Introduction
Osteoporosis is a common disease in the elderly, and
its incidence continues to rise. With the aging of the population
in China, there are increasing number of patients with
osteoporosis. For spinal surgeons, internal fixation (1) is a routine treatment for osteoporosis
requiring nerve decompression and instrumented fusion such as
posterior lumbar interbody fusion (PLIF), which enables successful
fusion of the spine. The posterior spinal instrumentation subjects
the pedicle screw-bone interface to greater stress and affects the
stability of the pedicle screw. A number of studies have shown that
the stability of pedicle screws depends on the quality of the bone,
so patients with osteoporosis are more prone to instrumentation
failure (2-4). At
present, fatigue tests and withdrawal force testing of screws at
different bone densities indicate that the quality of the compact
trabecular bone enhances firm fixation of the screws, and
osteoporosis increases the failure rate of the internal fixation
(5-10).
The cement-reinforced [e.g. polymethylmethacrylate (PMMA) or
calcium-based bone cement] pedicle screw technology can enhance the
stability of the internal fixation system. However, after the bone
cement is strengthened, loosening of the screws may occur
again.
In order to address this problem, a new type of
spine-expansion pedicle screw was invented by Lei and Wu (11). According to a large number of
experimental studies on the biomechanics of animal vertebral
specimens, it was found that the axial withdrawal force of the new
expandable pedicle screws is significantly enhanced compared with
the conventional pedicle screw. In a large number of intact animal
experiments (12), the new
expandable pedicle screws and bone formed a staggered structure,
which increased the stability of the screw. This type of expansion
screw has been shown to be safe, effective, and practical through
biomechanical testing, imaging evaluation, and epidemiological
investigation (13). The expansion
screw has obtained a number of patents and is used in clinical
practice (14). Following the
development of the expansion screw, we also developed a composite
screw-bone cement anchor bolt, and biomechanical and animal
experiments have proven that this new bone cement screw has good
fixation strength and low cement leakage rate (15), but it is not effective for complex
osteoporosis. We therefore established a three-dimensional frame
structure to ensure stability. This study analyzed the stability of
a three-dimensional frame structure based on cemented screw
reinforcement through biomechanical testing.
Materials and methods
Screws and augmentation materials
A composite threaded bone cement anchoring screw
(Shandong Weigao Orthopedic Device Company) was used. The details
of the screw: diameter 6.5 mm x length 45 mm, proximal 9 threads,
distal 10 threads, total 19 threads. The thread density is
increased at the proximal end. At the distal end the depth of the
thread is increased, the pitch is increased, and a V-shaped nail is
present. The screw is hollow with an inner diameter of 1.6 mm. The
screw has a total of 6 side holes, with the side holes enlarged
from the proximal end to the distal end. The two apertures are
symmetrically distributed within one thread. Mendec Spine PMMA bone
cement is produced by TECRES. Denture base material resin type II
was used (self-curing denture acrylic: 100 g x 7 bottles and liquid
for denture acrylic 500 ml x 1 bottle) Shanghai Medical Devices
Co., Ltd. holding.
Specimen
Seven intact human spine specimens (T12-L5) from
people with an average age of 72 years were used. The bone mineral
density of the specimens was detected by dual energy X-ray
absorptiometry (DEXA method). The test results showed that all of
the specimens were osteoporotic.
The study was approved by the Ethics Committee of
Xijing Hospital (Xi’an, China), and written informed consents were
signed by the patients and/or the guardians.
Experimental apparatus.
Screw insertion devices including hole openers, hand
drills, nail holders, staple handles and other instruments were
provided by Shandong Weigao Orthopedic Device Co., Ltd. Digital
X-ray machines (Philips) and 64-row spiral CT (Picker PQ6000) were
provided by the Department of Radiology of the Fourth Military
Medical University. The biomechanical experimental instrument was a
microcomputer-controlled electronic universal testing machine,
provided by the Mechanics Laboratory of the Mechanical College of
Xi'an Jiaotong University.
Methods
Experimental grouping
Three specimens were separated into 18 vertebral
bodies for the biomechanical testing of a single screw. Nine
vertebral bodies were randomly selected and bone cement screws were
implanted on both sides. Bone cement was used to form a bridge at
the front end of the two screws (single vertebral group A).
The other nine vertebral bodies were implanted with
cement screws on both sides, but the front ends of the two screws
were not bridged (single vertebral group B).
The remaining spine specimens were used for
biomechanical testing of the overall stability of the
three-dimensional frame.
The four specimens were osteotomized, then two
specimens were randomly selected. Bone cement screws were implanted
on both sides of the vertebral body, and a bone cement bridge was
formed at the front end of the two screws to establish a
three-dimensional frame structure (multi-vertebral group A).
The other two spine specimens were implanted with
cement screws on both sides of the vertebral body, but the front
ends of the two screws were not bridged (multi-vertebral group B)
(Table I).
 | Table IExperimental grouping. |
Table I
Experimental grouping.
| Group | Group A | Group B |
|---|
| Single vertebral | 9 (triangular sTable
structure) | 9 |
| Multi-vertebral | 2 (three-dimensional
frame) | 2 |
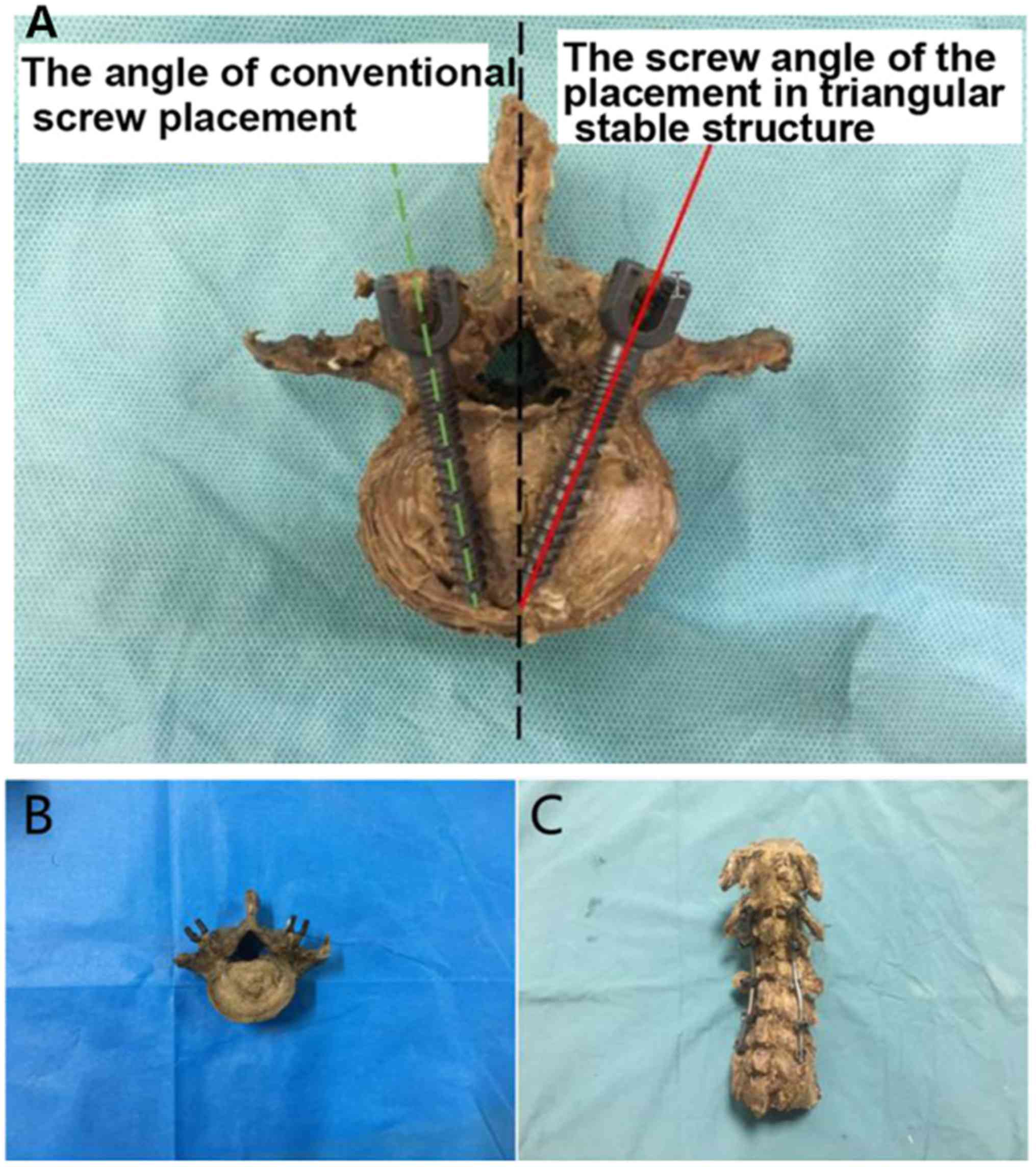
Screw placement. According to the standard
surgical procedure for this clinical operation, following the
herringbone crest vertex technique, the specimen was first fixed,
and an open cone was used to punch the vertex of the specimen at
the Herringbone crest vertex. A nail path was prepared with a depth
of 40 mm and perpendicular to the side of the specimen. A composite
threaded bone cement anchoring screw was inserted into the
cancellous bone of the specimen at an angle to the vertebral
specimen until the screw was fully screwed into the specimen.
During the screw placement process, the vertebral specimen should
be prevented from moving as that would destroy the structure. The
experimental vertebral specimens could not be pre-tapped to avoid
affecting the stability of the screws. The PMMA bone cement powder
and the water agent were uniformly mixed in the formulated ratio,
and the mixture was injected into the injection device during the
spinning period. During the cement injection process, the bone
cement flows out from the side holes and diffuses into the
cancellous bone around the screw. Attention should be paid to the
presence or absence of bone cement leakage from the rear end of the
screw. The above operations of screw placement were performed by a
clinically experienced spine surgeon. Following the methodology of
a previous study, all vertebral bodies were infused with 2.5 PMMA
for intensification, and the amount of bone cement in the hollow
part of the screw was subtracted (Fig.
1).
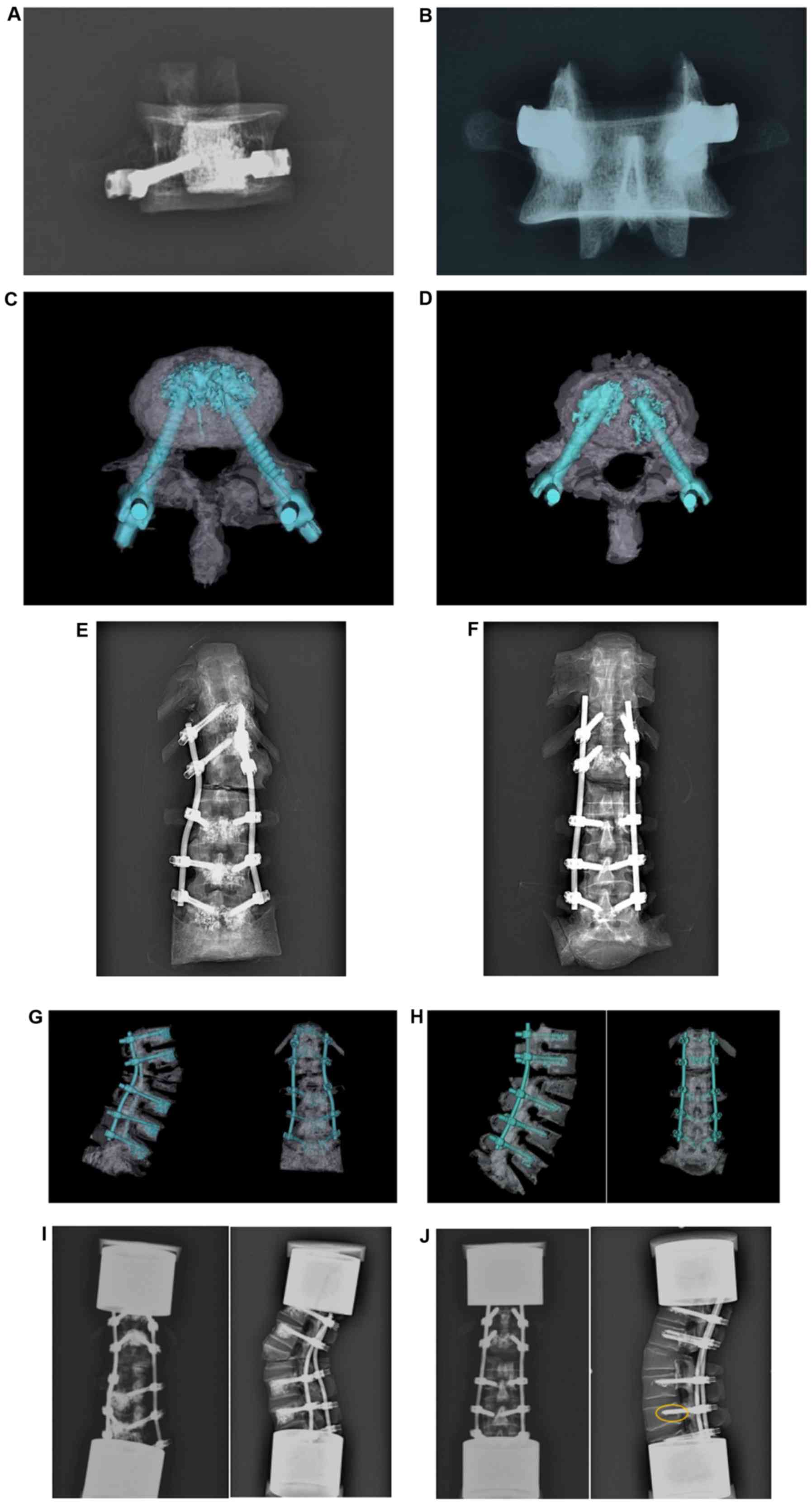
Radiographic evaluation. When the bone cement
screw placement and bone cement filling of the vertebral body
specimens was completed, the vertebral body specimens were allowed
to stand at room temperature for 24 h. After the bone cement in the
vertebral body specimen was completely solidified, CT scanning was
performed using an X-ray machine and 64-slice spiral CT (parameter:
200 mA, 130 KV, 1 mm slice thickness). In the later stage of the
experiment, the three-dimensional reconstruction of the bone cement
screw and the bone cement was performed using Mimics software, and
the positional relationship of the bone cement screw, the bone
cement and the cancellous bone of the vertebral body specimen was
observed. In this way, the shape of the bone cement in the
vertebral body, the position of the cement screw, and whether the
bone cement screw and the bone cement formed a bridge were
studied.
The axial withdrawal force test. The axial
pull-out force experiment was performed on a single vertebral
specimen with the help of a microcomputer-controlled electronic
universal testing machine. The vertebral body specimen was attached
to a special fixture, which was then fixed to the base of the
testing machine. The direction of the specimen was adjusted so that
the long axis direction of the bone cement screw was consistent
with the direction of the robot arm of the testing machine. The
arms and screw tails were secured by the upper clamp. The
extraction rate of the cement screw was set to a constant rate of 5
mm/min, and continued until the pull-out force decreased,
indicating that the cement screw was completely withdrawn. The
computer automatically recorded the load signal data of the test
machine and generated the load-displacement curve. The maximum
pullout strength (Fmax) of the cement screw was calculated by the
corresponding computer software (Fig.
2).
Cyclic loading test. Four spine specimens of
multiple vertebral bodies were embedded, and the lower end of the
spine specimen was trimmed, keeping the specimen erect and slightly
forward. The specimen was placed in an 8.6 cm-diameter embedding
tank, and embedded in a ratio of 2:1 with 100 g of a foundation
base material resin type II (self-curing denture acrylic) and 100
ml of liquid for denture acrylic. The specimen was kept up and down
horizontally for self-condensation. The specimen was then fixed on
a LETRY biomechanical fatigue testing machine. The upper end of the
specimen was fixed to the center of the groove of the embedding
block to provide an anterior flexion load for the test, and the
angle of the vise was adjusted to form the flexion angle required
for the cyclic load test. The fatigue testing machine was set to a
cyclic loading state with the following loading schedule: 3 h
total, cycle of 60/min, 10,000 revolutions, initial pressure of 300
N, peak pressure of 3,000 N, front flexion of 8˚ (Fig. 3).
Statistical analysis
The axial withdrawal force and cyclic load
experimental data were analyzed by SPSS 13.0 statistical software.
The measurement data were expressed as average ± standard deviation
(mean ± SD). Two independent sample t-tests were used for
comparison between groups. P<0.05 was considered statistically
significant.
Results
Imaging results
Through imaging analysis, all 9 specimens of the
single vertebral body group A were seen to have formed a triangular
stable structure by increasing the angle during the process of
screw placement. Nine specimens of the single vertebral body group
B were prepared according to the conventional screw placement and
did not have a front end bridge. In the multi-vertebral group A
(stereoscopic frame structure), the three-dimensional frame
structure was observed. The absence of obvious bone cement leakage
was confirmed by X-ray and CT three-dimensional reconstruction. The
multi-vertebral group B did not have a three-dimensional frame
structure (Fig. 4).
The result of maximal axial pull-out
strength test
The maximal pull-out force of the single-vertebral
group A, the screw front-end bridging group, was experimentally
measured as 1395.693±85.775. The maximal pull-out force of the
single-vertebral group B was 889.62±63.5. A statistically
significant difference (P<0.05) was found. The triangular
structure of the single vertebral body group A was stable, so the
maximum extraction force of the pedicle screw was higher.
The result of cyclic loading test
After the cyclic load test, the strain and
displacement of both groups increased, the stiffness decreased, and
the stability of the entire lumbar vertebra decreased. However, by
comparing the two groups, it was found that the screws of
multi-vertebral group A (stereoscopic frame) did not loosen
(Fig. 4I), while screw loosening
occurred in multi-vertebral group B (Fig. 4J). When compared with multi-vertebral
body group B, the stability of the spine in multi-vertebral group A
is better. As the cyclic loading force increases, this trend tends
to be obvious. The reason may be that an osteotomy specimen is used
for testing, which can more realistically simulate the clinical
situation. The biomechanical effects of the specimens are less
pronounced when subjected to smaller cyclic loads. As the cyclic
load increases, the influence becomes increasingly obvious,
resulting in the biomechanical instability of the spine and screw
loosening.
Discussion
An increasing challenge in spinal surgery is to
achieve optimal fixation of pedicle screws in poor bone conditions,
such as severe osteoporosis.
The restricted area is still a problem for some
patients with complex osteoporosis. In this study, the theory of
triangular stability of the single vertebral body was proposed, and
a three-dimensional framework structure was used to solve this
medical problem.
Studies have shown that under normal physiological
conditions, the various structures of the spine maintain their
normal positional relationship with each other and do not cause
compression and damage to the spinal cord or spinal nerve roots,
which is called ‘clinical stability’. When the spine loses this
function, it is termed ‘clinical instability’. The common method of
internal fixation cannot be used to sustain the stability of a
spine that is destroyed through serious osteoporosis and spinal
deformity.
This study proposes a theory that the triangular
stability of a single vertebral body and the three-dimensional
frame structure of multiple vertebral bodies can achieve the
stability of spinal internal fixation. The structure of internal
fixation used in clinical practice has been considered as a
quadrilateral structure of a single vertebral body. However, a
triangle is more stable compared with a quadrilateral when the edge
length and three angles of the triangle are fixed. As early as
1303, Zhu Shijie, an outstanding Chinese mathematician, published
this famous theory of triangles in his writing named Jade Mirror of
the Four Unknowns. When the two edges of a triangle are selected
randomly and the non-common endpoints of the two edges are
connected by the third side that is not flexible or bent, the
distance between the two ends and the angle between the two edges
is fixed. This is the explanation for the stability of a triangle.
If two adjacent edges of an n (n≥4)-sided polygon are selected
randomly, the non-common endpoints of the two sides are connected
by more than one edge. Therefore, the distance between the two
endpoints and the angle between the two edges is not fixed,
indicating that the n (n≥4)-sided polygon is unstable. In real
life, there are numerous buildings, designs and equipment using
triangles to achieve better stability. The frame of a bicycle,
fixing of doors and windows and the construction of buildings and
bridges, have all used the stability of triangles. In this study,
the triangular stability is used in the field of spinal internal
fixation to propose a theory of the triangular stability of a
single vertebral body and the three-dimensional frame structure of
multiple vertebral bodies.
The model was established through imaging analysis
of single vertebral triangular stability models and multiple
vertebral three-dimensional frame structure models, and the safe
dose of bone cement injection that was calculated using the finite
element model from previous experiments. By examining the X-ray and
CT three-dimensional reconstruction of the model, it could be seen
that the two bone cement screw front ends of the single vertebral
body were bridged and the multiple vertebral spine model had
established a three-dimensional frame structure, indicating that
the model was constructed successfully.
Patients with complex osteoporosis cannot be
operated on because of the loosening of screws. In addition, the
maximum axial pull-out strength of the spine is an important
indicator. Kiner et al (16)
compared the application of 8 mm diameter pedicle screws with
PMMA-enhanced 6 mm diameter pedicle screws in the vertebral body by
cyclic constant loading test. They found that the initial and final
stiffness of the larger diameter screws increased after cyclic
constant loading test. However, the 8 mm diameter pedicle screws
may be difficult to implant into all vertebral segments. Similarly,
Frankel et al (17) tested
the reconstructed thoracolumbar osteoporotic vertebral internal
fixation, and found that the cementation resulted in a 1.6-fold
increase in axial pull-out force. In addition, Moore et al
(18) and Renner et al
(19) both found that PMMA screw
reinforcement increased the axial pull-out force to 1.5 times the
normal pull-out force.
These studies have shown that there are two methods
to increase the axial pull-out strength of the screw. One is to
increase the diameter of the screw, which can make it difficult to
implant into all spinal segments. The other is to inject PMMA,
which can increase the maximum pull-out strength of the screw.
However, there is a risk of leakage if the amount of bone cement is
increased, and the pull-out strength of the screw will plateau when
the amount of bone cement reaches a certain dose value.
In this study, the front ends of the two screws were
bridged by controlling the angle of screw implantation and the
amount of bone cement. According to the experimental results, the
maximum pull-out strength of the single-vertebral group A, that is
the screw front-end bridging group, was 1395.693±85.775, and the
maximum pull-out strength of the single-vertebral group B was
889.62±63.5. The difference between the two groups was
statistically significant (P<0.05). The single vertebral body
group A was triangular stable, and the maximum pull-out strength of
the pedicle screw was stronger than that of group B, which made the
screw more stable.
The reason for patients with severe spinal deformity
having a surgical exclusion zone is that there is no strong, stable
internal fixation system to support the spine after surgery, and
structural stability is difficult to establish. Chiang et al
(20) isolated the lumbar vertebrae
and fractured vertebral bodies of three cadavers, and performed
vertebroplasty on the injured vertebral body alone or on the upper
level, applying cyclic compression force. When prophylactic
vertebroplasty was not performed in the vertebral segment, greater
height loss was observed in its vicinity. The authors hypothesized
that the non-reinforced vertebral body deformed more than the
articular surface, which resulted in increased bending moments and
greater height loss. Kebaish et al (21) used 18 spine specimens and managed
T10-L5 with internal fixation. In one group, the first fixed
segment of the uppermost of the segments to be internally fixed was
reinforced. The first fixed segment and the upper vertebral body of
the segment requiring internal fixation were cemented with bone
cement in all specimens. The reinforced and non-reinforced groups
were then compared, with vertical compression applied to both
experimental groups until the internal fixation failed. In the
non-reinforced group, the fracture rate at the proximal junction
was reduced by 33%. In the reinforced group, the fracture rate of
the proximal joint was reduced by 83%. In another study on internal
fixation biomechanics, Tan et al (22) confirmed that cement augmentation of
pedicle screws resulted in the most stable vertebral reconstruction
compared to a separate posterior screw-rod system, while flexible
rod extension minimized changes in range of motion at both adjacent
rod extension and distal non-instrumented levels. Finally, in a
finite element model of the posterior-lateral pedicle screw
structure of the short segment around a thoracolumbar burst
fracture, vertebroplasty reduces the stress applied to the screws
and rods (23).
Cement-reinforced pedicle screws clearly have an
effect on the vertebral body and biomechanical studies on the
spine. In addition to simple screw fixation, the factors of total
spinal stability should also be considered. It is important not
only to stabilize the pedicle screw of a single centrum, but also
to establish an effective internal fixation frame structure. This
study proposes a multi-vertebral space frame structure. A
three-dimensional frame spine model was established and a
controlled cyclic loading experiment was performed on a LETRY
biomechanical fatigue testing machine. In this study, the
three-dimensional frame spine model was subjected to cyclic loading
to simulate the daily stress of human spine, including axial and
buckling load external forces, in order to validate the multiple
vertebral three-dimensional frame structure. The results showed
that the height of intervertebral discs in both groups decreased
after cyclic constant loading test. An increase in displacement,
and a decrease in stiffness and the stability of the whole lumbar
spine also occurred in both groups. However, the stability of the
spine in group A was higher than that in group B. With the increase
of cyclic constant loading strength, the stability of the spine in
group A improved. This may be due to the use of osteotomy specimens
in the cyclic constant loading test, which was more realistic in
simulating the clinical situation. The effect of biomechanics is
not obvious when the specimens are subjected to small cyclic
constant loading strength, but it becomes more obvious with the
increase of cyclic constant loading strength, which leads to a
biomechanical instability of the spine.
We verified the triangular stability of a single
vertebral body and the availability of three-dimensional frame
theory through imaging evaluation, pull-out strength test and
cyclic constant loading test, which can provide a novel treatment
for patients with serious osteoporotic spinal diseases.
In conclusion, the results showed that the stability
of screws was significantly improved after the cement screw front
ends of the single vertebral body were bridged, and the stability
of a multiple vertebral spine was significantly improved after a
three-dimensional frame structure was established. This study can
provide a new method to improve the stability and reliability of
internal fixation in patients with serious osteoporotic spinal
diseases.
Acknowledgements
Not applicable.
Funding
The study was funded by National Natural Science
Foundation of China (no. 81301292).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JX wrote the manuscript. JX and TB performed Axial
Withdrawal Force Test. YY and ZW were responsible for Cyclic
Loading Test. ZY and WL contributed to observation indexes
analysis. The final version was read and adopted by all the
authors. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Xijing Hospital (Xi’an, China) and written informed consents were
signed by the patients and/or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bernhardt M, Swartz DE, Clothiaux PL,
Crowell RR and White AA III: Posterolateral lumbar and lumbosacral
fusion with and without pedicle screw internal fixation. Clin
Orthop Relat Res. 284:109–115. 1992.PubMed/NCBI
|
|
2
|
Wray S, Mimran R, Vadapalli S, Shetye SS,
McGilvray KC and Puttlitz CM: Pedicle screw placement in the lumbar
spine: Effect of trajectory and screw design on acute biomechanical
purchase. J Neurosurg Spine. 22:503–510. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
La Maida GA, Luceri F, Gallozzi F, Ferraro
M and Bernardo M: Complication rate in adult deformity surgical
treatment: Safety of the posterior osteotomies. Eur Spine J. 24
(Suppl 7):879–886. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Galbusera F, Volkheimer D, Reitmaier S,
Berger-Roscher N, Kienle A and Wilke HJ: Pedicle screw loosening: A
clinically relevant complication? Eur Spine J. 24:1005–1016.
2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Law M, Tencer AF and Anderson PA:
Caudo-cephalad loading of pedicle screws: Mechanisms of loosening
and methods of augmentation. Spine. 18:2438–2443. 1993.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Chao KH, Lai YS, Chen WC, Chang CM,
McClean CJ, Fan CY, Chang CH, Lin LC and Cheng CK: Biomechanical
analysis of different types of pedicle screw augmentation: A
cadaveric and synthetic bone sample study of instrumented vertebral
specimens. Med Eng Phys. 35:1506–1512. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Higashino K, Kim JH, Horton WC and Hutton
WC: A biomechanical study of two different pedicle screw methods
for fixation in osteoporotic and nonosteoporotic vertebrae. J Surg
Orthop Adv. 21:198–203. 2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hamasaki T, Tanaka N, Kim J, Okada M, Ochi
M and Hutton WC: Pedicle screw augmentation with polyethylene tape:
A biomechanical study in the osteoporotic thoracolumbar spine. J
Spinal Disord Tech. 23:127–132. 2010.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Tsai KJ, Murakami H, Horton WC, Fei Q and
Hutton WC: Pedicle screw fixation strength: A biomechanical
comparison between 4.5-mm and 5.5-mm diameter screws in
osteoporotic upper thoracic vertebrae. J Surg Orthop Adv. 18:23–27.
2009.PubMed/NCBI
|
|
10
|
Becker S, Chavanne A, Spitaler R, Kropik
K, Aigner N, Ogon M and Redl H: Assessment of different screw
augmentation techniques and screw designs in osteoporotic spines.
Eur Spine J. 17:1462–1469. 2008.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lei W and Wu Z: Biomechanical evaluation
of an expansive pedicle screw in calf vertebrae. Eur Spine J.
15:321–326. 2006.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Liu D, Wu ZX, Gao MX, Wan SY, Shi L, Fu
SC, Wang J and Lei W: A new method of partial screw augmentation in
sheep vertebrae in vitro: Biomechanical and interfacial evaluation.
J Spinal Disord Tech. 24:318–324. 2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Wan SY, Lei W, Wu ZX, Lü R, Wang J, Li B,
Fu SC and Zhan C: Micro-CT evaluation and histological analysis of
screw-bone interface of expansile pedicle screw in osteoporotic
sheep. Zhonghua Wai Ke Za Zhi. 45:1271–1273. 2007.(In Chinese).
PubMed/NCBI
|
|
14
|
Hao YX, Wu ZX and Yang Z: The clinical
application of expandable pedicle screws in the short segment
lumber fusion surgery in osteoporosis patients. Zhongguo Ji Zhu Ji
Sui Za Zhi. 27:136–141. 2017.(In Chinese).
|
|
15
|
Liu D, Shi L, Lei W, Wei MQ, Qu B, Deng SL
and Pan XM: Biomechanical comparison of expansive pedicle screw and
polymethylmethacrylate-augmented pedicle screw in osteoporotic
synthetic bone in primary implantation: An experimental study. Clin
Spine Surg. 29:E351–E357. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kiner DW, Wybo CD, Sterba W, Yeni YN,
Bartol SW and Vaidya R: Biomechanical analysis of different
techniques in revision spinal instrumentation: Larger diameter
screws versus cement augmentation. Spine. 33:2618–2622.
2008.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Frankel BM, D'Agostino S and Wang C: A
biomechanical cadaveric analysis of
polymethylmethacrylate-augmented pedicle screw fixation. J
Neurosurg Spine. 7:47–53. 2007.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Moore DC, Maitra RS, Farjo LA, Graziano GP
and Goldstein SA: Restoration of pedicle screw fixation with an in
situ setting calcium phosphate cement. Spine. 22:1696–1705.
1997.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Renner SM, Lim TH, Kim WJ, Katolik L, An
HS and Andersson GB: Augmentation of pedicle screw fixation
strength using an injectable calcium phosphate cement as a function
of injection timing and method. Spine. 29:E212–E216.
2004.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Chiang CK, Wang YH, Yang CY, Yang BD and
Wang JL: Prophylactic vertebroplasty may reduce the risk of
adjacent intact vertebra from fatigue injury: An ex vivo
biomechanical study. Spine. 34:356–364. 2009.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kebaish KM, Martin CT, O'Brien JR, LaMotta
IE, Voros GD and Belkoff SM: Use of vertebroplasty to prevent
proximal junctional fractures in adult deformity surgery: A
biomechanical cadaveric study. Spine J. 13:1897–1903.
2013.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Tan JS, Singh S, Zhu QA, Dvorak MF, Fisher
CG and Oxland TR: The effect of cement augmentation and extension
of posterior instrumentation on stabilization and adjacent level
effects in the elderly spine. Spine. 33:2728–2740. 2008.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Xu G, Fu X, Du C, Ma J, Li Z and Ma X:
Biomechanical effects of vertebroplasty on thoracolumbar burst
fracture with transpedicular fixation: A finite element model
analysis. Orthop Traumatol Surg Res. 100:379–383. 2014.PubMed/NCBI View Article : Google Scholar
|