Introduction
Bronchial asthma is a clinically common disease in
the Respiratory Department. It is an airway inflammatory disease
characterized by airway hyperreactivity and increased secretion of
airway mucus. This disease is closely related to tissue
inflammation caused by massive inflammatory cell infiltration
(1). According to epidemiological
statistics, asthma tends to occur in children, putting a heavy
burden on patients, families and society (2). Moreover, it is proved that asthmatic
infants with rickets account for about 20.1% of asthmatic infants
in clinical practice (3). Vitamin D
deficiency, as the main cause of infant rickets, can also lead to
the imbalance of immunomodulatory mechanism in infants and young
children, affecting the inherent immune system and acquired immune
system, thus causing the attack of asthma (4). Vitamin D is positively correlated with
the incidence of infection, which is the main cause of respiratory
tract infection in children with rickets, and repeated respiratory
tract infection can lead to increased airway responsiveness, which
leads to asthma (5). Vitamin D not
only adjusts calcium and phosphorus metabolism, but also plays an
important role in cell growth, differentiation and immune function.
Studies have shown that vitamin D deficiency can lead to B cell
differentiation and maturation disorder, which in turn leads to
hypoglobulin (6,7). There is a certain correlation between
vitamin D, inflammatory factors and immunoglobulin in infants with
asthma complicated with rickets.
This study investigated the correlation between
asthmatic infants with rickets and vitamin D, inflammatory factors
and immunoglobulin, so as to identify the risk factors of infantile
asthma with rickets.
Patients and methods
General data
A total of 60 children diagnosed as asthma and
treated for the first time from January 2016 to October 2017 in The
First Affiliated Hospital of Xinjiang Medical University (Urumqi,
China) were collected. Among them, according to the diagnostic
criteria of rickets, 17 asthmatic infants with rickets were set as
the observation group, while 43 children with simple asthma were
regarded as the control group. There were 10 males and 7 females
aged 1.23±1.52 years in the observation group, while there were 28
males and 15 females aged 1.83±1.21 years in the control group. No
differences were found in age and gender between the two groups,
which were comparable.
The study was approved by the Ethics Committee of
The First Affiliated Hospital of Xinjiang Medical University and
written informed consents were signed by the guardians.
Diagnostic criteria
Diagnostic criteria of infantile asthma (8): i) age ≤3 years; ii) wheeze more than
three times: 3 points; iii) wheezing rale: 2 points; iv) sudden
attack of wheezing: 1 point; and v) other specific medical history:
1 point. The patients with the total score >5 points could be
diagnosed as infantile asthma. The diagnostic criteria of rickets
referred to the textbook of Pediatrics (9). i) Serum 25 (OH) D 3 and 1, 25 (OH) 2D3
were significantly lower than normal. ii) Increased excretion of
alkaline phosphatase in urine. iii) In the early stage of X-ray,
the calcification preparation line of long bone metaphysis was
blurred. In stadium acmes, calcification preparation line
disappeared, the epiphyseal end widened, the metaphysis changed in
the shape of cup or brush, the bone was sparse, and the shaft was
curved and deformed or fractured.
Inclusion criteria
The inclusion criteria were: i) patients who met the
above-mentioned diagnostic criteria for infantile asthma and
rickets; ii) patients without other critical diseases; iii)
patients who received no relevant treatment at the first visit; and
iv) patients whose guardians agreed to participate in the study and
complied with the doctor's advice.
Methods Collection of specimen
Venous blood was immediately drawn from subjects in
the observation group and the control group after admission. The
blood was centrifuged at 3,000 x g for 15 min at 4˚C, and then
supernatant was collected. The expression levels of interleukin-1
(IL-1), IL-6 and IL-17 in venous blood serum were determined in
accordance with instructions of the ELISA kit (cat. nos. ab46052,
ab178013 and ab119535; Abcam), vitamin D and immunoglobulin E
levels in venous blood serum were detected using a fully-automatic
biochemical analyzer, and wheezing duration of child patients was
recorded by the average time of 6 consecutive asthma attacks.
ELISA detection
i) Sample loading: 100 µl standard sample or the
serum to be detected was added to each well and fully mixed, and
then the plate was placed for reaction at 37˚C for 40 min. ii)
Washing: the reaction plate was rinsed by washing liquid 4-6 times,
and dried on filter paper. iii) 50 µl distilled water and 50 µl
first antibody working fluid in the kit were added to each well
(except the blank group) and fully mixed, and then the plate was
placed for reaction at 37˚C for 20 min. iv) Washing: The plate was
rinsed by washing liquid 4-6 times, and dried on filter paper. v)
100 µl enzyme-labeled antibody working fluid in the kit was added
to each well, and then the plate was placed for reaction at 37˚C
for 10 min. vi) Washing: The plate was rinsed by washing liquid 4-6
times, and dried on filter paper. vii) 100 µl substrate working
fluid in the kit was added to each well, and then the plate was
placed for reaction in a dark place at 37˚C for 15 min. viii) 100
µl stop buffer in the kit was added to each well and fully mixed.
ix) The absorbance value was detected by a microplate reader at 450
nm.
Detection using the fully-automatic
biochemical analyzer
The collected venous blood serum was put into the
fully-automatic biochemical instrument. Vitamin D and
immunoglobulin levels in serum were detected after the detection
parameters were set.
Statistical analysis
SPSS 20.0 software (SPSS, Inc.) was adopted for
statistical analysis in this study. Enumeration data were expressed
as mean ± standard deviation. The t-test was used for data in line
with normal distribution and homogeneity of variance, and the
corrected t-test was utilized for data in line with normal
distribution and heterogeneity of variance. Non-parametric test was
adopted for data not in line with normal distribution and
homogeneity test of variance, rank sum test for rank data, and
Chi-square test for enumeration data. Pearson correlation analysis
was utilized for correlation analysis. P<0.05 was considered to
indicate a statistically significant difference.
Results
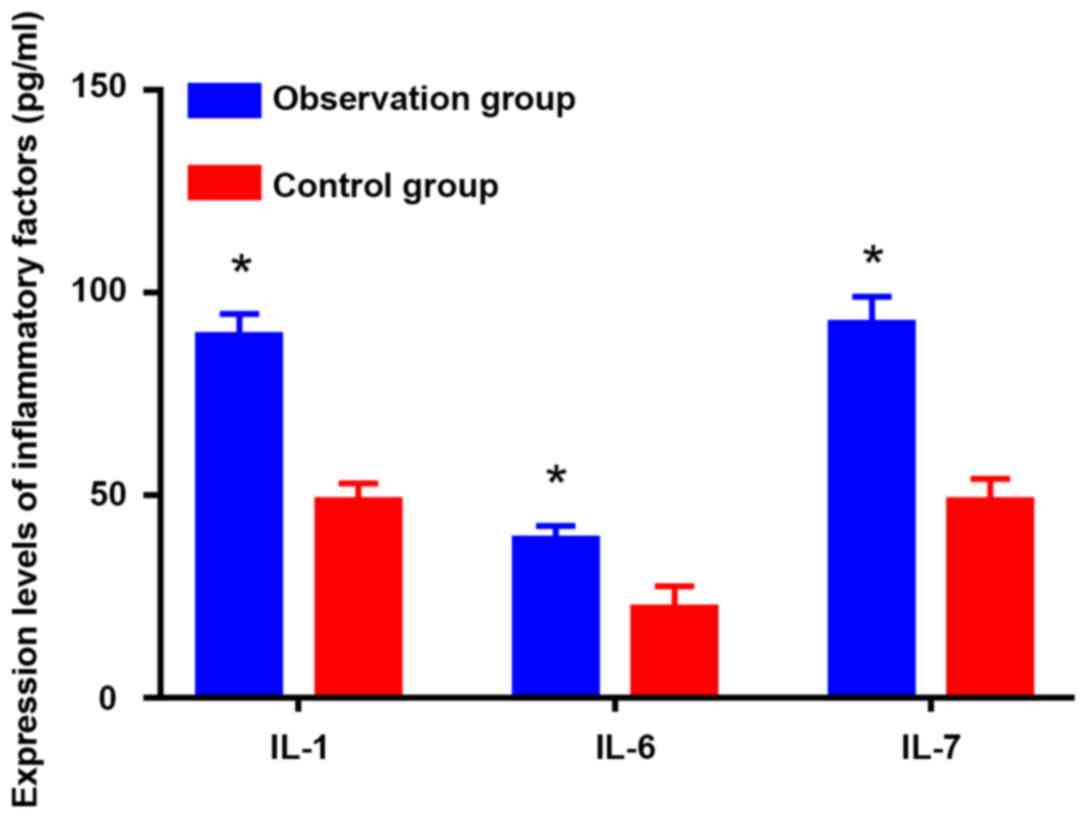
Detection of IL-1, IL-6 and IL-17
expression levels in serum using ELISA
As shown in Fig. 1,
the expression levels of IL-1 (47.45±4.77 pg/ml), IL-6 (29.87±5.21
pg/ml) and IL-17 (52.73.4±5.63 pg/ml) in serum of the observation
group were significantly higher than those of the control group
(84.39±4.88, 43.45±3.89 and 91.33±5.63 pg/ml) (P<0.05).
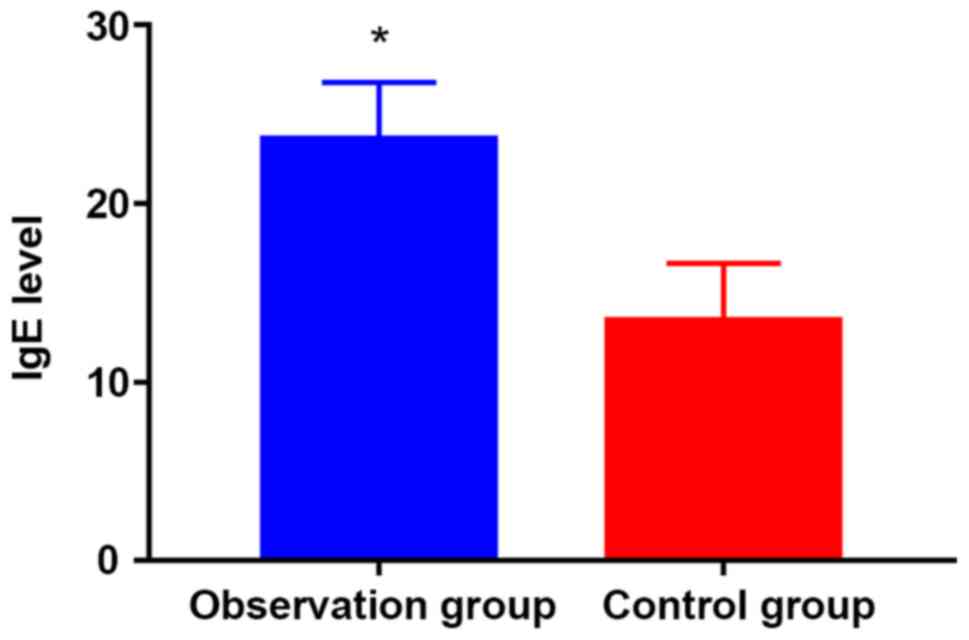
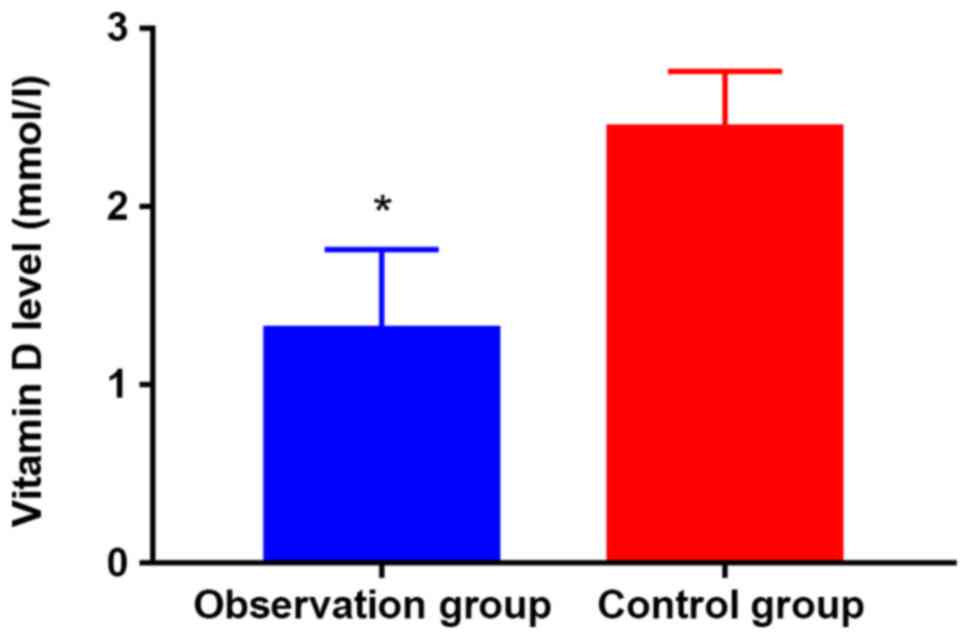
Detection of vitamin D and
immunoglobulin levels using fully-automatic biochemical
analyzer
As shown in Figs. 2
and 3, vitamin D (1.12±0.57 mmol/l)
and immunoglobulin (12.28±3.44 g/l) levels in venous blood serum of
the observation group were remarkably lower than those of the
control group (2.38±0.87 mmol/l, 14.66±4.34 g/l) (P<0.05).
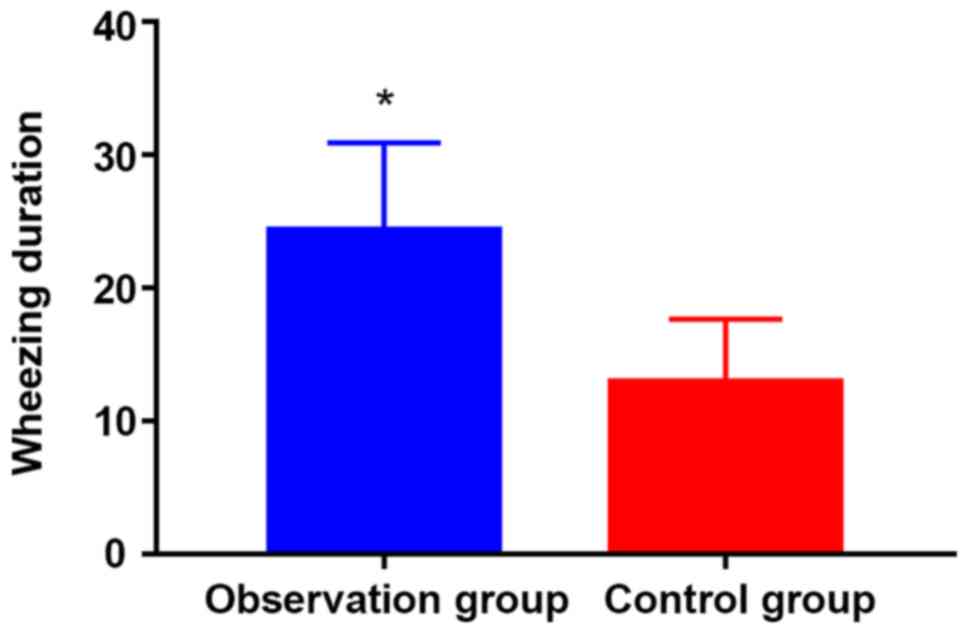
Wheezing duration
The wheezing duration of child patients in the
observation group (23.32±6.39 sec) was evidently longer than that
in the control group (14.87±5.49 sec) (P<0.05; Fig. 4).
Correlation analysis
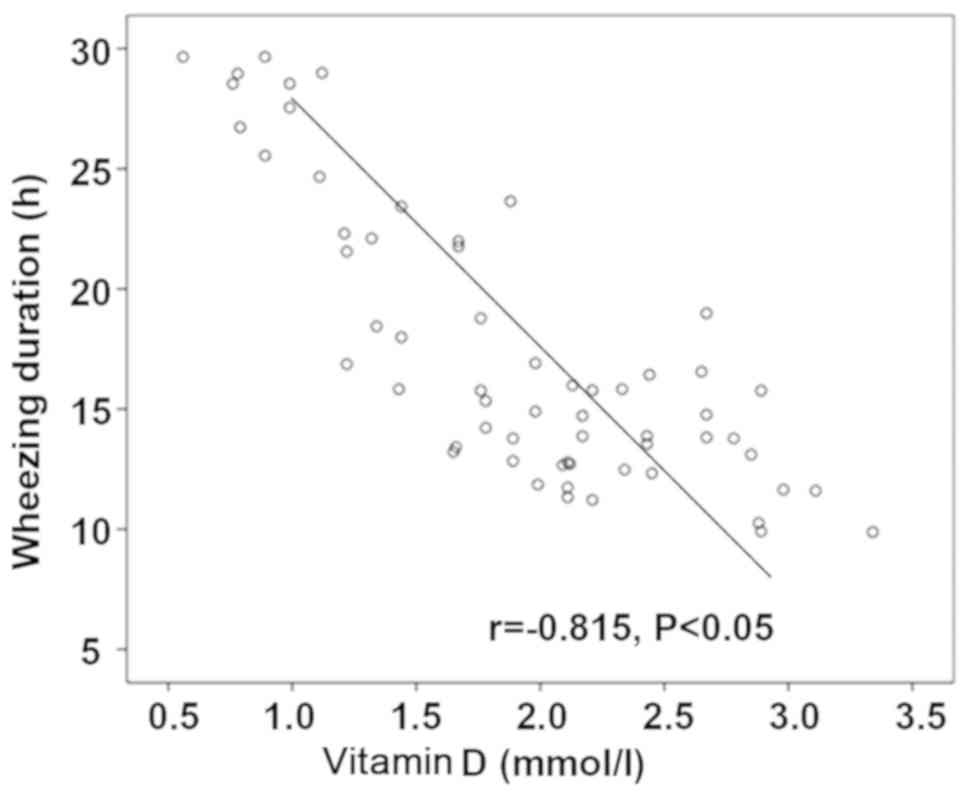
According to calculation, the r value of correlation
analysis between IL-17, IL-1 and IL-6 expression levels and wheeze
duration was 0.875, 0.851 and 0.882, respectively, demonstrating
that inflammatory factors are positively related to wheezing
duration (Figs.
5-7). The r value of correlation analysis between vitamin D and
wheezing duration was -0.815, suggesting that there is a negative
correlation between them (Fig. 8).
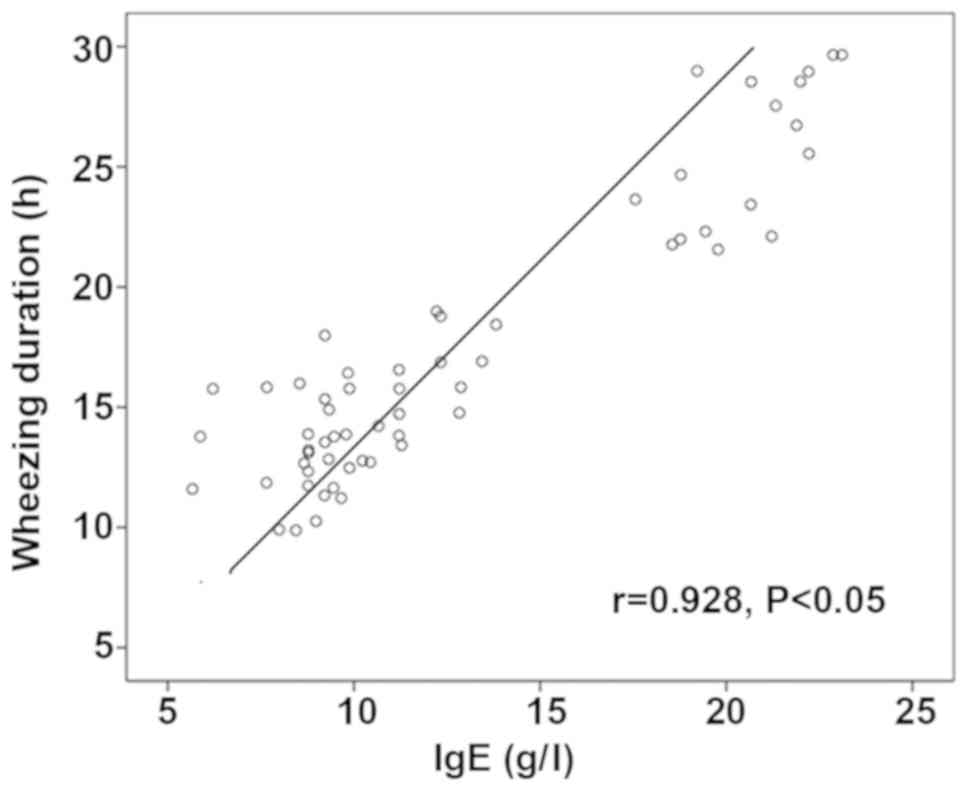
The r value of correlation analysis between immunoglobulin E level
and wheezing duration was 0.928, indicating that there is a
negative correlation between them (Fig.
9).
Discussion
Rickets is a common complication of infantile asthma
in clinical practice, which is characterized by frequent wheezing
attacks and high severity and difficult to control. It has been
found clinically that vitamin D or calcium is able to effectively
relieve wheezing symptoms in asthmatic infants with rickets,
suggesting the close relationship between infantile asthma and
rickets. Moreover, a number of risk factors are associated with the
disease (10,11). As a steroid hormone, vitamin D plays
an important role not only in skeletal diseases such as rickets,
but also in autoimmune diseases, cardiovascular diseases and cancer
(12). Vitamin D exerts an
indispensable role in immune regulation. The study indicates that
the appropriate amount of vitamin D can effectively reduce the
expression of T-helper (Th)-1 and Th2 cells, inhibit cellular
immune-mediated inflammation, and inhibit the expression of
inflammatory factors (13). Vitamin
D can also inhibit the expression and secretion of IL-4 in
bronchoalveolar lavage fluid, so as to inhibit airway inflammation.
Additionally, vitamin D inhibits inflammation by inhibiting IL-10
and transforming growth factor (TGF)-β (14). Furthermore, vitamin D can promote
IL-10 in patients with asthma tolerance induced by steroids
(15,16). During clinical treatment, the acute
attack of asthma and tolerance of asthma to glucocorticoid can be
reduced by vitamin D (17-19).
Given that there is a close relationship between vitamin D and
rickets, vitamin D may be a risk factor for infantile asthma with
rickets. Pro-inflammatory factors mainly secreted by Th17,
including IL-1, IL-6 and IL-17, were responsible for immune
regulation during asthma attack (20).
It has been proven that IL-1, IL-6 and IL-17 can not
only aggravate acute inflammation during asthma attack, but also
induce multiple immune cells to secrete inflammatory cytokine IL-6,
and increase airway mucus secretion, so as to play important roles
in airway remodeling (21).
Therefore, IL-1, IL-6 and IL-17 are of significance during all
aspects of asthma attack. Immunoglobulin E is considered to be one
of the important substances that trigger the immune response of
asthma, and it is a key factor in the pathogenesis of asthma.
Immunoglobulin E binds to a large number of immune cells, causing
the body to be in a higher state of sensitization (22,23).
When the body is stimulated by allergen, inflammation can occur,
the body's physiological function is disturbed, and asthma attack
is induced (24,25). The study indicates that the level of
immunoglobulin E in serum of asthmatic children is significantly
higher than that of normal children, and the level of
immunoglobulin E is closely related to the severity of asthma
(23). Therefore, immunoglobulin E
is also considered as one of the risk factors. The results of this
study displayed that IL-1, IL-6, IL-17 and immunoglobulin E levels
in serum of infantile asthma with rickets were significantly higher
than those in simple asthma children, and the vitamin D level was
remarkably lower than that in children with simple asthma. The
results of correlation analysis proved that inflammatory factors
and immunoglobulin E were positively related to infantile asthma
with rickets, but the vitamin D level was negatively associated
with infantile asthma with rickets. Therefore, the high expression
of inflammatory factors and immunoglobulin E and low expression of
vitamin D are considered as risk factors of infantile asthma with
rickets.
However, asthmatic infants with low Vitamin D, but
not rickets may be an interesting control to be explored.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AA was involved in writing the manuscript. AA and BY
analyzed general data of patients and collected the specimens. PX
performed ELISA. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
First Affiliated Hospital of Xinjiang Medical University (Urumqi,
China) and informed consents were signed by the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Menakongka A and Suthiphongchai T:
Involvement of PI3K and ERK1/2 pathways in hepatocyte growth
factor-induced cholangiocarcinoma cell invasion. World J
Gastroenterol. 16:713–722. 2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Masoli M, Fabian D, Holt S and Beasley R:
Global Initiative for Asthma (GINA) Program. The global burden of
asthma: Executive summary of the GINA Dissemination Committee
report. Allergy. 59:469–478. 2004.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chuansheng L, Chunwang L and Chenglu ZH:
Determination of the serum calcium, phosphorus, alkaline
phosphatase and immunoglobulin level in the asthmatic infants and
young children with rickets. J Clin Pedia. 21:299–300. 2003.(In
Chinese).
|
|
4
|
Hansdottir S, Monick MM, Lovan N, Powers
L, Gerke A and Hunninghake GW: Vitamin D decreases respiratory
syncytial virus induction of NF-kappaB-linked chemokines and
cytokines in airway epithelium while maintaining the antiviral
state. J Immunol. 184:965–974. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Folkerts G and Nijkamp FP: Virus-induced
airway hyperresponsiveness. Role of inflammatory cells and
mediators. Am J Respir Crit Care Med. 151:1666–1673; discussion
1673-1674. 1995.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Huijuan M: Analysis of related factors of
recurrent respiratory tract infection in children. Chin Hosl Infect
Sci. 22:951–952. 2012.
|
|
7
|
Spedding S, Vanlint S, Morris H and Scragg
R: Does vitamin D sufficiency equate to a single serum
25-hydroxyvitamin D level or are different levels required for
non-skeletal diseases? Nutrients. 5:5127–5139. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Asthma Workgroup, Chinese Thoracic
Society, Chinese Societ of General Practitioners. Chinese guideline
for the prevention and management of bronchial asthma (Primary
Health Care Version). J Thorac Dis. 5:667–677. 2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Weiping W: Pediatrics. People's Health
Publishing House, Beijing, p107, 2013 (In Chinese).
|
|
10
|
Trochoutsou AI, Kloukina V, Samitas K and
Xanthou G: Vitamin-D in the immune system: Genomic and non-genomic
actions. Mini Rev Med Chem. 15:953–963. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hewison M: Vitamin D and immune function:
An overview. Proc Nutr Soc. 71:50–61. 2012.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Cava RC and Javier AN: Vitamin D
deficiency. N Engl J Med 357: 1981, author reply 1981-1982,
2007.
|
|
13
|
Urry Z, Xystrakis E, Richards DF, McDonald
J, Sattar Z, Cousins DJ, Corrigan CJ, Hickman E, Brown Z and
Hawrylowicz CM: Ligation of TLR9 induced on human IL-10-secreting
Tregs by 1α,25-dihydroxyvitamin D3 abrogates regulatory function. J
Clin Invest. 119:387–398. 2009.PubMed/NCBI View
Article : Google Scholar
|
|
14
|
Robinson DS: Regulatory T cells and
asthma. Clin Exp Allergy. 39:1314–1323. 2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Xystrakis E, Kusumakar S, Boswell S, Peek
E, Urry Z, Richards DF, Adikibi T, Pridgeon C, Dallman M, Loke TK,
et al: Reversing the defective induction of IL-10-secreting
regulatory T cells in glucocorticoid-resistant asthma patients. J
Clin Invest. 116:146–155. 2006.PubMed/NCBI View
Article : Google Scholar
|
|
16
|
Frieri M: The role of vitamin D in
asthmatic children. Curr Allergy Asthma Rep. 11:1–3.
2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lötvall J, Langley S and Woodcock A:
Inhaled steroid/long-acting beta 2 agonist combination products
provide 24 hours improvement in lung function in adult asthmatic
patients. Respir Res. 7(110)2006.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Quirk SK, Rainwater E, Shure AK and
Agrawal DK: Vitamin D in atopic dermatitis, chronic urticaria and
allergic contact dermatitis. Expert Rev Clin Immunol. 12:839–847.
2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Brehm JM, Celedón JC, Soto-Quiros ME,
Avila L, Hunninghake GM, Forno E, Laskey D, Sylvia JS, Hollis BW,
Weiss ST, et al: Serum vitamin D levels and markers of severity of
childhood asthma in Costa Rica. Am J Respir Crit Care Med.
179:765–771. 2009.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Miossec P and Kolls JK: Targeting IL-17
and TH17 cells in chronic inflammation. Nat Rev Drug Discov.
11:763–776. 2012.PubMed/NCBI View
Article : Google Scholar
|
|
21
|
Charrad R, Berraïes A, Hamdi B, Ammar J,
Hamzaoui K and Hamzaoui A: Anti-inflammatory activity of IL-37 in
asthmatic children: Correlation with inflammatory cytokines TNF-α,
IL-β, IL-6 and IL-17A. Immunobiology. 221:182–187. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Yang J, Wang HX, Zhang YJ, Yang YH, Lu ML,
Zhang J, Li ST, Zhang SP and Li G: Astragaloside IV attenuates
inflammatory cytokines by inhibiting TLR4/NF-кB signaling pathway
in isoproterenol-induced myocardial hypertrophy. J Ethnopharmacol.
150:1062–1070. 2013.PubMed/NCBI
|
|
23
|
Arima M and Fukuda T: Prostaglandin
D2 and T(H)2 inflammation in the pathogenesis of
bronchial asthma. Korean J Intern Med. 26:8–18. 2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Yuan Y, Yang B, Ye Z, Zhang M, Yang X, Xin
C, Lin M and Huang P: Sceptridium ternatum extract exerts
antiasthmatic effects by regulating Th1/Th2 balance and the
expression levels of leukotriene receptors in a mouse asthma model.
J Ethnopharmacol. 149:701–706. 2013.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Hoskins G, McCowan C, Neville RG, Thomas
GE, Smith B and Silverman S: Risk factors and costs associated with
an asthma attack. Thorax. 55:19–24. 2000.PubMed/NCBI View Article : Google Scholar
|