Introduction
Corneal astigmatism is refractive error that impairs
uncorrected visual acuity (1). A
previous study analyzed 2,156 eyes of 1,317 patients with cataracts
and found that 73.7% of the eyes had corneal astigmatism of ≤1.50 D
and 26.3% had >1.50 D; furthermore, 7.4% of the eyes had ≥3.00 D
(2). Another study reported that
15-29% of patients with cataracts had refractive astigmatism of
>1.50 D (3). Patients cataracts
with corneal astigmatism who receive traditional spherical or
non-spherical monofocal intraocular lenses (IOLs) frequently
require spectacles or additional corneal refractive procedures,
such as photorefractive keratectomy, peripheral corneal relaxing
incisions, or laser in situ keratomileusis (LASIK), to
achieve good visual acuity (4).
However, peripheral corneal relaxing incisions have several latent
disadvantages, such as lack of precision, limited cylinder
correction, overcorrection, regression, wound gape, and varied
healing responses (5). Moreover,
potential complications of photorefractive keratectomy and LASIK
include haze, keratitis, dry eye, regression, overcorrection and
under-correction (6).
With the improved quality of life, cataract surgery
has developed from a procedure for removing the cloudy lens safely
so patients can acquire freedom from glasses and gain excellent
uncorrected visual acuity (7,8). When
patients undergo cataract surgery, implantation of toric IOL is
deemed the most effective choice for correcting corneal astigmatism
and reducing postoperative spectacle dependence (9). Nonetheless, fluctuating or inaccurate
preoperative keratometry (10),
undervaluation of the total astigmatism in IOL power calculations
(11-13),
unexpected surgically induced astigmatism (14), errors of IOL axis position (15), or IOL instability (16) could decrease the curative effect of
toric IOL. The optimal effect of toric IOLs is dependent on the
ability of the surgeon to minimize postoperative refractive error,
in particular astigmatism (17).
There are numerous types of toric IOLs; however,
AcrySof® IQ and TECNIS® toric IOL are most
frequently used in the Department of Opthalmology, First Affiliated
Hospital of Xi'an Jiaotong University. Before cataract surgery,
patients often requires help to select the optimal type of toric
IOL. The objective of the present study was to compare the
postoperative visual acuity, refractive outcome, contrast
sensitivity (CS), rotational stability and satisfaction of patients
with cataracts with corneal astigmatism following implantation of
two types of toric IOLs in a tertiary hospital of northwest China,
and to provide a clinical basis for selecting an appropriate toric
IOL.
Patients and methods
Participants
Clinical data were collected from 30 patients with
cataracts with low to high corneal astigmatism who received
cataract surgery with implantation of an AcrySof IQ (Alcon
Laboratories, Inc.) or TECNIS (Johnson & Johnson Vision;
Johnson & Johnson) toric IOL by the same ophthalmic surgeon at
the First Affiliated Hospital of Xi'an Jiaotong University (Xi'an,
China). The cohort consisted of 19 females and 11 males, with a
mean age of 68.87±16.07 years (range, 21-90 years). Before surgery,
patients were free to select their preferred type of toric IOL and
were assigned to groups based on their choice. In one group,
patients received the AcrySof IQ toric IOL (AcrySof group), and in
the other group, patients received the TECNIS toric IOL (Tecnis
group). The characteristics of these two types of toric IOLs are
shown in Table Ⅰ. The AcrySof IQ IOL cylinder power models include
1.00, 1.50, 2.25, 3.00, 3.75, 4.50, 5.25 and 6.00 D. The Tecnis IOL
cylinder power models include 1.00, 1.50, 2.25, 3.00 and 4.00 D.
Written informed consent was obtained from all patients before
cataract surgery. The study protocol was approved by the Ethics
Committee of the First Affiliated Hospital of Xi'an Jiaotong
University (Xi'an, China). This study was conducted in accordance
with the tenets of the Declaration of Helsinki. The inclusion
criteria were as follows: i) Patients older than 18 years; ii)
visually significant cataract diagnosis; and iii) preoperative
regular corneal astigmatism >0.75 D, with corneal topography of
with-the-rule astigmatism (direction of maximum refractive power,
90±30˚) and against-the-rule astigmatism (direction of maximum
refractive power, 180±30˚). Exclusion criteria included irregular
corneal astigmatism, a history of keratitis, corneal scarring,
prior corneal surgeries and active corneal diseases that could
compromise vision. Furthermore, patients with zonular weakness were
excluded.
Preoperative assessment
In addition to collection of demographic
information, all patients underwent a comprehensive ophthalmologic
examination prior to surgery, including slit-lamp examination,
dilated fundoscopy, measurement of uncorrected and corrected
distance visual acuity (UDVA and CDVA, respectively), manifest
refraction, intraocular pressure, corneal topography (Carl Zeiss
Meditec AG), and IOLMaster 500 partial coherence interferometry
(Carl Zeiss Meditec AG). The decimal values of visual acuity
obtained from the international visual chart at 5 M were converted
into logarithm of the minimum angle of resolution (LogMAR) values.
The required IOL cylinder power and axis placement were calculated
using online calculators from the respective IOL manufacturers. The
AcrySof toric calculator (www.acrysoftoriccalculator.com; v. 3.2.3) was used
with an A-constant of 119.2 for the AcrySof IQ toric IOL. The
TECNIS toric calculator (www.tecnistoriccalc.com; v. 3.28) was used with an
A-constant of 119.3 for the Tecnis toric IOL. In online calculator,
the surgically induced astigmatism was set at 0.50 D on the axis
where the main incision was made.
Operative technique
With the subject seated upright, the surgeon marked
the corneal limbus of the operative eye as reference markings (0
and 180˚) using a slit lamp and a marking pen. The axis marker was
aligned with the corneal reference marks intraoperatively. The
incision and the intended axis of the lens were inked with a
surgical skin marker. Surgery proceeded as in standard cataract
surgery. According to the surgeon's operation habit and experience,
the primary corneal incision was 3-mm at 120˚. The anterior capsule
was opened with a diameter of ~5.5 mm through a continuous-tear
capsulorhexis. After phacoemulsification and cataract removal,
lenses were folded and implanted using conventional instruments.
Once in the capsular bag, the toric IOL was rotated until the axis
indentations of the IOL were aligned with the subject's
intraoperative axis marking. All ophthalmic viscoelastic devices
were completely removed to avoid further rotation of the IOL.
Postoperative assessment
Patients who have undergone surgeries were reviewed
once between 1 month to 4 years postoperatively. Outcome measures
included visual acuities (LogMAR UDVA and CDVA), manifest
refraction (obtained by an optometrist), CS under mesopic, photopic
and mesopic glare at four spatial frequencies (CSV-1000E;
VectorVision, Inc.), slit-lamp examination, dilated fundoscopy,
toric axis using the ‘Toric IOL Rotation Summary’ software with OPD
Scan III workstation (Nidek Co., Ltd.) under mydriasis (1.0%
tropicamide; Santen Pharmaceutical Co., Ltd.), and a subjective
visual quality questionnaire drafted according to a previous study
(18). Rotation of the toric IOL
was evaluated as follows: A clockwise rotation was counted as
positive and counterclockwise rotation as negative.
Subjective visual quality
questionnaire
Patients were asked yes/no questions about spectacle
independence, incidence of postoperative optical or visual
disturbances such as ghosting, glare, difficulty in nighttime
vision, halos, visual distortion, and color vision or depth
perception impairment. Furthermore, patients were asked to evaluate
their satisfaction with visual improvement using a score scale from
0 to 10 at intervals of 1 (score 0, not at all satisfied; score 10,
very satisfied).
Calculation of refractive astigmatism
reduction
The mean percentage of refractive astigmatism
reduction was calculated using the American National Standards
Institute (ANSI) formula (19). The
following equation was used: (Postoperative refractive
cylinder-preoperative keratometric cylinder)/(target refractive
cylinder-preoperative keratometric cylinder) x100%.
Statistical analysis
All statistical analyses were performed using SPSS
for Windows (version 18.0; SPSS, Inc.). Data are presented as the
mean ± standard deviation or as frequencies. The Kolmogorov-Smirnov
test was used to test the normality assumption. To assess the
differences between AcrySof and Tecnis groups, Student's t-test was
applied if the values presented normal distribution, and
Mann-Whitney U test was performed if the values did not present
normal distribution. For a mixture of paired and unpaired data
comparisons, such as visual acuity and refraction, a mixed ANOVA
and simple main effects with Bonferroni correction were used. The
Fisher's exact test was used to analyze the gender distribution of
patients. Chi-square test was used for comparisons of postoperative
categorical variables. P<0.05 was considered to indicate a
statistically significant difference.
Results
Patients demographics and
characteristics
Among the 30 patients (44 eyes) included in the
current study, 18 patients (26 eyes) received the AcrySof IQ toric
IOL SN6AT3-T7 and 12 patients (18 eyes) received the TECNIS toric
IOL ZCT225-400. The collective characteristics and preoperative
clinical data are presented in Table
II. No significant difference was noted between the two
groups.
 | Table IIComparison of patient demographics
and preoperative clinical data between the two groups. |
Table II
Comparison of patient demographics
and preoperative clinical data between the two groups.
| Parameter | Acrysof group | Tecnis group | t
(u) | P-value |
|---|
| Age,
yearsb |
|
Mean ±
SD | 70.6±10.3 | 66.3±22.5 | 108.000 | 1.000 |
|
Range | 48-85 | 21-90 | | |
| Sex, n
(%)a | | | | 0.266 |
|
Female | 13(72) | 6(50) | | |
|
Male | 5(28) | 6(50) | | |
| UDVA,
LogMARb |
|
Mean ±
SD | 0.68±0.25 | 0.63±0.27 | -200.000 | 0.411 |
|
Range | 0.30 to 1.20 | 0.40-1.40 | | |
| CDVA,
LogMARb |
|
Mean ±
SD | 0.36±0.21 | 0.28±0.17 | 193.500 | 0.329 |
|
Range | 0.10-0.92 | 0-0.60 | | |
| Corneal
astigmatism, Db |
|
Mean ±
SD | 2.01±0.44 | 2.27±1.35 | 230.500 | 0.933 |
|
Range | 1.20-2.98 | 0.82-7.27 | | |
| IOL power, D |
|
Spherec | 19.63±6.05 | 21.14±3.53 | -0.947 | 0.349 |
|
Cylinder,
IOL planeb | 2.72±0.69 | 3.13±0.71 | 167.500 | 0.095 |
|
Cylinder,
corneal planeb | 1.88±0.50 | 2.14±0.49 | 187.500 | 0.248 |
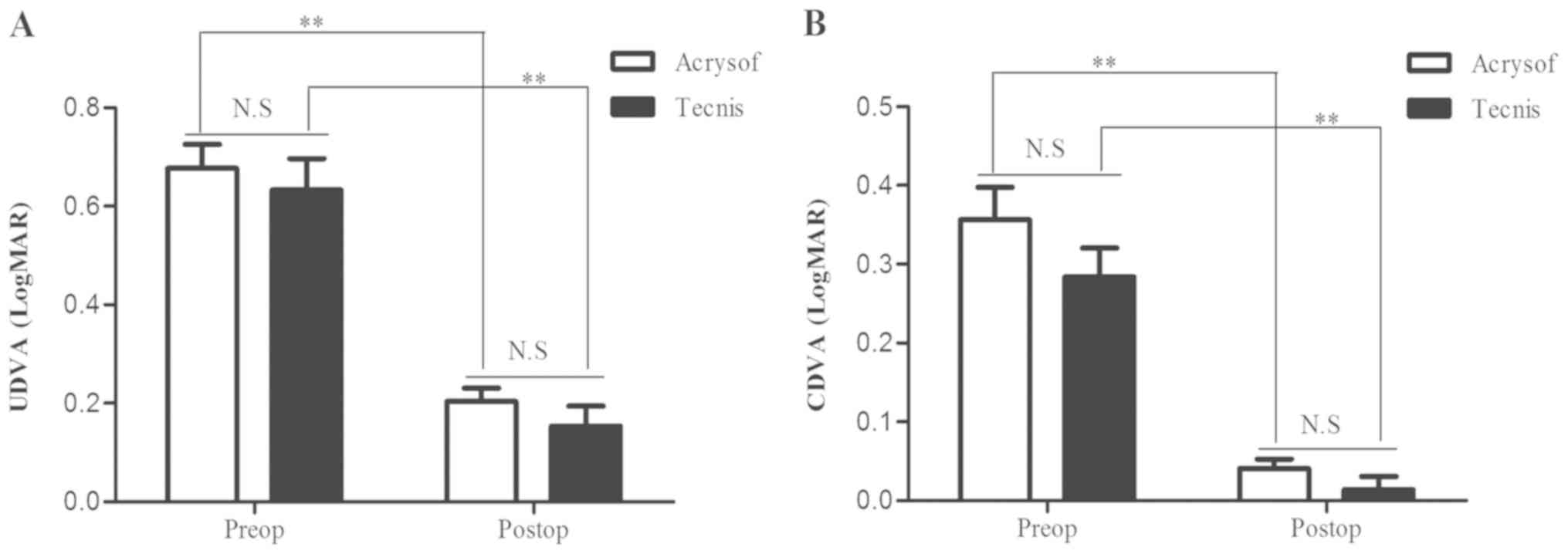
Visual acuity
There were no differences between the two groups in
preoperative UDVA or CDVA (P=0.288 and P=0.116, respectively;
Fig. 1A and B). Toric IOL implantation significantly
improved UDVA (AcrySof group: Preoperative, 0.68±0.25 LogMAR vs.
postoperative, 0.20±0.14 LogMAR, P<0.01; Tecnis group:
Preoperative, 0.63±0.27 LogMAR vs. postoperative, 0.15±0.17 LogMAR,
P<0.01; Fig. 1A) and CDVA
(AcrySof group: Preoperative, 0.36±0.21 LogMAR vs. postoperative,
0.04±0.06 LogMAR, P<0.01; Tecnis group: Preoperative 0.28±0.16
LogMAR vs. postoperative, 0.01±0.07 LogMAR, P<0.01; Fig. 1B). There were no differences between
the two groups in postoperative UDVA or CDVA (P=0.867 and P=0.926,
respectively; Fig. 1A and B). For postoperative mean UDVA, 92 and 83%
of the eyes achieved a value of ≥0.3 LogMAR in the AcrySof and
Tecnis groups, respectively. For postoperative mean CDVA, 100 and
94% of the eyes achieved a value of ≥0.1 LogMAR in the AcrySof and
Tecnis groups, respectively. These results indicated that the
visual effect of both toric IOLs was statistically and clinically
significant.
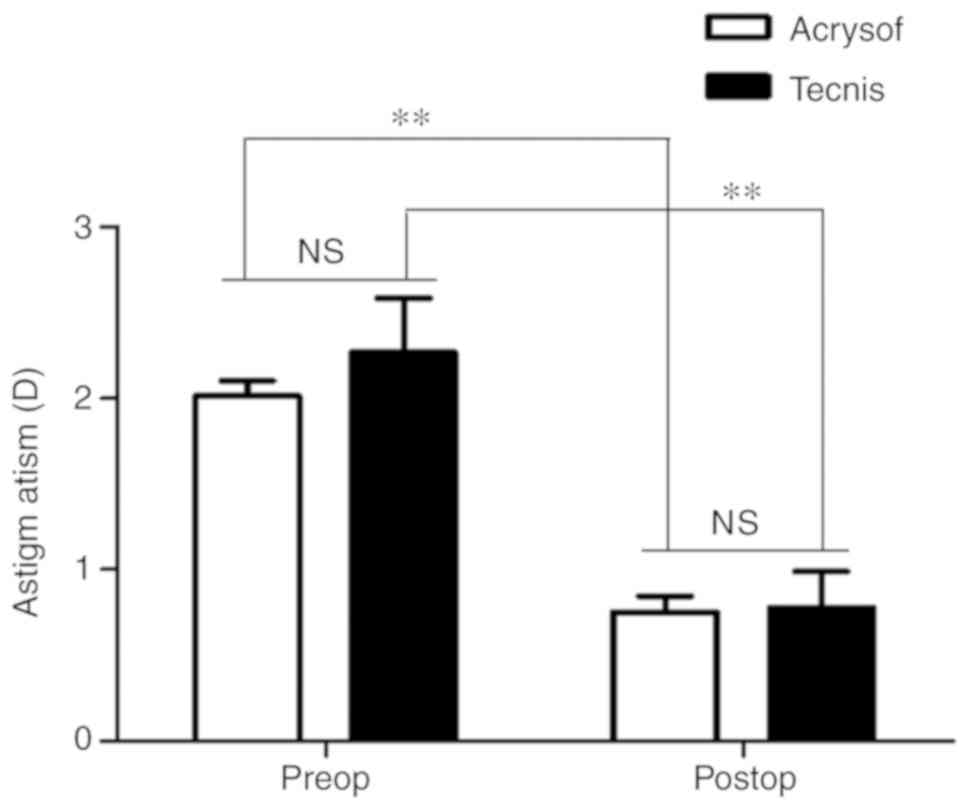
Refraction
No statistically significant between-group
differences were noted in preoperative corneal astigmatism (AcrySof
group, 2.01±0.44 D vs. Tecnis group, 2.27±1.35 D; P=0.381; Fig. 2) and postoperative residual
astigmatism (AcrySof group, 0.75±0.50 D vs. Tecnis group, 0.78±0.90
D; P=0.896; Fig. 2). In both
groups, refractive astigmatism was reduced significantly after a
toric IOL implantation (P<0.01). The median deviation of the
postoperative residual astigmatism from the predicted residual
astigmatism, based on manufactures' IOL calculators, was 0.71 D
with a range of -0.25-1.52 D in the AcrySof group and 0.30 D with a
range of -1.15-1.99 D in the Tecnis group. No significant
difference was noted between the two groups (P=0.23). Postoperative
residual astigmatism was within ±0.50 D of the predicted residual
astigmatism in 12 eyes (46%) in the AcrySof group and 9 eyes (50%)
in the Tecnis group, and within ±1.00 D in 19 eyes (73%) in the
AcrySof group and 14 eyes (78%) in the Tecnis group. According to
the ANSI formula for % refractive astigmatism reduction, in 36 eyes
(21 in the AcrySof group and 15 in the Tecnis group) with >-1.50
D preoperative corneal astigmatism, the mean percentage of
refractive astigmatism reduction was 66.84±27.70% in the Acrysof
group and 76.63±39.12% in the Tecnis group (data not shown).
CS
CS results under mesopic, photopic and mesopic glare
at four spatial frequencies are presented in Table III. There was no statistically
significant between-group difference in CS among the three
illumination conditions at 3, 6, 12 or 18 cycles per degree.
 | Table IIIComparison of postoperative contrast
sensitivity between the AcrySof and Tecnis groups. |
Table III
Comparison of postoperative contrast
sensitivity between the AcrySof and Tecnis groups.
| |
Mean
contrast sensitivity ± SD |
|---|
| | Mesopic | Photopic | Mesopic glare |
|---|
| Parameter SF,
cpd | 3 | 6 | 12 | 18 | 3 | 6 | 12 | 18 | 3 | 6 | 12 | 18 |
|---|
| AcrySof group | 1.61±0.30 | 1.67±0.18 | 1.41±0.46 | 0.87±0.43 | 1.66±0.26 | 1.74±0.25 | 1.31±0.25 | 0.82±0.39 | 1.54±0.28 | 1.65±0.39 | 1.15±0.36 | 0.76±0.37 |
| Tecnis group | 1.64±0.29 | 1.74±0.24 | 1.45±0.43 | 0.95±0.48 | 1.70±0.22 | 1.80±0.24 | 1.41±0.27 | 0.85±0.36 | 1.58±0.30 | 1.67±0.33 | 1.20±0.38 | 0.83±0.38 |
| P-value | 0.862a | 0.209a | 0.776b | 0.656a | 0.720a | 0.510a | 0.120a | 0.762a | 0.685a | 0.864b | 0.665a | 0.501a |
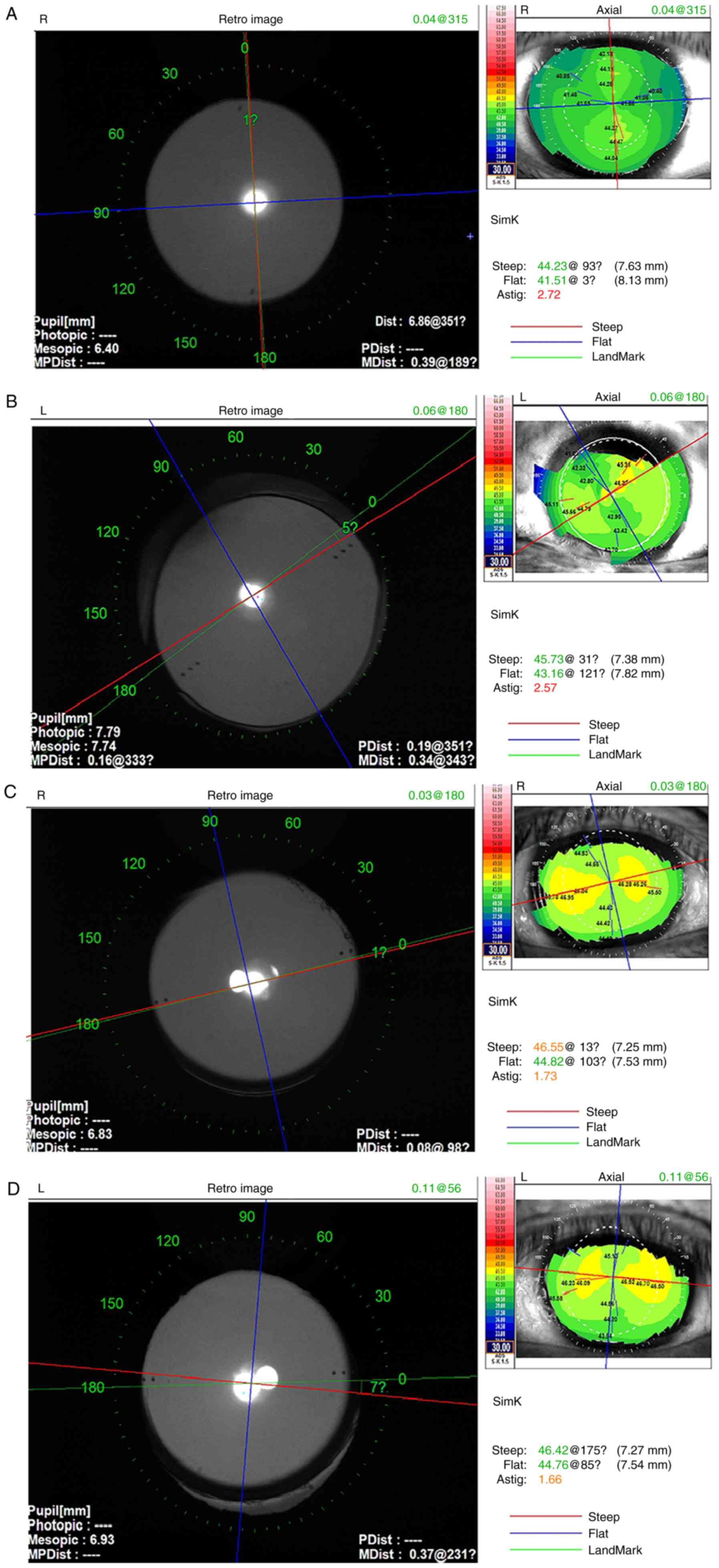
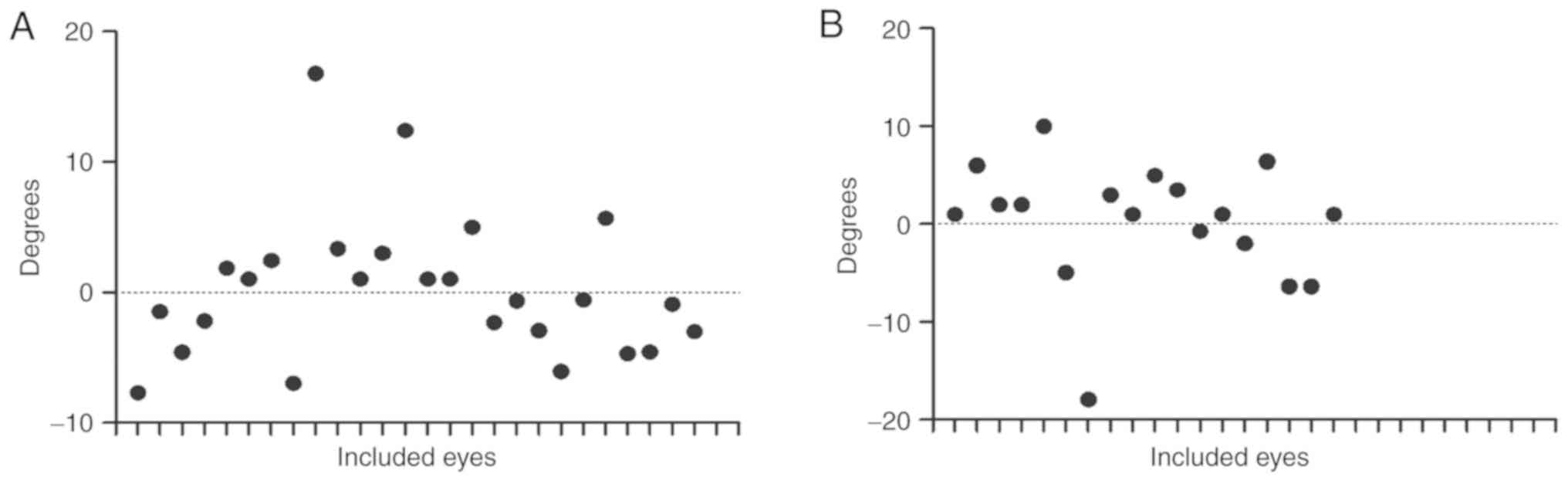
Rotational stability
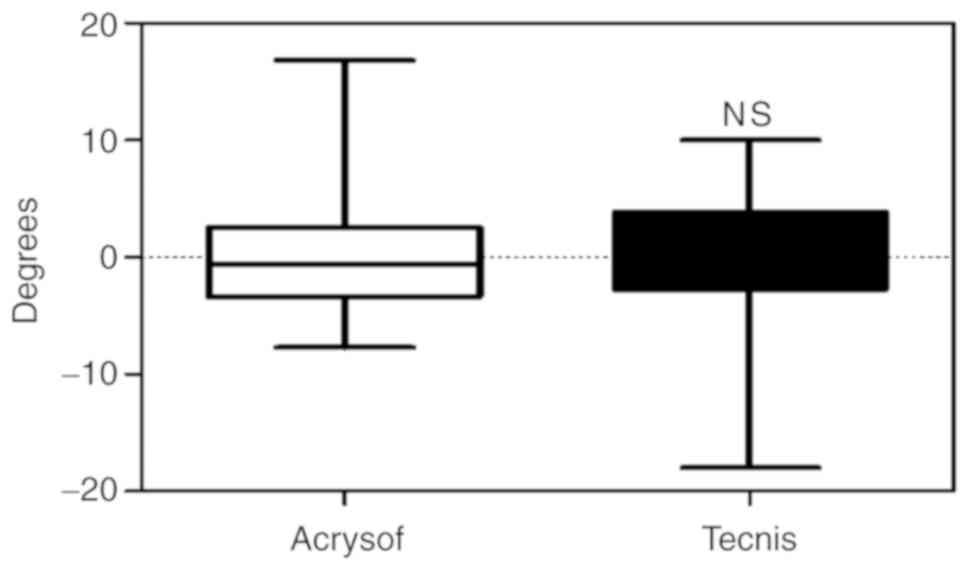
The current study evaluated the toric IOL alignment
using the OPD Scan III workstation (Fig. 3). IOL rotation results are presented
in Fig. 4. The overall mean
deviation of intraocular lens from the target position was
0.22±5.78˚ (range, -18.0 to 16.8˚). The mean deviation of
intraocular lens from the target position was 0.24±5.54˚ (range,
-7.7 to 16.8˚) in the AcrySof group and -0.19±6.28˚ (range, -18.0
to 10˚) in the Tecnis group (Fig.
5). There was no significant difference in IOL axis rotation
between the two groups (P=0.416). The misalignment was within ±5˚
in 32 of 44 eyes (72.7%) and ±10˚ in 41 of 44 eyes (93.2%).
However, significant rotation with >10˚ was found in three eyes,
among which two eyes received an AcrySof and one eye received a
TECNIS toric IOL. One of the AcrySof IQ toric IOL misalignments was
found to have rotated by 16.8˚ at 2 months after the operation,
with a UDVA of 0.20 LogMAR, CDVA of 0.07 LogMAR and no residual
refractive cylinder error. The other Acrysof IQ toric IOL
misalignment was found to have rotated by 12.4˚ at 8 months after
the operation, with a UDVA of 0.30 LogMAR, CDVA of 0.10 LogMAR and
a residual refractive cylinder of -1.75 D. This eye had concomitant
exotropia and had repeatedly undergone intravitreal drug injections
for macular edema resulting from diabetes prior to the operation.
The TECNIS toric IOL misalignment was found to have rotated by
-18.0˚ at 1 week after the operation, with a UDVA of 0.10 LogMAR,
CDVA of 0.00 LogMAR and a residual refractive cylinder of -0.50 D.
IOL repositioning was not performed for these three eyes because
the patients expressed good satisfaction and refused
reoperation.
Visual functioning questionnaire
results
Approximately 66.7% of subjects in the Acrysof group
and 100% of subjects in the Tecnis group reported a degree of
spectacle independence for distance vision. No patients reported
postoperative ghosting, halo, visual distortion, difficulty in
color vision or depth perception in both groups. Only 2 patients
(two eyes) reported slight glare and 4 patients (six eyes) reported
slight difficulty in nighttime vision in the Acrysof group. Three
patients (five eyes) reported slight glare in the Tecnis group.
There were no differences between the two groups in the percentage
of eyes without glare or slight difficulty in nighttime vision
(P=0.170 and P=0.081, respectively). The mean patient satisfaction
score was 8.46±1.21 in the AcrySof group and 8.78±1.44 in the
Tecnis group (P=0.260). Questionnaire results are summarized in
Table IV.
 | Table IVComparison of the results of the
postoperative subjective visual quality questionnaire between the
two groups. |
Table IV
Comparison of the results of the
postoperative subjective visual quality questionnaire between the
two groups.
| Result | AcrySof group | Tecnis group | P-value |
|---|
| No ghosting, % | 100.00 | 100.00 | |
| No glare, % | 92.31 | 72.22 | 0.170a |
| No difficulty in
nighttime vision, % | 76.92 | 100.00 | 0.081a |
| No halo, % | 100.00 | 100.00 | |
| No visual
distortion, % | 100.00 | 100.00 | |
| No difficulty in
color vision, % | 100.00 | 100.00 | |
| No difficulty in
depth vision, % | 100.00 | 100.00 | |
| Patient
satisfaction score | 8.46±1.21 | 8.78±1.44 | 0.260b |
Discussion
The current study indicated that patients with low
to high corneal astigmatism achieved comparable visual outcomes,
refraction correction, CS, rotational stability and satisfaction
after undergoing phacoemulsification with AcrySof and Tecnis toric
IOL implantation. The current study presented data for the
real-world refractive correction and rotational stability of toric
IOLs in a tertiary hospital in northwest China.
Management of corneal astigmatism during cataract
surgery is a routine consideration in modern clinical practice
(20). Published overview data
indicated that AcrySof toric IOL effectively reduced pre-existing
corneal astigmatism, resulting in better UDVA and less spectacle
dependence after surgery (21,22).
Excellent clinical results were obtained in this cohort. No
statistically significant between-group difference was noted in
postoperative UDVA or CDVA. The majority of patients achieved
highly significant UDVA and CDVA improvement. The current results
are consistent with those previously reported for a number of toric
IOLs, including Bi-Flex T, AcrySof, Rayner T-Flex® and
TECNIS (1,4,9,18).
There was no difference between the two groups in postoperative
residual astigmatism. Patients achieved significant correction of
corneal astigmatism in both groups and these results are consistent
with a previous study on AcrySof Toric IOL (23,24).
Waltz et al (19) found a
mean reduction in refractive astigmatism of 76.27±33.09% after the
TECNIS toric IOL implantation at 6 months, which was comparable
with the 76.63±39.12% in the Tecnis group reported in the current
study.
CS represents a useful summary of functional vision
and is a more sensitive index to predict performance impairment
than standard acuity measurements (25). Ninomiya et al (26) found no difference in CS between
different IOL cylinder power models of AcrySof IQ toric IOL. The
current study included a comparative analysis with CS under three
different illumination conditions and found no difference between
the two IOL groups.
Postoperative rotational stability of toric IOL has
a critical effect on the final visual outcome. Postoperative IOL
rotation may be affected by several factors, such as the IOL
material and diameter, design of IOL haptics, partial removal of
viscoelastics from the eye or significant capsule shrinkage after
surgery (27,28). In the present study, the deviation
of intraocular lens rotation from the target position with an
arithmetic mean postoperative misalignment was 0.24±5.54̊ in the
AcrySof group and -0.19±6.28̊ in the Tecnis group. This result
compared favorably with two published trials reporting on
rotational stability of AcrySof toric IOL (mean values, -1.75±2.93̊
and 5.06±4.21̊) (23,29). It can be hypothesized that a
misalignment of <5̊ may be attributed to reference marking
errors on the slit lamp, other than IOL rotation as stated
previously (30). In the current
study, postoperative IOL rotation was comparable between the
AcrySof and Tecnis groups. Overall, the rotational stability was
consistent with good visual and refractive outcomes. Significant
rotation of >10̊ was found in three eyes. In one eye,
significant toric IOL rotation with -1.75 D residual cylinder
appeared to have been associated with concomitant exotropia and
repeated intravitreal drug injections. It has been previously
reported that repeated intravitreal drug injections resulted in
zonular weakness or damage, and lead to significant capsule
shrinkage (31). In the other two
eyes with significant toric IOL rotation, good visual acuity and
low residual cylinder were achieved; therefore, preoperative
measurement or calculation errors of target axis may have caused
the rotation. The current study used toric IOL online calculators
provided by the respective manufacturers for cylinder power and
axis calculation. Nowadays, Barrett Universal II Formula was often
used in studies (32,33).
The current study achieved good satisfaction scores
in subjective visual quality evaluated using a questionnaire in
both groups. Approximately 66.7% of subjects in the AcrySof group
and 100% of subjects in the Tecnis group reported a degree of
spectacle freedom for distance vision. No patient reported issues
with subjective visual symptoms, such as ghosting, halo, visual
distortion, difficulty in color vision and impaired depth
perception. Only five eyes in the Tecnis group and two eyes in the
AcrySof were affected by slight glare. Only 4 patients who received
AcrySof IOLs reported slight difficulty with scotopia, which may
have been caused by blue light filtration. Mainster (34) indicated that blue blocking could
decrease scotopia, and conventional UV-only blocking IOLs provide
higher scotopic sensitivity than blue blocking IOLs. There were no
differences between the two groups in the percentage of eyes
without glare or slight difficulty in nighttime vision, and the
patient satisfaction score was comparable in the two groups.
Finally, there were no adverse events related to the
surgery or IOL during the postoperative follow-up period and
secondary intervention to reposition the toric IOL was not
required. Thus, all toric IOLs used in the current study were safe
for patients with cataracts with corneal astigmatism. The current
retrospective study had certain limitations. First, the number of
cases was relatively small making it difficult to perform analyses
with high statistical power. Second, the postoperative assessment
period ranged from 1 month to 4 years, which may have resulted in
bias. This was performed as it was intended that all clinical data
was collected from patients who underwent cataract surgery with
toric IOL implantation by the same one ophthalmic surgeon. Third,
vector analysis of residual astigmatism to evaluate changes in
refractive astigmatism was not performed in the current study;
however, this will be the subject of future studies. In spite of
these limitations, some conclusions may still be drawn based on
careful consideration of the available data.
In conclusion, patients with cataracts with corneal
astigmatism achieved comparable improvement in visual acuity,
astigmatism correction, CS, rotational stability and satisfaction,
following AcrySof and TECNIS toric IOL implantation in a tertiary
hospital in northwest China. Both toric IOLs appear equally
effective alternatives for patients with cataracts with corneal
astigmatism.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant no. 81740158), Young
Talent Scholar Grant (grant no. 2016KJXX-12) and Clinical Research
Grant from First Affiliated Hospital of Xi'an Jiaotong University
(grant no. XJTU1AF-CRF-2016-014).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LQ and JML conceived and designed the study. JJY
collected and analyzed the clinical data. YZQ analyzed the clinical
data. JJY and JML wrote the paper. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from all
patients before cataract surgery. The study protocol was approved
by the Ethics Committee of the First Affiliated Hospital of Xi'an
Jiaotong University (Xi'an, China). This study was conducted in
accordance with the tenets of the Declaration of Helsinki.
Patient consent for publication
All patients provided written informed consent for
the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bachernegg A, Rückl T, Strohmaier C, Jell
G, Grabner G and Dexl AK: Vector analysis, rotational stability,
and visual outcome after implantation of a new aspheric toric IOL.
J Refract Surg. 31:513–520. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Mohammadi M, Naderan M, Pahlevani R and
Jahanrad A: Prevalence of corneal astigmatism before cataract
surgery. Int Ophthalmol. 36:807–817. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Hoffmann PC and Hutz WW: Analysis of
biometry and prevalence data for corneal astigmatism in 23,239
eyes. J Cataract Refract Surg. 36:1479–1485. 2010.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Holland E, Lane S, Horn JD, Ernest P,
Arleo R and Miller KM: The AcrySof Toric intraocular lens in
subjects with cataracts and corneal astigmatism: A randomized,
subject-masked, parallel-group, 1-year study. Ophthalmology.
117:2104–2111. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Horn JD: Status of toric intraocular
lenses. Curr Opin Ophthalmol. 18:58–61. 2007.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Netto MV, Mohan RR, Ambrosio R Jr,
Hutcheon AE, Zieske JD and Wilson SE: Wound healing in the cornea:
A review of refractive surgery complications and new prospects for
therapy. Cornea. 24:509–522. 2005.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Yang JJ, Liu QP, Li JM and Qin L:
Comparison of visual outcomes with implantation of trifocal versus
bifocal intraocular lens after phacoemulsification: A
Meta-analysis. Int J Ophthalmol. 11:484–492. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Liu J, Zhao J, Ma L, Liu G, Wu D and Zhang
J: Contrast sensitivity and spherical aberration in eyes implanted
with AcrySof IQ and AcrySof Natural intraocular lens: The results
of a meta-analysis. PLoS One. 8(e77860)2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Buscacio ES, Patrao LF and de Moraes HV
Jr: Refractive and quality of vision outcomes with toric IOL
implantation in low astigmatism. J Ophthalmol.
2016(5424713)2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kobashi H, Kamiya K, Igarashi A, Ishii R,
Sato N, Wang G and Shimizu K: Comparison of corneal power, corneal
astigmatism, and axis location in normal eyes obtained from an
autokeratometer and a corneal topographer. J Cataract Refract Surg.
38:648–654. 2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Goggin M, Moore S and Esterman A: Outcome
of toric intraocular lens implantation after adjusting for anterior
chamber depth and intraocular lens sphere equivalent power effects.
Arch Ophthalmol. 129:998–1003. 2011.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Koch DD, Ali SF, Weikert MP, Shirayama M,
Jenkins R and Wang L: Contribution of posterior corneal astigmatism
to total corneal astigmatism. J Cataract Refract Surg.
38:2080–2087. 2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Visser N, Bauer NJ and Nuijts RM: Residual
astigmatism following toric intraocular lens implantation related
to pupil size. J Refract Surg. 28:729–732. 2012.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Berdahl JP and Hardten DR: Residual
astigmatism after toric intraocular lens implantation. J Cataract
Refract Surg. 38:730–732. 2012.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Jin H, Limberger IJ, Ehmer A, Guo H and
Auffarth GU: Impact of axis misalignment of toric intraocular
lenses on refractive outcomes after cataract surgery. J Cataract
Refract Surg. 36:2061–2072. 2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Chang DF: Comparative rotational stability
of single-piece open-loop acrylic and plate-haptic silicone toric
intraocular lenses. J Cataract Refract Surg. 34:1842–1847.
2008.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kohnen T: Astigmatism measurements for
cataract and refractive surgery. J Cataract Refract Surg.
38(2065)2012.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Lubinski W, Kazmierczak B,
Gronkowska-Serafin J and Podboraczynska-Jodko K: Clinical outcomes
after uncomplicated cataract surgery with implantation of the
tecnis toric intraocular lens. J Ophthalmol.
2016(3257217)2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Waltz KL, Featherstone K, Tsai L and
Trentacost D: Clinical outcomes of TECNIS toric intraocular lens
implantation after cataract removal in patients with corneal
astigmatism. Ophthalmology. 122:39–47. 2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Aujla JS, Vincent SJ, White S and
Panchapakesan J: Cataract surgery in eyes with low corneal
astigmatism: Implantation of the Acrysof IQ Toric SN6AT2
intraocular lens. J Ophthalmic Vis Res. 9:324–328. 2014.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Visser N, Bauer NJ and Nuijts RM: Toric
intraocular lenses: Historical overview, patient selection, IOL
calculation, surgical techniques, clinical outcomes, and
complications. J Cataract Refract Surg. 39:624–637. 2013.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Savini G, Hoffer KJ and Ducoli P: A new
slant on toric intraocular lens power calculation. J Refract Surg.
29:348–354. 2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Alio JL, Pinero DP, Tomas J and Aleson A:
Vector analysis of astigmatic changes after cataract surgery with
toric intraocular lens implantation. J Cataract Refract Surg.
37:1038–1049. 2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Visser N, Berendschot TT, Bauer NJ and
Nuijts RM: Vector analysis of corneal and refractive astigmatism
changes following toric pseudophakic and toric phakic IOL
implantation. Invest Ophthalmol Vis Sci. 53:1865–1873.
2012.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Plaza-Puche AB, Alio JL, Sala E and Mojzis
P: Impact of low mesopic contrast sensitivity outcomes in different
types of modern multifocal intraocular lenses. Eur J Ophthalmol.
26:612–617. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ninomiya Y, Minami K, Miyata K, Eguchi S,
Sato R, Okamoto F and Oshika T: Toric intraocular lenses in eyes
with with-the-rule, against-the-rule, and oblique astigmatism:
One-year results. J Cataract Refract Surg. 42:1431–1440.
2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Shah GD, Praveen MR, Vasavada AR, Vasavada
VA, Rampal G and Shastry LR: Rotational stability of a toric
intraocular lens: Influence of axial length and alignment in the
capsular bag. J Cataract Refract Surg. 38:54–59. 2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Pereira FA, Milverton EJ and Coroneo MT:
Miyake-Apple study of the rotational stability of the Acrysof Toric
intraocular lens after experimental eye trauma. Eye (Lond).
24:376–378. 2010.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Visser N, Berendschot TT, Bauer NJ, Jurich
J, Kersting O and Nuijts RM: Accuracy of toric intraocular lens
implantation in cataract and refractive surgery. J Cataract Refract
Surg. 37:1394–1402. 2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Carvalho MJ, Suzuki SH, Freitas LL, Branco
BC, Schor P and Lima AL: Limbal relaxing incisions to correct
corneal astigmatism during phacoemulsification. J Refract Surg.
23:499–504. 2007.PubMed/NCBI
|
|
31
|
Xue K, Jolly JK, Mall SP, Haldar S, Rosen
PH and MacLaren RE: Real-world refractive outcomes of toric
intraocular lens implantation in a United Kingdom National Health
Service setting. BMC Ophthalmol. 18(30)2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Moshirfar M, Buckner B, Ronquillo YC and
Hofstedt D: Biometry in cataract surgery: A review of the current
literature. Curr Opin Ophthalmol. 30:9–12. 2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Rong X, He W, Zhu Q, Qian D, Lu Y and Zhu
X: Intraocular lens power calculation in eyes with extreme myopia:
Comparison of Barrett Universal II, Haigis, and Olsen formulas. J
Cataract Refract Surg. 45:732–737. 2019.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Mainster MA: Violet and blue light
blocking intraocular lenses: Photoprotection versus photoreception.
Br J Ophthalmol. 90:784–792. 2006.PubMed/NCBI View Article : Google Scholar
|