Introduction
Esophageal variceal bleeding (EVB) is a serious
complication of liver cirrhosis that affects the life of patients
and has a high mortality rate (1).
Endoscopic variceal ligation (EVL) and endoscopic injection
sclerotherapy (EIS) are effective methods for preventing and
treating EVB (2,3). These two methods have become the
first-line treatment for EVB (4).
However, the incidence of post-operative rebleeding is a major
concern. Previous studies have indicated that risk factors for
rebleeding following endoscopic treatment include the following:
Varicose vein severity, Child-Pugh grade C, ascites volume
(medium-mass), portal vein thrombosis and previous history of
diabetes (5). It is important to
prevent rebleeding following endoscopic treatment and improve the
prognosis of patients. The present study demonstrated that in
addition to liver function-associated factors, diabetes is
associated with an increased prevalence of post-operative bleeding.
The control of repeated bleeding in these patients remains a
clinical challenge. Therefore, further studies are required to
explore the factors that are associated with post-operative
rebleeding in order to evaluate the effects of diabetes on this
complication that is encountered following endoscopic treatment.
Such investigations may lead to developments that may improve the
prognosis of patients with cirrhosis and diabetes. In the present
study, a retrospective analysis of risk factors for post-operative
rebleeding in patients with cirrhosis, EVB and diabetes was
performed.
Materials and methods
Patients
The data were obtained from patients who underwent
EVL or EIS for the prevention or treatment of EVB at the Department
of Gastroenterology, the First Affiliated Hospital of Anhui Medical
University (Hefei, China). The patients were enrolled between June
2015 and March 2018. The treatment provided to the patients did not
include EVL and EIS simultaneously. The inclusion criteria were as
follows: i) Patients aged 18-75 years; ii) patients diagnosed with
cirrhosis and esophageal varices without gastric varices; iii)
history of variceal bleeding and endoscopic sclerotherapy or
ligation. The exclusion criteria were as follows: i) Patients aged
<18 or >75 years; ii) gastrointestinal bleeding at other
sites or due to other reasons; iii) blood system diseases; iv)
other serious organ complications and/or malignant tumors; v)
history of interventional or surgical treatment. A total of 207
patients were enrolled, including 140 males and 67 females. The
average age was 53.31±9.76 years (range, 25-74 years). A total of
137 patients were diabetic and 70 patients were non-diabetic.
According to the diagnostic criteria for hepatogenic diabetes
mellitus (6), the patients had no
family history of diabetes. Diabetes was diagnosed following liver
cirrhosis or at the same time as liver cirrhosis. A total of 2
patients with an unclear medical history were excluded and 33 of
the remaining 68 patients exhibited hepatogenic diabetes. The
causes of cirrhosis were the following: Post-hepatitis B (n=111),
post-hepatitis C (n=6), alcoholic cirrhosis (n=23), cholestatic
cirrhosis (n=10), cirrhosis following autoimmune hepatitis (n=8),
schistosomiasis cirrhosis (n=6), cryptogenic cirrhosis (n=20),
Budd-Chiari syndrome (n=2), non-alcoholic steatohepatitis-cirrhosis
(n=1) and mixed cirrhosis (n=20).
The patients were divided into the EVL and the EIS
groups and each group was subdivided into diabetic and non-diabetic
subgroups. The EVL group comprised 115 patients, including 36 in
the diabetic group and 79 in the non-diabetic group. A total of 92
patients were present in the EIS group, including 34 in the
diabetic group and 58 in the non-diabetic group. All patients
provided written informed consent prior to surgery. The present
study was approved by the Ethics Committee of the First Affiliated
Hospital of Anhui Medical University (Hefei, China) and was
registered as a clinical trial.
Materials
An Olympus GIF-XQ260 electronic gastroscope
(Olympus) and an adjustable disposable needle (23G; Cook Co.) were
used; the sclerosant (lauromacrogol) was obtained from Shanxi
Tianyu Co., and the multiband ligation device (6-ring ligation
device; Cook Co.) was used.
Treatment
The patients were routinely administered
pre-operative treatment to reduce portal pressure and correct
anemia. A comprehensive assessment of the patients prior to surgery
was performed to ensure that their vital signs were stable. The
patients underwent routine gastroscopy prior to surgery to
determine the position, shape, number and size of the varicose
veins. The medical practitioner decided on the number of rings used
for EVL or the amount of the sclerosant required, and the
gastroscope was subsequently removed. The endoscopic treatment plan
for each patient was discussed by three doctors. Following
confirmation, the senior endoscopic expert completed the
procedure.
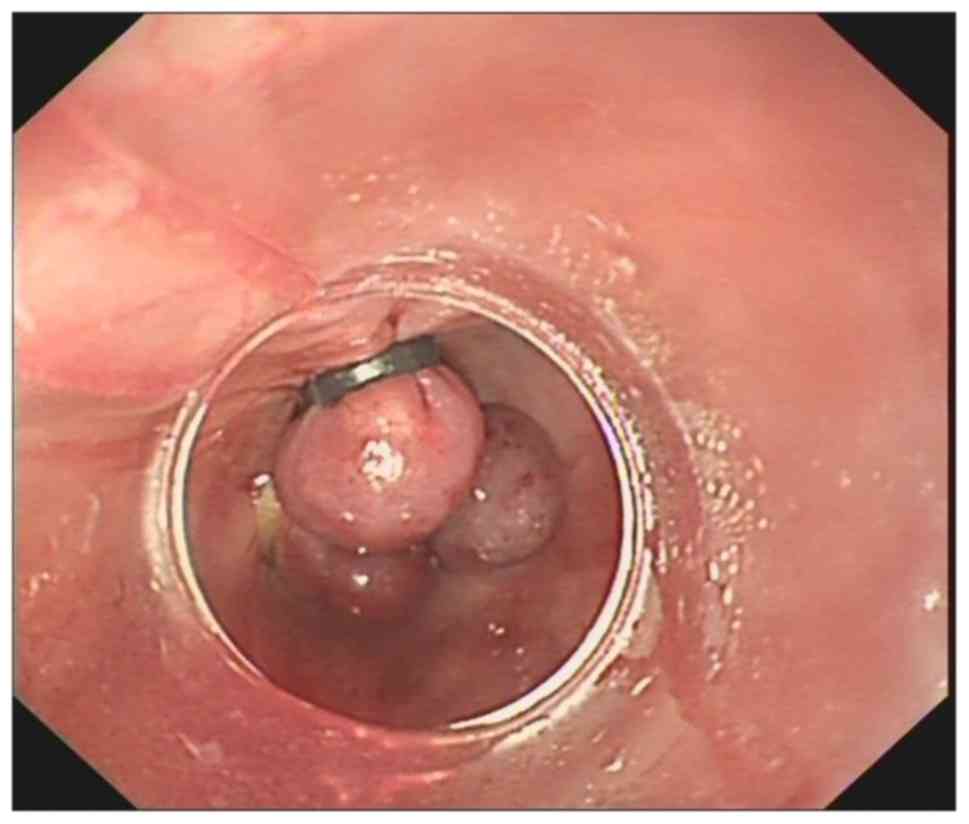
In the EVL group, ligation was performed from above
or below the dentate line, indicating the region where the
esophageal varicose vein was formed. The ligation point was
selected and the endoscope end was placed close to the varicose
vein. Negative pressure was used until the field of view was
completely red. The second ring was placed immediately adjacent to
the previous ring and ligation was performed from the top using the
same method (Fig. 1).
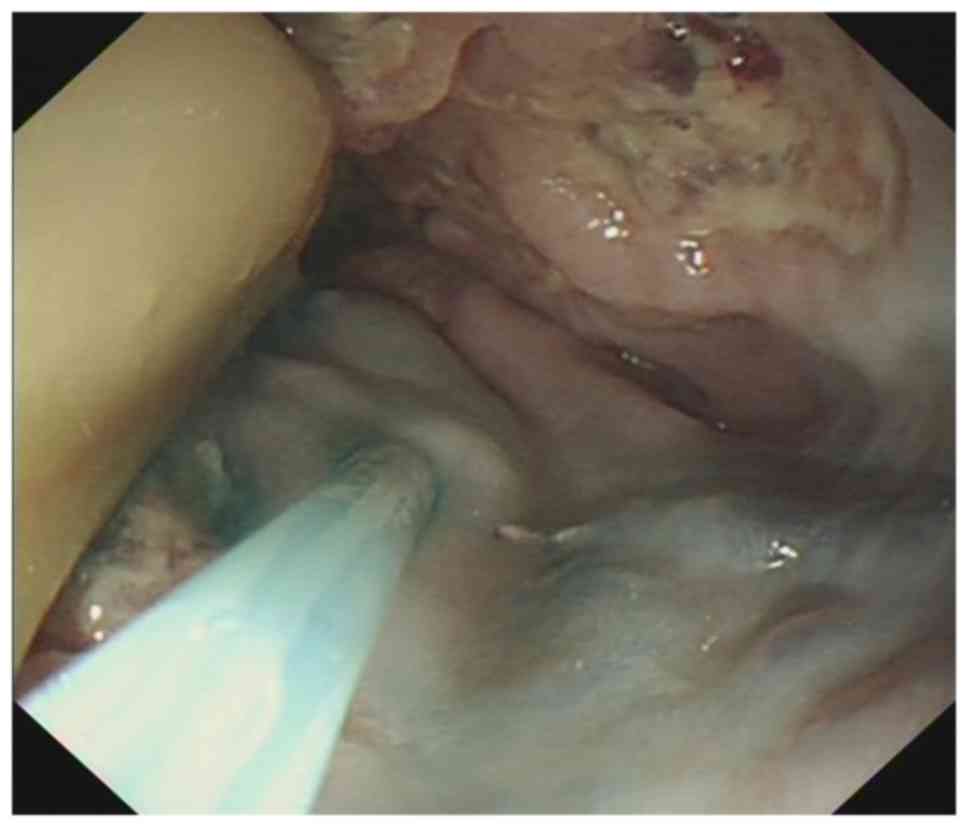
In the EIS group, a range of 2-7 points was used per
injection according to the severity of the varicose veins. The
total amount did not exceed 40 ml, with 0.5-10 ml per point
(lauromacrogol 10 ml + meilan 0.1 ml, until the filling of all
varicose veins was satisfactory). The patients were fasted for 24 h
following surgery and rehydrated. The secretion of gastric acid was
inhibited, the portal pressure was reduced and prophylactic
anti-infective treatment was administered. At 24-48 h following
surgery, the liquid diet was gradually changed to a semi-liquid
diet and subsequently to a soft food diet. The patients' daily diet
was mainly composed of soft food. Strenuous exercise was avoided. A
representative image of EIS is presented in Fig. 2.
Follow-up and analysis
At 1, 3 and 6 months following surgery, the patients
were followed up by gastroscopy to detect bleeding and determine
whether the varicose veins had disappeared. If the varicose veins
had not completely disappeared, consolidation treatment was
performed. The post-operative rebleeding rates were compared
between the EVL and EIS subgroups of the total patient group and
the total diabetic group. The rebleeding rate in the diabetic and
non-diabetic patients of the EVL and EIS groups was analyzed at 1,
3 and 6 months following surgery. The influence of the parameters
of age and liver function grade in the diabetic and non-diabetic
patients in the EIS group was controlled by binary logistic
regression. The post-operative rebleeding rate was compared between
the patients with hepatogenic and non-hepatogenic diabetes from the
total diabetic group. The total diabetic group was classified into
the Child-Pugh A and Child-Pugh B+C groups according to the liver
function grade. The rebleeding rate in the patients with diabetes
in the Child-Pugh A and Child-Pugh B/C groups was analyzed at 1, 3
and 6 months following surgery to observe whether liver function
grade had an influence on rebleeding in patients with cirrhosis and
diabetes.
Statistical analysis
Statistical analysis was performed using the SPSS
19.0 software (IBM Corp.). The measurement data that followed a
normal distribution were expressed as the mean ± standard deviation
and comparisons between the two groups were performed using the
independent-samples t-test. The enumeration data were expressed by
the number of cases and the rebleeding rate. The comparisons
between the two groups were performed using the χ2 test.
The influence of the confounding factors was controlled by using
binary logistic regression. Kaplan-Meier curve analysis and the
log-rank test were used to compare the rebleeding rates at
different durations between the two groups. The level of
significance was set as α=0.05. P<0.05 was considered to
indicate a statistically significant difference.
Results
Baseline data analysis
The baseline data of the patients in the EVL and the
EIS groups were collected and the diabetic and non-diabetic
subgroups of the EVL group did not exhibit any significant
differences. In the EIS group, the diabetic patients were older
than the non-diabetic patients and the number of patients with
liver function grades B and C was higher. The differences noted
were significant. No significant differences were evident in the
baseline data regarding gender, hemoglobin, varicose veins and the
presence or absence of portal vein thrombosis (Table I). In the total diabetic group, no
significant differences were noted in the baseline data between
patients with hepatogenic diabetes and non-hepatogenic
diabetes.
 | Table IBasic characteristics of the two
groups of patients with cirrhosis. |
Table I
Basic characteristics of the two
groups of patients with cirrhosis.
| | EVL group | EIS group |
|---|
| Item | Diabetic group
(n=36) | Non-diabetic group
(n=79) | P-value | Diabetic group
(n=34) | Non-diabetic group
(n=58) | P-value |
|---|
| Age (years) | 55.78±8.98 | 53.80±10.09 | 0.315 | 57.03±9.28 | 48.93±8.59 | <0.001 |
| Sex
(male/female) | 27/9 | 45/34 | 0.064 | 26/8 | 42/16 | 0.669 |
| Hemoglobin (g/l) | 85.50±24.80 | 83.21±20.61 | 0.606 | 75.38±21.86 | 78.91±23.52 | 0.478 |
| Platelet
(109/l) | 87.42±69.94 | 104.94±93.59 | 0.318 | 93.74±68.98 | 108.81±70.77 | 0.320 |
| White blood cell
(109/l) | 3.70±2.06 | 3.68±2.42 | 0.966 | 3.95±2.15 | 4.11±2.90 | 0.769 |
| Albumin (g/l) | 35.07±5.45 | 34.10±6.02 | 0.969 | 34.48±3.89 | 35.49±6.74 | 0.364 |
| Child-Pugh grade
(A/B/C) | 15/17/4 | 45/32/2 | 0.088 | 13/16/5 | 38/18/2 | 0.019 |
| MELD scores | 7.22±3.98 | 8.29±2.35 | 0.141 | 8.71±2.89 | 7.88±2.14 | 0.120 |
| Esophageal varices
(medium/heavy) | 3/33 | 3/76 | 0.375 | 4/30 | 10/48 | 0.480 |
| Red color | 33/36 | 72/79 | 0.926 | 33/34 | 57/58 | 0.699 |
| Diameter of EVs
(cm) | 0.967±0.13 | 0.929±0.15 | 0.192 | 0.935±0.14 | 0.955±0.13 | 0.489 |
| Portal vein
thrombosis | 10/26 | 17/62 | 0.463 | 9/25 | 18/39 | 0.606 |
Post-operative rebleeding rate in the
EVL and EIS groups in the total patient group and the total
diabetic group
Comparisons of the post-operative rebleeding rate in
the EVL and EIS groups in the total patient group and the total
diabetic group are provided in Table
II. In the total patient group, the rebleeding rate in the EVL
subgroup (11.3, 16.5 and 23.5%) was not significantly different
compared with that in the EIS subgroup (9.8, 17.4 and 29.3%) at 1,
3 and 6 months following surgery (P=0.724, 0.868 and 0.339,
respectively). In the total diabetic group, the rebleeding rate in
the EVL group (25.0, 36.1 and 44.4%) was not significantly
different compared with that in the EIS group (20.6, 32.4 and
47.1%) at 1, 3 and 6 months following surgery (P=0.660, 0.741 and
0.826, respectively).
 | Table IIPost-operative rebleeding rate of the
EVL and EIS subgroups of the total patient and the total diabetic
group. |
Table II
Post-operative rebleeding rate of the
EVL and EIS subgroups of the total patient and the total diabetic
group.
| | Total patients | Total diabetic
patients |
|---|
|
Time-point/rebleeding | EVL group | EIS group | EVL group | EIS group |
|---|
| 1 month | | | | |
|
Yes | 13 (11.3) | 9 (9.8) | 9 (25) | 7 (20.6) |
|
No | 102 (88.7) | 83 (90.2) | 27 (75) | 27 (79.4) |
|
P-value | 0.724 | | 0.660 | |
| 3 months | | | | |
|
Yes | 19 (16.5) | 16 (17.4) | 13 (36.1) | 11 (32.4) |
|
No | 96 (83.5) | 76 (82.6) | 23 (63.9) | 23 (67.6) |
|
P-value | 0.868 | | 0.741 | |
| 6 months | | | | |
|
Yes | 27 (23.5) | 27 (29.3) | 16 (44.4) | 16 (47.1) |
|
No | 88 (76.5) | 65 (70.7) | 20 (55.6) | 18 (52.9) |
|
P-value | 0.339 | | 0.826 | |
Rebleeding rates in diabetic and
non-diabetic patients and in hepatogenic and non-hepatogenic
diabetic patients
First, the rebleeding rates were compared between
diabetic and non-diabetic patients (Table III). In the EVL group, the
rebleeding rate in the diabetic subgroup was 25.0% (9/36), 36.1%
(13/36) and 44.4% (16/36) at 1, 3 and 6 months following surgery,
respectively. The rebleeding rates in the non-diabetic group were
5.1% (4/79), 7.6% (6/79) and 13.9% (11/79) at 1, 3 and 6 months
following surgery, respectively. The difference between the two
groups was significant (P=0.005, <0.001 and 0.001, respectively;
Table III).
 | Table IIIComparison of rebleeding rates between
diabetic and non-diabetic patients. |
Table III
Comparison of rebleeding rates between
diabetic and non-diabetic patients.
| | EVL group | EIS group |
|---|
|
Time-point/rebleeding | Diabetic group | Non-diabetic
group | Diabetic group | Non-diabetic
group |
|---|
| 1 month | | | | |
|
Yes | 9 (25.0) | 4 (5.1) | 7 (20.6) | 2 (3.4) |
|
No | 27 (75.0) | 75 (94.9) | 27 (79.4) | 56 (96.6) |
|
P-value | 0.005 | | 0.021 | |
| 3 months | | | | |
|
Yes | 13 (36.1) | 6 (7.6) | 11 (32.4) | 5 (8.6) |
|
No | 23 (63.9) | 73 (92.4) | 23 (67.6) | 53 (91.4) |
|
P-value | <0.001 | | 0.004 | |
| 6 months | | | | |
|
Yes | 16 (44.4) | 11 (13.9) | 16 (47.1) | 11 (19.0) |
|
No | 20 (55.6) | 68 (86.1) | 18 (52.9) | 47 (81.0) |
|
P-value | <0.001 | | 0.004 | |
In the EIS group, the rebleeding rate in the
diabetic subgroup was 20.6% (7/34), 32.4% (11/34) and 47.1% (16/34)
at 1, 3 and 6 months following surgery, respectively. The
rebleeding rate in the non-diabetic group was 3.4% (2/58), 8.6%
(5/58) and 19.0% (11/47) at 1, 3 and 6 months following surgery,
respectively. The difference between the two groups was significant
(P=0.021, 0.004 and 0.004, respectively; Table III).
Binary logistic regression was used to control for
age and liver function grade (Table
IV). The analysis indicated that diabetes was a risk factor for
post-operative rebleeding. In the EVL group, the odds ratio (OR)
with 95% CI was 5.518 (1.535-19.838), 5.861 (1.951-17.612) and
4.294 (1.668-11.054) at 1, 3 and 6 months following surgery
(P=0.004, <0.001, 0.001, respectively). During the first month
of treatment, the EIS group exhibited an OR (95% CI) of 5.900
(0.997-34.929, P=0.05) and at 3 and 6 months, the OR (95% CI) was
3.809 (1.053-13.770) and 3.878 (1.333-11.284), respectively
(P=0.041, 0.013; Table IV).
 | Table IVEffect of diabetes on postoperative
bleeding after controlling age and liver function classification
using binary logistic regression. |
Table IV
Effect of diabetes on postoperative
bleeding after controlling age and liver function classification
using binary logistic regression.
| | EVL group | EIS group |
|---|
| Time-point |
ORunadjust |
Punadjust |
ORadjust |
Padjust |
ORunadjust |
Punadjust |
ORadjust |
Padjust |
|---|
| 1 month | 6.250
(1.778-21.973) | 0.004 | 5.518
(1.535-19.838) | 0.009 | 7.259
(1.412-37.318) | 0.018 | 5.900
(0.997-34.929) | 0.050 |
| 3 months | 6.877
(2.347-20.147) | <0.001 | 5.861
(1.951-17.612) | 0.002 | 5.070
(1.581-16.251) | 0.006 | 3.809
(1.053-13.770) | 0.041 |
| 6 months | 4.945
(1.980-12.352) | 0.001 | 4.294
(1.668-11.054) | 0.003 | 3.798
(1.482-9.727) | 0.005 | 3.878
(1.333-11.284) | 0.013 |
A comparison of rebleeding rates between patients
with hepatogenic and non-hepatogenic diabetes is provided in
Table V. The rebleeding rate in
patients with hepatogenic diabetes was 18.2% (6/33), 30.3% (10/33)
and 39.4% (13/33) at 1, 3 and 6 months following surgery,
respectively. The rebleeding rate in patients with non-hepatogenic
diabetes was 22.9% (8/35), 34.3% (12/35) and 48.6% (17/35) at 1, 3
and 6 months following surgery, respectively. No significant
difference was noted between the two groups at the different
time-points (P=0.634, 0.726 and 0.446, respectively; Table V).
 | Table VComparison of rebleeding rates
between patients with hepatogenic and non-hepatogenic diabetes. |
Table V
Comparison of rebleeding rates
between patients with hepatogenic and non-hepatogenic diabetes.
| | 1 month | 3 months | 6 months |
|---|
| Pathology | Rebleeding | No rebleeding | Rebleeding | No rebleeding | Rebleeding | No rebleeding |
|---|
| Hepatogenic
diabetes | 6 (18.2) | 27 (81.8) | 10 (30.3) | 23 (69.7) | 13 (39.4) | 20 (60.6) |
| Non-hepatogenic
diabetes | 8 (22.9) | 27 (77.1) | 12 (34.3) | 23 (65.7) | 17 (48.6) | 19 (51.4) |
| P-value | 0.634 | | 0.726 | | 0.446 | |
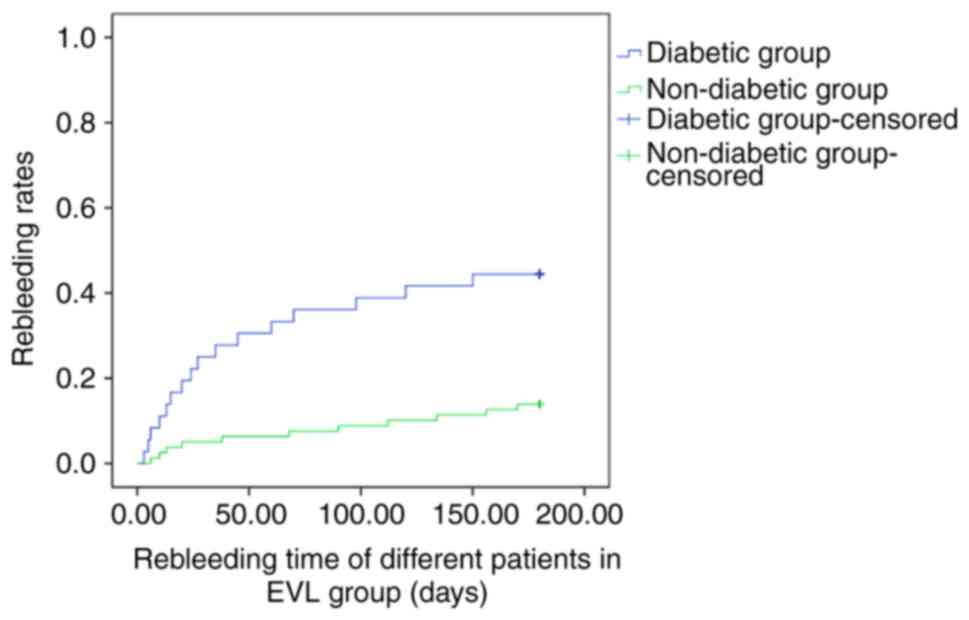
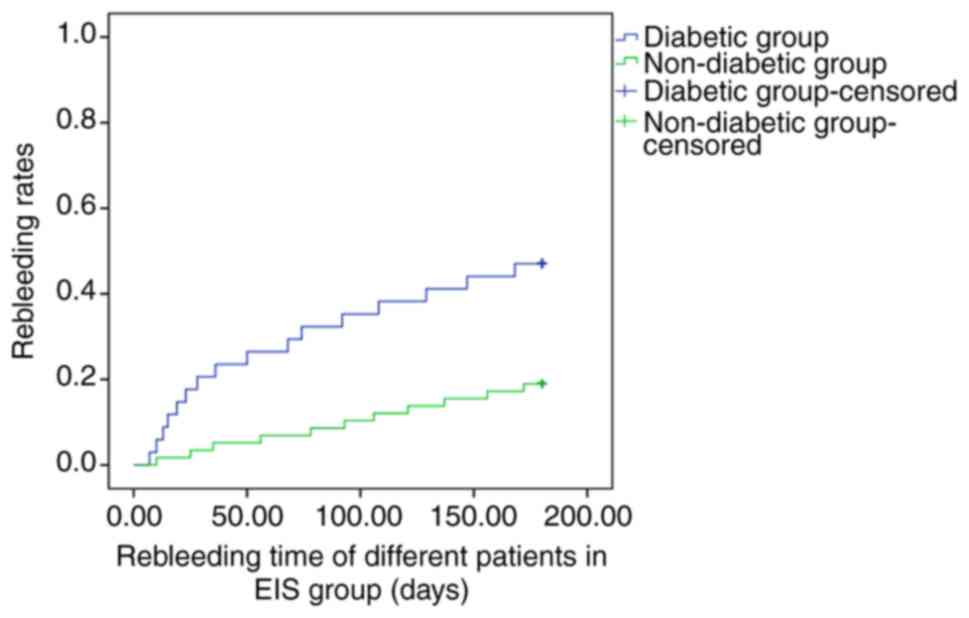
Kaplan-Meier curve analysis and the log-rank test
was used to compare the rebleeding rates after different time
periods between diabetic and non-diabetic groups. Diabetes was
associated with a higher bleeding rate and the difference between
diabetic and non-diabetic groups was significant in the EVL and the
EIS groups (P<0.001 and 0.002; Figs.
3 and 4, respectively).
Post-operative rebleeding rates in
diabetic patients with different liver function grades
The total patient group comprised 70 diabetic
patients, including 28 (40%) with liver function Child-Pugh grade A
and 42 (60%) with Child-Pugh grade of B/C. A total of 137
non-diabetic patients, 83 (60.6%) with liver function Child-Pugh
grade A and 54 (39.4%) with Child-Pugh grade B/C were enrolled. The
difference between the two groups was significant (P=0.005).
In the total diabetic group, the rate of rebleeding in the
Child-Pugh grade A subgroup was 14.3% (4/28), 17.9% (5/28) and
25.0% (7/28) at 1, 3 and 6 months following surgery, respectively.
The rebleeding rate in the Child-Pugh grade B/C group was 28.6%
(12/42), 45.2% (19/42) and 59.5% (25/42) at 1, 3 and 6 months
following surgery, respectively. The differences between the two
groups were not significant at 1 month following surgery (P=0.163),
whereas they were significant at 3 and 6 months following surgery,
respectively (P=0.018 and 0.005, respectively; Table VI).
 | Table VIComparison of post-operative
rebleeding rates in diabetic patients with different liver function
grades. |
Table VI
Comparison of post-operative
rebleeding rates in diabetic patients with different liver function
grades.
| | 1 month | 3 months | 6 months |
|---|
| Child-Pugh
grade | Rebleeding | No rebleeding | Rebleeding | No rebleeding | Rebleeding | No rebleeding |
|---|
| A | 4 (14.3) | 24 (85.7) | 5 (17.9) | 23 (82.1) | 7 (25.0) | 21 (75.0) |
| B/C | 12 (28.6) | 30 (71.4) | 19 (45.2) | 23 (54.8) | 25 (59.5) | 17 (40.5) |
| P-value | 0.163 | | 0.018 | | 0.005 | |
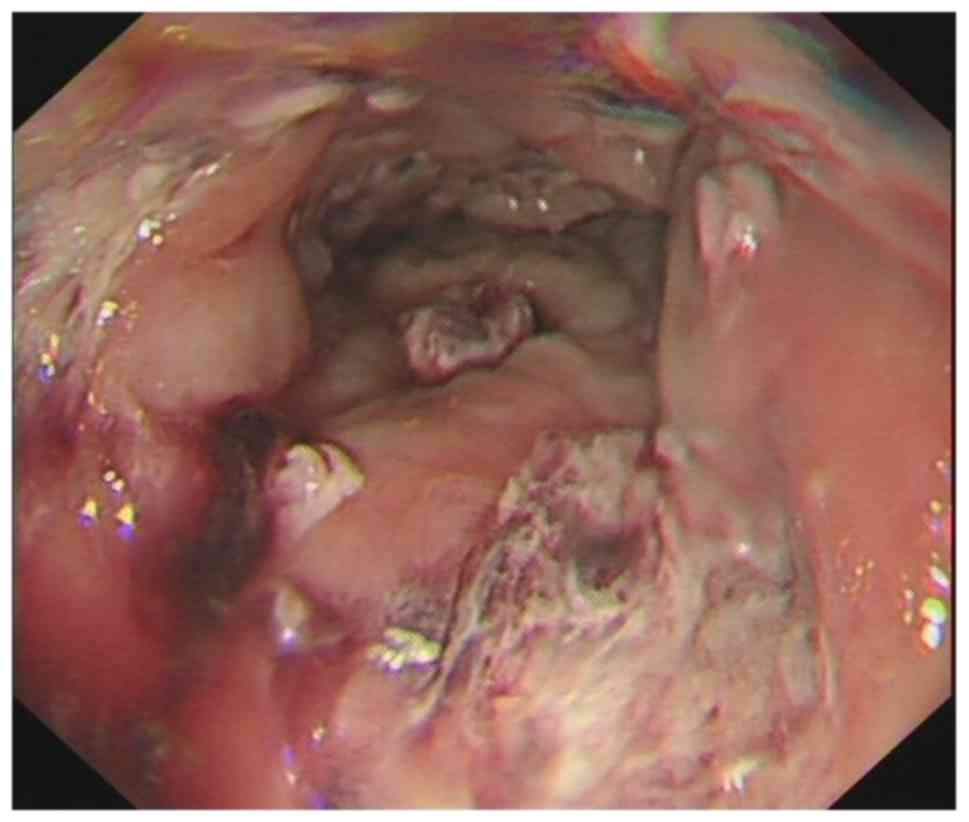
A patient with cirrhosis and diabetes
suffered from major bleeding on the 10th day after EVL
In the present study, one patient with cirrhosis and
diabetes suffered from major bleeding due to shedding of the apron
that occurred 10 days following EVL. The patient was re-admitted to
the First Affiliated Hospital of Anhui Medical University.
Following compression of the Sengstaken-Blakemore tube, the
patient's bleeding stopped. Gastroscopy revealed multiple large,
unhealed ulcers in the esophagus (Fig.
5). To prevent rebleeding, small blood vessels around the ulcer
were treated with sclerotherapy (Fig.
6).
Discussion
Endoscopic treatment is an effective method for EVB.
The emergency hemostasis rate may reach more than 90% (2), which may effectively prevent rebleeding
of patients. This method has become a mainstay of treatment for
esophageal varices. However, the post-operative rebleeding rate is
estimated at ~20%, which frequently affects patient survival
(4). Previous studies have suggested
that liver function Child-Pugh grade B or C, ascites, varicose vein
severity, coagulation function and diabetes are risk factors for
rebleeding following endoscopic treatment (5). These factors are associated with the
prognosis and mortality rate of patients. Hickman and Macdonald
(7) reported that patients with
liver cirrhosis and diabetes account for ~30% of patients with
liver cirrhosis. It was also indicated that diabetes may increase
the incidence of complications and mortality among patients with
cirrhosis (8). Qi et al
(9) and Bai et al (10) reported that diabetes was a
significant factor for predicting the short-term prognosis of
patients with acute upper gastrointestinal bleeding and cirrhosis,
and it was an independent predictor of in-hospital death. The
present retrospective study aimed to further clarify the effects of
diabetes on rebleeding in patients with cirrhosis following
endoscopic therapy.
The present results indicated that the
post-operative rebleeding rate was significantly higher in the
diabetic group compared with that in the non-diabetic group
regardless of the type of treatment (EVL or EIS). These results
indicated that patients with cirrhosis and diabetes exhibited a
higher rate of post-operative rebleeding. However, in the EIS
group, age and liver function grade at baseline were different in
patients with diabetes vs. those of non-diabetic patients. The age
of diabetic patients was higher than that of non-diabetic patients
and the proportion of the liver function grades B and C was higher.
To exclude the effects of these parameters on post-operative
bleeding, age and liver function grade in the EVL and the EIS
groups were controlled using binary logistic regression. The
results indicated that in the EVL group, diabetes was a risk factor
for rebleeding at 1, 3 and 6 months following surgery. In the EIS
group, diabetes was not a significant risk factor for rebleeding at
1 month following surgery (OR: 5.900, 95% CI: 0.997-34.929;
P=0.05). This outcome was possibly associated with the small sample
size (n=92). However, diabetes was a risk factor for rebleeding at
3 and 6 months following surgery. The Kaplan-Meier curve analysis
and the log-rank test further indicated that the differences
between the diabetic and the non-diabetic subgroups were
significant in the EVL and the EIS groups. The post-operative
rebleeding rates were not significantly different between the
patients with hepatogenic and non-hepatogenic diabetes. Patients
with diabetes exhibited a lower wound healing ability than healthy
patients due to continuous hyperglycemia (11,12).
Therefore, the wound healing time was delayed in patients with
cirrhosis and diabetes due to inadequate healing, irrespective of
the endoscopic treatment used, resulting in increased risk of
post-operative rebleeding.
The liver is an important organ of glucose
metabolism, which may effectively maintain the stability of blood
sugar in the human body. Liver cirrhosis damages normal liver
cells, leading to disorders of glucose metabolism, including
abnormal glucose tolerance or hepatogenic diabetes. Long-term
hyperglycemia may further aggravate liver function damage and liver
fibrosis (13,14). In the present study, the proportion
of patients in the diabetic group with a Child-Pugh grade B/C (60%)
was significantly higher than that of patients with Child-Pugh
grade A (40%). Patients with cirrhosis and diabetes exhibited
reduced liver function compared with that of patients without
diabetes. Hunter and Hamdy (15)
indicated that patients with poor liver function and cirrhosis were
more likely to develop rebleeding following surgery. The present
study demonstrated that in the total diabetic patients, the rate of
rebleeding in patients with Child-Pugh grade B/C (28.6%) was higher
than that in those with Child-Pugh grade A (14.3%), although the
differences were not significant. The rate of rebleeding in
patients with Child-Pugh grade B/C at 3 and 6 months following
surgery (45.2 and 59.5%, respectively) was significantly higher
than that in patients with Child-Pugh grade A (17.9 and 25.0%,
respectively). Furthermore, patients with poor liver function
frequently had high-risk factors for a series of hemorrhages,
including hypoalbuminemia, decreased blood coagulation and ascites.
Therefore, it may be hypothesized that improvement of the liver
function may in turn improve the overall condition of patients and
reduce the risk of rebleeding.
In conclusion, the present study demonstrated that
diabetes was a risk factor for post-operative rebleeding in
patients with cirrhosis. Patients with cirrhosis and diabetes
exhibited poor liver function and a high risk of post-operative
rebleeding. Therefore, the treatment of such patients requires
considerable attention in clinical practice. Blood glucose
monitoring and improvement of liver function of patients prior to
surgery are strict indications for the reduction of the risk of
post-operative rebleeding by ligation treatment. The present study
had certain limitations, including the small sample size, short
follow-up duration and lack of investigation of the mechanism by
which cirrhosis interacted with diabetes. Therefore, further
studies are required to address these limitations.
Acknowledgements
Not applicable.
Funding
The present study was supported by the research fund
project of the Anhui Provincial Institute of Translational Medicine
(grant no. 2017zhyx18) and the Anhui Science and Technology
Department: 2018 Key Research and Development Plan Projects (grant
no. 1804h08020260). The funders had no role in the study design,
data collection and analysis, decision to publish, or preparation
of the manuscript.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
DK provided technical support and designed the
study. XW performed the experiments, collected and analysed the
data and wrote the manuscript. XM performed the experiments and
collected and analysed the data. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The study protocol was approved by the Ethics
Committee of Anhui Medical University (Hefei, China) and all
patients provided written informed consent prior to inclusion. The
trial was registered in Chinese Clinical Trial Registry (Title:
Effects of diabetes on the rebleeding rate following endoscopic
treatment in patients with liver cirrhosis; no.
ChiCTR1800017772).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kumar S, Asrani SK and Kamath PS:
Epidemiology, diagnosis and early patient management of
esophagogastric hemorrhage. Gastroenterol Clin North Am.
43:765–782. 2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ali SM, Wu S, Xu H, Liu H, Hao J and Qin
C: A prospective study of endoscopic injection sclerotherapy and
endoscopic variceal ligation in the treatment of esophageal
varices. J Laparoendosc Adv Surg Tech A. 27:333–341.
2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Zargar SA, Javid G, Khan BA, Shah OJ,
Yattoo GN, Shah AH, Gulzar GM, Singh J, Shah NA and Shafi HM:
Endoscopic ligation vs. sclerotherapy in adults with extrahepatic
portal venous obstruction: A prospective randomized study.
Gastrointest Endosc. 61:58–66. 2005.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Garcia-Tsao G, Abraldes JG, Berzigotti A
and Bosch J: Portal hypertensive bleeding in cirrhosis: Risk
stratification, diagnosis, and management: 2016 practice guidance
by the American Association for the study of liver diseases.
Hepatology. 65:310–335. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Xu L, Ji F, Xu QW and Zhang MQ: Risk
factors for predicting early variceal rebleeding after endoscopic
variceal ligation. World J Gastroenterol. 17:3347–3352.
2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Nishida T, Tsuji S, Tsujii M, Arimitsu S,
Haruna Y, Imano E, Suzuki M, Kanda T, Kawano S, Hiramatsu N, et al:
Oral glucose tolerance test predicts prognosis of patients with
liver cirrhosis. Am J Gastroenterol. 101:70–75. 2006.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Hickman IJ and Macdonald GA: Impact of
diabetes on the severity of liver disease. Am J Med. 120:829–834.
2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Quintana JO, García-Compean D, González
JA, Pérez JZ, González FJ, Espinosa LE, Hernández PL, Cabello ER,
Villarreal ER, Rendón RF and Garza HM: The impact of diabetes
mellitus in mortality of patients with compensated liver
cirrhosis-a prospective study. Ann Hepatol. 10:56–62.
2011.PubMed/NCBI
|
|
9
|
Qi X, Peng Y, Li H, Dai J and Guo X:
Diabetes is associated with an increased risk of in-hospital
mortality in liver cirrhosis with acute upper gastrointestinal
bleeding. Eur J Gastroenterol Hepatol. 27:476–477. 2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Bai Z, Li B, Lin S, Liu B, Li Y, Zhu Q, Wu
Y, Yang Y, Tang S, Meng F, et al: Development and validation of
CAGIB score for evaluating the prognosis of cirrhosis with acute
gastrointestinal bleeding: A retrospective multicenter study. Adv
Ther. 36:3211–3220. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Khangholi S, Majid FA, Berwary NJ, Ahmad F
and Aziz RB: The mechanisms of inhibition of advanced glycation end
products formation through polyphenols in hyperglycemic condition.
Planta Med. 82:32–45. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Tian M, Qing C, Niu Y, Dong J, Cao X, Song
F, Ji X and Lu S: The relationship between inflammation and
impaired wound healing in a diabetic rat burn model. J Burn Care
Res. 37:e115–e124. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
García-Compeán D, Jáquez-Quintana JO,
González-González JA, Lavalle-González FJ, Villarreal-Pérez JZ and
Maldonado-Garza HJ: Diabetes in liver cirrhosis. Gastroenterol
Hepatol. 36:473–482. 2013.(In Spanish). PubMed/NCBI View Article : Google Scholar
|
|
14
|
Gundling F, Schepp W and Schumm-Draeger
PM: Hepatogenous diabetes in cirrhosis: Academic sport or a
neglected disease? Exp Clin Endocrinol Diabetes. 120:469–471.
2012.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hunter SS and Hamdy S: Predictors of early
re-bleeding and mortality after acute variceal haemorrhage. Arab J
Gastroenterol. 14:63–67. 2013.PubMed/NCBI View Article : Google Scholar
|