Introduction
Selection of the optimal treatment of major
hemorrhage in patients with pelvic fracture remains a challenge for
trauma surgeons (1–7). Uncontrollable major hemorrhage is a
major cause of mortality in patients with pelvic fractures
(8–11). Relatively aggressive measures are
imperative to manage this serious pathophysiological status; blood
transfusion is an effective protocol for the improvement of the
hypovolemic status and the use of other supportive care measures,
including external fixations, angiography and embolization, as well
as pre-peritoneal pelvic packing, may also be effective (8–11).
Previous studies have revealed that high-energy pelvic fracture is
associated with a relatively higher blood transfusion frequency
(12–14). These studies reported that blood
transfusion is required at 24 (12),
48 (14) or 72 h (13). The Young and Burgess classification
system (3) has been used to indicate
the requirement for blood transfusion. However, blood transfusion
administered in the initial 6 h after pelvic fracture is essential
for the emergency treatment of pelvic fracture, which may improve
the hypovolemic status immediately and decrease predictable
mortality and morbidity. In addition, the Arbeit fuer Osteosynthese
(AO) classification (15) of pelvic
fractures has not been well investigated with regard to the blood
transfusion volume. Type A is defined as a stable pelvic fracture,
type B as rotationally unstable and type C as rotationally and
vertically unstable fracture.
The aim of the present study was to evaluate the
clinical outcomes of pelvic fracture and determine the blood
transfusion volume required in the initial 6 h in association with
the pelvic fracture type. The AO classification system was used to
categorize patients into pelvic fracture subgroups and determine
any association with blood transfusion. These results will help
guide transfusion requirements and identify the optimal treatment
for patients in the initial 6 h after pelvic fracture.
Patients and methods
Patients
Patients with pelvic fractures admitted to a Level I
Trauma Centre in the Qingpu Branch of Zhongshan Hospital affiliated
to Fudan University (Shanghai, China) between January 2014 and
December 2016 were retrospectively identified using CT scanning
images from the Emergency Registry of the Qingpu Branch of
Zhongshan Hospital affiliated to Fudan University (Shanghai,
China). Demographic data, abbreviated injury scale (16), injury severity score (ISS) (17) and blood transfusion requirements in
the initial 6 h after presentation of patients with pelvic fracture
to the trauma centre were recorded.
Closed pelvic fractures were included in the present
study. Open pelvic fractures, pediatric pelvic fractures and severe
soft tissue injuries were excluded. Additionally, patients with
major internal bleeding, severe illness (hypertension, heart
disease and diabetes mellitus) and abnormal coagulation diseases
were excluded to diminish their influence on the investigation.
Complete data were available for 497 patients with pelvic fracture.
Mortality was defined as the proportion of deaths among patients
with different types of pelvic fractures, whilst the morbidity was
defined as the proportion of patients with pelvic fractures out of
all trauma cases (1297) who were transported to the trauma center
within 2 h of injury.
Radiographic classification
Patients were subjected to radiological examination
according to the guidelines of Advanced Trauma Life Support
(18). CT scanning was performed
using a 64-slice multidetector CT scanner with automated tube
current modulation (Lightspeed 64VCT; GE Healthcare) to determine
the pelvic fracture type and other body system injuries on
radiographs. A fellowship-trained orthopedic traumatologist with
>10 years of experience and the institution's primary surgeon
retrospectively classified the fractures according to the AO
classification system.
Blood transfusion and emergency
measures
The indications for blood transfusion for pelvic
fracture patients are systolic blood pressure of <90 mmHg, heart
frequency >130 bpm and clinical symptoms of shock. In an
emergency, combined transfusion of red blood cells, plasma and
platelets (6-4-1) is preferred (19). A baseline blood sample is collected
prior to blood transfusion. A pelvic belt is used for pre-hospital
care. Focused assessment with sonography for trauma (FAST)
(20) ultrasound is used to detect
free intraperitoneal effusion in B- and C-type pelvic fractures. A
positive FAST examination should be followed by laparotomy when
indicated, for further investigation of the abdominal injuries and
hemorrhage. External fixations are used to control the rotationally
unstable pelvic fractures in the emergency room. Angiography and
embolism are useful for patients with arterial injuries and
pre-peritoneal pelvic packing may be an effective measure for
patients with combined abdominal injury and require emergency
laparotomy.
Statistical analysis
The Kruskal-Wallis test was used to compare the
volume of blood transfusion among pelvic fracture types. The
frequency of blood transfusion was compared using a χ2
test for categorical variables and one-way ANOVA followed by
Student-Newman-Keuls post hoc test were applied for continuous
variables. Statistical analysis was performed using SAS version 9.1
(SAS Institute). P<0.01 was considered to indicate a
statistically significant difference.
Results
General data
Complete data were available for 497 patients with
pelvic fracture (Table I). The mean
age of the patients included in the study was 32±16.5 years (range,
18–48 years) and 276 patients were male (55.5%), while 203 patients
were female (44.5%). The mechanism of injury was high-energy
impact, including traffic collision and fall from height. In the
present study, 31 patients had a systolic blood pressure of <90
mmHg, accounting for 6.2% of all cases, and 44 patients had a heart
frequency of >130 beats per min, accounting for 8.9% of all
cases. A total of 104 (20.9%) patients received blood transfusion,
with a blood transfusion volume range of 0–10,000 ml in the first 6
h (mean, 1,213.94±1,354.11 ml).
 | Table I.General characteristics of the
patients (n=497). |
Table I.
General characteristics of the
patients (n=497).
| Characteristic | Value |
|---|
| Age (years) | 32±16.5 |
| Gender |
|
|
Male | 276 (55.5) |
|
Female | 221 (44.5) |
| Mean ISS | 16±9.08 |
| Cause of
injury |
|
| Motor
vehicle collision | 306 (61.6) |
| Fall
from height | 129 (26.0) |
| Crush
injury | 35 (7.0) |
| Fall on
the ground | 22 (4.4) |
|
Other | 5
(1.0) |
| AO
classification |
|
| A | 395 (79.5) |
|
A1 | 16 (3.2) |
|
A2 | 216 (43.5) |
|
A3 | 163 (32.8) |
| B | 63
(12.7) |
|
B1 | 18 (3.6) |
|
B2 | 39 (7.9) |
|
B3 | 6
(1.2) |
| C | 39 (7.9) |
|
C1 | 26 (5.2) |
|
C2 | 10 (2.0) |
|
C3 | 3
(0.6) |
| FAST | + |
| B | 23
(36.5) |
| C | 20
(51.3) |
| Systolic blood
pressure <90 mmHg | 31 (6.2) |
| Heart frequency
>130 beats per minute | 44 (8.9) |
| Number of blood
transfusion | 104 (20.9) |
| Mean volume of
blood transfusion (ml) |
1213.94±1354.11 |
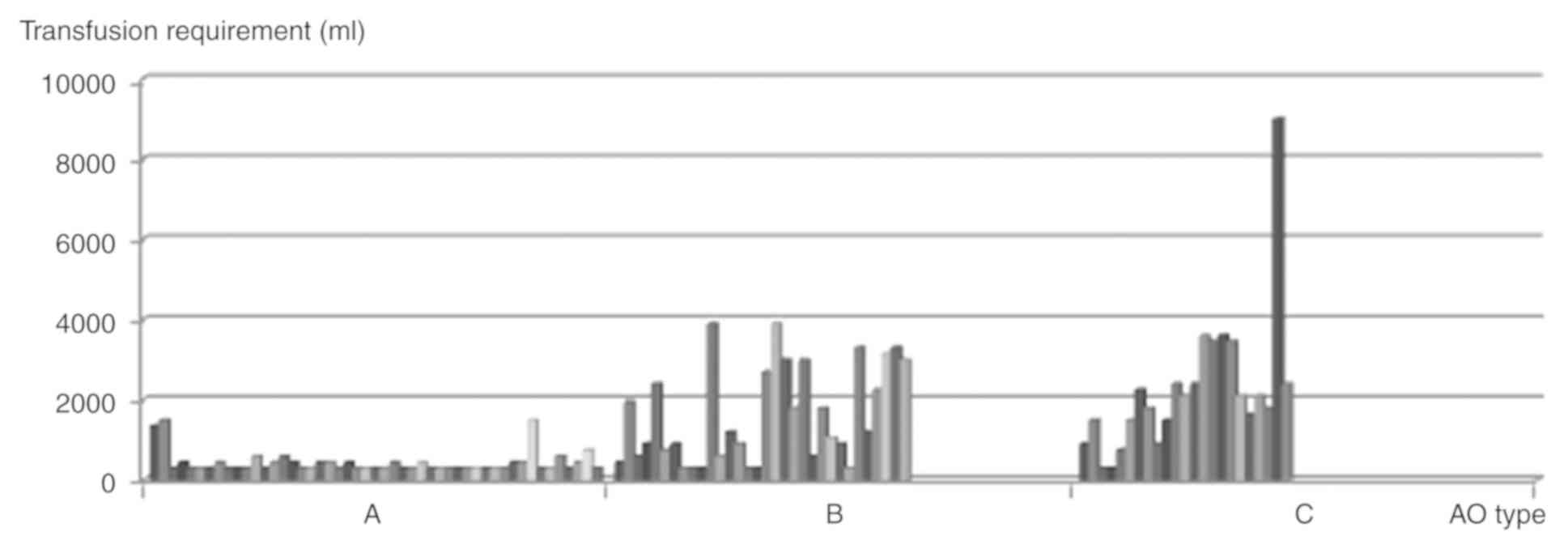
Blood transfusion
The mean blood transfusion volume was 437.76±282.02
ml for type A, 1,603.13±1,203.28 ml for type B and
2,191.30±1,740.93 ml for type C pelvic fractures (Table II). The Kruskal-Wallis test was used
to compare the blood transfusion volume among pelvic fracture
types. The results indicated a larger mean blood transfusion volume
in patients with C-type pelvic fractures as compared with that in
the other types (χ2=46.6789, degrees of freedom, F=2;
P<0.01; Fig. 1).
 | Table II.Blood transfusion and transfusion
volume compared among different AO types. |
Table II.
Blood transfusion and transfusion
volume compared among different AO types.
| AO type | Patients (n) | Transfusion | Volume (ml) |
|---|
| A | 395 | 49 (12.4) | 437.76±282.02 |
| B | 63 | 32 (50.1) |
1,603.13±1,203.28 |
| C | 39 | 323 (59.0) |
2,191.30±1,740.93a |
| Total | 497 | 104 (20.9) |
|
The distribution of the blood transfusion volume in
each pelvic fracture type was explored. There were 51 patients with
a transfusion volume of <600 ml (49.0%), 23 (22.1%) with a
transfusion volume of 600–1500 ml and 30 (28.9%) with a transfusion
volume of >1,500 ml (Table
III). The frequency of blood transfusion in the three pelvic
fracture types was determined using the χ2 test. The
results indicated that patients with C-type pelvic fractures were
significantly more likely to require a blood transfusion (59.0%)
than patients with A and B types (12.4 and 50.1%, respectively;
F=4, χ2=56.9067, P<0.01). Massive blood transfusion
was defined as >1,500 ml and compared among the groups using the
χ2 test. The results indicated that patients with C-type
pelvic fractures were significantly more likely to require massive
blood transfusion (F=2, χ2=39.7562, P<0.0001).
 | Table III.Distribution of blood transfusion
(n). |
Table III.
Distribution of blood transfusion
(n).
|
| Volume of blood
transfusion (ml) |
|
|---|
|
|
|
|
|---|
| AO type | <600 | 600–1,500 |
>1,500b | Total |
|---|
| A | 42 (79.3) | 7
(30.4) | 0 (0) | 49 |
| B | 7
(15.1) | 10 (39.1) | 15 (53.6) | 32 |
| C | 2 (5.7) | 6
(30.4) | 15 (46.4) | 23a |
| Total | 51 | 23 | 30 | 104 |
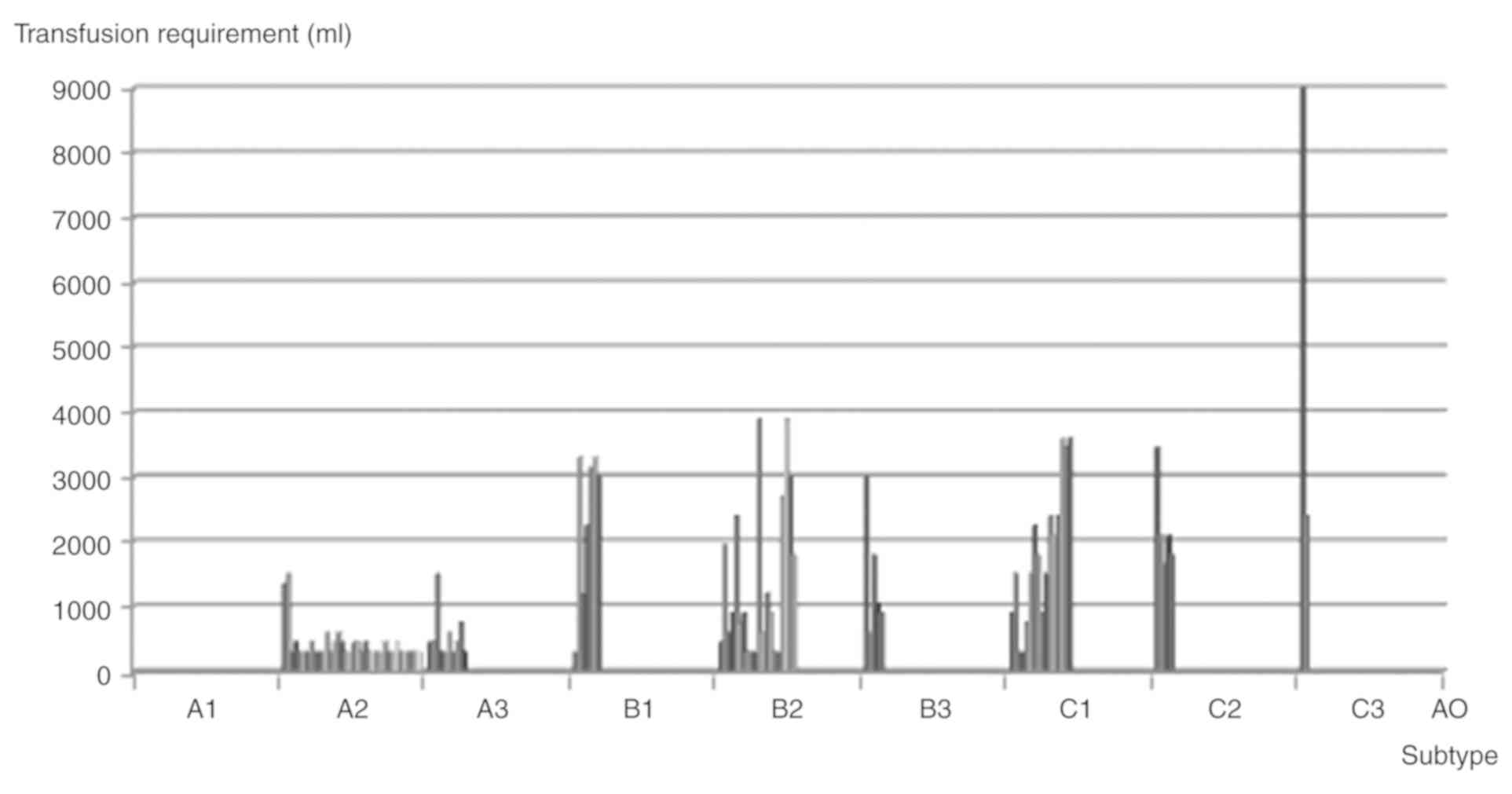
Patients with pelvic fracture were classified into
subtypes according to the AO classification system. The blood
transfusion volume in the subtypes was compared. The B3 subtype was
indicated to have the highest transfusion frequency, followed by
the C3, C1, B2 and C2 subtypes (Fig.
2). Statistical analysis was not performed due to the limited
numbers of subtypes. The mean transfusion volume for the C3 subtype
was the largest, followed by the B1, C2, C1, B3 and B2 subtypes
(Table IV).
 | Table IV.Blood transfusion and transfusion
volume compared among AO subtypes. |
Table IV.
Blood transfusion and transfusion
volume compared among AO subtypes.
| AO subtype | Patients (n) | Blood
transfusion | Volume (ml) |
|---|
| A1 | 16 | 0 (0) | 0 |
| A2 | 216 | 39 (18.1) | 407.69±255.09 |
| A3 | 163 | 10 (6.1) | 540.00±368.78 |
| B1 | 18 | 7 (38.9) |
2357.14±1183.37 |
| B2 | 39 | 20 (51.3) |
1372.50±1206.18 |
| B3 | 6 | 5 (83.3) | 1470.00±962.81 |
| C1 | 26 | 16 (61.5) |
1743.75±1000.81 |
| C2 | 10 | 5 (50.0) | 2220.00±714.67 |
| C3 | 3 | 2 (66.7) |
5700.00±4666.90 |
| Total | 497 | 104 (20.9) |
|
Comparison of the ISS among the pelvic fracture
types was performed using the Kruskal-Wallis test (Table V). It was indicated that the ISS in
the C-type pelvic fracture group was higher than that for types A
and B (χ2=106.8412, F=2, P<0.01).
 | Table V.ISS of different AO types. |
Table V.
ISS of different AO types.
| AO type | Patients (n) | ISS |
|---|
| A | 395 | 8.93±6.38 |
| B | 63 | 17.95±9.21 |
| C | 39 |
19.46±6.12a |
A total of 23 of the 63 patients with B-type pelvic
fractures (36.5%) and 20 of the 39 patients with C-type pelvic
fractures (51.3%) had a positive FAST result (Table I). A positive FAST examination should
be followed by laparotomy when indicated, in order to further
investigate the abdominal injuries and hemorrhage (20). External fixation was used in 96
patients, angiography was performed to identify arterial hemorrhage
and embolism in 9 patients with pelvic fractures. Pre-peritoneal
pelvic packing was performed in 5 patients to treat venous
hemorrhage. In addition, 150/497 (30.2%) of fracture patients were
hospitalized (mean stay, 18±6.5 days) and 59 were admitted to the
intensive care unit (ICU; mean stay, 9±7.3 days). Comparison of the
hospital and ICU days among the pelvic fracture types was performed
using Kruskal-Wallis tests (Table
VI). The mean hospital stay was found to be 10±2.0 days in type
A (69, 17.5%), 14±4.1 days in type B (42, 66.7%), and 24±3.8 days
in type C (39, 100%). The mean ICU stay was found to be 7±5.2 days
in type B (24, 38.1%) and 16±4.7 days in type C (35, 89.7%). The
results indicated that the number of days of stay at the hospital
and at the ICU of the C-type pelvic fracture group were higher than
those for types A and B (P<0.01). A total of 18 patients
contracted an infection, all of which were treated with antibiotics
and debridement. The infection was cured in all patients. A total
of 12 patients with pelvic fracture eventually suffered disability
of varying degrees.
 | Table VI.Hospital stay and ICU days. |
Table VI.
Hospital stay and ICU days.
| AO type | Total patients | Patients in
hospital [n, (%)] | Hospital stay
(days) | Patients in ICU [n,
(%)] | ICU stay
(days) |
|---|
| A | 395 | 69 (17.5) | 10±2.0 | 0 | 0 |
| B | 63 | 42 (66.7) | 14±4.1 | 24 (38.1) | 7±5.2 |
| C | 39 | 39 (100) | 24±3.8a | 35 (89.7) | 16±4.7a |
| Total | 497 | 150 (30.2) | 18±6.5 | 59 (11.9) | 9±7.3 |
Mortality and morbidity
A total of 9 patients died in the present study, 4
of which were categorized as type B, 4 as type C and 1 as type A.
The overall mortality rate in the present cohort was 1.8%. The 9
patients who died had suffered multiple injuries, including head
(n=3), thoracic (n=3), abdominal (n=2) spinal (n=2) and limb injury
(n=2). High ISS were observed in those patients (mean ISS, 29). The
mean volume of blood transfusion was 1,816 ml in the initial 6 h
for patients who died; specifically, it was 1,200 ml in type A,
1,686 ml in type B and 2,100 ml in type C (Table VII).
 | Table VII.Mortality and morbidity. |
Table VII.
Mortality and morbidity.
| AO type | Mortality | Morbidity | Volume of blood
transfusion (ml) |
|---|
| A | 1 (0.3) | 395
(30.5a) | 1,200 |
| B | 4 (6.3) | 63 (4.8) | 1,686 |
| C | 4b (10.3) | 39 (3.0) | 2,100 |
The association between mortality and pelvic
fracture type was determined using the χ2 test (Table VII). The mortality of each pelvic
fracture type was 0.3% (1/395) for type A, 6.3% (4/63) for type B
and 10.3% (4/39) for type C. The results suggested that the
mortality in type C was higher than that in types A and B (F=2,
χ2=28.3328, P<0.0001).
The morbidity of each pelvic fracture type was 30.5%
(395/1,297) for type A, 4.8% (63/1,297) for type B and 3.0%
(39/1,297) for type C. Comparison of the morbidity among the pelvic
fracture types was performed using the χ2 test. The
results suggested that the morbidity in type A was higher than that
in B and C (P<0.01).
Discussion
The clinical data provided in the present study
revealed that the blood transfusion frequency and volume increased
with the severity of pelvic ring disruptions. The B3 subtype with
injuries in the bilateral sacroiliac joints had the highest
transfusion frequency, while the C3 subtype with severe
displacement of pelvic fracture received the largest blood
transfusion volume.
High-energy impact of the anterior pelvic ring
changes the volume of the pelvis and pressure status, resulting in
major hemorrhage (5,11,13,21–23). A
vertical displacement of the pelvic fracture is likely to lead to
vessel ruptures (5,8,22,24).
Previous studies have reported the clinical outcomes of blood
transfusion in pelvic fracture patients and attempted to associate
the requirement for, frequency and volume of blood transfusion with
the pelvic fracture type (1–5,9,13,14,21,22). The
Young and Burgess classification system is used to determine the
requirement for blood transfusion. The anteroposterior compression
(APC II and III) and lateral compression (LC III) types have been
indicated to require a higher blood transfusion volume and be
associated with high mortality (3,5,8,12,22). On
the contrary, certain studies have been unable to demonstrate that
pelvic fracture types comprise a clinical predictor of blood
transfusion volume and frequency (4,21,25).
Magnussen et al (12)
reported that nearly 50% (10/25) of APC II and III or LC III
injuries require significant blood transfusion (3.5–12.0 units) in
the first 24 h after injury. Furthermore, patients with an APC
III-type pelvic fracture had a transfusion frequency of 61% and
transfusion volume of 12.6 units. Hamill et al (22) reported on 76 patients transfused with
6 or more units of blood in the first 24 h. The mean blood
transfusion requirement in the first 6 h from injury was 14 units
in embolized and 8 units in non-embolized patients. Transfusion
frequencies of 30–55% have been reported (12,13,22); in
the present study, the transfusion frequency was 20.6%, which was
close to that reported by Blackmore et al (13). Burgess et al (3) determined a progressively larger mean
transfusion volume with the progression from grade I to III in the
APC and LC fracture types. However, more frequent pelvic
fracture-associated injuries were also reported as the severity of
pelvic fracture increased, likely contributing to the increased
transfusion volume.
Previous studies have defined the timing of blood
transfusion from 24 (12), 48
(14) to 72 h (13) after admission. In the present study,
patients with pelvic fracture were transported to our Level I
Trauma Centre within 2 h from the trauma with the aid of a medical
rescue system. Blood transfusion was performed in the initial 6 h
after pelvic fracture, based on the results of physical examination
and clinical symptoms of shock.
The blood transfusion frequency and volume in the
present study was similar to that in the study by Burgess et
al (3). C-type pelvic fractures
require a considerably larger blood transfusion volume, with almost
60% of patients requiring transfusion. However, the same result was
reported for the APC III type (3,12). The
considerably larger mean transfusion volume in the APC III type in
Burgess' study compared with that in the present study supports
this conclusion, since the C1 type in the AO classification system
corresponds to the APC III type in that of Young and Burgess.
In the present study, ~50% pelvic fracture patients
(types B and C) received blood transfusions of >1,500 ml.
Similarly, unstable pelvic fractures, including APC II, APC III and
LC III injuries, received a high blood transfusion volume (3,5,8,12,22).
In addition, patients with pelvic fractures were
classified into subtypes according to the AO classification system.
The blood transfusion frequency and volume were analysed in
association with the subtypes. The B3 subtype of pelvic fracture
had the highest transfusion frequency (53.6%), which was consistent
with the results of Magnussen et al (12). Nearly 70% of patients of the C3
subtype received a blood transfusion volume of >1,500 ml. In the
present analysis, the AO classification system was proven to be as
effective as the system of Young and Burgess (26).
In the present study, massive blood transfusion was
defined as >1,500 ml. The results indicated that C-type pelvic
fractures are more likely to require massive blood transfusion. The
same results were reported in other studies (12,13,22).
The ISSs of unstable pelvic fractures (types B and
C) were higher than those for type A, due to the severity of pelvic
disruptions and associated injuries. This result was consistent
with that of Hamill et al (22).
Previous studies reported an overall mortality of
10–26% (5,13,27),
while that for type C was 20% (3).
The overall mortality in the present study was 1.8% and that of
type C was ≤10.3%, which was inconsistent with the results of the
aforementioned studies (3,5,13,27).
High ISS, severe associated injuries and massive blood transfusion
volume are recognized as risk factors for mortality in patients
with pelvic fracture (1,4). In the present study, multiple traumas
were observed in those patients that died, with the associated
injuries and high blood loss volume proving to be risk factors for
mortality. Of those patients, >2,000 ml blood transfusion was
required for patients with C-type pelvic fractures in the initial 6
h, which required addition intensive care. The blood transfusion
volume required in the initial 6 h for patients who died with types
A and B were >1,000 ml and 1,500 ml, respectively. This result
from the patients who died suggested an association between the
blood transfusion volume and the pelvic fracture type. However,
statistical analysis was not performed due to the limited numbers
of types, which was another limitation of present study.
Paydar et al (1) developed a system to determine whether
patients were in good or poor condition. Patients in poor condition
had a lower pH, base excess and hemoglobin level, and required more
packed red cell transfusion and a larger volume of infused
intravenous fluid.
In the present study, all pelvic fractures were
defined as closed injuries. Open pelvic fractures with combined
devastating soft-tissue injuries have been reported to have
relatively higher transfusion requirements and a higher mortality
rate (28). Hasankhani and
Omidi-Kashani (28) reported on 15
cases of open pelvic fracture associated with extensive perineal
injury. The average blood transfusion volume was 8 packed red blood
cell units (range, 4–21 units). A total of 2 patients with APC type
III fractures were in deep shock, 1 received 21 units of blood and
survived, and 1 received 18 units and died post-operatively due to
an associated intra-abdominal injury. The blood transfusion and
mortality rates in that study were considerably higher than those
in the present one.
The optimal treatment strategy would take into
consideration the hemodynamic status, disruptions of the pelvic
ring and associated injuries. The aim of pelvic fracture patient
management is to definitively restore hemodynamic and mechanical
stability of the pelvic ring and repair associated injuries. The
management of trauma must therefore be multidisciplinary and
ultimately based on the physiology of the patient and the mechanism
of the injury (29,30).
In the present study, a strong association was
observed between blood transfusion volume and frequency in the
initial 6 h and pelvic fracture type, and the subtypes with the
highest transfusion frequency and largest blood transfusion volume
were identified. Previous studies, which examined pelvic fracture
types and attempted to assess whether the type may predict the
outcome, have been limited by the time of transfusion and
classification systems for pelvic fractures. In the present study,
by demonstrating the marked association between pelvic fracture
type and clinical outcome, including blood transfusion, it was
indicated that pelvic fracture types may be used as an AO predictor
of pelvic blood transfusion and help develop and validate a
clinical prediction rule that relies on immediately obvious
clinical factors, including fracture type and emergency department
presentation, defining clinical predictors that may identify
patients that are highly likely to require massive blood
transfusion.
The present study had several significant
limitations. First, the study was a retrospective, single-center
investigation with the associated limitations. Furthermore, pelvic
fracture-associated injuries, which may have led to an increase in
the requirement for blood transfusion, were not entirely excluded
from the study. However, separation of pelvic fractures and
associated injuries may not represent the real severity of trauma
and the overall amount of hemorrhage. Finally, patients with pelvic
fracture may have delayed hemorrhage in the initial 6 h after
pelvic fracture.
In conclusion, patients with AO fracture type A, B
and C resulting from high-energy pelvic impact had a progressively
larger mean transfusion volume, transfusion frequency and mortality
in the initial 6 h after pelvic fracture. The B3 subtype was
indicated to have the highest frequency of blood transfusion and
the C3 subtype required the largest blood transfusion volume. The
AO classification system is an effective and validated protocol for
investigations on pelvic fracture.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All the data and materials are available from the
corresponding author on reasonable request, as applicable.
Authors' contributions
QY, KJ and XT were responsible for case collection;
TW was responsible for statistical analysis; LA and DG were
responsible for calculating volumes of blood transfusion; YF, NC
and FP were responsible for analysis of clinical information.
Ethics approval and consent to
participate
This study was approved by the ethics committee of
Qingpu Branch, Zhongshan Hospital affiliated to Fudan University
(approval no. 201914; Shanghai, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Paydar S, Chaabi M, Akhavan M, Ghahramani
Z and Dehghankhalili M: Outcome determinants of patients with
traumatic pelvic fractures: A cohort study in a level i trauma
center in southern iran. Malays Orthop J. 11:23–30. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rehwald R, Schönherr E, Petersen J, Jeske
HC, Fialkovska A, Luger AK, Grams AE, Loizides A, Jaschke W and
Glodny B: Prognostic factors in endovascular treated pelvic
haemorrhage after blunt trauma. BMC Surg. 17:892017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Burgess AR, Eastridge BJ, Young JW,
Ellison TS, Ellison PS Jr, Poka A, Bathon GH and Brumback RJ:
Pelvic ring disruptions: Effective classification system and
treatment protocols. J Trauma. 30:848–856. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Starr AJ, Griffin DR, Reinert CM, Frawley
WH, Walker J, Whitlock SN, Borer DS, Rao AV and Jones AL: Pelvic
ring disruptions: Prediction of associated injuries, transfusion
requirement, pelvic arteriography, complications, and mortality. J
Orthop Trauma. 16:553–561. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dalal SA, Burgess AR, Siegel JH, Young JW,
Brumback RJ, Poka A, Dunham CM, Gens D and Bathon H: Pelvic
fracture in multiple trauma: Classification by mechanism is key to
pattern of organ injury, resuscitative requirements, and outcome. J
Trauma. 29:981–1002. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Papadopoulos IN, Kanakaris N, Bonovas S,
Triantafillidis A, Garnavos C, Voros D and Leukidis C: Auditing 655
fatalities with pelvic fractures by autopsy as a basis to evaluate
trauma care. J Am Coll Surg. 203:30–43. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen TW, Yang ZG, Dong ZH, Tang SS, Chu ZG
and Shao H: Earthquake-related pelvic crush fracture vs.
non-earthquake fracture on digital radiography and MDCT: A
comparative study. Clinics (Sao Paulo). 66:629–634. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Eastridge BJ, Starr A, Minei JP, O'Keefe
GE and Scalea TM: The importance of fracture pattern in guiding
therapeutic decision-making in patients with hemorrhagic shock and
pelvic ring disruptions. J Trauma. 53:446–451. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Vaidya R, Waldron J, Scott A and Nasr K:
Angiography and embolization in the management of bleeding pelvic
fractures. J Am Acad Orthop Surg. 26:e68–e76. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hussami M, Grabherr S, Meuli RA and
Schmidt S: Severe pelvic injury: Vascular lesions detected by ante-
and post-mortem contrast medium-enhanced CT and associations with
pelvic fractures. Int J Legal Med. 131:731–738. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Burlew CC, Moore EE, Stahel PF, Geddes AE,
Wagenaar AE, Pieracci FM, Fox CJ, Campion EM, Johnson JL and
Mauffrey C: Preperitoneal pelvic packing reduces mortality in
patients with life-threatening hemorrhage due to unstable pelvic
fractures. J Trauma Acute Care Surg. 82:233–242. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Magnussen RA, Tressler MA, Obremskey WT
and Kregor PJ: Predicting blood loss in isolated pelvic and
acetabular high-energy trauma. J Orthop Trauma. 21:603–607. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Blackmore CC, Jurkovich GJ, Linnau KF,
Cummings P, Hoffer EK and Rivara FP: Assessment of amount of
hemorrhage and outcome from pelvic fracture. Arch Surg.
138:504–509. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Blackmore CC, Cummings P, Jurkovich GJ,
Linnau KF, Hoffer EK and Rivara FP: Predicting major hemorrhage in
pelvic fracture. J Trauma. 61:346–352. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Marsh JL, Slongo TF, Agel J, Broderick JS,
Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B
and Audigé L: Fracture and dislocation classification compendium
−2007: Orthopaedic trauma association classification, database and
outcomes committee. J Orthop Trauma. 21 (10 Suppl):S1–S133. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Association for the Advancement of
Automotive Medicine (AAAM), . The abbreviated injury scale
(AIS)-1990 revision. AAAM. (Chicago, IL). 11–15. 1990.
|
|
17
|
Baker SP, O'Neill B, Haddon W Jr and Long
WB: The injury severity score: A method for describing patients
with multiple injuries and evaluating emergency care. J Trauma.
14:187–196. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
American College of Surgeons Committee on
Trauma, . Advanced Trauma Life Support for Doctors. American
College of Surgeons. (Chicago, IL). 2004.
|
|
19
|
Lal DS and Shaz BH: Massive transfusion:
Blood component ratios. Curr Opin Hematol. 20:521–525. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Miller PR, Moore PS, Mansell E, Meredith
JW and Chang MC: External fixation or arteriogram in bleeding
pelvic fracture: Initial therapy guided by markers of arterial
hemorrhage. J Trauma. 54:437–443. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tang CH, Shivji F and Forward D: Major
haemorrhage in pubic rami fractures. BMJ Case Rep.
bcr20142080882015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hamill J, Holden A, Paice R and Civil I:
Pelvic fracture pattern predicts pelvic arterial hemorrhage. Aust N
Z J Surg. 70:338–343. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Barratt RC, Bernard J, Mundy AR and
Greenwell TJ: Pelvic fracture urethral injury in males-mechanisms
of injury, management options and outcomes. Transl Androl Urol. 7
(Suppl 1):S29–S62. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Jang JY, Shim H, Jung PY, Kim S and Bae
KS: Preperitoneal pelvic packing in patients with hemodynamic
instability due to severe pelvic fracture: Early experience in a
Korean trauma center. Scand J Trauma Resusc Emerg Med. 24:32016.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sarin EL, Moore JB, Moore EE, Shannon MR,
Ray CE, Morgan SJ and Smith WR: Pelvic fracture pattern does not
always predict the need for urgernt embolization. J Trauma.
58:973–977. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Osterhoff G, Scheyerer MJ, Fritz Y,
Bouaicha S, Wanner GA, Simmen HP and Werner CM: Comparing the
predictive value of the pelvic ring injury classification systems
by Tile and by Young and Burgess. Injury. 45:742–747. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Gustavo Parreira J, Coimbra R, Rasslan S,
Oliveira A, Fregoneze M and Mercadante M: The role of associated
injuries on outcome of blunt trauma patients sustaining pelvic
fractures. Injury. 31:677–682. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hasankhani EG and Omidi-Kashani F:
Treatment outcomes of open pelvic fractures associated with
extensive perineal injuries. Clin Orthop Surg. 5:263–268. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Coccolini F, Stahel PF, Montori G, Biffl
W, Horer TM, Catena F, Kluger Y, Moore EE, Peitzman AB, Ivatury R,
et al: Pelvic trauma: WSES classification and guidelines. World J
Emerg Surg. 12:52017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jovanovic B, Milan Z, Djuric O,
Markovic-Denic L, Karamarkovic A, Gregoric P, Doklestic K,
Avramovic J, Velickovic J and Bumbasirevic V: Twenty-eight-day
mortality of blunt traumatic brain injury and co-injuries requiring
mechanical ventilation. Med Princ Pract. 25:435–441. 2016.
View Article : Google Scholar : PubMed/NCBI
|