Introduction
Conventional filtering surgery is currently the gold
standard in surgical management of glaucoma not controlled with
medication (1) However, the high
risk of potentially vision-threatening peri- and postoperative
complications, combined with the failure rates associated with
standard trabeculectomy, delay surgical intervention.
Intra-operative complications associated with tissue manipulation,
such as inadequate scleral flap thickness and bleeding, may
compromise the outcome of the procedure. Postoperatively, hypotony
is a common, serious complication, which can persist in a small
percentage of cases, and is associated with flat anterior chamber
(A/C), corneal edema, cataract formation, maculopathy and loss of
vision. Other less common complications, but more difficult in
terms of management, include pupillary block, suprachoroidal
hemorrhage and aqueous misdirection (2). Fibroblastic proliferation and
sub-conjunctival fibrosis are the main challenges during follow up
as they lead to trabeculectomy failure. Antifibrotic agents are
currently used in an order to control fibrosis and sustain bleb
morphology, prolonging the hypotonic effect of the procedure.
However, the latter are associated with their own complications, of
which late-onset bleb leaks and bleb-related endophthalmitis are
the most serious (3,4). In an attempt to design a safe and
consistent surgical procedure, the present retrospective study
aimed to evaluate the effect and safety of a modified
trabeculectomy technique, stab incision mitomycin C (MMC)-assisted
rapid trabeculectomy (SMART), in achieving low intraocular pressure
(IOP) in primary patients with glaucoma.
Patients and methods
Patients
A total of 41 eyes with indication for
trabeculectomy underwent glaucoma surgery (31 eyes isolated
glaucoma surgery and 10 eyes combined cataract-glaucoma surgery).
Surgery indications were uncontrolled IOP on full medical
treatment, severe side effects to glaucoma medication and poor
compliance to treatment. Indication for combined
phacoemulsification with SMART (phaco-SMART) was Best Corrected
Visual Acuity <5/10. All surgical procedures were performed by
the same surgeon. There was no significant difference concerning
age, sex, preoperative IOP and number of preoperative glaucoma
medications between eyes undergoing SMART or phaco-SMART. The
primary exclusion criteria were angle closure glaucoma, secondary
glaucoma and cases where medical notes were unavailable or
incomplete. Patient characteristics are presented in Table I. Informed consent was obtained from
all patients prior to surgery and all data were collected according
to the principles of The Declaration of Helsinki. The Ethics
Committee of The Konstantopouleio-Patission General Hospital
approved the present study (reference no. 49/2.2.2017).
 | Table IPreoperative and postoperative patient
data. |
Table I
Preoperative and postoperative patient
data.
| Clinicopathological
characteristic | SMART, n=31 | phaco-SMART,
n=10 | P-value | Total, n=41 |
|---|
| Sex | | | | |
|
Male,
eyes | 15 | 9 | - | 24 |
|
Female,
eyes | 16 | 1 | - | 17 |
| Age, years | 72±10.16 | 70±7.87 | 0.1051 | 70.50±9.59 |
| Pre-operative IOP,
mmHg | 25.50±9.27 | 18.50±3.57 | 0.0255 | 23.80±8.75 |
| Postoperative IOP,
mmHg | | | | |
|
1st
week | 7.10±4.67 | 5.90±2.88 | 0.4389 | 6.80±4.30 |
|
1st
month | 9.00±3.66 | 11.50±2.99 | 0.0607 | 9.60±3.63 |
|
3rd
month | 10.20±4.9 | 10.90±2.73 | 0.6554 | 10.40±4.28 |
|
6th
month | 9.40±4.39 | 11.90±2.73 | 0.1013 | 10.00±4.16 |
|
1st
year | 10.70±3.31 | 12.00±2.67 | 0.2588 | 11.00±3.19 |
| Final visit IOP,
mmHg | 11.70±3.30 | 11.80±2.93 | 0.5982 | 11.70±3.19 |
| Follow-up time,
months | 29.30±11.80 | 22.40±9.99 | 0.1051 | 27.60±11.66 |
| IOP
decreasea, mmHg | 13.80±9.73 | 6.70±4.52 | 0.0102 | 12.10±9.44 |
| No. of
medications | | | | |
|
Preoperative | 3.40±1.38 | 3.00±1.33 | 0.4803 | 3.30±1.36 |
|
Postoperative | 0.70±1.05 | 0.60±1.07 | 0.8407 | 0.70±1.04 |
| Reduction in no. of
medications | 2.70±1.87 | 2.40±1.26 | 0.6650 | 2.60±1.73 |
| Complications,
n | | | | |
|
Shallow
A/C | 8 | 5 | - | 13 |
|
Hypotony | 1 | 0 | - | 1 |
|
Bleb
leak | 2 | 0 | - | 2 |
Pre-operative management
Careful assessment of the ocular surface was
performed prior to surgery. All patients were prepared 1 week
pre-operatively with fluorometholone drops, adequate lubrication of
ocular surface with tear substitutes, as well as proper lid
hygiene. Discontinuation of topical treatment and IOP management
with Acetazolamide per os was suggested in cases where IOP
permitted it.
Surgical techniques
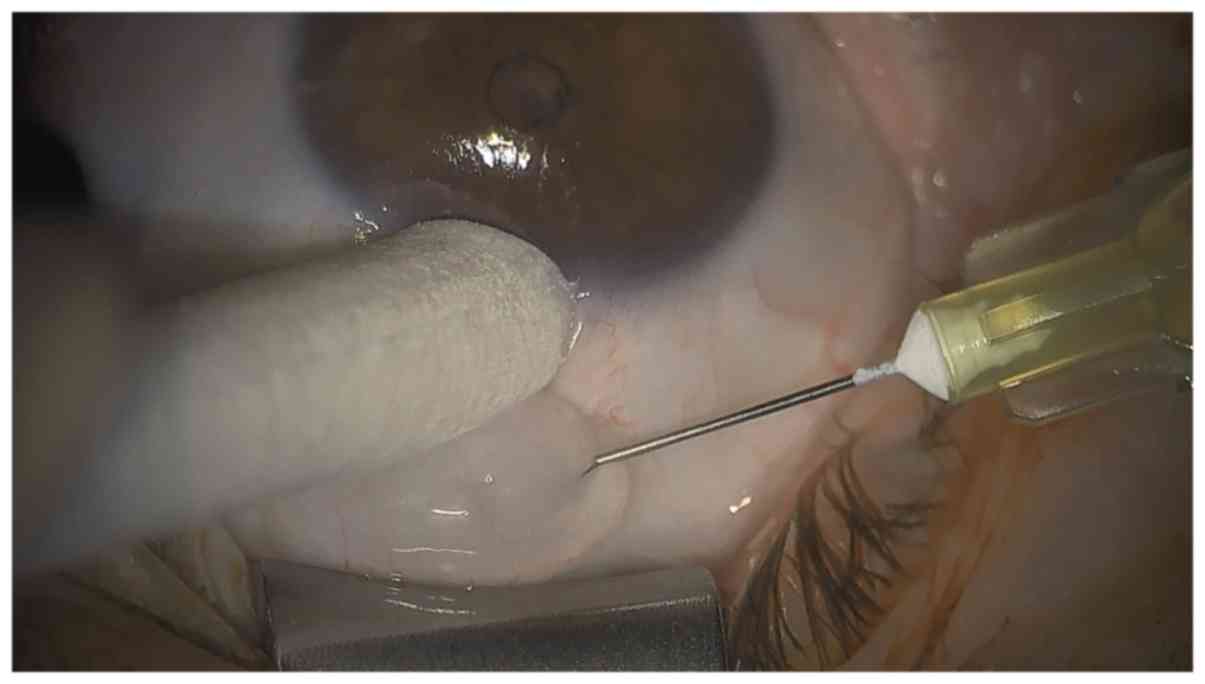
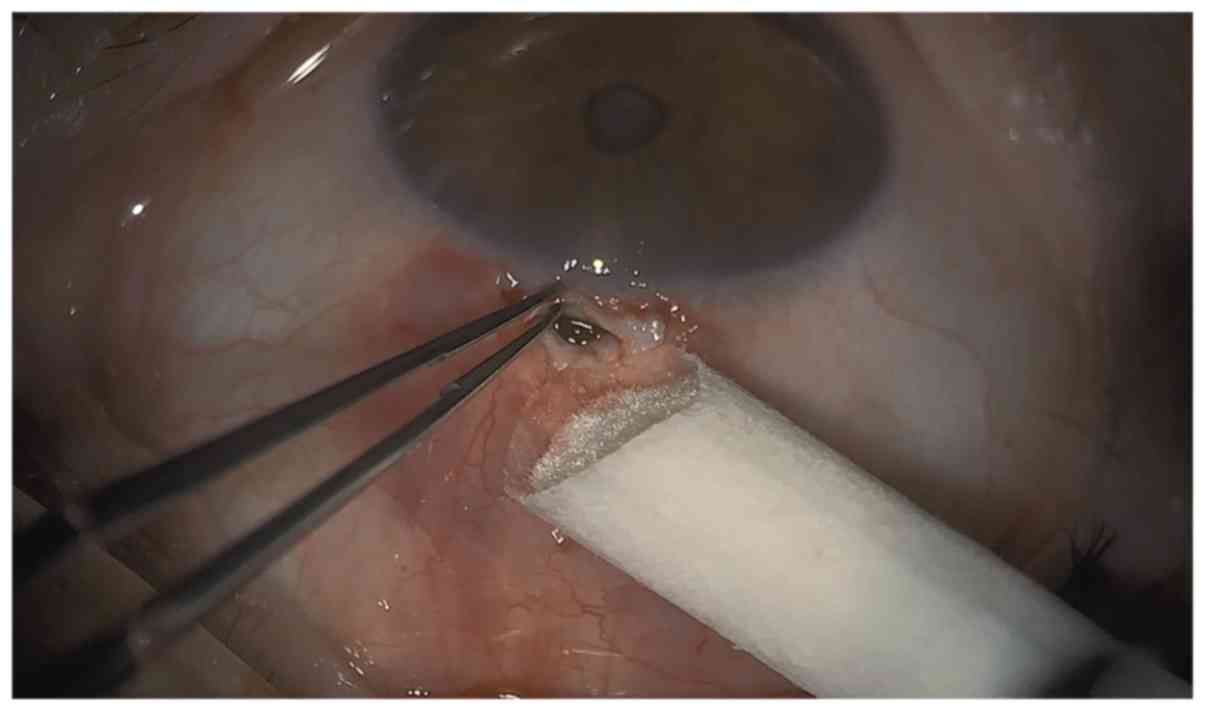
Immediately pre-operatively, a single application of
2% pilocarpine was instilled into the operative eye, while typical
mydriasis with phenylephrine and tropicamide was performed in the
phaco-SMART cases. Following insertion of a lid speculum, topical
anesthesia with 0.5% proxymetacaine was administered. A single dose
of 0.1 ml lidocaine mixed with 0.005 mg MMC was injected into the
superior subconjunctiva, ~8 mm from limbus and evenly spread
towards the limbus with a sponge tip up to 2 mm from limbus
(Fig. 1). Immediate irrigation
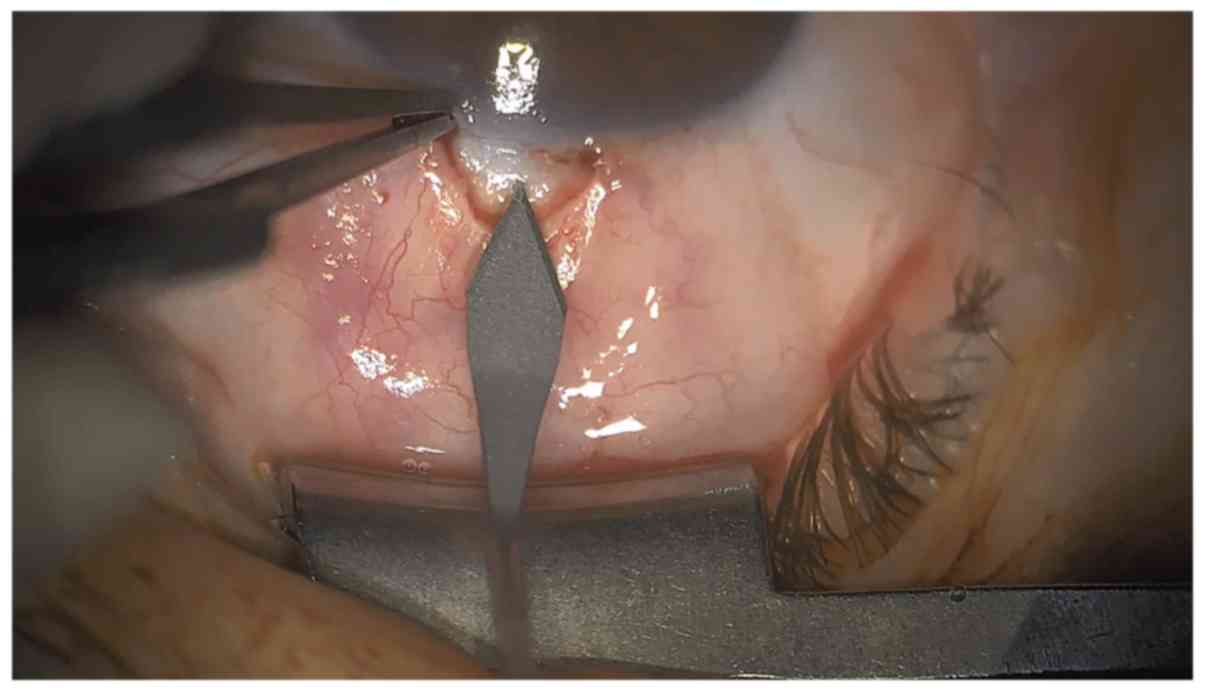
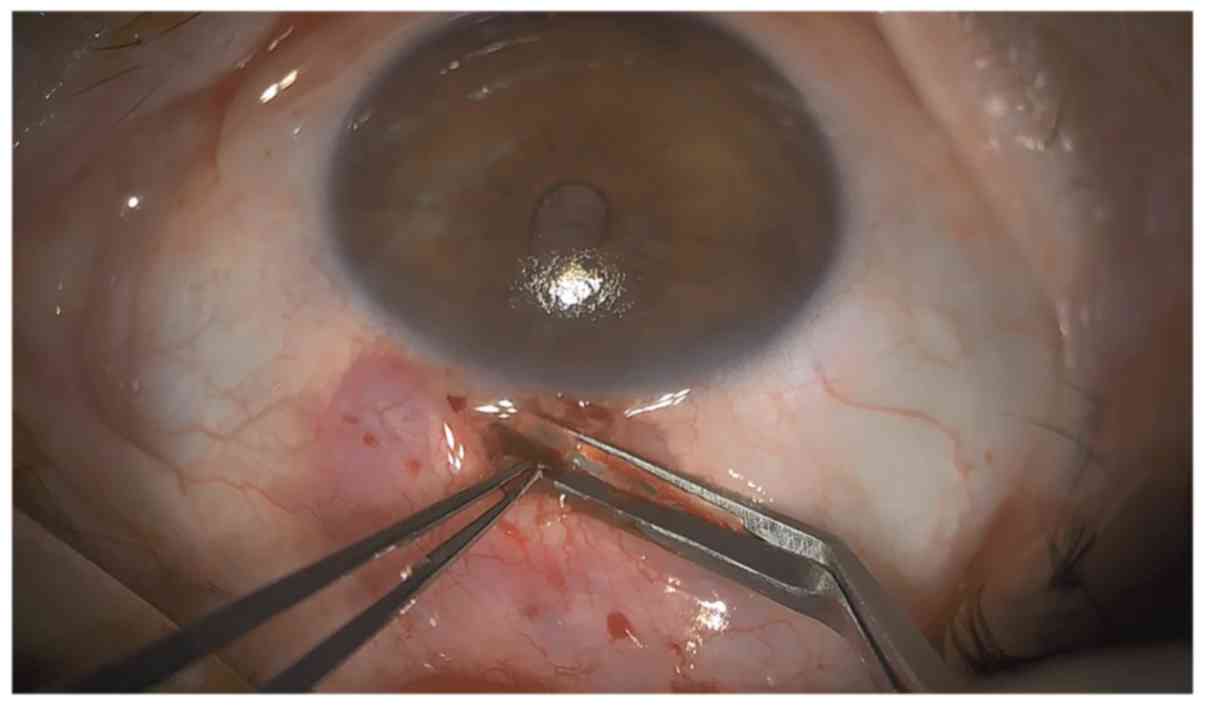
followed. A 3.5-mm fornix-based conjunctival opening was made with
careful Tenon's capsule separation from episclera as superiorly as
possible. Cautery of underlying sclera was done in the region where
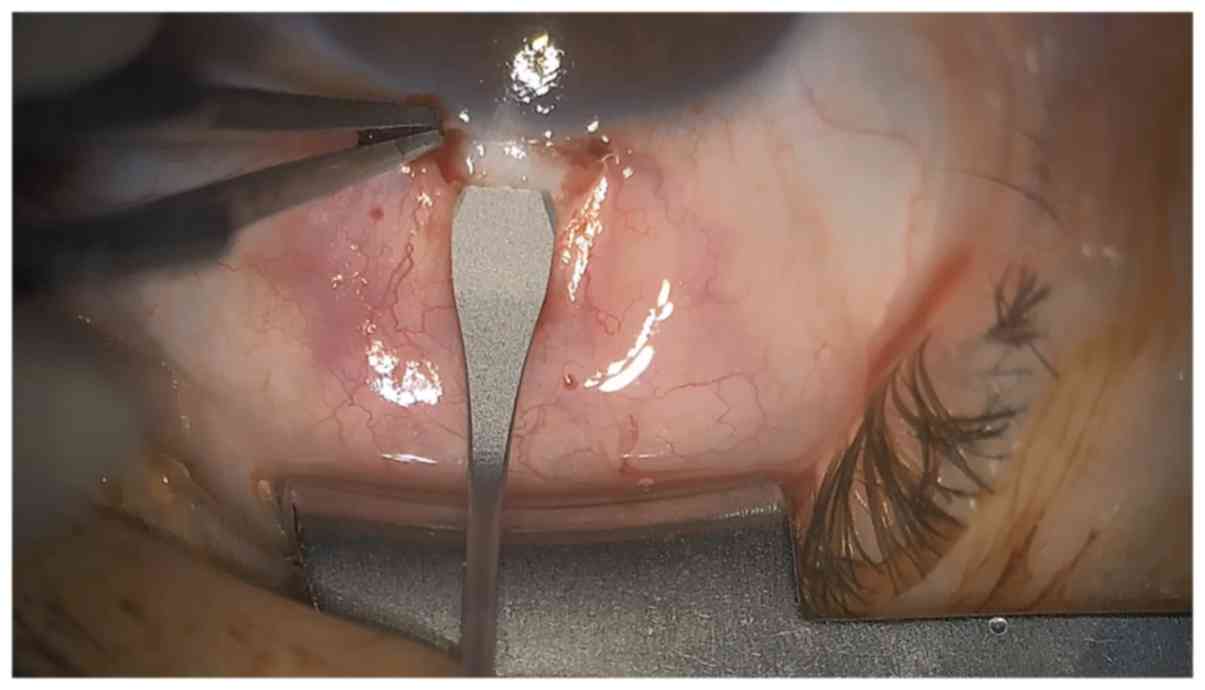
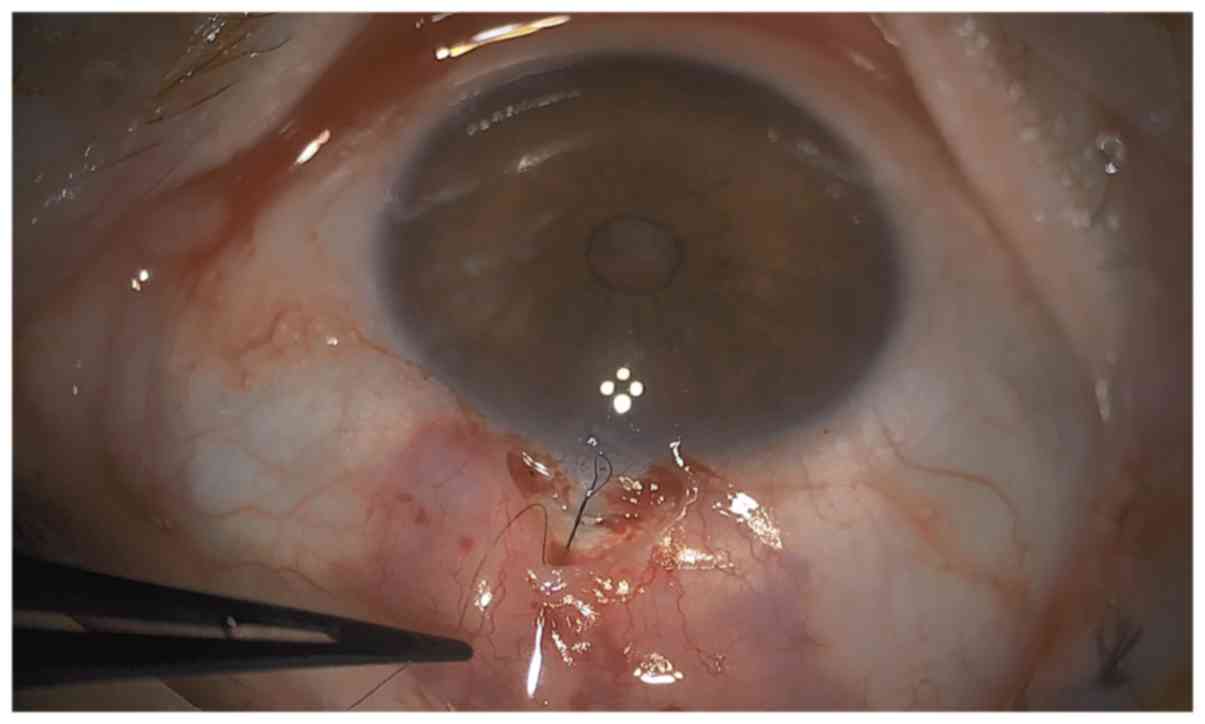
the incision was to be made. A stab incision was performed with a
2.4-mm bevel up slit cataract knife, entering the A/C 1.5 mm
posterior to limbus (Figs. 2 and
3), with slow retraction of the
knife and immediate A/C fill with visco-elastic substance through
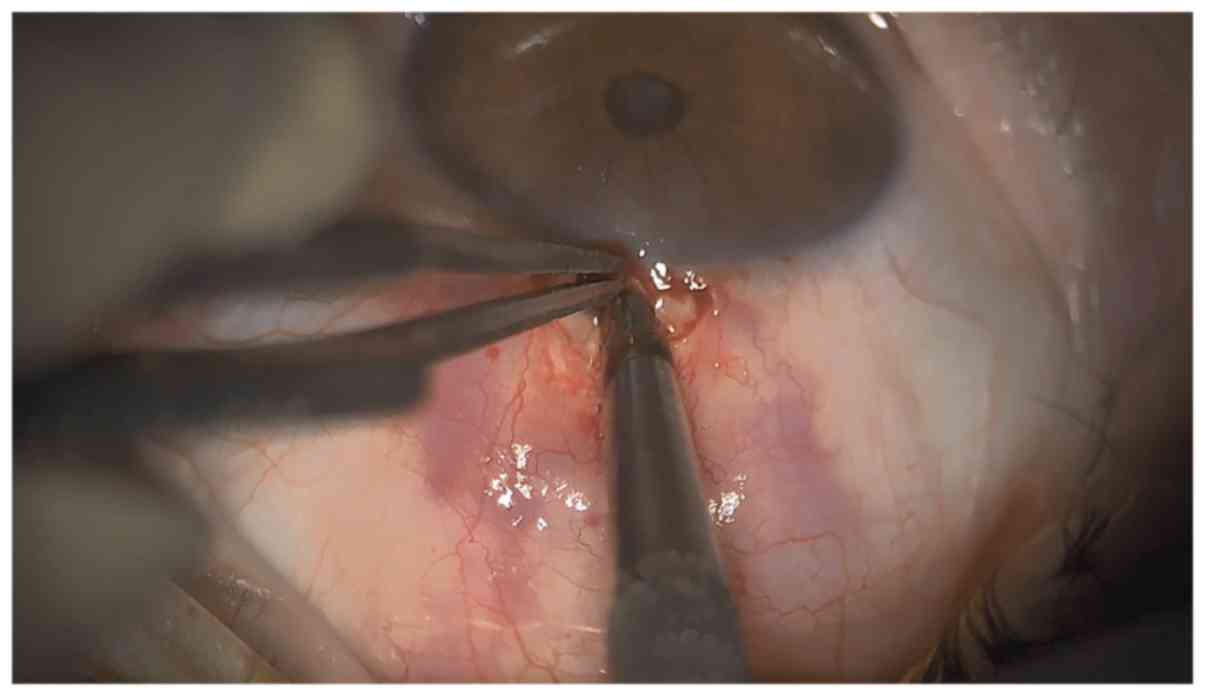
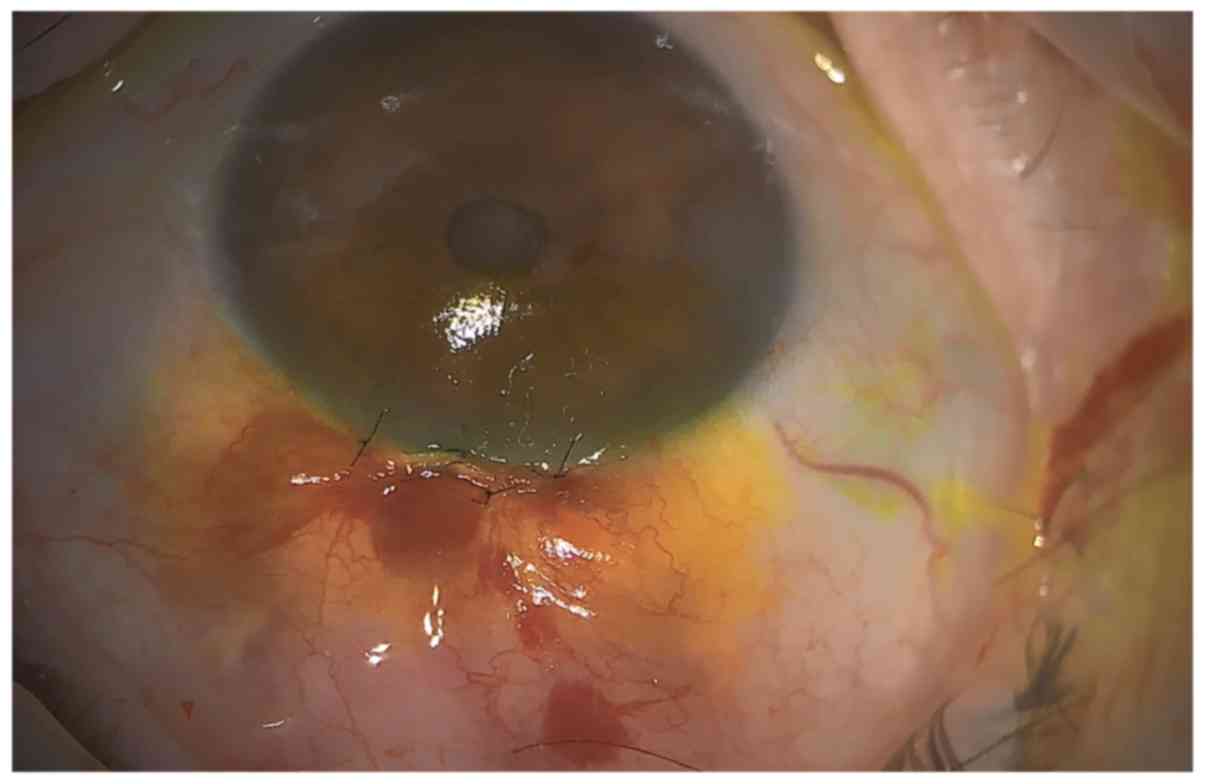
the stab incision. A double punch with the 0.75-mm Kelly punch
followed (Figs. 4 and 5). Peripheral iridectomy was performed and
one releasable suture (10-0 nylon) was placed to secure the opening
(Figs. 6 and 7). Matrix sutures (10-0 nylon) were used to
close the conjunctiva (Fig. 8).
In the SMART procedure, a side port was made at the
end of the procedure, in order to administer intracameral
cefuroxime and for postoperative management if necessary. In the
phaco-SMART cases, phacoemulsification was performed with clear
cornea incision at 105̊ and quick chop technique,
followed by SMART as described. Closure of incisions was made by
stroma hydration. At the end of the procedure, a soft contact lens
and a protective shell was applied to all patients.
Postoperative management
A strict follow-up schedule and medication scheme
was followed in all cases. Follow-up visits were made on the
1st, 3rd, 7th and 15th
days, followed by 1st, 3rd and 6th
months postoperatively. Follow-up was scheduled as necessary after
the initial 6-month period, with a minimum of two visits per year.
During follow-up visits, careful evaluation of bleb (position,
appearance and vascularity), A/C status, IOP and fundus was
performed. Additional 5-fluorouracil (5-FU) injections were
administered when beginning of encapsulation was suspected. The
standard protocol for postoperative medication is presented in
Table II.
 | Table IIPostoperative medication
protocol. |
Table II
Postoperative medication
protocol.
| Week
post-surgery |
Dexamethasone+Chloramphenicol | Dexamethasone
(preservative-free) | Bromfenac |
|---|
| Week 1 | 4 times a day | 3 times a day | 2 times a day |
| Week 2 | - | 6 times a day | 2 times a day |
| Week 3+4 | - | 5 times a day | 2 times a day |
| Week 5+6 | - | 4 times a day | 2 times a day |
| Week 7+8 | - | 3 times a day | - |
| Week 9+10 | - | 2 times a day | - |
Statistical analysis
Student's t-tests and χ2 tests were used
for comparison of the mean of the variables. The Mann-Whitney U
test was performed if data were not distributed normally. The
results are presented as the mean ± SD and as percentages where
appropriate. All statistical analyses were carried out using SPSS
21.0 (IBM, Corp.). P<0.05 was considered to indicate a
statistically significant difference.
Results
Hypotonic effect
There were no intra-operative complications.
Operation time from conjunctival opening to closure was 26.71±5.55
min for SMART and 36.60±1.95 min for phaco-SMART cases. The
follow-up period ranged from 12-46 months with a mean follow-up of
27.6±11.66 months. Mean IOP during follow-up tended to be lower in
the SMART cases but there was no statistically significant
difference, compared with phaco-SMART. The mean final IOP was
11.7±3.19 mmHg, which is a reduction of 12.1±9.44 mmHg, compared
with the pre-operative IOP. Specifically, at the 12-month follow-up
mark, which all patients reached, the mean IOP was 11±3.19 mmHg
(P<0.00001) with 0.7±1.04 mean number of medications
(P<0.00001), a reduction of 12.1±9.44 mmHg in IOP and 2.6±1.73
in the number of medications.
Bleb modulation
During follow-up, 22 out of 31 cases undergoing the
SMART procedure needed additional 5-FU injections, (mean 1.45±1.87
injections per eye) compared with 8 out of 10 cases in phaco-SMART
(mean 1.9±2.57 injections per eye; P=0.5841). No complaints were
reported by the patients concerning 5-FU injections.
Complications
Hypotony (defined as IOP ≤2 mmHg) occurred in one
case due to overfiltration of the bleb and was managed with
compressive sutures over the conjunctiva. This patient had
undergone the phaco-SMART approach; the sutures were removed after
2 weeks and up to 17 months postoperatively with two additional
5-FU injections, IOP remained at 10 mmHg. The most common
observation 1st day postoperatively was shallow A/C
(>1.5 mm; 13 out of 41 cases). Small choroidal detachment (<2
clock h) was usually observed a few days later (11 of the
aforementioned cases), and no choroidal folds or maculopathy
occurred in these cases. Typical management of shallow anterior
chamber with or without choroidal detachment was reformation of the
A/C with viscoelastic substance through the side ports when needed,
with none of these patients needing additional intervention in the
next follow-up visits. Patient data confirm that visual acuity
remained unaffected in these patients, with no impact on
postoperative trajectory or final IOP (data not shown). No flat A/C
was observed. Wound leak appeared in two cases (on the
1st and 3rd postoperative day) and was
managed by resuturing the conjunctiva. No major complications,
including persistent hypotony, maculopathy or bleb related
complication occurred, with all eyes maintaining an IOP <15 mmHg
(Table I).
Discussion
Trabeculectomy has undergone many changes since it
was first described by Cairns (4) in
1968, with many approaches and modifications to the traditional
procedure. The modifications that forged the technique described in
the present study aimed to minimize intraoperative tissue handling,
as well as pre- and postoperative inflammation.
One of the common causes for trabeculectomy failure
is fibrosis due to the wound healing response, appearing as
subconjunctival fibrosis of the bleb or as sub-Tenon's
encapsulation. It is recognized that an inflamed conjunctiva
compromises the success of trabeculectomy, because the conjunctival
scarring reaction is already activated (5). A pre-operative adjustment of glaucoma
medications has been adopted by many glaucoma surgeons, reducing
the number of drops preserved with benzalkonium chloride and/or
changing to preservative-free medication, in the weeks prior to
surgery (6). Additionally, evidence
suggested that 1-month pre-operative fluorometholone, improved the
state of the conjunctiva (7). Hence,
careful pre-operative preparation has long been the standard
approach with all glaucoma-filtering surgeries.
Antimetabolites are used in various concentrations,
usually in the form of sponges, in an attempt to reduce
postoperative fibrosis (8). However,
their use is not without risks, as bleb infection or leak,
hypotony, maculopathy, corneal epithelial toxicity and
endophthalmitis have been frequently reported with the
intra-operative use of MMC (9). The
use of intra-operative MMC in the form of sub-conjunctival
injection has been previously described with similar efficacy and
safety to MMC-soaked sponges but with a more favorable bleb
morphology and a predictable dose of delivery (9,10). In
addition, the reduced conjunctival manipulation with injection and
shorter waiting time compared with MMC sponges supported the use of
this approach in the present study, as it has been shown to reduce
the occurrence of fibrosis (11-17).
In the present study, a low MMC concentration (0.005 mg/0.1 ml) was
used in an attempt to minimize the side effects of MMC, which is
half the minimum dose described in the literature (9,10).
Of note, various types of conjunctival opening
formation have been described in the literature, with fornix base
opening being associated with less cystic bleb formation (15). The smaller fornix base conjunctival
opening used in the present study limits conjunctival manipulation
and requires fewer sutures for closure.
Modifications that use a scleral tunnel have been
described in the past, with positive results (18-20).
Jacob et al (21) was the
first to describe a stab incision approach, with a 2.8-mm keratome.
The technique described in the present study technique differs from
this approach, since the 2.4-mm incision, does not include the
overlying conjunctiva. Moreover, the formation of a scleral tunnel
instead of a scleral flap, as well as the small conjunctival
opening contribute to less surgical time in the procedure used in
the present study.
In addition, the releasable suture to the scleral
incision creates a more guarded environment in order to avoid
postoperative hypotony. Regarding the choice of suture, it has been
documented that trabeculectomies performed with and without
releasable sutures resulted in equivalent efficacy in IOP control,
with releasable sutures resulting in a lower incidence of hypotony
and flat A/C (22).
The main purpose of close postoperative monitoring
is to frequently evaluate bleb morphology and to intervene with
bleb needling augmented with 5-FU, if encapsulation is suspected
(23). In the present study, most of
the patients needed 5-FU injections without needling when
encapsulation was suspected or bleb vascularity was increased. All
5-FU injections were performed during the initial ‘high-risk’
follow-up period (3 months), with three patients having 5-FU
injections after the first year, after they underwent
phacoemalsufication in the trabeculectomised eye. Previous studies
demonstrated that a timely intervention with 5-FU injections can
produce long-term IOP control in a high proportion of patients and
appears to play a significant role in avoiding further surgery
(24-26).
Shallow A/C and choroidal detachment were associated
with a diffuse bleb and low IOP immediately postoperatively.
However, no further management was required for these cases as
typically the depth of the A/C was normal by the scheduled visit on
the 7th postoperative day.
In conclusion, success rates after trabeculectomy
with target IOP ≤22 mmHg ≤86% without medication and 98% with
medication have been previously reported (27-30).
However, in the present study, all patients had IOP ≤15 mmHg on the
final visit, 63.4% without medication and 36.6% with ≤2
antiglaucoma agents. In conclusion, SMART with wound modulation
appears to be a safe and quicker alternative to classic
trabeculectomy. A lower dose of MMC showed good efficiency. Few
minor and no major complications were observed during the first 2.5
years of follow-up. All patients showed good IOP control. The
primary limitations of the present study are its retrospective,
non-comparative design and the small number of patients involved. A
larger multicenter prospective study is required to confirm the
results described in the present study.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
CT conceived and designed the study. AT and GD
obtained, analyzed and interpreted the data. AT drafted the
manuscript. CT critically revised the manuscript. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
Informed consent was obtained from all patients
prior to surgery and all data were collected according to the
principles of The Declaration of Helsinki. The Ethics Committee of
The Konstantopouleio-Patission General Hospital approved the
present study (reference no. 49/2.2.2017).
Patient consent for publication
The patients provided written informed consent for
the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Jay JL and Murray SB: Early trabeculectomy
versus conventional management in primary open angle glaucoma. Br J
Ophthalmol. 72:881–889. 1988.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Vijaya L, Manish P, Ronnie G and Shantha
B: Management of complications in glaucoma surgery. Indian J
Ophthalmol. 59:S131–S140. 2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lee DA: Antiproliferative therapy for
filtration surgery. In: Epstein, David et al. eds. Chandler
and Grant's Glaucoma, 4th ed. Baltimore: Williams & Wilkins:
527-528, 1997.
|
|
4
|
Cairns JE: Trabeculectomy Preliminary
report of a new method. Am J Ophthalmol. 66:673–679.
1968.PubMed/NCBI
|
|
5
|
Hawker MJ and Broadway DC: Preoperative
conjunctival health and trabeculectomy outcome. In: Glaucoma:
Surgical Management. 2nd edition. Shaarawy T, Sherwood MB,
Hitchings RA and Crowston JG (eds). Saunders, London, pp87-94,
2009.
|
|
6
|
Broadway DC, Grierson I, Stürmer J and
Hitchings RA: Reversal of topical antiglaucoma medication effects
on the conjunctiva. Arch Ophthalmol. 114:262–267. 1996.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Baudouin C, Nordmann JP, Denis P,
Creuzot-Garcher C, Allaire C and Trinquand C: Efficacy of
indomethacin 0.1% and fluorometholone 0.1% on conjunctival
inflammation following chronic application of antiglaucomatous
drugs. Graefes Arch Clin Exp Ophthalmol. 240:929–935.
2002.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Al Habash A, Aljasim LA, Owaidhah O and
Edward DP: A review of the efficacy of mitomycin C in glaucoma
filtration surgery. Clin Ophthalmol. 9:1945–1951. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
S Khouri A, Huang G and Y Huang L:
Intraoperative injection vs sponge-applied mitomycin C during
trabeculectomy: One-year study. J Curr Glaucoma Pract. 11:101–106.
2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Pakravan M, Esfandiari H, Yazdani S,
Douzandeh A, Amouhashemi N, Yaseri M and Pakravan P: Mitomycin
C-augmented trabeculectomy: Subtenon injection versus soaked
sponges: A randomised clinical trial. Br J Ophthalmol.
101:1275–1280. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ehrnrooth P, Lehto I, Puska P and
Laatikainen L: Longterm outcome of trabeculectomy in terms of
intraocular pressure. Acta Ophthalmol Scand. 80:267–271.
2002.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Parc CE, Johnson DH, Oliver JE,
Hattenhauer MG and Hodge DO: The long-term outcome of glaucoma
filtration surgery. Am J Ophthalmol. 132:27–35. 2001.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Bevin TH, Molteno AC and Herbison P: Otago
glaucoma surgery outcome study: Long-term results of 841
trabeculectomies. Clin Exp Ophthalmol. 36:731–737. 2008.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Khaw PT: Advances in glaucoma surgery:
Evolution of antimetabolite adjunctive therapy. J Glaucoma. 10
(Suppl):S81–S84. 2001.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Agbeja AM and Dutton GN: Conjunctival
incisions for trabeculectomy and their relationship to the type of
bleb formation-A preliminary study. Eye (Lond). 1:738–743.
1987.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chang L, Wong T, Ohbayashi M, Bunce C,
Barton K, Ono SJ and Khaw PT: Increased mast cell numbers in the
conjunctiva of glaucoma patients: A possible indicator of
preoperative glaucoma surgery inflammation. Eye (Lond).
23:1859–1865. 2009.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Yu DY, Morgan WH, Sun X, Su EN, Cringle
SJ, Yu PK, House P, Guo W and Yu X: The critical role of the
conjunctiva in glaucoma filtration surgery. Prog Retin and Eye Res.
28:303–328. 2009.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Schumer RA and Odrich SA: A scleral tunnel
incision for trabeculectomy. Am J Ophthal. 120:528–530.
1995.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lai JS and Lam DS: Trabeculectomy using a
sutureless scleral tunnel technique: A preliminary study. J
Glaucoma. 8:188–192. 1999.PubMed/NCBI
|
|
20
|
Eslami Y, Mohammadi M, Khodaparast M,
Rahmanikhah E, Zarei R, Moghimi S and Fakhraie G: Sutureless tunnel
trabeculectomy without peripheral iridectomy: A new modification of
the conventional trabeculectomy. Int Ophthalmol. 32:449–454.
2012.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Jacob S, Figus M, Ashok Kumar D, Agarwal
A, Agarwal A and Areeckal Incy S: Stab incision glaucoma surgery: A
modified guarded filtration procedure for primary open angle
glaucoma. J Ophthalmol. 2016(2837562)2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Zhou M, Wang W, Huang W and Zhang X:
Trabeculectomy with versus without releasable sutures for glaucoma:
A meta-analysis of randomized controlled trials. BMC Ophthalmol.
14(41)2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Wells AP, Crowston JG, Marks J, Kirwan JF,
Smith G, Clarke JC, Shah R, Vieira J, Bunce C, Murdoch I and Khaw
PT: A pilot study of a system for grading of drainage blebs after
glaucoma surgery. J Glaucoma. 13:454–460. 2004.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Broadway DC, Bloom PA, Bunce C,
Thiagarajan M and Khaw PT: Needle revision of failing and failed
trabeculectomy blebs with adjunctive 5-fluorouracil: Survival
analysis. Ophthalmology. 111:665–673. 2004.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kapasi MS and Birt CM: The efficacy of
5-fluorouracil bleb needling performed 1 year or more
posttrabeculectomy: A retrospective study. J Glaucoma. 18:144–148.
2009.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Dalvi R, Orzech N, Kranemann C and Birt
CM: Five-year results of 5-fluorouracil augmented needling revision
of failing blebs. Ophthalmic Surg Lasers Imaging. 43:32–38.
2012.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Nouri-Mahdavi K, Brigatti L and Caprioli
J: Outcomes of trabeculectomy for primary open-angle glaucoma.
Ophthalmology. 102:1760–1769. 1995.PubMed/NCBI View Article : Google Scholar
|
|
28
|
D'Ermo F, Bonomi L and Doro D: A critical
analysis of the long-term results of trabeculectomy. Am J
Ophthalmol. 88:829–835. 1979.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Palmer SS: Mitomycin as adjunct
chemotherapy with trabeculectomy. Ophthalmology. 98:317–321.
1991.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Annen DJ and Sturmer J: Trabeculectomy
with low concentration of mitomycin (0.2 mg/ml for 1 minute)
Independent evaluation of a retrospective non-randomised pilot
study. Klinische Monatsblatter fur Augenheilkunde. 206:300–302.
1995.PubMed/NCBI View Article : Google Scholar
|