Introduction
Recurrent spontaneous abortion is a term used when
≥2 consecutive pregnancies and abortions occurred. The incidence
rate of women of childbearing age with recurrent spontaneous
abortion is 1-5% (1). The etiology
of recurrent spontaneous abortion is complex, and >50% is due to
embryonic chromosomal abnormalities (2). Villus tissue has the same genetic
characteristics as embryonic cells, and the detection of villus
tissue allows for genetic diagnosis of the cause of early abortion
(3). There are many methods for
chromosome detection (4). G-band
karyotype analysis is a commonly used detection method; although it
requires a large amount of sample, high detection failure rate, and
is unrestricted for structural anomalies <5 mb (5). Fluorescence in situ
hybridization (FISH) is another commonly used method for chromosome
detection (6). FISH is mainly used
to detect the presence or absence of aneuploidy abnormalities in
the seven chromosomes 13, 16, 18, 21, 22, X and Y, but cannot
analyze the entire genome (6).
Furthermore, it is impossible to detect structural abnormalities of
chromosomes and FISH cannot be used in clinical settings.
High-throughput sequencing technology is a detection method
(7) that covers 46 chromosome
aneuploidy and copy number variation >100 kb. It has high
detection resolution and is fast, accurate, flexible and
comprehensive (8). For patients with
recurrent spontaneous abortion, the psychological burden may be
heavy and mentally stressful (9).
Patients are concerned about the cause of the disease and have high
expectations for clinical test results (10). Therefore, obtaining more accurate
information on chromosomal abnormalities is crucial (11).
Pregnancy is a unique physiological process. During
embryonic development, immune rejection caused by semi-allogeneic
antigens is inhibited in the mother (12). The immune balance between T helper 1
(Th1) and Th2 cells was thought to play a key role in embryo
implantation (13). The Th17 and
regulatory T (Treg) balance has become increasingly important in
reproductive immunity research (14). Th17 cells that mediate immune
rejection and Treg cells that mediate immune tolerance maintain a
dynamic balance to maintain the normal immune status of the body
(15). The Th17 and Treg cell
imbalance may be an important immune factor in pregnancy failure
(16). During embryo implantation,
the endometrium serves as the primary and earliest tissue
constituting the maternal-fetal interface microenvironment, and the
recruitment of Treg cells plays an important role in local immunity
(17). Unexplained recurrent
spontaneous abortion may be associated with insufficient
recruitment of Treg cells in endometrial tissue (18). Changes in peripheral blood immune
cells reflect the immune status of the whole body and the decidual
tissue reflects the local immune status of the maternal-fetal
interface microenvironment (17).
Therefore, simultaneous detection of Th17 and Treg cells in
peripheral blood and decidual tissue may help to understand the
immunological pathogenesis of recurrent spontaneous abortion.
Human chorionic gonadotropin hormone (HCG) has been
used as a basic drug for the treatment of miscarriage (19). Although the therapeutic mechanism is
not fully understood, HCG plays an active role in the prevention
and treatment of recurrent abortion (20). Human immunoglobulin (IG) has also
been widely used in the treatment of recurrent abortion especially
for unexplained and poor outcome therapeutic cases with good
results (21). Previous studies have
shown that both HCG and IG can function by modulating immune
mechanisms (22-24). Treg cells have
HCG receptors on their surface and HCG is involved in the
recruitment of Treg cells (25). IG
increases the level of Treg cells in memory T cells via IgG
antibodies, and inhibits the differentiation and expansion of Th17
cells and the production of cytokines by Th17 cells (26). The present study hypothesized that a
combinatorial therapy of HCG and IG may improve the Th17 and Treg
imbalance.
The cause of recurrent abortion is complex and
involves many factors (27).
Identifying the exact cause is often challenging, and there are no
corresponding theoretical basis and effective measures for
treatment (12). The present study
hypothesized that embryo chromosomal abnormalities may be the
primary reason for recurrent spontaneous abortion. Other
unexplained recurrent abortions may be associated with immune
dysfunction at the maternal-fetal interface such as a Treg and Th17
cell imbalance. This immune imbalance may be improved by drug
therapy such as IG + HCG, thereby increasing clinical pregnancy
rates. However, the effectiveness of this treatment requires
further investigation.
In the present study, a high-throughput gene
sequencing method was used to analyze the villus chromosomes in
patients with recurrent spontaneous abortion in order to identify
possible genetic causes. In addition, the immune status and
correlation of Th17 and Treg cells in peripheral blood and decidual
tissue were analyzed. For patients with normal chorionic villus, IG
combined with HCG treatment was used, and the changes of peripheral
blood Th17 and Treg cells in patients with successful pregnancy
were re-evaluated. The present results may provide a novel
theoretical basis for the clinical diagnosis and treatment of
recurrent spontaneous abortion.
Patients and methods
Patients
A total of 56 patients with recurrent spontaneous
abortion (number of abortions, ≥2) were recruited in The Weihai
Central Hospital from January 2015 to December 2017. The ages of
patients ranged from 25 to 35 years, with a mean age of 29.2±3.6
years. The mean gestational period of patients during abortion was
62.2±9.5 days. Among them, 54 patients were enrolled and two
patients were excluded due to sample contamination. Inclusion
criteria were as followed: i) Number of abortions ≥2; ii)
pre-abortion ultrasound confirmed that the embryos stopped
developing; and iii) villus and decidua tissues were obtained
during the abortions. Exclusion criteria included patients who had
an abortion due to genital malformations, endocrine disease,
infections, thrombotic disease, male factors or autoimmune
diseases.
In addition, 42 patients who underwent abortion
during early pregnancy were selected as the control group. Of the
42 cases, ten cases with chromosomal abnormalities were excluded
and 32 cases were selected in the control group. Inclusion criteria
were as followed: i) Patients with fetal heartbeat in the color
ultrasound one week before the abortion; ii) patients without
spontaneous abortion; iii) patients without stillbirth; and iv)
patients without premature birth history. Exclusion criteria were
as follows: i) Contamination of the villus and decidua in the
abortion; and ii) failure to obtain specimens for testing. Written
informed consent was obtained from every patient, and the study was
approved by The Ethics Review Board of The Weihai Central
Hospital.
Sample collection and high-throughput
gene sequencing
After curettage, the villi tissues and decidual
tissues were aseptically collected and rinsed with normal saline.
For decidual tissues, blood clots and villus tissue were removed
aseptically and placed in physiological saline. The aponeurosis
membrane was repeatedly rinsed with PBS solution, cut to ~0.5
cm3 and sieved through a 300 mesh aperture to prepare a
suspension. Peripheral venous blood was also collected. The blood
sample and the decidual tissue suspension were separately diluted
and mixed with the PBS buffer. The mixture was placed on the
lymphocyte separation solution and centrifuged at 4˚C at 3,000 x g
for 30 min. The intermediate layer of lymphocytes was pipetted,
washed once with RPMI-1640 (BD Biosciences) and resuspended in
RPMI-1640 containing 10% calf serum (BD Biosciences) The cells were
counted under a light microscope (magnification, x400) and the cell
concentration was 1x106.
The villi tissues of patients with recurrent
spontaneous abortion were sent to Hunan Jiahui Genetics Hospital
for high-throughput gene sequencing. The high-throughput sequencing
results were matched to the chromosome on which each sequencing
sequence was read by Bowtie2 v2.1.0 alignment software (http://bowtie-bio.sourceforge.net/bowtie2/index.shtml).
Subsequent normalized Z-value analysis was performed to determine
the chromosomal abnormality. The clinical significance of the
measured copy number variation was obtained by searching the
DECIPHER database v9.28 (https://decipher.sanger.ac.uk/syndromes) and the
Genomic Variants database (http://dgv.tcag.ca/dgv/app/home).
Karyotype analysis
For control patients who underwent an abortion
during early pregnancy, G-band karyotype analysis of villus tissues
was performed as previously described (28). Villi were obtained aseptically and
cultured at room temperature for 5-15 days. The cells were
harvested by digestion. Following staining with Giemsa, cells were
subjected to G-band karyotype analysis.
Flow cytometry
Lymphocytes were isolated from peripheral blood and
decidual tissues from 30 patients without chromosome abnormalities
by Ficoll-Hypaque (1.077 g/ml; Sigma-Aldrich; Merck KGaA) and
gradient centrifugation (2,000 x g for 20 min at 20˚C). The cell
concentration was 2x106 with RPMI-1640 medium (Becton,
Dickinson and Company) containing 10% calf serum (Becton, Dickinson
and Company). In total, 100 µl of the cell suspension was used for
Treg cell detection. A total of 1x106 cells/well from
the cell suspension were then seeded to a 24-well plate and
incubated at 37˚C with 300 µg/ml phorbol ester and 1 µg/ml
ionomycin for 5 h. Then 0.4 µg/ml Monessen (Enzo Life Sciences,
Inc.) was added for another 1 h at 37˚C.
To detect Th17 cells, the stimulated cells were
collected and stained with the FITC-labeled CD4 antibody (1:500;
cat. no. 300532; BD Biosciences) at room temperature for 30 min.
Fixation and permeabilization was performed with a
fixation/permeabilization buffer (Cytofix/Cytoperm™;
cat. no. 554722; BD Biosciences) at room temperature in the dark
for 20 min. Then, the cells were stained with phycoerythrin
(PE)-labeled interleukin-17 monoclonal antibody (1:500; cat. no.
512306; BD Biosciecnes) for 20 min in the dark at room temperature.
The corresponding isotype IgG was also incubated at room
temperature for 20 min in the dark. The lymphocyte population was
gated, and the cells incubated with the corresponding isotype IgG
at room temperature for 20 min in the dark was used as negative
controls for the fluorescent (FL) 1 and FL2 channels. The
proportions of Th17 cells in peripheral blood and decidual tissue
CD4+ T cells were analyzed on FACSCalibur (BD
Biosciences) using CellQuest Pro 5.1 software (BD Biosciences).
Treg cells are positive for CD4, CD25 and forkhead
box P3 (Foxp3) (29). Single-cell
suspension was incubated with anti-FITC-labeled CD4 monoclonal
antibody (cat. no. 317408; clone OKT4; BD Biosciences) and
anti-PE-labeled CD25 monoclonal antibody (cat. no. 302618; clone
BC96; BD Biosciences) at room temperature for 20 min in the dark,
respectively. Fixation and permeabilization was performed with a
fixation/permeabilization buffer (Cytofix/Cytoperm™;
cat. no. 554722; BD Biosciences) at room temperature in the dark
for 20 min. Then, cells were stained with
anti-allophycocyanin-labeled Foxp3 antibody (cat. no. 320108; clone
206D; BDBiosciences) at room temperature for 15 min in the dark.
Antibodies were purchased from BD (USA). The
CD4+CD25+ and Foxp3+ cells were
gated and analyzed using flow cytometry (FACSCalibur; BD
Biosciences) using CellQuest Pro 5.1 software (BD Biosciences).
IG and HCG treatment
Among the 54 patients, 30 cases without chromosomal
abnormalities were treated with IG and HCG immediately after
confirmation of pregnancy (average gestational age 5-6 weeks).
Intramuscular injection of 0.3 g IG was repeated every 3 weeks up
until 12 weeks of gestation. Intramuscular injection of 5,000 IU
HCG was repeated twice a week up until 12 weeks of gestation. Then,
ultrasound examination was performed. If the embryo was developing
normally, 20 ml of peripheral blood was taken for examination. In
total, 18 patients were with successful pregnancy after IG and HCG
treatment.
Statistical analysis
SPSS 19.0 software (IBM Corp.) was used for data
analysis. Distribution of the data was analyzed with
Kolmogorov-Smirnov test. Quantitative data in accordance with
normal distribution are presented as mean ± SD. A Student's t-test
was used for comparison between groups and a paired t-test was used
for comparison within the same groups. Comparisons between groups
were performed using χ2 test. Correlation of the two
variables was analyzed using Pearson correlation test. P<0.05
was considered to indicate a statistically significant
difference.
Results
Analysis of villus chromosome
abnormalities and polymorphisms
To identify possible chromosome abnormalities,
high-throughput gene sequencing was performed in patients with
recurrent spontaneous abortion. All 54 patients were tested using
villus chromosome analysis. Among them, 30 cases had villous
chromosomes without abnormalities, of which 17 were 46XX and 13
were 46XY. In total, 24 cases had villus chromosomal abnormalities
and the abnormal rate was 46.2% (Table
I). In the present study, ~50% of the recurrent spontaneous
abortions were related to embryonic chromosomal abnormalities.
Among them, there were 19 cases with abnormal chromosome numbers
accounting for 79.2% of the abnormal proportion, including
three-body type, triploid, haploid and chimera. Among them, there
were 13 cases of autosomal trisomy and six cases of sex chromosome
abnormality (X, Y chromosome monomer, triploid and chimera). There
were five cases of abnormal chromosome structure, accounting for
20.8%. The chromosomes had 250-400 kb microrepeats and
microdeletions, and the chromosomal regions of the repeat and
deletion were identified. The present results indicated that
high-throughput sequencing for villus chromosome analysis may
provide more accurate genetic information for recurrent spontaneous
abortion.
 | Table IAnalysis of villus chromosome
abnormality. |
Table I
Analysis of villus chromosome
abnormality.
| Chromosome
abnormality | Cases |
|---|
| 47, XN, +16 | 2 |
| 47, XN, +21 | 2 |
| 47, XN, +10 | 2 |
| 47, XN, +13 | 1 |
| 47, XN, +18 | 1 |
| 47, XN, +22 | 1 |
| 47, XN, +12 | 1 |
| 47, XN, +4 | 1 |
| 45, XN, -21 | 1 |
| 69, XNN | 2 |
| 47, XN, +6 | 1 |
| 45, X [10%]/46,
XN | 1 |
| 45, X [30%]/46,
XN[70%] | 1 |
| 47, XN+15[85%]/46,
XN[15%] | 1 |
| 47, XN+18[70%]/46,
XN[30%] | 1 |
| 46, XY 10q11.22
segment 300 kb repeat | 1 |
| 46, XY
8p23.2-8p23.3 segment 350 kb repeat, | |
| 18p11.23 segment
250 kb repeat | 1 |
| 46, XX 7q31.1
segment 250 kb deletion | 1 |
| 46, XX 20p12.1
segment 400 kb deletion | 1 |
| 46, XY
4p16.1-4p16.3 segment 8.7 mb deletion | |
| 4q34.1-35.2 segment
15.2 mb repeat | 1 |
Expression analysis of Treg cells,
Th17 cells and the Th17 and Treg ratios in the two groups
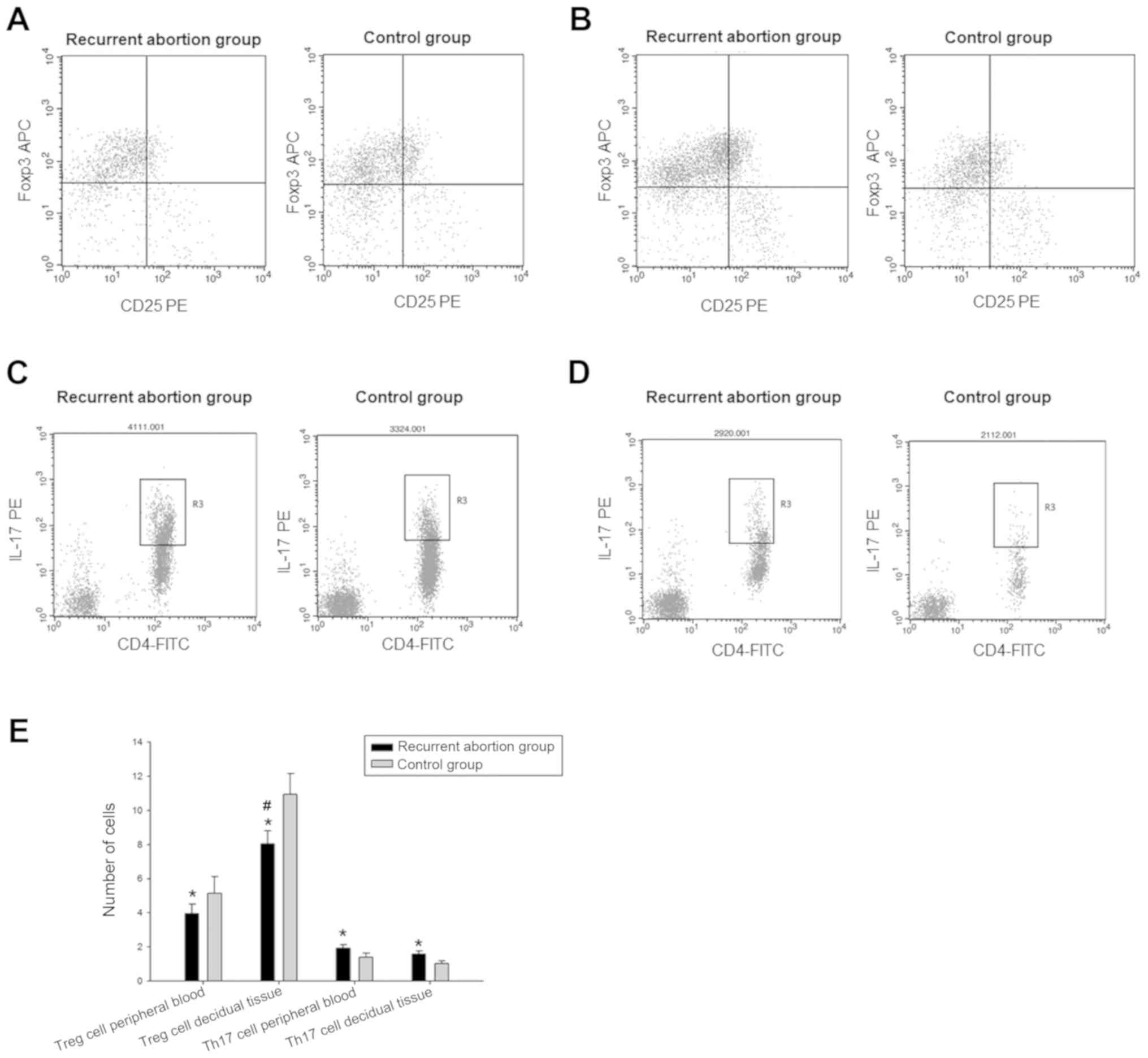
Flow cytometry was performed to detect the
percentage of Treg cells and Th17 cells in peripheral blood and
decidual tissues. The present representative flow cytometry results
were shown in Fig. 1A-D. Compared
with the control group, the expression level of Treg cells in the
recurrent abortion group was decreased and the expression level of
Th17 cells was increased (Fig. 1E).
In the recurrent abortion group, the expression level of Treg cells
in the decidual tissue (8.04±0.76) was significantly increased
compared with the peripheral blood (3.95±0.56; P<0.001)
(Fig. 1E). The Th17 and Treg cell
balance was biased toward Th17 cells. The present results suggested
that Th17 and Treg cells were abnormally expressed in patients with
recurrent spontaneous abortion and the immune balance was biased
toward Th17 cells.
Negative correlation between the
expression levels of Th17 cells and Treg cells in the two
groups
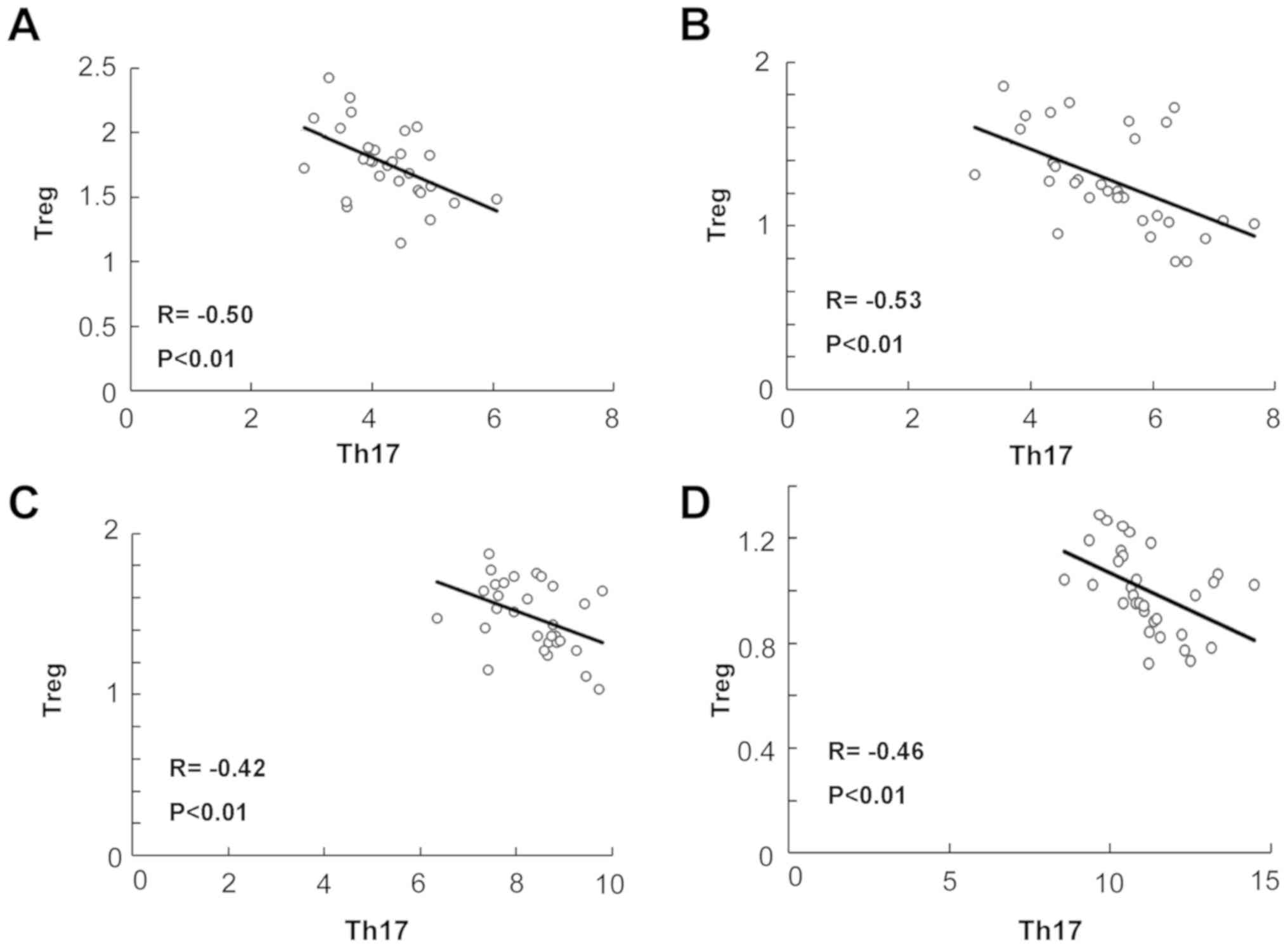
The correlation between Th17 cells and Treg cells in
the recurrent abortion group and the control group were analyzed.
Th17 cells were moderately negatively correlated with Treg cells in
peripheral blood (R=-0.50; P<0.01) and decidual tissue (R=-0.53;
P<0.01) in the recurrent abortion group (Fig. 2). Th17 cells were moderately
negatively correlated with Treg cells in peripheral blood (R=-0.42;
P<0.01) and decidual tissue (R=-0.46; P<0.01) in the control
group. There was a stronger correlation in decidua tissue compared
with peripheral blood (P<0.001). The present results suggested
that the expression levels of Th17 and Treg cells were negatively
correlated in patients with recurrent spontaneous abortion and were
higher in decidual tissue.
Expression of Treg cells and Th17
cells in peripheral blood of patients with successful pregnancy in
the recurrent abortion group
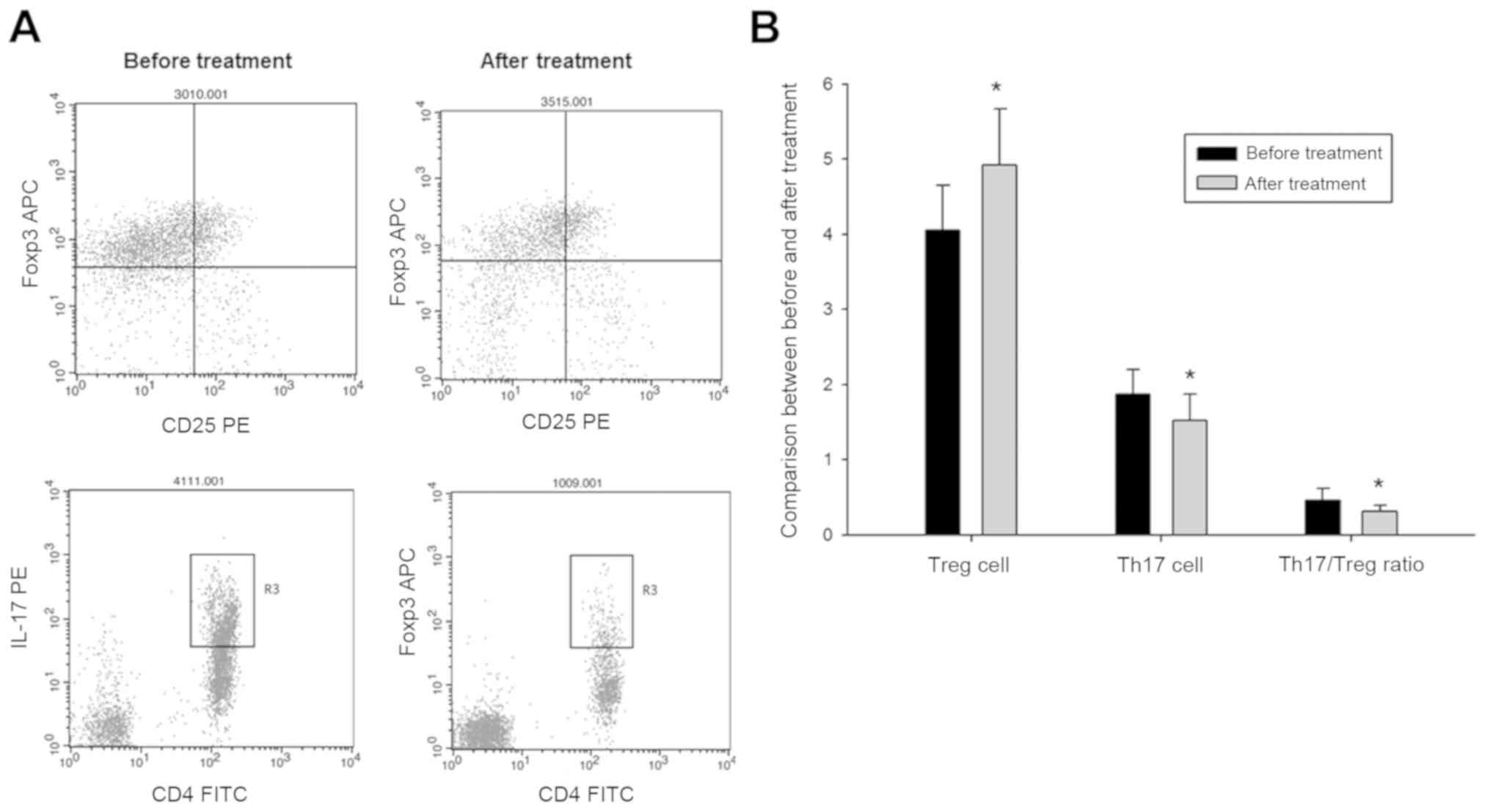
Expression levels of Treg and Th17 cells in
peripheral blood before and after treatment were analyzed. After IG
and HCG treatment, 18 cases had a successful pregnancy and the
pregnancy success rate was 60%. The proportion of Th17 cells and
the ratio of Th17 and Treg cells in patients after treatment
decreased, and the proportion of Treg cells increased compared with
levels in patients before treatment (Fig. 3; P<0.01). The present results
indicated that IG and HCG therapy may increase successful pregnancy
rates by reversing the Th17 and Treg cell imbalance.
Discussion
Recurrent abortion has a complicated etiology and is
a major problem in the medical field (30). Embryonic chromosomal abnormalities
are the most common causes; however, 50% of causes are still
unknown (31). High-throughput
sequencing is a new method for analyzing genomic abnormalities with
a high detection rate (32). In the
present study, the number of patients with recurrent spontaneous
abortions was 54. All patients were tested for villus chromosome
analysis. The detection rate of high-throughput gene sequencing
method was 100%. The chromosomes of 30 patients were without
abnormalities and those of 24 patients were abnormal. The abnormal
chromosomes consisted of trisomy, triploid, haploid and chimera,
and the chromosomal regions with abnormal chromosomal structural
repeats and deletions were identified. All of these chromosome
abnormalities could lead to abortions (33). The abnormal chromosomal structural
repeats and deletions could not be detected using traditional
karyotype analysis. Thus, high-throughput gene sequencing could
provide accurate genetic analysis of abortion and more accurate
clinical recommendations and genetic guidance for fertility.
Pregnancy is a unique physiological process. The
body exhibits rational immune tolerance to the embryo (34). In recent years, the theory of
maintaining immune balance of Th17 and Treg cells has become
important in reproductive immunity research (35). Th17 and Treg cells maintain a dynamic
balance to regulate the immune status of the body (14,19). The
present study used chromosomal analysis to exclude patients with
recurrent abortions caused by genetic factors. Patients with
genital malformations, endocrine diseases, infections or other
factors that had been confirmed to cause abortion were also
excluded. The enrolled patients who had unexplained abortions may
be caused by immune factors. The present results identified that
the proportion of Treg cells in peripheral blood decreased, while
the proportion of Th17 cells increased. Therefore, the Th17 and
Treg balance favored Th17 cells. The present results in the
decidual tissue were consistent with those in peripheral blood.
Therefore, unexplained recurrent spontaneous abortion may be
associated with abnormal Th17 and Treg immune function in the
microenvironment of the maternal-fetal interface. Previous studies
on the regulation of the differentiation of Th17 and Treg cells
found that the original T cells can differentiate into Th17 and
Treg transition-type cells, and the subsequent differentiation
depends on the surrounding cytokines and their concentrations
(36,37). Therefore, the present study performed
a correlation analysis between Th17 and Treg cells. The present
results indicated there was a moderate negative correlation in both
the peripheral blood and decidual tissue, which suggested that Th17
and Treg cell differentiation and regulation processes were closely
related, mutually restrictive and functionally antagonistic.
Drug therapy for recurrent abortion is continuously
being investigated and improved (38). At present, there are many therapeutic
drugs for recurrent spontaneous abortion (39). Among them, the application of IG and
HCG has achieved good clinical results (38,40). The
present study selected a combination of IG and HCG based on
previous clinical experience. The dosage and usage are as stated in
the paper, and the time of administration was 12 weeks of gestation
as recurrent spontaneous abortion occurred >12 weeks prior and
stabilized after 12 weeks. The main mechanism of recurrent
spontaneous abortion is not fully understood. The present study
hypothesized that the mechanism may be related to the regulation of
the immune imbalance status of Th17 and Treg cells. The present
study compared the pregnancy rate before and after drug treatment
and the changes in peripheral blood levels of Th17 and Treg cells.
The clinical pregnancy rate after treatment was 60%. The proportion
of Treg cells increased and the ratio of Th17 and Treg decreased,
suggesting the Th17 and Treg balance was favored towards Treg
cells. The present results suggested that IG and HCG could reverse
the Th17 and Treg imbalance to achieve a successful pregnancy
outcome.
The present study had some limitations. First, the
sample size was relatively small, thus future studies with larger
sample sizes are required. Second, the combination of IG and HCG
may have an impact on other clinical and laboratory indicators,
especially immunological indicators, but these were not tracked in
the present study. The impact of the drugs on other indicators
should be a focus of future research.
In conclusion, the analysis of the villus
chromosomes using high-throughput gene sequencing may provide more
accurate and comprehensive information for the diagnosis of
recurrent spontaneous abortion. Along with embryonic chromosomal
factors, the Th17 and Treg cell balance plays an important role in
maternal-fetal immune tolerance. The present results suggested HCG
and IG therapy could increase the rate of successful pregnancy by
reversing the imbalance between Th17 and Treg cells. The present
results may provide novel insights for the diagnosis and treatment
of recurrent spontaneous abortion.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZG and XL conceptualized the study. ZG, YX and QZ
performed the data acquisition. YL performed the statistical
analysis. ZG drafted the original manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from each
patient and the study was approved by The Ethics Review Board of
The Weihai Central Hospital.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Practice Committee of the American Society
for Reproductive Medicine: Evaluation and treatment of recurrent
pregnancy loss: A committee opinion. Fertil Steril 98: 1103-1111,
2012.
|
|
2
|
Yuan SM, Liao C, Li DZ, Huang JZ, Hu SY,
Ke M, Zhong HZ and Yi CX: Chorionic villus cell culture and
karyotype analysis in 1 983 cases of spontaneous miscarriage.
Zhonghua Fu Chan Ke Za Zhi. 52:461–466. 2017.(In Chinese).
PubMed/NCBI View Article : Google Scholar
|
|
3
|
Qi H, Cai LR, Zhu JJ, Yang K, Wen XH, Zeng
W and Chen JL: Application of copy number variation analysis based
on next-generation sequencing in the genetic analysis of missed
abortion chorionic villi. Zhonghua Fu Chan Ke Za Zhi. 51:92–96.
2016.(In Chinese). PubMed/NCBI View Article : Google Scholar
|
|
4
|
McQueen DB and Lathi RB: Miscarriage
chromosome testing: Indications, benefits and methodologies. Semin
Perinatol. 43:101–104. 2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Donaghue C, Mann K, Docherty Z, Mazzaschi
R, Fear C and Ogilvie C: Combined QF-PCR and MLPA molecular
analysis of miscarriage products: An efficient and robust
alternative to karyotype analysis. Prenat Diagn. 30:133–137.
2010.PubMed/NCBI View
Article : Google Scholar
|
|
6
|
Haoud K, Mellali S, Gouas L, Tchirkov A,
Vago P and Moulessehoul S: Prevalence of aneuploidies in products
of spontaneous abortion: Interest of FISH and MLPA. Morphologie.
98:40–46. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Soler A, Morales C, Mademont-Soler I,
Margarit E, Borrell A, Borobio V, Muñoz M and Sánchez A: Overview
of chromosome abnormalities in first trimester miscarriages: A
series of 1,011 consecutive chorionic villi sample karyotypes.
Cytogenet Genome Res. 152:81–89. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Duan J, Zhang JG, Deng HW and Wang YP:
Comparative studies of copy number variation detection methods for
next-generation sequencing technologies. PLoS One.
8(59128)2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lin PX, Qu YX, Hua SW, Wu HY, Gui YE, Tang
Y and Li YW: Analysis on psychological status of patients with
recurrent spontaneous abortion. Zhong Guo Fu You Bao Jian.
33:2764–2767. 2018.(In Chinese).
|
|
10
|
Qiao J: Preconception management of
recurrent abortion. Zhong Guo Shi Yong Fu Ke Yu Chan Ke Za Zhi.
34:1309–1313. 2016.(In Chinese).
|
|
11
|
Kaser D: The status of genetic screening
in recurrent pregnancy loss. Obstet Gynecol Clin North Am.
45:143–154. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Shima T, Sasaki Y, Itoh M, Nakashima A,
Ishii N, Sugamura K and Saito S: Regulatory T cells are necessary
for implantation and maintenance of early pregnancy but not late
pregnancy in allogeneic mice. J Reprod Immunol. 85:121–129.
2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Liang PY, Yin B, Cai J, Hu XD, Song C, Wu
TH, Zhao J, Li GG and Zeng Y: Increased circulating Th1/Th2 ratios
but not other lymphocyte subsets during controlled ovarian
stimulation are linked to subsequent implantation failure after
transfer of in vitro fertilized embryos. Am J Reprod Immunol.
73:12–21. 2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Zhu L, Chen H, Liu M, Yuan Y, Wang Z, Chen
Y, Wei J, Su F and Zhang J: Treg/Th17 Cell imbalance and IL-6
profile in patients with unexplained recurrent spontaneous
abortion. Reprod Sci. 24:882–890. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Jin LP, Fan DX, Zhang T, Guo PF and Li DJ:
The costimulatory signal upregulation is associated with Th1 bias
at the maternal-fetal interface in human miscarriage. Am J Reprod
Immunol. 66:270–278. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Li W, Geng L, Liu X, Gui W and Qi H:
Recombinant adiponectin alleviates abortion in mice by regulating
Th17/Treg imbalance via p38MAPK-STAT5 pathway. Biol Reprod.
100:1008–1017. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Qian J, Zhang N, Lin J, Wang C, Pan X,
Chen L, Li D and Wang L: Distinct pattern of Th17/Treg cells in
pregnant women with a history of unexplained recurrent spontaneous
abortion. Biosci Trends. 12:157–167. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Wang WJ, Zhang H, Chen ZQ, Zhang W, Liu
XM, Fang JY, Liu FJ and Kwak-Kim J: Endometrial TGF-β, IL-10, IL-17
and autophagy are dysregulated in women with recurrent implantation
failure with chronic endometritis. Reprod Biol Endocrinol.
17(2)2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wang H, Liu FM, Liu XY and Zhu XW: The
effect of hCG bind immunoglobin G on maternal-fetal interface's
Th1/Th2 type cytokines and pregnancy's out-come of abortion model.
Chin J Birth Health Heredity. 21:53–55. 2013.(In Chinese).
|
|
20
|
Schumacher A: Human chorionic gonadotropin
as a pivotal endocrine immune regulator initiating and preserving
fetal tolerance. Int J Mol Sci. 18(pii: E2166)2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Sha J, Liu F, Zhai J, Liu X, Zhang Q and
Zhang B: Alteration of Th17 and Foxp3+ regulatory T
cells in patients with unexplained recurrent spontaneous abortion
before and after the therapy of hCG combined with immunoglobulin.
Exp Ther Med. 14:1114–1118. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ahmadi M, Aghdam SA, Nouri M, Babaloo Z,
Farzadi L, Ghasemzadeh A, Hamdi K, Movassaghpour AA, Jadidi-Niaragh
F, Afkham A, et al: Intravenous immunoglobulin (IVIG) treatment
modulates peripheral blood Th17 and regulatory T cells in recurrent
miscarriage patients: Non randomized, open-label clinical trial.
Immunol Lett. 192:12–19. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kim DJ, Lee SK, Kim JY, Na BJ, Hur SE, Lee
M and Kwak-Kim J: Intravenous immunoglobulin G modulates peripheral
blood Th17 and Foxp3(+) regulatory T cells in pregnant women with
recurrent pregnancy loss. Am J Reprod Immunol. 71:441–450.
2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Muyayalo KP, Li ZH, Mor G and Liao AH:
Modulatory effect of intravenous immunoglobulin on Th17/Treg cell
balance in women with unexplained recurrent spontaneous abortion.
Am J Reprod Immunol. 80(e13018)2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Schumacher A, Brachwitz N, Sohr S,
Engeland K, Langwisch S, Dolaptchieva M, Alexander T, Taran A,
Malfertheiner SF, Costa SD, et al: Human chorionic gonadotropin
attracts regulatory T cells into the fetal-maternal interface
during early human pregnancy. J Immunol. 182:5488–5497.
2009.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Maddur MS, Vani J, Hegde P,
Lacroix-Desmazes S, Kaveri SV and Bayry J: Inhibition of
differentiation, amplification, and function of human TH17 cells by
intravenous immunoglobulin. J Allergy Clin Immunol.
127:823–830.e1-e7. 2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Obstetrics Subgroup, Chinese Society of
Obstetrics and Gynecology, Chinese Medical Association. Chinese
expert consensus on the diagnosis and tretment of recurrent
spontaneous abortion. Zhonghua Fu Chan Ke Za Zhi 51: 3-9, 2016 (In
Chinese).
|
|
28
|
Sun W, Wang JC and Su JR: Improved
karyotype preparation of early spontaneous abortion chorionic villi
and its clinical applications. Mod Lab Med. 27:98–103. 2012.
|
|
29
|
Cao W, Xu W, Chen T, Wang X, Wang X, Qiu
J, Chen N and Mao Y:
CD4+CD25+FoxP3+ regulatory T cells
and cytokines interact with estradiol in cases of missed abortion.
Exp Ther Med. 7:417–422. 2014.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Li J: Interpretation of the ‘Expert
Consensus on the Diagnosis and Treatment of Recurrent Abortion’ in
China in 2016 and the European ‘Guidelines for the diagnosis and
treatment of recurrent abortion’ in 2017. Shi Yong Fu Chan Ke Za
Zhi. 34:822–825. 2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Du Y, Chen L, Lin J, Zhu J, Zhang N, Qiu
X, Li D and Wang L: Chromosomal karyotype in chorionic villi of
recurrent spontaneous abortion patients. Biosci Trends. 12:32–39.
2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Jiang F, Ren J, Chen F, Zhou Y, Xie J, Dan
S, Su Y, Xie J, Yin B, Su W, et al: Noninvasive Fetal Trisomy
(NIFTY) test: An advanced noninvasive prenatal diagnosis
methodology for fetal autosomal and sex chromosomal aneuploidies.
BMC Med Genomics. 5(57)2012.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Luo XJ, Guo YY, Zhu ZR and Wei FX:
Prenatal diagnosis of chorionic villi chromosome structural
abnormalities at the first trimester of pregnancy. Shi Yong Yi Xue
Za Zhi. 31:4084–4087. 2015.
|
|
34
|
Poole JA and Claman HN: Immunology of
pregnancy. Implications for the mother. Clin Rev Allergy Immunol.
26:161–170. 2004.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Lee SK, Kim JY, Lee M, Gilman-Sachs A and
Kwak-Kim J: Th17 and regulatory T cells in women with recurrent
pregnancy loss. Am J Reprod Immunol. 67:311–318. 2012.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Jones LL, Alli R, Li B and Geiger TL:
Differential T cell cytokine receptivity and not signal quality
distinguishes IL-6 and IL-10 signaling during Th17 differentiation.
J Immunol. 196:2973–2985. 2016.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Gagliani N, Amezcua Vesely MC, Iseppon A,
Brockmann L, Xu H, Palm NW, de Zoete MR, Licona-Limón P, Paiva RS,
Ching T, et al: Th17 cells transdifferentiate into regulatory T
cells during resolution of inflammation. Nature. 523:221–225.
2015.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Theofanakis C, Drakakis P, Besharat A and
Loutradis D: Human chorionic gonadotropin: The pregnancy hormone
and more. Int J Mol Sci. 18(pii: E1059)2017.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Ling Y, Huang Y, Chen C, Mao J and Zhang
H: Low dose Cyclosporin A treatment increases live birth rate of
unexplained recurrent abortion-initial cohort study. Clin Exp
Obstet Gynecol. 44:230–235. 2017.PubMed/NCBI
|
|
40
|
Ahmadi M, Abdolmohammadi-Vahid S, Ghaebi
M, Aghebati-Maleki L, Dolati S, Farzadi L, Ghasemzadeh A, Hamdi K,
Younesi V, Nouri M and Yousefi M: Regulatory T cells improve
pregnancy rate in RIF patients after additional IVIG treatment.
Syst Biol Reprod Med. 63:350–359. 2017.PubMed/NCBI View Article : Google Scholar
|