Introduction
The primary insufficiency of adrenal cortex was
first described by Thomas Addison, in 1855. This had been a fatal
condition until 1949, when Kendall, Sarett, and Reichstein
introduced the substitution therapy with synthetic glucocorticoids.
The most common cause of primary adrenal insufficiency is
autoimmune adrenalitis (1). Other
causes are represented by adrenoleukodystrophy (2), bilateral hemorrhagic adrenal infarction
(3,4), infectious adrenalitis (5,6), and
adrenal insufficiency induced by administration of synthetic
cortisol (7).
Prevalence of Addison disease in the general
population in Europe is of 93-144 cases per million and it is
estimated that its incidence will reach 4.4-6 new cases per million
per year (8). From a
physiopathological perspective, Addison disease is characterized by
a deficit of glucocorticoid and mineralocorticoid hormones, with an
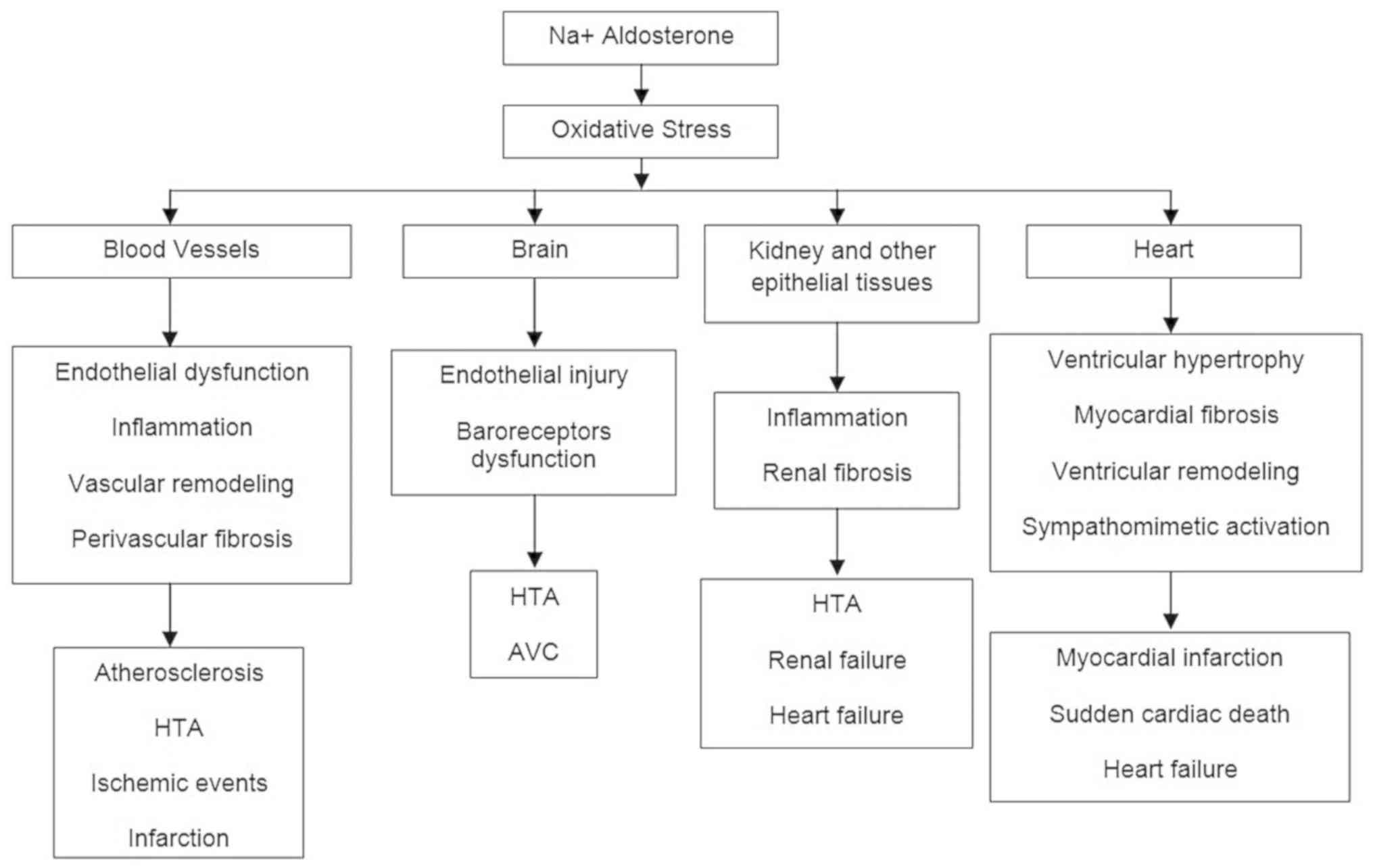
increase in blood plasma ACTH. Mineralocorticoids are known as
hormones of sodium and potassium homeostasis. Aldosterone, the most
active mineralocorticoid, acts mostly upon the distal and
collecting tubules of the kidney, to stimulate sodium and water
reabsorption, altogether with potassium excretion (Fig. 1). The general effect of aldosterone
is the increase of volemia and arterial blood pressure. Therefore,
the deficit of mineralocorticoids leads to: Hyponatremia and
hyperkalemia, severe dehydration, blood plasma hypertonia,
acidosis, decreased circulating blood volume, arterial hypotension,
and even cardiovascular failure. On the other hand, the most
important effects of glucocorticoids include: Hyperglycemia through
the stimulation of gluconeogenesis, increased arterial blood
pressure, anti-inflammatory and immunosuppressive activity.
Overall, the deficit of glucocorticoids causes arterial
hypotension, severe sensitivity to insulin and disorders in the
metabolism of carbohydrates, proteins and lipids.
The association between Addison disease and acute
coronary syndrome is rare. The physiopathological mechanisms that
cause the acute coronary syndrome with ST segment elevation in
Addison disease are partially known. The acute coronary syndrome
occurring in response to severe endothelial injury is a major
stress form, which stimulates the hypothalamus-hypophysis-adrenal
axis, which thereafter modulates the complex neurovascular and
hormonal response. The functional hypoadrenalism is accompanied by
significant morbidity-mortality in the critical patient (9).
Case report
A 71-year-old woman has been brought to the hospital
as an emergency case (by ambulance), for dehydration syndrome and
lipothymic condition. The patient has hereditary/collateral history
in the cardiovascular sphere: Father with stroke and a sister with
myocardial infarction. She had been diagnosed with Addison disease
30 years ago (i.e., at her age of 41). She is under treatment with
prednisone 5 mg/day. Her last endocrinological examination took
place 10 years ago (i.e., at her age of 61). She was
hysterectomized for cervical neoplasm 2 years ago (i.e. at her age
of 69).
The objective examination upon admission shows:
Altered general condition, without fever, normal weight (BMI 22.2
kg/m²), pale dehydrated teguments and mucosa, post-hysterectomy
median scar, arterial blood pressure 60/40 mmHg, heart rate 95/min,
rhythmic cardiac sounds, aortic systolic murmur III/VI with
irradiation on both carotids, lower limbs varices, enlarged abdomen
through adipose panicle, mobile with breath, diffusely painful at
deep palpation in the inferior abdominal level, palpable liver at
the right costal margin, vesical catheter à demeure (normochromic
urine).
Biological explorations upon admission show: Severe
hyponatremia (124 mmol/l) with hypochloremia (92 mmol/l); acidosis
(alkaline reserve 17 mmol/l); nitrogen retention syndrome (urea 93
mg/dl; creatinine 2.34 mg/dl); hyperglycemia (148 mg/dl);
leukocytosis (10,460/mm³) with lymphopenia (15.7%) and monocytosis
(13%); thrombocytosis (616,000/mm³); hypocholesterolemia (total
cholesterol 56 mg/dl; LDL-cholesterol 20 mg/dl, HDL-cholesterol
28.4 mg/dl); hypotriglyceridemia (48 mg/dl); significant glycosuria
at the urinalysis. BNP (natriuretic type B peptide) was normal upon
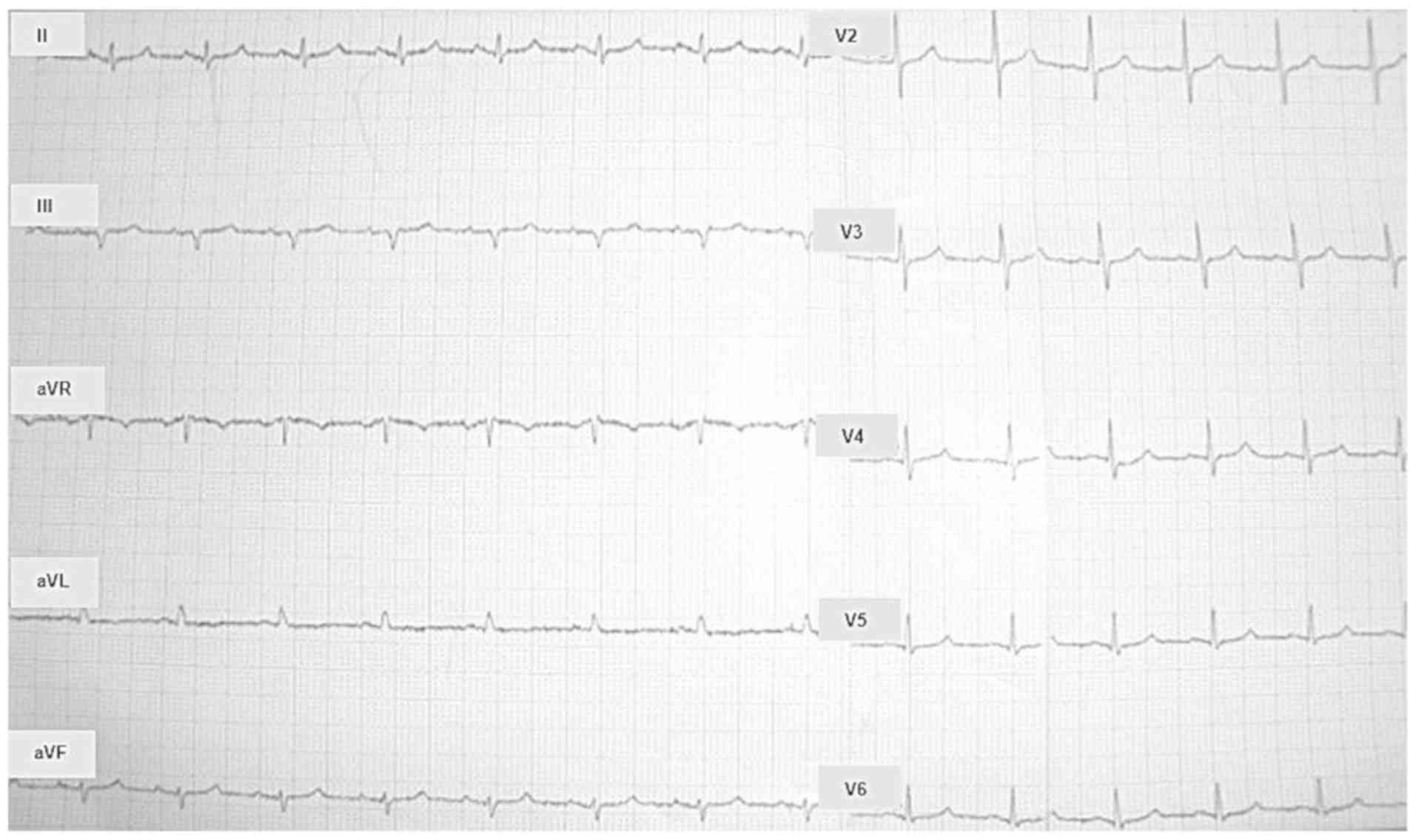
admission. Electrocardiogram was also normal at the time of
admission (Fig. 2).
Along the first 24 h from arrival to the Emergency
Admission Unit, the patient was the subject of the following
events, step by step: i) positive inotropic support and
hydro-electrolytic and acid-base rebalancing; ii) admission to
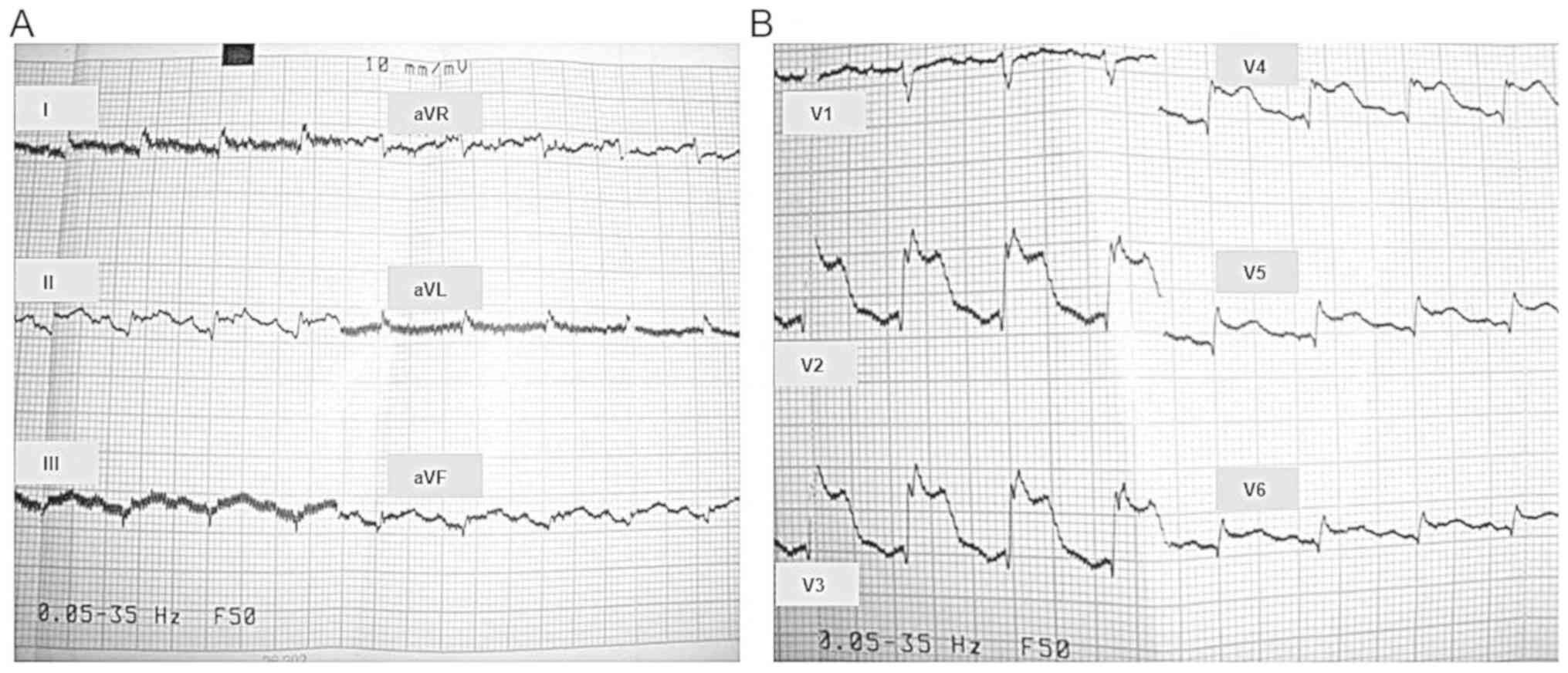
Endocrinology Clinic; iii) anginous pain and electrocardiographic
aspect of extended acute inferior and anterior myocardial
infarction (Fig. 3A and B), thus transfer to the Coronary Intensive
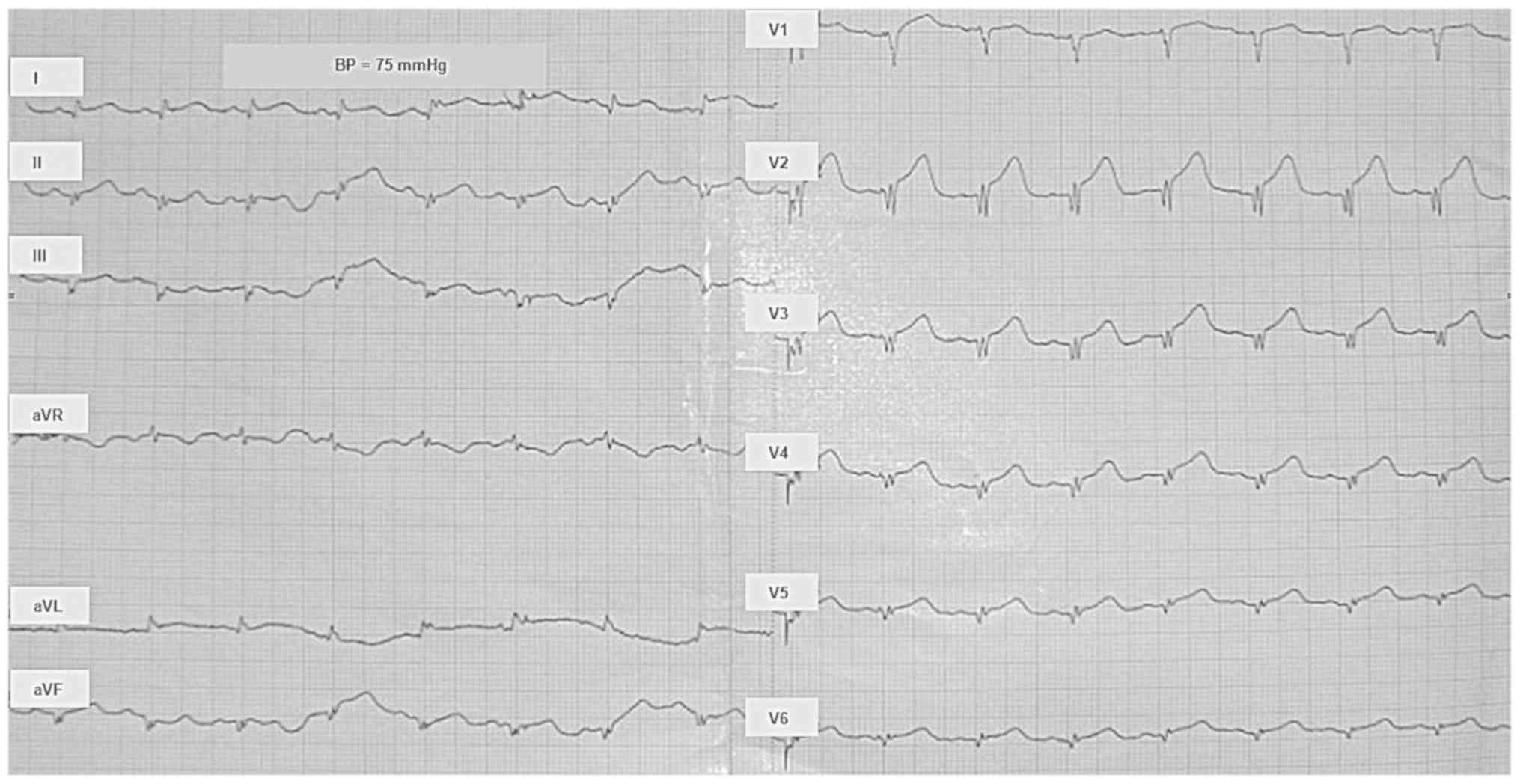
Therapy Unit (Fig. 4), at the moment
of transfer the myocytolysis enzymes being within normal limits and
iv) confirmation of infarction diagnosis and immediate thrombolytic
therapy, which proved to be successful. During monitorization in
the Coronary Intensive Therapy Unit, after for ten days, another
acute Addison episode occurred and the patient was again subjected
to rebalancing, but this time the endocrinologist opinion was asked
for and the decision was taken to increase the prednisone dose to
7.5 mg/day (5 mg each morning and 2.5 mg each afternoon).
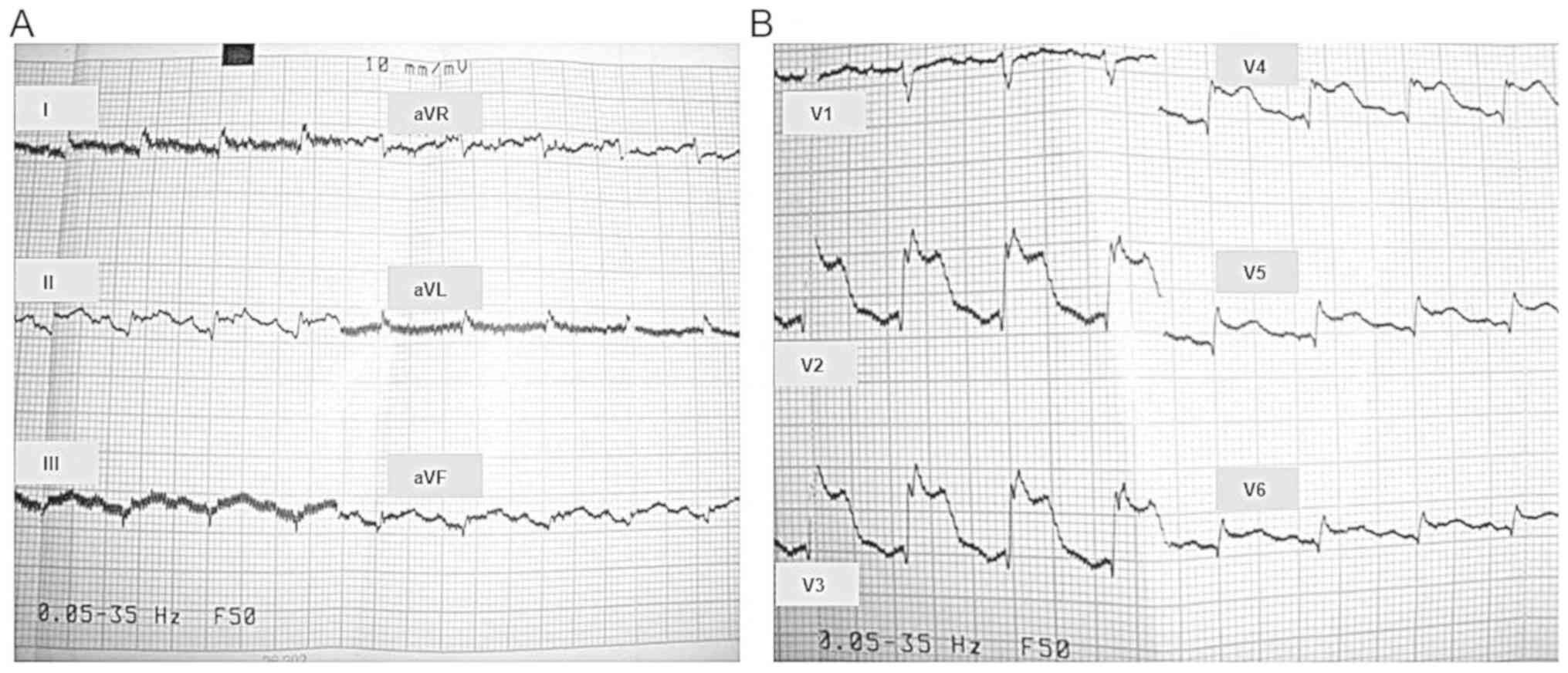 | Figure 3Electrocardiogram (ECG) during angina.
Traces correspond to the standard leads and (A) unipolar leads of
the limbs and (B) to the thoracic (precordial) leads. Analysis:
Heart rate (HR) 116/min; normal intermediary electrical axis of the
heart; qR aspect of the QRS complex and ST segment elevation in
leads I, aVL, V5, and V6; QRS complex appears
as a large monophasic wave in leads V2, V3,
and V4. The usual denominations are used for the
following: ECG waves (Q, R, S, and T; non-capital letters refer to
a small amplitude of the respective wave); standard bipolar ECG
leads (I, II, and III); amplified unipolar ECG leads of the limbs
(aVR, aVL, and aVF); thoracic (precordial) unipolar ECG leads
(V1 to V6). |
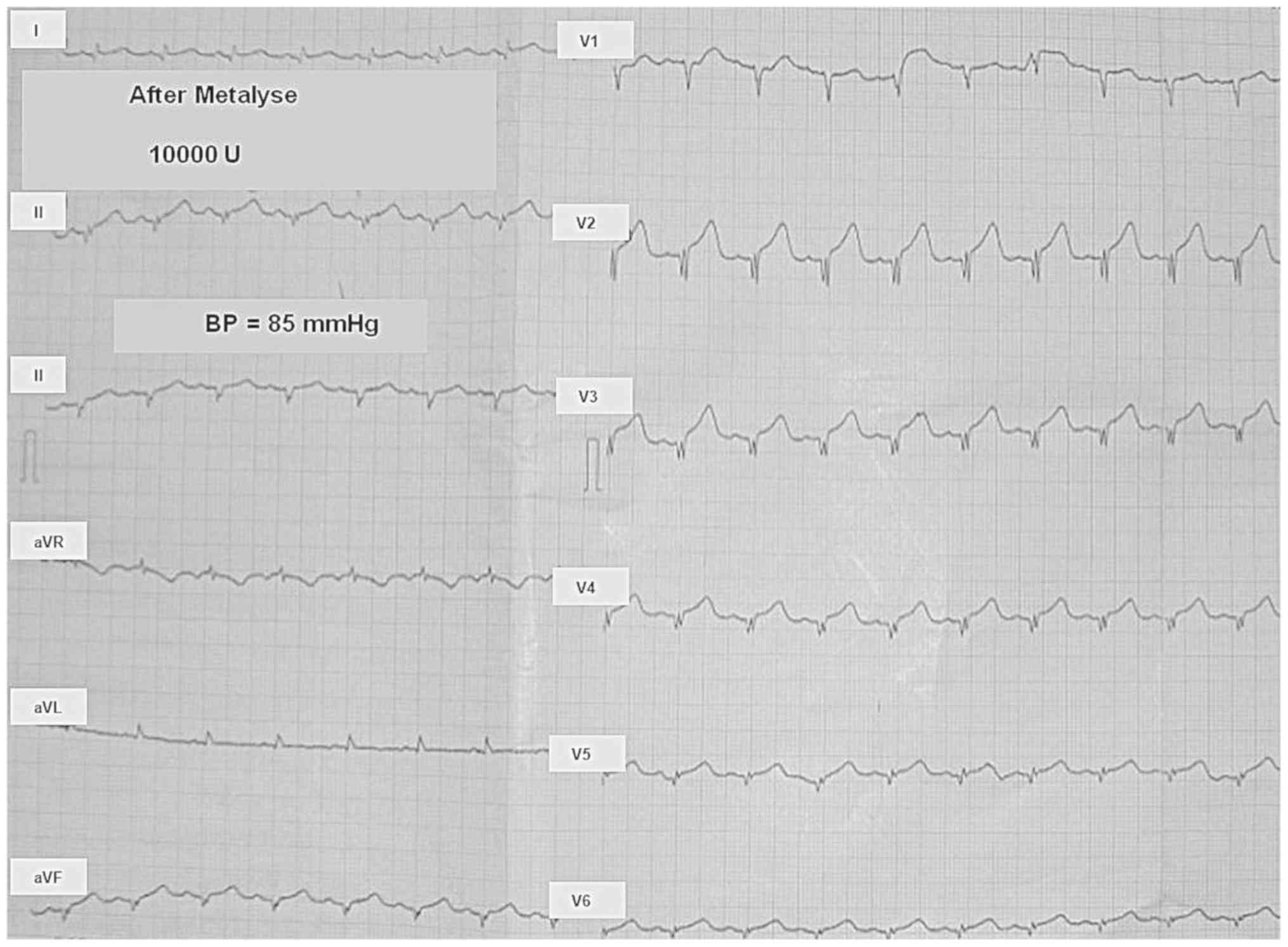
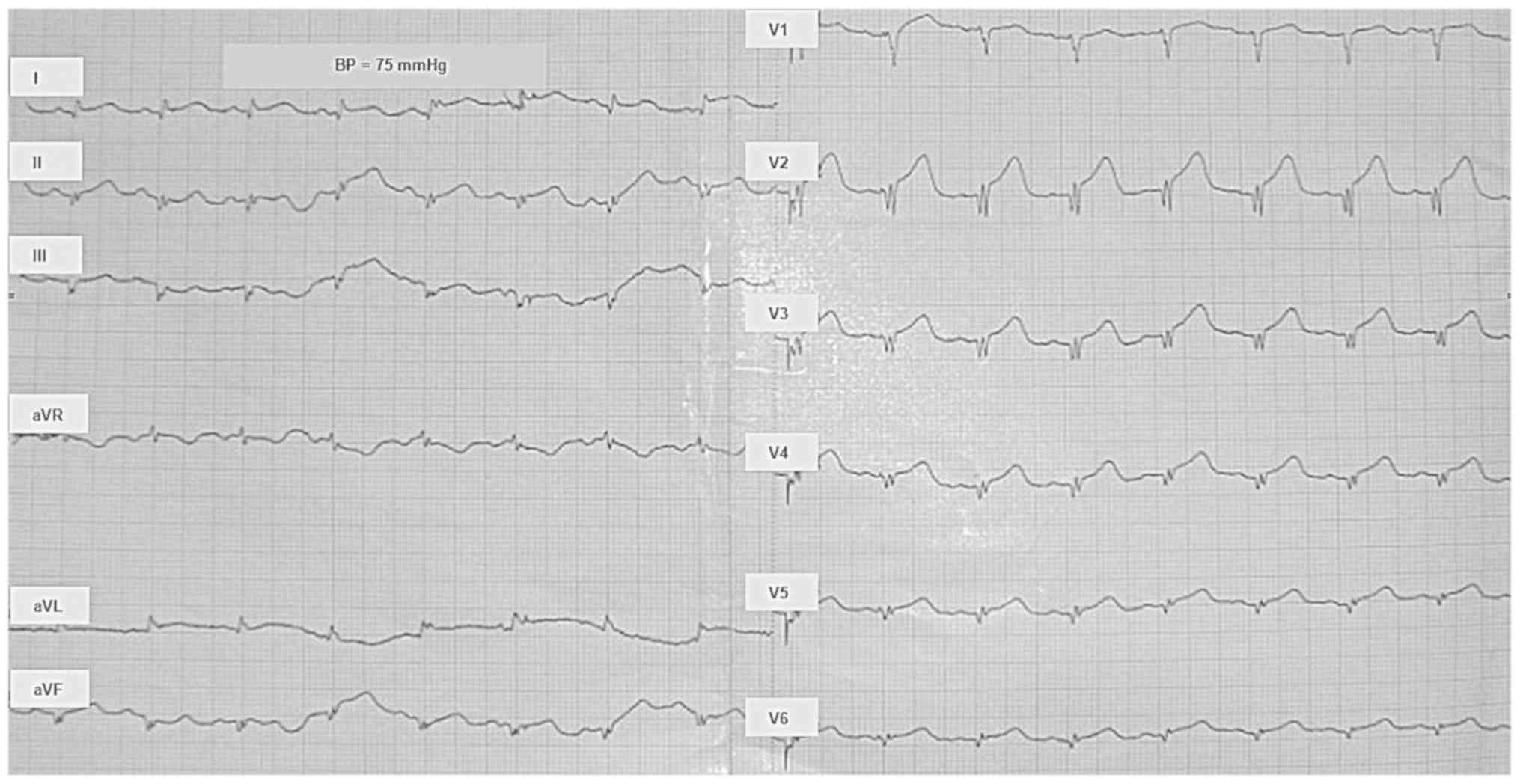 | Figure 4Electrocardiogram in the Cardiologic
Clinic. Heart rate (HR) 99/min; normal intermediary electrical axis
of the heart; arterial blood pressure (BP) 75 mmHg. The QRS complex
has the following aspects: qR in leads I, II, aVL, V5,
and V6; QS in leads III, aVF, and V1; QrS in
leads V1, V2, and V3. ST segment
elevation of ascending type is present in preordial leads
V2 to V5. The usual denominations are used
for the following: ECG waves (Q, R, S, and T; non-capital letters
refer to a small amplitude of the respective wave); standard
bipolar ECG leads (DI, DII, and DIII); amplified unipolar ECG leads
of the limbs (aVR, aVL, and aVF); thoracic (precordial) unipolar
ECG leads (V1 to V6). |
The positive diagnosis of acute myocardial
infarction was based on the clinical and electrocardiographic
criteria. Thrombolysis was applied, using Metalyse 10,000 U, with
clear subsequent favorable evolution (Figs. 5,6),
without an increase of the myocardial cytolysis enzymes. In fact,
myocardial enzymes, including troponin, were normal both before and
after thrombolysis. Echocardiography performed during chest pain
showed hypokinesis of the left ventricular apex and hypokinesis of
the lower wall, with an ejection fraction in normal limits (50%).
Emergency coronary angiography could not be performed, because the
service was unavailable at that time.
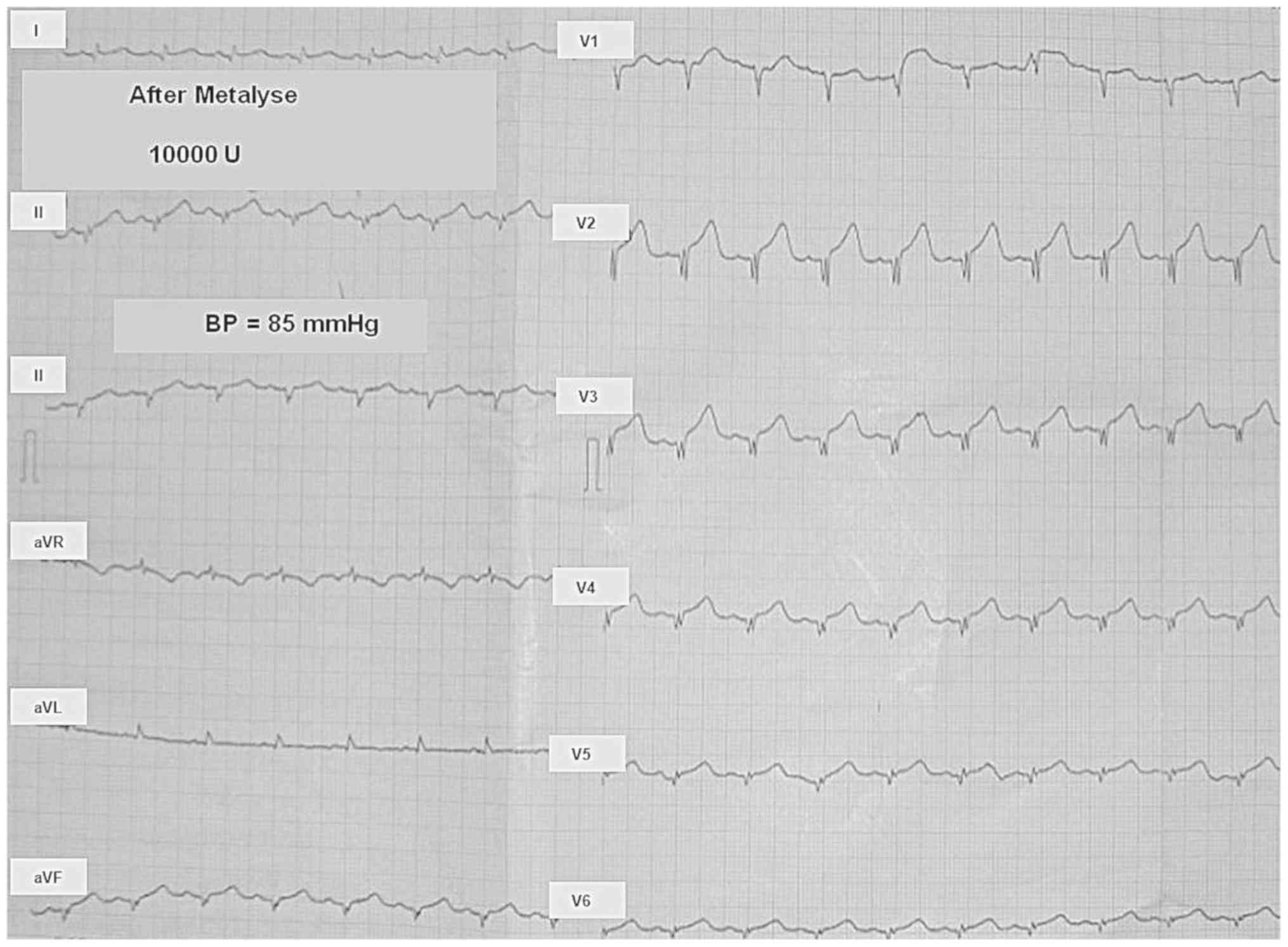
 | Figure 5Electrocardiogram (ECG) immediately
after Metalyse 10,000 u. Heart rate (HR) 90/min; normal
intermediary electrical axis of the heart; arterial blood pressure
(BP) 85 mmHg. The QRS complex has the following aspects: qR in
leads I, II, aVL, V5, and V6; QS in leads
III, aVF, and V1; QrS in leads V2,
V3, and V4. ST segment elevation of ascending
type is present in precordial leads V2 to V5.
The usual denominations are used for the following: ECG waves (Q,
R, S, and T, where non-capital letters refer to a small amplitude
of the respective wave); standard bipolar ECG leads (I, II, and
III); amplified unipolar ECG leads of the limbs (aVR, aVL, and
aVF); thoracic (precordial) unipolar ECG leads (V1 to
V6). |
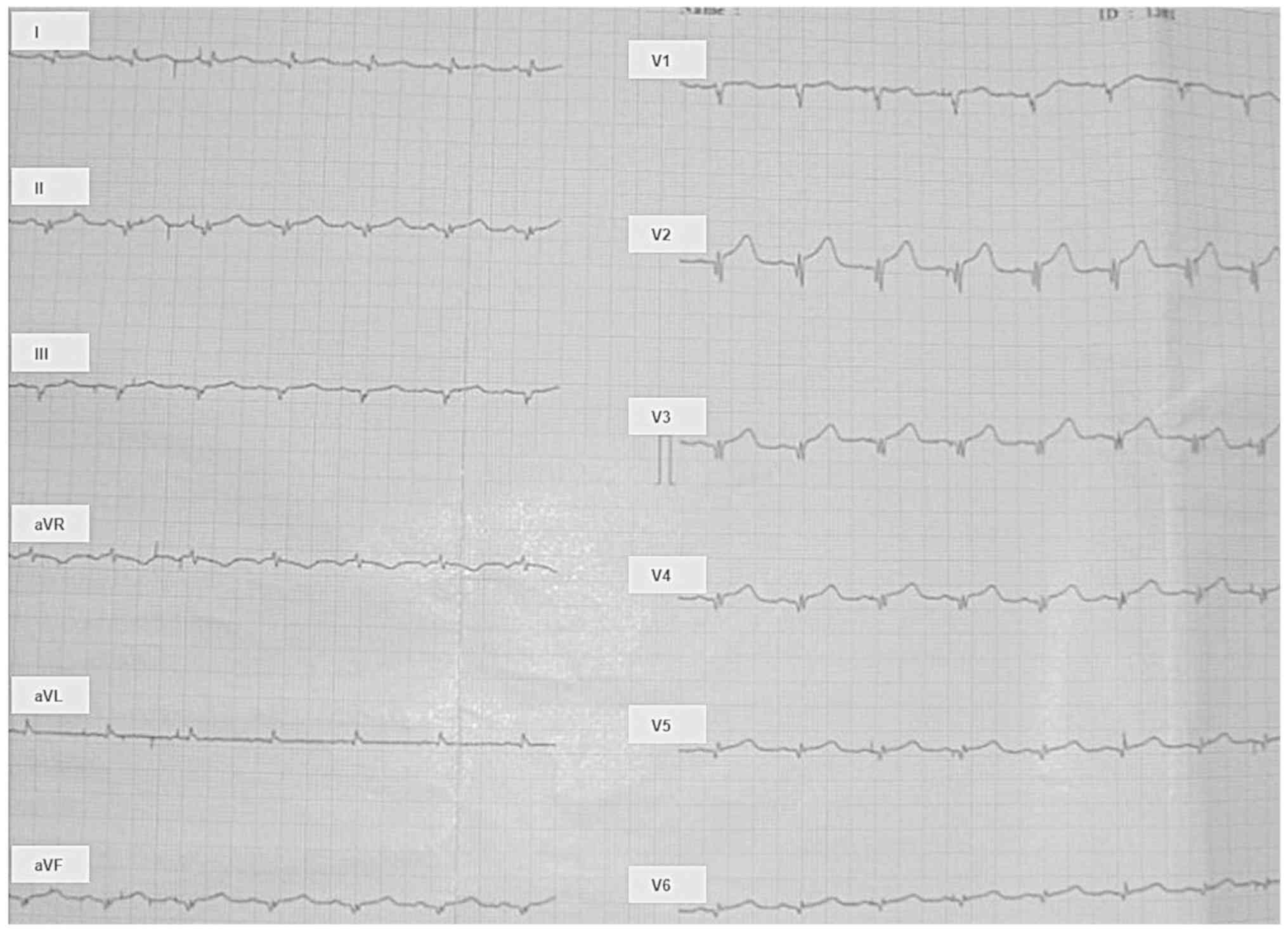
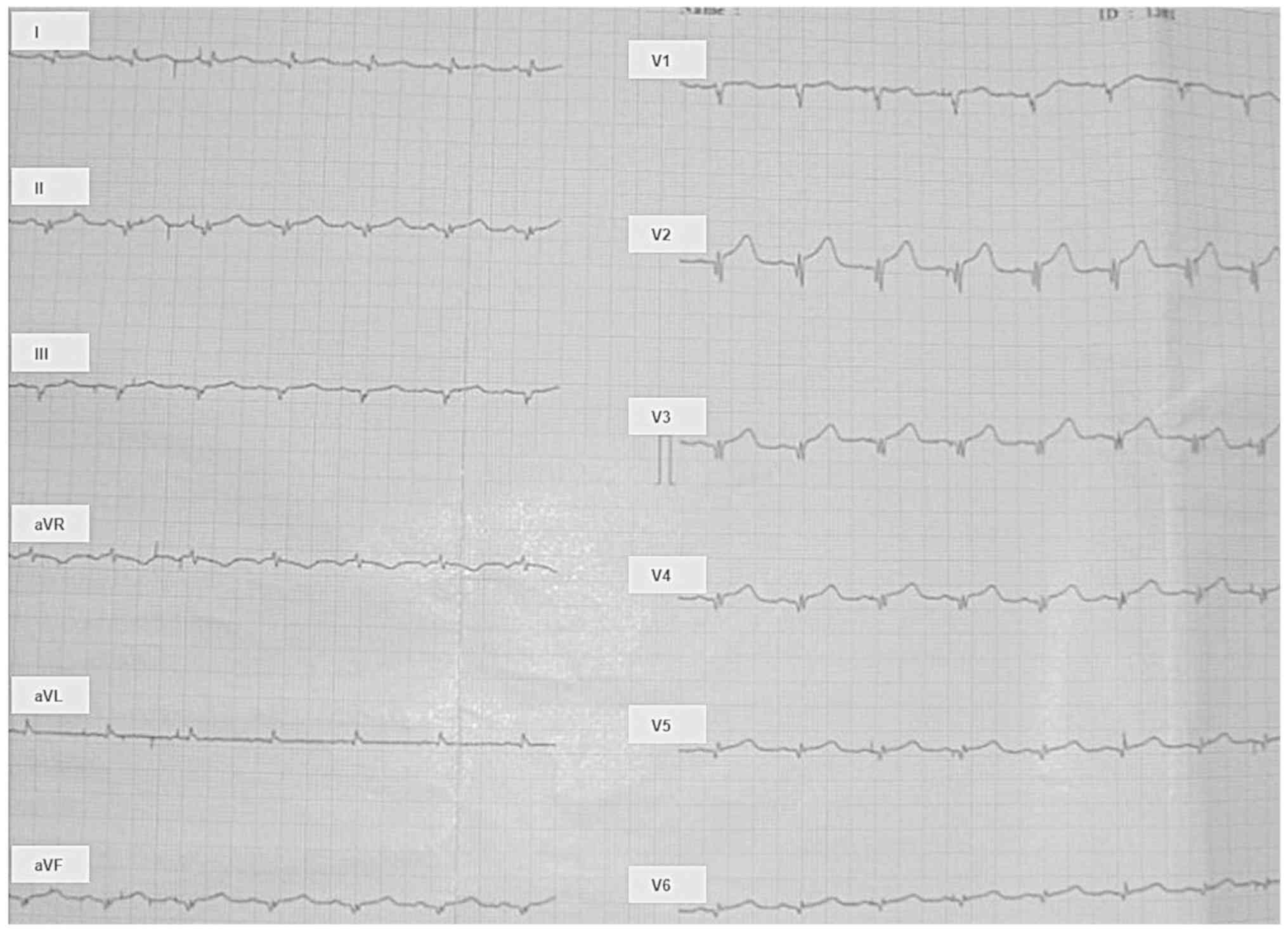 | Figure 6Electrocardiogram one hour after
Metalyse 10,000 u. Heart rate (HR) 90/min; normal intermediary
electrical axis of the heart; arterial blood pressure (BP) 85 mmHg.
The QRS complex has the following aspects: qR in leads I and aVL,
V5, and V6; Qr in leads II and aVF, QS in
lead V1; qrS in leads V2, V3, and
V4. ST segment elevation of ascending type is present in
precordial leads V2 to V5. The usual
denominations are used for the following: ECG waves (Q, R, S, and
T, where non-capital letters refer to a small amplitude of the
respective wave); standard bipolar ECG leads (I, II, and III);
amplified unipolar ECG leads of the limbs (aVR, aVL, and aVF);
thoracic (precordial) unipolar ECG leads (V1 to
V6). |
The clinical examination did not reveal cushingoid
manifestations (as possible adverse effect of an uncontrolled
glucocorticoid replacement therapy), while hormone measurements
showed the level of cortisol was 10.6 µg/dl and that of ACTH was
398 pg/ml. The abdominal CT performed shows, on the topography of
the adrenal glands, two inhomogeneous iodophile formations, with
calcareous structure.
So, prednisone was increased, from the previous dose
of 5 mg/day to the current dose of 7.5 mg/day, with the indication
to increase the dose up to 10-15 mg/day in case this was required
by intercurrent stress events. The lower prednisone dose, of 5
mg/day, proved to be insufficient in situations of superimposed
acute events, allowing manifest Addison crisis to occur. With this
higher prednisone dose, the patient has been stable thereafter,
without any acute cardiovascular or endocrinological
manifestations.
Discussion
Cardiovascular diseases constitute an important
public health issue in industrialized countries, in terms of both
morbidity and mortality. The most important mortality cause in the
entire world is atherosclerosis. The most feared complication of
chronic inflammation of the vascular wall, with the highest
mortality rate, is the acute coronary syndrome with ST segment
elevation (10). Atherosclerosis
produces rigidity, narrowing and obstruction of coronary arteries.
Inflammation represents the key element in the initiation,
progression and destabilization of the atheromatous plaque
(10). Endothelial dysfunction is
currently considered the trigger factor in the pathogenesis of
atherosclerotic plaque. Pro-inflammatory cytokines, such as
TNF-alpha (tumor necrosis factor) (11) and IL-1 beta (interleukin 1) (12) act on endothelial cells to initiate a
cascade of events that ultimately affect the endothelium
anti-adhesive and anticoagulant properties and also its
permeability. Alteration of endothelial permeability allows LDL
accumulation in the heart and favors the adhesion of circulating
monocytes/macrophages (13) and the
formation of thrombi through the increase of the pro-aggregant and
pro-coagulant functions. Unfortunately, no cytokines were measured
in the particular clinical case under discussion here.
Cortisol and ACTH are involved in atherogenesis, by
modulation of the endothelial functions, by recruitment of
circulating monocytes and their differentiation into macrophages,
and by production of pro- and anti-inflammatory interleukins.
Furthermore, these hormones are involved in development of acute
coronary syndrome, by modulating platelet aggregation and
thrombogenesis (14). Coronary
atherosclerosis has a multi-factorial etiology, which includes
non-modifiable factors (age, male sex, family predisposition) and
modifiable factors (dyslipidemia, arterial hypertension, smoking,
diabetes mellitus, obesity, sedentary lifestyle). Coronary
atherosclerosis is a silent process which evolves in stages of
years or tens of years.
In the case of our patient, coronary atherosclerosis
is the main cause for the acute myocardial infarction that she
developed during hospitalization. As reasons for these
circumstances we have the patient's age, the hereditary
cardiovascular history, the presence of systolic murmur at the
level of carotid arteries, as well as the fact that she is at
menopause. It is known that the clinical manifestations of
atherosclerosis occur after the fifth decade of life in women, when
the anti-aterosclerotic protective effect of oestrogen gradually
decreases at the onset of menopause.
Addison disease, also called primary corticoadrenal
insufficiency, is a hypofunction of the adrenal gland. From a
physiopathological perspective, the Addison disease appears as an
insufficient secretion of glucocorticoid and mineralocorticoid
hormones. The deficit of glucocorticoid hormones leads to arterial
hypotension, dysfunctions in the metabolism of carbohydrates,
lipids and proteins and the decrease of insulin sensitivity. The
deficit of mineralocorticoid hormones leads to an increase of the
sodium excretion and a decrease of the potassium excretion in
urine, which leads to hyponatremia and hyperkalemia. In this
context severe dehydration appears, accompanied by decreased
circulating volume and arterial hypotension.
Clearly applicable to the case presented here, a
more detailed analysis of the involved pathophysiological
mechanisms reveals the following. Hyponatremia, severe dehydration
and hypovolemia are accompanied by decreased blood pressure and
consequently, decreased myocardial perfusion occurs. On a
pre-existing atherosclerotic background, prolonged low blood
pressure may contribute to myocardial infarction, with an oxygen
supply-demand disproportion appearing in the myocardium. In Addison
disease, low blood pressure occurs, on one hand by decreased
cortisol synthesis, and on the other by severe hyponatremia, which
leads to decreased water reabsorption and extreme dehydration, with
decreased circulating blood volume. These factors may participate
in destabilizing the atheroma plaque and in the onset of acute
coronary syndrome with ST elevation. Such a mechanism is advocated
for by the following aspects present at the time of
hospitalization: Dehydrated teguments and mucous membranes at the
clinical examination; arterial blood pressure 60/40 mmHg, severe
hyponatremia (124 mmol/l).
The depletion of endogenous glucocorticoids is
correlated with the development of the myocardial dysfunction. In
murine models, adrenalectomy was associated with an impairment of
the myocardial contractility through the depletion of the
microsomal phosphorylase activity and a significant reduction of
calcium absorption in the sarcoplasmic reticulum. These lead to a
glycogenolysis dysfunction and the depression of the myocardial
contractility. Moreover, the glucocorticoids deficit reduces the
expression of adrenergic receptors and adrenalin synthesis and
affects the cardiovascular reactivity to catecholamines. These
mechanisms could explain the severe myocardial dysfunction
associated to adrenal insufficiency (15). However, we could not identify animal
studies explaining mechanisms associated with the occurrence of
acute coronary syndrome in adrenal insufficiency.
Treatment of Addison disease includes
glucocorticoids. Glucocorticoids stimulate atherogenesis and
vascular remodeling (16), via
glucocorticoid and mineralocorticoid receptors, a phenomenon which
involves the local enzyme 11b hydroxysteroid dehydrogenase
(17). In case of prolonged cortisol
treatment, the vasoconstriction that sets in is a consequence of
the decrease of nitric oxide production at the vascular level
(18). At the same time, the
administration of glucocorticoids produces an imbalance between the
vasoconstrictor and vasodilating factors, through decreased
synthesis of vasodilating prostacyclin and the increase of the
vasoconstricting thromboxane (19).
Our patient was diagnosed with Addison disease 41 years ago, thus
she received substitution treatment with prednisone starting at
that time. Prolonged administration of glucocorticoids increases
the risk of cardio-vascular events (20), but in patients with Addison disease
the adequate corticosteroid treatment is required as substitute and
the risk of cardio-vascular events is minimal. Moreover, this
patient had hypoadrenalism and only took a very small dose of
glucocorticoid replacement therapy, so the mechanisms described in
this paragraph actually do not apply. On the other side, only an
overdose of glucocorticoids promotes pro-atherosclerotic
dyslipidemia, as trigger for acute coronary syndrome, which is also
not the case here.
Maybe above all, this case presentation shows an
interesting acute issue, as follows. In the atherosclerotic context
and with a relatively sufficient chronic corticoid substitution, a
manifest acute Addison episode may lead to myocardial infarction.
In our case the infarction was mainly of thrombotic cause, as shown
by the successful thrombolysis. The hypotensive crisis lead to
emergency hospitalization and the patient suffered the infarction
the same day after admission and rebalancing. Even more, she had
another Addison crisis ten days later, which imposed an increase in
the corticoid substitution dose. The pathogenic complex behind this
sequence of events involves all the aspects discussed above,
regarding the atheroma in such conditions. Maybe with a special
relevance of all the abrupt hemodynamic changes, reflected in major
and sharp changes in shear stress, under circumstances of blunted
flow-mediated dilation due to endothelial dysfunction.
To conclude, in case of a patient with Addison
disease, the pre-existing coronary atherosclerosis is the main
cause that leads to the development of acute coronary syndrome with
elevation of ST segment. The severe hyponatremia, dehydration, and
hypovolemia, all found in this adrenal cortical insufficiency, can
be considered trigger factors, but they could not cause acute
coronary syndrome without the pathological basis of
atherosclerosis. Such factors, on a pre-existing atherosclerotic
background, increase the risk of major cardiovascular events, such
as acute myocardial infarction with ST-segment elevation, as in our
case report. This multifactorial pathogenic scene needs to include
thrombosis, coronary spasm and low blood pressure as causes of
myocardial infarction. These three mechanisms are more or less
related to the context of Addison disease and the required
corticotherapy, as discussed above. Last but not least, the
conclusion of this article is that corticoid substitution therapy,
which may seem sufficient, can become insufficient along the
evolution of cardiovascular disease (mainly with age), thus leading
to the manifest Addison crisis and even to major ischemic events,
as in the case discussed here.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MAM, CS, DNS and ILS contributed to conception and
design of the current study. MAM, CS, RAS, ND and LLH acquired the
data. All authors analyzed and interpreted the data. MAM and CS
drafted the manuscript and RAS, ND, LLH, DNS and ILS revised it
critically for important intellectual content. All authors gave
final approval of the this version of the manuscript to be
published.
Ethics approval and consent to
participate
Informed consent was obtained from the patient.
Patient consent for publication
Informed consent has been obtained from the patient
regarding the publication of the case details and any associated
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Erichsen MM, Løvås K, Skinningsrud B,
Wolff AB, Undlien DE, Svartberg J, Fougner KJ, Berg TJ, Bollerslev
J, Mella B, et al: Clinical, immunological, and genetic features of
autoimmune primary adrenal insufficiency: Observation from a
Norwegian registry. J Clin Endocrinol Metab. 94:4882–4890.
2009.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kemp S, Berger J and Aubourg P: X-linked
adrenoleukodystrophy: Clinical, metabolic, genetic and
pathophysiological aspects. Biochim Biophys Acta. 1822:1465–1474.
2012.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rao RH, Vagnucci AH and Amico JA:
Bilateral massive adrenal hemorrhage: early recognition and
treatment. Ann Intern Med. 110:227–235. 1989.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rao RH: Bilateral massive adrenal
hemorrhage. Med Clin North Am. 79:107–129. 1995.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Bhatia E, Jain SK, Gupta RK and Pandey R:
Tuberculous addison's disease: Lack of normalization of
adrenocortical function after anti-tuberculous chemotherapy. Clin
Endocrinol (Oxf). 48:355–359. 1998.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Walker BF, Gunthel CJ, Bryan JA, Watts NB
and Clark RV: Disseminated cryptococcos is in an apparently normal
host presenting as primary adrenal insufficiency: Diagnosis by fine
needle aspiration. Am J Med. 86:715–717. 1989.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Elias AN and Gwinup G: Effects of some
clinically encountered drugs on steroid synthesis and degradation.
Metabolism. 29:582–595. 1980.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Nicolaides NC, Chrousos, Charmandari E.
In: De Groot LJ, Chrousos G, Dungan K, Grossman A, Hershman JM,
Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer
F, Vinik A, editors. Adrenal Insuffiency Endotext [Internet]. South
Dartmouth (MA): MD http://Text.comsimpleText.com, Inc.; 2000-2013.
|
|
9
|
Norasyikin AW, Norlela S, Rozita M,
Masliza M, Shamsul AS and Nor Azmi K: Adrenal insufficiency in
acute coronary syndrome. Singapore Med J. 50:962–966.
2009.PubMed/NCBI
|
|
10
|
Sger HB and Nahrendorf M: Inflammation: A
trigger for acute coronary syndrome. Q J Nucl Med Mol Imaging.
60:185–193. 2016.PubMed/NCBI
|
|
11
|
Tabas I and Bornfeldt KE: Macrophage
phenotype and function in different stages of atherosclerosis. Circ
Res. 118:653–667. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Coll RC, Robertson AA, Chae JJ, Higgins
SC, Munoz-Planillo R, Inserra MC, Vetter I, Dungan LS, Monks BG,
Stutz A, et al: A small-molecule inhibitor of the NLRP3
inflammasome for the treatment of inflammatory diseases. Nat Med.
21:248–255. 2015.PubMed/NCBI View
Article : Google Scholar
|
|
13
|
Varol C, Mildner A and Jung S:
Macrophages: Development and tissue specialization. Annu Rev
Immunol. 33:643–675. 2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Fantidis P: The role of the stress-related
anti-inflammatory hormones ACTH and cortisol in atherosclerosis.
Curr Vasc Pharmacol. 8:517–525. 2010.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Shimizu M, Monguchi T, Takano T and Miwa
Y: Isolated ACTH deficiency presenting with severe myocardial
dysfunction. J Cardiol Cases. 4:e26–e30. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Shokr M, Rashed A, Lata K and Kondur A:
Dexamethasone associated ST elevation myocardial infarction four
days after an unremarkable coronary angiogram-another reason for
cautious use of steroids: A case report and review of the
literature. Case Rep Cardiol. 2016(4970858)2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Walker BR: Glucocorticoids and
cardiovascular disease. Eur J Endocrinol. 157:545–559.
2007.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Rogers KM, Bonar CA, Estrella JL and Yang
S: Inhibitory effect of glucocorticoid on coronary artery
endothelial function. Am J Physiol Heart Circ Physiol.
283:H1922–H1928. 2002.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Jun SS, Chen Z, Pace MC and Shaul PW:
Glucocorticoids downregulate cyclooxygenase-1 gene expression and
prostacyclin synthesis in fetal pulmonary artery endothelium. Circ
Res. 84:193–200. 1999.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Yildirim U, Gulel O, Soylu K, Yuksel S and
Sahin M: Steroid-induced recurrent myocardial ischemia. Rev Port
Cardiol. 33:473.e1–4. 2014.PubMed/NCBI View Article : Google Scholar
|