Introduction
Acute myocarditis, a common, easily misdiagnosed
disease with a high mortality rate, is defined as an inflammatory
infiltrate of the myocardium that results from viral infections,
autoimmune diseases or cardiotoxic agents (1,2). This
inflammation may lead to acute heart failure, chest pain and
electrocardiographic abnormalities (3).
Various electrocardiogram (ECG) findings have been
reported in patients with myocarditis (4-6).
The common ECG findings are ST-T wave changes, Q waves, QT interval
prolongation, QRS prolongation, low voltage, atrioventricular block
(AVB), bundle branch block (BBB) and ventricular tachycardia (VT)
(4-7).
However, studies on this topic are currently limited, focusing on
abnormal ECG findings and their rate of abundance in patients with
acute myocarditis (4,8). Furthermore, most of the aforementioned
ECG findings (such as VT, AVB, QRS prolongation and low voltage)
are associated with the severity of myocarditis (5,7,8).
However, these studies are mainly on certain ECG changes for
predicting outcomes, and the associations between ECG findings and
the severity are simply mentioned (5,7).
Fulminant myocarditis (FM) is an acute and severe form of
myocarditis (9). FM causes acute
hemodynamic instability which may prove fatal (10). FM is associated with a wide variety
of serious arrhythmias such as VF and AVB (11). AVB is an important ECG aberration in
patients with myocarditis, which is associated with the severity of
the disease (7). However, the
association between AVB and CA remains to be fully elucidated.
Furthermore, ST-T wave changes, including T-wave inversion and ST
segment elevation, are the most common and the most widely studied
ECG changes in myocarditis (2,5). Most
patients with myocarditis present with ST elevation mimicking ECG
alterations caused by AMI. There is currently a shortage of studies
on the characteristics of ST elevation in a large cohort of
patients with myocarditis (1,4).
Furthermore, it has been indicated that certain patients with
myocarditis with ST elevation progress further to T-wave inversion
(11). However, only a small number
of studies with small sample of patients present data regarding the
prognosis of such patients (1,4).
Although ECGs may be easily recorded, the ECG
results of only a small sample of patients with abnormal ECG
findings in myocarditis are currently available (1,4,5,12).
The ECG abnormalities, their association with severity and the
characteristics of ST elevation remain to be fully investigated in
a large cohort of patients with myocarditis. The purpose of the
present study was to identify the role of and draw attention to the
use of ECG in myocarditis. The present study specifically sought to
identify specific ECG findings associated with FM and assess the
characteristics of ST elevation in these patients on admission
through a review of patient databases at two centres in China.
Materials and methods
Study population
The present study was a two-centre retrospective
review of all patients aged ≥13 years who were hospitalized with a
diagnosis of acute myocarditis between August 2007 and November
2019. The medical records were reviewed with permission from ethics
committee of The First Affiliated Hospital of Wenzhou Medical
University (approval no. KY2020-103) and Wenzhou People's Hospital
(approval no. 2020-96). On the basis of the diagnostic criteria of
European Society of Cardiology (2)
and Japanese Circulation Society (10), the diagnosis of acute myocarditis
was confirmed by a recent history of gastrointestinal/upper
respiratory tract infection and/or complaints of cardiac symptoms
and increasing myocardiocytolysis markers and/or presentation with
a new abnormality on the 12-lead ECG, combined with at least one of
the following: i) Active or borderline biopsy according to the
Dallas criteria (13); ii) positive
infectious origin of ventricular dysfunction; iii) delayed
enhancement on cardiac MRI consistent with myocarditis; or iv)
serological tests, ECGs, ultrasonic cardiogram (UCG), coronary
angiography and ventriculography to exclude acute myocardial
infarction (AMI), stress cardiomyopathy, congenital heart disease,
myocarditis secondary to sepsis, valve disease, hyperthyroidism,
autoimmune disease and rheumatic fever. The exclusion criteria were
as follows: i) Incomplete data; ii) a history of congenital heart
disease, cardiomyopathy or arrhythmias; iii) myocarditis not being
the primary diagnosis for an admission; and iv) absence of cardiac
symptoms. Cardiac symptoms were considered to comprise chest pain,
chest discomfort, syncope, dyspnoea, palpitations, shock, seizure
and cyanosis (10).
Diagnosis of FM and patient
management
In patients with acute myocarditis, a diagnosis of
FM was determined upon identification of one or more of the
following: Haemodynamic instability due to cardiogenic shock or
arrhythmia; left ventricular dysfunction and low cardiac output
syndrome requiring inotropes or mechanical circulatory support;
mechanical ventilation; and/or cardiac arrest (CA) (9,14,15).
In the present study, FM was diagnosed in 77 patients (28.1%) on
the basis of the aforementioned criteria, whereas the remaining 197
patients (71.9%) were classified as non-FM. The treatment plan was
established according to the guidelines for different stages of the
disease and the patient's condition (2,10).
ECG data collection and analysis
Standard hospital procedures were followed. When the
patient suspected to have myocarditis was admitted to the hospital,
a standard 12-lead ECG was performed immediately and 24-h ECG
monitoring was performed in parallel. If the ECG exhibited any
abnormality in the right ventricular or posterior wall of the left
ventricle, an 18-lead ECG was added (16). If the ECG indicated arrhythmia, a
1-min ECG was added. If the condition of the patient had changed or
the 24-h ECG monitoring indicated changes in any ECG parameter, the
standard 12-lead/18-lead/1-min ECG was again performed immediately.
ECG changes, including ST elevation or depression, abnormal T
waves, low voltage, abnormal Q waves, QTc prolongation, AVB, BBB,
premature beats, atrial fibrillation, supraventricular tachycardia
and VT were recorded and compared with the ECG abnormality onsets.
Once ECGs were performed, the rhythm, heart rate, PR interval, QRS
duration, QTc interval and ST segment/T-wave changes of all ECGs
obtained during the hospital stay were analyzed independently by
two electrophysiologists (JC, LL) to identify any abnormalities
without any further delay. The discrepancies between the evaluation
results determined by the electrophysiologists were solved by
discussion and a vote (ZL, HW).
Electrocardiographic definitions
ST elevation was defined as an elevation of the J
point in at least two contiguous leads of ≥0.2 mV in chest leads
V2-V3, and/or of ≥0.1 mV in other leads or limb leads with or
without reciprocal ST depression (1,17,18).
ST depression was defined as ST segment depression ≥0.2 mV in at
least two leads, not concurrent with ST elevation (5). Abnormal T waves included flat,
inverted or diphasic T waves. T-wave inversion was defined as a
negative T wave ≥0.1 mV in at least two of the following leads: I,
II, avL and V2-V6(18). Any Q waves
>40 msec were considered abnormal (4). Low voltage was defined as voltages
≤0.5 mV in all limb leads or ≤1.0 mV in all precordial leads
(5). The QT interval was corrected
using the Bazett formula (QTc=QT/√RR) (8). QTc prolongation was defined as a QTc
duration ≥440 msec (8). QRS
prolongation was defined as a QRS duration ≥120 msec in sinus
rhythm (8). VT was diagnosed when
six or more consecutive premature ventricular contractions occurred
(4).
Bradyarrhythmias/tachyarrhythmias and conduction disturbances,
including premature beats, sinus tachycardia or bradycardia,
supraventricular tachycardia, AVB and new BBB, were identified by
referring to the ECG and 1-min ECG. AVB included AVBs that were
non-advanced (first-degree AVB, non-advanced second-degree AVB) or
high-degree (second-degree Mobitz type II AVB and complete AVB)
(7).
Statistical analysis
Data were analyzed using the statistical program
SPSS version 18.0 (SPSS, Inc.). Numerical data are expressed as the
mean ± standard deviation and categorical data are expressed as n
(%). Student's t-test was used for numerical variables and
Pearson's χ2 test for categorical variables. A
χ2 test was used to evaluate and compare the abnormal
ECG findings between the FM and non-FM groups. Multivariate
(unconditional) logistic regression analysis was performed to
further evaluate ECG findings associated with FM and was performed
for significant variables (P≤0.05). A main effect model was used in
logistic regression analysis. The Mann-Whitney U test was used to
compare the duration of cardiac symptoms prior to admission for ST
elevation at admission. A two-sided P<0.05 was considered to
indicate statistical significance.
Results
Basic data
A total of 274 cases of acute myocarditis (234 cases
from The First Affiliated Hospital of Wenzhou Medical University
and 40 cases from Wenzhou People's Hospital), including 186 males
and 88 females, were included in the present study. The mean age of
the patients was 36.97±16.22 years (range, 13-93 years; Table SI). Among all cases, 77 were
diagnosed with FM, 71 cases experienced cardiogenic shock, 27 cases
experienced CA and 14 died. The median duration of cardiac symptoms
prior to admission was 2 days (range, 1-3 days) and the median
length of hospital stay was 8 days (range, 5-12 days). All 1,814
ECGs were collected and analyzed (not including the initial ECG
recording during CA). A mean of 4 ECGs (range, 2-9 ECGs) was
obtained per patient, with the greatest number of ECGs in a patient
being 62.
ECG findings and their association
with FM
Among the 274 cases of myocarditis, 251 cases
(91.6%) presented with abnormal ECG findings. There were at least
two abnormal findings in each of the 192 patients, with the
greatest number of findings in a patient being 10. The most common
ECG findings were abnormal T waves (57.7%)/T-wave inversion (48.2%)
and ST elevation (44.2%) (Table I).
A comparison of general data for FM and non-FM are listed in
Table SI (all P>0.05). Compared
with the non-FM group, the FM group had significantly higher values
for 12 ECG parameters, which are listed in Table II (all P<0.05). Multivariate
logistic regression analysis revealed that the independent
predictive factors associated with FM were VT, high-degree AVB,
sinus tachycardia, low voltage and QRS duration of ≥120 msec (all
P<0.05; Table III).
 | Table IAbnormal findings on
electrocardiograms in patients with acute myocarditis. |
Table I
Abnormal findings on
electrocardiograms in patients with acute myocarditis.
| Variable | N (%) |
|---|
| Abnormal T
waves | 158 (57.7) |
| T-wave
inversion | 132 (48.2) |
| ST elevation | 121 (44.2) |
| Sinus
tachycardia | 72 (26.3) |
| QRS duration of
≥120 msec | 68 (24.8) |
| Right bundle branch
block | 46 (16.8) |
| Left bundle branch
block | 17 (6.2) |
| Intraventricular
block | 11 (4.0) |
| QTc
prolongation | 61 (22.3) |
| Abnormal Q
waves | 48 (17.5) |
| Low voltage | 44 (16.1) |
| High-degree
atrioventricular block | 32 (11.7) |
| Reduced R-wave
height | 28 (10.2) |
|
Ventricular/junctional escape beats | 26 (9.5) |
| Sinus
bradycardia | 24 (8.8) |
| Ventricular
premature beats | 23 (8.4) |
| ST depression | 18 (6.6) |
| Ventricular
tachycardia | 17 (6.2) |
| Atrial premature
beats | 13 (4.7) |
| Sinus
arrhythmia | 13 (4.7) |
| Non-advanced
atrioventricular block | 12 (4.4) |
| Paroxysmal rapid
atrial fibrillation | 9 (3.3) |
| Accelerated
idioventricular/idiojunctional rhythm | 8 (2.9) |
| Interference
atrioventricular dissociation | 5 (1.8) |
| Paroxysmal
supraventricular tachycardia | 3 (1.1) |
 | Table IIComparison of the significant
electrocardiogram findings for FM and non-FM. |
Table II
Comparison of the significant
electrocardiogram findings for FM and non-FM.
| Variable | N | FM 77 (28.1%) | Non-FM 197
(71.9%) | χ2 | P-value |
|---|
| ST elevation | 121 | 42 (54.5) | 79 (40.1) | 4.684 | 0.030 |
| Sinus
tachycardia | 72 | 35 (45.5) | 37 (18.8) | 20.331 | <0.001 |
| QRS duration of
≥120 msec | 68 | 36 (46.8) | 32 (16.2) | 27.619 | <0.001 |
| Abnormal Q
waves | 48 | 23 (29.9) | 25 (12.7) | 11.308 | 0.001 |
| Low voltage | 44 | 21 (27.3) | 23 (11.7) | 9.992 | 0.002 |
| High-degree
atrioventricular block | 32 | 25 (32.5) | 7 (3.6) | 44.871 | <0.001 |
| Reduced R-wave
height | 28 | 14 (18.2) | 14 (7.1) | 7.401 | 0.007 |
|
Ventricular/junctional escape beats | 26 | 15 (19.5) | 11 (5.6) | 12.448 | <0.001 |
| Ventricular
premature beats | 23 | 11 (14.3) | 12 (6.1) | 4.834 | 0.028 |
| Ventricular
tachycardia | 17 | 16 (20.8) | 1 (0.5) | 35.687 | <0.001 |
| Non-advanced
atrioventricular block | 12 | 8 (10.4) | 4 (2.0) | 7.349 | 0.007 |
| Paroxysmal rapid
atrial fibrillation | 9 | 7 (9.1) | 2 (1.0) | 8.965 | 0.003 |
 | Table IIIMultivariate regression analysis of
factors associated with fulminant myocarditis. |
Table III
Multivariate regression analysis of
factors associated with fulminant myocarditis.
| Variable | β | Std. Error | Wald | P-value | OR | 95.0% CI for
OR |
|---|
| Ventricular
tachycardia | 3.213 | 1.122 | 8.199 | 0.004 | 24.859 | 2.756-224.236 |
| High-degree
atrioventricular block | 3.142 | 0.714 | 19.379 | <0.001 | 23.157 | 5.716-93.816 |
| Sinus
tachycardia | 1.288 | 0.379 | 11.576 | 0.001 | 3.627 | 1.727-7.618 |
| Low voltage | 1.089 | 0.433 | 6.318 | 0.012 | 2.972 | 1.271-6.951 |
| QRS duration of
≥120 msec | 0.904 | 0.393 | 5.279 | 0.022 | 2.468 | 1.142-5.336 |
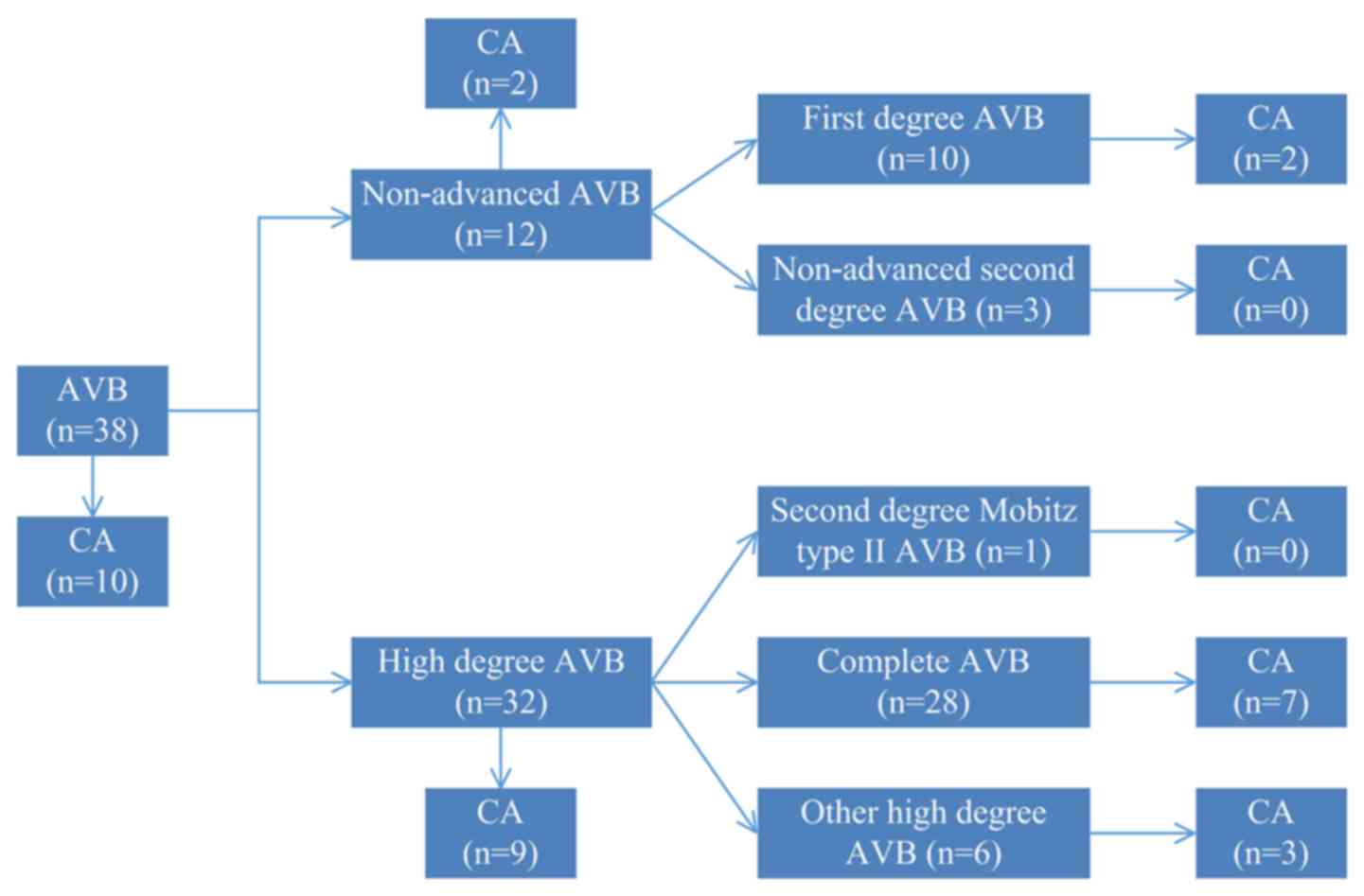
The incidence of CA in different types
of AVB and the initial ECG recorded during CA
As presented in Fig.
1, 38 cases presented with AVB, including 6 cases that had both
non-advanced AVB and high-degree AVB (of the aforementioned 6
patients, 1 case with CA). A total of 12 cases had non-advanced
AVB, including 2 cases with CA; and 32 cases had high-degree AVB,
including 9 cases with CA. The incidence rate of CA (7.2 vs. 26.3%;
P=0.001) was different between the non-AVB (n=236) and AVB groups
(n=38); and the incidence of CA (7.2 vs. 28.1%; P=0.001) was
different between non-AVB (n=236) and high-degree AVB (n=32)
patients (Table SII). A total of
27 patients experienced CA. The initial rhythm of 21 patients
(77.8%) was a shockable rhythm [ventricular fibrillation (VF) or
pulseless VT]. The initial rhythm of 5 patients (18.5%) was a
non-shockable rhythm, including 3 cases of pulseless electrical
activity (11.1%) and 2 cases of asystole (7.4%). The initial rhythm
of 1 patient was unknown (Fig.
S1).
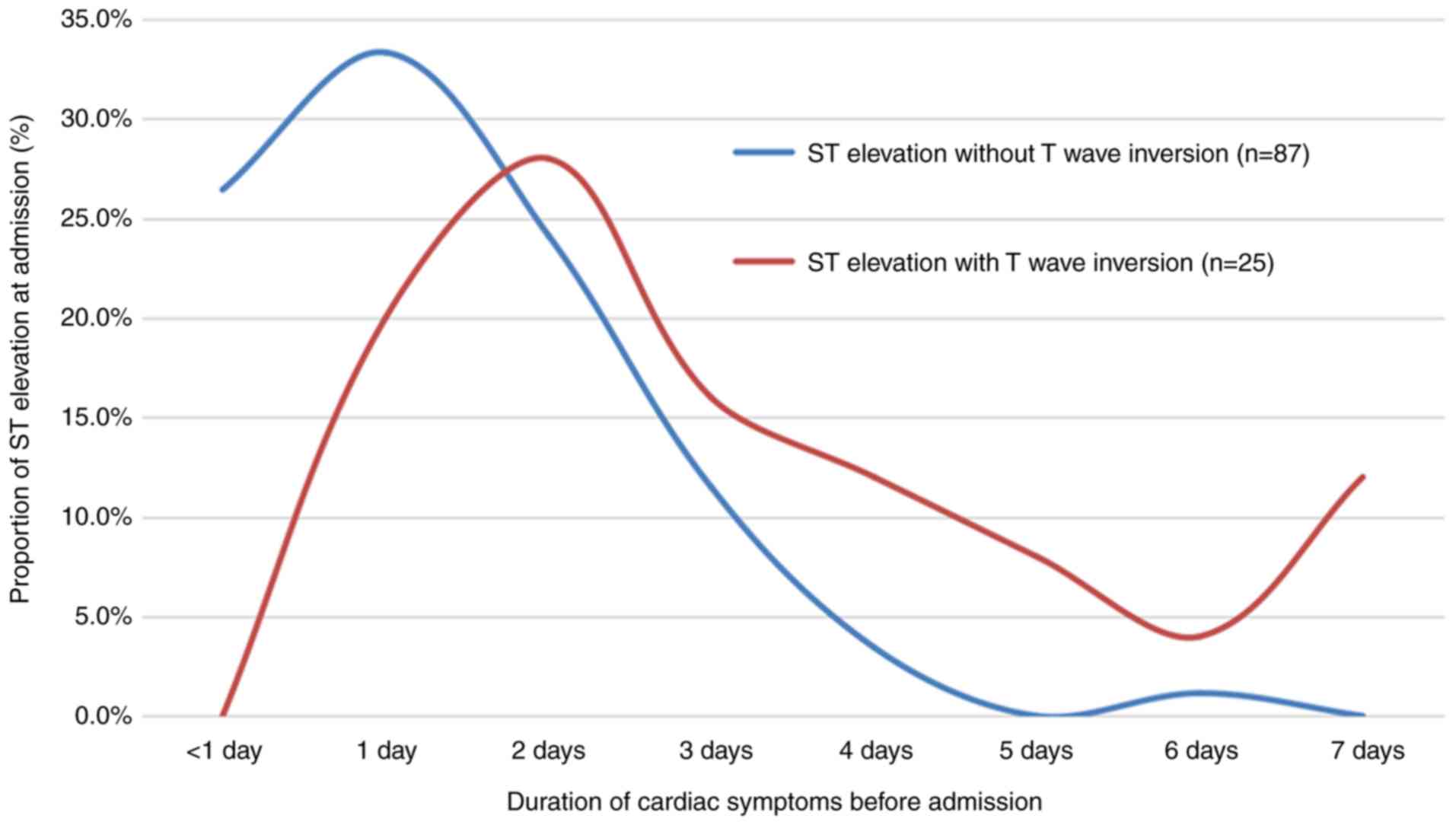
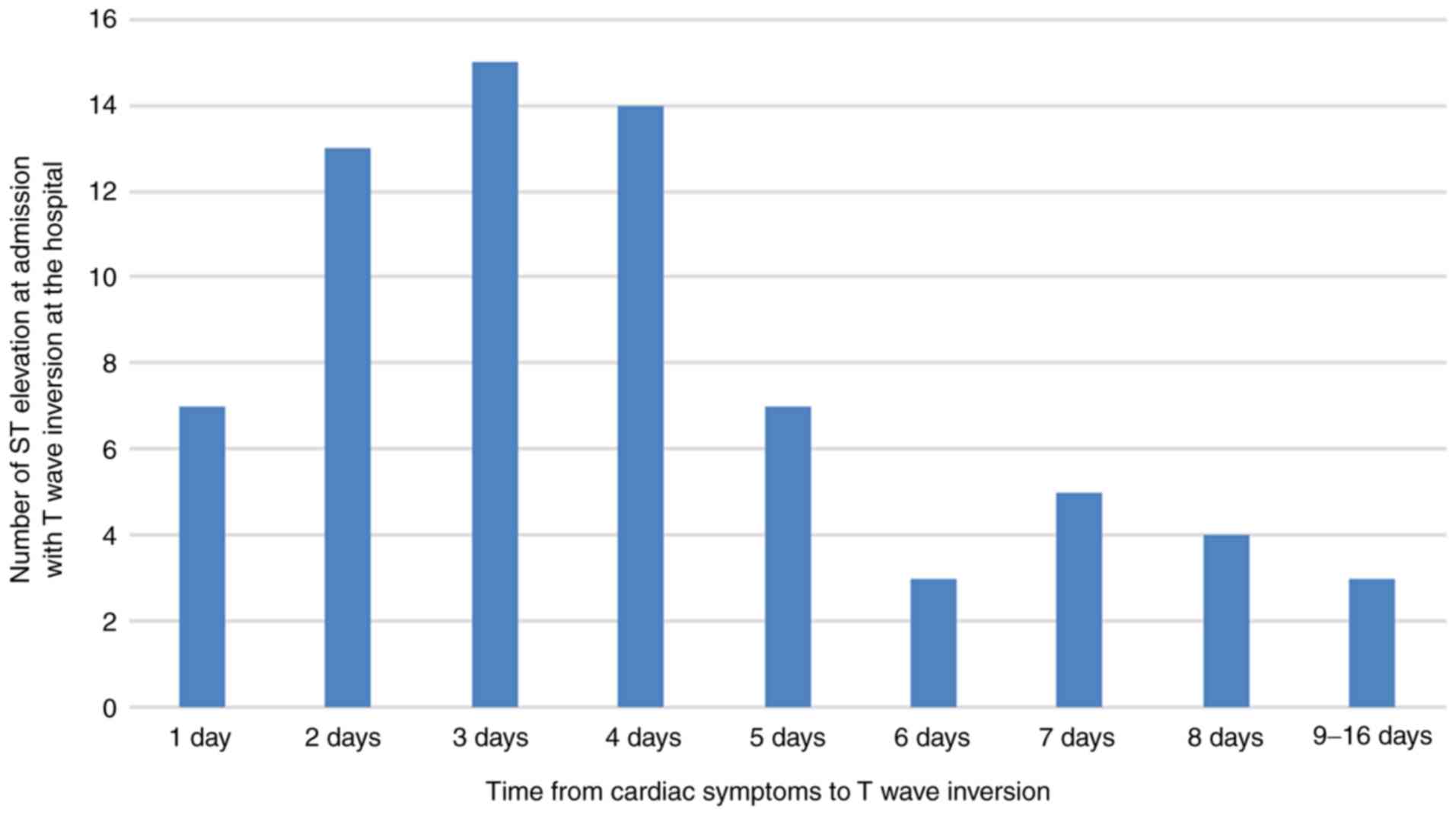
Investigation of patients presenting
with ST elevation at admission
Of the 121 cases with ST elevation (of which 5 cases
had reciprocal ST depression), 112 cases displayed ST elevation at
admission (of which 3 cases had reciprocal ST depression). Of
these, 87 had ST elevation without T-wave inversion and the median
duration of cardiac symptoms prior to admission was 1.5 days
(range, 0.1-6.0 days). A total of 25 patients had ST elevation with
T-wave inversion and the median duration of cardiac symptoms prior
to admission was 3.1 days (range, 1.0-7.0 days). ST elevation
without T-wave inversion was associated with a shorter duration of
cardiac symptoms (median value, 1.5 vs. 3.1 days; P<0.001)
compared with ST elevation with T wave inversion (Fig. 2; Table
SIII). Of the 87 patients with ST elevation without T-wave
inversion at admission, 71 patients (81.6%) had T-wave inversions
at the hospital. The median time from the onset of cardiac symptoms
to T-wave inversion was 4.0 days (range, 1.0-16.0 days; Fig. 3). The ECG changes in the evolution
from ST elevation at admission to T-wave inversion of a 14-year-old
male patient are presented in Fig.
4.
 | Figure 4Evolution from ST elevation at
admission to T-wave inversion in a 14-year-old male patient. (A)
ECG on admission indicated ST elevation in leads I, II, avF and
V4-V6 (arrow) (0.5 days from the onset of cardiac symptoms). (B) At
one day after admission, the ST elevation (arrow) on ECG was higher
compared with that on the previous ECG. (C) On the second day after
admission, the ECG exhibited a slight inversion of T-waves in leads
II, III, avF and V5-V6 (triangle), and the ST elevation was lower
compared with that in the previous ECG. (D) On the third day after
admission, the ECG indicated an obvious inversion of T-waves in
leads II, III, avF and V4-V6 (triangle), and the ST elevation was
lower compared with that in the previous ECG. In addition, the ST
elevation in leads III and avF had almost disappeared (arrow). ECG,
electrocardiogram. |
Discussion
Acute myocarditis, a common, easily misdiagnosed
disease with a high mortality rate, is defined as an inflammatory
infiltrate of the myocardium with necrosis and degeneration of
adjacent myocytes as a result of viral infections, autoimmune
diseases or cardiotoxic agents (1,2). Since
myocarditis has a highly variable clinical presentation, ranging
from mild symptoms to severe heart failure associated with the
transition of ECG changes to fatal arrhythmia, the evaluation of
patients with myocarditis is a key clinical dilemma (2,3,19). ECG
is a non-invasive, quick, safe and widely used screening tool that
has a crucial role in diagnostics and differential diagnostics,
assessments of severity, determinations of patient prognosis and
analyses of the disease course. To the best of our knowledge, the
present case series of 274 patients is the largest study to date
describing ECG findings for acute myocarditis, ECG findings
associated with FM and the characteristics of ST elevation at
admission. In patients with myocarditis, the occurrence rate of ECG
changes ranges from 88.2 to 100%, and various ECG abnormalities may
exist (4-6,15).
In the present study, univariate analysis demonstrated that 12 ECG
parameters were associated with FM. Furthermore, multivariate
logistic regression analysis revealed that 5 of these factors were
independent predictive factors for FM. These independent predictive
factors were VT, high-degree AVB, sinus tachycardia, low voltage
and QRS duration of ≥120 msec.
VT is a common tachyarrhythmia that frequently
occurs in viral myocarditis (19).
The present study indicated that VT accounted for 6.2% and was an
independent predictive factor of FM. Miyake et al (5) demonstrated that arrhythmias (70% VF)
were associated with FM and poor outcomes. This was in accordance
with the present study. The mechanisms underlying arrhythmias may
be associated with transient inflammatory-cell infiltration of the
myocardium, oedema of myocardial cells and the intramyocardial
cellular space, myocardial fibrosis, ion-channel dysfunction and
ischemia (5,11,19).
Sinus tachycardia was the most common arrhythmia, a typical finding
of tachyarrhythmias (11). In the
present study, sinus tachycardia, accounting for 26.3%, was also an
independent predictive factor of FM. Cardiogenic shock, occurring
in 71/77 of FM cases in the present study, was the most common
symptom of FM, which may explain why sinus tachycardia is an
independent predictive factor.
High-degree AVB/complete AVB, with an incidence
ranging from 1.1 to 14.8%, has been associated with the severity of
the disease, which is similar to the results of the present study
(6,7,14). The
present study indicated that high-degree AVB was an independent
predictive factor of FM and the incidence rate of CA (7.2 vs.
28.1%; P=0.001) was different between patients with non-AVB and
high-degree AVB. This result was higher compared with the incidence
rate of CA determined by Ogunbayo et al (7), who reported a difference between
patients with non-heart block and high-degree AVB (CA incidence of
1.7 vs. 17.4%, respectively; P<0.001). In addition, the present
study indicated that 6 patients had both non-advanced AVB and
high-degree AVB, which indicated that high-degree AVB and
non-advanced AVB may be present in parallel as the disease
progresses. In 27 cases of CA, the initial rhythm was shockable
(VT/VF) in 21 patients (77.8%). Similarly, according to recent
guidelines, AMI-induced CA also has a high rate of shockable
rhythms as the first rhythms (19).
Survival statistics appear to be better when the first rhythms are
identified as shockable compared with pulseless electrical activity
or asystole (20). For secondary
prevention, the 2017 guidelines recommend that an implantable
cardioverter defibrillator is mandatory after VF or VT that is not
due to reversible causes (19).
Pavlicek et al (21)
revealed that half of patients with suspected myocarditis
experienced VF or VT after implantable cardioverter defibrillator
therapy.
Low voltage is a common ECG abnormality in
myocarditis and is associated with the severity of the disease.
Casadonte et al (14)
examined paediatric patients with FM and indicated that low voltage
was present in 16 of 27 patients. Lee et al (6) studied patients with histologically
confirmed lymphocytic myocarditis and indicated that low voltage
was present in 28 of 35 patients. Miyake et al (5) studied patients ≤21 years hospitalized
with acute myocarditis between 1996 and 2012 and demonstrated that
low voltage, detected in 81 of 85 patients, was associated with the
occurrence of clinically significant arrhythmias. In the large
cohort of patients in the present study, low voltage was present in
44 of 274 patients and was associated with FM. The multivariate
analysis further verified that low voltage was an independent
predictive factor of FM. Although low voltage is frequently
encountered in myocarditis, the pathophysiology remains elusive.
Myocardial oedema may be an explanation for low voltage (5). Furthermore, the present study
suggested that a QRS duration of ≥120 msec (including left BBB,
right BBB and intraventricular block) was an independent predictive
factor of FM. Ukena et al (8) studied patients with clinically
suspected acute myocarditis between 1995 and 2009 and determined
that a QRS duration of ≥120 msec (left BBB, right BBB and
indeterminate BBB) was an independent predictor of cardiac death or
heart transplantation. Morgera et al (22) indicated that adult myocarditis
presenting with left BBB was associated with unfavourable outcome.
Miyake et al (5) suggested
that in paediatric myocarditis, left BBB increased the risk of poor
outcome by 7.8-fold. These results suggested that QRS prolongation
was an independent factor for predicting poor outcomes, which was
corroborated by the results of the present study.
As mentioned above, ECG has a key role in the
assessment of severity. Of note, UCG, whose diagnostic criteria
have been suggested and adopted for myocarditis patients, may also
be used to distinguish FM from myocarditis (23,24).
In the near future, the role of UCG in myocarditis patients we be
further studied. Generally speaking, compared with UCG assessment,
ECG is more rapid, timely and convenient. The ECG may detect
certain dynamic changes over time, which are meaningful and helpful
in guiding treatments, including cardioversion, defibrillation and
pacemaker implantation.
Undoubtedly, T-wave inversion and ST elevation are
the most common and the most widely studied ECG changes in
myocarditis, both of which are types of ST-T-wave changes (2,5,14,15).
The present study suggested that T-wave inversion (48.2%) was not
associated with FM, which was similar to the results of the study
by Ukena et al (8), which
indicated that T-wave inversion, documented in one-third of all
patients, was the most frequently observed ECG abnormality and was
not predictive of cardiac death or heart transplantation. Most of
the patients with myocarditis presented with ST elevation in
partial leads, mimicking ECG alterations caused by AMI (4). Due to the lack of a relevant
systematic study, differentiating between myocarditis and AMI
presents a clinical dilemma (1). In
a small study of 11 cases of myocarditis, Nakashima et al
(4) observed ST elevation in 8
patients, of which only one exhibited reciprocal ST depression.
These results are in line with the present findings, which are
based on a larger cohort of patients. The present study indicated
that 121 patients presented with ST elevation (of which 5 patients
had reciprocal ST depression), and 112 patients displayed ST
elevation at admission (of which 3 patients had reciprocal ST
depression). Therefore, it is generally accepted that in a young
patient with flu-like prodrome, ST elevation without reciprocal ST
depression may be used to distinguish AMI to avoid unreasonable
treatments (1,4). Furthermore, the present study
indicated that the FM group had significantly higher ST elevation
compared with the non-FM group. However, multivariate analysis did
not reveal that ST elevation was an independent predictive factor.
Miyake et al (5) suggested
that ST segment changes in ECG substantially increased the risk by
raising subacute arrhythmias. Nakashima et al (4) mentioned that severe inflammatory
changes in the myocardium and/or pericardial involvement may
contribute to ST elevation. ST segment changes may reflect ongoing
myocardial oedema that leads to worsening of cell membrane leakage,
the accumulation of bioproducts and a decrease in energy delivery
and oxygenation of myocardial tissue (5).
Of note, ST-T-wave changes in patients with
myocarditis evolve as the disease progresses. Certain patients with
ST elevation return to normal over several days, while others
progress further to T-wave inversion (11). The present study indicated that of
87 patients with ST elevation without T-wave inversions at
admission, 71 (81.6%) had T-wave inversions at the hospital. This
rate was higher compared with that determined by Wu et al
(1), who reported on 18 cases of ST
elevation without T-wave inversion at admission, of which 7 cases
had achieved T-wave inversion at discharge. The present results
were in line with the previous observation that the number of leads
with ST elevation, from the acute to the convalescent stage, was
notably decreased and was frequently replaced by negative T waves
(4). In addition, the present study
further indicated that the time of T-wave inversion since the
initial cardiac symptom onset was 4.0 days. Finally, the present
study comprised 25 patients that had ST elevation with T-wave
inversion at admission, not including the 87 patients with ST
elevation without T-wave inversion. ST elevation without T-wave
inversion was associated with a lower duration of cardiac symptoms
compared with ST elevation with T-wave inversion (1.5 vs. 3.1 days;
P<0.001). These data may help to analyse the course of disease
development.
In conclusion, acute myocarditis is a common disease
with high mortality and various dynamic changes in the ECG. ECG
should be widely used to assess disease severity and for the
analysis of the characteristics of ST elevation at admission. The
present data will provide an important reference for managing
patients with suspected myocarditis.
Supplementary Material
Initial ECG recorded during CA. A
total of 27 patients experienced CA. The initial rhythm of 21
patients (77.8%) was a shockable rhythm (VF or pulseless VT). The
initial rhythm of 5 patients (18.5%) was a non-shockable rhythm,
including 3 cases of pulseless electrical activity (11.1%) and 2
cases of asystole (7.4%). The initial rhythm of 1 patient (3.7%)
was unknown. ECG, electrocardiogram; CA, cardiac arrest; VF,
ventricular fibrillation; VT, ventricular tachycardia.
Comparison of general data.
Comparison of the incidence of CA in
AVB patients.
Time distribution of cardiac symptoms
prior to admission for ST elevation on admission.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JC, SC, ZL, WH and YL were involved in the
conception and design of the study. JC, PZ, HW, JS, YN and LL
collected the data. JC, HW and LL analyzed the ECG. JC and YL
drafted the manuscript. JC, PZ, JS, YN and YL analyzed and
interpreted the data and performed the statistical analysis. SC,
ZL, WH and YL were major contributors in writing and revising the
manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the ethics committee of
The First Affiliated Hospital of Wenzhou Medical University
(approval no. KY2020-103) and Wenzhou People's Hospital (approval
no. 2020-96).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wu S, Yang YM, Zhu J, Wan HB, Wang J,
Zhang H and Shao XH: Clinical characteristics and outcomes of
patients with myocarditis mimicking ST-segment elevation myocardial
infarction: Analysis of a case series. Medicine (Baltimore).
96(e6863)2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Caforio AL, Pankuweit S, Arbustini E,
Basso C, Gimeno-Blanes J, Felix SB, Fu M, Heliö T, Heymans S, Jahns
R, et al: Current state of knowledge on aetiology, diagnosis,
management, and therapy of myocarditis: A position statement of the
European society of cardiology working group on myocardial and
pericardial diseases. Eur Heart J. 34:2636–2648, 2648a-2648d.
2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Biesbroek PS, Beek AM, Germans T, Niessen
HW and van Rossum AC: Diagnosis of myocarditis: Current state and
future perspectives. Int J Cardiol. 191:211–219. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Nakashima H, Honda Y and Katayama T:
Serial electrocardiographic findings in acute myocarditis. Intern
Med. 33:659–666. 1994.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Miyake CY, Teele SA, Chen L, Motonaga KS,
Dubin AM, Balasubramanian S, Balise RR, Rosenthal DN, Alexander ME,
Walsh EP and Mah DY: In-hospital arrhythmia development and
outcomes in pediatric patients with acute myocarditis. Am J
Cardiol. 113:535–540. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lee KJ, McCrindle BW, Bohn DJ, Wilson GJ,
Taylor GP, Freedom RM, Smallhorn JF and Benson LN: Clinical
outcomes of acute myocarditis in childhood. Heart. 82:226–233.
1999.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ogunbayo GO, Elayi SC, Ha LD, Olorunfemi
O, Elbadawi A, Saheed D and Sorrell VL: Outcomes of heart block in
myocarditis: A review of 31,760 Patients. Heart Lung Circ.
28:272–276. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ukena C, Mahfoud F, Kindermann I, Kandolf
R, Kindermann M and Bohm M: Prognostic electrocardiographic
parameters in patients with suspected myocarditis. Eur J Heart
Fail. 13:398–405. 2011.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Veronese G, Ammirati E, Cipriani M and
Frigerio M: Fulminant myocarditis: Characteristics, treatment, and
outcomes. Anatol J Cardiol. 19:279–286. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
JCS Joint Working Group. Guidelines for
diagnosis and treatment of myocarditis (JCS 2009): Digest version.
Circ J. 75:734–743. 2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Baksi AJ, Kanaganayagam GS and Prasad SK:
Arrhythmias in viral myocarditis and pericarditis. Card
Electrophysiol Clin. 7:269–281. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ichikawa R, Sumitomo N, Komori A, Abe Y,
Nakamura T, Fukuhara J, Matsumura M, Miyashita M, Kanamaru H,
Ayusawa M and Mugishima H: The follow-up evaluation of
electrocardiogram and arrhythmias in children with fulminant
myocarditis. Circ J. 75:932–938. 2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Aretz HT, Billingham ME, Edwards WD,
Factor SM, Fallon JT, Fenoglio JJ Jr, Olsen EG and Schoen FJ:
Myocarditis. A histopathologic definition and classification. Am J
Cardiovasc Pathol. 1:3–14. 1987.PubMed/NCBI
|
|
14
|
Casadonte JR, Mazwi ML, Gambetta KE, Palac
HL, McBride ME, Eltayeb OM, Monge MC, Backer CL and Costello JM:
Risk factors for cardiac arrest or mechanical circulatory support
in children with fulminant myocarditis. Pediatr Cardiol.
38:128–134. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ammirati E, Cipriani M, Lilliu M, Sormani
P, Varrenti M, Raineri C, Petrella D, Garascia A, Pedrotti P, Roghi
A, et al: Survival and left ventricular function changes in
fulminant versus nonfulminant acute myocarditis. Circulation.
136:529–545. 2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kligfield P, Gettes LS, Bailey JJ,
Childers R, Deal BJ, Hancock EW, van Herpen G, Kors JA, Macfarlane
P, Mirvis DM, et al: Recommendations for the standardization and
interpretation of the electrocardiogram: Part I: The
electrocardiogram and its technology a scientific statement from
the American heart association electrocardiography and arrhythmias
committee, council on clinical cardiology; the American college of
cardiology foundation; and the heart rhythm society endorsed by the
international society for computerized electrocardiology. J Am Coll
Cardiol. 49:1109–1127. 2007.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lei YL, Chen SQ, Li ZP, Xue JK, Wang TT,
Zhou ZL, Xu HQ, Lu YR, Li HP, Huang WJ and Cheng JT: Percutaneous
coronary intervention improved outcomes of cardiac arrest after
acute myocardial infarction: A 2-year study. Int J Clin Exp Med.
10:3097–3105. 2017.
|
|
18
|
Rautaharju PM, Surawicz B, Gettes LS,
Bailey JJ, Childers R, Deal BJ, Gorgels A, Hancock EW, Josephson M,
Kligfield P, et al: AHA/ACCF/HRS recommendations for the
standardization and interpretation of the electrocardiogram: Part
IV: The ST segment, T and U waves, and the QT interval: a
scientific statement from the American heart association
electrocardiography and arrhythmias committee, council on clinical
cardiology; the american college of cardiology foundation; and the
heart rhythm society. Endorsed by the international society for
computerized electrocardiology. J Am Coll Cardiol. 53:982–991.
2009.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Al-Khatib SM, Stevenson WG, Ackerman MJ,
Bryant WJ, Callans DJ, Curtis AB, Deal BJ, Dickfeld T, Field ME,
Fonarow GC, et al: 2017 AHA/ACC/HRS guideline for management of
patients with ventricular arrhythmias and the prevention of Sudden
cardiac death: A Report of the American college of
cardiology/American heart association task force on clinical
practice guidelines and the heart rhythm society. Circulation.
138:e272–e391. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Myerburg RJ, Halperin H, Egan DA, Boineau
R, Chugh SS, Gillis AM, Goldhaber JI, Lathrop DA, Liu P, Niemann
JT, et al: Pulseless electric activity: Definition, causes,
mechanisms, management, and research priorities for the next
decade: Report from a national heart, lung, and blood institute
workshop. Circulation. 128:2532–2541. 2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Pavlicek V, Kindermann I, Wintrich J,
Mahfoud F, Klingel K, Böhm M and Ukena C: Ventricular arrhythmias
and myocardial inflammation: Long-term follow-up of patients with
suspected myocarditis. Int J Cardiol. 274:132–137. 2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Morgera T, Di Lenarda A, Dreas L,
Pinamonti B, Humar F, Bussani R, Silvestri F, Chersevani D and
Camerini F: Electrocardiography of myocarditis revisited: Clinical
and prognostic significance of electrocardiographic changes. Am
Heart J. 124:455–467. 1992.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Matshela MR: The role of echocardiography
in acute viral myocarditis. Cardiovasc J Afr. 30:239–244.
2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Chang YJ, Hsiao HJ, Hsia SH, Lin JJ, Hwang
MS, Chung HT, Chen CL, Huang YC and Tsai MH: Analysis of clinical
parameters and echocardiography as predictors of fatal pediatric
myocarditis. PLoS One. 14(e0214087)2019.PubMed/NCBI View Article : Google Scholar
|