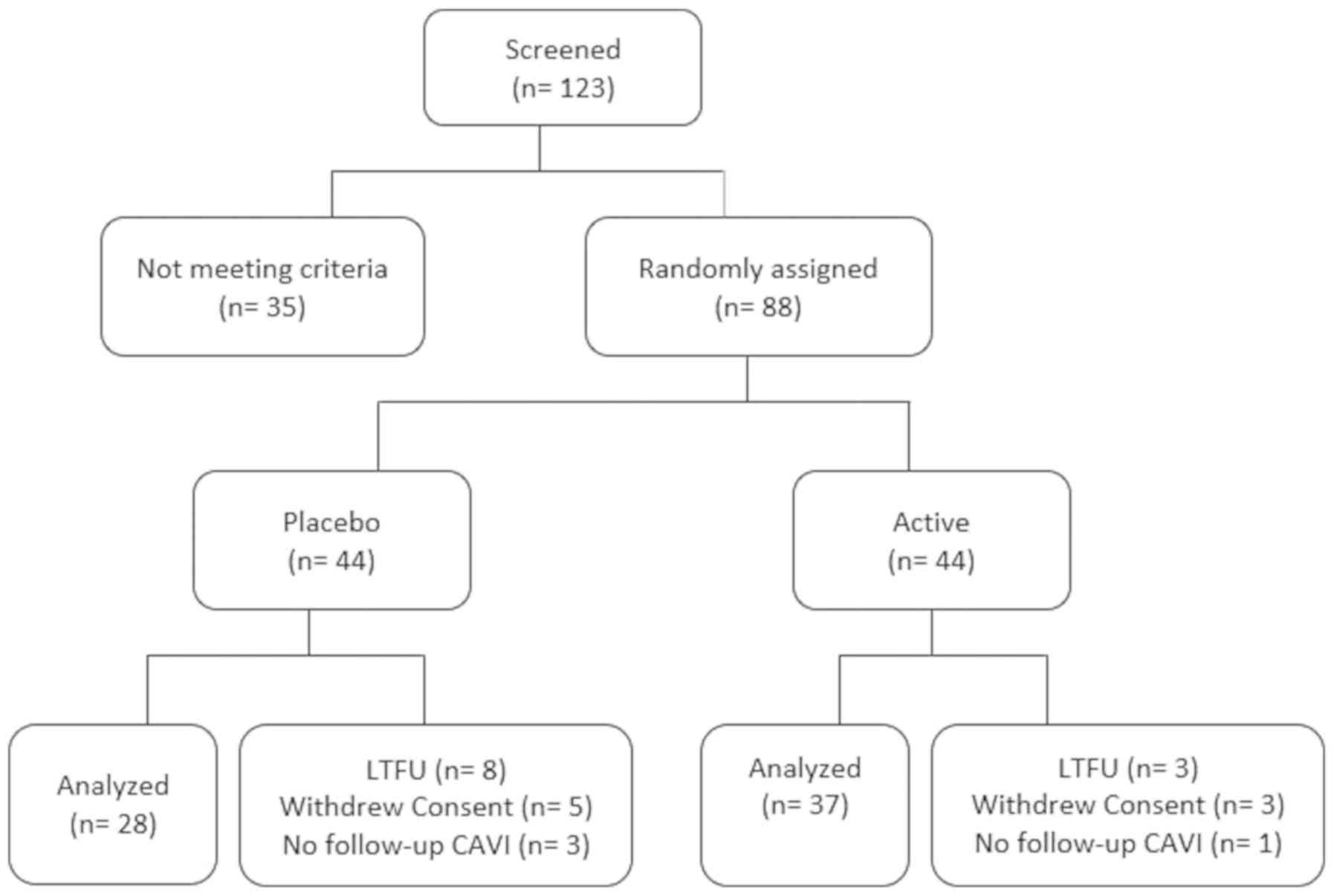
A total of 88 patients with type 2 diabetes were
enrolled in a double-blind, placebo-controlled randomized study,
who met the eligibility criteria (inclusion and exclusion
criteria), after signing a written informed consent that was
approved by the Institutional Review Board (IRB) of the Lundquist
Institute for Biomedical Innovation at Harbor UCLA Medical Center
(NCT03931434). Of these 88 patients, 23 patients were unable to
undergo all follow-up visits (Fig.
1). Cardiovascular risk factors, and hemoglobin A1c (HbA1c) and
serum lipid profiles were obtained using standard techniques at
baseline. Participants were followed-up for 3 months with CAVI
measured at baseline and again at 3 months.
Patients were randomized at a 1:1 ratio to receive
AGE (active group) or the placebo. All participants were advised to
take 2 capsules twice daily with water for 3 months. The 2,400 mg
of AGE capsules were provided by Wakunaga of America Co., Ltd. with
a matched placebo pill which looked similar to AGE, but did not
contain any garlic or active ingredient. Both the active and
placebo study drugs were similar in size and color. The study drug
was packaged in the containers sent by the sponsor as per the
randomization list and was sent to the site with a printed label
containing only the number of the patient. The randomization key
was provided to the principal investigator and was opened only
after the completion of the study. We conducted an inter-trial
phone visit to ensure study medication compliance. The AGE capsule
used in this study is commercially available in the market.
Inclusion criteria
We enrolled patients between age 30–75 years with a
known history of type 2 diabetes mellitus (HbA1c >6.5% or
fasting blood sugar >125 mg/dl or taking antidiabetic
medications) and who signed an informed consent form.
Exclusion criteria
We excluded patients with known hypersensitivity to
AGE, a body weight in excess of 350 pounds, a history of coronary
artery disease (CAD), myocardial infarction (MI), stroke or
life-threatening arrhythmia within the prior 6 months, New York
Heart Association Functional Classification II–IV heart failure,
renal impairment (serum creatinine >1.4 mg/dl), current tobacco
use, a history of bleeding disorders or use of anticoagulants,
hypertensive encephalopathy or cerebrovascular accident, or who
were currently enrolled in another placebo-controlled trial.
Measurement of CAVI
CAVI was measured using the VaSera (Fukuda Denshi
non-invasive BP, pulse wave velocity (PWV) and heart sound
monitor/measuring device that integrated the values to compute an
ankle-brachial index (ABI) and a proxy of arterial stiffness
(CAVI). Briefly, blood pressure cuffs were applied to the bilateral
upper arms and ankles, with the subject lying in the supine
position and the head held in midline position.
Electrocardiographic electrodes were placed on both wrists and a
microphone was placed on the sternal angle for phonocardiography.
After resting for 10 min, the examinations were performed. To
detect the brachial and ankle pulse waves with cuffs, a low cuff
pressure from 30 to 50 mmHg was used to ensure minimal effect of
cuff pressure on hemodynamics. Following automatic measurements,
the obtained data were analyzed using VSS-10 software (Fukuda
Denshi), and the values of the right and left CAVI were measured.
The averages of the right and left CAVIs were used for
analysis.
Statistical analysis
Continuous variables are expressed as the means ±
SD, while categorical variables are stated as counts and
percentages. A Student's t-test or Chi-square test was used to
determine differences in all baseline parameters between the
placebo and AGE group. An ANOVA model with treatment as the main
effect was used to compare changes with CAVI from baseline to
follow-up between the groups, while using Tukey's procedure for
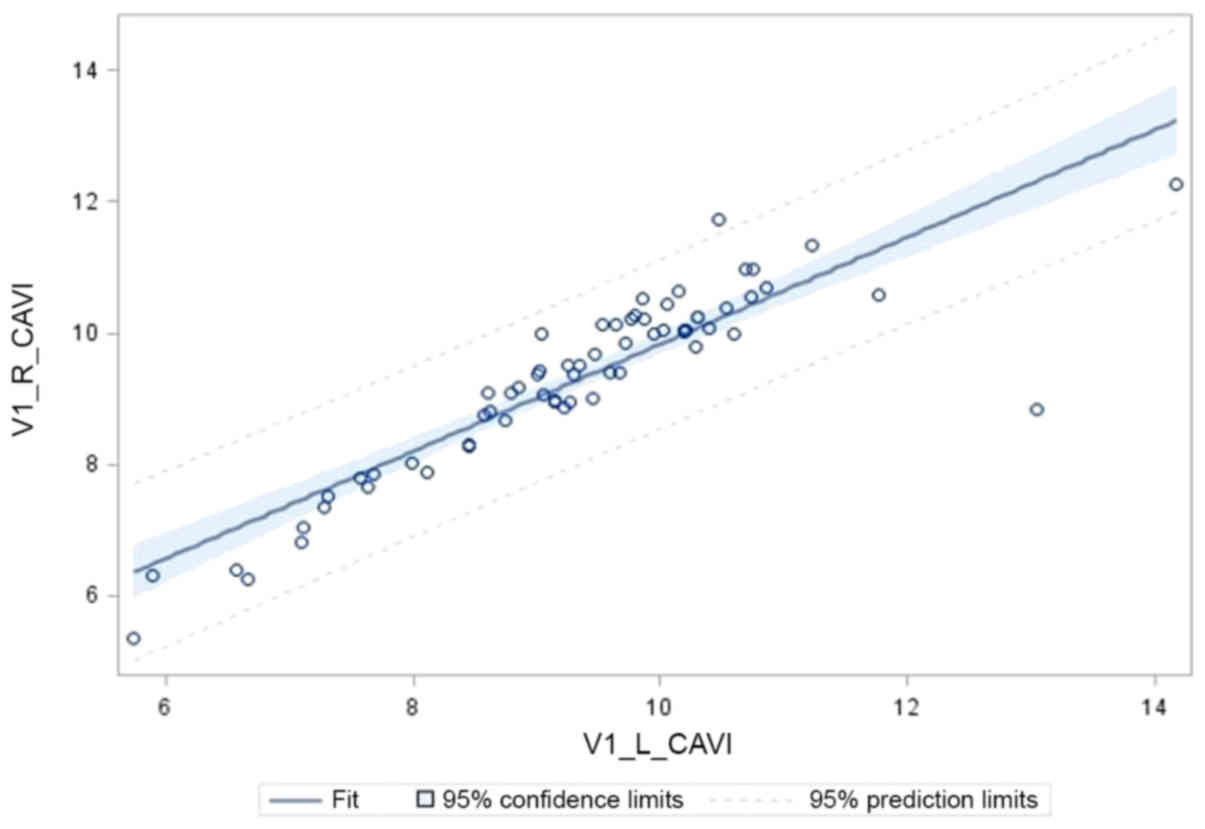
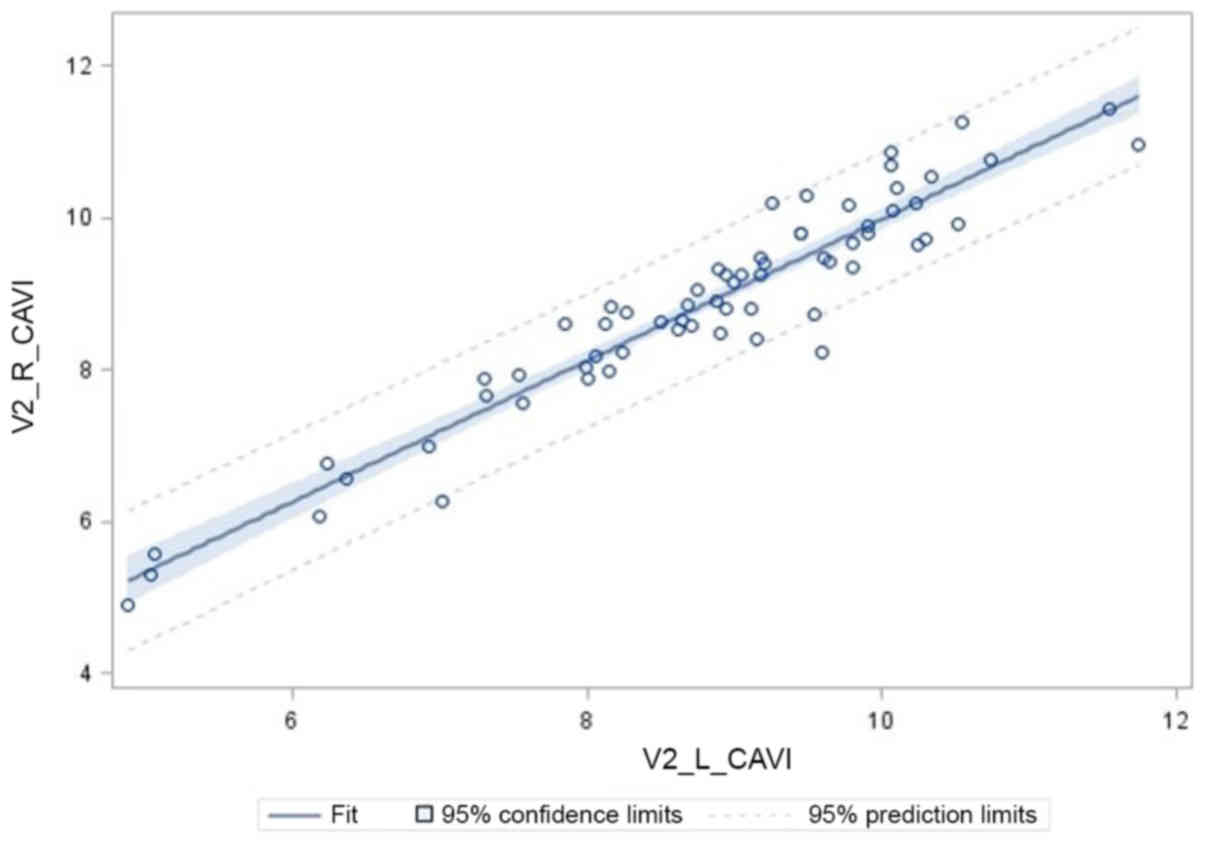
post hoc analysis and comparison of multiple groups. Pearson's
correlation coefficient was used to analyze the strength of the
correlation between the left and right CAVI measures at each visit.
A P-value of <0.05 was considered to indicate a statistically
significant difference. SAS software (version 9.4) was used to
carry out all statistical analyses.
Results
A total of 65 patients (38 men and 27 women; mean
age 58.45±11.25 years) completed 2 study visits (baseline and 3
months), where baseline and follow-up CAVI measures were assessed
(Fig. 1). Out of the 65 patients, 37
were randomized to the treatment (AGE; active) group (19 males;
mean age, 59.3±10.8 years). Patients current medications, such as
aspirin, hypertensive or hyperlipidemia or diabetic medications,
did not change during the 3 months of the study. The baseline
characteristics of the patients have been published elsewhere
(14).
The primary objective of this study was reduction in
CAVI over a 3-month period. As shown in Table I, CAVI was significantly reduced on
the right arm by 0.64±1.09, relative to the placebo group reduction
of 0.11±0.92 (P=0.04). On the left arm, CAVI was trending toward a
significant reduction by 0.79±1.58, relative to 0.16±1.05 in the
placebo group (P=0.07). The reduction based upon the average of
both arms was 0.71±1.27 in AGE vs. 0.13± 0.94 (P=0.04). As shown
Table II, the CAVI measures
completed on the right and left arms for both visits were highly
and significantly correlated, (Pearsons's r for visit 1 = 0.89,
P<0.0001; visit 2 = 0.95, P<0.0001) indicating a high degree
of consistency in the CAVI measures (Figs. 2 and 3).
 | Table I.CAVI index within and between both
groups. |
Table I.
CAVI index within and between both
groups.
| Group | Variable | Visit 1 (mean ±
SD) | Visit 2 (mean ±
SD) | Within group (mean ±
SD) | Between group (mean ±
SD) | P-value |
|---|
| Active (n=37) | L_CAVI | 9.4±1.5 | 8.6±1.5 | 0.79±1.58 | 0.63±1.38 | 0.07 |
| Placebo (n=28) | L_CAVI | 9.2±1.5 | 9.0±1.4 |
0.16±1.05 |
|
|
| Active (n=37) | R_CAVI | 9.3±1.4 |
8.7±1.4 | 0.64±1.09 | 0.53±1.02 | 0.04 |
| Placebo (n=28) | R_CAVI | 9.2±1.4 | 9.1±1.4 | 0.11±0.92 |
|
|
| Active (n=37) | Mean both CAVI | 9.4±1.4 | 8.7±1.4 | 0.71±1.27 | 0.58±1.14 | 0.04 |
| Placebo (n=28) | Mean both CAVI | 9.2±1.4 | 9.1±1.4 | 0.13±0.94 |
|
|
 | Table II.Pearson's correlations of left and
right CAVI measures at baseline and follow-up. |
Table II.
Pearson's correlations of left and
right CAVI measures at baseline and follow-up.
| Group | Pearson's r | P-value |
|---|
| Visit 1,
left/right | 0.89 | <0.0001 |
| Visit 2,
left/right | 0.95 | <0.0001 |
Discussion
To the best of our knowledge, this is the first
study to demonstrate the effects of AGE on arterial stiffness by
improving endothelial function, which was measured by CAVI over a
period of 3 months in patients with type 2 diabetes. Diabetic
patients with a high 10-year atherosclerotic cardiovascular disease
(ASCVD) risk score have been noted to have high CAVI (>9)
(15). CAVI is independent of blood
pressure and highly reproducible, which is significantly higher in
patients with coronary artery stenosis (1,6–9,16). In
comparison to PWV, CAVI reflects the smooth muscle contraction
rather than changes in BP, and changes over a short period of time
in response to sympathetic tone and pharmacological influences
(17). The current study
demonstrated AGE reduced the arterial stiffness, which was
demonstrated by CAVI, which inturn reduces the risk of coronary
events.
Arterial stiffness increases with age through the
loss of elastin and collagen fibers, which results in increased
blood pressure (18). Kobayashi
et al (19) demonstrated the
significant association between endothelial dysfunction and
increased arterial stiffness. Tomiyama et al (20) demonstrated the significant
association of bFMD endothelial measurements with arterial
stiffness assessed by PWV. Previous studies have indicated that
treatments targeting to reduce arterial stiffness and wave
reflections can reduce the risk of CVD along with a reduction in BP
(21). Larijani et al
(11) demonstrated the beneficial
effects of AGE and CoQ10 on vascular elasticity and endothelial
function in firefighters (mean reduction of PWV, 1.21; 95% CI, −2.1
to −0.32; P=0.005). Ried and Fakler (22) demonstrated the potential effect of
garlic in lowering BP through a meta-analysis, including 20
clinical trials with hypertensive individuals (8–9 mmHg of SBP and
6–7 mmHg of DBP; P<0.0001). Furthermore, Breithaupt-Grögler
et al (23) demonstrated the
protective effects of garlic extract on arterial stiffness assessed
by PWV (active vs. placebo; 8.3±1.46 vs. 9.8±2.45 m/sec;
P<0.0001) and pressure-standardized elastic vascular resistance
(EVR) (active vs. placebo; 0.63±0.21 vs. 0.9±0.44 m2 · sec-2 · mm
Hg-1; P<0.0001) compared to the placebo. The results of the
current study are consistent with those of previous studies and the
mean of both right and left CAVI was significantly improved in AGE
group relative to the placebo (0.71+1.27 vs. 0.13+0.94;
P=0.04).
Oxidative stress and systemic inflammation play a
key role in endothelial dysfunction, which impairs the pathways
leading to the production of endothelial-derived relaxing factors,
such as nitric oxide (NO), prostacyclin, tissue plasminogen
activator and vasoconstrictors (eg, leukotrienes and endothelin-1)
(24). Increased oxidative stress
accelerates the production of reactive oxygen species (ROS),
leading to the inactivation of two anti-atherosclerotic enzymes,
such as endothelial nitric oxide synthase (eNOS) and prostacyclin
synthases (25,26). Endogenous NO is a potent vasodilator
and is produced by two pathways. The first one is by the oxidation
of L-arginine in the vascular endothelium by eNOS and the other is
by reducing the dietary nitrate (NO3-) to nitrite
(NO2-) to NO (27,28). The
uncoupling of NOS is a mechanism which plays a critical role in
endothelial dysfunction, resulting in the generation of high levels
of superoxide (O2-), leading to the formation of potent
oxidant peroxynitrite (ONOO-), which is highly toxic,
damaging biomolecules, including proteins, lipids and DNA (22,29).
Previous studies have used bFMD as an index of endothelial NO
regulation of vascular tone, and targeting ROS with vitamin C and
dietary nitrate supplement improved vascular function in a number
of conditions known to be associated with excess oxidative stress
(e.g., type II diabetes, hypertension and CAD) (30–32).
AGE contains water soluble S-allyl cysteine (SAC)
and S-allymercaptocysteine (SAMC), which have potent antioxidant
properties to protect the vascular endothelium from oxidative
stress (11) and has also been
reported to have a cholesterol-lowering effect (33). The thiol components
(γ-glutamylcysteine) of garlic have the ability to reduce blood
pressure by modulating NO, H2S and endothelial synthesis as
previously described (21,34–36).
Furthermore, AGE has been shown to exert an anti-inflammatory
effect by decreasing the expression of CD36 on foam cells and
oxidized LDL uptake by macrophages (37). Taken together, the antioxidant and
anti-inflammatory properties of garlic increase the enzymatic
activity of endothelial cells, such as eNOS, catalase, glutathione
peroxidase and superoxide reductase to maintain vascular
hemostasis, which may be useful for the prevention of CVD (38).
The current study has several limitations. First,
the sample size was relatively small and follow-up was relatively
short-term to demonstrate the effects of AGE on BP. Second,
patients were under different therapies for hyperlipidemia,
hypertension and type 2 diabetes mellitus at different doses. Due
to our small sample size, a separate analysis by different
background medications was not performed.
In conclusion, this study indicates that at the end
of 3 months, the change in CAVI was significantly greater in the
AGE group than in the placebo group. Further studies however, are
required to evaluate whether AGE has the ability to improve
arterial stiffness and endothelial function and thereby decrease
adverse cardiovascular events.
Acknowledgements
Not applicable.
Funding
This study was funded by Wakunaga of America Co.,
Ltd., Mission Viejo, CA, USA.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article or are available from the
corresponding author on reasonable request.
Authors' contributions
MJB conceived of and designed the study. SH, LC, DB,
BTC and MJB collected the patient information and generated the
clinical data. AK, LC, DB, SM, KS, FF, SKR and MJB analyzed and/or
interpreted the data; and SH, LC, DB, AK, KS, BTC, FF and MJB
drafted or revised the manuscript. All authors have read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
All patients were enrolled in this study after
signing a written informed consent that was approved by the
Institutional Review Board (IRB) of the Lundquist Institute for
Biomedical Innovation at Harbor UCLA Medical Center
(NCT03931434).
Patient consent for publication
Not applicable.
Competing interests
MJB discloses work for the National Institutes of
Health and General Electric Healthcare. All the other authors
declare that they have no competing interests.
References
|
1
|
Nakamura K, Tomaru T, Yamamura S,
Miyashita Y, Shirai K and Noike H: Cardio-ankle vascular index is a
candidate predictor of coronary atherosclerosis. Circ J.
72:598–604. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Endemann DH and Schiffrin EL: Endothelial
dysfunction. J Am Soc Nephrol. 15:1983–1992. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Williams MJA, Sutherland WHF, McCormick
MP, Yeoman DJ and de Jong SA: Aged garlic extract improves
endothelial function in men with coronary artery disease. Phytother
Res. 19:314–319. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Huck CJ, Bronas UG, Williamson EB, Draheim
CC, Duprez DA and Dengel DR: Noninvasive measurements of arterial
stiffness: Repeatability and interrelationships with endothelial
function and arterial morphology measures. Vasc Health Risk Manag.
3:343–349. 2007.PubMed/NCBI
|
|
5
|
Shekar C, Li D, Cherukuri L, Shaikh K,
Hamal S, Birudaraju D, Shodhan S, Nezarat N, Dailing C, Flores F,
et al: Abstract 16894: Association Between Flow Mediated
Vasodilation and Coronary Artery Disease. Circulation.
138:A168942018.
|
|
6
|
Kanamoto M, Matsumoto N, Shiga T, Kunimoto
F and Saito S: Relationship between coronary artery stenosis and
cardio-ankle vascular index (CAVI) in patients undergoing
cardiovascular surgery. J Cardiovasc Dis Res. 4:15–19. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sairaku A, Eno S, Hondo T, Teragawa H,
Nakano Y, Matsuda K, Kisaka T and Kihara Y: Head-to-head comparison
of the cardio-ankle vascular index between patients with acute
coronary syndrome and stable angina pectoris. Hypertens Res.
33:1162–1166. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Miyoshi T, Doi M, Hirohata S, Sakane K,
Kamikawa S, Kitawaki T, Kaji Y, Kusano KF, Ninomiya Y and Kusachi
S: Cardio-ankle vascular index is independently associated with the
severity of coronary atherosclerosis and left ventricular function
in patients with ischemic heart disease. J Atheroscler Thromb.
17:249–258. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
9
|
Izuhara M, Shioji K, Kadota S, Baba O,
Takeuchi Y, Uegaito T, Mutsuo S and Matsuda M: Relationship of
cardio-ankle vascular index (CAVI) to carotid and coronary
arteriosclerosis. Circ J. 72:1762–1767. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shaikh K, Cherukuri L, Birudaraju D,
Nakanishi R, Almeida S, Jayawardena E, Shekar C, Flores F, Hamal S,
Sheikh S, et al: Aged garlic extract reduces low attenuation plaque
in coronary arteries of patients with diabetes in a prospective
randomized double-blind study. J Am Coll Cardiol. 73:16452019.
View Article : Google Scholar
|
|
11
|
Larijani VN, Ahmadi N, Zeb I, Khan F,
Flores F and Budoff M: Beneficial effects of aged garlic extract
and coenzyme Q10 on vascular elasticity and endothelial function:
The FAITH randomized clinical trial. Nutrition. 29:71–75. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zeb I, Ahmadi N, Nasir K, Kadakia J,
Larijani VN, Flores F, Li D and Budoff MJ: Aged garlic extract and
coenzyme Q10 have favorable effect on inflammatory markers and
coronary atherosclerosis progression: A randomized clinical trial.
J Cardiovasc Dis Res. 3:185–190. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dhananjayan R, Koundinya KSS, Malati T and
Kutala VK: Endothelial dysfunction in type 2 diabetes mellitus.
Indian J Clin Biochem. 31:372–379. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hutchins E, Shaikh K, Kininger A,
Cherukuri L, Birudaraju D, Mao SS, Nakanishi R, Almeida S,
Jayawardena E, Shekar C, Flores F, et al: Aged garlic extract
reduces left ventricular myocardial mass in patients with diabetes:
A prospective randomized controlled double-blind study. Exp Ther
Med (In Press).
|
|
15
|
Park SY, Chin SO, Rhee SY, Oh S, Woo JT,
Kim SW and Chon S: Cardio-Ankle Vascular Index as a Surrogate
Marker of Early Atherosclerotic Cardiovascular Disease in Koreans
with Type 2 Diabetes Mellitus. Diabetes Metab J. 42:285–295. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Horinaka S, Yabe A, Yagi H, Ishimura K,
Hara H, Iemua T and Matsuoka H: Comparison of atherosclerotic
indicators between cardio ankle vascular index and brachial ankle
pulse wave velocity. Angiology. 60:468–476. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sun CK: Cardio-ankle vascular index (CAVI)
as an indicator of arterial stiffness. Integr Blood Press Control.
6:27–38. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mattace-Raso FUS, van der Cammen TJM,
Hofman A, van Popele NM, Bos ML, Schalekamp MADH, Asmar R, Reneman
RS, Hoeks AP, Breteler MM, et al: Arterial stiffness and risk of
coronary heart disease and stroke: The Rotterdam Study.
Circulation. 113:657–663. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kobayashi K, Akishita M, Yu W, Hashimoto
M, Ohni M and Toba K: Interrelationship between non-invasive
measurements of atherosclerosis: Flow-mediated dilation of brachial
artery, carotid intima-media thickness and pulse wave velocity.
Atherosclerosis. 173:13–18. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tomiyama H, Ishizu T, Kohro T, Matsumoto
C, Higashi Y, Takase B, Suzuki T, Ueda S, Yamazaki T, Furumoto T,
et al: Longitudinal association among endothelial function,
arterial stiffness and subclinical organ damage in hypertension.
Int J Cardiol. 253:161–166. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Boutouyrie P, Fliser D, Goldsmith D, Covic
A, Wiecek A, Ortiz A, Martinez-Castelao A, Lindholm B, Massy ZA,
Suleymanlar G, et al: Assessment of arterial stiffness for clinical
and epidemiological studies: Methodological considerations for
validation and entry into the European Renal and Cardiovascular
Medicine registry. Nephrol Dial Transplant. 29:232–239. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ried K and Fakler P: Potential of garlic
(Allium sativum) in lowering high blood pressure: Mechanisms
of action and clinical relevance. Integr Blood Press Control.
7:71–82. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Breithaupt-Grögler K, Ling M, Boudoulas H
and Belz GG: Protective effect of chronic garlic intake on elastic
properties of aorta in the elderly. Circulation. 96:2649–2655.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lerman A and Zeiher AM: Endothelial
function: Cardiac events. Circulation. 111:363–368. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Craige SM, Kant S and Keaney JF Jr:
Reactive oxygen species in endothelial function - from disease to
adaptation. Circ J. 79:1145–1155. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Du X, Edelstein D, Obici S, Higham N, Zou
M-H and Brownlee M: Insulin resistance reduces arterial
prostacyclin synthase and eNOS activities by increasing endothelial
fatty acid oxidation. J Clin Invest. 116:1071–1080. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Duncan C, Dougall H, Johnston P, Green S,
Brogan R, Leifert C, Smith L, Golden M and Benjamin N: Chemical
generation of nitric oxide in the mouth from the enterosalivary
circulation of dietary nitrate. Nat Med. 1:546–551. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lundberg JO and Govoni M: Inorganic
nitrate is a possible source for systemic generation of nitric
oxide. Free Radic Biol Med. 37:395–400. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Förstermann U and Sessa WC: Nitric oxide
synthases: regulation and function. Eur Heart J. 33:829–837,
837a-837d. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Carlström M, Larsen FJ, Nyström T, Hezel
M, Borniquel S, Weitzberg E and Lundberg JO: Dietary inorganic
nitrate reverses features of metabolic syndrome in endothelial
nitric oxide synthase-deficient mice. Proc Natl Acad Sci USA.
107:17716–17720. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lara J, Ashor AW, Oggioni C, Ahluwalia A,
Mathers JC and Siervo M: Effects of inorganic nitrate and beetroot
supplementation on endothelial function: A systematic review and
meta-analysis. Eur J Nutr. 55:451–459. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Levine GN, Frei B, Koulouris SN, Gerhard
MD, Keaney JF Jr and Vita JA: Ascorbic acid reverses endothelial
vasomotor dysfunction in patients with coronary artery disease.
Circulation. 93:1107–1113. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ackermann RT, Mulrow CD, Ramirez G,
Gardner CD, Morbidoni L and Lawrence VA: Garlic shows promise for
improving some cardiovascular risk factors. Arch Intern Med.
161:813–824. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Sendl A, Elbl G, Steinke B, Redl K, Breu W
and Wagner H: Comparative pharmacological investigations of Allium
ursinum and Allium sativum. Planta Med. 58:1–7. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kim-Park S and Ku DD: Garlic elicits a
nitric oxide-dependent relaxation and inhibits hypoxic pulmonary
vasoconstriction in rats. Clin Exp Pharmacol Physiol. 27:780–786.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Benavides GA, Squadrito GL, Mills RW,
Patel HD, Isbell TS, Patel RP, Darley-Usmar VM, Doeller JE and
Kraus DW: Hydrogen sulfide mediates the vasoactivity of garlic.
Proc Natl Acad Sci USA. 104:17977–17982. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ide N, Keller C and Weiss N: Aged garlic
extract inhibits homocysteine-induced CD36 expression and foam cell
formation in human macrophages. J Nutr. 136 (Suppl):755S–758S.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ahmadi N, Nabavi V, Zughaib H, Patel N,
Rathod A, Flores F, Mao S, Hajsadeghi F and Budoff M: Aged Garlic
Extract with Supplement is Associated with Beneficial Effect on
Bone Mineral Density and Predicts Lack of Progression of
Atherosclerosis: A Prospective Double Blinded Randomized Trial. Int
J Cardiovasc Res. 4:32015.
|