Introduction
Post-arthroscopic osteonecrosis is a rare disease
that may progress to end-stage osteoarthritis, which was first
reported by Brahme et al (1)
in 1991. In addition, it has been reported as ‘post-meniscectomy’,
‘post-arthroscopy’ or ‘osteonecrosis in the post-operative knee’ in
later years (2-5).
Santori et al (6) reported
only two cases of osteonecrosis among >2,000 patients who
underwent knee arthroscopy (0.2%). Pruès-Latour et al
(7) reported 9 cases in 585 patients
who underwent arthroscopic meniscectomies and were >50 years old
(1.5%). Post-arthroscopic osteonecrosis is more likely to occur in
elderly patients, without any sex bias. Nowadays, it is a rare
condition and its morbidity remains elusive. However, compared with
the large number of arthroscopic surgery performed worldwide every
year, the number of reported cases of post-arthroscopic
osteonecrosis is low.
The etiology of post-arthroscopic osteonecrosis
remains elusive. Certain studies have suggested that it may be due
to the effect of the heat generated by radiofrequency on the
subchondral bone (8). Other studies
have hypothesized that the mechanical shavers used may cause damage
to the cartilage (9). Furthermore,
certain studies have reported the lesion as a subchondral fracture
(10). Another theory is that the
increased biomechanical load in the medial compartment following
medial meniscus resection may be the major reason (7).
The present study describes a case of
post-arthroscopic knee osteonecrosis and delineation identified
during surgery. In addition, a literature review was performed and
the latest progress in the diagnosis and treatment of
post-arthroscopic osteonecrosis was summarized. Finally, the
present study aimed to provide additional details regarding the
prevention and treatment of this disease.
Case report
An 81-year-old man suffered from left knee pain
without any history of trauma for 3 months. The pain was aggravated
by walking and the range of motion was indicated to be limited. The
patient had a history of Parkinson's disease for 6 years and a
history of hypertension and diabetes for >10 years. There was no
history of sports injury, alcohol abuse or intra-articular steroid
injections. The patient went to see the doctor at his local
hospital in February 2018. His body mass index was ~27
kg/m2. Physical examination revealed no ligamentous
instability. The tenderness was on the medial joint line on
palpation and McMurray's test was positive. Conservative treatment,
including non-steroidal anti-inflammatory drugs (NSAIDs) and a
topical patch, was initiated for 1 month; however, this was
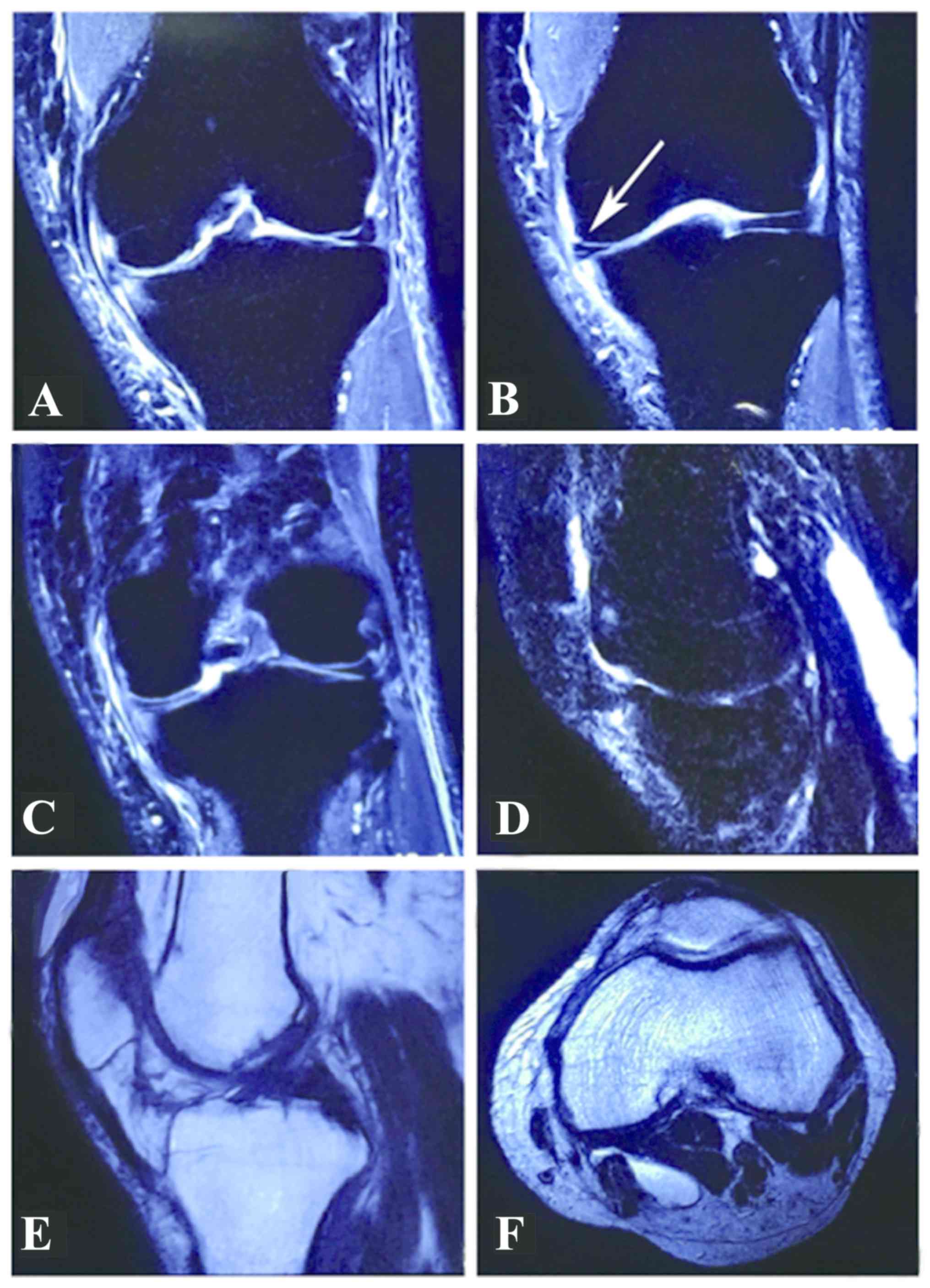
ineffective. MRI was performed at the local hospital and revealed
evidence of a medial meniscus tear with unremarkable articular
chondral damage (Fig. 1).
Arthroscopic surgery was performed under spinal anesthesia in March
2018. A tear in the posterior horn of the medial meniscus was
identified. Subsequently, arthroscopic partial medial meniscectomy
was performed using basket forceps and a shaver (Smith &
Nephew) without any cartilage intervention. No radiofrequency or
laser was used. The surgery lasted for ~40 min. NASIDs were
prescribed for 7 days postoperatively. He felt that the pain was
relieved, therefore NSAIDS was not taken after 7 days. Although
some of the pain that could not be relieved even after NSAIDs
administration pre-operatively, the patient felt that the operation
improved this condition initially. However, the pain in the left
knee aggravated 1 month after arthroscopic surgery, with worsening
of the symptoms as the activity level and weight-bearing increased.
There was also swelling in the whole knee, which was different from
the knee prior to the first surgery. Prior to the operation, the
knee did not exhibit any swelling. The patient stated that he did
not receive any steroid treatment and there was no injury after the
primary surgery. Conservative treatment, including non-steroidal
anti-inflammatory drugs (NSAIDs) and physiotherapy, as well as ice
compressions, were administered for 2 months; however, this was
ineffective.
Subsequently, the patient came to our hospital for
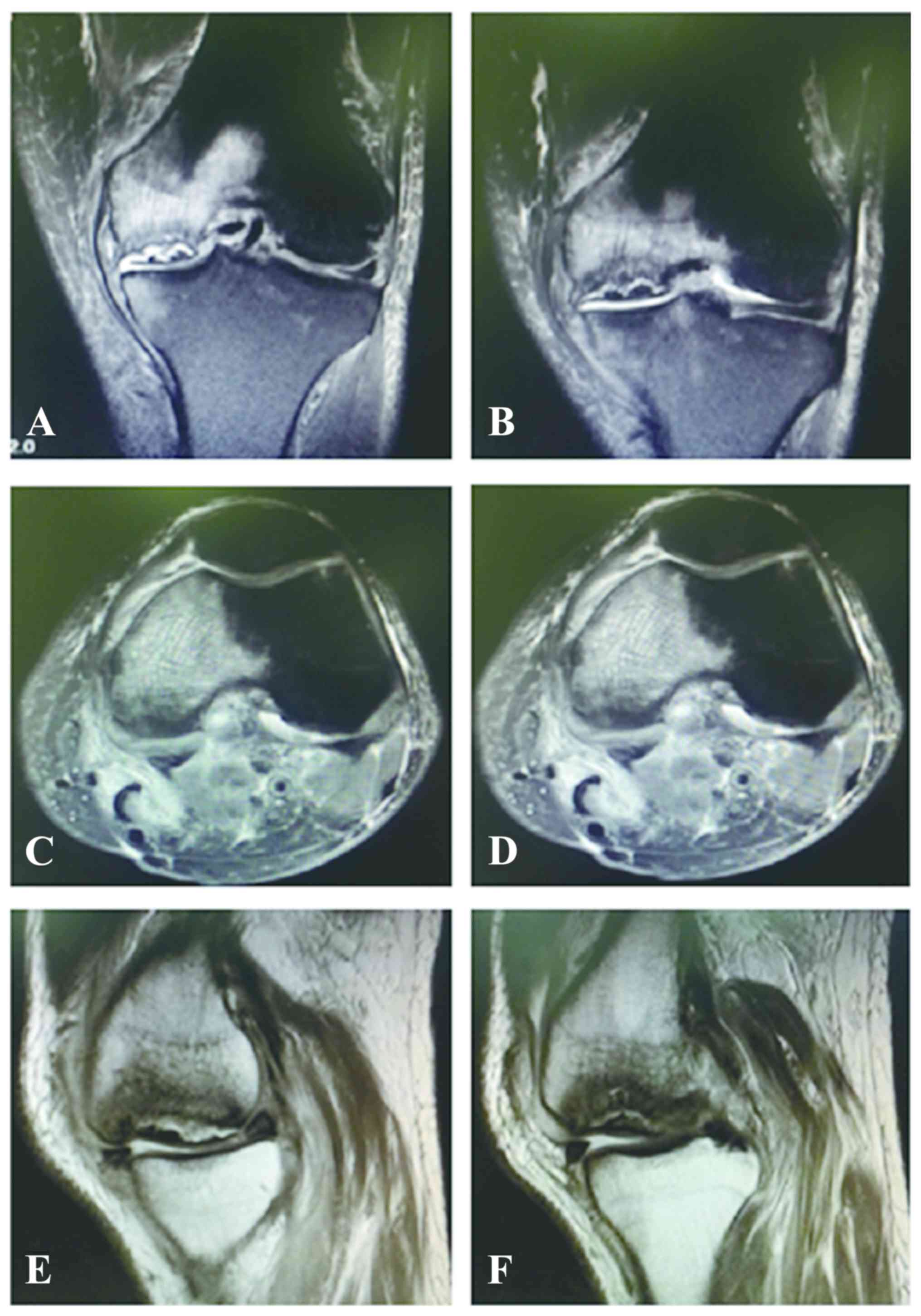
further treatment in June 2018. The pre-operative MRI and X-ray
were re-evaluated. The X-ray revealed collapse in the femoral
medial condyle and narrowing of the joint space (Fig. 2). The pre-operative MRI revealed a
large area of bone marrow edema (BME) in the medial femoral condyle
with cartilage delamination and subchondral flattening. Recurrence
of meniscal tear was not observed (Fig.
3).
Considering the patient was elderly (81 years) and
the necrotic bone lesion area on MRI was large, treatments such as
high tibial osteotomy (HTO) and arthroscopic core decompression and
osteochondral autograft were not ideal for this patient. Therefore,
it was decided to perform total knee arthroplasty (TKA). In
addition, a metal prosthesis was prepared in case the bone defect
would have been identified as too large during the surgery.
Surgical procedure
The patient received combined spinal and epidural
anesthesia. Subsequently, the patient took a supine position and a
tourniquet was fixed on the left thigh. The medial parapatellar
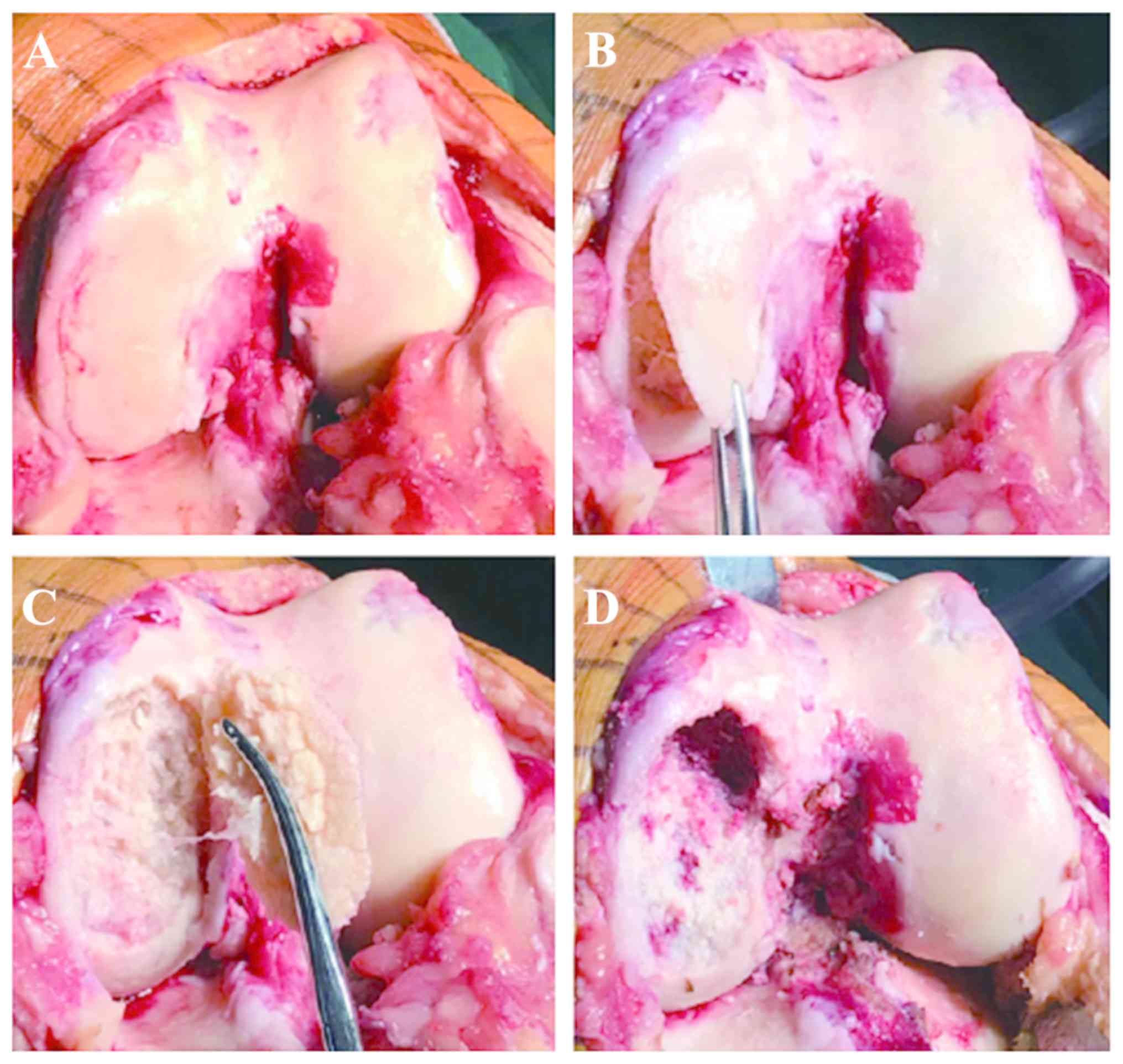
approach was taken. During the surgery, it was identified that the
cartilage of the left femur, tibia and patella was severely defaced
and worn. The cartilage of the medial femur condyle was separated
from the subchondral bone and had become soft and delaminated. The
subchondral bone of the medial femoral condyle was found to be
collapsed and necrotized. The size of the area of the lesion was
~4x2 cm (Fig. 4). This was
consistent with the pre-operative MRI findings. In addition, the
anterior cruciate ligament was degenerated. Subsequently, a
tourniquet with a pressure of 250 mmHg was applied. All the lesions
were debrided. Subsequently, the distal femoral and proximal tibia
were correctly osteotomized and the irrigation pump was used. Then,
the osteotomized cancellous bone was cut into a small bone mass and
filled into the bone defect area of the femoral medial condyle
without using the metal prosthesis pad. Finally, a
posterior-stabilized knee prosthesis was implanted. The tourniquet
time was 50 min. The entire surgery lasted ~85 min.
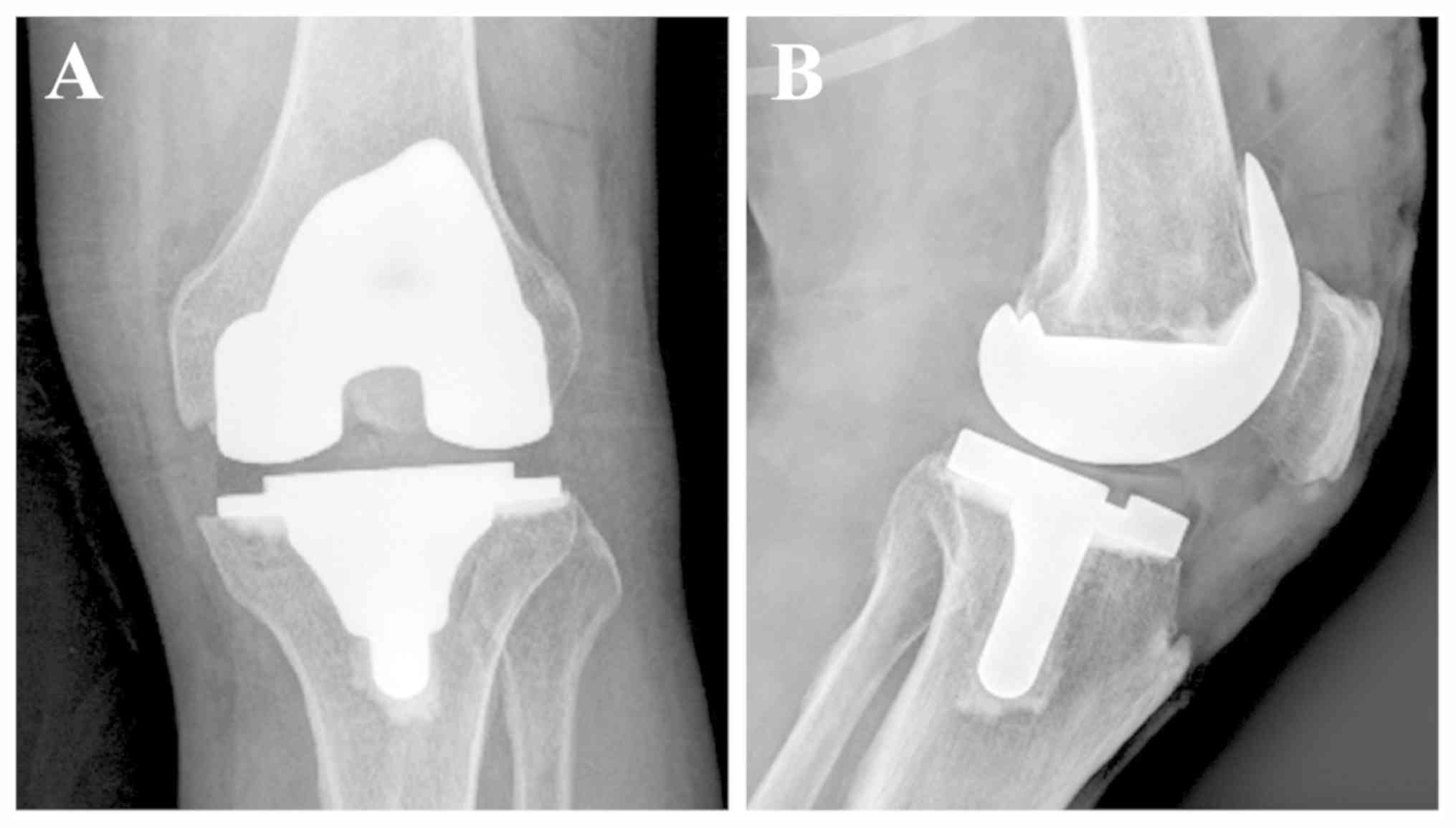
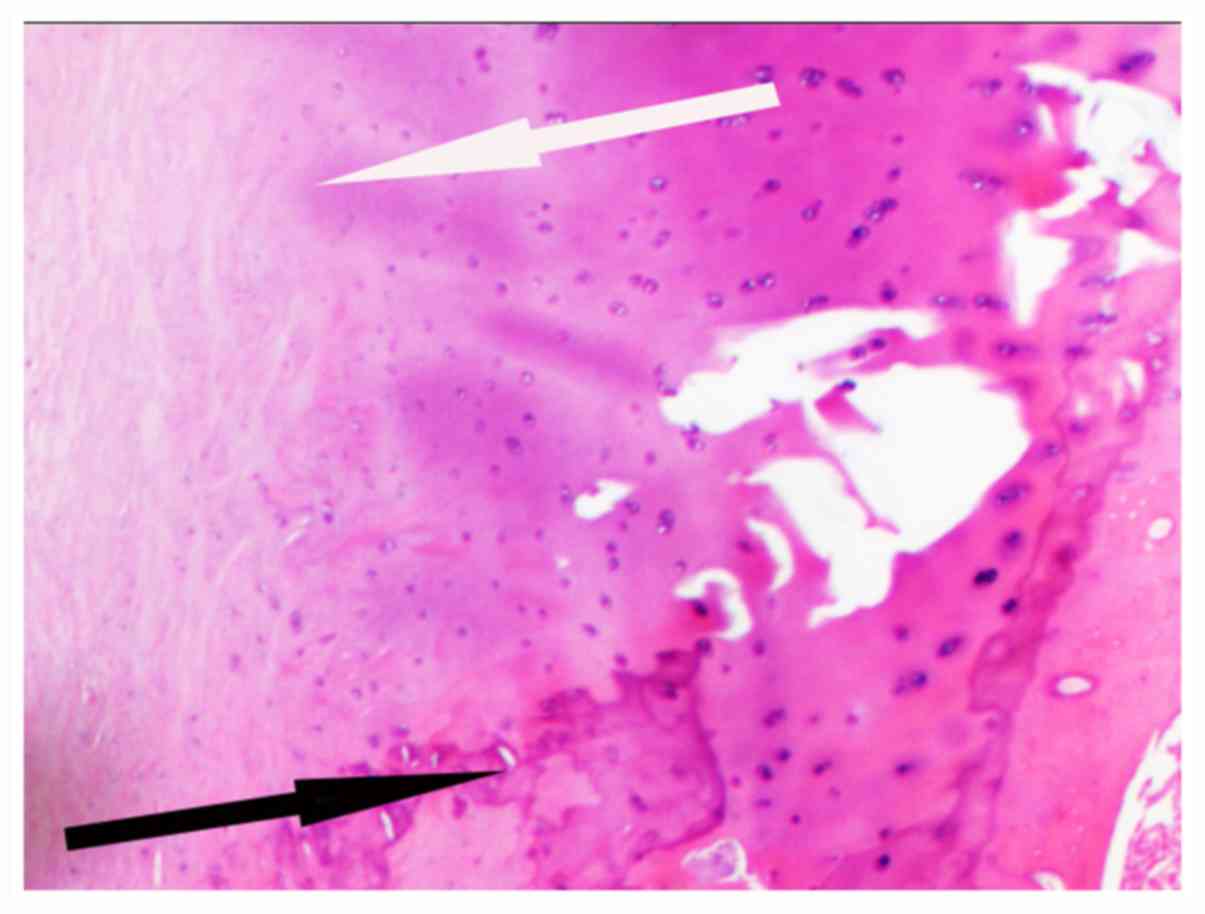
After the surgery, an X-ray revealed that the
position of the prosthesis was good (Fig. 5). Histopathological analysis revealed
osteonecrosis of the cartilage (Fig.
6). The patient received routine analgesia and anti-coagulant
therapy post-operatively and was discharged from hospital 6 days
post-operatively. At that time, the patient was able to walk
without crutches. The Knee Society Knee Score improved from 44
points pre-operatively to 90 points at the 1-year follow-up
post-operatively and the Knee Society Functional Score (11) increased from 35 to 90 points.
Similarly, the Oxford Knee Score (OKS; patient-reported outcome
measures) (12,13) was 16 at the 1-year follow-up. The OKS
is a 12-item questionnaire, which evaluates the pain and function
of the knee. The patient is currently pain-free in his left knee
and satisfied with the knee function.
Systematic review
A review of relevant articles published between
January 1995 and January 2019 was performed to compare the present
results with those of previously published case reports in the
PubMed, Web of Science and Cochrane Library databases. The keywords
included ‘arthroscopy’, ‘osteonecrosis’, ‘knee’, ‘meniscal tear’,
‘meniscal tears’, ‘meniscectomy’, ‘ACL reconstruction’,
‘radiofrequency’ and ‘chondroplasty’ and nine reports matching the
criteria were found (2,3,6,8,10,14-17).
These reports included most of the existing studies between January
1995 and January 2019. Two authors (ZZ and KC) reviewed each paper
separately to reach a consensus regarding data abstraction and
article inclusion. Subsequently, the variables in the literature
were compared with those of the present case. Table I lists the basic characteristics of
the included studies.
 | Table IFicat classification. |
Table I
Ficat classification.
| Stage | Description |
|---|
| 0 | This stage is
preclinical and pre-radiographic |
| I | No radiographic
evidence of knee osteonecrosis. The bone presents with no sclerosis
and maintained curvature. |
| II | Signs of mottled
sclerosis but the normal curvature of the bone remains intact. |
| III | The presence of a
crescent sign is indicative of subchondral fracture, which defines
this stage. |
| IV | Collapse of the
subchondral bone. |
Discussion
Arthroscopy is a useful method to treat various
types of knee disorder (18).
Countless arthroscopic surgeries are performed worldwide every
year. Post-arthroscopic osteonecrosis is a rare complication of
arthroscopy. It has been reported in patients who received
arthroscopic knee surgery, particularly in patients undergoing
meniscectomy. However, it may also occur in association with other
types of arthroscopic surgery. Furthermore, a previous study has
suggested that it may be a rare complication of the anterior
cruciate ligament reconstruction (14). The most common location of necrosis
is the medial femoral condyle, followed by the lateral femoral
condyle, whereas the lateral tibia, the medial tibial plateau and
the patella are rarely affected.
The mechanism of post-arthroscopic osteonecrosis
remains elusive. It has been hypothesized that alteration in the
load distribution in the knee joint may be a cause of
osteonecrosis. Meniscalplasty under arthroscopy has been
demonstrated to be an effective method to relieve knee pain and
improve the daily life of affected patients (19); however, the change in the knee
biomechanics after meniscectomy may lead to higher tibiofemoral
contact pressure. In addition, tears of the medial meniscal root
are considered to increase the peak pressure of the femoral condyle
more than that in the horizontal tears of the posterior horn. Under
these conditions, it may lead to incomplete fracture of the
cartilage and subchondral bone (10,15),
followed by leakage of synovial fluid and subchondral collapse.
These pathological changes may result in osteonecrosis of the knee.
In certain circumstances, if there is pre-existing cartilage damage
prior to arthroscopic surgery, the arthroscopic fluid may
infiltrate into the pathologic area, which may aggravate the
subchondral edema (7). Furthermore,
manipulation during the arthroscopic surgery, including the use of
laser or radiofrequency, that generates thermal energy, has been
reported to potentially increase the risks of osteonecrosis
(20,21). However, this remains to be further
validated.
In the present case, laser or radiofrequency
treatment were not used. There are several possible reasons for the
osteonecrosis observed in the present case. First, elderly
individuals have a narrow medial joint space. Excessive
intra-operative manipulation to expose the posterior horn of the
medial meniscus may cause damage to the chondral lesions of the
femoral condyle. Furthermore, excessive meniscal resection,
particularly of the posterior horn of the meniscus, changes the
mechanical distribution in the knee. In addition, osteoporosis,
early post-operative weight-bearing and functional rehabilitation
exercises increase the tibiofemoral pressure, which may accelerate
the development of post-arthroscopic osteonecrosis. MRI is the most
important tool for the diagnosis of post-arthroscopic osteonecrosis
(22). In early necrotic stages, MRI
T2-weighted imaging reveals a heterogenous, non-specific, large
area of BME in the meniscectomy compartment. Similarly, close to
the BME, a line of low signal may be observed around the necrotic
area. In the later stages of post-arthroscopic osteonecrosis, the
bone sequestration exhibits a high signal rim accompanied by
flattening of the femoral condyle.
Even though BME may be present in the post-operative
MRI, it is absent in a pre-operative MRI in the early stages. The
time interval (‘window period’) between the onset of osteonecrosis
symptoms and a positive MRI finding should be addressed. The exact
time interval remains to be determined. The ‘window period’ was
defined based on an animal study previously performed by Nakamura
et al (23), in which a
canine model of femoral head osteonecrosis was established to
demonstrate that ≥4 weeks was required to obtain positive MRI
findings post-operatively. Johnson et al (2) and Türker et al (24) also regarded ≥6 weeks after symptom
onset as the ‘window period’ to exclude the early stage of
spontaneous osteonecrosis of the knee (SPONK). Therefore, ≥6 weeks
was also chosen for the present study. This may be the differential
diagnosis point between the early stage of the spontaneous
osteonecrosis and post-arthoscopic osteonecrosis.
If a patient complains of persistently worsening
knee pain following arthroscopy, a diagnosis of post-arthroscopic
osteonecrosis should be considered. Post-arthroscopy osteonecrosis
should be distinguished from secondary osteonecrosis, SPONK and
recurrent meniscal tear (25,26).
Secondary osteonecrosis has a multifactorial etiology, including
trauma, chemotherapy, alcohol abuse and corticosteroid treatment.
The patients are typically <45 years old and occurrence is more
common in females than in males (26). Most cases of secondary osteonecrosis
are bilateral and secondary osteonecrosis may also involve other
joints (26). Spontaneous
osteonecrosis is idiopathic and it may be caused by chronic
mechanical stress or a weight-bearing articular surface subjected
to altered stresses as the result of subchondral fracture, or the
progression of osteoarthritis. The patients are usually >50
years old and the female-to-male ratio is ~3:1. Spontaneous
osteonecrosis is mainly unilateral and without the involvement of
other joints (25).
Post-arthroscopic osteonecrosis is associated with subchondral
collapse with altered knee mechanics. Patients of any age may be
affected and it occurs without sex bias (26,27). For
secondary and spontaneous osteonecrosis, bone edema may be observed
soon after the onset of symptoms. On the other hand, for recurrent
meniscus tear, bone edema and epicondyle necrosis are not
identified (26).
The treatment strategy should be based on the
disease stage at which osteonecrosis is diagnosed. The Ficat
classification was first applied to classify osteonecrosis of the
femoral head. This classification system describes the different
degrees of osteonecrosis (28). It
has also been widely used to describe osteonecrosis of the knee
(27,29,30).
According to this system, osteonecrosis is divided into five
stages. A description of the different stages is provided in
Table II. The outcomes of
post-arthroscopic osteonecrosis have a limited association with the
size of the lesion, since even small bone marrow changes observed
on MRI may lead to osteonecrosis.
 | Table IIPrevious case reports of knee
osteonecrosis after arthroscopic surgery. |
Table II
Previous case reports of knee
osteonecrosis after arthroscopic surgery.
| Author (year) | Cases (n) | Patient age (years),
sex | Primary
operation | ON location
involved | Treatment | (Refs.) |
|---|
| Santori (1995) | 2 | 21, M | PMM | MFC | Non-weight
bearing | (6) |
| | | 47, F | PMM | MFC | Non-weight
bearing | |
| Lansdown
(2015) | 5 | 30, M | ACL
reconstruction | MFC, LFC
patella | Core decompression
with iliac crest bone grafting for 1 patient; arthroscopic
debridement for the other cases. | (14) |
| | | 23, M | ACL
reconstruction | MFC, LFC | | |
| | | 40, M | ACL
reconstruction+meniscal debridement | MFC, LFC | | |
| | | 46, F | ACL
reconstruction+PMM | MFC, LFC | Removal of ACL in 2
patients. | |
| | | 27, F | ACL
reconstruction+lateral meniscal repair | LFC | TKA 4 years after
ACL Reconstruction for 1 patient. | |
| Garino (1995) | 6 | 44, F | PMM | MFC, MTP | Local autogenous
cancellous bone grafting. | (8) |
| | | 44, M | PMM | LFC, LTP | Observation and
symptomatic treatment | |
| | | 30, F | MFC and the
majority of the patella | Mild femoral
condyle and the majority of the patella | Patellectomy | |
| | | 30, F | Bilateral
laser-assisted patellar chondroplasty | Bilateral
Chondromalacia patellae | Conservative care
valid, patellectomy is under consideration | |
| | | 50, F | Laser chondroplasty
of LFC | Partial thickness
chondral fracture | Treated
symptomatically | |
| Johnson (2000) | 7 | 79, F | PMM, CP | MFC | TKA | (2) |
| | | 58, M | PMM, CP | MFC+CM | MFC, MTP valgus
HTO, CPMF | |
| | | 75, F | PLM | MFC | TKA, valgus
HTO | |
| | | 41, M | PMM | LFC | Core
decompression | |
| | | 54, M | CP, PLM | MFC+patella | Conservative
care | |
| | | 53, F | CP, PMM | MTP | Lost to
follow-up | |
| | | 62, F | PMM, CP | MFC | TKA | |
| DeFalco (2003) | 1 | 48, M | PMM | MFC | Arthroscopy with
drilling of the lesion | (16) |
| MacDessi
(2008) | 8 | 67 | PMM | MFC | TKA | (10) |
| | | 56 |
PMM+chondroplasty | MFC | TKA | |
| | | 78 | PMM+PLM | MFC | TKA | |
| | | 53 | PMM | MFC | TKA | |
| | | 66 | PMM | MFC | TKA | |
| | | 69 |
PMM+chondroplasty | MFC | TKA | |
| | | 64 | PMM | MTP | TKA | |
| | | 54 |
PMM+chondroplasty | MFC | TKA | |
| Son (2013) | 1 | 50, M | PMM | MFC | UKA | (17) |
| Faletti (2002) | 1 | 66, M | Meniscal
recontouring | MFC | Shock-wave
therapy | (3) |
| Bonutti (2006) | 19 | Average 69 years; F
(n=5) M (n-14) | 5 Arthroscopy with
associated laser treatment; 1 underwent a laser-assisted
arthroscopy, 10 arthroscopy with associated radiofrequency
treatment, 3 treated with a shaver and adjunctive microfracture
surgery. | 13 knees (68%)
presented with distal femoral involvement, 2 knees (11%) had
involvement of the proximal aspect of the tibia and 4 knees (21%)
presented with both femoral and tibial involvement. The medial
femoral condyle was involved in 14 knees; the lateral femoral
condyle in 3 knees; the medial tibial plateau in 5 knees; and the
lateral tibial plateau in 1 knee | UKA and TKA | (20) |
Conservative treatment is used for patients whose
lesions are still at the pre-collapse early stages (29). This treatment includes avoiding full
weight-bearing, NSAIDs, bisphosphonates and hyperbaric oxygen
treatment. Partial weight-bearing with crutches and taking NSAIDs
for 4-8 weeks are usually recommended. Early surgical intervention
is not recommended, since it may accelerate the damage to the
joint. However, the success rate of conservative treatment is not
satisfactory. Pape et al (27) reported 47 cases of post-arthroscopic
osteonecrosis treated by conservative methods; however, only 3
cases exhibited improvement. Surgical treatment is reserved for
patients with failed conservative treatment and late-stage lesions
at the time of diagnosis (29).
For patients with Ficat stage I-II, there is
pre-existing chondral bone collapse. The surgical methods include
arthroscopic debridement, microfracture, bone grafting, core
decompression, antegrade drilling, retrograde drilling and high
tibial osteotomy (29). Arthroscopic
debridement does not change the course of the disease. It is used
only in patients who have mechanical symptoms due to unsteady
chondral fragments or loose bodies. Microfractures or retrograde
drilling are performed to stimulate revascularization within the
lesion. However, this may damage the intact articular surface and
it is not easy to locate the lesion accurately. Antegrade drilling
or core decompression is another treatment method. It is regarded
to be a better option than microfractures or retrograde drilling.
Jacobs et al (31) was the
first to report core decompression in stage-I and -II SPONK. They
reported that seven cases of stage I and II with mild femorotibial
alignment had good results. Bone grafting is beneficial in patients
who have subchondral collapse and require restoration of the
cartilage surface (32,33). After decompression is finished, bone
grafting may be performed. Autogenic, allogenic cancellous bone or
demineralized bone matrix are optional. HTO is considered for
young, active individuals with early-stage osteonecrosis. Since
this is a joint-preserving technique, the weight-bearing axis may
be transferred laterally so that the medial condyle is less
affected. For patients with Ficat stage III-IV, since irreversible
destruction occurred in the subchondral bone and articular
cartilage and the lesion area is large, unicompartment knee
arthroplasty (UKA) and TKA may be considered (26).
In the present case, the medial parapatellar
approach was utilized. It would have been convenient to select UKA
or TKA based on the range and depth of bone necrosis and the
situation of anterior cruciate ligament during the surgery. The
anterior cruciate ligament and the lateral femoral condyle were
degenerated. In addition, the necrotic area of the medial femoral
condyle was almost 8 cm2 and the bone involvement was
extended. If UKA had been chosen, the prosthesis coverage at the
lesion would have been insufficient, which may have led to bone
collapse around the prosthesis and prosthesis loosening, so TKA was
the most viable option. In the present study, the visual
osteonecrosis images and the findings during surgery were presented
to learn more about the disease intuitively and the treatment
procedure was illustrated. All of these are rarely presented in
other case reports.
It is well-known that TKA is a common surgery option
for patients with end-stage osteoarthritis; however, certain
clinicians are concerned about its application in post-arthroscopic
osteonecrosis due to poor bone quality.
To date, only few studies have reported on the
long-term follow-up of arthroplasty for patients with
post-arthroscopy osteonecrosis. Only one case report was identified
in the literature search that described the follow-up outcome. In
this study, Bonutti et al (20) reported 19 cases of post-arthroscopic
necrosis treated by UKA (4 cases) or TKA (15 cases), and the
midterm results with a mean follow-up of 62 months (range, 24-133
months). In their study, 95% of the patients had a Knee Society
objective score of >80 points and the mean Knee Society
objective score was 92 points. The follow-up period in the present
case was just 1 year and the final outcome was good, which was
consistent with the study by Bonutti et al (20). However, a longer follow-up period is
required.
In summary, the treatment strategies should be
dependent on the individual patient, including the necrosis stage
and function of the other areas of the joint. Table I lists the features of previous
studies on post-arthroscopic necrosis.
In conclusion, post-arthroscopic osteonecrosis is a
rare event following arthroscopic surgery. For elderly patients,
arthroscopy manipulation should be gentler and the amount of
meniscectomy should be reduced. If the patient complains of
persistent and worsening pain after arthroscopy, post-arthroscopic
osteonecrosis should be suspected, particularly in elderly
osteoporotic patients with meniscal tears or chondral lesions.
Early diagnosis and treatment are important in the management of
this condition. The prognosis of post-arthroscopic osteonecrosis is
mostly associated with the timing of the diagnosis but not the size
of the lesions.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
The datasets used during the present study are
available from the corresponding author on reasonable request.
Authors' contributions
ZZ and KC contributed equally to the study. ZZ and
KW conceived the study. ZZ and KC performed the literature search
and wrote the manuscript. BH contributed to the interpretation of
data and literature review. YS contributed to assembling the
figures and the follow-up of the patient. QZ, FZ and DS collected
and assembled the data. ZZ and DS contributed to the interpretation
of data and the revision of the manuscript. All authors have read
and approved the final manuscript.
Ethics approval and consent to
participate
Not required due to the retrospective nature of the
study.
Patient consent for publication
The patient provided consent for publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Brahme SK, Fox JM, Ferkel RD, Friedman MJ,
Flannigan BD and Resnick DL: Osteonecrosis of the knee after
arthroscopic surgery: Diagnosis with MR imaging. Radiology.
178:851–853. 1991.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Johnson TC, Evans JA, Gilley JA and DeLee
JC: Osteonecrosis of the knee after arthroscopic surgery for
meniscal tears and chondral lesions. Arthroscopy. 16:254–261.
2000.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Faletti C, Robba T and de Petro P:
Postmeniscectomy osteonecrosis. Arthroscopy. 18:91–94.
2002.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kobayashi Y, Kimura M, Higuchi H, Terauchi
M, Shirakura K and Takagishi K: Juxta-articular bone marrow signal
changes on magnetic resonance imaging following arthroscopic
meniscectomy. Arthroscopy. 18:238–245. 2002.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Patel DV, Breazeale NM, Behr CT, Warren
RF, Wickiewicz TL and O'Brien SJ: Osteonecrosis of the knee:
Current clinical concepts. Knee Surg Sports Traumatol Arthrosc.
6:2–11. 1998.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Santori N, Condello V, Adriani E and
Mariani P: Osteonecrosis after arthroscopic medial meniscectomy.
Arthroscopy. 11:220–224. 1995.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Pruès-Latour V, Bonvin JC and Fritschy D:
Nine cases of osteonecrosis in elderly patients following
arthroscopic meniscectomy. Knee Surg Sports Traumatol Arthrosc.
6:142–147. 1998.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Garino JP, Lotke PA, Sapega AA, Reilly PJ
and Esterhai JL Jr: Osteonecrosis of the knee following
laser-assisted arthroscopic surgery: A report of six cases.
Arthroscopy. 11:467–474. 1995.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Strauss EJ, Kang R, Bush-Joseph C and Bach
BR Jr: The diagnosis and management of spontaneous and
post-arthroscopy osteonecrosis of the knee. Bull NYU Hosp Jt Dis.
69:320–330. 2011.PubMed/NCBI
|
|
10
|
MacDessi SJ, Brophy RH, Bullough PG,
Windsor RE and Sculco TP: Subchondral fracture following
arthroscopic knee surgery: A series of eight cases. J Bone Joint
Surg Am. 90:1007–1012. 2008.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Insall JN, Dorr LD, Scott RD and Scott WN:
Rationale of the Knee Society clinical rating system. Clin Orthop
Relat Res. 248:13–14. 1989.PubMed/NCBI
|
|
12
|
Petersen CL, Kjærsgaard JB, Kjærgaard N,
Jensen MU and Laursen MB: Thresholds for Oxford Knee Score after
total knee replacement surgery: A novel approach to post-operative
evaluation. J Orthop Surg Res. 12(89)2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ramkumar PN, Harris JD and Noble PC:
Patient-reported outcome measures after total knee arthroplasty: A
systematic review. Bone Joint Res. 4:120–127. 2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Lansdown DA, Shaw J, Allen CR and Ma CB:
Osteonecrosis of the knee after anterior cruciate ligament
reconstruction a report of 5 cases. Orthop J Sports Med 24.
3(2325967115576120)2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hall FM: Osteonecrosis in the
postoperative knee. Radiology. 236:370–371; author reply 371.
2005.PubMed/NCBI View Article : Google Scholar
|
|
16
|
DeFalco RA, Ricci AR and Balduini FC:
Osteonecrosis of the knee after arthroscopic meniscectomy and
chondroplasty: A case report and literature review. Am J Sports
Med. 31:1013–1016. 2003.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Son IJ, Kim MK, Kim JY and Kim JG:
Osteonecrosis of the knee after arthroscopic partial meniscectomy.
Knee Surg Relat Res. 25:150–154. 2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Li L, Wang H, He Y, Si Y, Zhou H and Wang
X: Treatment of recurrent patellar dislocation via knee arthroscopy
combined with C-armfluoroscopy and reconstruction of the medial
patellofemoral ligament. Exp Ther Med. 15:5051–5057.
2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Shi Y, Tian Z, Zhu L, Zeng J, Liu R and
Zhou J: Clinical efficacy of meniscus plasty under arthroscopy in
middle-aged and elderly patients with meniscus injury. Exp Ther
Med. 16:3089–3093. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bonutti PM, Seyler TM, Delanois RE,
McMahon M, McCarthy JC and Mont MA: Osteonecrosis of the knee after
laser or radiofrequency-assisted arthroscopy: Treatment with
minimally invasive knee arthroplasty. J Bone Joint Surg Am. 88
(Suppl 3):S69–S75. 2006.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Cetik O, Cift H, Comert B and Cirpar M:
Risk of osteonecrosis of the femoral condyle after arthroscopic
chondroplasty using radiofrequency: A prospective clinical series.
Knee Surg Sports Traumatol Arthrosc. 17:24–29. 2009.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Lotke PA, Ecker ML, Barth P and Lonner JH:
Subchondral magnetic resonance imaging changes in early
osteoarthrosis associated with tibial osteonecrosis. Arthroscopy.
16:76–81. 2000.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Nakamura T, Matsumoto T, Nishino M, Tomita
K and Kadoya M: Early magnetic resonance imaging and histologic
findings in a model of femoral head necrosis. Clin Orthop Relat
Res. 68–72. 1997.PubMed/NCBI
|
|
24
|
Türker M, Çetik Ö, Çırpar M, Durusoy S and
Cömert B: Postarthroscopy osteonecrosis of the knee. Knee Surg
Sports Traumatol Arthrosc. 23:246–250. 2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Karim AR, Cherian JJ, Jauregui JJ, Pierce
T and Mont MA: Osteonecrosis of the knee: Review. Ann Transl Med.
3(6)2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Di Caprio F, Meringolo R, Navarra MA,
Mosca M and Ponziani L: Postarthroscopy Osteonecrosis of the Knee:
Current Concepts. Joints. 5:229–236. 2017.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Pape D, Seil R, Anagnostakos K and Kohn D:
Postarthroscopic osteonecrosis of the knee. Arthroscopy.
23:428–438. 2007.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Ficat RP: Idiopathic bone necrosis of the
femoral head. Early diagnosis and treatment. J Bone Joint Surg Br.
67:3–9. 1985.PubMed/NCBI
|
|
29
|
Mont MA, Marker DR, Zywiel MG and Carrino
JA: Osteonecrosis of the knee and related conditions. J Am Acad
Orthop Surg. 19:482–494. 2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Kraenzlin ME, Graf C, Meier C, Kraenzlin C
and Friedrich NF: Possible beneficial effect of bisphosphonates in
osteonecrosis of the knee. Knee Surg Sports Traumatol Arthrosc.
18:1638–1644. 2010.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Jacobs MA, Loeb PE and Hungerford DS: Core
decompression of the distal femur for avascular necrosis of the
knee. J Bone Joint Surg Br. 71:583–587. 1989.PubMed/NCBI
|
|
32
|
Duany NG, Zywiel MG, McGrath MS, Siddiqui
JA, Jones LC, Bonutti PM and Mont MA: Joint-preserving surgical
treatment of spontaneous osteonecrosis of the knee. Arch Orthop
Trauma Surg. 130:11–16. 2010.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Tanaka Y, Mima H, Yonetani Y, Shiozaki Y,
Nakamura N and Horibe S: Histological evaluation of spontaneous
osteonecrosis of the medial femoral condyle and short-term clinical
results of osteochondral autografting: A case series. Knee.
16:130–113. 2009.PubMed/NCBI View Article : Google Scholar
|