Introduction
A cerebral aneurysm is an abnormal enlargement of a
cerebral artery, and cerebral aneurysms may lead to poor outcomes
if the aneurysm ruptures (1). Giant
aneurysms are defined by the fact that their largest diameter is
>25 mm, and these types of aneurysms represent 3-5% of all
cerebral aneurysms (2,3). Additionally, 15% of giant aneurysms
originate in the internal carotid artery (4). The incidence of posterior inferior
cerebellar artery (PICA) aneurysms is <0.5-3% of all
intracranial aneurysms, and only a few cases have been reported in
previous studies (5-8).
Giant complicated distal PICA aneurysms are relatively rare,
constituting <30% of all PICA aneurysms (5,9). The
treatment of giant PICA aneurysms is a challenging task for
neurovascular surgeons and neurosurgeons, especially for aneurysms
arising from any segment of the distal PICA. Surgical clipping may
result in numerous complications because of the intimate anatomical
relationships between the proximal PICA and the brainstem as well
as the lower cranial nerves (10,11). An
increasing number of studies have reported that endovascular
treatment is being used as both a primary or alternative method,
but this is often associated with a high rate of complications such
as aneurysm regrowth and brain ischemia (7,10,11).
Additionally, important limitations of this method are the
substantial costs of treatment and the ischemic symptoms.
The present study reports the case of a giant
complicated distal PICA aneurysm treated with surgical clipping and
removal of most of the aneurysm. A review of the literature is also
presented, as well as the discussion of topics related to the
correct diagnosis and treatment of this condition.
Case report
A 46-year-old woman presented to a regional hospital
after suffering from headaches and dizziness for 3 years, these
symptoms were aggravated and combined with limb weakness for 1 day
without any obvious cause. There was no previous history of trauma.
The past medical history of the patient demonstrated hypertension
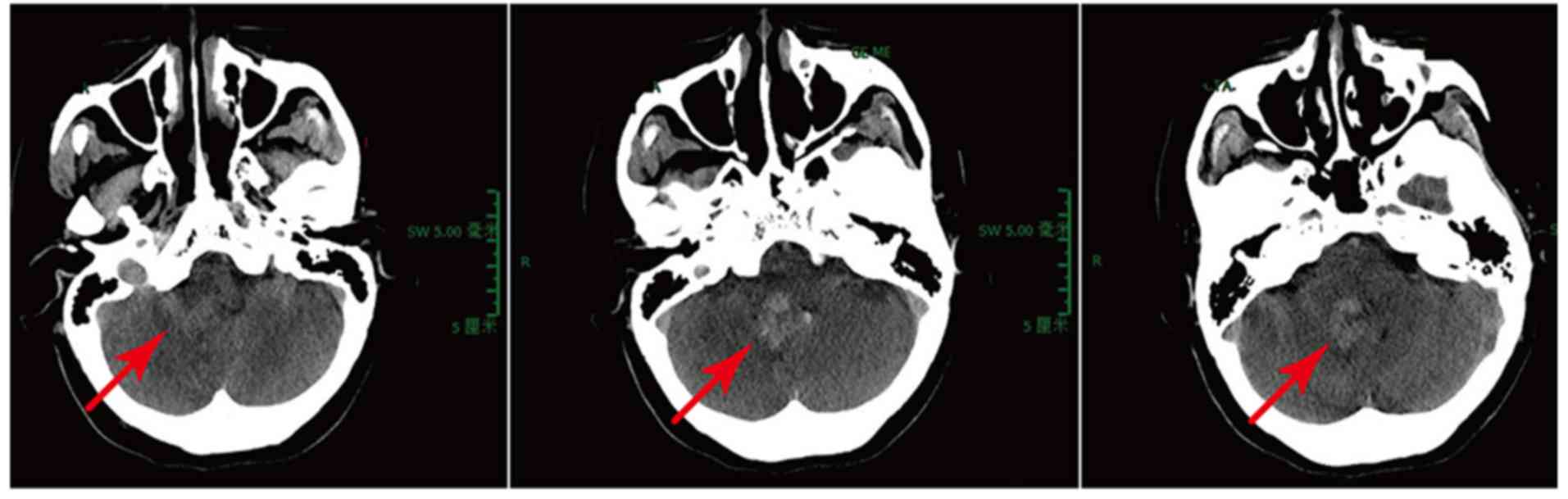
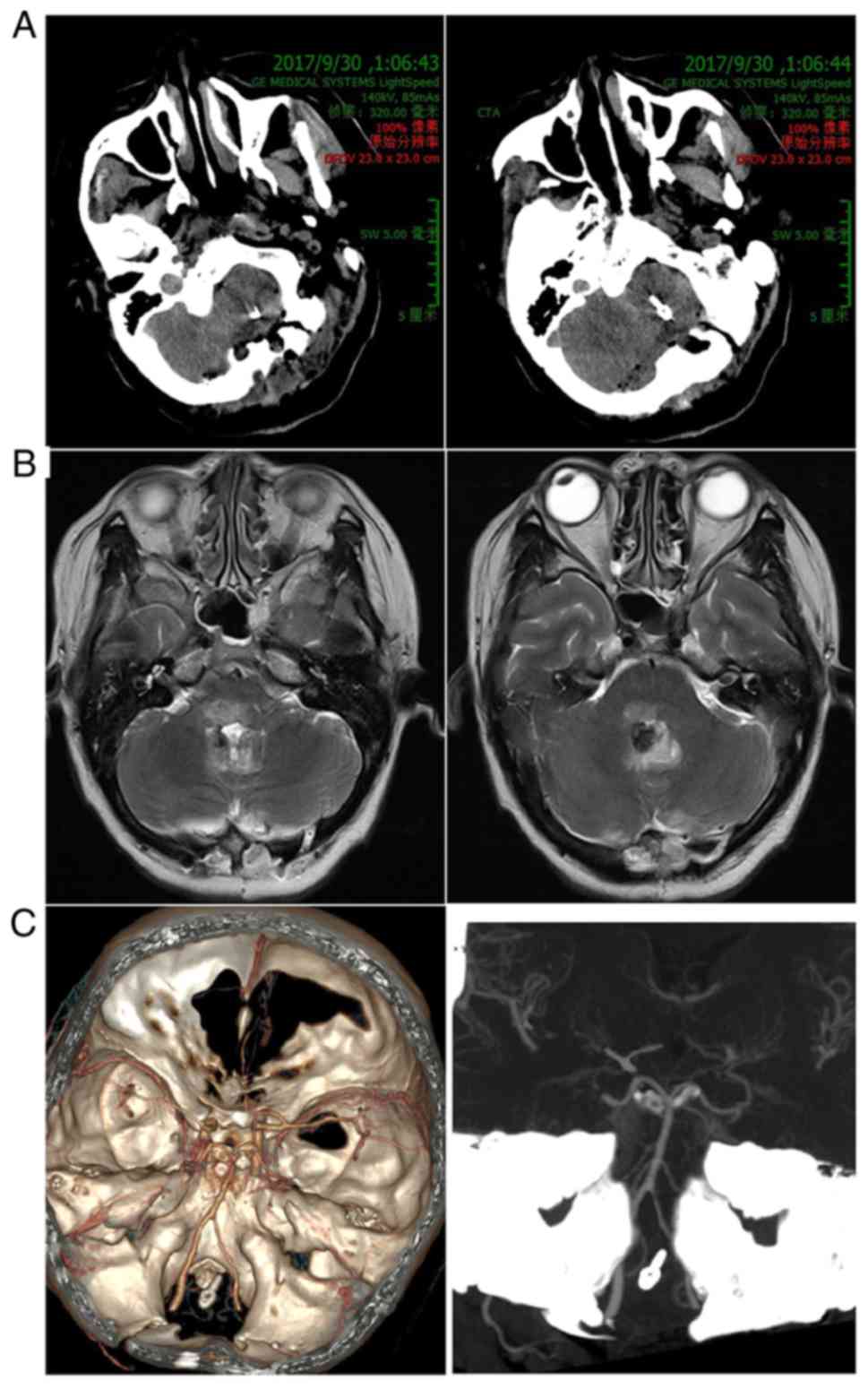
and a history of hysteroscopic myomectomy. A CT scan showed a
lesion occupying the fourth ventricle, with slight bleeding
(Fig. 1). The regional hospital
doctors considered that surgery would be difficult, and that the
diagnosis was difficult to confirm; therefore, the patient was
admitted to Wuxi Clinical College of Anhui Medical University,
904th Hospital of Joint Logistic Support Force of PLA (Wuxi, China)
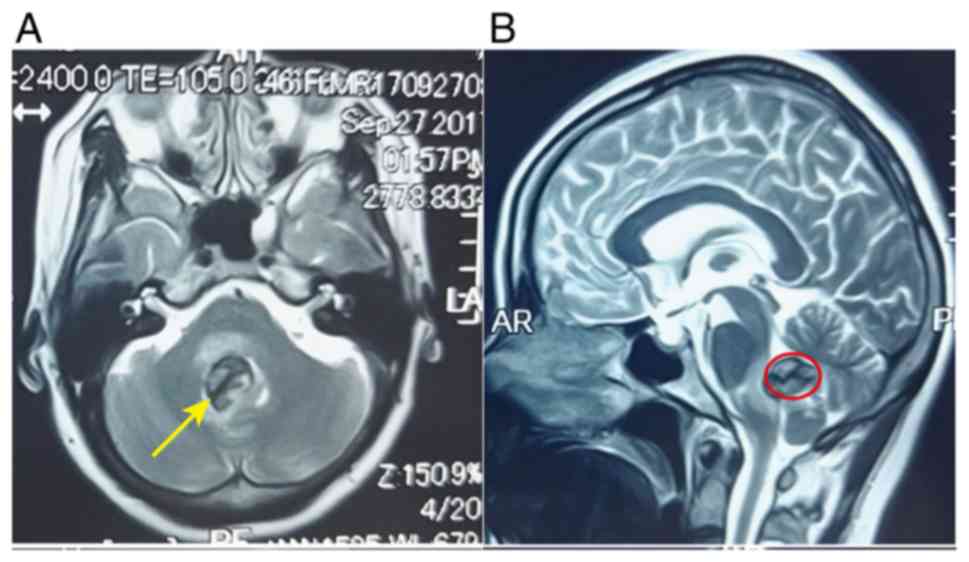
after 2 days. Before the patient was discharged from the regional
hospital, a MR scan also revealed a lesion occupying the fourth
ventricle and compressing the brainstem, and distortion of the
cisterns around the brainstem (Fig.
2). A neurological examination performed upon admission
revealed no other abnormalities, except for the fact that there was
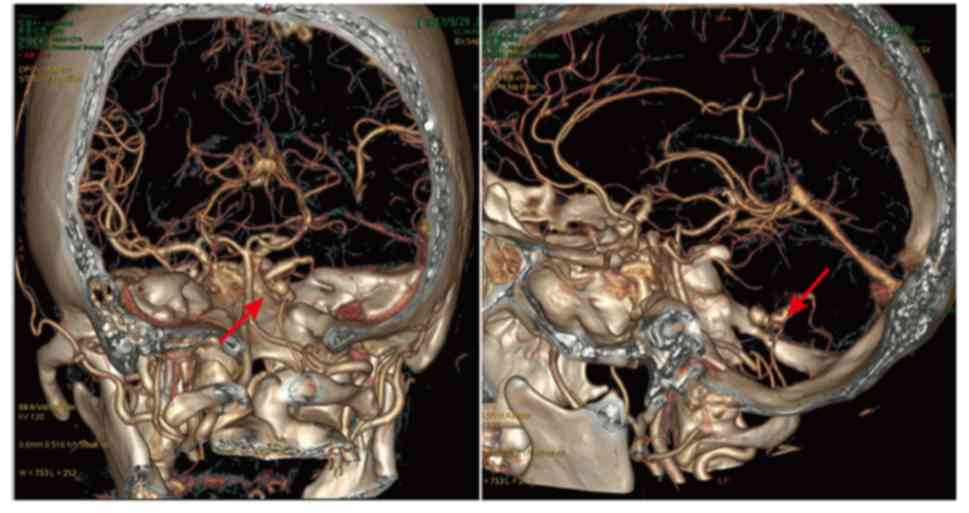
weakness in all limbs [Glasgow Coma Scale (GCS), 15] (4). Next, a CT angiography (CTA) examination
was performed on the patient, which showed a giant irregular
aneurysm located in the PICA, with a size of ~3.5x2.2x1.8 cm; the
aneurysm was serpentiform and irregular, so it was considered
difficult to clip (Fig. 3). Although
simply occluding the PICA via endovascular embolization would be
easy, it would not relieve the mass effect, and it may aggravate
the symptoms. After discussion, the neurosurgeons and vascular
interventional physicians agreed on the microsurgical clipping of
the aneurysm and resection of most of the aneurysm.
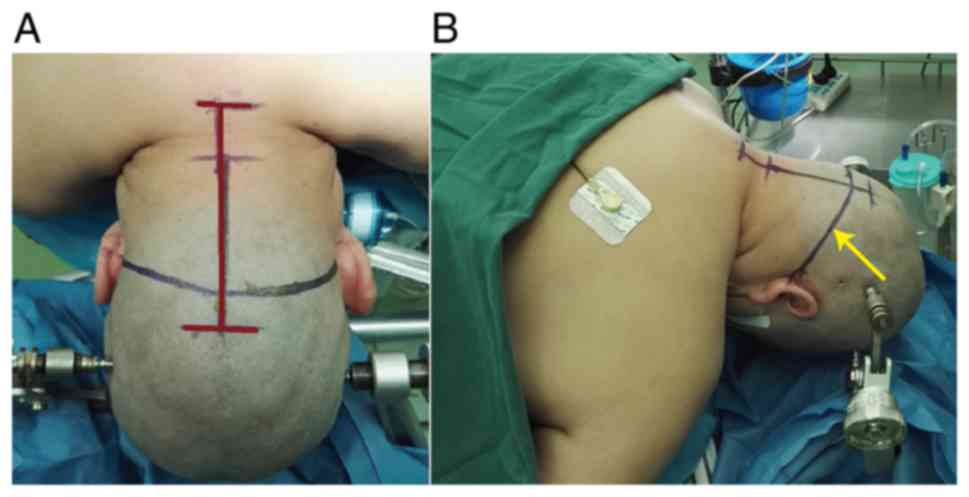
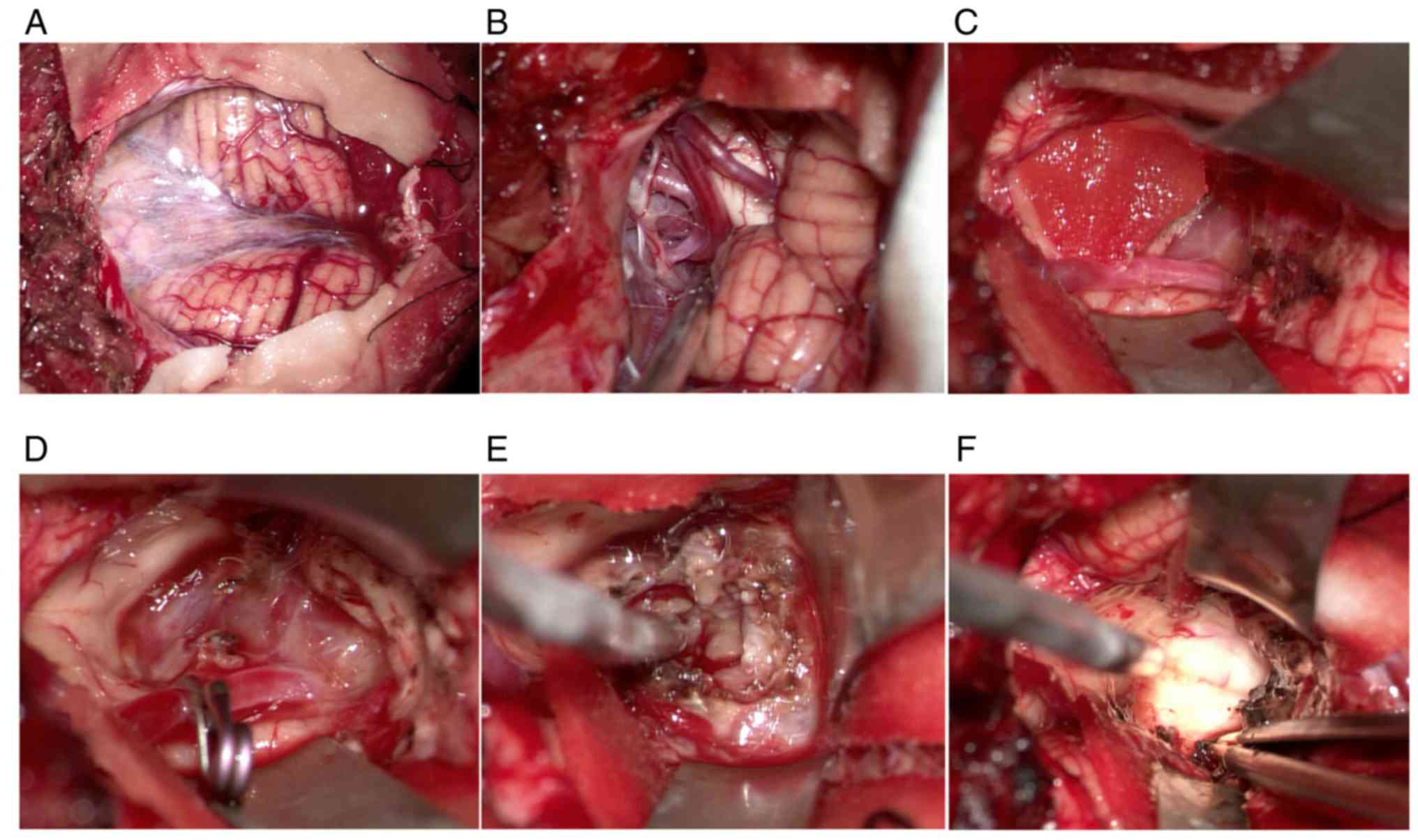
After all preparation procedures were completed, a
median suboccipital approach was selected to expose the aneurysm
(Fig. 4). First, the foramen magnum
was exposed and opened completely. Then, the dura mater was cut,
and the PICA was observed (Fig. 5A
and B). Subsequently, dissection was
carried out along the PICA, and the basilar part of the aneurysm
was explored; the PICA was then temporarily occluded to adequately
expose the aneurysm and its boundary (Fig. 5C and D). It was difficult to perform clipping
alone, as the aneurysm was very large. However, it was also very
important to resect the giant aneurysm to effectively avoid
obstruction of cerebrospinal fluid reflux. The PICA was then
occluded and the aneurysm was removed with another optimal method
(Fig. 5E). The aneurysm was very
regular and ball-shaped and consisted of organized granulation
tissue and fibrous tissues. After the aneurysm was mostly removed,
brainstem compression was alleviated, and the cerebrospinal fluid
moved more fluently (Fig. 5F).
After the operation, blood pressure was maintained
below the typical level of ~10 mmHg systolic blood pressure. The
patient left the Neurosurgery Intensive Care Unit after 3 days,
with a GCS score of 15/15, and without nerve dysfunction. The CT,
MR, and CTA results showed that the PICA aneurysm had been clipped
completely and that brainstem compression had been alleviated
without complications (Fig. 6). A
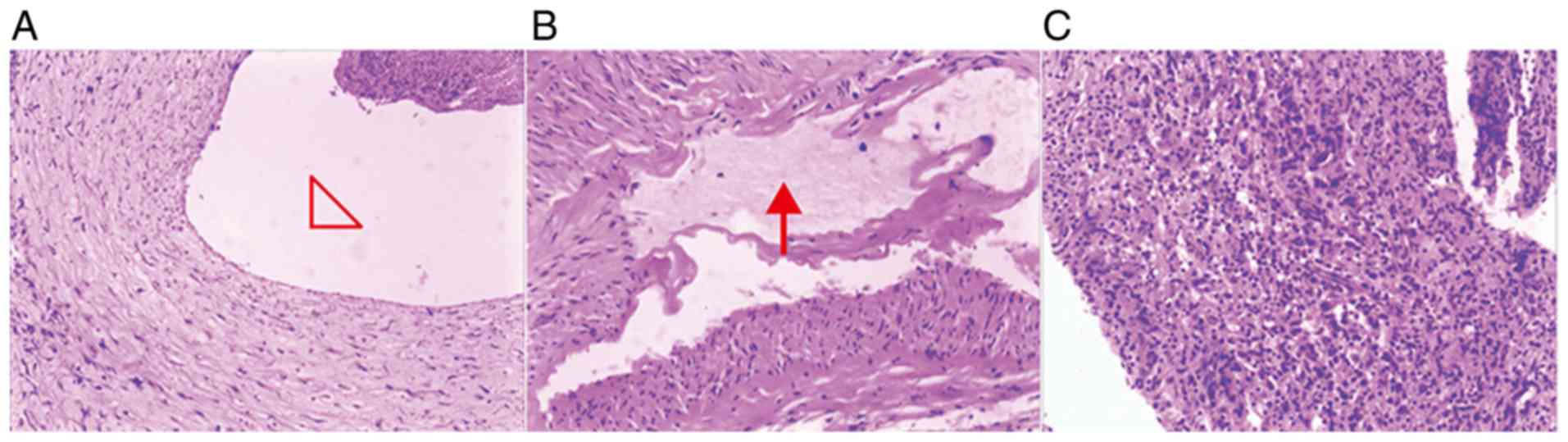
postoperative histopathological examination confirmed a giant
irregular aneurysm and fibrous tissue proliferation (Fig. 7). A total of 6 months after the
operation, the patient had a good outcome with no neurological
dysfunction, and the symptoms of headache and dizziness had
disappeared completely.
Discussion
The PICA is the largest branch of the vertebral
artery, and ruptured PICA aneurysms can lead to cerebral infarction
and cranial nerve compression in patients; some patients with
severe rupture may die due to cardiopulmonary arrest (5,12).
Aneurysms of the vertebral artery (VA)-PICA represent only 0.5-3%
of all aneurysms and only 20% of those in the posterior fossa
(12). Distal PICA aneurysms are
rare, accounting for approximately one-third of PICA aneurysms
(5,9).
CT and MR imaging only indicate subarachnoid or
intraventricular hemorrhage and/or infarction but cannot confirm a
diagnosis of an aneurysm. In the present study, CT indicated a mass
effect and brain edema, calcification and hemorrhage. MR imaging
demonstrated a well-defined mass, with intra-aneurysmal thrombosis,
a boundary, brainstem compression and no contrast-enhancing
components. This information offered by MR was very important for
microsurgical clipping. Cerebral angiography is the most important
diagnostic modality and is the ‘gold standard’ for revealing the
true nature of a lesion (13). In
the present report, a diagnosis was confirmed using 3D-CTA, which
showed a shape of serpentine aneurysm or fusiform aneurysm.
However, the size of the aneurysm according to CTA was
significantly different from the actual size. The reason for this
outcome was the presence of intra-aneurysmal thrombosis and a thick
aneurysm wall. However, an incorrect evaluation before surgery may
lead to incorrect management strategies and negative
consequences.
There are several management strategies for distal
PICA aneurysms, such as surgical clipping, bypass, parent artery
sacrifice (surgical or endovascular) and endovascular aneurysm
embolization. However, different strategies have various advantages
and disadvantages. Previous studies have suggested that surgical
methods, including proximal clipping, trapping, and wrapping or
resection, are very important and effective methods (8,14,15). A
prior clinical study reported that of 52 patients (11 male
patients, 41 female patients) treated surgically for VA-PICA
aneurysms, 47 (79.8%) showed a good outcome, and only one patient
(1.9%) died due to cardiomyopathy during the follow-up period
(10). Horowitz et al
(16) also reported that 24/27
patients (88.9%) had a good outcome and that only two patients
(7.4%) died at the 1-year follow-up. Wu et al (17) described a similarly favorable outcome
rate in a single Chinese center. However, surgery may lead to a
high risk of postoperative neurological morbidity because of the
close relationship between the PICA and the brainstem, as well as
the lower cranial nerves (10,13,16).
Endovascular aneurysm embolization is very important
and is the most common management strategy for PICA aneurysms.
Endovascular technology and intervention materials are ideal
methods, and various endovascular methods described for the
treatment of PICA aneurysms include silicon or latex balloon
occlusion of the aneurysm (7,18). This
treatment easily and effectively avoids rebleeding, cranial nerve
dysfunction and postoperative complications (18). However, few articles have been
published describing the long-term follow-up outcomes of VA-PICA
aneurysms treated with embolization (10,18). A
clinical study, which included 23 patients treated with
endovascular embolization of ruptured PICA aneurysms, found that
the procedure-related morbidity rate was 13%, with no
procedure-related instances of death; a good outcome was reported
in 86.4% patients and three patients (13%) died within 2 months of
treatment (18). Ogilvy et al
(19) also reported that
endovascular coiling of posterior circulation aneurysms, including
PICA aneurysms in eight patients, resulted in a good outcome in
77.2% patients. Few publications have documented the specific
recurrence rate with a long-term follow-up. Byrne et al
(20) reported that recurrent
filling occurred in 14.7% of 259 embolization aneurysms; however,
this study included only 16 PICA aneurysms.
Surgical or endovascular trapping of the dissected
arterial segment, especially for the first three segments of the
PICA (anterior medullary, lateral medullary, and tonsillar
medullary), may lead to two main complications: An infarct in the
distal territory of the PICA, and an ischemic lesion of the medulla
due to the occlusion of perforators in the trapped segment
(13). Intraoperative fluorescence
angiography and Doppler ultrasonography are useful for reducing the
rate of infarct and confirming the location of the aneurysm
(3,4).
The treatment time used for patients with VA-PICA
aneurysms remains controversial (11,17,21).
Most authors have recommended early surgery (first 24 h) after
diagnosis, especially for Hunt and Hess grade IV and V patients
(4,11,21). In
our center, it is recommended that ultra-early surgery (12 h) or
emergency surgery may be beneficial for patients, especially for
patients with severe subarachnoid hemorrhage (SAH). However, Wu
et al (17) reported delayed
surgery improved outcomes of proximal PICA aneurysms in a single
center study, that all the surgeries of proximal PICA aneurysms
were performed in a delayed fashion, several days to weeks after
the presentation of SAH. No systematic clinical studies have
analyzed or summarized the different outcomes of early surgery and
delayed surgery. The biggest risk for cerebral aneurysms is
rupture, and there is a high cerebral rupture risk with delayed
timing of surgical treatment (4);
hence our recommendation of early or emergency surgery. However,
the disadvantage of early or emergency surgery is that this could
lead to inadequate perioperative preparation for a relatively
difficult operation, particularly in the case of SAH.
An understanding of PICA anatomy is essential before
surgery. Lower cranial nerve palsy and cerebellar infarction are
common postoperative complications that occur after VA-PICA
aneurysm surgery (10,17). Most distal PICA aneurysms are located
superficial to the lower cranial nerves (5,17). If
the PICA is occluded, adverse effects, such as headache, vomiting,
ipsilateral cerebellar ataxia, difficulty swallowing, hoarseness
and dizziness, may occur, and severe cerebellar infarction may lead
to obstructive hydrocephalus (17).
A study by Horowitz et al (16) found that 47% of posteroinferior
cerebellar artery aneurysms patients had cranial nerve IX and X
palsy after operation, and only four patients (22%) continued to
have dysphagia at the 1-year follow-up. Hudgins et al
(5) also reported a lower cranial
nerve dysfunction rate of 23.8% compared with with Horowitz's
study. Therefore, it is very important to understand the
relationship between the origin of the PICA and lower cranial
nerves. However, this anatomic relationship is irregular and highly
variable (17,22). Al-khayat (10) described some reasons for
post-operative complications in the cranial nerves after PICA
aneurysm surgery as follows: i) There is a rapid or abrupt change
caused by stretching and manipulation, as occurs in vascular
surgery; ii) temporary clips may physically limit the already
confined space in the posterior fossa, leading to an increased risk
of mechanical trauma to the lower cranial nerves; and iii) total
occlusion may cause the nerves to be more vulnerable to trauma by
decreasing the blood supply. Most patients with lower cranial nerve
palsy and cerebellar infarction recover completely within 6 months
(10,16). Intraoperative electrophysiological
monitoring is useful and may avoid accidental injury during
vascular surgery.
Fusiform and wide neck aneurysms present a challenge
to endovascular surgeons, with a high risk of parent artery
embolization, neurologic deficits and residual aneurysms (18,19).
More importantly, as endovascular therapeutic techniques cannot
improve the symptoms of mass effect, and as microsurgical clipping
may result in numerous clip-related complications, it may be
necessary to utilize other methods. In the future, bypass and new
flow diversion stents may become very important techniques for
aneurysm treatment. Several studies have reported that PICA-to-PICA
bypass or occipital artery-to-PICA bypass are able to treat distal
PICA aneurysms (11,23,24).
However, additional studies and randomized clinical controlled
trials are needed to confirm these findings.
In conclusion, giant distal PICA aneurysms are very
rare and are often combined with posterior fossa syndrome. In the
present study, giant distal PICA aneurysm treatment by surgical
clipping and removal of the aneurysm was reported with a good
outcome and without any complications. It was concluded that
surgical treatment was a useful and safe option. Surgery may
prevent rebleeding and can also remove space-occupying lesions,
especially thrombosed aneurysms. In the future, bypass and flow
diversion stent techniques may be used in the treatment of VA-PICA
aneurysms.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
JZ, LY, YC, ZL, XQ, KZ and BZ analyzed and
interpreted the patient data. EP and JC performed the operation,
data analysis, follow-up and revised the manuscript. JZ, LY and JC
performed the histological examination of the aneurysm, and were
major contributors in writing the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study protocol was approved by the Anhui Medical
University-Affiliated Wuxi Clinical College Clinical Research
Ethics Committee. Written informed consent was obtained from the
patient.
Patient consent for publication
The patient provided written consent for the
publication of their data and images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wiebers DO, Whisnant JP, Huston J III,
Meissner I, Brown RD Jr, Piepgras DG, Forbes GS, Thielen K, Nichols
D, O'Fallon WM, et al: Unruptured intracranial aneurysms: Natural
history, clinical outcome, and risks of surgical and endovascular
treatment. Lancet. 362:103–110. 2003.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Choi IS and David C: Giant intracranial
aneurysms: Development, clinical presentation and treatment. Eur J
Radiol. 46:178–194. 2003.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lawton MT and Spetzler RF: Surgical
strategies for giant intracranial aneurysms. Neurosurg Clin N Am.
9:725–742. 1998.PubMed/NCBI
|
|
4
|
Chen J, Zhu J, He J, Wang Y, Chen L, Zhang
C, Zhou J and Yang L: Ultra-early microsurgical treatment within 24
h of SAH improves prognosis of poor-grade aneurysm combined with
intracerebral hematoma. Oncol Lett. 11:3173–3178. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Hudgins RJ, Day AL, Quisling RG, Rhoton AL
Jr, Sypert GW and Garcia-Bengochea F: Aneurysms of the posterior
inferior cerebellar artery: A clinical and anatomical analysis. J
Neurosurg. 58:381–387. 1983.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Locksley HB, Sahs AL and Sandler R: Report
on the cooperative study of intracranial aneurysms and subarachnoid
hemorrhage: Part 3-subarachnoid hemorrhage unrelated to
intracranial aneurysm and A-V malformation: A study of associated
diseases and prognosis. J Neurosurg. 24:1034–1056. 1966.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Maimon S, Saraf-Lavi E, Rappaport ZH and
Bachar G: Endovascular treatment of isolated dissecting aneurysm of
the posterior inferior cerebellar artery. AJNR Am J Neuroradiol.
27:527–532. 2006.PubMed/NCBI
|
|
8
|
Wetjen NM, Link MJ, Reimer R, Nichols DA
and Giannini C: Clinical presentation and surgical management of
dissecting posterior inferior cerebellar artery aneurysms: 2 case
reports. Surg Neurol. 64:462–467. 2005.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Ishikawa T, Suzuki A and Yasui N: Distal
posterior inferior cerebellar aneurysms: Report of 12 cases. Neurol
Med Chir (Tokyo). 30:100–108. 1990.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Al-khayat H, Al-Khayat H, Beshay J, Manner
D and White J: Vertebral artery-posteroinferior cerebellar artery
aneurysms: Clinical and lower cranial nerve outcomes in 52
patients. Neurosurgery. 56:2–11. 2005.PubMed/NCBI
|
|
11
|
Lewis SB, Chang DJ, Peace DA, Lafrentz PJ
and Day AL: Distal posterior inferior cerebellar artery aneurysms:
Clinical features and management. J Neurosurg. 97:756–766.
2002.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yasargil MG: Vertebrobasilar aneurysms, in
microneurosurgery: Clinical considerations, surgery of the
intracranial aneurysms and results. Stuttgart, Georg Thieme.
2:232–295. 1984.
|
|
13
|
Sedat J, Chau Y, Mahagne MH, Bourg V,
Lonjon M and Paquis P: Dissection of the posteroinferior cerebellar
artery: Clinical characteristics and long-term follow-up in five
cases. Cerebrovasc Dis. 24:183–190. 2007.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hamada J, Nagahiro S, Mimata C, Kaku T and
Ushio Y: Reconstruction of the posterior inferior cerebellar artery
in the treatment of giant aneurysms: Report of two cases. J
Neurosurg. 85:496–499. 1996.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Yamakawa H, Kaku Y, Yoshimura S, Ohkuma A
and Sakai N: Two cases of dissecting aneurysm of the distal
posterior inferior cerebellar artery: Possible involvement of
segmental mediolytic arteriopathy in the pathogenesis. Clin Neurol
Neurosurg. 107:117–122. 2005.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Horowitz M, Kopitnik T, Landreneau F,
Krummerman J, Batjer HH, Thomas G and Samson D: Posteroinferior
cerebellar artery aneurysms: Surgical results for 38 patients.
Neurosurgery. 43:1026–1032. 1998.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wu J, Xu F, Yu ZQ, Zhou YX, Cui G, Li XD,
Zhou D, Zhang SM and Wang Z: Clinical experiences of ruptured
posteroinferior cerebellar artery aneurysms and anatomical analysis
in the Cadaver in a single center of China. Clinical Neurology and
Neurosurgery. 114:366–371. 2012.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Mukonoweshuro W, Laitt RD and Hughes DG:
Endovascular treatment of PICA aneurysms. Neuroradiology.
45:188–192. 2003.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ogilvy CS, Hoh BL, Singer RJ and Putman
CM: Clinical and radiographic outcome in the management of
posterior circulation aneurysms by use of direct surgical or
endovascular techniques. Neurosurgery. 51:14-21; discussion 21-22.
2002.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Byrne JV, Sohn MJ, Molyneux AJ and Chir B:
Five-year experience in using coil embolization for ruptured
intracranial aneurysms: Outcomes and incidence of late rebleeding.
J Neurosurg. 90:656–663. 1999.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Horiuchi T, Tanaka Y, Hongo K, Nitta J,
Kusano Y and Kobayashi S: Characteristics of distal posteroinferior
cerebellar artery aneurysms. Neurosurgery. 53:589–596.
2003.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Macchi V, Porzionato A, Parenti A and De
Caro R: The course of the posterior inferior cerebellar artery may
be related to its level of origin. Surg Radiol Anat. 26:60–65.
2004.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Lemole GM Jr, Henn J, Javedan S, Deshmukh
V and Spetzler RF: Cerebral revascularization performed using
posterior inferior cerebellar artery-posterior inferior cerebellar
artery bypass: Report of four cases and literature review. J
Neurosurg. 97:219–223. 2002.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Yoon SM, Shim JJ, Kim SH and Chang JC:
Bilateral vertebral artery dissecting aneurysms presenting with
subarachnoid hemorrhage treated by staged coil trapping and covered
stents graft. J Korean Neurosurg Soc. 51:155–159. 2012.PubMed/NCBI View Article : Google Scholar
|