|
1
|
Sampson N, Untergasser G, Plas E and
Berger P: The ageing male reproductive tract. J Pathol.
211:206–218. 2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Afriyie DK, Asare GA, Bugyei K, Adjei S,
Lin JM, Peng J and Hong ZF: Treatment of benign prostatic
hyperplasia with Croton membranaceus in an experimental animal
model. J Ethnopharmacol. 157:90–98. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Gratzke C, Schlenker B, Weidlich P, Seitz
M, Reich O and Stief CG: Benign prostatic hyperplasia: Background
and diagnosis. MMW Fortschr Med. 149:25–28. 2007.(In German).
PubMed/NCBI
|
|
4
|
Schauer IG and Rowley DR: The functional
role of reactive stroma in benign prostatic hyperplasia.
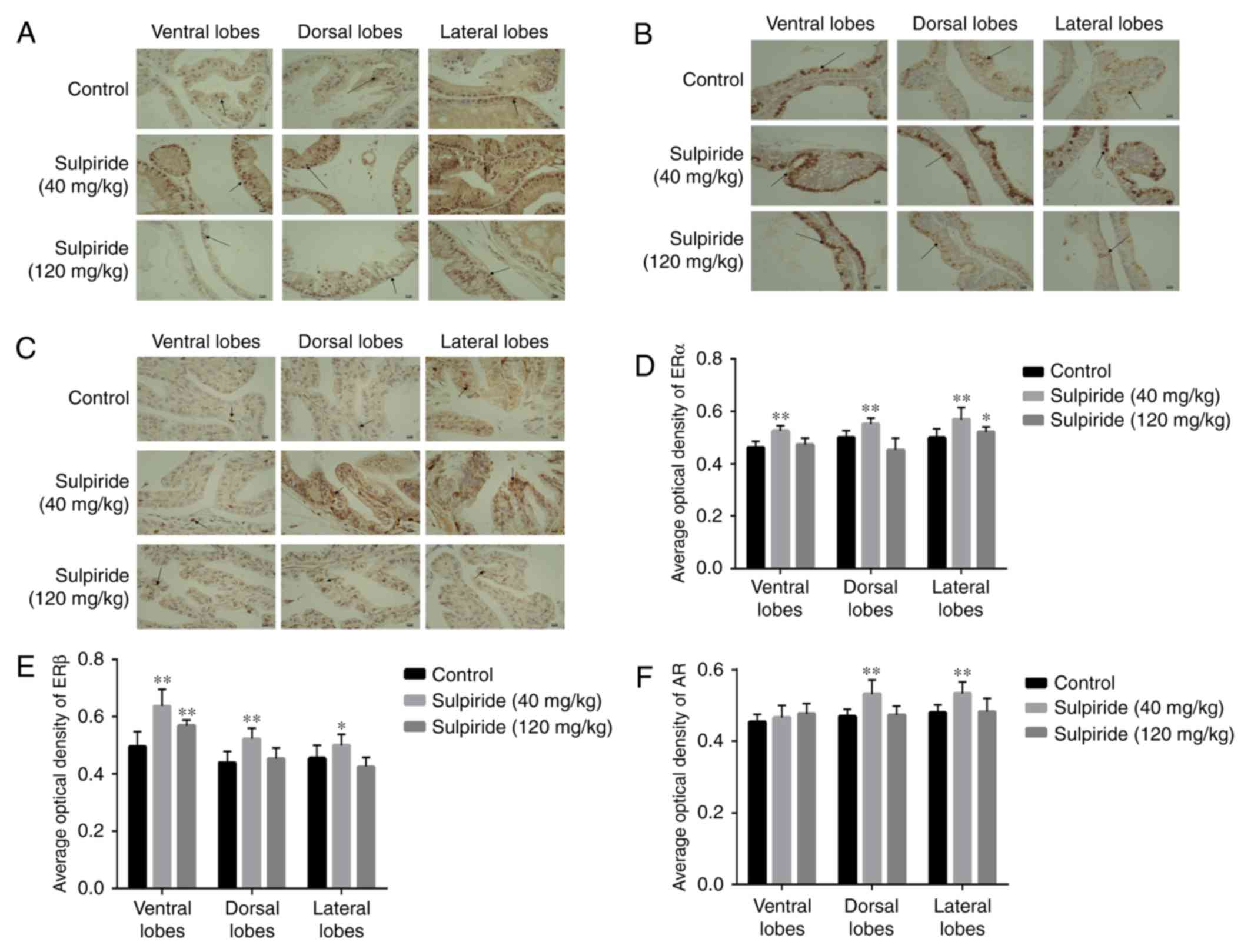
Differentiation. 82:200–210. 2011.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Akanni OO, Abiola OJ and Adaramoye OA:
Methyl Jasmonate ameliorates testosterone propionate-induced
prostatic hyperplasia in castrated wistar rats. Phytother Res.
31:647–656. 2017.PubMed/NCBI View
Article : Google Scholar
|
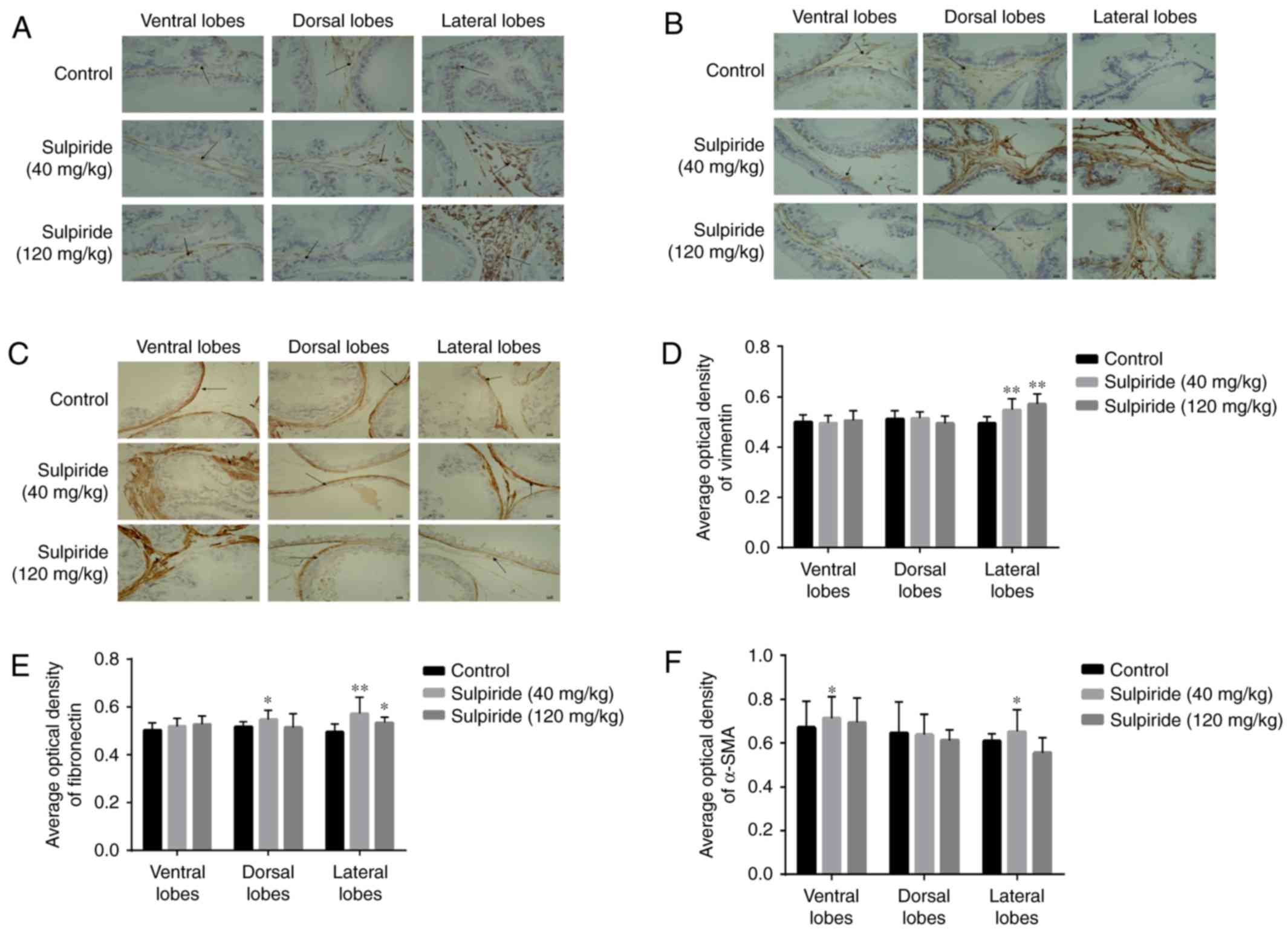
|
6
|
Kristiansen JE, Dastidar SG, Palchoudhuri
S, Roy DS, Das S, Hendricks O and Christensen JB: Phenothiazines as
a solution for multidrug resistant tuberculosis: From the origin to
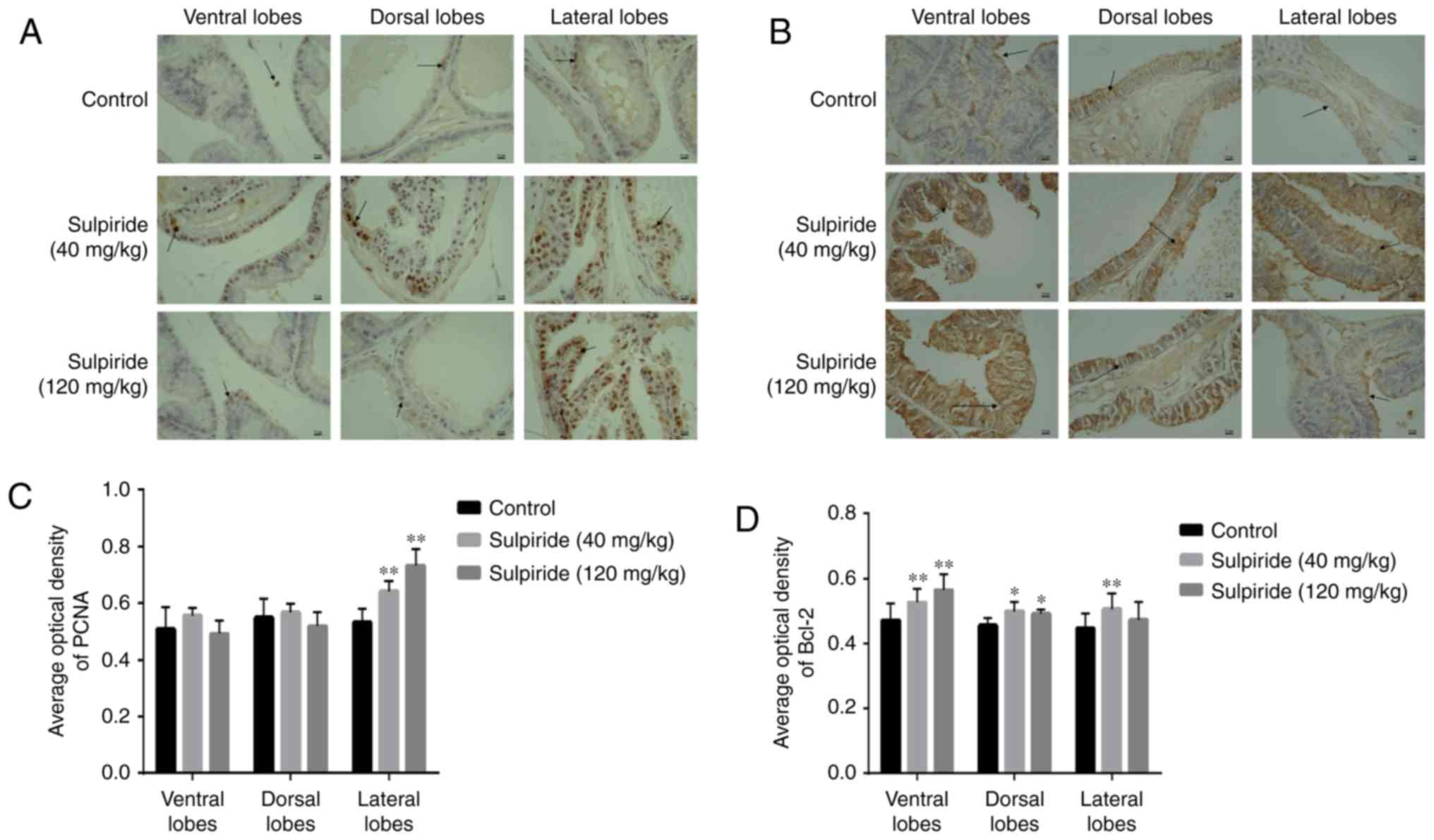
present. Int Microbiol. 18:1–12. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Martynova NA and Gorokhova LG: Toxicity
assessment of sulpiride as the basis of its hygienic
standardization. Gig Sanit. 94:114–117. 2015.PubMed/NCBI
|
|
8
|
Van Coppenolle F, Slomianny C, Carpentier
F, Le Bourhis X, Ahidouch A, Croix D, Legrand G, Dewailly E,
Fournier S, Cousse H, et al: Effects of hyperprolactinemia on rat
prostate growth: Evidence of androgeno-dependence. Am J Physiol
Endocrinol Metab. 280:E120–E129. 2001.PubMed/NCBI View Article : Google Scholar
|
|
9
|
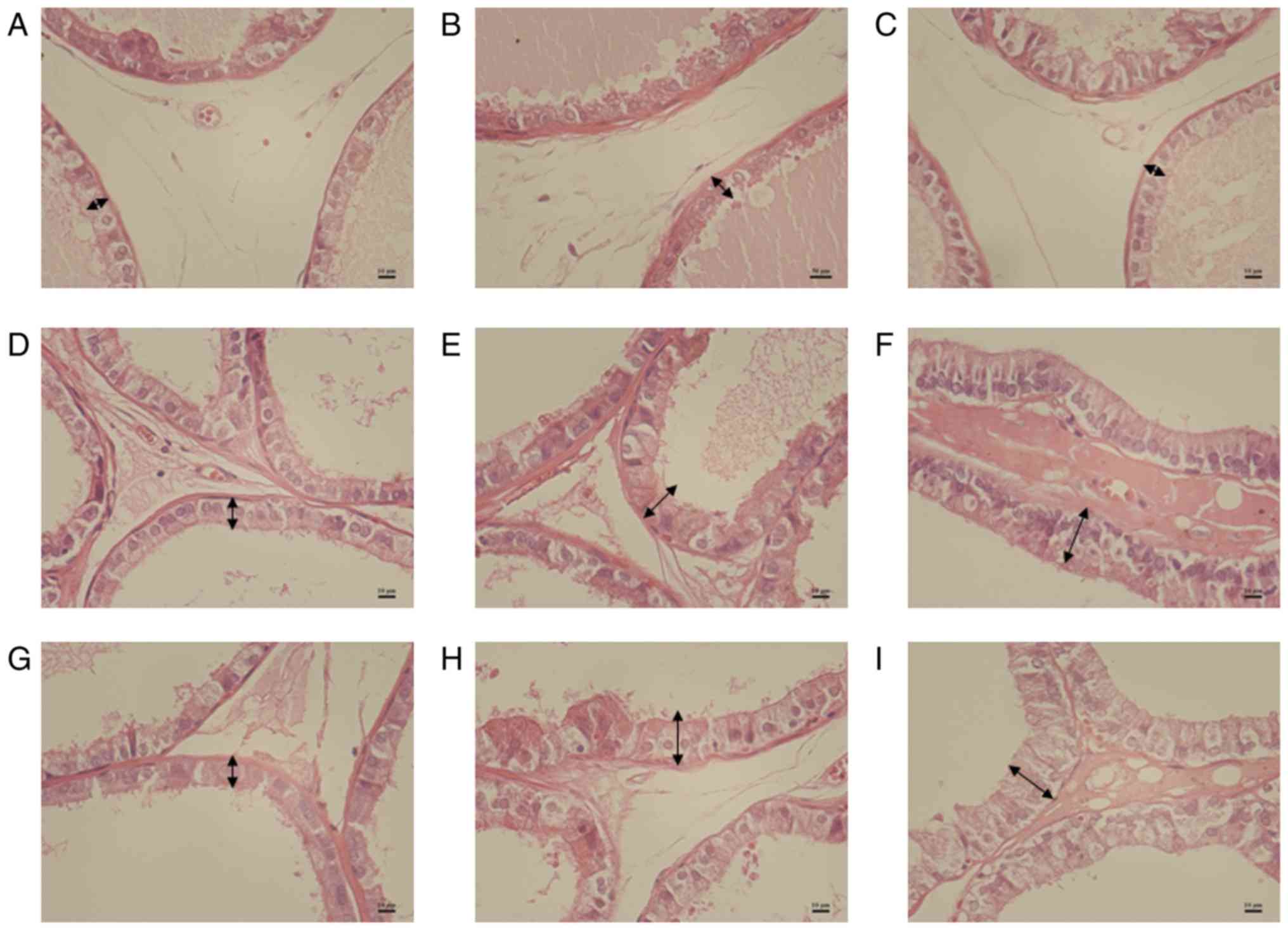
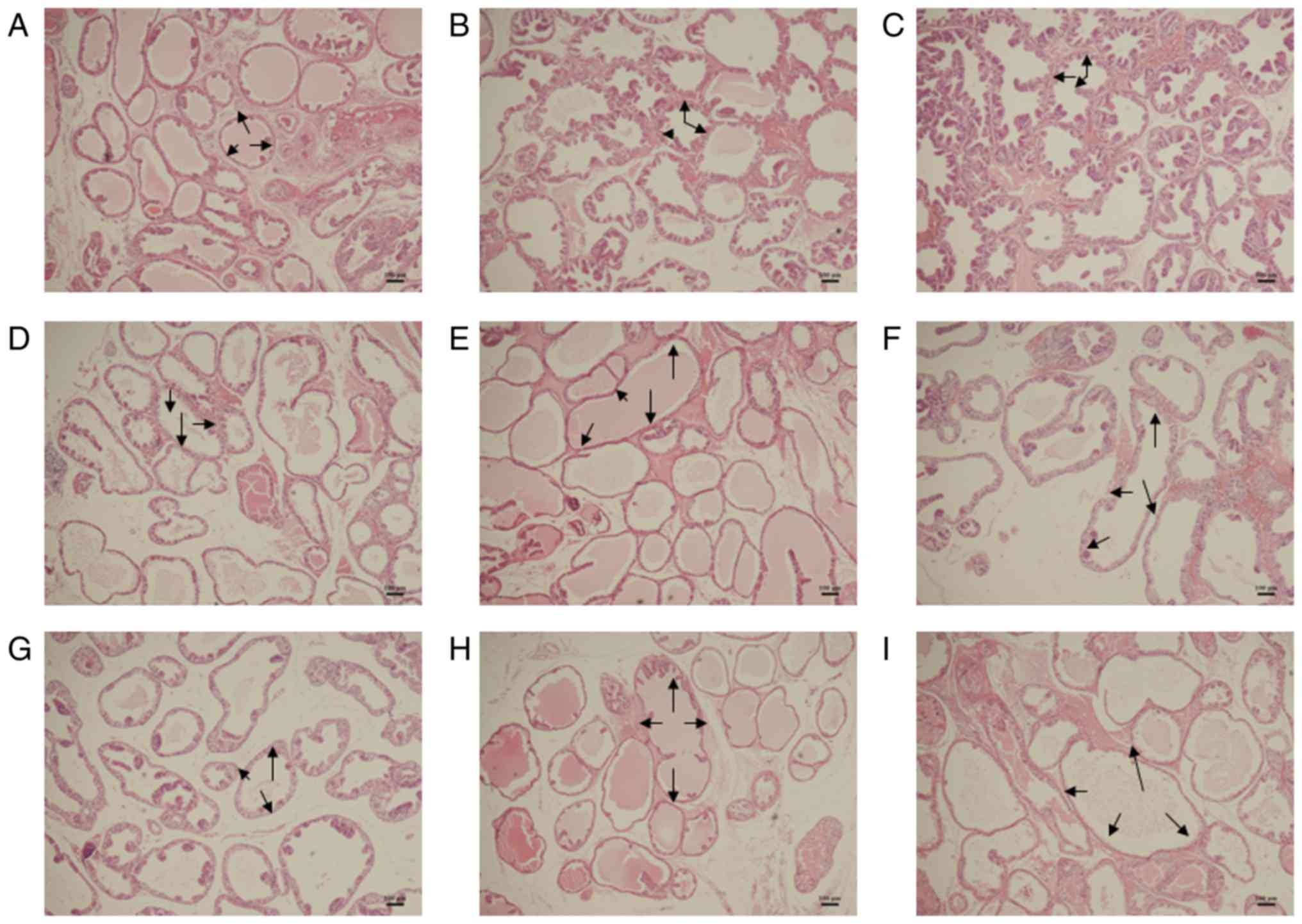
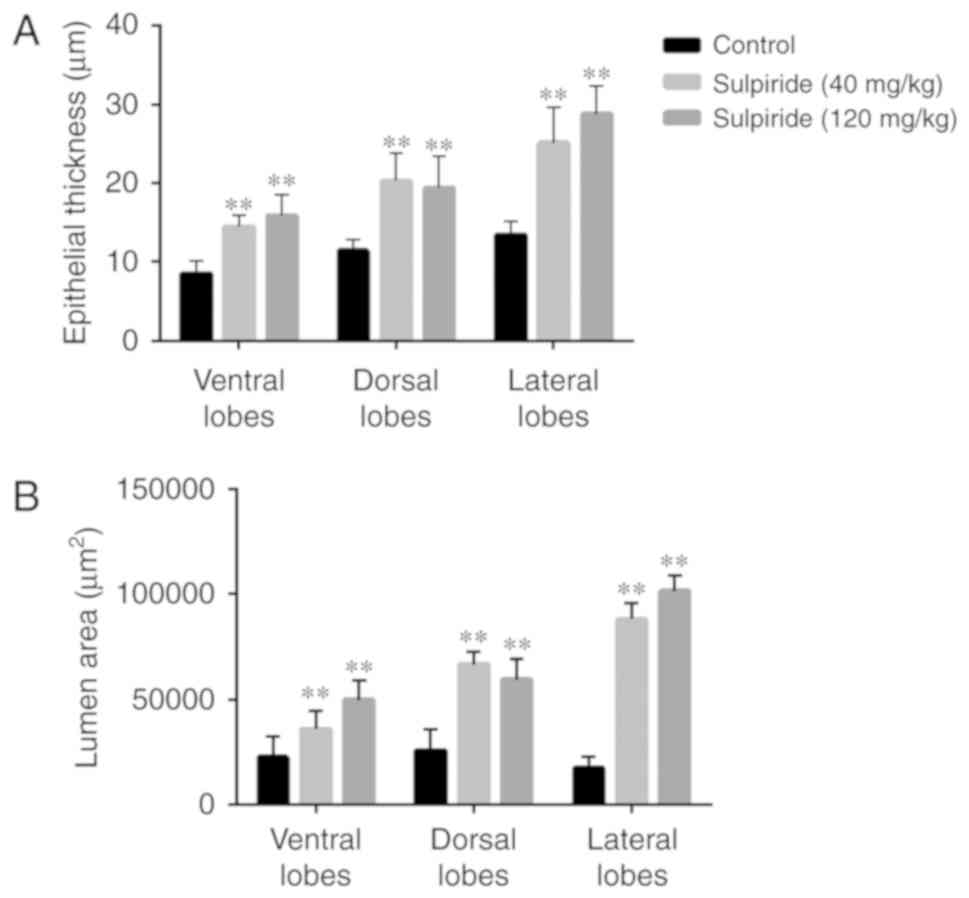
Słuczanowska-Głąbowska S, Laszczyńska M,
Wylot M, Głąbowski W, Piasecka M and Gącarzewicz D: Morphological
and immunohistochemical comparison of three rat prostate lobes
(lateral, dorsal and ventral) in experimental hyperprolactinemia.
Folia Histochem Cytobiol. 48:447–454. 2010.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Payne MR, Howie PW, McNeilly AS, Cooper W,
Marnie M and Kidd L: Sulpiride and the potentiation of progestogen
only contraception. Br Med J (Clin Res Ed). 291:559–561.
1985.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Farnsworth WE: Prolactin effect on the
permeability of human benign hyperplastic prostate to testosterone.
Prostate. 12:221–229. 1988.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wolf K, Kayacelebi H, Urhausen C,
Piechotta M, Mischke R, Kramer S, Einspanier A, Oei CH and
Gunzel-Apel A: Testicular steroids, prolactin, relaxin and prostate
gland markers in peripheral blood and seminal plasma of normal dogs
and dogs with prostatic hyperplasia. Reprod Domest Anim. 47:(Suppl
6). 243–246. 2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Drobnis EZ and Nangia AK: Psychotropics
and male reproduction. Adv Exp Med Biol. 1034:63–101.
2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Zeng QS, Xu CL, Liu ZY, Wang HQ, Yang B,
Xu WD, Jin TL, Wu CY, Huang G, Li Z, et al: Relationship between
serum sex hormones levels and degree of benign prostate hyperplasia
in Chinese aging men. Asian J Androl. 14:773–777. 2012.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ahonen TJ, Härkönen PL, Rui H and
Nevalainen MT: PRL signal transduction in the epithelial
compartment of rat prostate maintained as long-term organ cultures
in vitro. Endocrinology. 143:228–238. 2002.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Thomas LN, Merrimen J, Bell DG, Rendon R
and Too CK: Prolactin- and testosterone-induced carboxypeptidase-D
correlates with increased nitrotyrosines and Ki67 in prostate
cancer. Prostate. 75:1726–1736. 2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Pechenino AS and Brown TR: Superoxide
dismutase in the prostate lobes of aging brown Norway rats.
Prostate. 66:522–535. 2006.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Reiter E, Lardinois S, Klug M, Sente B,
Hennuy B, Bruyninx M, Closset J and Hennen G: Androgen-independent
effects of prolactin on the different lobes of the immature rat
prostate. Mol Cell Endocrinol. 112:113–122. 1995.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Bole-Feysot C, Goffin V, Edery M, Binart N
and Kelly PA: Prolactin (PRL) and its receptor: Actions, signal
transduction pathways and phenotypes observed in PRL receptor
knockout mice. Endocr Rev. 19:225–268. 1998.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Costello LC and Franklin RB: Effect of
prolactin on the prostate. Prostate. 24:162–166. 1994.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Roehrborn CG: Pathology of benign
prostatic hyperplasia. Int J Impot Res. 20 (Suppl 3):S11–S18.
2008.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Porcaro AB, Migliorini F, Petrozziello A,
Sava T, Romano M, Caruso B, Cocco C, Ghimenton C, Zecchinini AS,
Lacola V, et al: Follicle-stimulating hormone and the
pituitary-testicular-prostate axis at the time of initial diagnosis
of prostate cancer and subsequent cluster selection of the patient
population undergoing standard radical prostatectomy. Urol Int.
90:45–55. 2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Chowen-Breed J, Fraser HM, Vician L,
Damassa DA, Clifton DK and Steiner RA: Testosterone regulation of
proopiomelanocortin messenger ribonucleic acid in the arcuate
nucleus of the male rat. Endocrinology. 124:1697–1702.
1989.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Rasmussen DD, Sarkar DK, Roberts JL and
Gore AC: Chronic daily ethanol and withdrawal: 4. Long-term changes
in plasma testosterone regulation, but no effect on GnRH gene
expression or plasma LH concentrations. Endocrine. 22:143–150.
2003.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ottenweller JE, Li MT, Giglio W, Anesetti
R, Pogach LM and Huang HF: Alteration of follicle-stimulating
hormone and testosterone regulation of messenger ribonucleic acid
for Sertoli cell proteins in the rat during the acute phase of
spinal cord injury. Biol Reprod. 63:730–735. 2000.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Mattsson P and Medvedev A: Modeling of
testosterone regulation by pulse-modulated feedback. Adv Exp Med
Boil. 823:23–40. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Schanbacher BD: Testosterone regulation of
luteinizing hormone and follicle stimulating hormone secretion in
young male lambs. J Anim Sci. 51:679–684. 1980.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Alonso-Magdalena P, Brössner C, Reiner A,
Cheng G, Sugiyama N, Warner M and Gustafsson JA: A role for
epithelial-mesenchymal transition in the etiology of benign
prostatic hyperplasia. Proc Natl Acad Sci USA. 106:2859–2863.
2009.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Shoieb SM, Esmat A, Khalifa AE and
Abdel-Naim AB: Chrysin attenuates testosterone-induced benign
prostate hyperplasia in rats. Food Chem Toxicol. 111:650–659.
2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Shi X, Peng Y, Du X, Liu H, Klocker H, Lin
Q, Shi J and Zhang J: Estradiol promotes epithelial-to-mesenchymal
transition in human benign prostatic epithelial cells. Prostate.
77:1424–1437. 2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Tsurusaki T, Aoki D, Kanetake H, Inoue S,
Muramatsu M, Hishikawa Y and Koji T: Zone-dependent expression of
estrogen receptors alpha and beta in human benign prostatic
hyperplasia. J Clin Endocrinol Metab. 88:1333–1340. 2003.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Nicholson TM and Ricke WA: Androgens and
estrogens in benign prostatic hyperplasia: Past, present and
future. Differentiation. 82:184–199. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Song L, Shen W, Zhang H, Wang Q, Wang Y
and Zhou Z: Differential expression of androgen, estrogen, and
progesterone receptors in benign prostatic hyperplasia. Bosn J
Basic Med Sci. 16:201–208. 2016.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Choi HM, Jung Y, Park J, Kim HL, Youn DH,
Kang J, Jeong MY, Lee JH, Yang WM, Lee SG, et al: Cinnamomi Cortex
(Cinnamomum verum) suppresses testosterone-induced benign prostatic
hyperplasia by regulating 5α-reductase. Sci Rep.
6(31906)2016.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Roper WG: The prevention of benign
prostatic hyperplasia (bph). Med Hypotheses. 100:4–9.
2017.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Luo Y, Waladali W, Li S, Zheng X, Hu L,
Zheng H, Hu W and Chen C: 17beta-estradiol affects proliferation
and apoptosis of rat prostatic smooth muscle cells by modulating
cell cycle transition and related proteins. Cell Biol Int.
32:899–905. 2008.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Saito M, Tsounapi P, Oikawa R, Shimizu S,
Honda M, Sejima T, Kinoshita Y and Tomita S: Prostatic ischemia
induces ventral prostatic hyperplasia in the SHR; possible
mechanism of development of BPH. Sci Rep. 4(3822)2014.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Byun SS, Jeong H, Jo MK and Lee E:
Relative proportions of tissue components in the prostate: Are they
related to the development of symptomatic BPH in Korean men?
Urology. 66:593–596. 2005.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Lean FZ, Kontos S and Palmieri C:
Expression of β-catenin and mesenchymal markers in canine prostatic
hyperplasia and carcinoma. J Comp Pathol. 150:373–381.
2014.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Wu JH, Jiang XR, Liu GM, Liu XY, He GL and
Sun ZY: Oral exposure to low-dose bisphenol A aggravates
testosterone-induced benign hyperplasia prostate in rats. Toxicol
Ind Health. 27:810–819. 2011.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Shao R, Shi J, Liu H, Shi X, Du X, Klocker
H, Lee C, Zhu Y and Zhang J: Epithelial-to-mesenchymal transition
and estrogen receptor α mediated epithelial dedifferentiation mark
the development of benign prostatic hyperplasia. Prostate.
74:970–982. 2014.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Sanchez P, Torres JM, Vilchez P, Del Moral
RG and Ortega E: Effects of sulpiride on mRNA levels of steroid
5alpha-reductase isozymes in prostate of adult rats. Iubmb Life.
60:68–72. 2008.PubMed/NCBI View
Article : Google Scholar
|
|
43
|
Lee BH, Kang SG, Kim TW, Lee HJ, Yoon HK
and Park YM: Hyperprolactinemia induced by low-dosage amisulpride
in Korean psychiatric patients. Psychiatry Clin Neurosci. 66:69–73.
2012.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Martinot JL, Paillère-Martinot ML, Poirier
MF, Dao-Castellana MH, Loc'H C and Mazière B: In vivo
characteristics of dopamine D2 receptor occupancy by amisulpride in
schizophrenia. Psychopharmacology (Berl). 124:154–158.
1996.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Abe Y, Yonemura K, Nishida K and Takagi K:
Giant cell tumor of bone: Analysis of proliferative cells by
double-labeling immunohistochemistry with anti-proliferating cell
nuclear antigen antibody and culture procedure. Nihon Seikeigeka
Gakkai Zasshi. 68:407–414. 1994.PubMed/NCBI
|
|
46
|
Sun HB, Xia SJ and Tang XD: Expression of
different genes in transitional zone and peripheral zone of human
normal prostate. Zhonghua Yi Xue Za Zhi. 85:610–613. 2005.(In
Chinese). PubMed/NCBI
|
|
47
|
Liu YN, Abou-Kheir W, Yin JJ, Fang L,
Hynes P, Casey O, Hu D, Wan Y, Seng V, Sheppard-Tillman H, et al:
Critical and reciprocal regulation of KLF4 and SLUG in transforming
growth factor β-initiated prostate cancerepithelial-mesenchymal
transition. Mol Cell Biol. 32:941–953. 2012.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Shao R, Shi J, Liu H, Shi X, Du X, Klocker
H, Lee C, Zhu Y and Zhang J: Epithelial-to-mesenchymal transition
and estrogen receptor α mediated epithelial dedifferentiation mark
the development of benign prostatic hyperplasi. Prostate.
74:970–982. 2014.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Sánchez P, Torres JM, Castro B, Frias JF
and Ortega E: Effects of metoclopramide on mRNA levels of steroid
5α-reductase isozymes in prostate of adult rats. J Physiol Biochem.
69:133–140. 2013.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Kindblom J, Dillner K, Ling C, Törnell J
and Wennbo H: Progressive prostate hyperplasia in adult prolactin
transgenic mice is not dependent on elevated serum androgen levels.
Prostate. 53:24–33. 2002.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Wennbo H, Kindblom J, Isaksson OG and
Törnell J: Transgenic mice overexpressing the prolactin gene
develop dramatic enlargement of the prostate gland. Endocrinology.
138:4410–4415. 1997.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Rubin RT, Poland RE and Tower BB:
Prolactin-related testosterone secretion in normal adult men. J
Clin Endocrinol Metab. 42:112–116. 1976.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Rubin RT, Gouin PR, Lubin A, Poland RE and
Pirke KM: Nocturnal increase of plasma testosterone in men:
Relation to gonadotropins and prolactin. J Clin Endocrinol Metab.
40:1027–1033. 1975.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Shen YC, Kang CH and Chiang PH: Efficacy
of switching therapy of luteinizing hormone-releasing hormone
analogue for advanced prostate cancer. Kaohsiung J Med Sci.
32:567–571. 2016.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Miki K, Sasaki H, Kido M, Takahashi H,
Aoki M and Egawa S: A comparative study on the efficacies of
gonadotropin-releasing hormone (GnRH) agonist and GnRH antagonist
in neoadjuvant androgen deprivation therapy combined with
transperineal prostate brachytherapy for localized prostate cancer.
BMC Cancer. 16(708)2016.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Yamanaka H, Kosaku N, Makino T and Shida
K: Fundamental and clinical study of the anti-prostatic effect of
allylestrenol. Hinyokika Kiyo. 29:1133–1145. 1983.(In Japanese).
PubMed/NCBI
|
|
57
|
Liu RF, Fu G, Li J, Yang YF, Wang XG, Bai
PD and Chen YD: Roles of autophagy in androgen-induced benign
prostatic hyperplasia in castrated. rats. Exp Ther Med.
15:2703–2710. 2018.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Hammond GL, Kontturi M, Määttälä P, Puukka
M and Vihko R: Serum FSH, LH and prolactin in normal males and
patients with prostatic diseases. Clin Endocrinol (Oxf). 7:129–135.
1977.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Porcaro AB, Petrozziello A, Ghimenton C,
Migliorini F, Sava T, Caruso B, Cocco C, Romano M and Artibani W:
Along the pituitary-testis-prostate axis, serum total testosterone
is a significant preoperative variable independently contributing
to separating the prostate cancer population into prostatectomy
Gleason score groups. Anticancer Res. 32:5015–5022. 2012.PubMed/NCBI
|
|
60
|
Yuan ZF, Yang SC and Pan JT: Effects of
prolactin-releasing peptide on tuberoinfundibular dopaminergic
neuronal activity and prolactin secretion in estrogen-treated
female rats. J Biomed Sci. 9:112–118. 2002.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Calogero AE, Weber RF, Raiti F, Burrello
N, Moncada ML, Mongioi A and D'Agata R: Involvement of
corticotropin-releasing hormone and endogenous opioid peptides in
prolactin-suppressed gonadotropin-releasing hormone release in
vitro. Neuroendocrinology. 60:291–296. 1994.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Ogura T, Tanaka Y, Tamaki H and Harada M:
Docetaxel induces Bcl-2- and pro-apoptotic caspase-independent
death of human prostate cancer DU145 cells. Int J Oncol.
48:2330–2338. 2016.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Ellem SJ and Risbridger GP: The dual,
opposing roles of estrogen in the prostate. Ann N Y Acad Sci.
1155:174–186. 2009.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Weng YI, Hsu PY, Liyanarachchi S, Liu J,
Deatherage DE, Huang YW, Zuo T, Rodriguez B, Lin CH, Cheng AL and
Huang TH: Epigenetic influences of low-dose bisphenol A in primary
human breast epithelial cells. Toxicol Appl Pharmacol. 248:111–121.
2010.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Huang DY, Zheng CC, Pan Q, Wu SS, Su X, Li
L, Wu JH and Sun ZY: Oral exposure of low-dose bisphenol A promotes
proliferation of dorsolateral prostate and induces
epithelial-mesenchymal transition in aged rats. Sci Rep.
8(490)2018.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Banerjee PP, Banerjee S and Brown TR:
Increased androgen receptor expression correlates with development
of age-dependent, lobe-specific spontaneous hyperplasia of the
brown Norway rat prostate. Endocrinology. 142:4066–4075.
2001.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Prins GS: Prolactin influence on cytosol
and nuclear androgen receptors in the ventral, dorsal, and lateral
lobes of the rat prostate. Endocrinology. 120:1457–1464.
1987.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Holland JM and Lee C: Effects of pituitary
grafts on testosterone stimulated growth of rat prostate. Biol
Reprod. 22:351–355. 1980.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Da J, Lu M and Wang Z: Estrogen receptor
alpha (ERα)-associated fibroblasts promote cell growth in prostate
cancer. Cell Biochem Biophys. 73:793–798. 2015.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Corradi LS, Jesus MM, Fochi RA, Vilamaior
PS, Justulin LJ Jr, Góes RM, Felisbino SL and Taboga SR: Structural
and ultrastructural evidence for telocytes in prostate stroma. J
Cell Mol Med. 17:398–406. 2013.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Zhang S, Wu H and Liu C: Inhibition of
lymphocyte proliferation: An ability shared by murine mesenchymal
stem cells, dermal fibroblasts and chondrocytes. Transpl Immunol
Feb. 20:2018.(Epub ahead of print). PubMed/NCBI View Article : Google Scholar
|
|
72
|
Van de Voorde WM, Elgamal AA, Van Poppel
HP, Verbeken EK, Baert LV and Lauweryns JM: Morphologic and
immunohistochemical changes in prostate cancer after preoperative
hormonal therapy. A comparative study of radical prostatectomies.
Cancer-Am Cancer Soc. 74:3164–3175. 1994.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Grant CM and Kyprianou N: Epithelial
mesenchymal transition (EMT) in prostate growth and tumor
progression. Transl Androl Urol. 2:202–211. 2013.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Hetzl AC, Montico F, Kido LA and Cagnon
VH: Prolactin, EGFR, vimentin and α-actin profiles in elderly rat
prostate subjected to steroid hormonal imbalance. Tissue Cell.
48:189–196. 2016.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Lindsay CR, Le Moulec S, Billiot F, Loriot
Y, Ngo-Camus M, Vielh P, Fizazi K, Massard C and Farace F: Vimentin
and Ki67 expression in circulating tumour cells derived from
castrate-resistant prostate cancer. BMC Cancer.
16(168)2016.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Burch TC, Watson MT and Nyalwidhe JO:
Variable metastatic potentials correlate with differential plectin
and vimentin expression in syngeneic androgen independent prostate
cancer cells. PLoS One. 8(e65005)2013.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Haixuan Qiao, Qingming Wang and Huipeng
Chen: Changes in vimentin during apoptosis. Bull Acad Military Med
Sci. 275(277)2005.
|
|
78
|
Morishima N: Changes in nuclear morphology
during apoptosis correlate with vimentin cleavage by different
caspases located either upstream or downstream of Bcl-2 action.
Genes Cells. 4:401–414. 1999.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Wu D: Mechanism of apoptosis induced by
knockdown of fbronectin in mesangial cells. (unpublished PhD
thesis). General Hospital of PLA.
|