Introduction
In 2017, the Tear Film and Ocular Surface Society
International Dry Eye Workshop II revised the definition of dry eye
disease (DED) and pointed out that its major pathology includes
tear film instability, hyperosmolarity, ocular surface
inflammation, damage and neurosensory abnormalities (1). Multiple risk factors for the
development of dry eye have been repeatedly identified, including
increasing age and female sex (particularly post-menopausal
females) (2,3) long-term contact lens wear, (4) months after laser-assisted in
situ keratomileusis (LASIK), (5)
prolonged use of video display screens, (6,7) and
exposure to dry environments (8).
Due to the decrease of tear film stability and the high osmolarity
of tears, patients may complain of burning, pricking, foreign
bodies, tearing, eye fatigue and dryness (9,10).
DED has been one of the most common and prevalent
eye disorders for which ophthalmological intervention is sought
(11). Several studies have revealed
that the prevalence of DED ranges from 2 to 50% in different
regions of the world, with a higher incidence among older adults
and females, particularly menopausal and post-menopausal females
(4,12-14).
With the excessive use of video display terminals (VDT), the number
of patients with DED has consistently increased in recent years
(15,16). As the population ages and the use of
VDTs increases, the direct and indirect cost of managing DED exerts
enormous pressure on the health care system (17). It has been reported that the annual
economic burden of DED in the US is 55.4 billion dollars (18).
Belmonte and Gallar (19) reported that weakening of nerve
stimulation function and a decrease in tear secretion produced
corneal surface dryness. Decreased tear secretion, coupled with
loss of epithelial cell viability, leads to a decrease in ocular
surface neurotrophins. Nerve growth factor, a vital component of
neurotrophins, is essential for the development and survival of
sympathetic neurons. It also has a significant role in nutritional
support after nerve injury (20).
Tear evaporation has a crucial role in the pathogenesis of DED. It
decreases the corneal temperature and repeatedly stimulates the
cold-sensitive corneal nerves. Continuous long-term stimulation
changes the function of thermal sensors to nociceptors (pain
sensors) (21).
Acupuncture is widely known as one of the common
forms of complementary and alternative medicine. A large number of
randomized controlled trials (RCTs) and systematic reviews have
indicated that acupuncture is effective in the treatment of various
conditions, including vomiting, dental pain, chronic pain, lower
back pain and eye disease (22-25).
In addition, several systematic reviews have confirmed that
acupuncture is effective for DED (26-28).
Lee et al (26) reported that
the effect of acupuncture on dry eye was better than that of
artificial tears (AT) as indicated by the results of Schirmer's I
test (SIT), tear break up time (BUT) test, response rate and
corneal fluorescein staining (CFS). The study by Kim et al
(27) is principally based on the
analysis of results of SIT, BUT and Ocular Surface Disease Index
(OSDI) (28), and confirmed that
acupuncture was more effective than AT in the treatment of dry eye.
Subgroup analysis was also performed to further prove the efficacy
of acupuncture. Yang et al (29) indicated the effectiveness of
acupuncture in the treatment of dry eye by comparing the results of
SIT and the BUT prior to and after treatment. Acupuncture has been
proven to promote the secretion of tears, relieve discomfort and
improve visual function by modulating ocular surface inflammation
in DED (30,31). However, to the best of our knowledge,
no systematic summary of the therapeutic effect of multi-acupoint
selection on DED has so far been provided. Therefore, a systematic
review and meta-analysis were performed in the present study to
evaluate the efficacy of periocular acupoints, as well as
periocular acupoints plus body acupoints, with the latest
literature on DED. On this basis, it was attempted to determine the
optimal acupoints for acupuncture treatment of DED.
Materials and methods
Databases and search strategy
The PubMed, Cochrane Library, Embase, Ovid, China
National Knowledge Infrastructure (CNKI), Chonqing VIP Information,
Co., Ltd. (CQVIP) and Wanfang databases were searched from
inception through to 10 July 2018. CNKI, CQVIP and Wanfang are
Chinese databases. The following medical search terms were used:
‘dry eye’, ‘dry eye syndrome’, ‘ophthalmoxerosis’,
‘keratoconjunctivitis sicca’, ‘xerophthalmia’, ‘acupuncture’,
‘electroacupuncture’, ‘Gan Yan’ (DED), ‘Gan Yan Zheng’ (DED), ‘Zhen
Jiu’ (acupuncture and moxibustion), ‘Zhen Ci’ (acupuncture) and
‘Dian Zhen’ (electroacupuncture). To identify additional articles,
reference lists of selected reviews and studies were manually
searched. There were no language restrictions.
Study selection
The two authors independently selected eligible
studies and discussed any emerging inconsistencies amongst each
other. The specific study inclusion criteria were as follows: i)
RCTs of patients with DED; ii) acupuncture or electroacupuncture
compared with several alternatives, including AT, other
non-acupuncture therapies or conventional treatment; iii)
acupuncture treatment combined with other interventions (including
AT or other non-acupuncture therapies) and comparison with the
other interventions; iv) outcomes included SIT results, BUT,
Symptoms score, CFS and visual analogue scale (VAS); and v) full
text available.
Studies fulfilling the following criteria were
excluded: i) Participants with Sjögren's syndrome; ii) acupuncture
combined with other treatments, including Chinese herbal,
warming-promotion needling and moxibustion, including thunder-fire
miraculous moxa; ii) control group treated with acupuncture therapy
only or combined with other interventions (including AT or other
non-acupuncture therapies); iv) animal studies or studies lacking a
control group, or articles published as case reports, reviews,
commentaries or letters.
Data extraction and risk of bias
assessment
Two independent reviewers (QBW, N D) read the full
texts of all selected articles and used a standardized collection
form to extract the following content: First author name and year
of publication, participant information, sample size, study
selection (inclusion and exclusion criteria), treatment protocol
(acupoints, duration, treatment sessions and frequency of
treatment) and major outcome data (BUT, SIT results, Symptoms
score, CFS, OSDI and VAS).
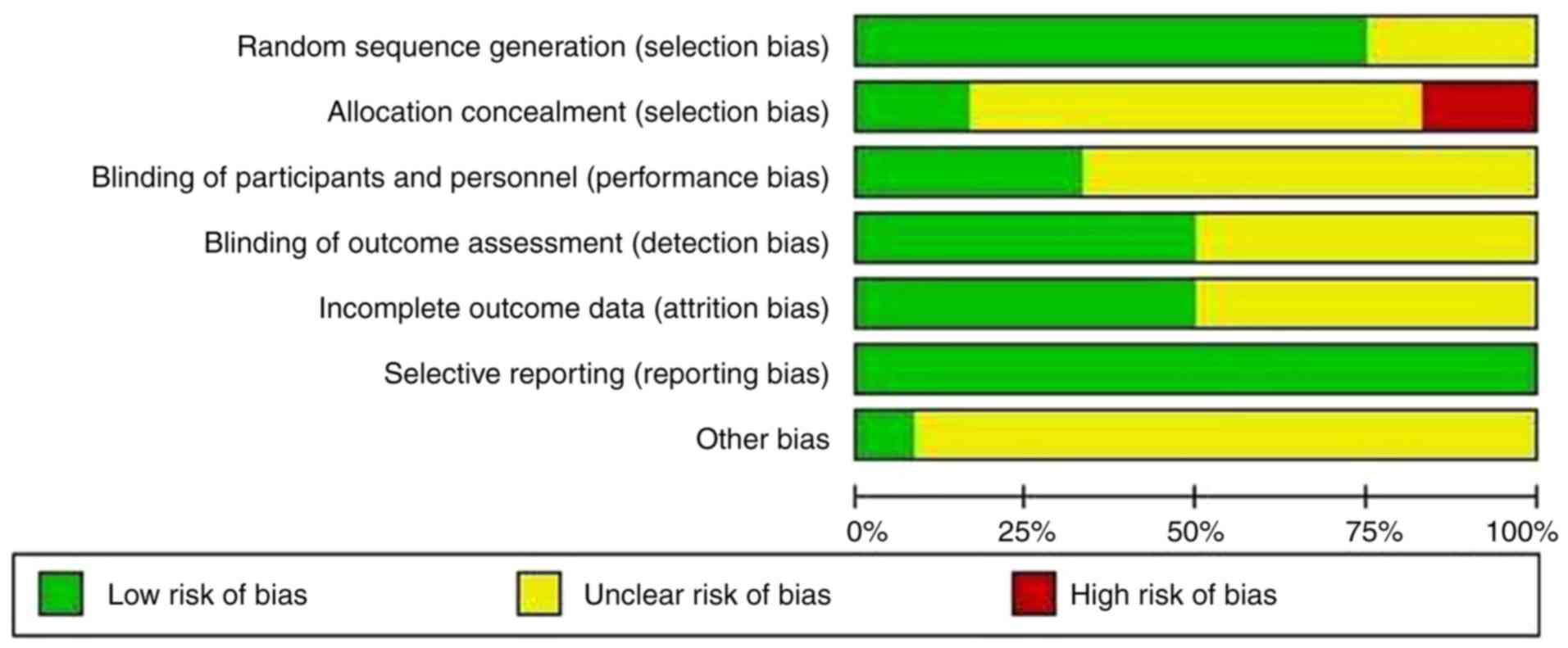
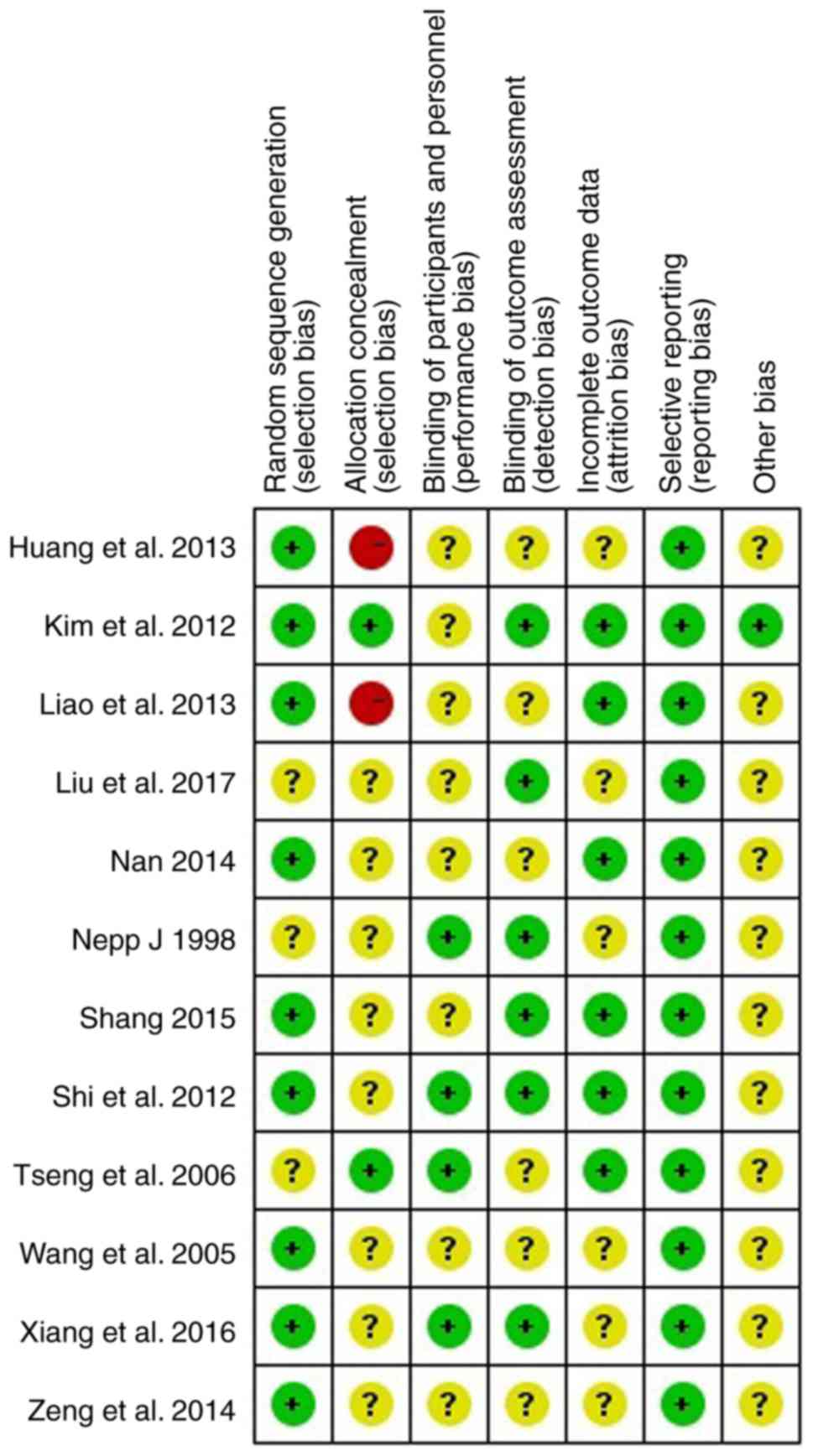
The risk-of-bias assessment of the included RCTs was
independently performed according to the Cochrane Collaboration
Tool (31). The following items were
included in the risk-of-bias assessment: Random sequence
generation, allocation concealment, blinding (participants and
personnel, outcome assessment), incomplete outcome data, selective
reporting and other biases (31).
Two reviewers (QBW, ND) independently assessed the quality of the
articles and discussed any emerging inconsistencies with a third
reviewer (JJW).
Data synthesis and statistical
methods
The statistical software Review Manager 5.3 for
Windows (provided by the Cochrane Collaboration) was applied for
data synthesis and statistical analysis. To evaluate the effect of
acupoint selection on DED, the weighted mean difference (WMD) with
95% CIs were used to analyze subgroup continuous data.
Heterogeneity in studies was assessed using the χ2 test
and Higgins I2 test (32). A fixed-effect model was used for
homogeneity (considered significant at P>0.1); a random-effect
model was used for heterogeneity (P<0.1).
Results
Search results
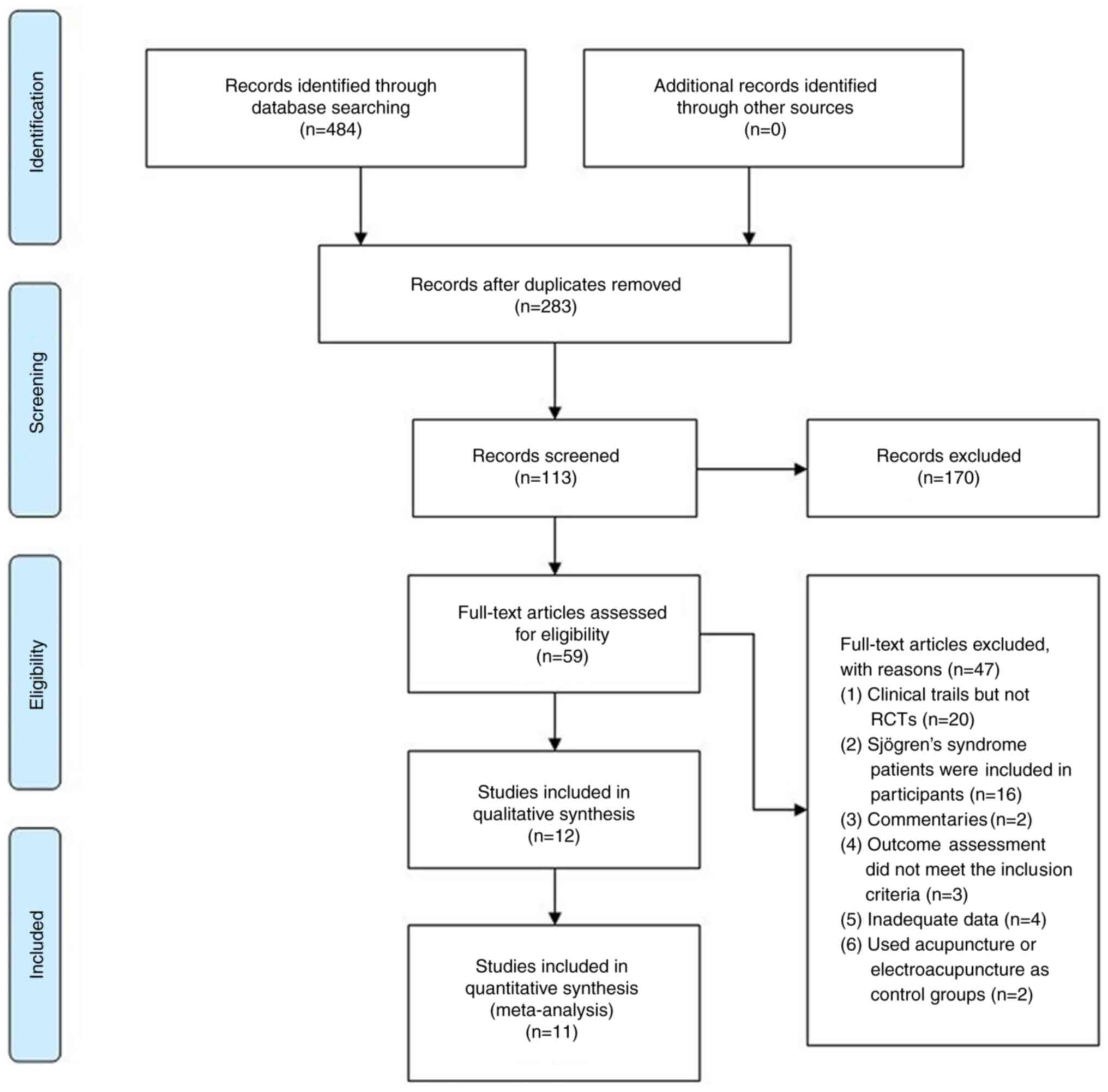
A total of 484 entries of potential relevance were
identified from the database search. After excluding duplicate
studies, screening of article titles and abstracts, 59 potentially
relevant studies were retrieved. After reviewing the full texts, 47
studies were excluded for the following reasons: i) Clinical trials
but not RCTs (n=20); ii) studies including patients Sjögren's
syndrome as participants (n=16); iii) commentaries (n=2); iv)
outcome assessment did not meet the inclusion criteria (n=3); v)
inadequate data (n=4); vi) acupuncture or electroacupuncture used
in the control groups (n=2). A flow diagram of the literature
search and study selection process is presented in Fig. 1.
Study characteristics
A total of 12 studies with 900 participants were
included in this review. A majority of the studies compared manual
acupuncture with AT (33-43).
An applied form of acupuncture was used in 4 of the studies,
including 1 study using silver spike point electro-therapy
(35), 1 study using
electroacupuncture (44) and 2
studies using combined acupuncture at the phenomaxillary ganglia
with acupoints (41,42). Participants in the study by Zeng
et al (40) were patients who
experienced DED for >1 month after LASIK. Furthermore, 2 studies
focused on DED in post-menopausal or peri-menopausal females
(38,43). Regarding the sensation of acupoints,
4 studies reported on de-qi (soreness, numbness, sensation of
heaviness or swelling) associated with the needling (35,37,40,44). A
total of 10 of the studies were performed in China (34-36,38-44).
Detailed descriptions of the studies and the acupuncture treatments
are provided in Tables I and
II.
 | Table IBaseline characteristics of the
randomized controlled trials included in the meta-analysis that
investigated the effects of acupuncture in dry eye disease. |
Table I
Baseline characteristics of the
randomized controlled trials included in the meta-analysis that
investigated the effects of acupuncture in dry eye disease.
| First author
(year) | Country | Sample
sizea | Gender (M/F) | Mean age
(range) | Duration (m or
y)b | Treatment regime in
intervention group | Treatment regime in
control group | Major outcomes | (Refs.) |
|---|
| Nepp (1998) | Austria | 52 (30/22) | NA | NA | NA | Acupuncture | AT | BUT, SIT, drop
frequency | (33) |
| Wang (2005) | China | 45 (15/15/15) | Intervention 1
(7/8) Intervention 2 (5/10) Control (5/10) | Intervention 1 51.7
(27-75) Intervention 2 51.8 (24-74) Control 51.5 (30-73) | Intervention 1
6m-10y Intervention 2 6m-10y Control 2m-10y | Acupuncture | AT | BUT, SIT, and
CFS | (34) |
| Tseng (2006) | China (Taiwan) | 43 (17/17/9) | Intervention 1
(4/13) Intervention 2 (6/11) Control (6/3) | Intervention 1
52.24 Intervention 2 47.58 Control 51.33 | Intervention 1
2.65±1.80 y Intervention 2 3.24±3.17 y Control 4.00±3.35 y | Intervention 1: SSP
+ AT, Intervention 2: Acupuncture + AT | AT | BUT, SIT, VAS,
overall score of eye condition | (35) |
| Shi (2012) | China | 68 (33/35) | Intervention
(14/19) Control (16/19) | Intervention 47.4
(29-63) Control 51.4 (27-65) | NA | Acupuncture | AT | ST, BUT, tear
lactoferrin concentration | (36) |
| Kim (2012) | South Korea | 150 (75/75) | Intervention
(22/53) Control (19/56 | Intervention 47.95
Control 46.05 | NA | Acupuncture | AT | OSDI, VAS, BUT,
SIT, QOL | (37) |
| Liao (2013) | China | 40 (0/40) | Intervention (0/20)
Control (0/20) | Intervention 52.7
(45-55) Control 53.1 (45-55) | NA | Acupuncture +
AT | AT | BUT, SIT, symptoms
score, VRQOL | (38) |
| Nan (2014) | China | 60 (30/30) | Intervention
(12/18) Control (13/17 | Intervention 48.57
(24-68) Control 47.56 (22-66) | Intervention 9.15 m
(2 m-8 y) Control 10.55 m (3 m-9 y) | Eye acupuncture +
AT | AT | ST, BUT, total
score | (39) |
| Zeng (2014) | China | 52 (28/24) | Intervention
(13/15) Control (11/13 | Intervention 33
(28-41) Control 31 (27-39) | Intervention 4-14
Control 6-18m | Acupuncture +
AT | AT | BUT, SIT, FLS | (40) |
| Shang (2015) | China | 148 (72/76) | Intervention
(40/32) Control (38/38 | Intervention 38
(24-61) Control 40 (21-64) | Intervention 4.3 y
(3 m-19 y) Control 4.6y(2m-22y) | Acupuncture | AT | Symptoms score,
VAS | (41) |
| Xiang (2016) | China | 88 (44/44) | Intervention
(20/24) Control (16/28) | Intervention 34.27
(20-64) Control 36.11 (22-59) | Intervention 15.07
(3-48) m Control 13.30 (3-48) m | Acupuncture | AT | OSDI, BUT, SIT,
FLS | (42) |
| Liu (2017) | China | 28 (14/14) | Intervention (0/14)
Control (0/14) | Intervention 60.714
Control 60.786 | Intervention
3.857±3.225y Control 3.786±3.011y | Acupuncture +
AT | AT | SIT, BUT, OSDI,
scores of symptoms and signs, protein analysis | (43) |
| Huang (2013) | China | 126 (64/62) | Intervention
(23/41) Control (20/42) | Intervention 42.32
(19-62) Control 41.18 (20-61) | Intervention 6.08
(1-15) m Control 5.17 (1-14) m |
Electroacupuncture | AT | Symptoms score,
BUT, SIT, FLS | (43) |
 | Table IIDetails of acupuncture treatment
characteristics of the randomized controlled trials included in the
present meta-analysis. |
Table II
Details of acupuncture treatment
characteristics of the randomized controlled trials included in the
present meta-analysis.
| First author
(year) | Acupoints | Treatment
frequency | Therapeutic
course | Duration of
acupuncture (min) | Insertion
depth | Needle type | De-qi | (Refs.) |
|---|
| Nepp (1998) | Periocular
acupoints: GB 1, BL 2, EX-HN2; other acupoints: ST 5, LI 4, SI 3,
LI 3, KI 6, TE 5 | Intervention: 1
time per week; Control: NA | Intervention: 10
weeks Control: NA | 30 | NA | NA | NA | (33) |
| Wang (2005) | Acupuncture 1: Heat
ablaze and yin injury: LI 11, LI 4, SP 6, KI 3, ST 2, LI 20; Phlegm
and blood | Intervention 1:
Once in 2 days, 10 times/course, 10 days' rest after; | Intervention 1: 3
courses; Intervention 2: a course | 20-25 | NA | NA | NA | (34) |
| | stasis: ST 2, SP
10, SP 9, ST 36, SP 6, ST 40; Acupuncture 2: BL 2, TE 23, GB 14, ST
1 | Intervention 2:
Once in 2 days, 10 times/course, 10 days rest after a; course
Control: 5 times a day | 3 courses; Control:
30 days | | | | | |
| Tseng (2006) | Periocular
acupoints: EX-HN5, TE 23, GB 14, ST 2; other acupoints: SP 6 | Intervention 1:
Twice a week, 2-3 days apart; Intervention 2: Twice a week, 2-3
days apart; Control: NA | Intervention 1: 8
weeks; Intervention 2: 8 weeks; Control: NA | 20 | NA | Points on the face:
No. 36 one-inch needles, the lower extremities: No. 32 two-inch
needles | De-qi | (35) |
| Shi (2012) | Periocular
acupoints: ST 1, BL 1, EX-HN 5, TE 23; other acupoints: GV 20, LI
4, ST 36 | Intervention: 3
times per week; Control: 3-4 times a day | Intervention: 3
weeks; Control: 3 weeks | 25 | NA | 40x0.25 mm
disposable acupuncture needles | NA | (36) |
| Kim (2012) | Periocular
acupoints: ST 1, BL 2, TE 23, GB 14, Ex 1, GV 23; other acupoints:
GB 20, LI 4, LI 11 | Intervention: 3
times per week; Control: Use as required (at least once per
day) | Intervention: 4
weeks; Control: 4 weeks | 20 | The acupuncture
points at the face and head: 0.6 to 3 cm, and 3 to 4.5 cm for
points of hand (LI 4) and arm (LI 11). | 0.20x30 mm
disposable acupuncture needles | De-qi | (37) |
| Liao (2013) | Periocular
acupoints: BL 1, ST 1, TE 23 penetrating EX-HN4; other acupoints:
KI 3, LR 3, SP 6, ST 36 | Intervention: 1
time a day; Control: 4 times a day | Intervention: 14
days; Control: 14 days | 30 | NA | NA | NA | (38) |
| Nan (2014) | Eye acupuncture
(liver area, gallbladder area, kidney area, spleen stomach area,
upper jiao area) | Intervention: 1
time a day; Control: 5 times a day | Intervention: 20
days; Control: 20 days | 15-20 | Liver area and
gallbladder area: 0.5 cun | 0.18x13 mm
disposable acupuncture needles | NA | (39) |
| Zeng (2014) | Periocular
acupoints: GB 1, BL 1, LI 20, BL 2, ST 2, EX-HN5; other acupoints:
SP 6, SP 10, ST 36, KI 3 | Intervention:
Acupuncture 1 time a day, Tears Naturale II 3 times a day, Refresh
plus 1 time a day; Control: Tears Naturale II 3 times a day,
Refresh Plus 1 time a day | Intervention: 10
days; Control: 10 days | NA | BL 1: 0.5 cun, GB
1: 0.7 cun | NA | De-qi | (40) |
| Shang (2015) | Periocular
acupoints: phenomaxillary ganglia, BL 1, EX-HN5, ST 2 | Intervention:
acupuncture 1 time per week; Control: AT 1 time a day | Intervention: 24
weeks; Control: 15 days | NA | Phenomaxillary
ganglia: 55 mm | Phenomaxillary
ganglia: 0.35x60 mm needles | De-qi | (41) |
| Xiang (2016) | Periocular
acupoints: phenomaxillary ganglia, BL 2, Shangjingming (Extra), TE
23, ST 2 | Intervention: First
week: Continuous acupuncture 5 times, and the rest 2 weeks: 3 times
a week (1 time every other day); Control: AT 4 times a day | Intervention: 3
weeks; Control: 3 weeks | 30 | Phenomaxillary
ganglia: 50 mm | Phenomaxillary
ganglia: 0.25x60 mm, periocular acupoints: 0.25x25 mm | De-qi | (42) |
| Liu (2017) | Periocular
acupoints: BL 1, BL 2, TE 23, EX-HN5, ST 2, ST 1; other acupoints:
LI 4, GB 20, GV 20 | Intervention:
Acupuncture three times a week, AT: NA; Control: NA | Intervention: 8
weeks; Control: 8 weeks | 30 | NA | NA | NA | (43) |
| Huang (2013) | Periocular
acupoints: EX-HN5, ST 1, BL 1, BL 2, Ex-HN7; the acupoints: LU 7,
GB 37, KI 3, LR 3; Ex-HN5 and ST 1 were connected to EA
apparatus | Intervention: 1
time a day; Control: 4 times a day | Intervention: 30
times; Control: 30 times | 30 | NA | 40 mm disposable
acupuncture needles | De-qi | (44) |
Risk-of-bias assessment
The results of the risk-of-bias assessment are
summarized in Figs. 2 and 3. No serious risk of bias was detected. All
studies included in the systematic review and meta-analysis
mentioned randomization. Furthermore, 9 studies described the
method of random sequence generation (using a random number Table
or a computerized random-number generator) (34,36-42,44).
Clear and adequate allocation concealment was performed in only two
studies (35,37) and assessor blinding was used in six
studies (33,36,37,41-43).
Sufficient details of drop-out rates and reasons were described in
six studies (35-39,41).
Bias was suspected in two studies that did not mention the
intervention time in the control group (33,35).
Meta-analysis for comparison between
periocular acupoints and periocular acupoints plus body acupoints
with AT
The study by Nepp et al (33) was excluded from the present
meta-analysis, as it contained no detailed data except a graph.
Therefore, the results of 11 of 12 studies were used to analyze
BUT, SIT results and Symptoms score.
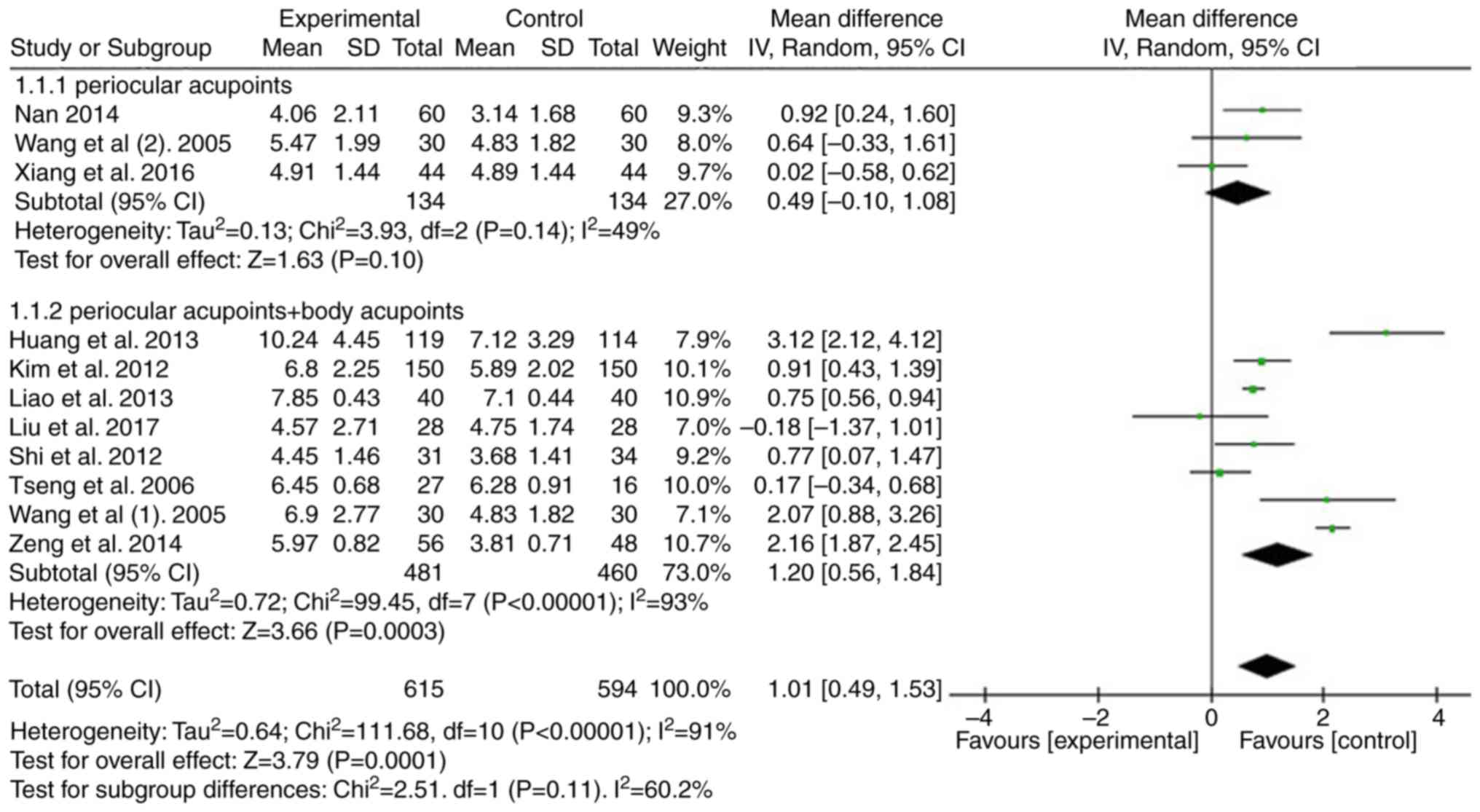
A total of 10 studies were analyzed to compare the
effect of periocular acupoints or periocular acupoints plus body
acupoints with those of AT in patients with DED in terms of the
results of the BUT test (34-40,42-44).
Compared with the AT group, significant improvement was identified
among the acupuncture groups (n=1,209, WMD=1.01, 95% CI: 0.49-1.53,
P=0.0001). Of note, subgroup analysis indicated no significant
advantage of periocular acupoint intervention (P=0.10), but there
was a significant difference in periocular acupoints plus body
acupoint intervention (P=0.0003; Fig.
4).
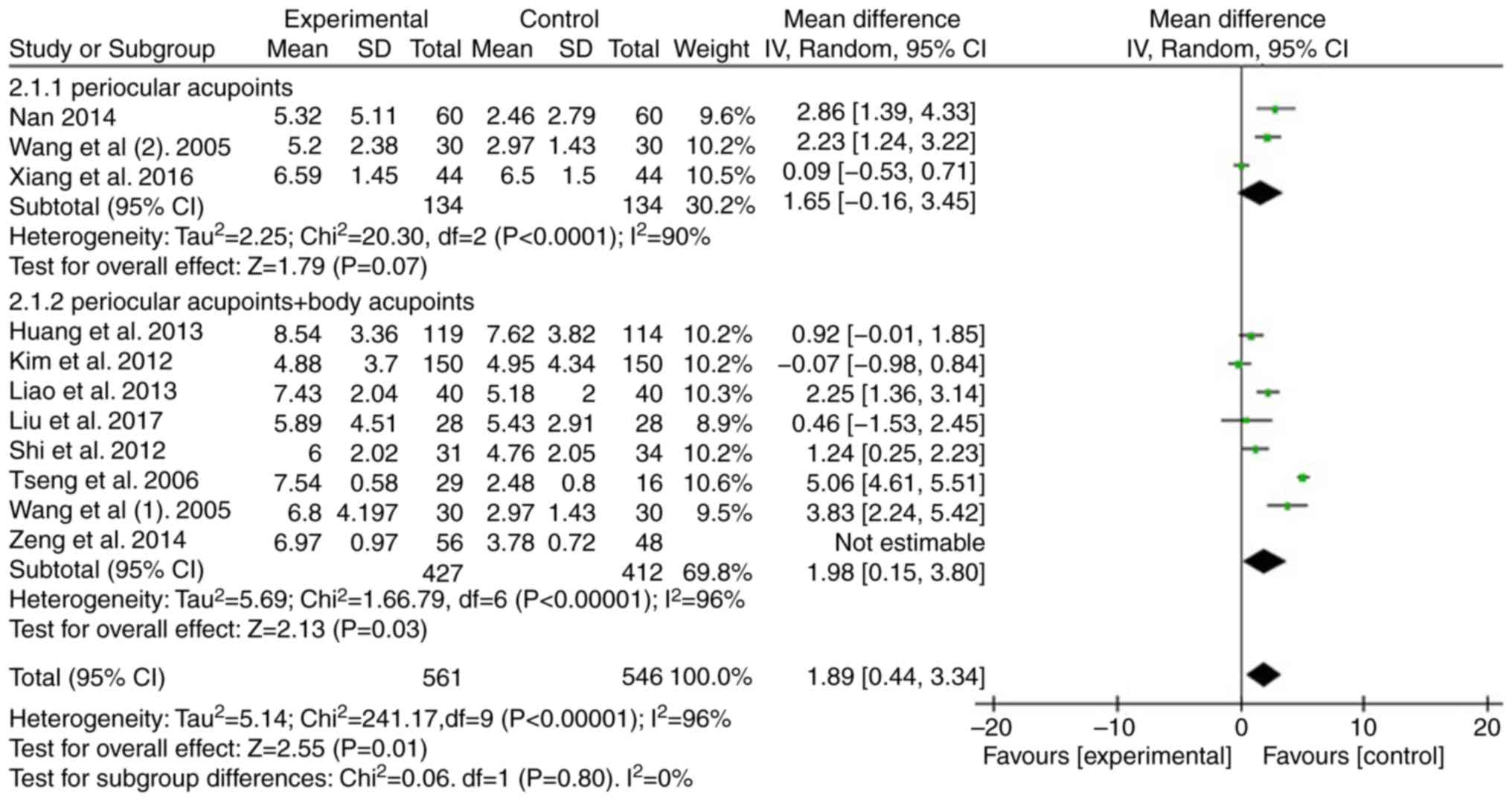
For the results of the SIT, 10 studies were used to
compare the effect of periocular acupoints or periocular acupoints
plus body acupoints with those of AT in patients with DED (34-40,42-44).
Compared with the AT group, significant improvement was determined
among the acupuncture groups (n=1,107, WMD=1.98, 95% CI: 0.44-3.34,
P=0.01). The subgroup analysis indicated no significant difference
in periocular acupoint intervention (P=0.07), but there was a
significant difference in periocular acupoints plus body acupoints
intervention (P=0.03; Fig. 5).
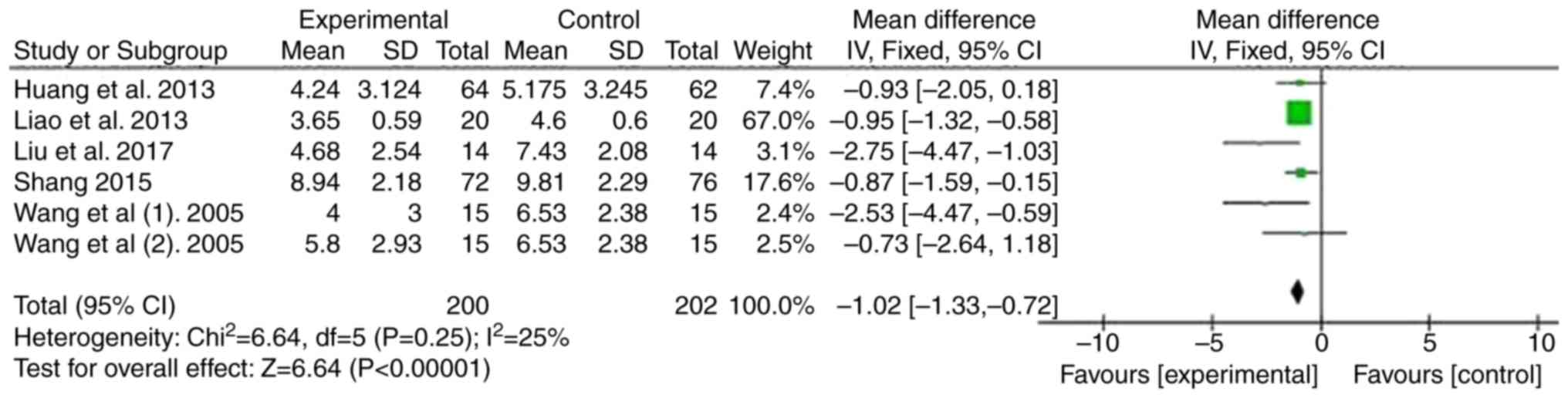
In addition, five studies were used to evaluate the
Symptoms score (34,38,39,42,44).
Compared with the AT group, the results indicated a significant
difference among acupuncture groups (n=402, WMD=-1.02, 95% CI:
-1.33 to -0.72, P<0.00001; Fig.
6).
Discussion
The purpose of the present systematic review and
meta-analysis was to analyze the difference between each
acupuncture modality group (periocular acupoints group and
periocular acupoints plus body acupoints group) and the AT group.
Although previous systematic reviews and meta-analyses have
confirmed that acupuncture may effectively relieve DED (26-28),
to the best of our knowledge, the present study was the first
systematic review evaluating the therapeutic effects of
multi-acupoint acupuncture on DED. In comparison with previous
studies, stricter inclusion and exclusion criteria were adopted.
After the selection process, the studies included were compared
with those of the previous meta-analyses. Certain studies included
in the previous meta-analyses were not included in the present
study. The entire text of those studies was read and they were
found unsuitable, principally because they included patients with
Sjogren's syndrome and non-randomized controlled clinical trials.
The present systematic review and meta-analysis initially included
11 RCTs comprising 848 patients with DED. The overall results
indicated that acupuncture significantly improved the BUT, SIT
results and Symptom scores compared with AT.
Although there are numerous predisposing factors and
various clinical manifestations of DED, the major pathologies
include hyperosmolarity, ocular surface inflammation and damage,
tear film instability and neurosensory abnormalities (1). Tear film osmolarity has an important
role in the pathogenesis of DED. It varies with the changes in
internal and external factors, including body hydration, tear film
stability, environmental conditions, blink interval, eyelid opening
width and characteristics of tear film lipid layer (45). An increase in the osmolarity of the
tear film is mainly caused by its excessive evaporation and reduced
tear production (46-48). Exposure to
tears with high osmolarity may lead to apoptosis of cells, loss of
goblet cells, and dysfunction in corneal and conjunctival mucin
expression. In addition, tear hyperosmolarity may activate a series
of inflammatory events and contribute to further morphological
changes in the cornea and conjunctiva. These changes may aggravate
tear film instability and persistence of the condition (45,49,50).
In the theory of Traditional Chinese Medicine,
acupoints are specific points that reflect the internal state of
the body and regulate its function (51). The major purpose of acupoint
stimulation includes the regulation of local and systemic effects.
In the present study, the additional effect of stimulation of body
acupoints in other parts of the body besides the periocular
acupoints was examined, mainly for the purpose of distinguishing
between the local therapeutic effects and remote sensing
therapeutic effects. Histological investigations have confirmed
that the local acupoints may be composed of the following parts:
High-density nerve endings, high concentration of nerve and
vascular elements, and mast cells, which have the function of
perceiving stimuli (52). Zhang
et al (53) proved that the
skin resistance of acupoints in healthy individuals is
significantly lower than that in non-acupoint areas. When the
acupoints are stimulated, local biological molecules may be
released, thus having a role in regulating the local effects
(54). Studies have confirmed that
acupuncture stimulates the afferent nerves of the skin and muscle
at acupoints, and the somatic sensory information is then
transmitted to the cerebral cortex and different nuclei of the
brain stem and hypothalamus. At the same time, it may regulate the
autonomic function of the body (55,56).
Therefore, the combination of periocular acupoints and the body
acupoints not only increases the local effects but also increases
the local therapeutic effects but also increases the remote sensing
therapeutic effects, which is more conducive to the treatment of
dry eye.
Acupuncture therapy has a long history in the
treatment of ophthalmic diseases. Systematic reviews have confirmed
that acupuncture is effective in the treatment of myopia, amblyopia
and optic atrophy (57-59). In recent
decades, the use of acupuncture therapy for the treatment of DED
has aroused interest and its efficacy has been actively explored
(60). Although acupuncture
treatment of dry eye has yielded encouraging results, rigorous
clinical trials are required to confirm its therapeutic effect
(26). Numerous studies have
confirmed that acupuncture is useful for the treatment of dry eye,
but the mechanism of action remains elusive. It is thought that
acupuncture stimulates the lacrimal gland to secrete tears
(61), promote corneal wound healing
(62), reduce tension and reduce
pain intensity or increase the pain threshold (63), regulate the autonomic nervous system
and immune system (64,65), reduce local inflammatory response
(43) and increase the flow velocity
of the ophthalmic artery (66). Most
of the acupuncture treatments for dry eye are based on the
acupoints around the eyes, but there is no further research on the
selection of acupoints. The most commonly used periocular acupoints
include EX-HN5, BL1, GB1, BL2, ST1 and TE23.
Most clinicians still rely on conventional
diagnostic tests, including the BUT test and SIT, for the diagnosis
of DED (67). The measurement of
tear film stability is usually performed by the BUT test (28), while the tear capacity is reflected
by the SIT. Most patients seek ophthalmological intervention due to
ocular discomfort. Although DED is usually diagnosed based on
symptoms, there is no correlation between symptoms and signs of
DED. The ability to quantify ocular surface symptoms helps to
establish an additional medical assessment for dry eye. They have a
critical guiding role in monitoring the development of DED and the
prognosis after treatment (28).
Therefore, in the present meta-analysis, the BUT, SIT results and
Symptoms score were used as the outcome indexes, which may reflect
the effect of acupuncture treatment from different angles. The
present meta-analysis indicated that the BUT and SIT result of
patients with DED exhibited statistically improvement in the
acupuncture group, and the treatment effect of periocular acupoints
plus body acupoints was more efficient than that using periocular
acupoints only. At the same time, the present meta-analysis
indicated that the symptoms score of patients with DED exhibited
statistically improvement in the acupuncture group.
The present study indicated that the acupuncture
group exhibited significant improvements in BUT, SIT result and
Symptoms score compared with those in the control group. However,
high heterogeneity was noted in the BUT (I2=91%) and SIT
results (I2=96%). To reduce the heterogeneity of the
present results, the studies were screened more strictly than in
previous meta-analyses, excluding those studies on patients with
Sjögren's syndrome and on acupuncture combined with other
treatments, including moxibustion, Chinese herbal medicine,
warming-promotion needling or thunder-fire miraculous moxa.
However, the problem of high heterogeneity was not completely
resolved. Different acupuncturists, different AT and the frequency
of AT administration are important contributors to the high
heterogeneity and affect the evaluation of the present results.
The present systematic review and meta-analysis has
several limitations. The RCTs included in the present study
exhibited a variation in acupuncture intervention programs
(including acupoint selection, duration of treatment and course of
treatment) and patient characteristics (including age, sex,
ethnicity, environment and severity of DED). Due to insufficient
data from RCTs, it was impossible to perform in-depth
investigations of specific changes. Thus, individual patient data
are required for future meta-analyses. Further limitations include
the lack of standard protocols and the lack of high-quality RCTs.
Only three studies reported on adverse reactions to acupuncture in
the treatment of dry eye (36,37,40).
Follow-up evaluation of acupuncture treatment for dry eye is
necessary (37). Although the
present study confirmed that acupuncture is more effective than AT,
the latter has the advantage of being convenient to use, while
needling is time-consuming and inconvenient for most patients with
DED. A previous study indicated that the effect of acupuncture
lasts longer than that of AT (37).
Further large-cohort studies are required to confirm the long-term
efficacy of acupuncture treatment.
In conclusion, the present meta-analysis revealed
that in terms of BUT and SIT results, the effect of acupuncture is
better than AT. However, due to the relatively small sample size,
short treatment duration, lack of a sham-acupuncture control and
insufficient observation of long-term efficacy, further
large-sample RCTs are required to evaluate the efficacy of
acupuncture in the treatment of DED.
Acknowledgements
Not applicable.
Funding
The present study was funded by the National Natural
Science Foundation of China (grant no. 81774419).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article
Authors' contributions
Conception and design: WPG and QBW. Literature
search and data extraction: QBW, WW, ND and JJW. Drafting of the
manuscript: QBW and WW. Data interpretation and research
supervision: WPG. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Craig JP, Nichols KK, Akpek EK, Caffery B,
Dua HS, Joo CK, Liu Z, Nelson JD, Nichols JJ, Tsubota K and
Stapleton F: TFOS DEWS II definition and classification report.
Ocul Surf. 15:276–283. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Sriprasert I, Warren DW, Mircheff AK and
Stanczyk FZ: Dry eye in postmenopausal women: A hormonal disorder.
Menopause. 23:343–351. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Qiu X, Gong L, Sun X and Jin H:
Age-related variations of human tear meniscus and diagnosis of dry
eye with Fourier-domain anterior segment optical coherence
tomography. Cornea. 30:543–549. 2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Gayton JL: Etiology, prevalence, and
treatment of dry eye disease. Clin Ophthalmol. 3:405–412.
2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Donnenfeld ED, Ehrenhaus M, Solomon R,
Mazurek J, Rozell JC and Perry HD: Effect of hinge width on corneal
sensation and dry eye after laser in situ keratomileusis. J
Cataract Refract Surg. 30:790–797. 2004.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Moon JH, Lee MY and Moon NJ: Association
between video display terminal use and dry eye disease in school
children. J Pediatr Ophthalmol Strabismus. 51:87–92.
2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Nakamura S, Kinoshita S, Yokoi N, Ogawa Y,
Shibuya M, Nakashima H, Hisamura R, Imada T, Imagawa T, Uehara M,
et al: Lacrimal hypofunction as a new mechanism of dry eye in
visual display terminal users. PLoS One. 5(e11119)2010.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Iyer JV, Lee SY and Tong L: The dry eye
disease activity log study. ScientificWorldJournal.
2012(589875)2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Terry MA: Dry eye in the elderly. Drugs
Aging. 18:101–107. 2001.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Begley CG, Chalmers RL, Abetz L,
Venkataraman K, Mertzanis P, Caffery BA, Snyder C, Edrington T,
Nelson D and Simpson T: The relationship between habitual
patient-reported symptoms and clinical signs among patients with
dry eye of varying severity. Invest Ophthalmol Vis Sci.
44:4753–4761. 2003.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Craig JP, Nelson JD, Azar DT, Belmonte C,
Bron AJ, Chauhan SK, de Paiva CS, Gomes JAP, Hammitt KM, Jones L,
et al: TFOS DEWS II report executive summary. Ocul Surf.
15:802–812. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
McCarty CA, Bansal AK, Livingston PM,
Stanislavsky YL and Taylor HR: The epidemiology of dry eye in
Melbourne, Australia. Ophthalmology. 105:1114–1119. 1998.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lu P, Chen X, Liu X, Yu L, Kang Y, Xie Q,
Ke L and Wei X: Dry eye syndrome in elderly Tibetans at high
altitude: A population-based study in China. Cornea. 27:545–551.
2008.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hashemi H, Khabazkhoob M, Kheirkhah A,
Emamian MH, Mehravaran S, Shariati M and Fotouhi A: Prevalence of
dry eye syndrome in an adult population. Clin Exp Ophthalmol.
42:242–248. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Golden MI, Fries PL and Patel BC (Eds):
Dry eye syndrome. StatPearls Publishing, Treasure Island, FL,
2019.
|
|
16
|
Rossi GCM, Scudeller L, Bettio F,
Pasinetti GM and Bianchi PE: Prevalence of dry eye in video display
terminal users: A cross-sectional Caucasian study in Italy. Int
Ophthalmol. 39:1315–1322. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Miljanović B, Dana R, Sullivan DA and
Schaumberg DA: Impact of dry eye syndrome on vision-related quality
of life. Am J Ophthalmol. 143:409–415. 2007.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Yu J, Asche CV and Fairchild CJ: The
economic burden of dry eye disease in the United States: A decision
tree analysis. Cornea. 30:379–387. 2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Belmonte C and Gallar J: Cold
thermoreceptors, unexpected players in tear production and ocular
dryness sensations. Invest Ophthalmol Vis Sci. 52:3888–3892.
2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Sacchetti M and Lambiase A: Neurotrophic
factors and corneal nerve regeneration. Neural Regen Res.
12:1220–1224. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Belmonte C, Brock JA and Viana F:
Converting cold into pain. Exp Brain Res. 196:13–30.
2009.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Vickers AJ, Vertosick EA, Lewith G,
MacPherson H, Foster NE, Sherman KJ, Irnich D, Witt CM and Linde K:
Acupuncture Trialists' Collaboration: Acupuncture for chronic pain:
Update of an individual patient data meta-analysis. J Pain.
19:455–474. 2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kaptchuk TJ: Acupuncture: Theory,
efficacy, and practice. Ann Intern Med. 136:374–383.
2002.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Manheimer E, White A, Berman B, Forys K
and Ernst E: Meta-analysis: Acupuncture for low back pain. Ann
Intern Med. 142:651–663. 2005.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Smith JR, Spurrier NJ, Martin JT and
Rosenbaum JT: Prevalent use of complementary and alternative
medicine by patients with inflammatory eye disease. Ocul Immunol
Inflamm. 12:203–214. 2004.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Lee MS, Shin BC, Choi TY and Ernst E:
Acupuncture for treating dry eye: A systematic review. Acta
Ophthalmol. 89:101–106. 2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Kim BH, Kim MH, Kang SH and Nam HJ:
Optimizing acupuncture treatment for dry eye syndrome: A systematic
review. BMC Complement Altern Med. 18(145)2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Wolffsohn JS, Arita R, Chalmers R,
Djalilian A, Dogru M, Dumbleton K, Gupta PK, Karpecki P, Lazreg S,
Pult H, et al: TFOS DEWS II diagnostic methodology report. Ocul
Surf. 15:539–574. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Yang L, Yang Z, Yu H and Song H:
Acupuncture therapy is more effective than artificial tears for dry
eye syndrome: Evidence based on a meta-analysis. Evid Based
Complement Alternat Med. 2015(143858)2015.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Zhang X, Liu Z, Ding W, Zhang J, Shi H and
Zhu W: Efficacy and safety of acupuncture at a single BL1 acupoint
in the treatment of moderate to severe dry eye disease: Protocol
for a randomized, controlled trial. Medicine (Baltimore).
97(e10924)2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Higgins JP, Altman DG, Gøtzsche PC, Jüni
P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L and Sterne JA:
Cochrane Bias Methods Group; Cochrane Statistical Methods Group:
The Cochrane Collaboration's tool for assessing risk of bias in
randomised trials. BMJ. 343(d5928)2011.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Higgins JP and Green S: Cochrane Handbook
for Systematic Reviews of Interventions: Cochrane Book Series
2008.
|
|
33
|
Nepp J, Wedrich A, Akramian J, Derbolav A,
Mudrich C, Ries E and Schauersberger J: Dry eye treatment with
acupuncture. A prospective, randomized, double-masked study. Adv
Exp Med Biol. 438:1011–1016. 1998.PubMed/NCBI
|
|
34
|
Wang ZL, He HQ, Huang D and Shi CG: Effect
of integral syndrome differentiation acupuncture on the tear film
stability in the patient of xerophthalmia. Zhongguo Zhen Jiu.
25:460–463. 2005.(In Chinese). PubMed/NCBI
|
|
35
|
Tseng KL, Liu HJ, Tso KY, Woung LC, Su YC
and Lin JG: A clinical study of acupuncture and SSP (silver spike
point) electro-therapy for dry eye syndrome. Am J Chin Med.
34:197–206. 2006.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Shi JL and Miao WH: Effects of acupuncture
on lactoferrin content in tears and tear secretion in patients
suffering from dry eyes: A randomized controlled trial. Zhong Xi Yi
Jie He Xue Bao. 10:1003–1008. 2012.(In Chinese). PubMed/NCBI View Article : Google Scholar
|
|
37
|
Kim TH, Kang JW, Kim KH, Kang KW, Shin MS,
Jung SY, Kim AR, Jung HJ, Choi JB, Hong KE, et al: Acupuncture for
the treatment of dry eye: A multicenter randomised controlled trial
with active comparison intervention (artificial teardrops). PLoS
One. 7(e36638)2012.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Liao L, Wei Q and Gong X: Effects of
nourishing liver and kidney by acupuncture for vision related
quality of life in perimenopausal women with dry eye. J Trad Chin
Ophthalmol. 23:403–406. 2013.
|
|
39
|
Nan H: Clinical Observation of 60 Cases of
Dry Eye Syndrome by the Treatment of Eye Acupuncture Combining the
ArtifiCiaI Tears: Hubei University of Chinese Medicine; 2014.
|
|
40
|
Zeng Z, Ma Q, Song C and Xia H: Clinical
observation on 28 cases of dry eye after LASIK treated by
acupuncture and artificial tear. Hunan J Trad Chin Med. 30:105–107.
2014.
|
|
41
|
Shang XJ: Therapeutic observation of
acupuncture at phenomaxillary ganglia for dry eye syndrome.
Shanghai J Acu Mox. 9:870–872. 2015.(In Chinese).
|
|
42
|
Xiang S, Jiang X, Li Y and Dou R: The
efficacy of acupuncture at phenomaxillary ganglion and periocular
acupiont for the treatment of dry eye. J Zhejiang Univ Trad Chin
Med. 40:730–734. 2016.(In Chinese).
|
|
43
|
Liu Q, Liu J, Ren C, Cai W, Wei Q, Song Y
and Yu J: Proteomic analysis of tears following acupuncture
treatment for menopausal dry eye disease by two-dimensional
nano-liquid chromatography coupled with tandem mass spectrometry.
Int J Nanomedicine. 12:1663–1671. 2017.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Huang R, Wu X and Li D: Observation on
therapeutic effect of acupuncture on dry eye. Chin J Information on
TCM. 20:67–68. 2013.(In Chinese).
|
|
45
|
Bron AJ, de Paiva CS, Chauhan SK, Bonini
S, Gabison EE, Jain S, Knop E, Markoulli M, Ogawa Y, Perez V, et
al: TFOS DEWS II pathophysiology report. Ocul Surf. 15:438–510.
2017.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Li Y, Liu H, Zeng W and Wei J: Edaravone
protects against hyperosmolarity-induced oxidative stress and
apoptosis in primary human corneal epithelial cells. PLoS One.
12(e0174437)2017.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Gilbard JP, Rossi SR and Heyda KG: Tear
film and ocular surface changes after closure of the meibomian
gland orifices in the rabbit. Ophthalmology. 96:1180–1186.
1989.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Xie Y and Wang L: Correlation between tear
osmolarity and the dry eye severity. Chinese J Experimental
Ophthalmology. 30:1022–1025. 2012.(In Chinese).
|
|
49
|
Cong C, Bi H and Wen Y: Research advance
of the pathogenesis and treatment of dry eye. Guoji Yanke Zazhi
(Int Eye Sci). 12:464–467. 2012.(In Chinese).
|
|
50
|
Baudouin C, Aragona P, Messmer EM,
Tomlinson A, Calonge M, Boboridis KG, Akova YA, Geerling G,
Labetoulle M and Rolando M: Role of hyperosmolarity in the
pathogenesis and management of dry eye disease: Proceedings of the
OCEAN group meeting. Ocul Surf. 11:246–258. 2013.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Melzack R, Stillwell DM and Fox EJ:
Trigger points and acupuncture points for pain: Correlations and
implications. Pain. 3:3–23. 1977.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Li F, He T, Xu Q, Lin LT, Li H, Liu Y, Shi
GX and Liu CZ: What is the Acupoint? A preliminary review of
Acupoints. Pain Med. 16:1905–1915. 2015.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Zhang WB, Jeong DM, Lee YH and Lee MS:
Measurement of subcutaneous impedance by four-electrode method at
acupoints located with single-power alternative current. Am J Chin
Med. 32:779–788. 2004.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Wang Y, Yin LM, Xu YD, Lui YY, Ran J and
Yang YQ: The research of acupuncture effective biomolecules:
Retrospect and prospect. Evid Based Complement Alternat Med.
2013(608026)2013.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Andersson S and Lundeberg T:
Acupuncture-from empiricism to science: Functional background to
acupuncture effects in pain and disease. Med Hypotheses.
45:271–281. 1995.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Takahashi T: Mechanism of acupuncture on
neuromodulation in the gut-a review. Neuromodulation. 14:8–12.
2011.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Zhi FY, Liu J, Ma XP, Hong J, Zhang J,
Zhang D, Zhao Y, Wu LJ, Yang YT, Wu DY, et al: Manual acupuncture
for optic atrophy: A systematic review and meta-analysis. Evid
Based Complement Alternat Med. 2019(1735967)2019.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Wei ML, Liu JP, Li N and Liu M:
Acupuncture for slowing the progression of myopia in children and
adolescents. Cochrane Database Syst Rev. (CD007842)2011.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Yan X, Zhu T, Ma C, Liu A, Dong L and Wang
J: A meta-analysis of randomized controlled trials on acupuncture
for amblyopia. Evid Based Complement Alternat Med.
2013(648054)2013.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Lin T, Gong L, Liu X and Ma X:
Fourier-domain optical coherence tomography for monitoring the
lower tear meniscus in dry eye after acupuncture treatment. Evid
Based Complement Alternat Med. 2015(492150)2015.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Gong L, Sun X and Chapin WJ: Clinical
curative effect of acupuncture therapy on xerophthalmia. Am J Chin
Med. 38:651–659. 2010.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Müller LJ, Marfurt CF, Kruse F and Tervo
TM: Corneal nerves: Structure, contents and function. Exp Eye Res.
76:521–542. 2003.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Nepp J, Tsubota K, Goto E, Schauersberger
J, Schild G, Jandrasits K, Abela C and Wedrich A: The effect of
acupuncture on the temperature of the ocular surface in
conjunctivitis sicca measured by non-contact thermography:
Preliminary results. Adv Exp Med Biol. 506:723–726. 2002.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Bäcker M, Grossman P, Schneider J,
Michalsen A, Knoblauch N, Tan L, Niggemeyer C, Linde K, Melchart D
and Dobos GJ: Acupuncture in migraine: Investigation of autonomic
effects. Clin J Pain. 24:106–115. 2008.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Kavoussi B and Ross BE: The neuroimmune
basis of anti-inflammatory acupuncture. Integr Cancer Ther.
6:251–257. 2007.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Zhu C: Effect of acupuncture on visual
system and its mechanism. Heilongjiang Med J. 29:744–5. 2005.
|
|
67
|
Pflugfelder SC, Solomon A and Stern ME:
The diagnosis and management of dry eye: A twenty-five-year review.
Cornea. 19:644–649. 2000.PubMed/NCBI View Article : Google Scholar
|