Introduction
Renal interstitial fibrosis (RIF) is a final common
pathway for progression of all the various chronic kidney diseases
(CKD) to end-stage renal disease (ESRD), causing the need of
continuous renal replacement therapy in form of dialysis or
transplantation (1). The main
features of RIF, including renal tubular atrophy/dilatation,
interstitial inflammatory cell infiltration, induction of
apoptosis, fibroblasts activation and extracellular matrix (ECM)
deposition, have been previously described (2). However, the antifibrotic therapeutic
strategies currently available have not been able to effectively
delay progression of CKD to ESRD or to inhibit the side effects
associated with kidney diseases (3,4).
Therefore, it is of great importance to understand the mechanism
underlying RIF in order to develop optimal strategies that are
effective and safe for treating patients with CKD.
The mammalian target of rapamycin (mTOR), a
serine/threonine protein kinase, is a member of the
phosphatidylinositol-related kinase (PI3K) family and serves an
important role in cell growth, proliferation and differentiation
(5). Accumulating evidence
demonstrated that persistent activation of mTOR is associated with
the development of RIF in a rat model of hypertensive nephropathy
(6), and in mice models of
unilateral ureteral obstruction (UUO) (7) and polycystic nephropathy (8,9).
Therefore, inhibition of mTOR activity may be an effective
therapeutic strategy for CKD treatment.
The activity of endogenous mTOR is not only
regulated by its own expression level, but also by its antagonists.
The DEP domain-containing mTOR interacting protein (Deptor) is an
important component of the mTOR complex and a constitutive
inhibitor of mTOR activity, acting as an endogenous negative
regulator of the mTOR signaling pathway (10). Deptor is involved in several
cellular processes, such as cell growth, apoptosis, autophagy and
anti-inflammatory responses (11).
Several previous studies have showed that Deptor is highly
expressed in mesangial cells, proximal tubular epithelial cells and
embryonic kidney cells, and it is less expressed in renal cancer
cells (11-13).
Moreover, accumulating evidence demonstrated that Deptor is
associated with the pathogenesis of various kidney diseases
(14-16).
Nevertheless, to the best of our knowledge, no previous studies
showed that Deptor is involved in the development of RIF caused by
UUO in rat.
Metformin is a biguanide compound that has been used
as an oral anti diabetic drug for >50 years. In addition to its
glycemia-lowering effects, metformin has anti-inflammatory,
anti-cancer and anti-aging effects (17). Furthermore, metformin may prevent or
delay the onset and progression of renal fibrosis in mice with UUO
(18). Recently, it was reported
that the anti-cancer effect of metformin is associated with the
inhibition of the Deptor-mTOR signaling pathway (17). However, to the best of our
knowledge, whether the mechanism underlying the anti-renal
interstitial fibrosis efficacy of metformin is associated with the
regulation of the Deptor-mTOR signaling pathway in the kidney has
not been previously studied. Therefore, the present study aimed to
investigate whether the effect and mechanism of metformin against
RIF involved the Deptor-mTOR signaling pathway using an
experimental model of RIF in rats following UUO.
Materials and methods
Animals
Ten-week-old male Sprague-Dawley (SD) rats, (weight,
180-220 g) were purchased from the Laboratory Animal Center of
Xuzhou Medical University (Xuzhou, China). The animals were housed
in a 12-h light/dark cycle under controlled temperature (23±1˚C)
and at 65-70% relative humidity. All animal experiments were
approved by The Animal Ethics Committee of Xuzhou Medical
University (Xuzhou, China). Every effort was made to minimize
animal stress.
Animal grouping and experimental
protocols
54 SD rats were randomly divided into various
groups: i) A sham-operated group (sham group); ii) three UUO groups
examined at three different time points (3, 7 and 14 days after
UUO); iii) a M50 group (UUO rats treated with low-dose metformin at
50 mg/kg/day); iv) a M100 group (UUO rats treated with medium-dose
metformin at 100 mg/kg/day); and v) a M200 group (UUO rats treated
with high-dose metformin at 200 mg/kg/day). Rats treated with
metformin were treated once a day (1 ml/100 g) for 14 consecutive
days after surgery. The rats in the sham and UUO groups were
administered equal volumes of 0.5% sodium carboxymethyl cellulose
(CMC-Na, vehicle). Metformin and vehicle were given via
intragastric administration. In addition, metformin was
administered orally to the normal rats with the high dose at 200
mg/kg simply had no influence on the weight and renal function
compared with the sham group, which excluded the renal toxicity of
the drug, and that was consistent with the previous research
(19).
For UUO surgery, rats were anesthetized with 10%
chloral hydrate (350 mg/kg) by intraperitoneal injection (i.p.
injection), and the left lateral dorsal surface of the rat was
incised, the left ureter was isolated and ligated with silk
sutures, which were cut at the middle of the ligation sites to
prevent retrograde urinary tract infections. Sham surgeries were
performed in a similar manner, except for the ureter ligation. At
the end of the experiment, each rat (weight, 210-250 g) was
euthanized via exsanguination from the abdominal aorta (blood
volume extracted, ~9 ml) under deep anesthesia (10% chloral
hydrate, 400 mg/kg, i.p. injection), and death was confirmed by
checking for lack of breath and heartbeat. The kidney was removed,
and one part of the kidney was fixed in 4% paraformaldehyde for
subsequent histological analysis. The remaining parts of the
kidneys and blood samples were stored at -80˚C for biochemical
analysis. Sham operation-induced minor renal damage in the sham
group, there was no significant change in the content of collagen
and renal function within two weeks, and sample of the sham group
was collected at 14 days after UUO surgery. Following
intraperitoneal administration of chloral hydrate, no obvious signs
and symptoms of peritonitis were observed in any animal during the
course of the experiment.
Renal function assessment
The serum creatinine (Scr) was measured using a
picric acid method and blood urea nitrogen (BUN) was measured using
a urease assay as previously described (20,21).
Serum was obtained from blood samples collected in non-heparinized
vacuum tubes, then centrifuged at 3,500 x g for 15 min. Serum
samples were stored at -80˚C for further analysis. The Scr and BUN
levels of the rats were measured with Scr and BUN assay kits
(Jiancheng Bioengineering Institute, Nanjing, China),
respectively.
Histological analysis
Kidney tissues were fixed in 4% formaldehyde and
embedded in paraffin for histological analysis. Then, 4-µm-thick
paraffin sections were dewaxed and hydrated. The sections were
stained with a Sirius-Red staining kit (Bogoo Biotechnology Co.
Ltd.) according to the manufacturer's protocol. Then, the sections
were dehydrated to transparency, mounted with neutral gum and
examined using an Olympus BX43F microscope (Olympus Corporation).
All histopathological alterations were evaluated by two blinded
investigators, five sections were randomly selected in each slide,
and five randomly-selected fields of view were analyzed in each
section. The percentage of positive areas were analyzed using the
Image-Pro Plus 4.0 software. The kidney weight index (mg/g) was
calculated as the ratio between the weight of the left or right
kidney (mg) and the body weight (g) of the rat.
Immunohistochemistry analysis
Assays of Deptor and CD68 levels by
immunohistochemistry were performed as previously described
(22). The kidney sections embedded
with paraffin were deparaffinized in xylene and hydrated through a
decreasing series of alcohol. To inhibit endogenous peroxidase
activity, sections were subsequently placed in 3%
H2O2. Then, the sections were blocked with 3%
BSA, and incubated with anti-Deptor (1:100; Cell Signaling
Technology, Inc.) and anti-CD68 (1:50; Boster) antibodies overnight
at 4˚C. The sections were stained using a polymer HRP detection kit
(ZSGB-BIO) and counterstained with hematoxylin. An Olympus BX43F
microscope (Olympus Corporation) was used to examine the sections,
and the positive Deptor and CD68 signals were quantified using the
integrated optical density value with the Image-Pro Plus 4.0
software.
Western blot analysis
Proteins were extracted from kidney tissues using
RIPA lysis buffer as previously described (23). The supernatant was collected, and
the concentration was determined using a bicinchoninic acid protein
assay kit (Beyotime Institute of Biotechnology). Then, protein
samples (40-60 µg) were separated using 8-10% SDS-PAGE and
transferred onto nitrocellulose membranes. The membranes were then
blocked in PBS containing 3% BSA and incubated overnight at 4˚C
with appropriate primary antibodies, including anti-mTOR (1:1,000;
Cell Signaling Technology, Inc.), anti-phosphorylated (p-)mTOR (Ser
2448, 1:1,000; Cell Signaling Technology, Inc.), anti-p70S6K
(1:500; Cell Signaling Technology, Inc.), anti-p-p70S6K (Ser 371,
1:500; Cell Signaling Technology, Inc.), anti-Deptor (1:800; Cell
Signaling Technology, Inc.) and anti-α-SMA (1:1,000; Abcam).
Near-infrared fluorescence-conjugated secondary antibodies
(1:10,000; LI-COR) were used to detect the proteins at room
temperature and were developed colorimetrically using the Odyssey
biocolor infrared fluorescence imaging system (LI-COR).
Quantification was performed by measuring the signal intensity
using the ImageJ software.
Statistical analysis
The results are presented as the mean ± SEM.
Comparisons between groups were performed using one-way ANOVA
followed by Tukey's test. P<0.05 was considered to indicate a
statistically significant difference. Statistical analysis was
performed using SPSS 13.0 statistical software.
Results
Dynamic changes of Deptor during
RIF
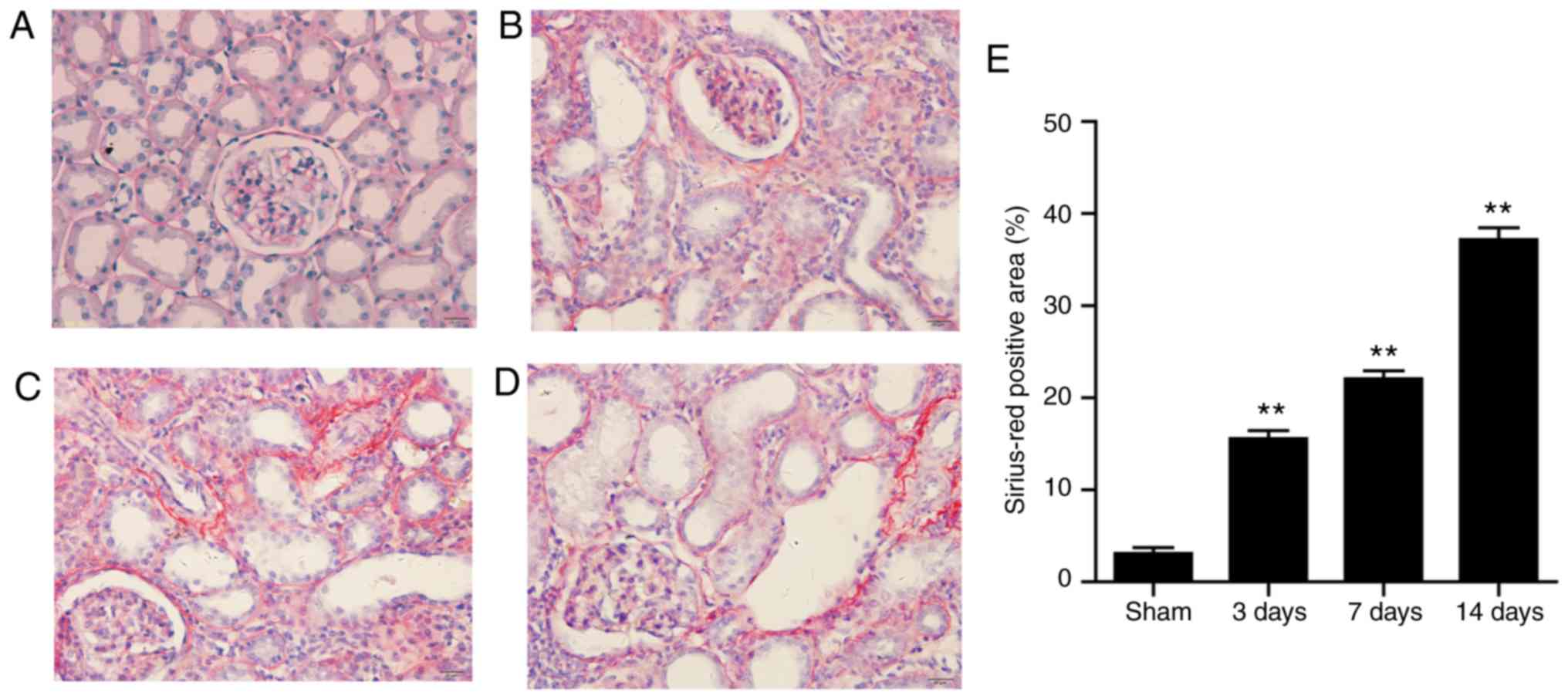
The amount of fibrotic tissue as measured by
Sirius-Red staining. Kidneys from sham-operated rats exhibited no
or very weak positive Sirius-Red staining, while large amount of
fibrotic tissue was measured by Sirius-Red staining was accumulated
in the glomeruli and interstitial regions of UUO rats, which
increased gradually over time. Highest level of collagen was
detected at 14 days after surgery (Fig.
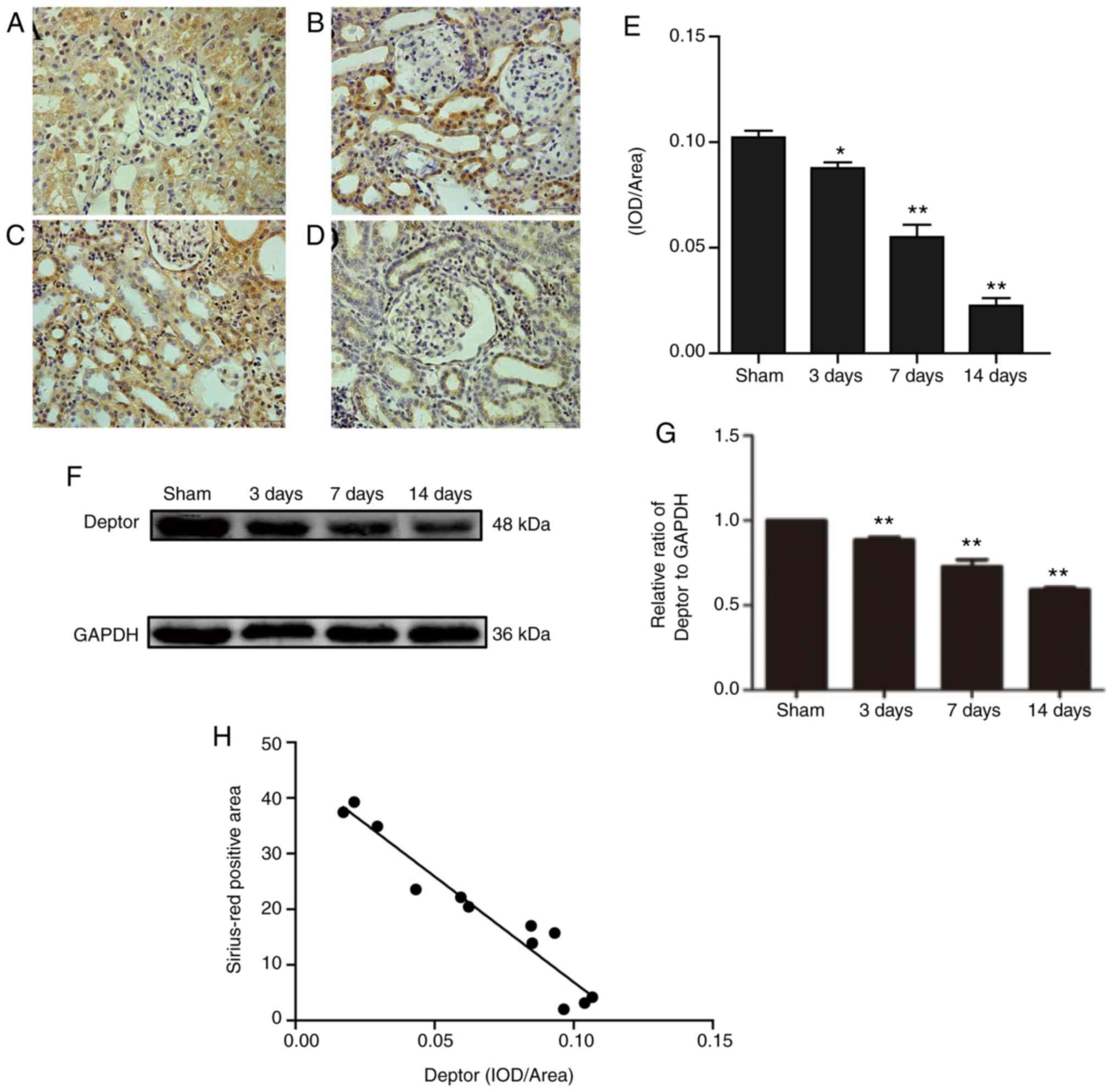
1A-E). Immunohistochemistry staining results showed that Deptor
decreased in the interstitial and glomerular mesangial area in the
UUO groups (Fig. 2A-E). Western
blotting results were in line with the immunohistochemistry
staining results (Fig. 2F and
G). Furthermore, a correlation was
identified between collagen and Deptor levels. The present results
suggested that collagen and Deptor levels were negatively
correlated (Fig. 2H).
Effects of metformin on hypertrophy of
kidney and renal functions in UUO rats
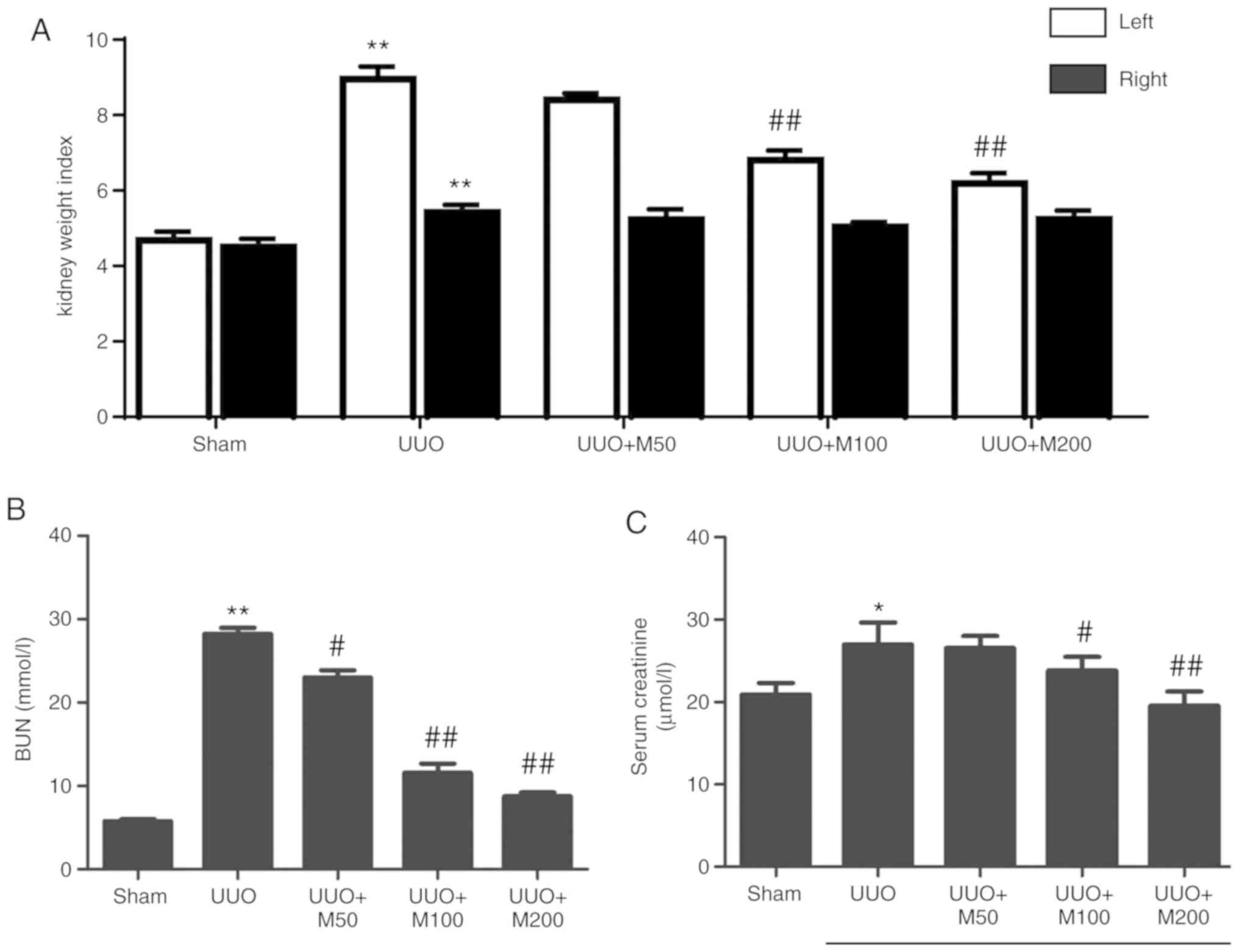
Compared with the sham group, UUO rats had
significantly higher left and right kidney weight index, and the
left kidney weight index was increased at higher levels than that
in the right kidney (Fig. 3A).
Compared with the UUO group, medium and high doses of metformin
significantly inhibited the increase in left kidney weight index.
Low dose of metformin slightly reduced the left kidney weight of
UUO rats, but the difference was not statistically significant. By
contrast, the three doses of metformin did not significantly
affected the right kidney weight index.
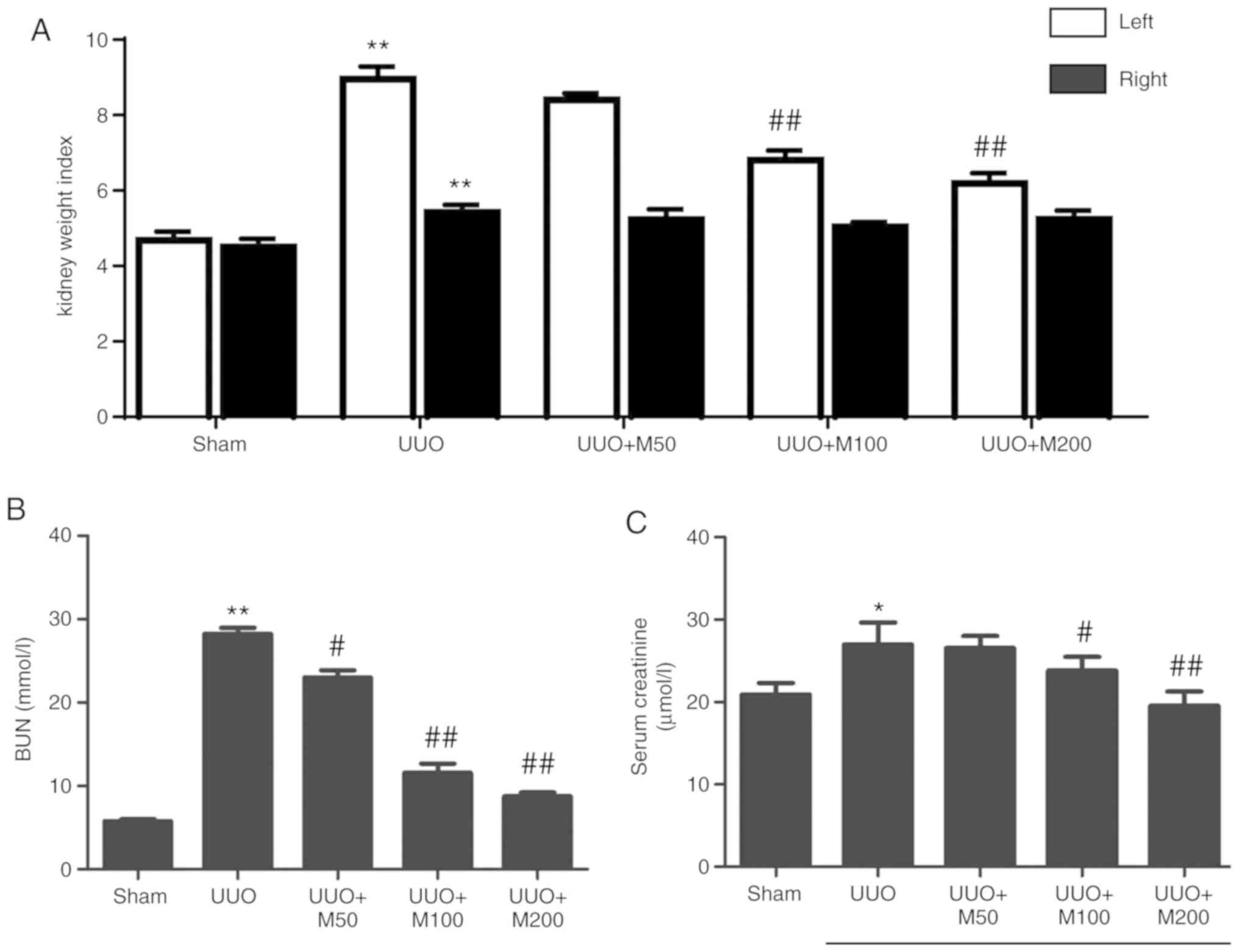 | Figure 3Effect of metformin on hypertrophy of
kidney and renal function. Kidney weight index (mg/g) was expressed
as the ratio of final kidney weight (mg) to final body weight (g).
(A) Statistical analysis of kidney weight index. (B) Statistical
analysis of BUN. (C) Statistical analysis of serum creatinine. All
data are presented as the mean ± SEM. n=6. *P<0.05,
**P<0.01 vs. sham group; #P<0.05,
##P<0.01 vs. UUO group. Sham, Sham-operated group;
UUO, unilateral ureteral obstruction group; UUO + M50, UUO rats
treated with low-dose metformin, 50 mg/kg/day; UUO + M100, UUO rats
treated with intermediate-dose metformin, 100 mg/kg/day; UUO +
M200, UUO rats treated with high-dose metformin, 200 mg/kg/day;
BUN, blood urea nitrogen. |
The results of renal function test showed that the
levels of BUN (Fig. 3B) and Scr
(Fig. 3C) in the UUO group
increased significantly compared with sham rats. Compared with the
UUO untreated group, low, medium and high doses of metformin
significantly reduced the level of BUN in UUO rats (Fig. 3B). High and medium doses of
metformin reduced the level of Scr (Fig. 3C). Low dose of metformin reduced the
level of Scr, but the difference was not statistically significant
(Fig. 3C).
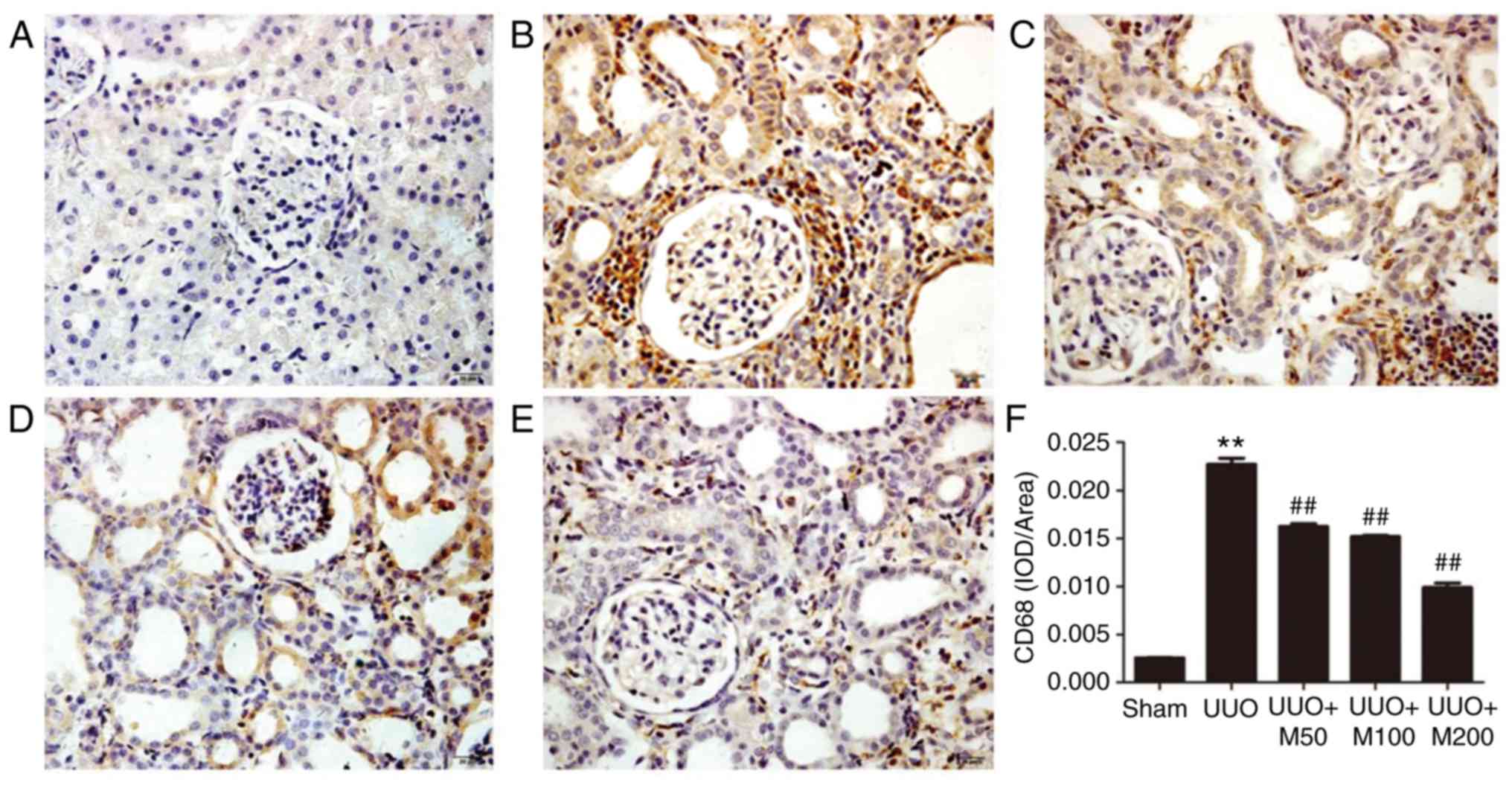
Effects of metformin on CD68 in UUO
rats
CD68 protein was lowly expressed in glomerular
mesangial and renal interstitial regions in the sham group. By
contrast, a high number of regions positive for CD68 staining were
identified in the UUO group, indicating the presence of an
increased number of infiltrating macrophages. Compared with the UUO
group, three doses of metformin reduced the area positive for CD68
in the kidney (P<0.01), indicating that metformin reduced the
infiltration of macrophages in kidney (Fig. 4A-F).
Effects of metformin on renal fibrosis
in UUO rats
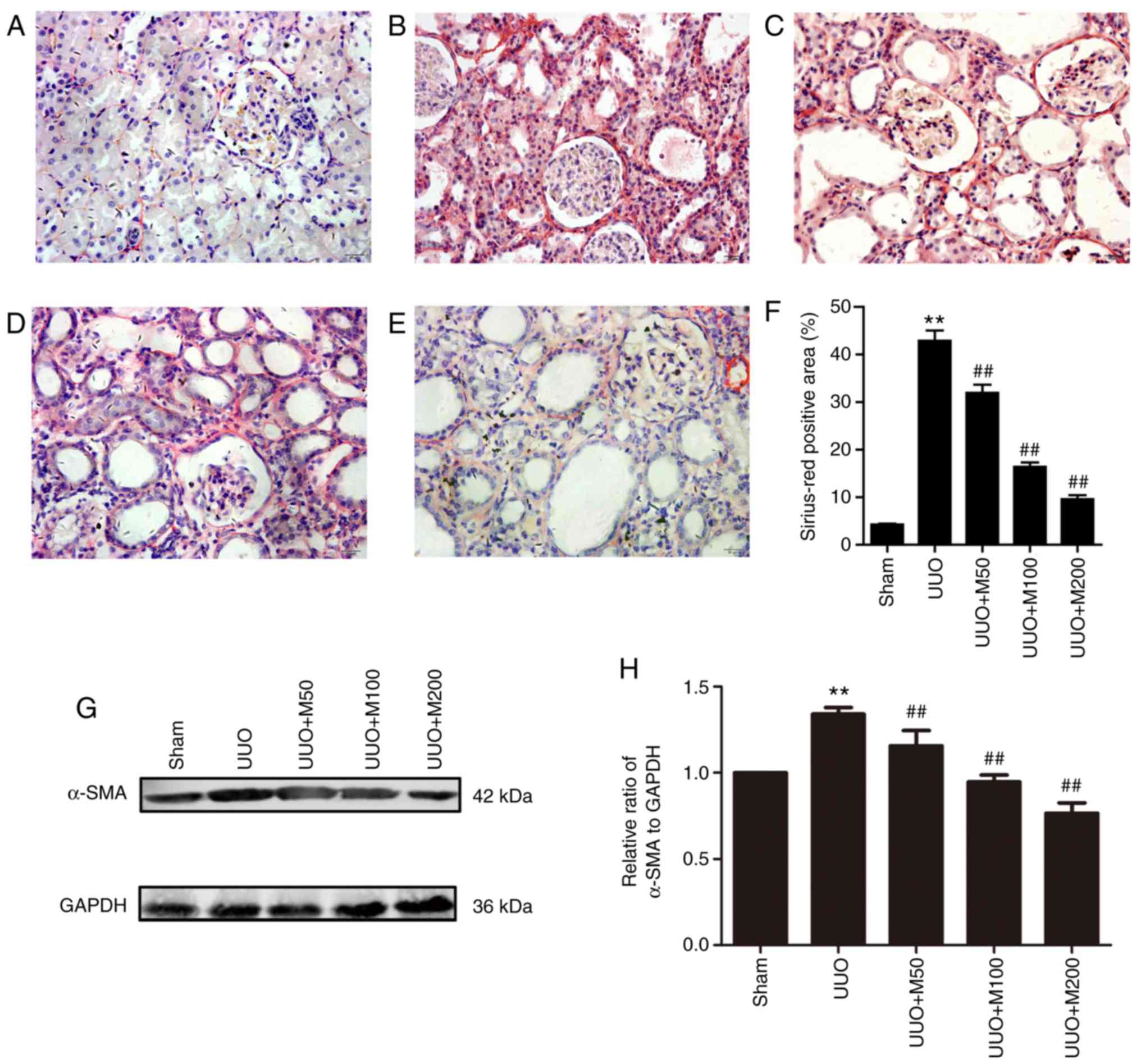
To observe the effect of metformin on collagen
deposition, the degree of RIF in rats was examined by Sirius-Red
staining. As shown in Fig. 5,
collagen deposition was reduced in the sham group. However, there
were a large number of red-positive areas in the UUO group,
indicating that collagen deposition increased in the kidney of UUO
rats. Compared with the UUO group, three doses of metformin
significantly decreased the collagen deposition in renal tubules
and renal interstitial regions (P<0.01), suggesting that
metformin decreased the deposition of collagen in renal tissue of
UUO rats (Fig. 5A-F).
The myofibroblast, an activated fibroblast
characterized by α-SMA positive expression, plays an important role
in RIF. Therefore, the protein expression level of α-SMA was
detected by western blotting. α-SMA protein in the kidney of normal
rats was lowly expressed. However, the expression of α-SMA protein
in the kidney of UUO rats was significantly higher than that in the
sham group. Low, medium and high doses of metformin reversed the
protein expression level of α-SMA in rat kidney. The present
results suggested that metformin reduced the UUO-induced RIF
(Fig. 5G and H).
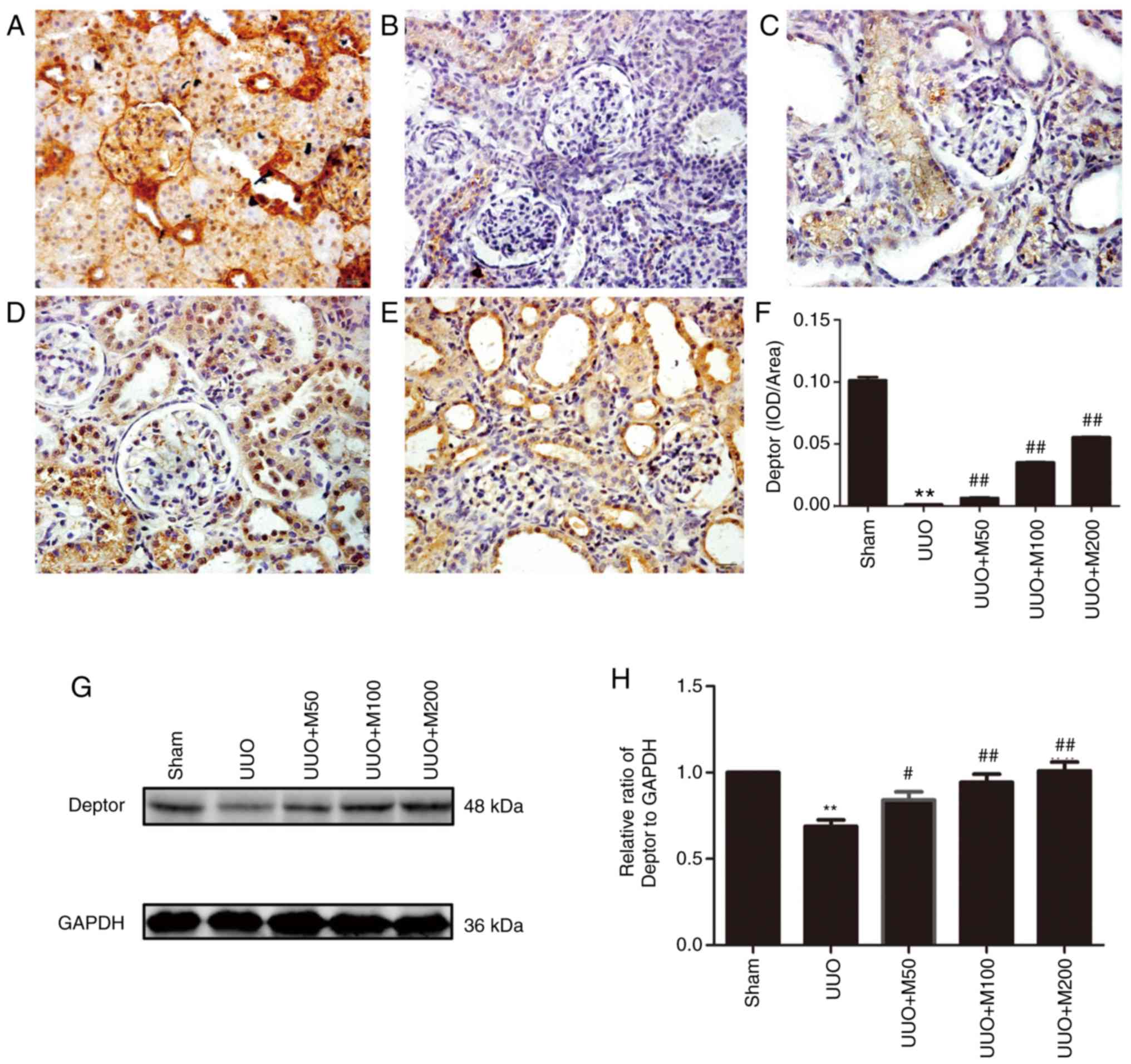
Effects of metformin on expression of
Deptor in the kidneys of UUO rats
The expression of Deptor protein was decreased
during RIF and was negatively correlated with collagen expression.
Therefore, the effects of metformin on Deptor protein expression
were examined in renal tissue of UUO rats. Immunohistochemistry and
western blotting suggested that Deptor protein was highly expressed
in the kidney of rats in the sham group. Compared with the sham
group, the expression of Deptor in UUO rats was significantly
decreased, whereas the three doses of metformin upregulated the
expression level of Deptor protein in the kidneys (Fig. 6A-H).
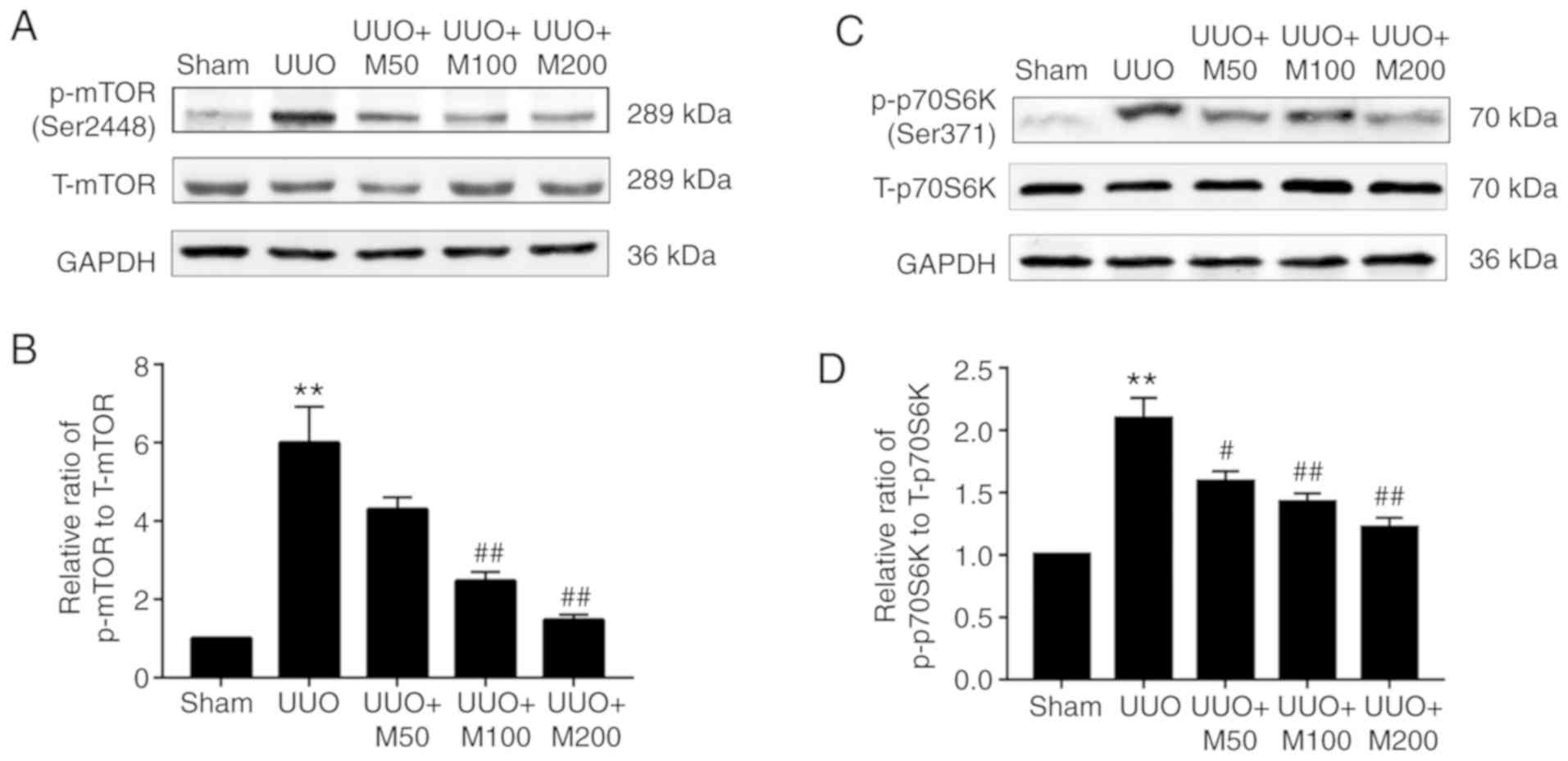
Effects of metformin on the activity
of the mTOR/p70S6K pathway in the kidneys of UUO rats
Deptor is an mTOR endogenous antagonist and
metformin can upregulate Deptor expression. Therefore, the
activation of the mTOR/p70S6K signaling pathway was examined in
renal tissues of UUO rats. The western blotting results suggested
that there was no significant difference in the expression of total
mTOR (T-mTOR) and total p70S6K (T-p70S6K) in the kidneys of each
group. The protein expression levels of p-mTOR and p-p70S6K in the
kidneys of sham rats were almost absent. Compared with the sham
group, the protein expression levels of p-mTOR and p-p70S6K in the
kidneys of UUO rats were significantly increased, however metformin
significantly decreased the phosphorylation levels of mTOR and
p70S6K in the kidney of UUO rats, but only low dose of metformin
had no significant difference (Fig.
7A-D).
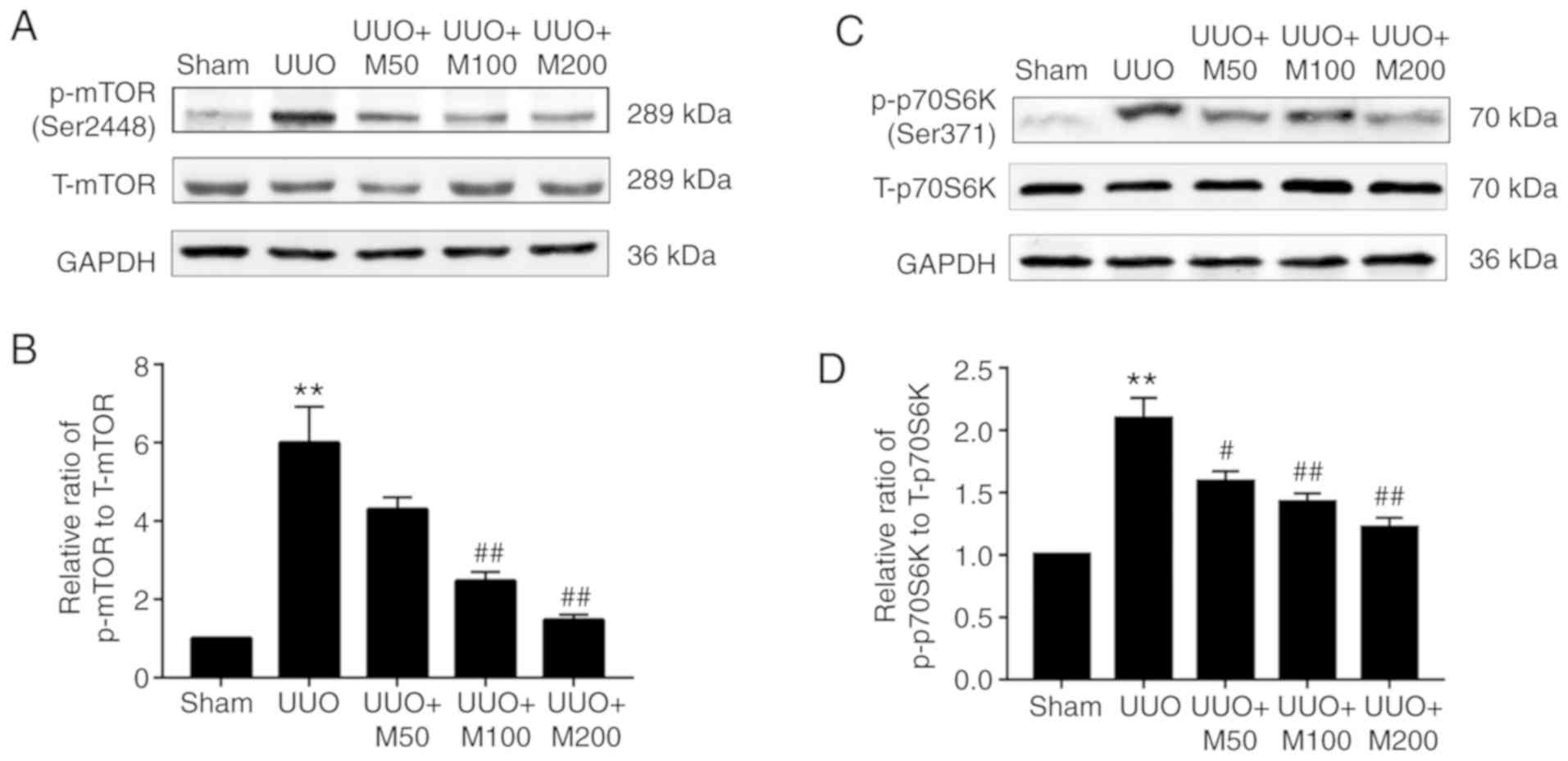 | Figure 7Effect of metformin on the
mTOR/p70S6K pathway in obstructed kidneys. Western blot and
quantitative analysis of the levels of p-mTOR (Ser2448) and p-
p70S6K (Ser371) was performed following normalization to T-mTOR and
T-p70S6K, respectively. GAPDH was used as an internal control. (A)
p-mTOR levels were detected in rat kidneys by western blotting. (B)
Statistical analysis of the levels of p-mTOR. (C) p-p70S6K levels
were detected in rat kidneys by western blotting. (D) Statistical
analysis of the levels of p-p70S6K. All data are presented as the
mean ± SEM. n=3. **P<0.01 vs. sham group;
#P<0.05, ##P<0.01 vs. UUO group. Sham,
Sham-operated group; UUO, unilateral ureteral obstruction group;
UUO + M50, UUO rats treated with low-dose metformin, 50 mg/kg/day;
UUO + M100, UUO rats treated with intermediate-dose metformin, 100
mg/kg/day; UUO + M200, UUO rats treated with high-dose metformin,
200 mg/kg/day; p-, phosphorylated; T-, total; p70S6K, ribosomal
protein S6 kinase. |
Discussion
RIF is the most important factor determining the
renal outcomes and clinical course of kidney diseases. In the
present study, the expression level of Deptor was progressively
downregulated over time in UUO rats. Moreover, the expression of
collagen was found to be negatively correlated with the expression
of Deptor in renal tissues of UUO rats. However, metformin
significantly upregulated the protein expression level of Deptor,
and downregulated the protein expression levels of p-mTOR and
p-p70S6K, and three doses of metformin nearly reversed the changes
stated above, except for the level of p-mTOR in low dose of
metformin group.
Deptor, an endogenous mTOR inhibitory factor
discovered by Peterson et al (10), is involved in the regulation of cell
proliferation, survival, transdifferentiation and autophagy.
Bruneau et al (11) reported
that Deptor serves a key role in endogenous mechanisms of
anti-inflammation and pro-resolution by regulating the endothelial
cell-specific expression of chemokines and adhesion molecules,
leukocyte-endothelial adhesion, and endothelial migratory
responses. Recent studies found that Deptor serves an important
role in various human diseases including kidney diseases (12,24,25).
Transforming growth factor beta 1 (TGF-β1) serves an important role
in the pathogenesis of renal fibrosis. TGF-β1 can mediate chronic
inflammation, myofibroblast activation and may promote ECM
accumulation. It has been reported that TGF-β1 can increase the
activity of mTOR and promote collagen secretion by down-regulating
Deptor expression (12,15). The present study identified
gradually increasing collagen deposition in the kidneys of rats in
the UUO group in a time-dependent manner, whereas the expression of
Deptor in UUO kidneys decreased over time, indicating that Deptor
may be involved in the development of the pathogenesis of renal
fibrosis.
Metformin is the most widely used first-line
biguanide drug in the treatment of type 2 diabetes. Metformin, in
addition to its hypoglycemic effect, can also reduce cardiovascular
complications in diabetic patients (26). Additionally, a previous study showed
that metformin has antifibrotic activity (18). In animal models of non-alcoholic
steatohepatitis, metformin could reduce the inflammatory response
to prevent hepatic fibrosis (27).
The present study found that metformin reduced the left renal mass
index, Scr and BUN levels in UUO rat. Sirius-Red staining showed
that metformin treatment also reduced the collagen area in renal
tubules and interstitial regions of UUO rats. The present results
suggested that metformin may significantly alleviate UUO-induced
RIF and improve renal function.
Excessive deposition of ECM is one of the most
important features of RIF. α-SMA+ myofibroblast can
secret ECM components such as collagen. In the present study, the
protein level of α-SMA was upregulated in the kidney of UUO rats,
suggesting an accumulation of myofibroblasts in the renal tissue of
rats following UUO. The three concentrations of metformin tested in
the present study were able to significantly reduce α-SMA protein
level and inhibit the formation of myofibroblast. In addition,
Sirius-Red staining suggested that metformin reduced the deposition
of collagen in the kidneys of UUO rats.
CD68 is an important marker of macrophages, and
several previous studies demonstrated that macrophage infiltration
promotes the development of RIF. Previous studies reported that
macrophages could release inflammatory mediators such as
interleukin-β (IL-β) and a large number of cytokines to promote the
expression of adhesion factors, increasing the accumulation of
inflammatory factors in the inflammatory site, thus aggravating the
inflammatory response (28). In
addition, macrophages can also transform into myofibroblasts (MMT)
to promote the synthesis of ECM, thus leading to RIF (29). The present results suggested that
the expression of CD68 protein was increased in the kidney of UUO
rats, and metformin treatment effectively inhibited its expression,
indicating that metformin decreased the infiltration of
macrophages, and reduced the inflammatory response and the MMT
process, thereby delaying the progression of renal fibrosis.
Accumulating evidence demonstrated the detrimental
effects of the mTOR/p70S6K pathway in renal fibrosis. In response
to various stimuli, mTOR can be activated through phosphorylation,
and the activated p-mTOR is involved in the regulation of protein
synthesis by inducing the phosphorylation of p70S6K, which can
phosphorylate the ribosomal protein S6 that is involved in protein
translation (30,31). Previous animal studies demonstrated
that mTOR is highly activated in kidneys of diabetic nephropathy
rats, but rapamycin could ameliorate glomerular hypertrophy,
reducing proinflammatory cytokines expression, and relieving renal
interstitial inflammation and fibrosis (32). In addition, rapamycin reduced
macrophage infiltration in obstructed kidneys, reversed EMT
progression and alleviated RIF (33). The present study suggested that the
mTOR/p70S6K signaling pathway was inactive in kidneys from the sham
group. However, the protein expression levels of p-mTOR and
p-p70S6K were significantly upregulated following UUO via the
activation of the mTOR/p70S6K signaling pathway in the kidneys of
UUO rats. Administration of metformin for 14 days effectively
inhibited the activation of the mTOR/p70S6K pathway induced by
UUO.
Several reports have demonstrated that activation of
adenosine monophosphate-activated protein kinase (AMPK) improves
renal function in experimental models of acute kidney injury (AKI)
(34) and CKD (35). The effects of metformin are mainly
driven by the activation of AMPK, which regulates downstream
signaling pathways (36). It was
reported that AMPK also affects proteasomal degradation, and AMPK
activation by metformin leads to an inhibition of proteasomal
function (37). Evidences show that
the protein levels of Deptor are known to be regulated by a
proteasome-mediated proteolytic degradation (10). Previous study has reported that
metformin increases the protein levels of Deptor via suppression of
proteasome activity in an AMPK-dependent manner (17). In the present study, the expression
of Deptor was significantly decreased in the kidneys of UUO rats,
and metformin treatment efficiently increased the expression level
of this protein. Therefore, we infer that activation of AMPK by
metformin could inhibit the activity of proteasome, and
subsequently upregulate the expression of Deptor, which leads to
anti-fibrotic effect on rat renal fibrosis by suppressing mTOR
signaling.
In conclusion, the present study suggested that
metformin ameliorated the impaired renal function in a model of
UUO-induced renal fibrosis, and the mechanism mediating this effect
may be associated with the upregulation of Deptor expression level
and the inhibition of the mTOR/p70S6K signaling pathway. Therefore,
in addition to the anti-diabetic therapeutic potential of
metformin, this drug may also be considered as a potential
therapeutic for the treatment of renal fibrosis.
Acknowledgements
Not applicable.
Funding
The present study was supported by a grant from the
Natural Science Foundation of Jiangsu Province (grant no.
BK20161179).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AZX, YXW and YL conceived and designed the study.
YL, LHL and YW performed the experiments. AZX and YXW wrote the
manuscript. YXP and SZ analyzed the data. All authors read and
approved the manuscript and agreed to be accountable for all
aspects of the research in ensuring that the accuracy or integrity
of any part of the work are appropriately investigated and
resolved.
Ethics approval and consent to
participate
All animal experiments were approved by the Animal
Ethics Committee of Xuzhou Medical University.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bai J, Hao J, Zhang X, Cui H, Han J and
Cao N: Netrin-1 attenuates the progression of renal dysfunction by
blocking endothelial-to-mesenchymal transition in the 5/6
nephrectomy rat model. BMC Nephrol. 17(47)2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Zeisberg M and Neilson EG: Mechanisms of
tubulointerstitial fibrosis. J Am Soc Nephrol. 21:1819–1834.
2010.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rostaing L and Kamar N: mTOR
inhibitor/proliferation signal inhibitors: Entering or leaving the
field? J Nephrol. 23:133–142. 2010.PubMed/NCBI
|
|
4
|
Deblon N, Bourgoin L, Veyrat-Durebex C,
Peyrou M, Vinciguerra M, Caillon A, Maeder C, Fournier M, Montet X,
Rohner-Jeanrenaud F and Foti M: Chronic mTOR inhibition by
rapamycin induces muscle insulin resistance despite weight loss in
rats. Br J Pharmacol. 165:2325–2340. 2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kim D, Cheng GZ, Lindsley CW, Yang H and
Cheng JQ: Targeting the phosphatidylinositol-3 kinase/Akt pathway
for the treatment of cancer. Curr Opin Investig Drugs. 6:1250–1258.
2005.PubMed/NCBI
|
|
6
|
Takenaka T, Inoue T, Miyazaki T, Kobori H,
Nishiyama A, Ishii N, Hayashi M and Suzuki H: Klotho ameliorates
medullary fibrosis and pressure natriuresis in hypertensive rat
kidneys. Hypertension. 72:1151–1159. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chen G, Chen H, Wang C, Peng Y, Sun L, Liu
H and Liu F: Rapamycin ameliorates kidney fibrosis by inhibiting
the activation of mTOR signaling in interstitial macrophages and
myofibroblasts. PLoS One. 7(e33626)2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Aboudehen K, Farahani S, Kanchwala M, Chan
SC, Avdulov S, Mickelson A, Lee D, Gearhart MD, Patel V, Xing C and
Igarashi P: Long noncoding RNA Hoxb3os is dysregulated in autosomal
dominant polycystic kidney disease and regulates mTOR signaling. J
Biol Chem. 293:9388–9398. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Raman A, Parnell SC, Zhang Y, Reif GA, Dai
Y, Khanna A, Daniel E, White C, Vivian JL and Wallace DP: Periostin
overexpression in collecting ducts accelerates renal cyst growth
and fibrosis in polycystic kidney disease. Am J Physiol Renal
Physiol. 315:F1695–F1707. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Peterson TR, Laplante M, Thoreen CC,
Sancak Y, Kang SA, Kuehl WM, Gray NS and Sabatini DM: DEPTOR is an
mTOR inhibitor frequently overexpressed in multiple myeloma cells
and required for their survival. Cell. 137:873–886. 2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Bruneau S, Nakayama H, Woda CB, Flynn EA
and Briscoe DM: DEPTOR regulates vascular endothelial cell
activation and proinflammatory and angiogenic responses. Blood.
122:1833–1842. 2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Das F, Ghosh-Choudhury N, Bera A, Dey N,
Abboud HE, Kasinath BS and Choudhury GG: Transforming growth factor
β integrates Smad 3 to mechanistic target of rapamycin complexes to
arrest deptor abundance for glomerular mesangial cell hypertrophy.
J Biol Chem. 288:7756–7768. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Das F, Ghosh-Choudhury N, Lee DY, Gorin Y,
Kasinath BS and Choudhury GG: Akt2 causes TGFβ-induced deptor
downregulation facilitating mTOR to drive podocyte hypertrophy and
matrix protein expression. PLoS One. 13(e0207285)2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Maity S, Bera A, Ghosh-Choudhury N, Das F,
Kasinath BS and Choudhury GG: microRNA-181a downregulates deptor
for TGFβ-induced glomerular mesangial cell hypertrophy and matrix
protein expression. Exp Cell Res. 364:5–15. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Das F, Bera A, Ghosh-Choudhury N, Abboud
HE, Kasinath BS and Choudhury GG: TGFβ-induced deptor suppression
recruits mTORC1 and not mTORC2 to enhance collagen I (α2) gene
expression. PLoS One. 9(e109608)2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Wang C, Dai H, Xiong Z, Song Q, Zou Z, Li
M, Nie J, Bai X and Chen Z: Loss of DEPTOR in renal tubules
protects against cisplatin-induced acute kidney injury. Cell Death
Dis. 9(441)2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Obara A, Fujita Y, Abudukadier A,
Fukushima T, Oguri Y, Ogura M, Harashima S, Hosokawa M and Inagaki
N: DEPTOR-related mTOR suppression is involved in metformin's
anti-cancer action in human liver cancer cells. Biochem Biophys Res
Commun. 460:1047–1052. 2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Cavaglieri RC, Day RT, Feliers D and
Abboud HE: Metformin prevents renal interstitial fibrosis in mice
with unilateral ureteral obstruction. Mol Cell Endocrinol.
412:116–122. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Oda SS: Metformin protects against
experimental acrylamide neuropathy in rats. Drug Dev Res.
78:349–359. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Montinaro V, Hevey K, Aventaggiato L,
Fadden K, Esparza A, Chen A, Finbloom DS and Rifai A: Extrarenal
cytokines modulate the glomerular response to IgA immune complexes.
Kidney Int. 42:341–353. 1992.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Sun D, Liu CX, Ma YY and Zhang L:
Protective effect of prostaglandin E1 on renal microvascular injury
in rats of acute aristolochic acid nephropathy. Ren Fail.
33:225–232. 2011.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Chen YJ, Kong L, Tang ZZ, Zhang YM, Liu Y,
Wang TY and Liu YW: Hesperetin ameliorates diabetic nephropathy in
rats by activating Nrf2/ARE/glyoxalase 1 pathway. Biomed
Pharmacother. 111:1166–1175. 2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Xia A, Xue Z, Li Y, Wang W, Xia J, Wei T,
Cao J and Zhou W: Cardioprotective effect of betulinic Acid on
myocardial ischemia reperfusion injury in rats. Evid Based
Complement Alternat Med. 2014(573745)2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Caron A, Baraboi ED, Laplante M and
Richard D: DEP domain-containing mTOR-interacting protein in the
rat brain: Distribution of expression and potential implication. J
Comp Neurol. 523:93–107. 2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Davies J, Zachariades E, Rogers-Broadway
KR and Karteris E: Elucidating the role of DEPTOR in Alzheimer's
disease. Int J Mol Med. 34:1195–1200. 2014.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Wang CP, Lorenzo C, Habib SL, Jo B and
Espinoza SE: Differential effects of metformin on age related
comorbidities in older men with type 2 diabetes. J Diabetes
Complications. 31:679–686. 2017.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Kita Y, Takamura T, Misu H, Ota T, Kurita
S, Takeshita Y, Uno M, Matsuzawa-Nagata N, Kato K, Ando H, et al:
Metformin prevents and reverses inflammation in a non-diabetic
mouse model of nonalcoholic steatohepatitis. PLoS One.
7(e43056)2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Guiteras R, Flaquer M and Cruzado JM:
Macrophage in chronic kidney disease. Clin Kidney J. 9:765–771.
2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Meng XM, Wang S, Huang XR, Yang C, Xiao J,
Zhang Y, To KF, Nikolic-Paterson DJ and Lan HY: Inflammatory
macrophages can transdifferentiate into myofibroblasts during renal
fibrosis. Cell Death Dis. 7(e2495)2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Kapoor V, Zaharieva MM, Das SN and Berger
MR: Erufosine simultaneously induces apoptosis and autophagy by
modulating the Akt-mTOR signaling pathway in oral squamous cell
carcinoma. Cancer Lett. 319:39–48. 2012.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Krause U, Bertrand L and Hue L: Control of
p70 ribosomal protein S6 kinase and acetyl-CoA carboxylase by
AMP-activated protein kinase and protein phosphatases in isolated
hepatocytes. Eur J Biochem. 269:3751–3759. 2002.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Yang Y, Wang J, Qin L, Shou Z, Zhao J,
Wang H, Chen Y and Chen J: Rapamycin prevents early steps of the
development of diabetic nephropathy in rats. Am J Nephrol.
27:495–502. 2007.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Wu MJ, Wen MC, Chiu YT, Chiou YY, Shu KH
and Tang MJ: Rapamycin attenuates unilateral ureteral
obstruction-induced renal fibrosis. Kidney Int. 69:2029–2036.
2006.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Feng J, Li H, Zhang Y, Wang Q, Zhao S,
Meng P and Li J: Mammalian STE20-like kinase 1 deletion alleviates
renal ischaemia-reperfusion injury via modulating mitophagy and the
AMPK-YAP signalling pathway. Cell Physiol Biochem. 51:2359–2376.
2018.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Zhou X, Muise ES, Haimbach R, Sebhat IK,
Zhu Y, Liu F, Souza SC, Kan Y, Pinto S, Kelley DE and Hoek M:
PAN-AMPK activation improves renal function in a rat model of
progressive diabetic nephropathy. J Pharmacol Exp Ther. 371:45–55.
2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Brynildsen JK, Lee BG, Perron IJ, Jin S,
Kim SF and Blendy JA: Activation of AMPK by metformin improves
withdrawal signs precipitated by nicotine withdrawal. Proc Natl
Acad Sci USA. 115:4282–4287. 2018.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Viana R, Aguado C, Esteban I, Moreno D,
Viollet B, Knecht E and Sanz P: Role of AMP-activated protein
kinase in autophagy and proteasome function. Biochem Biophys Res
Commun. 369:964–968. 2008.PubMed/NCBI View Article : Google Scholar
|