Introduction
Diabetes mellitus (DM) is an endocrine metabolic
disease that affects different organs of the body and is considered
the leading cause of mortality in adults worldwide (1). DM patients are prone to develop
multiple cardiovascular complications, including coronary heart
disease, cardiomyopathy (DMCM) and chronic heart failure (2,3). DMCM is
the major complication of DM that occurs in the heart and is
responsible for significant alterations in the myocardial structure
and function of patients with DM. On average, 40-60% of DM patients
will develop DMCM after suffering DM for 10 years (4). DM is one of the major causes of
mortality worldwide and DMCM is the major chronic complication of
DM that leads to morbidity and mortality in diabetic patients.
Therefore, its prevention and treatment is crucial for DM patients
(5,6).
The use of anti-diabetic drugs has been previously
employed for the treatment of DMCM. However, these compounds were
reported as ineffective and their application was associated with
cardiovascular adverse reactions (7). Therefore, additional novel therapeutic
strategies are necessary for the treatment of this disease
(8). A previous study highlighted
that conventional western medicine combined with traditional
Chinese medicine could be used to treat DMCM (9). At present, it has been shown that Panax
Notoginseng (PNS) exhibits therapeutic effects in the heart tissues
of diabetic subjects (10).
PNS is a widely used traditional Chinese medicine
extracted from the Sanqi or Tianqi plants. This agent exhibits a
wide range of pharmacological and biochemical effects and can be
used to treat specific diseases, such as cardiovascular and
inflammatory disease, bleeding or pain due to injury, as well as
trauma (11). Several chemical
compounds and active ingredients have been isolated from PNS,
including saponins, flavonoids and cyclopeptides. The compound
20(S)-25-OCH3-PPD (25-OH-PPD) was isolated by extraction from the
leaves of PNS. PPD exhibited good therapeutic effects on
cardiovascular diseases, notably as an adjunctive therapy in DMCM
(12).
PPD is the active ingredient of the terpene-saponin
fraction separated and isolated from the leaves of pseudo-ginseng
(13). It has been reported to
possess various types of pharmacological and biochemical effects on
the cardiovascular and immune systems, including anti-inflammatory,
anti-diabetic and anti-atherosclerotic actions (14). It has been previously confirmed that
PPD exhibits a dose-dependent action. However, the exact mechanism
regarding its therapeutic effects in DMCM is currently unclear.
Therefore, in the present study the therapeutic
effects of PPD were evaluated with regard to the progression of
DMCM by monitoring the inhibition of hypertrophy in cardiomyocytes
and by investigating the associated mechanism mediated via the
Akt/glycogen synthase kinase (GSK)-3β pathway. In the present
study, the structure and function of a pathologic left ventricle
was observed and compared with the levels of plasma brain
natriuretic peptide (BNP) and with the volume of myocardial
collagen fraction (CVF). The expression levels of inflammatory
cytokines, including transforming growth factor beta 1 (TGF-β1) and
connective tissue growth factor (CTGF), and of the cell adhesion
molecules α-smooth muscle actin (α-SMA) and vascular adhesion
molecule 1 (VCAM-1) were measured in order to estimate the effects
of PPD on DMCM and the potential signaling mechanisms. Furthermore,
the association of PPD with the Akt/GSK-3β signaling pathway was
examined in the present study.
Materials and methods
Experimental animals and
treatments
Experimental animal care was carried out according
to the guide for the laboratory animals (15) and the present study was followed and
approved by the Medical Ethics Committee of Jinzhou Medical
University. The animals were kept at room temperature in 40-50%
humidity and given access to normal light (12 h light/dark cycle).
A total of 50 SD rats were used in this experiment: 12-week-old
male rats weighing 200-220 g were provided by the Animal lab center
of the Jinzhou Medical University, Jinzhou, China, SYXK: 2014-0002.
The DM animal model was established in 40 SD rats by
intraperitoneal injection of streptozotocin (cat. no. S0130;
Sigma-Aldrich; Merck KGaA). STZ; 50 mg·kg-1 STZ in 0.1 M
citrate buffer solution, pH 4.5). STZ was injected for three days
to induce diabetes and the levels of blood glucose (BG) were tested
using a Gluco-Meter (Accu-Chek Performa, Roche Diagnostics). Values
of BG >200 mg·dl-1 were used as an indication of
successful establishment of the model. The normal group (NG group)
comprised 10 SD experimental animals treated with normal
saline.
Animals groups
The aforementioned 40 diabetic rats were randomly
allocated into four groups as follows: DM model group,
PPD-treatment group [it has been shown in a previous study that PPD
exhibited a dose-dependent mechanism of action (13)], PPD/LY294002 group (LY294002,
inhibitor of PI3K/Akt, 10 µmol·l-1). The
PPD/LiCl-treated group (LiCl, inhibitor of GSK-3β, 20
µmol·l-1). PPD was administered daily at dosages of 5
mg·kg-1 intraperitoneally for 12 weeks. LY294002 and
LiCl were administered daily intravenously. The tested animals in
the NG and DM groups were administered with the same volume of
normal saline as the rats in the PPD groups. The rats of each group
were housed under suitable temperature and humidity conditions for
12 weeks. The DM rats of each different group were provided
high-fat and high-sugar diet (18% fat). The rats in each group were
weighed and non-fasting BG was measured every week in order to
determine the successful establishment of the model. The tested
animals were anesthetized with urethane (intraperitoneally, 1
g·kg-1) following 12 weeks of the appropriate treatment.
The left cardiac functions were examined in order to prove the
presence of cardiomyopathy in the diabetic rats.
Observation of myocardial levels of
creatine phosphokinase isoenzyme (CK-MB), BNP and CVF
Following examination of the left cardiac functions,
the rats were anaesthetized with urethane (intraperitoneally, 1 g
kg-1), the skin and fascia of the chest were cut, the
thorax was opened and the heart removed. The tissues were washed
with PBS solution (0.01 mol·l-1). The extraction and
separation of plasma was performed in order to assess the levels of
the blood biochemical indices by the biochemical analyzer RA50 Semi
auto (Bayer AG). The levels of CK-MB and BNP were also measured in
each group. The heart tissues were cut into sections, then the
samples were treated with 10% polyformaldehyde for 72 h for
fixation, different concentrations of alcohol for dehydration (70,
80, 90, and 100%, each step for 2 min) and xylene to make them
transparent (2 times, 2 min). Samples were then paraffin embedded
and uniform intermittent sections were obtained at a thickness of 5
µm, each of these steps were performed at room temperature 25˚C.
Cardiac collagen and paravascular collagen tissues were stained
using 0.1% Ponceau red at 4˚C stained for 5 min. The volume of CVF
was assessed by the random selection of five fields (CVF=the
collagen area divided by total area x100%).
Measurement of the levels of α-SMA and
VCAM-1
To investigate the inhibitory effects of 25-OH-PPD
on myocardial hypertrophy in DMCM rats, the expression levels of
α-SMA and VCAM-1 were investigated since these factors were shown
to be involved in the proliferation and hypertrophy of myocardial
tissues. The contents of cardiac α-SMA and VCAM-1 in different
groups were tested by ELISA kits (cat. no. PV951; Beyotime
Institute of Biotechnology). The determination was performed
according to the manufacturer's instructions (BD Opt-EIA ELISA Set,
BD Biosciences). The contents of α-SMA and VCAM-1 were measured in
picogram per milliliter (pg ml-1).
Detection of TGF-β1 and CTGF mRNA
levels
TRIzol reagent (Invitrogen, Thermo Fisher
Scientific, Inc.) and the QIA-gen RNA kit (Qiagen GmbH) were used
to collect and purify total RNA. 100 mg heart tissue was added into
1 ml Trizol reagent, and stored at -80˚C. Subsequently, 0.2 ml of
chloroform was added at room temperature, shaken for 15 sec,
centrifuged for 15 min at 12,000 x g at 4˚C, and the supernatant
was then kept at 25˚C for 3 min. A total of 0.6 ml isopropanol was
added to the supernatant, the mixture was gently mixed and after 10
min at 20˚C, the mixture was centrifuged at 12,000 x g, for 10 min
at 4˚C. The supernatant was discarded, 1 ml 75% ethanol was added
to wash the RNA precipitate and the mixture was centrifuged at
7,500 x g, for 5 min at 4˚C. The RNA samples were almost completely
dried at 25˚C and store at -80˚C. When ready to use, the samples
were dissolved in Depc Water (10 min at 55-60˚C, dried in vacuum
for 5-10 min at 25˚C, and then the concentration of RNA was
measured at 260 nm, and stored at -80˚C. The Prime script cDNA
synthesis kit (Bio-Rad Laboratories, Inc.) was used for reverse
transcription of total RNA. Reverse transcription synthesis cDNA.
The OD280 value was determined by UV spectrophotometer after adding
2 µl total RNA into 98 µl sterilized water. DNA Eraser (1 µl) +
total RNA (7 µl) + DNA Eraser buffer (2 µl), 42˚C for 2 min. After
centrifuged at 7,500 x g, for 10 min at 4˚C, the mixture was placed
in the PCR machine at 37˚C for 15 min, followed by 85˚C for 5 sec.
The samples were cooled on ice and stored at -20˚C. The sequence of
the TGF-β1 forward primer was 5'-GAGGGGGAGGAGGAGTGGGA-3' and the
reverse primer was 5'-CCGGGTAGCGATCGAGTGTC-3'. The product length
was 169 bp. CTGF forward primer was 5'-GCAAATAGCCTGTCAATCTC-3' and
the reverse primer was 5'-TCCATAAAAATCTGGCTTGT-3'. The product
length was 414 bp. β-actin was used as the internal control and its
forward primer was 5'-GTGGGCCGCTCTAGGCACCAA-3' and the reverse
primer was 5'-CTCTTTGATGTCACGCACATTTC-3'. Reaction conditions were
as follows: 95˚C, 5 min, pre-denaturation; followed by 94˚C, 30
sec, denaturation; 61˚C, 20 sec, annealing; 72˚C, 20 sec,
extension; 72˚C, 7 min, final extension, for 40 cycles;
Subsequently at 4˚C, thermal insulation. CTGF reaction conditions:
95˚C, 5 min, pre-denaturation; followed by 94˚C, 30 sec,
denaturation; 60˚C, 20 sec, annealing; 72˚C, 30 sec, extension;
72˚C, 7 min, final extension, for 40 cycles; Subsequently at 4˚C,
thermal insulation. PCR was carried out for 40 cycles using the
Bio-Rad iCycle iQ Real Time Detection System. The results were
quantitative analysis by the 2-ΔΔCT method.
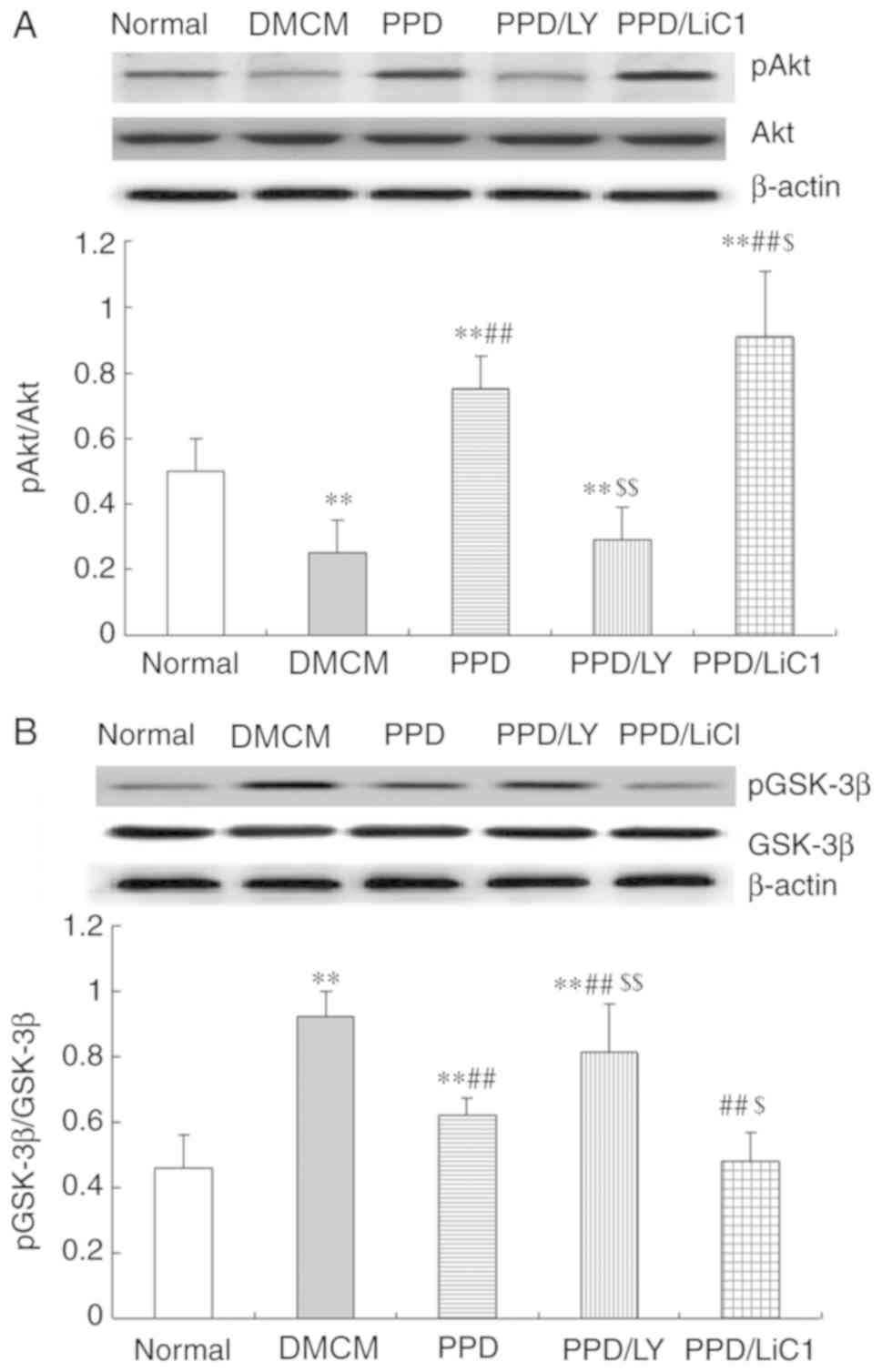
Expressions of AKT and p-AKT
The expression levels of AKT and p-AKT in the heart
tissues of different rats were determined. The BSA protein assay
was used to quantify protein levels. 100 mg myocardial specimens
were added to a 1.5 ml EP tube. A total of 200 µl RIPA buffer
solution (Thermo Fisher Scientific, Inc.) was added and then
crushed by ultrasound. The specimens were left to rest for 30 min
and centrifuged for 25 min at 4˚C at 12,000 x g/min. The proteins
were extracted from tissue homogenates and 50 µg aliquots were
subjected to SDS-PAGE (7.5%) and transferred onto nitrocellulose
membranes. The initial voltage used was 90 V. The transfer was
initially performed for 40 min and subsequently adjusted to 110 V
for 90 min. The membrane was incubated with the following primary
antibodies, which were all diluted to 1:500 in TBS: Rabbit anti-rat
monoclonal antibodies targeting Akt (cat. no. AA326; Beyotime
Institute of Biotechnology Co., Ltd.), phosphorylated (p)-Akt (cat.
no. AA329; Beyotime Institute of Biotechnology), GSK-3β (cat. no.
AG751, Beyotime Institute of Biotechnology Co., Ltd) and p-GSK-3β
(cat. no. AG753; Beyotime Institute of Biotechnology). Incubations
were maintained at 4˚C overnight before rinsing with TTBS 3 times,
each time for 3 min. The membrane was incubated with goat
anti-rabbit alkaline phosphatase labeled anti-second antibodies
(cat. no. A0239; Beyotime Biotechnology Co., Ltd.; 1:500) at room
temperature for 1-2 h. Subsequently, the films were washed with
TTBS 3 times, each time for 10 min. The NBT/BCIP color kit (cat.
no. C3206; Beyotime Biotechnology Co., Ltd.) developing solution
was then added and the reaction was stopped. In the presence of
alkaline phosphatase, BCIP is hydrolyzed to produce a highly
reactive product that reacts with NBT to form an insoluble dark
blue NBT-formazan. The protein bands were analyzed using the
ImageQuant LAS GEL imaging system (GE Healthcare Life Sciences Co.,
Ltd.; 4000 biomolecular imager). This imaging software was used to
analyze the band gray values and calculate the relative protein
expression levels. Protein expression were applied for analysis
using phosphorylated Akt, (p)-Akt, GSK-3β, p-GSK-3β and β-actin
antibodies by Quantitative analysis.
Statistical analysis
Statistical analysis was performed with SPSS version
14.0 statistics software (SPSS, Inc.) and the values were expressed
as the mean ± SD. one-way ANOVAs followed by post-hoc LSD or
Tukey's tests of multiple comparisons were used for statistical
analysis. P<0.05 was considered to indicate a statistically
significant difference..
Results
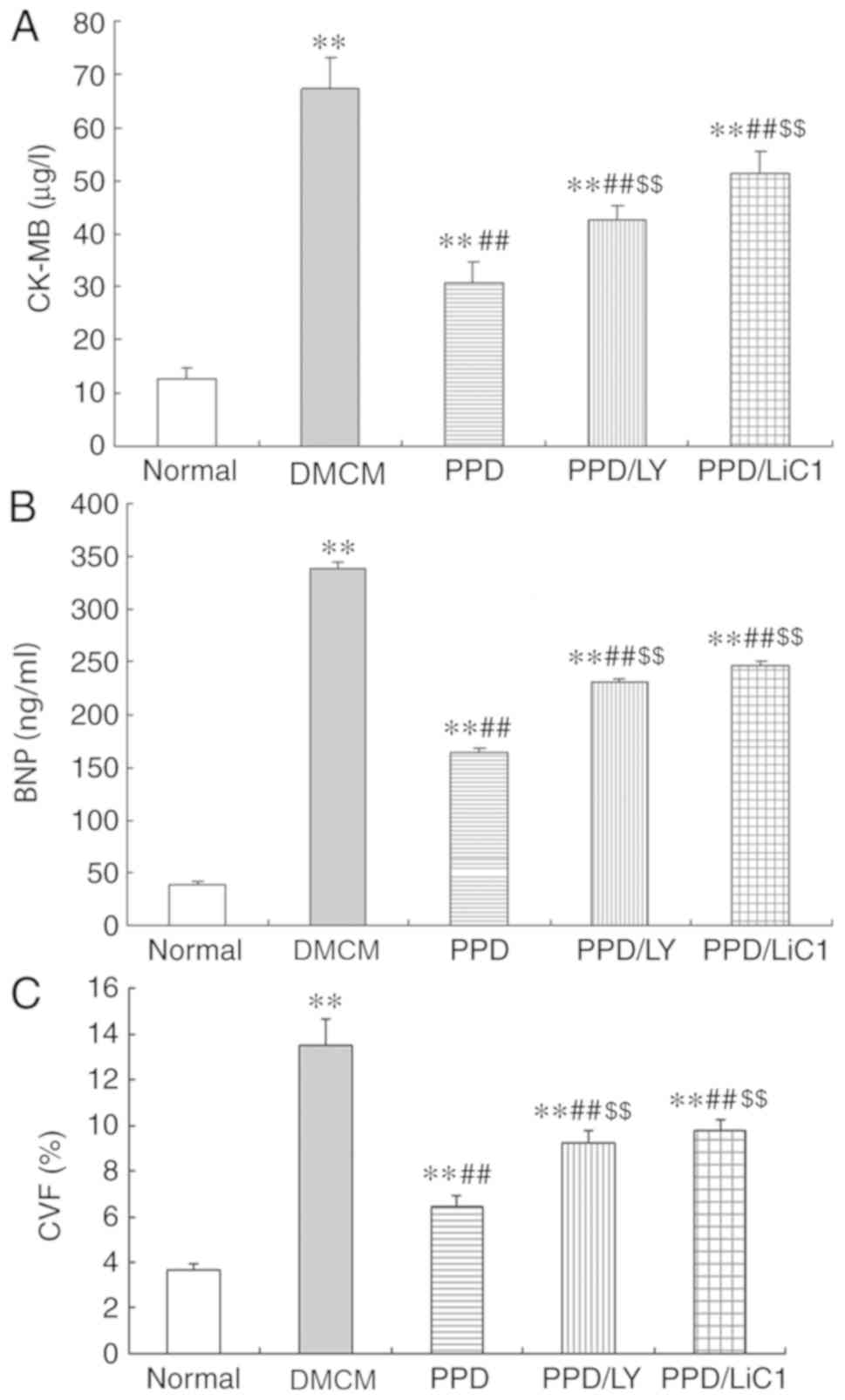
25-OH-PPD reduces the expression
levels of CK-MB, BNP and CVF in diabetic rats
In the present study, PPD increased the body weight
and reduced the blood glucose levels in DM rats. The levels of
CK-MB, BNP and the volume of CVF were all significantly increased
in the DM groups, including the PPD, PPD/LY294002 and PPD/LiCl
groups compared with those noted in the NS control group
(P<0.05). However, the opposite effects were noted by 25-OH-PPD
treatment and significant reductions in the levels of CK-MB, BNP
and the volume of CVF were evident in diabetic animals compared
with those of the DMCM group (P<0.05). The effects of 25-OH-PPD
on the aforementioned results were partially reduced in the
presence of LY294002 and LiCl, whereas an increase in the levels of
CK-MB, BNP and CVF was noted in the PPD/LY294002 and PPD/LiCl
groups (P<0.05) compared with the PPD alone group (Fig. 1A-C).
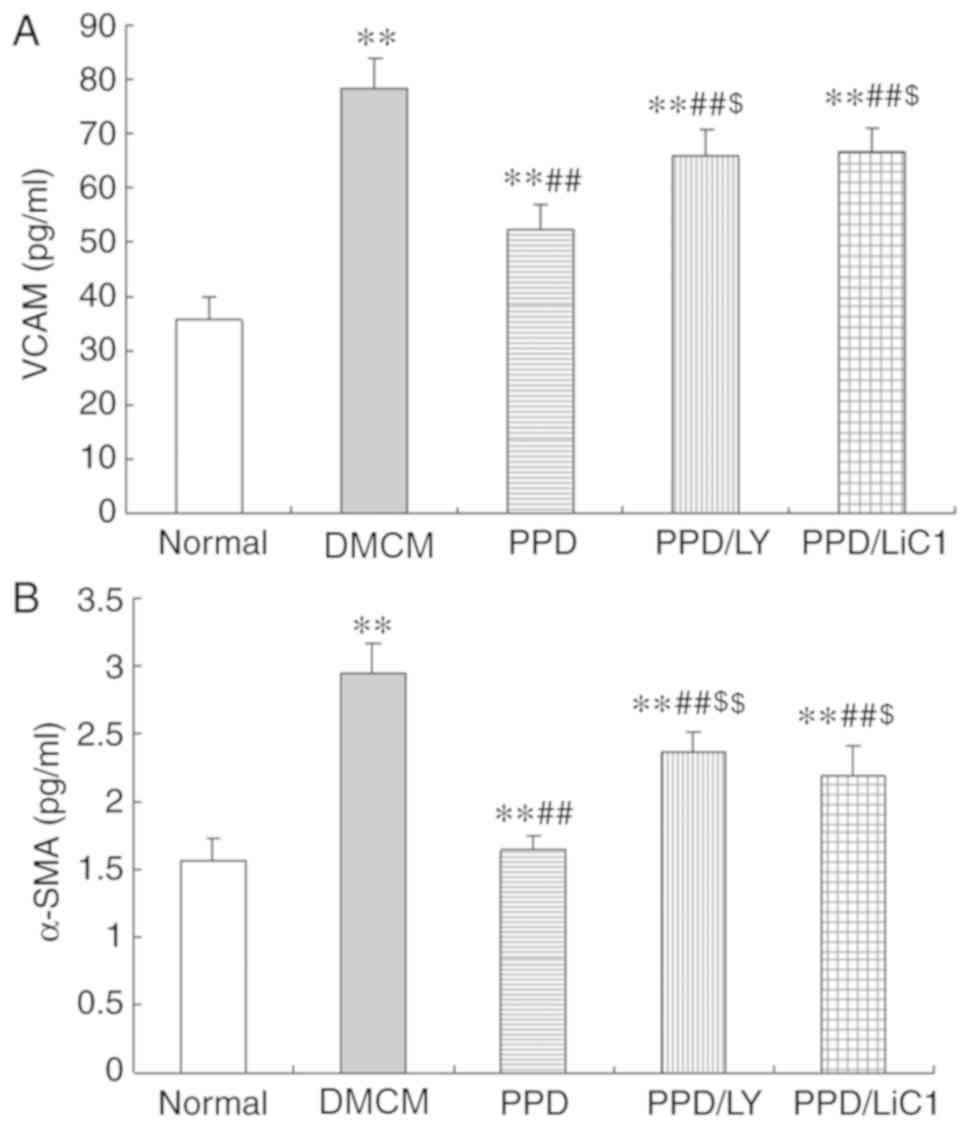
25-OH-PPD reduces the expression
levels of α-SMA and VCAM-1
In the present study, the expression levels of α-SMA
and VCAM-1 were significantly increased in DM animals compared with
those noted in the NS group (P<0.05). In addition, 25-OH-PPD
caused a significant reduction in the levels of α-SMA and VCAM-1 in
the diabetic rats (P<0.01). The effects of PPD on α-SMA and
VCAM-1 were partially attenuated in the LY294002 and LiCl groups
(P<0.05). The expression levels of α-SMA and VCAM-1 were
increased in the PPD/LY294002 and PPD/LiCl groups (P<0.05;
Fig. 2A and B).
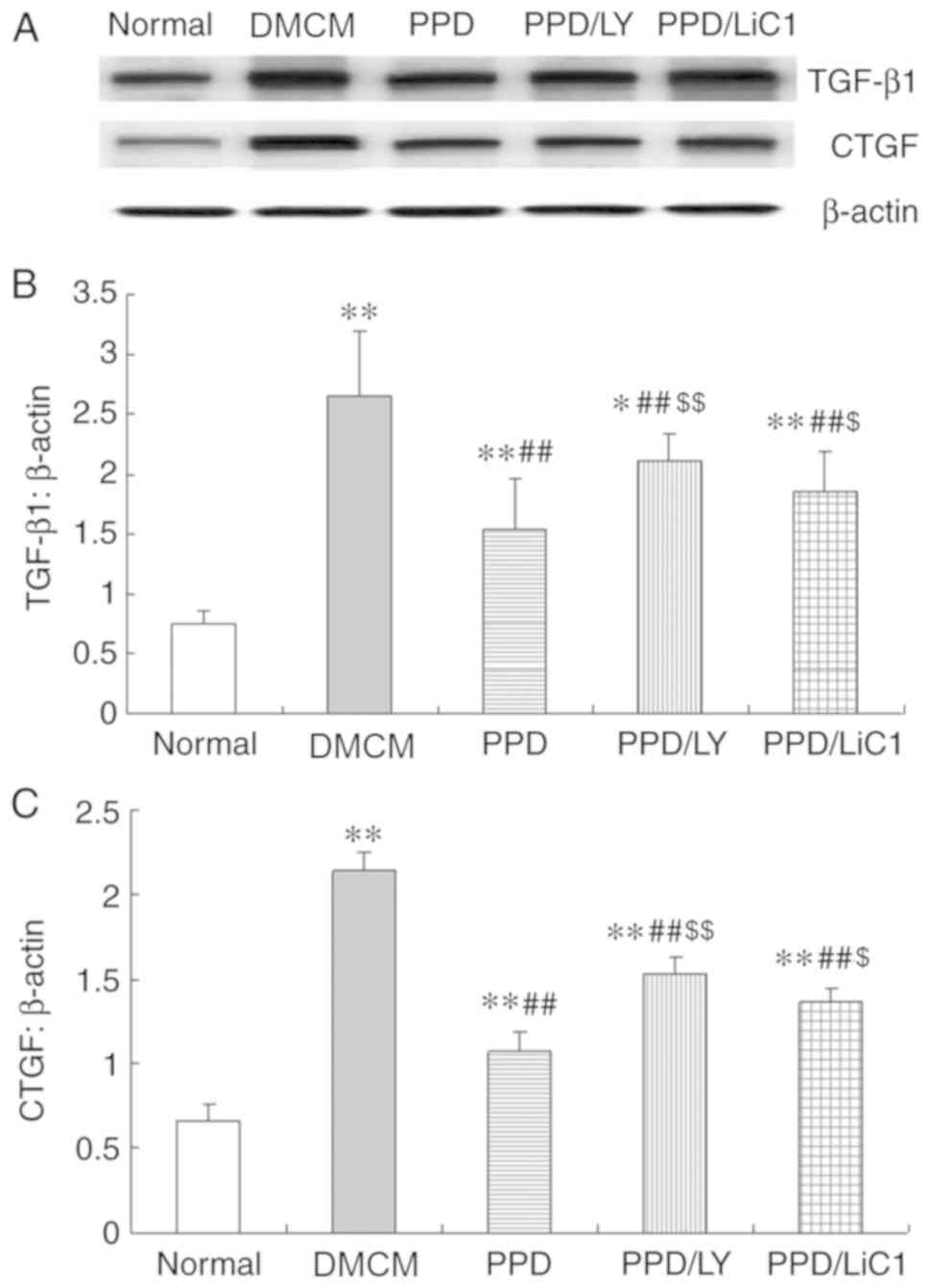
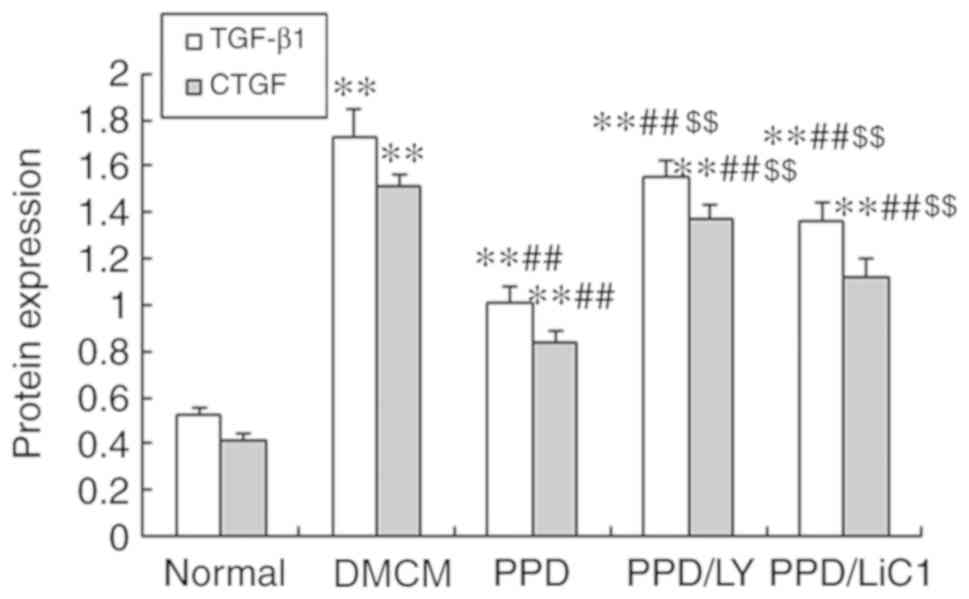
25-OH-PPD reduces the expression
levels of TGF-β1 and CTGF
The data indicated that the expression levels of
TGF-β1 and CTGF were enhanced in the DM and PPD treatment groups,
whereas they were increased in the PPD/LY294002 and PPD/LiCl
groups. These were higher than those noted in the control NS group
(P<0.05). In the present study, it was shown that PPD decreased
both TGF-β1 and CTGF expression levels in DMCM rats and that these
effects were partially weakened by the administration of LY294002
and LiCl (P<0.01 compared with treatment of PPD alone). In
addition, the expression levels of TGF-β1 and CTGF were higher in
the LY294002 and LiCl groups compared with those noted following
single treatment of the animals with 25-OH-PPD (Figs. 3 and 4).
25-OH-PPD activates the PI3k/Akt/GSK-3
β pathway
In the present study, the results demonstrated that
the expression levels of Akt were significantly inhibited and that
the expression levels of GSK-3β were increased in the heart tissues
of DMCM rats. The expression levels of the GSK-3β
pathway-associated proteins were monitored and the results
indicated that Akt levels were reduced in the DMCM group. In
contrast to these findings, 25-OH-PPD significantly enhanced Akt
phosphorylation levels and decreased the expression levels of
p-GSK-3β in diabetic myocardial tissues compared with those of the
DMCM model group. In addition, p-Akt levels were suppressed and
GSK-3β levels were increased in the PPD/LY294002 groups compared
with those noted in the PPD group. In addition, single treatment of
the animals with PPD resulted in a significant increase in the
expression levels of p-Akt and a significant decrease in the
expression levels of GSK-3β in the PPD with LiCl group (P<0.01)
compared with those noted in the control group (Fig. 5A-B).
Discussion
PNS serves as a traditional Chinese drug with
several pharmacological effects. It is commonly applied in the
treatment of specific diseases, such as diabetic retinopathy and
bleeding disorders causing inhibition of bleeding and simultaneous
prevention of thrombosis (16).
Additional applications of this herbal product include improved
wound healing, inhibition of bone and muscle tissue inflammation,
edema and pain management and treatment of traumatic injury
(17).
PNS contains several active compounds, including
anti-oxidant flavonoids, oxygen-rich polysaccharides, ginsenosides,
cyclopeptides and saponins, which are generally useful to enhance
body tissue functions (18).
Previous studies have shown that 25-OH-PPD is a new active
ingredient separated and isolated from the leaves of pseudo-ginseng
that contributes to cellular metabolism (13,14).
This compound exhibits a positive outcome on cardiovascular health
and regulates the immune system by demonstrating anti-inflammatory
and anti-atherosclerotic activities (14,19).
Therefore, it can also be used in the treatment of complications
caused by DM. According to previous studies, 25-OH-PPD has been
shown to regulate blood glucose levels and enhance insulin
sensitivity in diabetes (13,14,19).
Subsequent reduction in blood glucose levels may be applied for the
treatment of non-insulin dependent diabetes mellitus (type 2,
NIDDM). These results suggested that 25-OH-PPD could be used as a
drug target for the treatment of insulin resistant and diabetic
complications (10). However, it is
still uncertain if its protective effects and molecular mechanism
exhibit potential clinical applications for the treatment of
DMCM.
In the present study, 25-OH-PPD reduced the levels
of BNP and CK-MB following 12 weeks of administration to the
diabetic animals. The volume of CVF was increased in the diabetic
rats that exhibited DMCM and existent myocardial damage. These
findings suggested that 25-OH-PPD was beneficial for the treatment
of DM by reversing the complications of DMCM. This finding was
consistent with a previous study that used diabetic rats in the
presence of PPD and characterized the levels of collagen
accumulation and the induction of cardiac hypertrophy and
remodeling (11). DMCM is a major
complication of DM and can induce cardiac dysfunction (dysfunction
of sugar and fat metabolism) in diabetic patients (20). The major pathophysiological changes
noted in DMCM include cardiomyocyte degeneration and necrosis with
myocardial interstitial fibrosis, which in turn induces myocardial
hypertrophy and remodeling (21).
The pathophysiological changes induce myocardial remodeling and
play an important role in the pathogenesis of DMCM (22). The results of the present study
suggested that 25-OH-PPD could inhibit hypertrophy and reverse the
remodeling of DMCM.
The data of the present study indicated that
25-OH-PPD could significantly reduce the levels of α-SMA and VCAM-1
in the diabetic rat model. VCAM-1 is an inflammatory mediator
involved in obesity, diabetes and cardiovascular and inflammatory
diseases. It also plays a key function in the progression of
hypertrophy and cardiac remodeling in DMCM (23). In addition, α-SMA is the major factor
which induces tissue and cell fibroblast differentiation by
regulating these processes. α-SMA overexpression increases collagen
contraction and promotes proliferative activity as demonstrated by
a previous study (24). Inhibition
of α-SMA expression may reduce development of tissue fibrosis,
notably in acellular fibrotic lung scaffolds (25). Previous studies have suggested that
the increased levels of α-SMA expression induced by high-glucose
conditions are an important event in renal tubule-interstitial
fibrosis, which is a clinical manifestation of diabetic nephropathy
(26,27). In the present study, the results
indicated that 25-OH-PPD-inhibited overexpression of α-SMA and that
VCAM may serve as a potential therapeutic target for vascular
injury and myofibroblast migration (28,29). In
addition, the effects of 25-OH-PPD on α-SMA and VCAM-1 expression
levels were partially suppressed in the presence of LY294002 and
LiCl, suggesting that inhibition of the proliferative effects of
25-OH-PPD may be mediated via the PI3K/Akt/GSK3β signaling pathway
in DMCM.
At present, the pathogenesis of DMCM is still
unclear and its causes are believed to be multifactorial. Previous
studies have shown that complications of DMCM involve
hyperglycemia, fat metabolism disorders, inflammatory reactions,
apoptosis and oxidative stress (5,30). High
glucose levels can lead to enhanced expression levels of myocardial
TGF-β1 and CTGF (31). However,
25-OH-PPD reduced the expression levels of these factors and its
action was accompanied with the subsequent inhibition of cardiac
fibrosis mediated by the inactivation of the PI3k/Akt/GSK-3β
signaling pathway (32). It has been
shown that the inflammatory cytokines, namely TGF-β1 and CTGF are
highly expressed in diabetic cardiomyocytes, which results in the
development of various biological processes including
differentiation, extracellular matrix accumulation, cell
proliferation, reconstitution, apoptosis and remodeling (33). TGF-β1 is a major inflammatory factor
and a potent profibrotic cytokine (34). The levels of this cytokine were
significantly increased by high blood glucose concentrations, which
triggered tissue fibrosis. TGF-β1 promotes the synthesis and
secretion of collagen by myocardial fibroblasts and induces
myocardial hypertrophy (35). CTGF
acts as a downregulation factor of TGF-β1 in this process (36). In the present study, the expression
levels of TGF-β1 and CTGF in the diabetic group were significantly
higher compared with the NG group, indicating that 25-OH-PPD could
reduce TGF-β1 and CTGF levels in the DM rats suggesting its role in
the inhibition of cardiac remodeling and in the treatment of
DMCM.
The results of the present study further
demonstrated that p-Akt levels were suppressed and that GSK-3β
levels were enhanced in the PPD/LY294002 group compared with those
in the PPD group. In addition, the expression levels of p-Akt were
increased and those of GSK-3β were decreased in the PPD/LiCl group
compared with the PPD group. The Akt signaling pathway promotes
cellular survival by inhibiting the action of a series of target
proteins in the apoptotic signaling pathway. Akt exhibits distinct
key roles in regulating cardiovascular functions, such as blood
pressure, regulation of myocardial systolic and diastolic
functions, coronary angiogenesis and atherosclerosis (37). GSK-3β is the major substrate of the
Akt-GSK-3β pathway that exerts specific physiological and
biochemical functions in glycogen metabolism and plays a decisive
role in diabetes-induced inflammation and fibrosis (38). Previous investigations have
demonstrated that the Akt-GSK-3β signaling pathway plays an
important function in diabetes-induced energy metabolic dysfunction
and consequently in heart hypertrophy (39,40). In
diabetes mellitus, the expression levels of p-Akt were decreased by
free fatty acids and inflammatory cytokines, which led to the
activation of GSK-3β (41,42). In addition, the data of the present
study indicated that triciribine could partially reduce the actions
of 25-OH-PPD on DMCM. These findings suggested that PPD prevented
the development of DMCM via the p-Akt-GSK-β signaling pathway.
In summary, the results of the present study
demonstrated that 25-OH-PPD could inhibit the progression of
cardiac dysfunction, myocardial hypertrophy and inflammation in
DMCM. The cell growth inhibitory mechanism of 25-OH-PPD was
mediated by downregulation of TGF-β1 and CTGF expression via the
PI3K-Akt-GSK-β signaling pathway. The present study demonstrated
the application and mechanism of action of an effective therapeutic
drug that can be used for the treatment of DMCM.
The present study provided evidence that 25-OH-PPD
could suppress α-SMA/VCAM expression and downregulate the levels of
the inflammatory cytokines, such as TGF-β1 and CTGF. In addition,
it significantly improved cardiac functions and inhibited
myocardial hypertrophy and inflammation in DMCM via the
PI3k-Akt-GSK-3β signaling pathway.
Acknowledgements
We thank Dr Junxian (Department of pharmacy, Beijing
friendship hospital of capital medical university) for expert
technical assistance.
Funding
The present study was supported by the Natural
Foundation Guidance Plan of Liaoning Province (grant nos.
2019-ZD-0822 and 2019-ZD-0821) and the Key Research and Development
Program Guidance Program Project of Liaoning Province (grant no.
2018225030).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XL performed the experiments in the present study;
FS prepared the animal models; CL was responsible for the
statistics and writing the article, as well as organizing the
study; YZ analyzed the immunohistochemistry data. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
This experiment was approved by the ethics committee
of JinZhou Medical University.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Gregg EW, Cheng YJ, Srinivasan M, Lin J,
Geiss LS, Albright AL and Imperatore G: Trends in cause-specific
mortality among adults with and without diagnosed diabetes in the
USA: An epidemiological analysis of linked national survey and
vital statistics data. Lancet. 16:2430–2440. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Jun JE, Lee SE, Choi MS, Park SW, Hwang YC
and Kim JH: Clinical factors associated with the recovery of
cardiovascular autonomic neuropathy in patients with type 2
diabetes mellitus. Cardiovasc Diabetol. 18:29–30. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Mahajan UB, Chandrayan G, Patil CR, Arya
DS, Suchal K, Agrawal Y, Ojha S and Goyal SN: Eplerenone attenuates
myocardial infarction in diabetic rats via modulation of the
PI3K-Akt pathway and phosphorylation of GSK-3β. Am J Transl Res.
10:2810–2821. 2018.PubMed/NCBI
|
|
4
|
Hölscher ME, Bode C and Bugger H: Diabetic
cardiomyopathy: Does the type of diabetes matter? Int J Mol Sci.
17(2136)2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Furuya F, Ishii T and Kitamura K: Chronic
inflammation and progression of diabetic kidney disease. Contrib
Nephrol. 198:33–39. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lombardi C, Spigoni V, Gorga E and Dei Cas
A: Novel insight into the dangerous connection between diabetes and
heart failure. Herz. 41:201–207. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Huber SA: Viral myocarditis and dilated
cardiomyopathy: Etiology and pathogenesis. Curr Pharm Des.
22:408–426. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Yoshida Y, Boren SA, Soares J, Popescu M,
Nielson SD, Koopman RJ, Kennedy DR and Simoes EJ: Effect of health
information technologies on cardiovascular risk factors among
patients with diabetes. Curr Diab Rep. 19(28)2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Guo X, Xue M, Li CJ, Yang W, Wang SS, Ma
ZJ, Zhang XN, Wang XY, Zhao R and Chang BC: Protective effects of
triptolide on TLR4 mediated autoimmune and inflammatory response
induced myocardial fibrosis in diabetic cardiomyopathy. J
Ethnopharmacol. 193:333–344. 2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kitamura K, Takamura Y, Iwamoto T, Nomura
M, Iwasaki H, Ohdera M, Murakoshi M, Sugiyama K, Matsuyama K,
Manabe Y, et al: Dammarane-type triterpene extracts of Panax
notoginseng root ameliorates hyperglycemia and insulin sensitivity
by enhancing glucose uptake in skeletal muscle. Biosci Biotechnol
Biochem. 81:335–342. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hu S, Liu T, Wu Y, Yang W, Hu S, Sun Z, Li
P1 and Du S: Panax notoginseng saponins suppress
lipopolysaccharide-induced barrier disruption and monocyte adhesion
on bEnd.3 cells via the opposite modulation of Nrf2 antioxidant and
NF-κB inflammatory pathways. Phytother Res. 33:3163–3176.
2019.PubMed/NCBI View
Article : Google Scholar
|
|
12
|
Jin X, Luo Y, Chen Y, Ma Y, Yue P and Yang
M: Novel breviscapine nanocrystals modified by panax notoginseng
saponins for enhancing bioavailability and synergistic
anti-platelet aggregation effect. Colloids Surf B Biointerfaces.
175:333–342. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Yu J, Liu C, Li Z, Zhang C, Wang Z and Liu
X: Inhibitory effects and mechanism of 25-OH-PPD on glomerular
mesangial cell proliferation induced by high glucose. Environ
Toxicol Pharmacol. 44:93–98. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Shi X, Yu W, Yang T, Qiu S, Yao C, Feng Z,
Wei W, Wu W and Guo D: Panax notoginseng saponins provide
neuroprotection by regulating NgR1/RhoA/ROCK2 pathway expression,
in vitro and in vivo. J Ethnopharmacol. 190:301–312.
2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Liu X, Liu C, Li J, Zhang X, Song F and Xu
J: Urocortin attenuates myocardial fibrosis in diabetic rats via
the Akt/GSK-3β signaling pathway. Endocr Res. 41:148–157.
2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Xie W, Meng X, Zhai Y, Zhou P, Ye T, Wang
Z, Sun G and Sun X: Panax notoginseng saponins: A review of its
mechanisms of antidepressant or anxiolytic effects and network
analysis on phytochemistry and pharmacology. Molecules.
17(940)2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Loh YC, Tan CS, Ch'ng YS, Ng CH, Yeap ZQ
and Yam MF: Mechanisms of action of Panax notoginseng ethanolic
extract for its vasodilatory effects and partial characterization
of vasoactive compounds. Hypertens Res. 42:182–194. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Chan YS, Wong JH and Ng TB: Bioactive
proteins in Panax notoginseng roots and other panax species. Curr
Protein Pept Sci. 20:231–239. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Yin Z, Ma L, Xu J, Xia J and Luo D:
Pustular drug eruption due to Panax notoginseng saponins. Drug Des
Devel Ther. 16:957–961. 2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Joubert M, Manrique A, Cariou B and Prieur
X: Diabetes-related cardiomyopathy: The sweet story of glucose
overload from epidemiology to cellular pathways. Diabetes Metab.
45:238–247. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Guo X, Sun W, Luo G, Xia J and Luo D:
Panax notoginseng saponins alleviate skeletal muscle insulin
resistance by regulating the IRS1-PI3K-AKT signaling pathway and
GLUT4 expression. FEBS Open Bio. 9:1008–1019. 2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ding W, Chang WG, Guo XC, Liu Y, Xiao DD,
Ding D, Wang JX and Zhang XJ: Exenatide protects against cardiac
dysfunction by attenuating oxidative stress in the diabeticmouse
heart. Front Endocrinol (Lausanne). 10(202)2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Shinde AV, Humeres C and Frangogiannis NG:
The role of α-smooth muscle actin in fibroblast-mediated matrix
contraction and remodeling. Biochim Biophys Acta. 1863:298–309.
2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Guo SJ, Zhang P, Wu LY, Zhang GN, Chen WD
and Gao PJ: Adenovirus-Mediated overexpression of septin 2
attenuates α-Smooth muscle actin expression and adventitial
myofibroblast migration induced by angiotensin II. J Vasc Res.
53:309–316. 2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Sun KH, Chang Y, Reed NI and Sheppard D:
α-Smooth muscle actin is an inconsistent marker of fibroblasts
responsible for force-dependent TGFβ activation or collagen
production across multiple models of organ fibrosis. Am J Physiol
Lung Cell Mol Physiol. 310:L824–L836. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Huang H, Zheng F, Dong X, Wu F, Wu T and
Li H: Allicin inhibits tubular epithelial-myofibroblast
transdifferentiation under high glucose conditions in vitro.
Exp Ther Med. 13:254–262. 2017.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Zhang J, Chu HR, Guo Y, Liu JH, Li WP, Li
H and Cheng M: The effects and mechanisms of high glucose on the
phenotype transformation of rat vascular smooth muscle cells.
Zhongguo Ying Yong Sheng Li Xue Za Zhi. 31:458–461. 2015.PubMed/NCBI(In Chinese).
|
|
28
|
Yu GI, Jun SE and Shin DH: Associations of
VCAM-1 gene polymorphisms with obesity and inflammation markers.
Inflamm Res. 66:217–225. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Weber ZA, Kaur P, Hundal A, Ibriga SH and
Bhatwadekar AD: Effect of the pharmacist-managed cardiovascular
risk reduction services on diabetic retinopathy outcome measures.
Pharm Pract (Granada). 17(1319)2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Wang SQ, Li D and Yuan Y: Long-term
moderate intensity exercise alleviates myocardial fibrosis in type
2 diabetic rats via inhibitions of oxidative stress and TGF-β1/Smad
pathway. J Physiol Sci. 69:861–873. 2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Abdel-Hamid AAM and Firgany AEL: Favorable
outcomes of metformin on coronary microvasculature in experimental
diabetic cardiomyopathy. J Mol Histol. 49:639–649. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Zhao B, Guan H, Liu JQ, Zheng Z, Zhou Q,
Zhang J, Su LL and Hu DH: Hypoxia drives the transition of human
dermal fibroblasts to a myofibroblast-like phenotype via the
TGF-β1/Smad3 pathway. Int J Mol Med. 39:153–159. 2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Wang Y, Zhao L, Jiao FZ, Zhang WB, Chen Q
and Gong ZJ: Histone deacetylase inhibitor suberoylanilide
hydroxamic acid alleviates liver fibrosis by suppressing the
transforming growth factor-β1 signal pathway. Hepatobiliary
Pancreat Dis Int. 17:423–429. 2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kim KK, Sheppard D and Chapman HA: TGF-β1
Signaling and tissue fibrosis. Cold Spring Harb Perspect Biol.
2(a022293)2018.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Chen JQ, Guo YS, Chen Q, Cheng XL, Xiang
GJ, Chen MY, Wu HL, Huang QL, Zhu PL and Zhang JC: TGFβ1 and HGF
regulate CTGF expression in human atrial fibroblasts and are
involved in atrial remodelling in patients with rheumatic heart
disease. J Cell Mol Med. 23:3032–3039. 2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Tsai CC, Wu SB, Kau HC and Wei YH:
Essential role of connective tissue growth factor (CTGF) in
transforming growth factor-β1 (TGF-β1)-induced myofibroblast
transdifferentiation from Graves' orbital fibroblasts. Sci Rep.
8(7276)2018.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Wang X, Pan J, Liu D, Zhang M, Li X, Tian
J, Liu M, Jin T and An F: Nicorandil alleviates apoptosis in
diabetic cardiomyopathy through PI3K/Akt pathway. J Cell Mol Med.
23:5349–5359. 2019.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Zheng W, Shang X, Zhang C, Gao X, Robinson
B and Liu J: The effects of carvedilol on cardiac function and the
AKT/XIAP signaling pathway in diabetic cardiomyopathy rats.
Cardiology. 136:204–211. 2017.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Shang L, Pin L, Zhu S, Zhong X, Zhang Y,
Shun M, Liu Y and Hou M: Plantamajoside attenuates
isoproterenol-induced cardiac hypertrophy associated with the HDAC2
and AKT/GSK-3β signaling pathway. Chem Biol Interact. 307:21–28.
2019.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Wang CY, Li XD, Hao ZH and Xu D:
Insulin-like growth factor-1 improves diabetic cardiomyopathy
through antioxidative and anti-inflammatory processes along with
modulation of Akt/GSK-3β signaling in rats. Korean J Physiol
Pharmacol. 20:613–619. 2016.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Liu X, Liu C, Zhang X, Zhao J and Xu J:
Urocortin ameliorates diabetic cardiomyopathy in rats via the
Akt/GSK-3β signaling pathway. Exp Ther Med. 9:667–674.
2015.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Yang Q, Huang DD, Li DG, Chen B, Zhang LM,
Yuan CL and Huang HH: Tetramethylpyrazine exerts a protective
effect against injury from acute myocardial ischemia by regulating
the PI3K/Akt/GSK-3β signaling pathway. Cell Mol Biol Lett.
24(17)2019.PubMed/NCBI View Article : Google Scholar
|