Introduction
Coronary heart disease (CHD) is a major public
health problem (1). In 2016, the
American Heart Association reported that there were 400,000 deaths
due to CHD each year in the United States, and that the number of
new cases has increased to 785,000(2). Dual antiplatelet therapy (DAPT) is a
cornerstone treatment for arterial coronary disease, and second
line for the prevention of cardiovascular and cerebrovascular
events. Therefore, endoscopists are encountering increasing numbers
of patients on DAPT.
Post-polypectomy bleeding (PPB) is the most common
complication of colonoscopy with polypectomy, ranging in prevalence
from 0.6-6.1% (3). Antiplatelet
agents such as the thienopyridines and aspirin have been used
widely to decrease thrombotic events, particularly in patients who
have had coronary stents, peripheral stents for vascular disease,
myocardial infarctions and cerebrovascular events (4). For patients on antiplatelet therapy
undergoing polypectomy, the management of perioperative therapy is
a common clinical dilemma (5). The
physician needs to weigh the increased risk of PPB against the
thrombotic risk caused by discontinuation of the antiplatelet
agents. Although the interruption of clopidogrel decreases PPB, it
has been associated with higher mortality rates, due to
complications such as stent thrombosis, myocardial infarction and
stroke (6). Nonetheless, there is no
consensus on how the risk of PPB and of thrombotic events should be
balanced, resulting in considerable variability in current clinical
practice (7). A retrospective study
discovered that the incidence of delayed PPB within 30 days
following polypectomy was significantly higher inpatients on
clopidogrel and concomitant aspirin/nonsteroidal anti-inflammatory
drugs (6). However, another study
showed that the delayed PPB rate inpatients on clopidogrel was
<1%, which was within acceptable ranges reported for the general
population not undergoing clopidogrel therapy. There was no
significant difference in the PPB rates between patients receiving
and not receiving clopidogrel (8).
However, a prospective study demonstrated that the rate of
immediate PPB (persistent bleeding observed at the time of
polypectomy) and delayed PPB was significantly higher in patients
on uninterrupted thienopyridines (9). Moreover, two meta-analyses both
demonstrated that continued clopidogrel therapy increased the risk
of delayed PPB and suggested deferring elective polypectomy until
it was safe to terminate clopidogrel therapy (10,11).
Therefore, the current guidelines recommend temporary cessation of
thienopyridine agents prior to high-risk endoscopic procedures,
such as polypectomy, but uninterrupted thienopyridines for low-risk
endoscopic procedures, such as biopsy (12,13).
However, a recent prospective observational study showed that the
risk of early major cardiac adverse events was increased to 7.04
following the cessation of antiplatelet agents, and was highest in
the first 7 days (14). In addition,
a meta-analysis revealed a notably high risk of major cardiac
adverse events following the interruption of antiplatelet therapy
in patients with coronary stents [odds rate (OR), 89.78; 95%
confidence interval (CI), 29.9-269.6] (15). Interestingly, the most recent
prospective study reported that patients on continued clopidogrel
had a slightly higher incidence rate of immediate and delayed PPB
compared with those on discontinued clopidogrel; however, this
difference was not statistically significant (16). This observation could be challenged
with guidelines and by most gastroenterologists (17).
Overall, the management of medications in the
periprocedural period lacks sufficient data and guidelines
(18). Thus, a meta-analysis was
performed to assess the risks of immediate and delayed PPB
associated with the continued use of clopidogrel during colonoscopy
and polypectomy, based on the available medical literature.
Materials and methods
Search strategy
A systemic search was conducted via the PubMed
(https://www.ncbi.nlm.nih.gov/pubmed/), Web of Science
(http://webofscience.com) and Cochrane library
(https://www.cochranelibrary.com/)
databases to identify available publications, in order to compare
PPB rates in patients on continued or discontinued clopidogrel. The
keywords used are listed: ‘clopidogrel or thienopyridine’ and
‘colonoscopy or polypectomy’. A manual search for additional
relevant publications was also conducted by screening the included
studies. This study was performed in accordance with the Preferred
Reporting Items for Systematic Reviews and Meta-Analysis guidelines
(19). This study was registered in
PROSPERO (no. CRD42018118325).
Inclusion and exclusion criteria
The inclusion criteria were as follows: i)
Randomized controlled trials (RCTs) and retrospective cohort or
case-control studies reported in English; ii) patients on continued
clopidogrel and non-clopidogrel undergoing colonoscopic
polypectomy; iii) defining immediate PPB as bleeding at the time of
polypectomy; iv) defining delayed PPB as bleeding occurring as late
as 4 weeks or 30 days after the procedure [in the present study,
delayed PPB was considered to be clinically significant delayed
PPB, which included hemodynamic instability and a hemoglobin drop
of at least 2 g/l, hospitalization, packed red cell transfusion,
endoscopy intervention or surgery (20)]; v) patients receiving concomitant
aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs);
and vi) patients who had had their clopidogrel discontinued for
>5 days were included and placed in the non-clopidogrel group.
The exclusion criteria were as follows: i) Patients receiving
concomitant anticoagulant medication, such as warfarin and heparin;
and ii) patients who were not taking clopidogrel on the day of the
polypectomy, or in whom polypectomy was not performed.
Outcomes
The primary outcome was the incidence of
colonoscopic PPB inpatients on continued clopidogrel and those who
received interrupted antiplatelet therapy. The secondary outcomes
were immediate PPB, delayed PPB and serious cardio-thrombotic
events.
Quality assessment
Quality assessment was independently carried out by
three reviewers, according to the Newcastle-Ottawa Scale (NOS)
(21) for retrospective case-control
studies and the Jadad Scale (22)
for prospective controlled trials. Total scores of 0-3, 4-5 and 6-8
corresponded to low, moderate and high quality in the retrospective
case-control studies, respectively. Good trials had a score of 3-5,
whereas total scores of 0-2 corresponded to poor trials in
RCTs.
Statistical analysis
All pooled data were analyzed with Review Manager
5.3 software (Cochrane Informatics and Knowledge Management
Department, http://tech.cochrane.org/revman/download). Dichotomous
variables were expressed as a risk ratio (RR) with a 95% CI. The
χ2 test and I2 test were used to test
heterogeneity, and a value of 25, 50 or 75% suggested low, moderate
and high heterogeneity, respectively. The random-effects model was
used for high heterogeneity; otherwise, the fixed-effects model was
used (23). A two-sided P<0.05
was considered to indicate a statistically significant difference.
A funnel plot for colonoscopic PPB, immediate PPB and delayed PPB
was generated to assess the body of literature for publication
bias.
Results
Search results
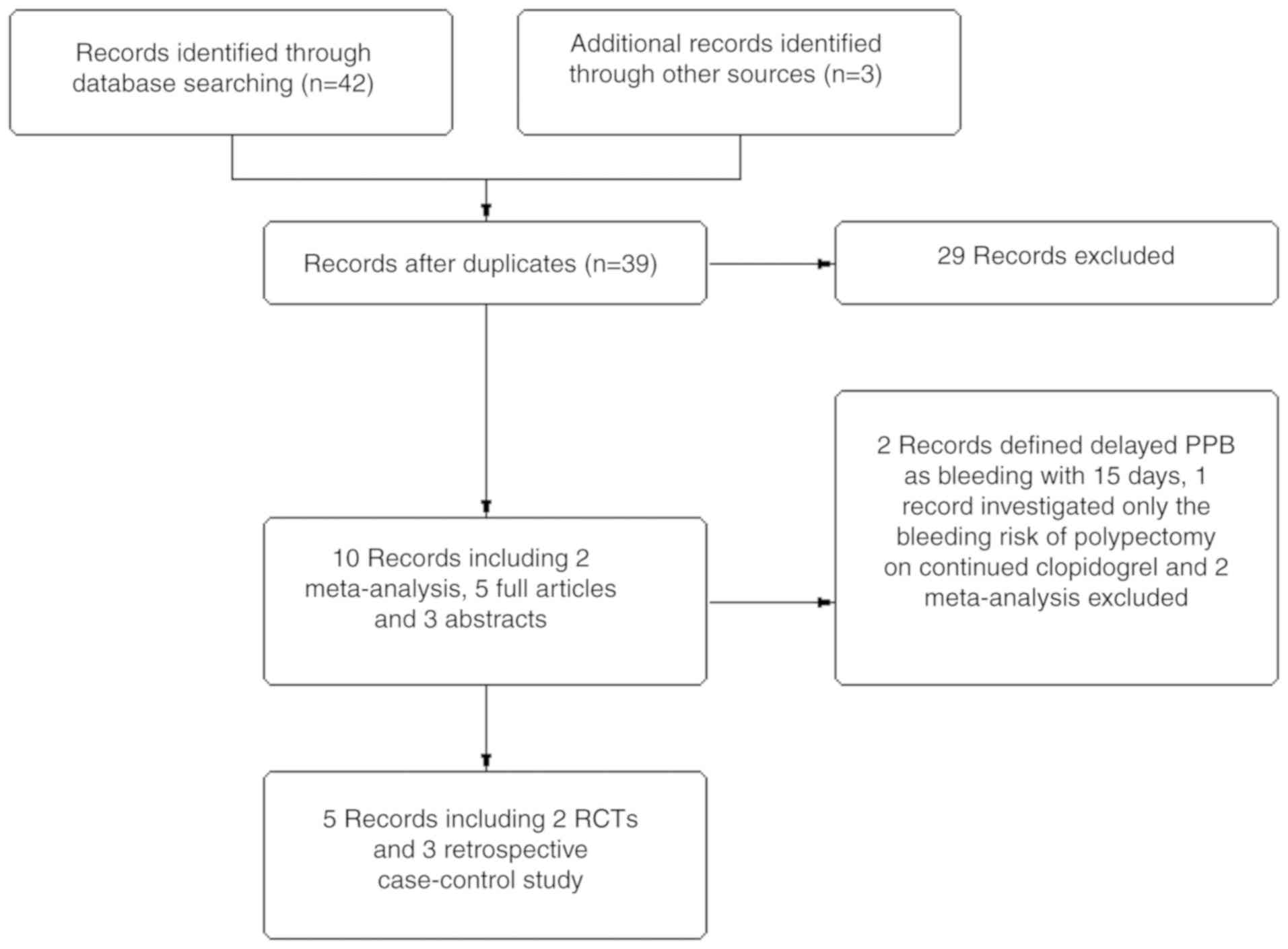
A total of 42 studies were identified by the present
search strategy, of which 39 were complete articles and three were
abstracts. A total of 10 studies, including two meta-analyses, five
complete articles and three abstracts that assessed PPB rates in
patients on continued clopidogrel met the inclusion criteria;
however, two abstracts defined delayed PPB as bleeding within 15
days after polypectomy, one complete article investigated only the
bleeding risk of polypectomy in patients on clopidogrel, and two
meta-analysis articles were excluded. In total, four complete
articles and one abstract, containing two prospective controlled
trials, and three retrospective case-control studies were included
in the present meta-analysis (Fig.
1).
Characteristics of included
studies
Five eligible studies (Table I) reported on 7,275 patients
undergoing colonoscopy with polypectomy, of whom 655 patients
(9.0%) were in the continued clopidogrel group and 6,620 patients
(91%) were in the control group. In the study by Singh et al
(6), which included 142 patients on
continued clopidogrel and 1,243 patients not on clopidogrel, 54% of
patients on continued clopidogrel also received concomitant aspirin
treatment, and 32% of patients in the control group were taking
aspirin. The rate of immediate PPB was similar in both groups;
however, the rate of delayed PPB was higher in the continued
clopidogrel group. The study by Grossman et al (24) was published as a conference abstract,
which included 70 patients taking clopidogrel only and 3,121
patients on non-clopidogrel therapy. Patients on continued
clopidogrel demonstrated increased risk of both immediate and
delayed PPB. In the study by Feagins et al (8), containing 118 patients on clopidogrel
and 1,849 patients not taking clopidogrel, concomitant aspirin use
was prevalent in 78.8% of clopidogrel users compared with 27.9% of
the control group. It was found that continued clopidogrel did not
increase the rate of delayed PPB. The Feagins et al
(9) study was a prospective trial
including 219 patients receiving clopidogrel and 297 patients not
receiving clopidogrel; most of the patients were receiving
concomitant aspirin. It was demonstrated that only delayed PPB was
elevated in the continued clopidogrel group. The study by Chan
et al (16) was also a
prospective trial, including 226 patients treated with clopidogrel
alone or in combination with other anti-platelet medications (e.g.
aspirin). Of these patients, 106 received uninterrupted clopidogrel
and 110 received a 7-day interruption of clopidogrel. It was
demonstrated that continued clopidogrel resulted in a small
increase in immediate and delayed PPB; however, this difference was
not statistically significant.
 | Table ICharacteristics of included
studies. |
Table I
Characteristics of included
studies.
| Author, year | Study type | Patients with
polypectomy, n | Clopidegrol and
ASA/NSAIDs users, n (%) | Non-clopidegrol and
ASA/NSAIDs users, n (%) | Clopidegrol users
with bleed, n (%) | Non-Clopidegrol
users with bleed, n (%) | (Refs.) |
|---|
| Singh et al,
2010 | RCC | 3,601 | 142 (10.3%); 77
(54.0%); 14 (9.8%) | 1,243 (89.7%); 398
(32.0%); 170 (13.7%) | 3/142 (2.1%)
Immediate; 5/142 (3.5%) Delayed | 26/1,243 (2.1%)
Immediate; 12/1,243 (1.0%) Delayed | (6) |
| Feagins et
al, 2011 | RCCb | 6,031 | 118 (6.0%); 93
(78.8%); 9 (7.6%) | 1,849 (94%); 515
(27.9%), 271 (14.7%) | N/A Immediate;
1/118 (0.8%) Delayed | N/A Immediate;
6/1,849 (0.3%) Delayed | (8) |
| Feagins et
al, 2013 | RCT | 1,732 | 219 (42.4%); 192
(87.7%); 25 (11.5%) | 297 (57.6%); 119
(40.1%); 40 (13.5%) | 16/219 (7.3%)
Immediate; 5/210 (2.4%) Delayed | 14/297 (4.7%)
Immediate; 0/286 Delayed | (9) |
| Chan et al,
2019 | RCTa | 449 | 106 (48.8%); 84
(79.2%); N/A | 111 (52.2%); 86
(78.2%); N/A | 9/106 (8.5%)
Immediate; 4/106 (3.8%) Delayed | 6/110 (5.5%)
Immediate; 4/110 (3.6%) Delayed | (16) |
| Grossman et
al, 2010 | RCC | 3,191 | 70 (2.2%); N/A;
N/A | 3,121 (97.8%); 627
(20.1%); 90 (2.9%) | 3/70 (4.3%)
Immediate; 3/70 (4.3%) Delayed | 38/3121 (1.2%)
Immediate 33/3121 (1.1%) Delayed | (24) |
| Total | | 15004 | 655 | 6620 | 49 | 139 | |
Quality of included studies
Jadad scores and Newcastle-Ottawa scores for 2 RCTs
and 3 retrospective case-control studies are shown in Tables II and
III, respectively. All studies were scored as high quality.
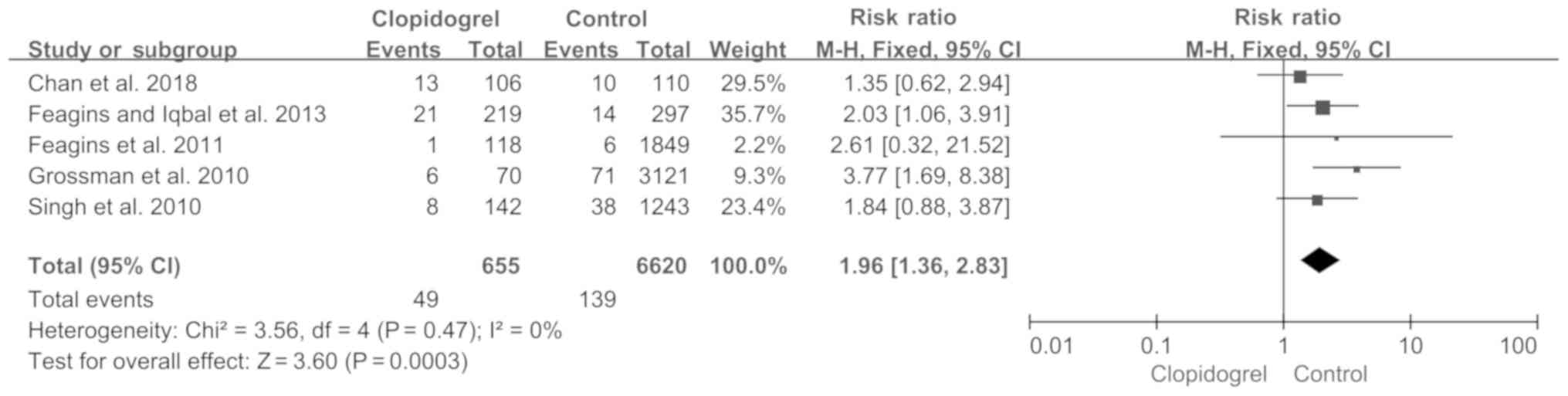
Colonoscopic PPB
A total of five studies met the inclusion criteria
and were eventually selected for analysis. The pooled PPB rate was
calculated using a fixed-effect model, as the heterogeneity was not
significantly different among these studies (P=0.47; I2,
0%; Fig. 2). Based on the data of
655 patients on continued clopidogrel (49/655) and 6,620 patients
in the control group (139/6,620), the RR of PPB increased to 1.96
in the continued clopidogrel group (P=0.0003; 95%CI, 1.36-2.83;
Fig. 2).
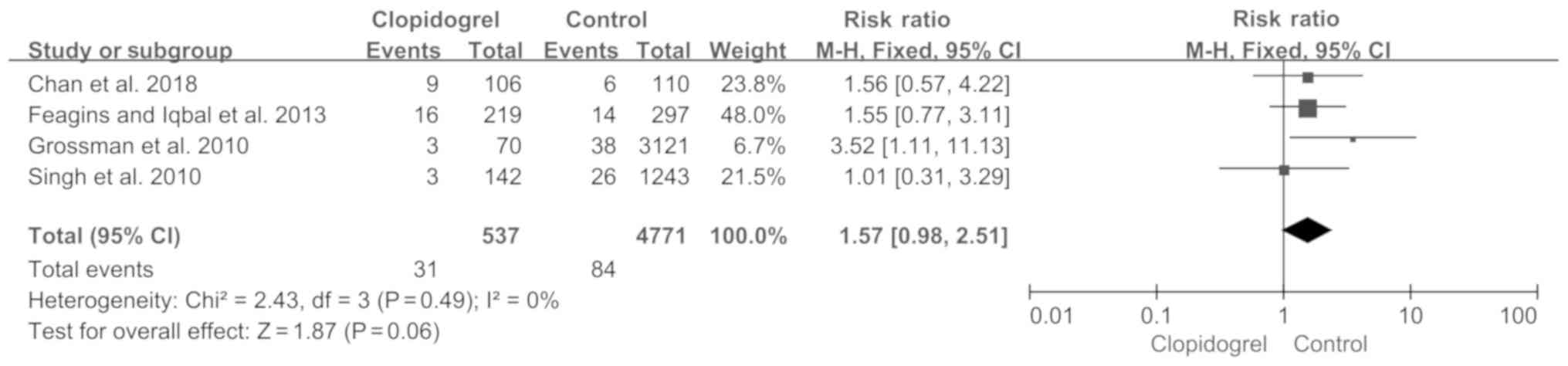
Immediate PPB
Four studies measured immediate PPB, where a total
of 31/537 patients on continued clopidogrel and 84/4,771 patients
not receiving clopidogrel developed immediate PPB. The immediate
PPB rate was slightly higher in the continued clopidogrel group
(5.77%) compared with the control group (1.77%); however, this was
not significant (fixed-effect model; P=0.06; RR, 1.57; 95%CI
0.98-2.51) and there was no heterogeneity (P=0.49; I2,
0%; Fig. 3).
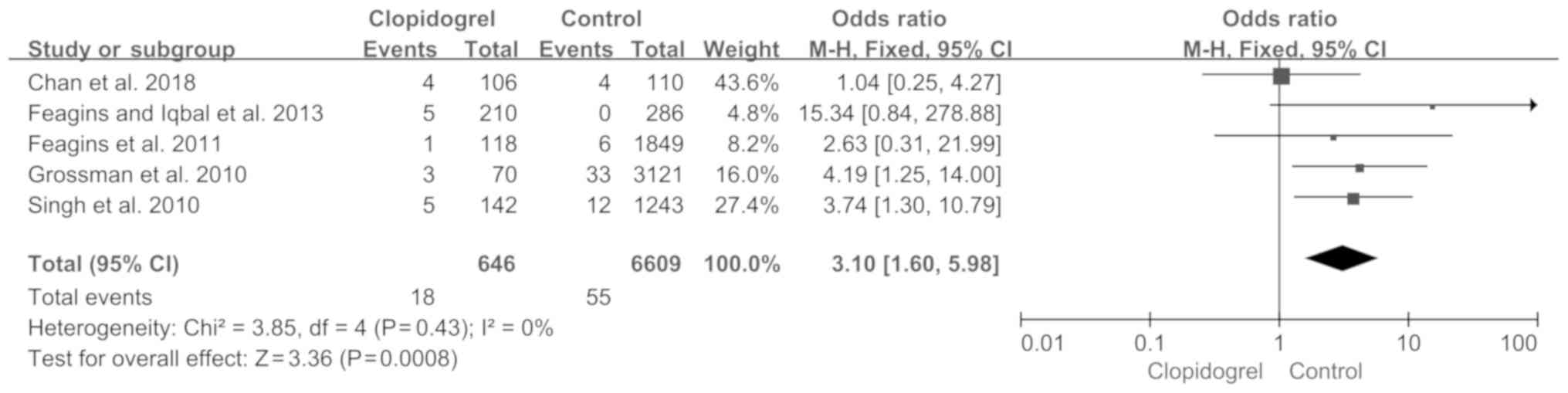
Delayed PPB
A total of five studies reported delayed PPB. As
shown in Fig. 4, the pooled RR of
the delayed PPB was increased to 3.10 (P=0.0008; 95%CI, 1.60-5.98),
based on a fixed-effects model with no heterogeneity (P=0.43;
I2, 0%).
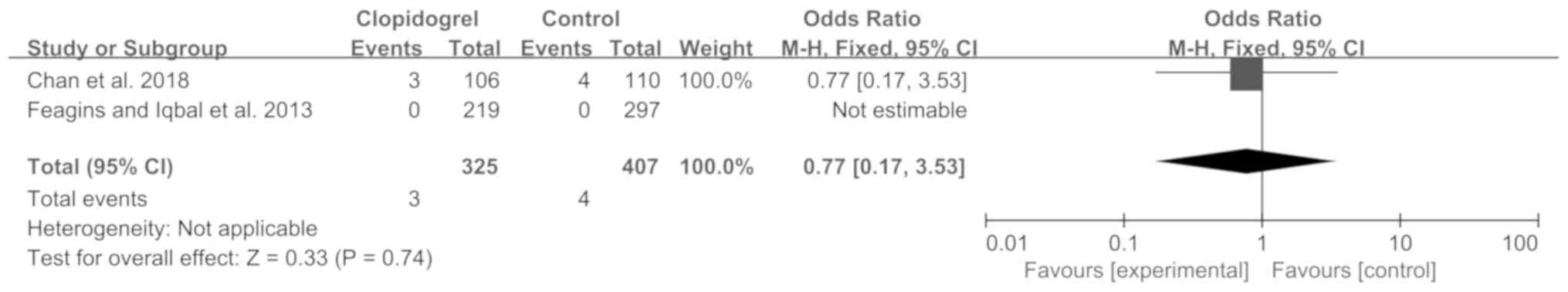
Serious cardio-thrombotic events
Only two studies assessed serious cardio-thrombotic
events, which were observed in 3 out of 325 patients on clopidogrel
(0.92%) compared with 4 out of 407 patients (0.98%) in the control
group, with a non-significant pooled RR of 0.78 within 30 days
(P=0.74; 95%CI, 0.18-3.40; Fig.
5).
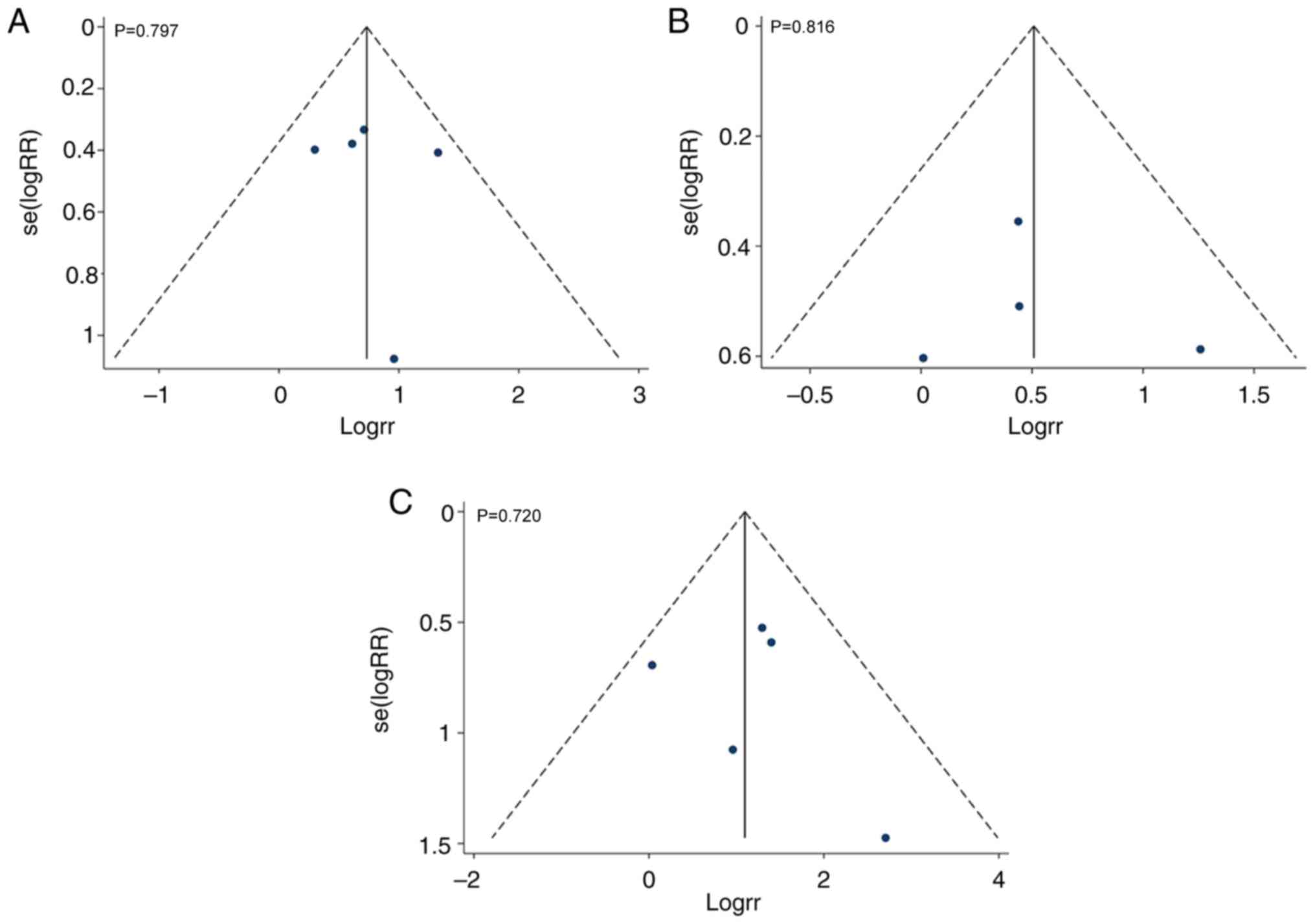
Publication bias
There was no publication bias in colonoscopic PPB,
immediate PPB and delayed PPB demonstrated by funnel plot analysis
(P=0.797, P=0.816 and P=0.720, respectively; Fig. 6).
Discussion
Colorectal cancer (CRC) ranks third in terms of
incidence but second in terms of mortality of all cancer types in
the USA (25). It is estimated that
there will be 140,250 new cases and 50,630 deaths in the United
States in 2018(25). Currently, the
preferred modality for detection and prevention of CRC is an
endoscopic procedure every 10 years, beginning at 50 years of age.
However, most patients with known heart disease are over 50 years
and are taking clopidogrel and other thienopyridines (26). Active antiplatelet therapy
complicates colorectal detection by increasing the risk of
complications, including PPB. Interruption of antiplatelet therapy
may pose a high thrombosis risk and be associated with high
mortality inpatients during endoscopic procedures, particularly
polypectomy (27). In the present
study, a meta-analysis was performed to estimate the rate of PPB in
patients on continued clopidogrel.
The results of the present study demonstrated that
continued clopidogrel increased the occurrence of delayed PPB,
which is consistent with the current guidelines and previously
published meta-analyses (10,11).
However, one published meta-analysis included only one prospective
controlled trial and four retrospective case-control studies, and
the definition of delayed PPB was inconsistent between these
studies; four studies defined delayed PPB as bleeding within 4
weeks, whereas another study defined it as bleeding within 15 days,
indeed, this inconsistency may affect the accuracy of the results
and publication bias was not assessed (10). Another published meta-analysis
included only two retrospective case-control studies; however, one
study defined delayed PPB as bleeding within 15 days after
polypectomy (11). In the present
meta-analysis, two prospective controlled trials and three
retrospective case-control studies were included, delayed PPB was
defined as bleeding within 4 weeks or 30 days after
post-polypectomy, and all patients who were receiving concomitant
aspirin or other NSAIDs were included. Therefore, the present study
evaluated the rate of PPB more rigorously. To the best of our
knowledge, the present study is the first to demonstrate that
continued clopidogrel therapy did not increase the number of
serious cardio-thrombotic events.
A number of limitations remain in this
meta-analysis. The first major limitation was the small number of
RCTs, which may limit the statistical power of these findings. The
present study demonstrated that continued clopidogrel therapy did
not increase the number of serious cardio-thrombotic events, which
was inconsistent with previous publications (14,15), and
thus required further confirmation. Secondly, the present study
included three retrospective case-control studies, which can lead
to selection bias. Thirdly, patient-associated factors contributing
to PPB have been described, such as increased age (28), chronic renal disease (28), coronary artery disease (CAD)
(29) and hypertension (30). In the present study, the patients on
clopidogrel were older and had more comorbidities than the
non-clopidogrel users, and this difference contributed to elevated
rates of PPB in the continued clopidogrel group. Furthermore,
polyp- and procedure-associated risk factors, such as polyp size
(31,32), polyp location (31,32), the
number of removed polyps (33),
endoscopists experience (32,34) and
removal modality (28), were
associated with the rate of PPB. However, these factors were not
considered in the present study, due to limited data. Moreover,
because endoscopists were not blinded during polypectomy in the
study, prophylactic clip placement was routinely applied after
polypectomy, which could decrease the PPB rate in the clopidogrel
group (18,28). Parikh et al (35) suggested that the prophylactic clip
placement may be cost-effective for patients on clopidogrel therapy
following polypectomy. However, 2 randomized controlled trials and
1 meta-analysis showed that preventative clip placement did not
significantly benefit patients receiving thienopyridines (36-38).
The present study does not discriminate the effect of concomitant
aspirin or NSAID therapy. A meta-analysis showed that the rate of
delayed PPB was elevated in patients on clopidogrel therapy, who
were also receiving other anti-platelet medicines, compared with
non-clopidogrel users (11).
However, a retrospective case control study did not yield similar
results (39). Finally, whether
resuming antiplatelet agents may increase the rate of delayed PPB
after polypectomy remains in question. A retrospective case control
study showed that resuming the intake of antithrombotics earlier
(within 1 week) can elevate the rate of delayed PPB (39). At present, little data have been
published on this subject.
Despite these limitations, the present study also
offers some important implications for clinical practice. The
effect of continued clopidogrel therapy on serious
cardio-thrombotic events, compared with discontinued clopidogrel,
requires further study. However, the present study showed that the
rates of immediate PPB and delayed PPB in patients on continued
clopidogrel were 5.77 and 2.78%, respectively. Moreover, although
the rate of PPB was significantly higher in the continued
clopidogrel group, it was controlled adequately by blood
transfusions and repeat colonoscopy, and no patients died or
required surgery. However, these treatments could also increase the
economic burden of medical health care. The findings of the present
study suggested that endoscopists should prepare to prevent
bleeding in the perioperative period, in the event that polypectomy
cannot be reasonably postponed and clopidogrel therapy could not be
interrupted.
Acknowledgements
The authors would like to thank Professor Yu-Qiang
Nie (Guangzhou First People's Hospital, Guangzhou Medical
University) for their support with the methods and Professor Wei
Fan (Cedars-Sinai Medical Center) for revising the manuscript.
Funding
This study was supported by Natural Science
Foundation of Hunan Province (grant no. 2017JJ3270), Natural
Science Foundation of Guangdong Province (grant no.
2018A0303100024), Three Engineering Training Funds in Shenzhen
(grant nos. SYLY201718, SYJY201714 and SYLY201801) and Technical
Research and Development Project of Shenzhen (grant no.
JCYJ20150403101028164).
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
DL, XC, LW and JY designed the study and reviewed
the manuscript. DL and XC drafted the manuscript and performed
statistical analysis. JW, ZY, CW, FX, XF and ZX, screened for
literature and assessed the quality of studies. DZ, TL and ML
retrieved the data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kim AS and Johnston SC: Global variation
in the relative burden of stroke and ischemic heart disease.
Circulation. 124:314–323. 2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Writing Group Members. Mozaffarian D,
Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de
Ferranti S, Després JP, et al: Executive summary: Heart disease and
stroke statistics-2016 update: A report from the American heart
association. Circulation. 133:447–454. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rosen L, Bub DS, Reed JF III and Nastasee
SA: Hemorrhage following colonoscopic polypectomy. Dis Colon
Rectum. 36:1126–1131. 1993.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Reaume KT, Regal RE and Dorsch MP:
Indications for dual antiplatelet therapy with aspirin and
clopidogrel: Evidence-based recommendations for use. Ann
Pharmacother. 42:550–557. 2008.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Spertus JA, Kettelkamp R, Vance C, Decker
C, Jones PG, Rumsfeld JS, Messenger JC, Khanal S, Peterson ED, Bach
RG, et al: Prevalence, predictors, and outcomes of premature
discontinuation of thienopyridine therapy after drug-eluting stent
placement: Results from the PREMIER registry. Circulation.
113:2803–2809. 2006.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Singh M, Mehta N, Murthy UK, Kaul V, Arif
A and Newman N: Postpolypectomy bleeding in patients undergoing
colonoscopy on uninterrupted clopidogrel therapy. Gastrointest
Endosc. 71:998–1005. 2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Carter D, Beer-Gabel M, Eliakim R, Novis
B, Avidan B and Bardan E: Management of antithrombotic agents for
colonoscopic polypectomies in Israeli gastroenterologists relative
to published guidelines. Clin Res Hepatol Gastroenterol.
37:514–518. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Feagins LA, Uddin FS, Davila RE, Harford
WV and Spechler SJ: The rate of post-polypectomy bleeding for
patients on uninterrupted clopidogrel therapy during elective
colonoscopy is acceptably low. Dig Dis Sci. 56:2631–2638.
2011.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Feagins LA, Iqbal R, Harford WV, Halai A,
Cryer BL, Dunbar KB, Davila RE and Spechler SJ: Low rate of
postpolypectomy bleeding among patients who continue thienopyridine
therapy during colonoscopy. Clin Gastroenterol Hepatol.
11:1325–1332. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Gandhi S, Narula N, Mosleh W, Marshall JK
and Farkouh M: Meta-analysis: Colonoscopic post-polypectomy
bleeding in patients on continued clopidogrel therapy. Aliment
Pharmacol Ther. 37:947–952. 2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Shalman D and Gerson LB: Systematic review
with meta-analysis: The risk of gastrointestinal haemorrhage
post-polypectomy in patients receiving anti-platelet,
anti-coagulant and/or thienopyridine medications. Aliment Pharmacol
Ther. 42:949–956. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kato M, Uedo N, Hokimoto S, Ieko M,
Higuchi K, Murakami K and Fujimoto K: Guidelines for
gastroenterological endoscopy in patients undergoing antithrombotic
treatment: 2017 appendix on anticoagulants including direct oral
anticoagulants. Dig Endosc. 30:433–440. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Chan FKL, Goh KL, Reddy N, Fujimoto K, Ho
KY, Hokimoto S, Jeong YH, Kitazono T, Lee HS, Mahachai V, et al:
Management of patients on antithrombotic agents undergoing
emergency and elective endoscopy: Joint Asian Pacific Association
of Gastroenterology (APAGE) and Asian Pacific Society for Digestive
Endoscopy (APSDE) practice guidelines. Gut. 67:405–417.
2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Mehran R, Baber U, Steg PG, Ariti C, Weisz
G, Witzenbichler B, Henry TD, Kini AS, Stuckey T, Cohen DJ, et al:
Cessation of dual antiplatelet treatment and cardiac events after
percutaneous coronary intervention (PARIS): 2 year results from a
prospective observational study. Lancet. 382:1714–1722.
2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Eisenberg MJ, Richard PR, Libersan D and
Filion KB: Safety of short-term discontinuation of antiplatelet
therapy in patients with drug-eluting stents. Circulation.
119:1634–1642. 2009.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chan FKL, Kyaw MH, Hsiang JC, Suen BY, Kee
KM, Tse YK, Ching JYL, Cheong PK, Ng D, Lam K, et al: Risk of
postpolypectomy bleeding with uninterrupted clopidogrel therapy in
an industry-independent, double-blind, randomized trial.
Gastroenterology. 156:918–925. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Plumé Gimeno G, Bustamante-Balén M,
Satorres Paniagua C, Díaz Jaime FC and Cejalvo Andújar MJ:
Endoscopic resection of colorectal polyps in patients on
antiplatelet therapy: An evidence-based guidance for clinicians.
Rev Esp Enferm Dig. 109:49–59. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Abdel Samie A, Theilmann L and Labenz J:
ALGK : Endoscopic procedures in patients under clopidogrel or dual
antiplatelet therapy: A survey among German gastroenterologists and
current guidelines. Z Gastroenterol. 52:425–428. 2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Liberati A, Altman DG, Tetzlaff J, Mulrow
C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J
and Moher D: The PRISMA statement for reporting systematic reviews
and meta-analyses of studies that evaluate health care
interventions: Explanation and elaboration. Ann Intern Med.
151:W65–W94. 2009.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Nelson DB, McQuaid KR, Bond JH, Lieberman
DA, Weiss DG and Johnston TK: Procedural success and complications
of large-scale screening colonoscopy. Gastrointest Endosc.
55:307–314. 2002.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Stroup DF, Berlin JA, Morton SC, Olkin I,
Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA and Thacker
SB: Meta-analysis of observational studies in epidemiology: A
proposal for reporting. Meta-analysis Of Observational Studies in
Epidemiology (MOOSE) group. JAMA. 283:2008–2012. 2000.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Jadad AR, Moore RA, Carroll D, Jenkinson
C, Reynolds DJ, Gavaghan DJ and McQuay HJ: Assessing the quality of
reports of randomized clinical trials: Is blinding necessary?
Control Clin Trials. 17:1–12. 1996.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Higgins JP, Thompson SG, Deeks JJ and
Altman DG: Measuring inconsistency in meta-analyses. BMJ.
327:557–560. 2003.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Grossman EB, Maranino AN, Zamora DC, et
al: Antiplatelet Medications Increase the Risk of Post-Polypectomy
Bleeding. GastrointestEndosc. 71(AB138)2010.
|
|
25
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2018. CA Cancer J Clin. 68:7–30. 2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Zhao D, Liu J, Wang M, Zhang X and Zhou M:
Epidemiology of cardiovascular disease in China: Current features
and implications. Nat Rev Cardiol. 16:203–212. 2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Iakovou I, Schmidt T, Bonizzoni E, Ge L,
Sangiorgi GM, Stankovic G, Airoldi F, Chieffo A, Montorfano M,
Carlino M, et al: Incidence, predictors, and outcome of thrombosis
after successful implantation of drug-eluting stents. JAMA.
293:2126–2130. 2005.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Kim HS, Kim TI, Kim WH, Kim YH, Kim HJ,
Yang SK, Myung SJ, Byeon JS, Lee MS, Chung IK, et al: Risk factors
for immediate postpolypectomy bleeding of the colon: A multicenter
study. Am J Gastroenterol. 101:1333–1341. 2006.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Sawhney MS, Salfiti N, Nelson DB, Lederle
FA and Bond JH: Risk factors for severe delayed postpolypectomy
bleeding. Endoscopy. 40:115–119. 2008.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Watabe H, Yamaji Y, Okamoto M, Kondo S,
Ohta M, Ikenoue T, Kato J, Togo G, Matsumura M, Yoshida H, et al:
Risk assessment for delayed hemorrhagic complication of colonic
polypectomy: Polyp-related factors and patient-related factors.
Gastrointest Endosc. 64:73–78. 2006.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Rutter MD, Nickerson C, Rees CJ, Patnick J
and Blanks RG: Risk factors for adverse events related to
polypectomy in the English Bowel Cancer Screening Programme.
Endoscopy. 46:90–97. 2014.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Choung BS, Kim SH, Ahn DS, Kwon DH, Koh
KH, Sohn JY, Park WS, Kim IH, Lee SO, Lee ST and Kim SW: Incidence
and risk factors of delayed postpolypectomy bleeding: A
retrospective cohort study. J Clin Gastroenterol. 48:784–789.
2014.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Heldwein W, Dollhopf M, Rösch T, Meining
A, Schmidtsdorff G, Hasford J, Hermanek P, Burlefinger R, Birkner
B, Schmitt W, et al: The Munich Polypectomy Study (MUPS):
Prospective analysis of complications and risk factors in 4000
colonic snare polypectomies. Endoscopy. 37:1116–1122.
2005.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Rabeneck L, Paszat LF, Hilsden RJ, Saskin
R, Leddin D, Grunfeld E, Wai E, Goldwasser M, Sutradhar R and
Stukel TA: Bleeding and perforation after outpatient colonoscopy
and their risk factors in usual clinical practice.
Gastroenterology. 135:1899–1906.e1891. 2008.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Parikh ND, Zanocco K, Keswani RN and
Gawron AJ: A cost-efficacy decision analysis of prophylactic clip
placement after endoscopic removal of large polyps. Clin
Gastroenterol Hepatol. 11:1319–1324. 2013.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Matsumoto M, Kato M, Oba K, Abiko S, Tsuda
M, Miyamoto S, Mizushima T, Ono M, Omori S, Takahashi M, et al:
Multicenter randomized controlled study to assess the effect of
prophylactic clipping on post-polypectomy delayed bleeding. Dig
Endosc. 28:570–576. 2016.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Boumitri C, Mir FA, Ashraf I,
Matteson-Kome ML, Nguyen DL, Puli SR and Bechtold ML: Prophylactic
clipping and post-polypectomy bleeding: A meta-analysis and
systematic review. Ann Gastroenterol. 29:502–508. 2016.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Dokoshi T, Fujiya M, Tanaka K, Sakatani A,
Inaba Y, Ueno N, Kashima S, Goto T, Sasajima J, Tominaga M, et al:
A randomized study on the effectiveness of prophylactic clipping
during endoscopic resection of colon polyps for the prevention of
delayed bleeding. Biomed Res Int. 2015(490272)2015.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Lin D, Soetikno RM, McQuaid K, Pham C,
Doan G, Mou S, Shergill AK, Somsouk M, Rouse RV and Kaltenbach T:
Risk factors for postpolypectomy bleeding in patients receiving
anticoagulation or antiplatelet medications. Gastrointest Endosc.
87:1106–1113. 2018.PubMed/NCBI View Article : Google Scholar
|