Introduction
Chronic kidney disease has an incidence of ~10.8%
and poses a threat to human health (1,2).
Although chronic kidney disease may be effectively treated, a
considerable number of patients with end-stage renal disease (ESRD)
remain and hemodialysis is the primary alternative treatment option
(3,4). However, hemodialysis is associated with
numerous serious complications. Cardiovascular events are one of
the primary causes of decreased quality of life and ultimately
death in hemodialysis patients with ESRD (5,6).
Numerous studies have demonstrated that the risk of death from
cardiovascular events in patients with ESRD is >11 times greater
compared with that in patients who did not receive any dialysis
(7). After correction for risk
factors, including hypertension, diabetes and hyperlipidemia,
hemodialysis patients still have an elevated risk of cardiovascular
events (8,9).
The neutrophil-to-lymphocyte ratio (NLR), defined as
the ratio of the percentage of neutrophils to the percentage of
lymphocytes, has been widely used to assess the prognosis of
patients with specific types of tumor, appendicitis and
post-operative cardiovascular disease (10,11).
Several studies have reported that the NLR may reflect the
inflammatory state of hemodialysis patients, and may be associated
with cardiovascular events in hemodialysis patients (12,13). The
red blood cell distribution width (RDW)-to-platelet ratio (RPR) and
NLR are routinely used biochemical parameters. Several studies have
reported that increased RDW is an independent risk factor for
cardiovascular death in hemodialysis patients (14,15). In
addition, platelets serve an important role in the occurrence and
development of cardiovascular events (16). The RPR, a combination of the two
independent parameters, may be of high predictive value regarding
cardiovascular events in hemodialysis patients.
The present study determined the predictive value of
the NLR and RPR regarding the occurrence and development of
cardiovascular events in hemodialysis patients, as well as their
prognosis. The clinical data of 555 patients who were maintained on
hemodialysis were retrospectively analyzed and the association
between the NLR or RPR of dialysis patients and cardiovascular
events, and the early diagnostic and prognostic value of these
parameters was determined.
Materials and methods
Patients
In the present study, the clinical data of 555
hemodialysis patients who were undergoing dialysis at the First
People's Hospital of Yancheng (Yancheng, China) and the Fifth
People's Hospital of Wuxi (Wuxi, China) between May 2015 and March
2018 were analyzed. All patients had ESRD. The patients were
divided into four groups: Patients on hemodialysis that experienced
cardiovascular events (HCE) in the original cohort (n=219); those
on hemodialysis that experienced cardiovascular events in the
validation cohort (n=30); those with no cardiovascular events
(HNCE) in the original cohort (n=276); and those on hemodialysis
that experienced cardiovascular events in the validation cohort
(n=30). The specific cardiovascular events included were angina
pectoris, acute myocardial infarction, symptomatic heart failure
and arrhythmia, and all patients were clinically diagnosed as
presenting with one of these diseases.
The inclusion criteria were as follows: i) Patients
received regular dialysis for >3 months; and ii) patients did
not receive any other treatments during the same period. The
following exclusion criteria were applied: i) Serious complications
of any other organs; ii) patients who had previously undergone
kidney transplantation and immunosuppressive therapy; iii) patients
with an infection, blood transfusion or receiving immunosuppressive
drugs, as this may have affected the inflammatory response within
the 3 months; iv) patients who were pregnant; v) patients who had a
mental illness; and vi) patients with diabetes, hypertension, or
any other diseases; or smoking and other lifestyle choices that may
have affected ‘inflammation-malnutrition-atherosclerosis’ and thus
influenced the NRL and RDW.
The follow-up period was 24 months and all the
patients were followed up using medical records and telephone
interviews. The follow-up endpoints were all-cause death or new
cardiovascular events (angina pectoris, acute myocardial infarction
or acute cardiac insufficiency), stroke (hemorrhage or ischemia)
and peripheral vascular events. If a patient had multiple
cardiovascular events, the first cardiovascular event was
considered the endpoint.
Hemodialysis treatment
The patients of the two groups were given dialysis
for 12 h per week. The blood flow was maintained at 250-280 ml/min
and the dialysate flow was maintained at 500-800 ml/min. Low
molecular weight heparin was used to prevent coagulation. Dialysis
management was performed according to the Guidelines for Clinical
Practice of Chronic Kidney Disease and Dialysis (17).
Clinical information and laboratory
examination
The clinical characteristics and laboratory test
results on admission, including hemoglobin, neutrophil, lymphocyte
and white blood cell (WBC) counts, serum alanine aminotransferase
(ALT), aspartate aminotransferase (AST), γ-glutamyl transferase
(GGT), total bilirubin (TBIL), albumin (ALB), creatinine (CR),
blood urea nitrogen (UREA), uric acid (UA), parathyroid hormone
(PTH), total cholesterol (TC), calcium (CA), platelet counts (PLT),
hemoglobin (Hb), brain natriuretic peptide (BNP), creatine kinase
isoenzyme-MB (CK-MB), cardiac troponin I (cTnI), glomerular
filtration rate (GFR) and results of the electrocardiogram (ECG)
examination in all patients were recorded. All patients were
examined using a Philips iE33 real-time three-dimensional color
doppler echocardiograph (Philips Medical Systems, Inc.) at one the
day after dialysis. Systolic pulmonary pressure (SPAP), left
ventricular diastolic diameter (LVDd), dialyzer clearance of urea
(K), dialysis time (t), volume of distribution of urea (V),
efficiency criteria for hemodialysis treatment (Kt/V), left
ventricular systolic diameter (LVDs) and left atrial diameter were
measured every 6 months and the average value was used.
Statistical analysis
Statistical analyses were performed using GraphPad
Prism version 7 (GraphPad Software, Inc.). Values are expressed as
the mean ± standard deviation when data were normally distributed
or as the median and range if the distribution was skewed.
Comparisons between groups were performed using analysis of
variance. Correlation analyses between variables were performed
using Pearson's rank correlation coefficient analysis. P<0.05
was considered to indicate a statistically significant difference.
Receiver operating characteristic (ROC) curves were plotted and
areas under the ROC curves (AUCs) were calculated to determine the
discrimination threshold of each marker. The appropriate cut-off
points for the optimal combination of sensitivity and specificity
were determined using Youden's J statistics. Binary logistic
regression analyses were used to determine factors associated with
the incidence of cardiovascular events in hemodialysis patients.
Binary logistic regression analyses were used to calculate the
adjusted odds ratio and 95% confidence interval values based on
maximum likelihood estimation of NLR and RPR.
Results
Patient characteristics
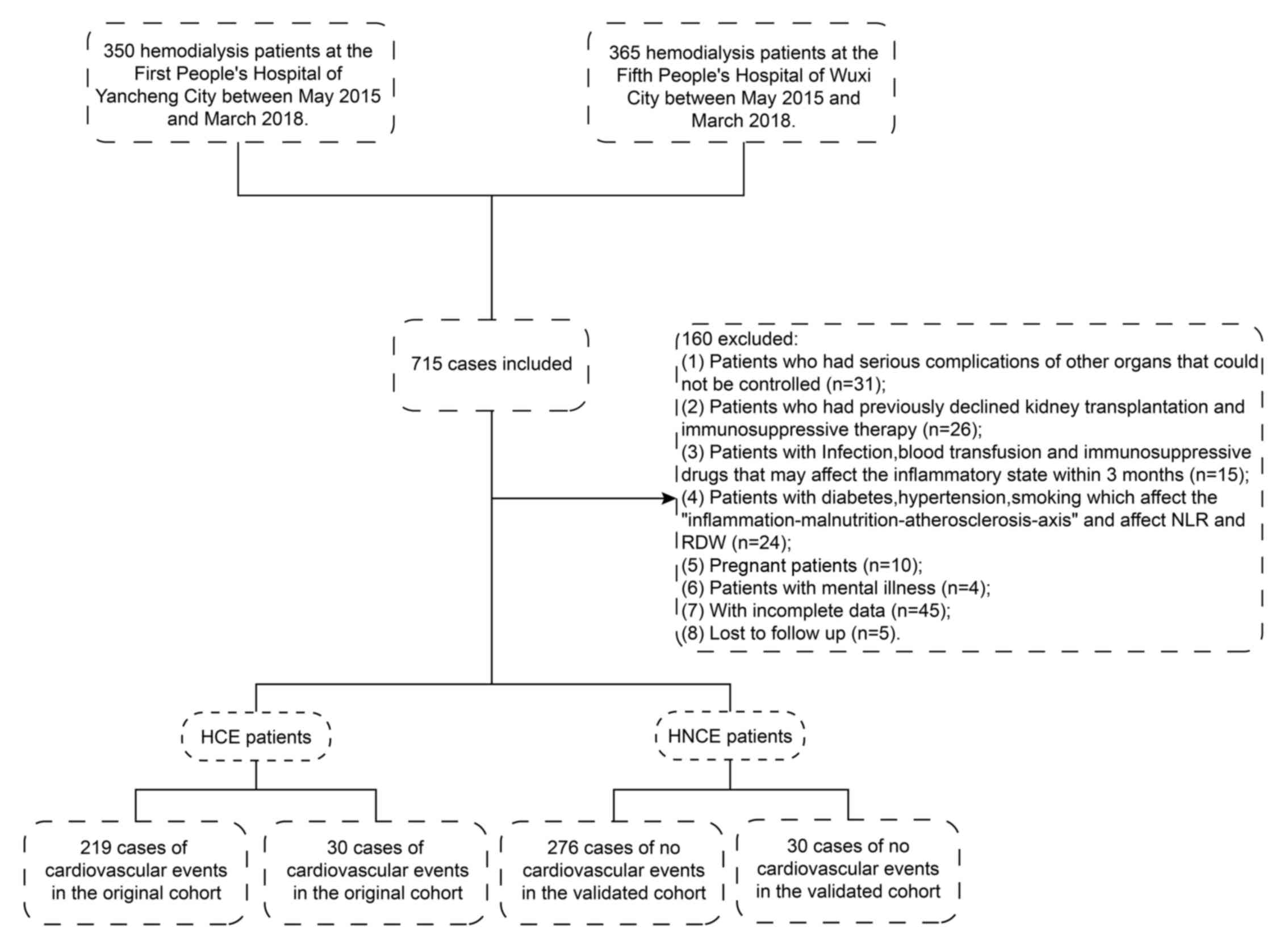
From a total of 715 hemodialysis patients, a
cross-sectional group of 495 patients were enrolled in the original
cohort. Fig. 1 presents a flow chart
for the screening of hemodialysis patients from the two hospitals.
The demographics, characteristics and biochemical parameters of HCE
patients and HNCE patients are summarized in Table I. No significant differences between
the two groups were identified regarding age, sex, time of
hemodialysis, GGT, CA, UA, TC, ALT, TBIL and GFR. However, the
average levels of serum AST, phosphorus, PTH, UREA, CR, neutrophil
ratio, WBC, BNP, CK-MB, cTnI, LVDd, LVDs, SPAP and left atrial
diameter in the HCE group were significantly higher compared with
those in the HNCE group. The levels of ALB, Hb, Kt/V, lymphocyte
count and PLT were significantly lower compared with those in the
HNCE group.
 | Table ICharacteristics of the patients
enrolled. |
Table I
Characteristics of the patients
enrolled.
| Variable | HCE group
(n=219) | HNCE group
(n=276) | P-value |
|---|
| Age (years) | 50.25 (29-79) | 51.34 (28-81) | 0.102 |
| Gender (F/M) | 124/95 | 166/110 | 0.117 |
| Time of hemodialysis
(months) | 22 (9-43) | 24 (10-47) | 0.687 |
| Hb (g/l) | 75.24±13.11 | 94.53±20.11 | 0.036 |
| Neutrophil ratio
(%) | 82.61±3.11 | 68.22.1±2.98 | 0.025 |
| Lymphocyte count
(109/l) | 0.75±0.36 | 2.75±1.23 | 0.042 |
| WBC
(109/l) | 13.22±3.65 | 7.11±2.17 | 0.032 |
| PLT
(109/l) | 85.12±14.27 | 142.14±25.19 | 0.017 |
| ALT (U/l) | 30.12±8.72 | 29.92±7.22 | 0.513 |
| AST (U/l) | 67.02±4.75 | 16.06±4.09 | 0.029 |
| GGT (U/l) | 38.00
(27.00-44.00) | 35.00
(23.00-41.00) | 0.978 |
| Kt/V | 1.22±0.14 | 1.59±0.29 | 0.033 |
| ALB (g/l) | 34.02±3.21 | 45.56±4.29 | 0.021 |
| TBIL (µmol/l) | 8.98±3.87 | 9.04±4.12 | 0.679 |
| Ca (mmol/l) | 2.24±0.13 | 2.27±0.19 | 0.752 |
| P (mmol/l) | 2.12±0.64 | 1.79±0.52 | 0.035 |
| PTH (pmol/l) | 19.51 (7.12,
59.45) | 12.44 (7.25,
29.45) | 0.022 |
| UREA (mmol/l) | 29.61±5.94 | 19.61±4.11 | 0.029 |
| CR (µmol/l) | 882.21±113.21 | 712.61±103.61 | 0.039 |
| UA (µmol/l) | 412.01±97.45 | 389.01±87.11 | 0.895 |
| TC (mmol/l) | 3.98±0.36 | 3.83±0.32 | 0.357 |
| GFR (ml/min x 1.73
m2) | 2.7 (0.72,
3.15) | 2.6 (0.71,
3.2) | 0.962 |
| WBC
(109/l) | 13.22±3.65 | 7.11±2.17 | 0.032 |
| BNP (pg/ml) | 7565±873.12 | 4456±421.27 | <0.001 |
| CK-MB (U/l) | 22.05±5.22 | 19.71±4.13 | 0.002 |
| cTnI (ng/ml) | 14.25±3.88 | 5.71±1.97 | <0.001 |
| LVDd (cm) | 5.65±0.69 | 5.15±0.44 | 0.042 |
| LVDs (cm) | 3.89±0.43 | 3.14±0.35 | 0.007 |
| SPAP (mmHg) | 41.22±6.19 | 32.24±1.35 | 0.009 |
| Left atrial
diameter (cm) | 4.29±0.47 | 3.80±0.39 | 0.005 |
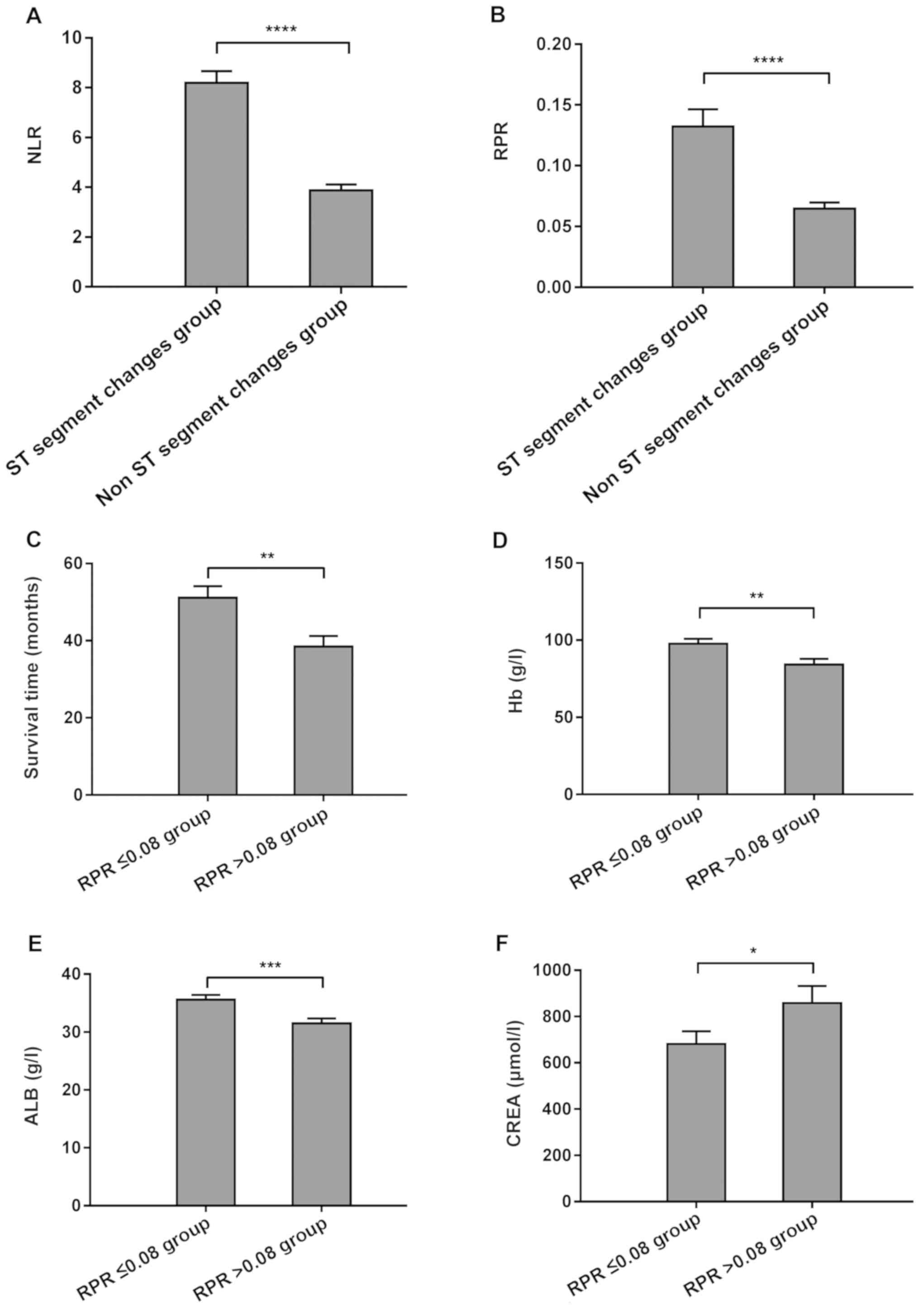
NLR and RPR may be used to predict
cardiovascular events in hemodialysis patients
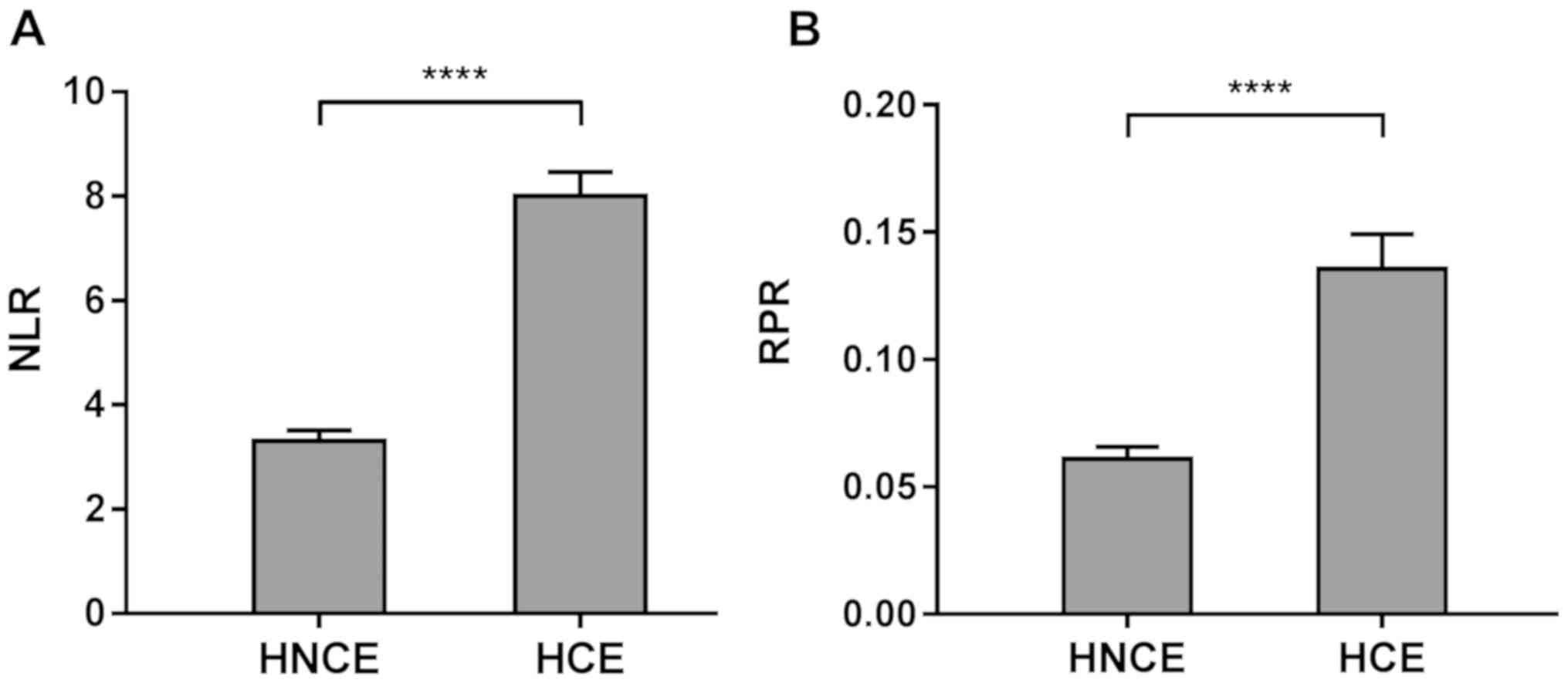
The NLR and RPR of each group were determined and it
was revealed that in the HCE group, these two ratios were
significantly higher compared with those in the HNCE group
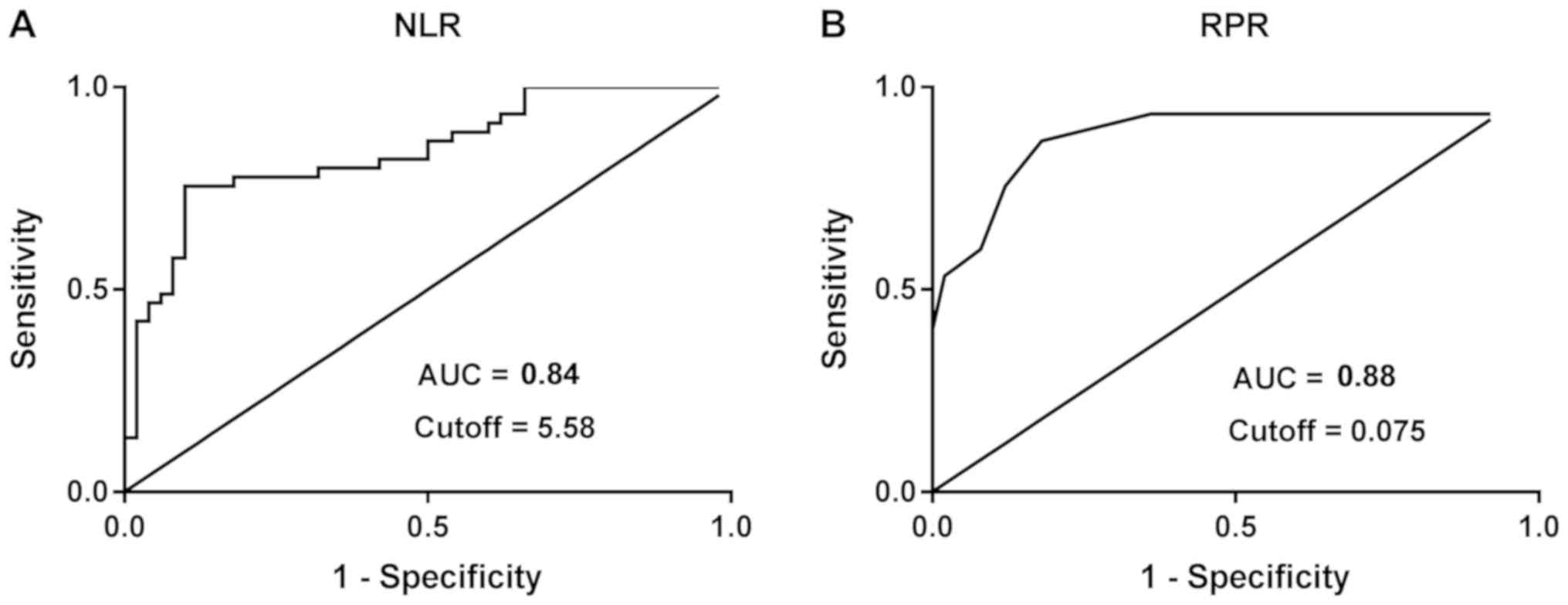
(P<0.05; Fig. 2). ROC analysis
was then performed for the NLR or RPR regarding the prediction of
cardiovascular events in hemodialysis patients. The AUC of the RPR
and NLR for predicting cardiovascular events in hemodialysis
patients was 0.88 and 0.84, respectively. According to the cutoff
values of RPR (0.075) and NLR (5.58), the sensitivity and
specificity of the RPR for predicting cardiovascular events in
hemodialysis patients were 0.87 and 0.82 respectively, and for NLR,
they were 0.75 and 0.79, respectively (Fig. 3).
Logistic regression models adjusting for known risk
factors (elevated BNP, elevated cTnI, increased LVD) were used to
determine whether the NLR and RPR are significant predictors of
cardiovascular events. The results of this analysis suggested that
the RPR is an independent risk factor for cardiovascular events in
hemodialysis patients (Table
II).
 | Table IIAssociation of RDW or RPR with the
risk of cardiovascular events in hemodialysis patients: OR (95%CI)
using binary logistic regression. |
Table II
Association of RDW or RPR with the
risk of cardiovascular events in hemodialysis patients: OR (95%CI)
using binary logistic regression.
| | Univariate
analysis | Multivariate
analysis |
|---|
| Variable | OR (95% CI) | P-value | OR (95% CI) | P-value |
|---|
| RPR | 2.26
(1.23-4.16) | 0.009 | 7.04
(3.44-14.44) | <0.0001 |
| RDW | 0.53
(0.28-0.99) | 0.045 | 1.00
(0.84-1.19) | 0.964 |
The diagnostic efficacy of the two parameters was
validated with an additional 30 HCE patients and 30 HNCE patients.
Using the cutoff values for the NLR (5.58) and the RPR (0.075)
determined above, the predictive abilities of the NLR and RPR for
cardiovascular events in hemodialysis patients were similar to the
results obtained in the original cohort (Table III).
 | Table IIIPerformances of NLR and RPR in the
diagnosis of patients with hemodialysis in the validation cohort
was performed using ROC analysis. |
Table III
Performances of NLR and RPR in the
diagnosis of patients with hemodialysis in the validation cohort
was performed using ROC analysis.
| Parameter | HCE patients | HNCE patients | AUROC (95% CI) | Sensitivity | Specificity | +LR | -LR | PPV | NPV | Youden | P-value |
|---|
| NLR | | | 0.83 | 0.73 | 0.80 | 3.27 | 0.23 | 43.18 | 94.87 | 0.59 | <0.001 |
|
>5.58 | 22 | 6 | | | | | | | | | |
|
≤5.58 | 8 | 24 | | | | | | | | | |
| RPR | | | 0.87 | 0.87 | 0.83 | 4.32 | 0.07 | 63.46 | 97.14 | 0.73 | <0.001 |
|
>0.075 | 26 | 5 | | | | | | | | | |
|
≤0.075 | 4 | 25 | | | | | | | | | |
Correlations between NLR or RPR and
parameters of cardiovascular function
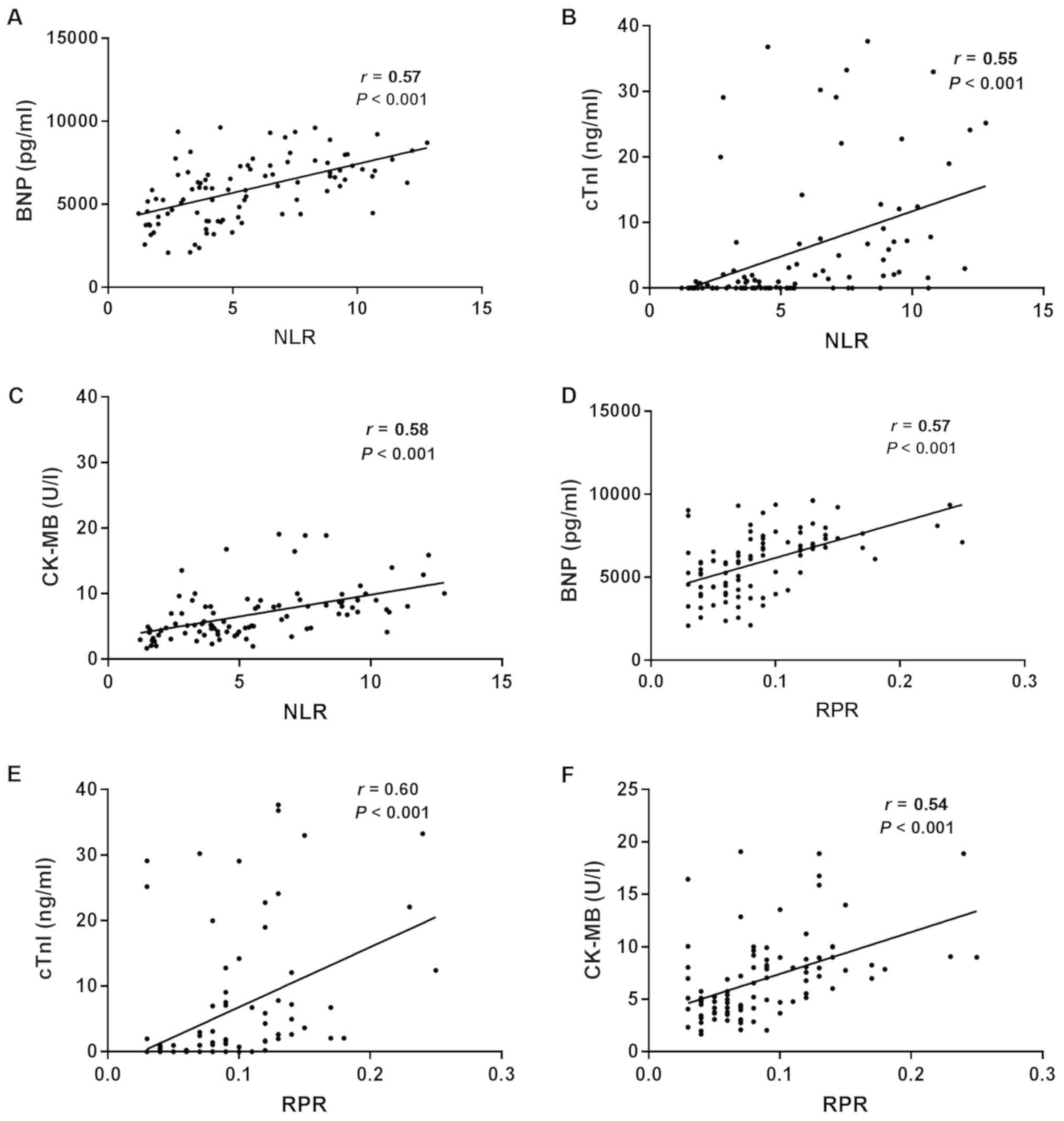
To further confirm the roles of the NLR and RPR in
predicating cardiovascular events, the correlation between the NLR
or RPR and other cardiovascular function parameters in the HCE
group were analyzed. In the HCE group, the NLR and RPR were
positively correlated with serum BNP, cTnI and CK-MB (all
P<0.05; Fig. 4). In order to
investigate the correlations between the NLR or RPR and ST segment
changes in the ECG, the HCE patients were divided into two groups
based on whether ST segment changes were observed on the ECG (ST
segment changes group and no ST segment changes group). The NLR and
RPR in the ST segment changes group were significantly higher
compared with those in the no ST segment changes group (P<0.0001
for each; Fig. 5A and B).
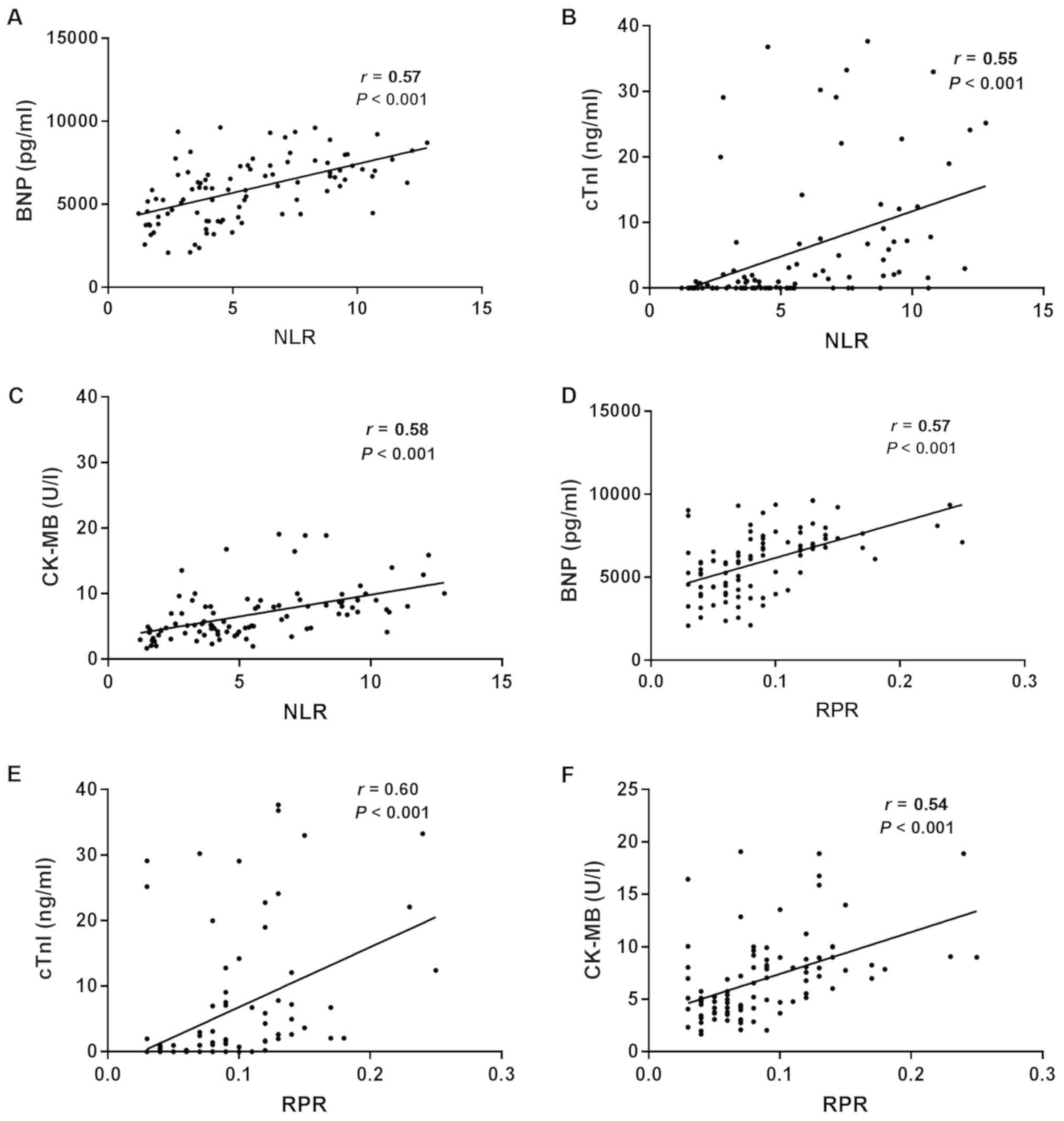 | Figure 4Correlation between NLR, RPR and BNP,
cTnI and CK-MB in HCE patients. (A) BNP vs. NLR, (B) cTnI vs. NLR,
(C) CK-MB vs. NLR, (D) BNP vs. RPR, (E) cTnI vs. RPR and (F) CK-MB
vs. RPR. BNP, brain natriuretic peptide; cTnI, cardiac troponin I;
CK-MB, creatine kinase isoenzyme MB; NLR, neutrophil-to-lymphocyte
ratio; RPR, red blood cell distribution width-to-platelet
ratio. |
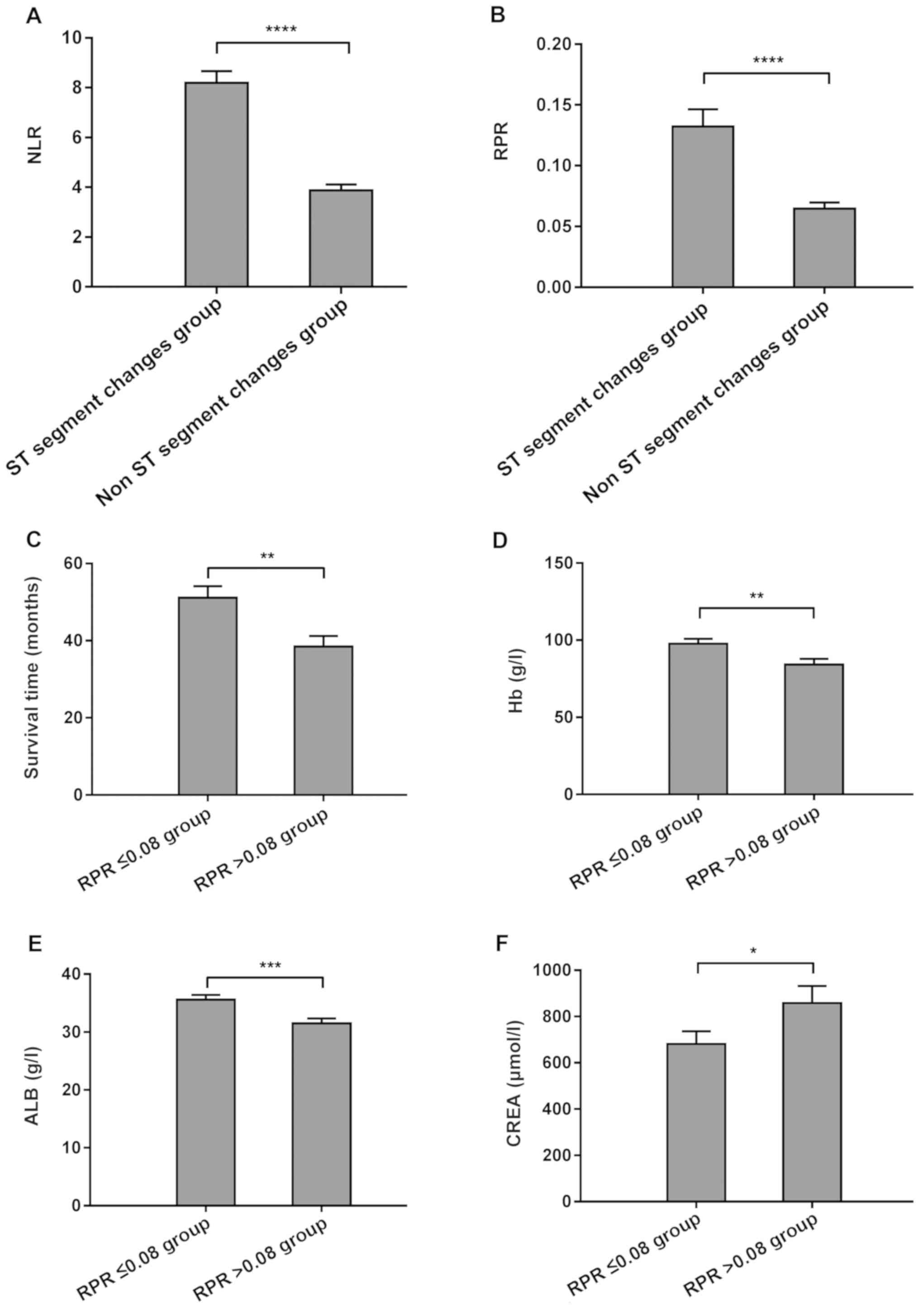
 | Figure 5Associations between NLR or RPR and
clinicopathological parameters of HCE patients. (A) NLR in HCE
patients with and without ST segment changes; (B) RPR in HCE
patients with and without ST segment changes. (C) Survival time,
(D) Hb levels, (E) ALB and (F) CREA in HCE patients with RPR
>0.08 and ≤0.08. *P<0.05, **P<0.01,
***P<0.001, ****P<0.0001. ALB, serum
albumin; Hb, hemoglobin; CREA, creatinine; NLR,
neutrophil-to-lymphocyte ratio; RPR, red blood cell distribution
width-to-platelet ratio; HCE patients, hemodialysis patients with
cardiovascular events. |
Predictive value of NLR and RPR
regarding cardiovascular events and survival in hemodialysis
patients
To determine the predictive value of the NLR and RPR
regarding the prediction of cardiovascular events in hemodialysis
patients and their survival, the HCE patients were divided into two
groups based on treatment outcomes, namely the recovery/improvement
group and the treatment failure/death group. AUC analysis was then
performed for the NLR and RPR to predict cardiovascular events in
hemodialysis patients. The AUC analysis revealed that the RPR was
an independent risk factor for the prognosis of cardiovascular
events in hemodialysis patients (Table
IV). The correlations between the RPR and other prognostic
parameters of cardiovascular events in hemodialysis patients of the
HCE group were then analyzed by dividing them into two groups
according to the cutoff value for RPR (0.08), namely the RPR ≤0.08
group and RPR >0.08 group. The levels of Hb and ALB in the RPR
>0.08 group were significantly lower compared with those in the
RPR ≤0.08 group (P<0.05 each), whereas the level of CREA in the
RPR >0.08 group was significantly higher compared with that in
the RPR ≤0.08 group (P<0.05). The survival time in the RPR
>0.08 group was significantly shorter compared with that in the
RPR ≤0.08 group (P<0.05 each; Fig.
5C-F).
 | Table IVAssociation of RPR with prognosis
regarding cardiovascular events in hemodialysis patients: OR
(95%CI) using binary logistic regression. |
Table IV
Association of RPR with prognosis
regarding cardiovascular events in hemodialysis patients: OR
(95%CI) using binary logistic regression.
| | Prognosis | | | | |
|---|
| RPR | Treatment
failure/death group |
Recovery/improvement group | χ2 | P-value | OR | 95% CI |
|---|
| >0.08 | 28 | 12 | 11.65 | <0.01 | 4.42 | 1.88-10.38 |
| ≤0.08 | 19 | 36 | | | | |
Discussion
In the present study, the role of the NLR and RPR in
predicting the occurrence of cardiovascular events in hemodialysis
patients and their prognosis was analyzed. Compared with those in
patients from the HNCE group, the NLR and RPR were higher in
patients from the HCE group. Positive associations between
increased NLR and RPR and the incidence of cardiovascular events in
hemodialysis patients were identified. The ROC analysis indicated a
good sensitivity and specificity of the RPR for predicting
cardiovascular events in hemodialysis patients. In addition, the
RPR was an independent risk factor for the survival prognosis of
cardiovascular events in hemodialysis patients. Encouragingly, the
present study also showed that, RPR has a good relationship with
other prognostic parameters of cardiovascular events in
hemodialysis patients. The NLR and the RPR were correlated with
BNP, cTnI and CK-MB, and associated with ST segment changes in HCE
patients.
Microinflammation is the initial step in the
development of ‘inflammation-malnutrition-atherosclerosis’ in
hemodialysis patients with ESRD (18,19). The
state of microinflammation is closely associated with
cardiovascular events. The prevalence of microinflammation in
hemodialysis patients results in an increased risk of
cardiovascular events (20,21). The WBC count in the blood is closely
associated with systemic inflammation, such as the involvement of
neutrophils in vascular endothelial injury and atherosclerosis
(22). Lymphocytes and neutrophils
are subtypes of WBCs that participate in the pathogenesis of
various diseases and serve important roles in the immune defense
system of the body (23,24). Peripheral blood neutrophils are
highly regulated and their count is significantly increased during
infection (25). The neutrophil
count reflects the inflammatory state in the course of disease
progression, while the presence and abundance of lymphocytes
represent the outcome of regulated immunity (26,27). Of
note, blood viscosity plays a key role in the determination of
atherosclerosis-related thrombosis (28). During the complex process, hematocrit
is a key indicator. Lu et al (29), indicated that the low level of ALT
prior to hemodialysis in patients with chronic renal failure may be
due to hemodilution. In previous studies, the NLR was reported to
be associated with cardiovascular events to reflect the
inflammatory state in hemodialysis patients (30,31).
In the present study, the total WBC count and
neutrophil count in the HCE group were significantly higher
compared with those in the HNCE group, but the lymphocyte count in
the serum was significantly lower compared with that in the HNCE
group. Binary logistic regression analysis suggested that the NLR
was an independent factor for predicting cardiovascular events in
hemodialysis patients, but not for prognosis in the HCE group.
However, the NLR was significantly different between the HCE and
HNCE groups, with lower sensitivity and specificity compared with
RPR. The NLR was positively correlated with the BNP, cTnI and
CK-MB, and associated with ST segment changes in HCE patients.
The association between the RDW and cardiovascular
events in hemodialysis patients has been investigated in several
studies (32,33). It has been reported that an increased
RDW is an independent risk factor for cardiovascular death in
hemodialysis patients (34). As
platelets serve an important role in the occurrence and development
of cardiovascular events, the ability of the RPR, the combination
of the RDW and the platelet ratio, for predicting the occurrence
and development of cardiovascular events in hemodialysis patients,
as well as their prognosis, was assessed in the present study. It
was demonstrated that the RPR in patients from the HCE group was
significantly increased compared with that in patients from the
HNCE group. Furthermore, the RPR was correlated with the severity
of cardiovascular events in HCE patients. The RPR was an
independent predictive factor for the incidence of cardiovascular
events in hemodialysis and HCE patients. In addition, the RPR had
good sensitivity and specificity for predicting cardiovascular
events in hemodialysis patients.
In conclusion, the present study demonstrated the
value of the NLR and RPR in predicting the occurrence, development
and prognosis of cardiovascular events in hemodialysis patients.
The NLR and RPR were able to predict the occurrence and development
of cardiovascular events in hemodialysis patients, among which RPR
had a better efficacy. The RPR was also useful for predicting the
prognosis of HCE patients. Taken together, the present results
suggest that these routinely available parameters, which may be
obtained non-invasively and economically, may be repurposed as
novel diagnostic parameters for cardiovascular events in
hemodialysis patients.
Acknowledgements
Not applicable.
Funding
This research was supported by the Youth Medical
Talent of Jiangsu Province (grant no. QNRC2016163 to JL).
Availability of data and materials
All data generated or analyzed during this study are
included in the published article.
Authors' contributions
XZ contributed to the conception and design of the
study, acquisition of data, analysis and interpretation of data,
and drafting of the manuscript. GL and SL contributed to the
statistical analysis. ZG contributed to the conception and
supervision of the study, and the critical revision of the
manuscript. JL and SS contributed to the study conception and
design, study supervision and critical revision of the
manuscript.
Ethics approval and consent to
participate
The present study was approved by The Ethics
Committees of the First People's Hospital of Yancheng (Yancheng,
China) and the Fifth People's Hospital of Wuxi (Wuxi, China), and
was performed in accordance with the Declaration of Helsinki.
Informed consent was obtained from each patient.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Jaykumar AB, Caceres PS, King-Medina KN,
Liao TD, Datta I, Maskey D, Naggert JK, Mendez M, Beierwaltes WH
and Ortiz PA: Role of Alström syndrome 1 in the regulation of blood
pressure and renal function. JCI Insight. 3(95076): Epub ahead of
print. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kaur G, Singh J and Kumar J: Vitamin D and
cardiovascular disease in chronic kidney disease. Pediatr Nephrol.
34:2509–2522. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lundquist AL and Nigwekar SU: Optimal
management of bone mineral disorders in chronic kidney disease and
end stage renal disease. Curr Opin Nephrol Hypertens. 25:120–126.
2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Krolewski AS, Skupien J, Rossing P and
Warram JH: Fast renal decline to end-stage renal disease: An
unrecognized feature of nephropathy in diabetes. Kidney Int.
91:1300–1311. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Schmitt R: ZAG-a novel biomarker for
cardiovascular risk in ESRD patients? Kidney Int. 94:858–860.
2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
O'Shaughnessy MM, Liu S, Montez-Rath ME,
Lafayette RA and Winkelmayer WC: Cause of kidney disease and
cardiovascular events in a national cohort of US patients with
end-stage renal disease on dialysis: A retrospective analysis. Eur
Heart J. 40:887–898. 2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Lu W and Jiang GR and Jiang GR: HD/HP
versus HD trial Group. Randomised, open-label, multicentre trial
comparing haemodialysis plus haemoperfusion versus haemodialysis
alone in adult patients with end-stage renal disease (HD/HP vs HD):
Study protocol. BMJ Open. 8(e022169)2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Liu CC, Chou LP, Chen TS, Chen CA and Tsai
YF: Significant association of anti-platelet factor 4/heparin
antibody with cardiovascular disease in hemodialysis patients: A
longitudinal 7-year study. Int Urol Nephrol. 50:2289–2297.
2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Takahashi G, Honda H, Takahashi K, Ikeda
M, Hosaka N, Ogata H, Koiwa F, Shishido K and Shibata T: Truncal
adiposity influences high-density lipoprotein cholesterol levels
and cardiovascular events in hemodialysis patients. J Ren Nutr.
29:235–242. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Balta S: Mean platelet volume,
neutrophil-lymphocyte ratio, and long-term major cardiovascular
events. Angiology. 70:289–290. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yin Y, Wang J, Wang X, Gu L, Pei H, Kuai
S, Zhang Y and Shang Z: Prognostic value of the neutrophil to
lymphocyte ratio in lung cancer: A meta-analysis. Clinics (São
Paulo). 70:524–530. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Chávez Valencia V, Orizaga de la Cruz C,
Mejía Rodríguez O, Gutiérrez Castellanos S, Lagunas Rangel FA and
Viveros Sandoval ME: Inflammation in hemodialysis and their
correlation with neutrophil-lymphocyte ratio and platelet-
lymphocyte ratio. Nefrologia. 37:554–556. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
DiGangi C: Neutrophil-lymphocyte ratio:
Predicting cardiovascular and renal complications in patients with
diabetes. J Am Assoc Nurse Pract. 28:410–414. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Chen X, Shen B, Zou J, Liu Z, Lv W, Cao X,
Yu J, Nie Y, Xu J, Wang L, et al: The prognostic value of red blood
cell distribution width in patients on maintenance hemodialysis.
Blood Purif. 42:314–321. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Mo L, Chen Y, Li Z, Xu L, Dong W, Zhang L,
Liang H, Li R, Tao Y, Shi W, et al: Red blood cell distribution
width as a marker of cerebral infarction in hemodialysis patients.
Ren Fail. 39:712–718. 2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Hvas AM and Neergaard-Petersen S:
Influence of exercise on platelet function in patients with
cardiovascular disease. Semin Thromb Hemost. 44:802–812.
2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Weckmann GFC, Stracke S, Haase A, Spallek
J, Ludwig F, Angelow A, Emmelkamp JM, Mahner M and Chenot JF:
Diagnosis and management of non-dialysis chronic kidney disease in
ambulatory care: A systematic review of clinical practice
guidelines. BMC Nephrol. 19(258)2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Mitsides N, Cornelis T, Broers NJH,
Diederen NMP, Brenchley P, van der Sande FM, Schalkwijk CG, Kooman
JP and Mitra S: Extracellular overhydration linked with endothelial
dysfunction in the context of inflammation in haemodialysis
dependent chronic kidney disease. PLoS One.
12(e0183281)2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Tian J, Hou X, Hu L, Chen T, Wu K, Cai C
and Bai X: Efficacy comparison of atorvastatin versus rosuvastatin
on blood lipid and microinflammatory state in maintenance
hemodialysis patients. Ren Fail. 39:153–158. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Tsirpanlis G, Bagos P, Ioannou D, Bleta A,
Marinou I, Lagouranis A, Chatzipanagiotou S and Nicolaou C: The
variability and accurate assessment of microinflammation in
haemodialysis patients. Nephrol Dial Transplant. 19:150–157.
2004.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zhang J, Hua G, Zhang X, Tong R, Du X and
Li Z: Regulatory T cells/T-helper cell 17 functional imbalance in
uraemic patients on maintenance haemodialysis: A pivotal link
between microinflammation and adverse cardiovascular events.
Nephrology (Carlton). 15:33–41. 2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Lu J, Xiang G, Liu M, Mei W, Xiang L and
Dong J: Irisin protects against endothelial injury and ameliorates
atherosclerosis in apolipoprotein E-Null diabetic mice.
Atherosclerosis. 243:438–448. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Anne Morrison C, Moran A, Patel S,
Vidaurre MP, Carrick MM and Tweardy DJ: Increased apoptosis of
peripheral blood neutrophils is associated with reduced incidence
of infection in trauma patients with hemorrhagic shock. J Infect.
66:87–94. 2013.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Horvathova L, Tillinger A, Sivakova I,
Mikova L, Mravec B and Bucova M: Chemical sympathectomy increases
neutrophil-to-lymphocyte ratio in tumor-bearing rats but does not
influence cancer progression. J Neuroimmunol. 278:255–261.
2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Havenstein N, Langer F, Stefanski V and
Fietz J: It takes two to tango: Phagocyte and lymphocyte numbers in
a small mammalian hibernator. Brain Behav Immun. 52:71–80.
2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Jaffey JA, Amorim J and DeClue AE: Effects
of calcitriol on apoptosis, toll-like receptor 4 expression, and
cytokine production of endotoxin-primed canine leukocytes. Am J Vet
Res. 79:1071–1078. 2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Feng F, Zheng G, Wang Q, Liu S, Liu Z, Xu
G, Wang F, Guo M, Lian X and Zhang H: Low lymphocyte count and high
monocyte count predicts poor prognosis of gastric cancer. BMC
Gastroenterol. 18(148)2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Xiang F, Chen R, Cao X, Shen B, Liu Z, Tan
X, Ding X and Zou J: Monocyte/lymphocyte ratio as a better
predictor of cardiovascular and all-cause mortality in hemodialysis
patients: A prospective cohort study. Hemodial Int. 22:82–92.
2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Lu X, Wang S, Zhang G, Xiong R and Li H:
High neutrophil-to-lymphocyte ratio is a significant predictor of
cardiovascular and all-cause mortality in patients undergoing
peritoneal dialysis. Kidney Blood Press Res. 43:490–499.
2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Lippi G, Targher G, Montagnana M, Salvagno
GL, Zoppini G and Guidi GC: Relationship between red blood cell
distribution width and kidney function tests in a large cohort of
unselected outpatients. Scand J Clin Lab Invest. 68:745–748.
2008.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Tarantino G, Barrea L, Capone D, Citro V,
Mosca T and Savastano S: Hematocrit values predict carotid
intimal-media thickness in obese patients with non-alcoholic fatty
liver disease: A cross-sectional study. Front Endocrinol
(Lausanne). 9(203)2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Lopes EP, Sette LH, Sette JB, Luna CF,
Andrade AM, Moraes M, Sette PC, Menezes R, Cavalcanti RL and
Conceição SC: Serum alanine aminotransferase levels, hematocrit
rate and body weight correlations before and after hemodialysis
session. Clinics (São Paulo). 64:941–945. 2009.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Yoon HE, Kim SJ, Hwang HS, Chung S, Yang
CW and Shin SJ: Progressive rise in red blood cell distribution
width predicts mortality and cardiovascular events in end-stage
renal disease patients. PLoS One. 10(e0126272)2015.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Czyzewski L, Wyzgal J, Czyzewska E,
Kurowski A, Sierdzinski J, Truszewski Z and Szarpak L: Assessment
of arterial stiffness, volume, and nutritional status in stable
renal transplant recipients. Medicine (Baltimore).
95(e2819)2016.PubMed/NCBI View Article : Google Scholar
|