Introduction
Rheumatoid arthritis (RA) is a painful and disabling
polyarticular autoimmune disease (1). In recent decades it has been estimated
that ≤1% of the global population is affected by RA (1). This disease is characterized by
proliferation and inflammation of the synovium, which is the
membrane lining the inner surface of the joint capsule. RA
progression leads to the formation of the pannus, a layer of
fibrovascular or granulation tissue, which causes progressive
degradation of the adjacent articular cartilage, ligaments and bone
(2-6).
The normal synovial lining is 2-4 layers thick. However, in RA, the
synovial lining forms a layer 10-15 cells deep. This tissue is then
infiltrated with macrophages, B cells, mast cells, fibroblast-like
synoviocytes and CD4+ T lymphocytes, which contribute to
synovial inflammation and joint destruction (4,7).
First-line therapy for RA consists of reducing synovial
inflammation and controlling pain, which primarily comprises the
use of medication, such as nonsteroidal anti-inflammatory drugs
(NSAIDs), disease-modifying antirheumatic drugs and oral
corticosteroids (8). Although
various medications are used orally, some joints often remain
refractory to this type of treatment. In general, intra-articular
corticosteroid injections are considered effective an treatment for
inflamed focal synovitis and are widely and conventionally used for
the management of RA joint pain. However, because of possible
negative effects, this type of treatment is controversial. Although
the immediate ameliorating results of local administration are
clear, the long-term effects of corticosteroid injections remain
unknown. In addition, corticosteroids can have adverse effects,
such as allergic reactions, flushing, hyperglycemia,
immunosuppression, menstrual changes and adrenal suppression
(9,10).
Sluijter et al (11) introduced an isothermal
radiofrequency treatment called pulsed radiofrequency (PRF)
stimulation, which can be applied to specific nerves causing
neuropathic pain. It has been suggested that the electric field
rather than the temperature generated by PRF is responsible for the
clinical effects of this treatment (11). Notably, this treatment does not
substantially destroy nerves and tissues. PRF therapy uses a brief
stimulation followed by a long resting phase and exposes the target
tissue to a high electric field around an electrode tip and shaft
without producing sufficient heat to cause structural damage
(11). Due to its minimally
destructive effects on neural tissues, PRF stimulation has been
further developed and rapidly adopted in clinical practice. More
recently, the effectiveness of PRF has encouraged certain
clinicians to use this method in the intra-articular space to
manage arthritic pain (12-14).
Previous studies have reported that applying intra-articular PRF
into the knee joints ameliorates the severity of the disease in
addition to reducing swelling, exudates in joint fluid and damage
to cartilage (12,13). Schianchi et al (14) suggested that intra-articular PRF may
induce significant long-term pain relief in patients with joint
pain. Patients with intractable shoulder, knee, trapezio-metacarpal
and first metatarso-phalangeal joint pain were treated with
intra-articular PRF and the reported success rate appeared to be
high in small joints. However, few clinical studies have
investigated the effects of intra-articular PRF on arthritic pain
(12-14),
and there are no reports on PRF treatment using an animal RA
model.
In the present study, antigen-induced RA was
established in rabbits, as described by Wollheim et al
(15). This method induces
arthritis that manifests in only one joint and exhibits many
histological similarities to RA in humans. The aim of the present
study was to investigate the effects of intra-articular PRF
stimulation on pain-related behavior using motion analysis and
histopathological evaluation in the synovium and cartilage of this
RA rabbit model.
Materials and methods
Animals
New Zealand white rabbits (18; age, 12-weeks;
weight, 2.0-2.5 kg) were provided (Daehan Biolink Co., Ltd.) for
the present study. The rabbits were housed in cages at room
temperature with 40-60% humidity under a 12-h light-dark cycle with
free access to food and water. After adaptive feeding for 1 week,
RA was induced in the rabbits using ovalbumin (OVA) injection, as
described by Wollheim et al (15). Briefly, 20.0 mg/ml OVA solution was
prepared using phosphate-buffered saline at pH 7.4, mixed with
equal volumes of Complete Freund's Adjuvant, and sufficiently
emulsified at 4˚C. An injection of 1.0 ml OVA solution containing
10.0 mg OVA was subcutaneously injected into five areas between the
scapular region of the rabbit, and two additional weekly injections
were likewise administered to strengthen the immune response. RA
was induced on week 5 by injecting 0.5 ml of the OVA solution
containing 5.0 mg OVA into the right articular cavity.
Pulsed radiofrequency administration
procedures
The rabbits were randomly divided into three groups
(n=6 in each group) as follows: i) Intra-articular PRF
administration group; ii) sham stimulation group; and iii)
intra-articular corticosteroid injection group (steroid). Four
weeks after the introduction of RA, the rabbits received either
intra-articular PRF administration, sham stimulation, or a
corticosteroid injection. An intramuscular injection of 15 mg/kg
Zoletil (tiletamine hydrochloride and zolazepam hydrochloride;
Virbac) and 5 mg/kg Rompun (xylazine; Bayer AG) compound was
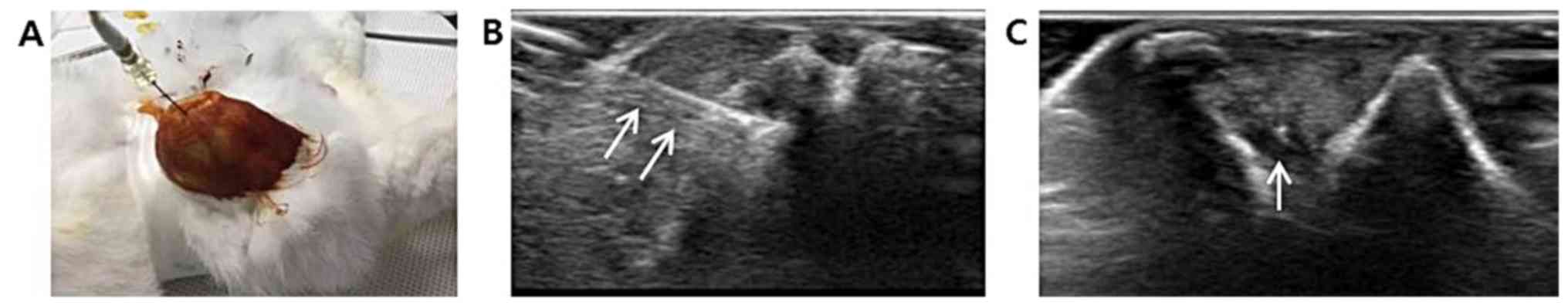
administered to anesthetize the animals (16). PRF was administered by placing an
electrode (Cosman RFG-1A generator and RF Thermocouple Electrode;
500 mm; CoMedical) into the articular cavity of the right knee
using ultrasound guidance with a 5-13 MHZ multifrequency linear
transducer (Antares; Siemens Healthcare), as displayed in Fig. 1. A 5-Hz PRF current was administered
for 120 sec at 45 V. The left knee was used as a control. The
present PRF protocol is based on clinical studies on the
application of intra-articular PRF (14,17).
For rabbits in the sham PRF group, the electrode was placed in
precisely the same manner, with the instrument turned off so that
PRF stimulation was not applied to the articular cavity. In the
steroid group, 1 mg triamcinolone in a 0.1 ml volume was injected
into the articular cavity of the right knee using ultrasound
guidance.
Motion analyses
Rabbits with ovalbumin-induced arthritis received
motion analysis before treatment, then 2, 4 and 8 weeks after
treatment. All animals were allowed to acclimatize in an open space
for 30 min before their movements were analyzed. The rabbits were
then left to move freely in a 3x3 m space for 5 min and their
horizontal movements were recorded using a camera equipped with a
SMART video-tracking observation system (version 3.0.03; Panlab;
Harvard Bioscience, Inc.). The movements were measured using
walking distance, fast walking time and mean walking speed
(18).
Histopathological analysis
To compare the effects of PRF stimulation and the
steroid injection on the RA joint cavity, two rabbits from each
group were sacrificed 2, 4 and 8 weeks after receiving PRF or
steroid treatment. Both the distal femurs and surrounding synovium
were removed and fixed in 4% (w/v) paraformaldehyde for 24 h at
room temperature. The femurs were also decalcified with 10% nitric
acid solution for 24 h at room temperature. The decalcified femur
and synovium that had not undergone the decalcification process
were embedded in paraffin for sectioning at a thickness of 4 µm.
Hematoxylin and eosin (H&E) staining was performed using an
automated slide stainer (Sakura® Tissue-Tek®
DRS™ 2000) for 8 min of hematoxylin and 5 min of eosin
staining at room temperature. For Toluidine blue staining, sections
were equilibrated in 95% alcohol, and then stained with solution of
toluidine blue for 10 min at room temperature. The histological
sections were observed under a light microscope (magnification,
x100 and x200) and a semiquantitative histopathological score for
the distal femurs was assigned according to the method of Cake
et al (19), using a
five-point scale based on structure (0-10), cellularity (0-4),
chondrocyte cloning (0-4), territorial toluidine blue staining
(0-4) and interterritorial toluidine blue staining (0-4). A mean
aggregate score was determined as the average of these values,
ranging between 0 (normal) and 26(19). Additionally, the morphological
parameters of synovitis were assessed using a light microscope
(magnification, x200) according to the method of Krenn et al
(20) as follows: i)
Hyperplasia/enlargement of synovial lining layer; ii) degree of
inflammatory infiltration; and iii) activation of resident
cells/synovial stroma. All parameters were graded as 0 (absent), 1
(slight), 2 (moderate) or 3 (strong positive), and the scores
ranged from 0 (no synovitis) to 9. One blinded pathologist who did
not have any information about the intervention evaluated and
scored the slides.
Statistical analysis
Motion analysis and histopathological data from the
intra-articular PRF, steroid, and sham PRF groups were analyzed
using the Kruskal-Wallis test, followed by Dunn's post hoc test.
Changes in motion analysis according to time, group, and the
combined effect of time/group were analyzed using a univariate
Generalized Linear Model (GLM), and multiple comparisons were
conducted using simple contrast. A medical statistician conducted
data analysis using SPSS version 19.0 (IBM Corp.). All tests were
two-sided and P<0.05 was considered to indicate a statistically
significant difference.
Results
Motion analysis
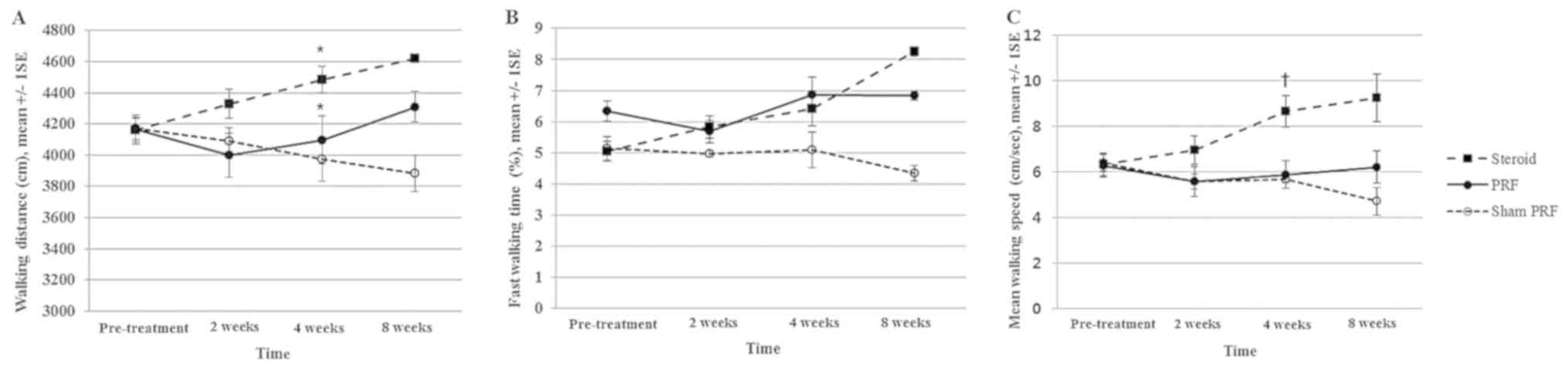
Motion analyses were conducted to assess the effect
of PRF or corticosteroid treatments on movement over time. Analysis
of fast walking time showed significant time effect (P=0.021),
group effect (P<0.001), and group and time interaction
(P=0.003). Analysis of walking distance and mean walking speed
showed no significant time effect (P>0.05). However, there was a
significant group effect (P<0.001) and group and time
interaction (P<0.05) in both walking distance and mean walking
speed. Indeed, walking distance significantly differed in both the
PRF and steroid groups, compared with the sham PRF group 4 weeks
after treatment (P=0.048, PRF vs. sham PRF group; P=0.018, steroid
vs. sham PRF group). In addition, the steroid group exhibited
significantly faster movements, compared with the PRF and sham PRF
groups at 4 weeks (P=0.031, steroid vs. PRF group, P=0.023, steroid
vs. sham PRF group). However, fast walking time at 2, 4 and 8 weeks
after treatment did not differ across the three groups (Fig. 2).
Histopathological analysis
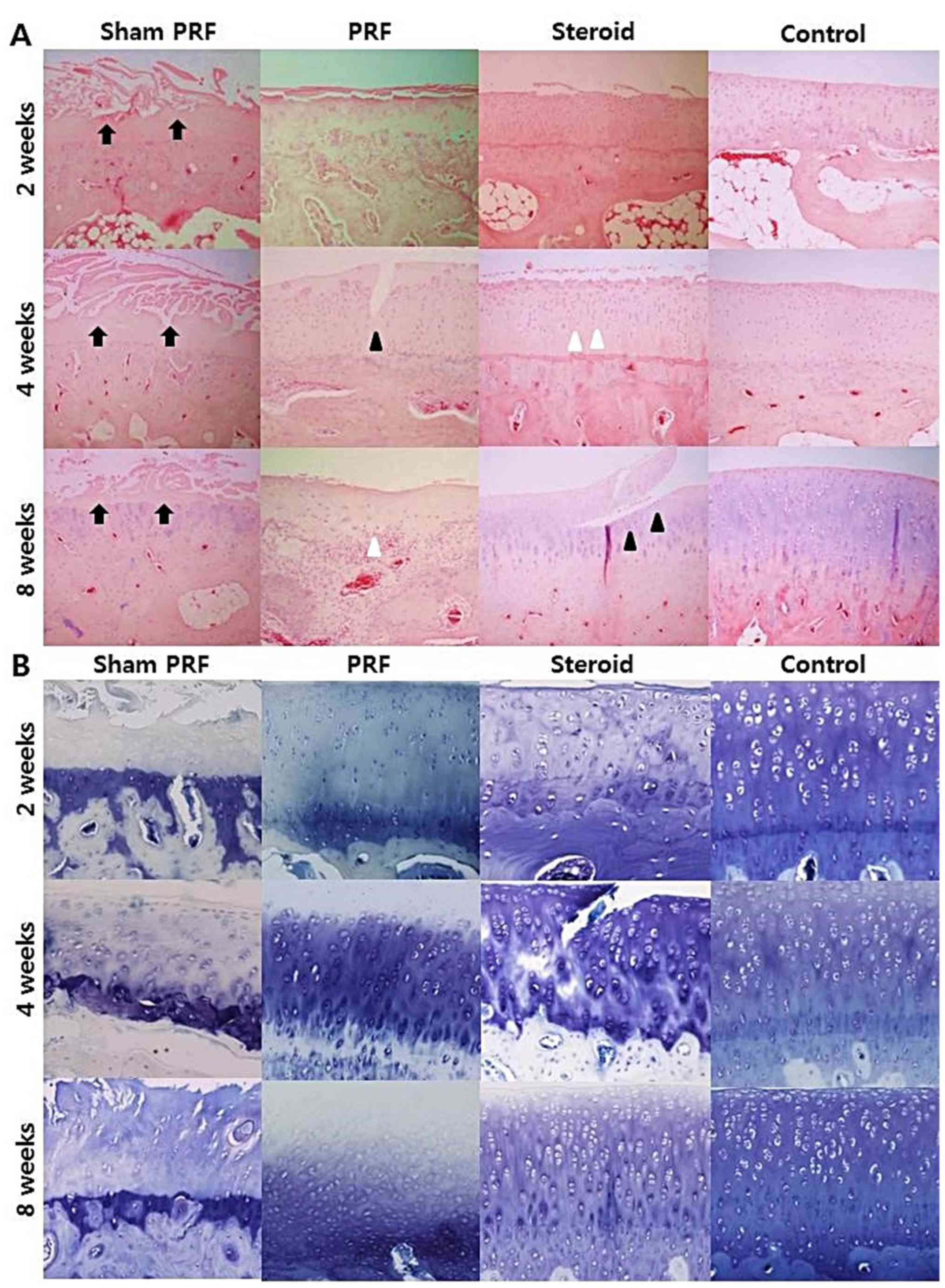
The distal femurs and surrounding synovium were
observed 2, 4 and 8 weeks after treatment. H&E staining of the
distal femurs indicated severe fibrillation and/or erosion of the
cartilage in the sham PRF group. The sham group also displayed a
severe decrease in territorial and interterritorial toluidine blue
staining of the distal femurs, indicating loss of articular
cartilage integrity. In both the PRF and steroid groups, surface
irregularities with clefts of the cartilage were observed (Fig. 3). Histopathological score for the
distal femurs demonstrated significantly lower score at 2 and 4
weeks after treatment in the PRF and steroid groups compared with
in the sham PRF group (P<0.05; Table
I).
 | Table IHistopathological scores for the
distal femurs 2, 4 and 8 weeks after intra-articular PRF
administration, corticosteroid injection (steroid) or sham PRF. |
Table I
Histopathological scores for the
distal femurs 2, 4 and 8 weeks after intra-articular PRF
administration, corticosteroid injection (steroid) or sham PRF.
| | Time |
|---|
| Group | 2 weeks | 4 weeks | 8 weeks |
|---|
| Control | 4.000±0.584 | 4.625±0.519 | 4.458±0.513 |
| Sham PRF |
15.875±1.546a |
16.25±0.968a |
16.750±0.323a |
| PRF |
12.000±2.051a,b |
13.250±1.963a,b |
14.250±1.451a |
| Steroid |
10.375±0.747a,b |
12.250±1.785a,b |
8.125±1.008a-c |
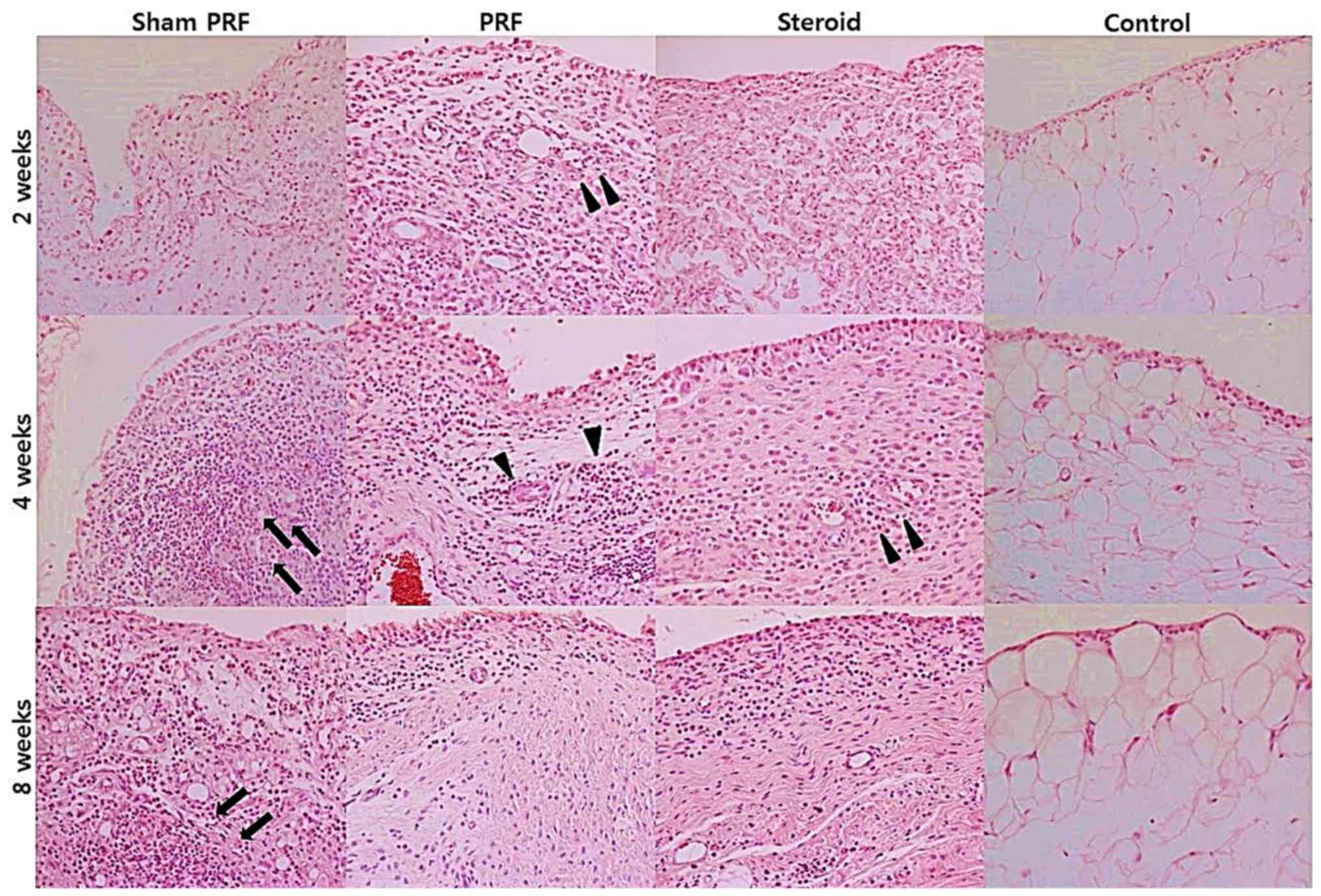
H&E staining of the synovium displayed strong
inflammatory infiltration of lymphatic follicles and/or confluent
subsynovial lymphatic infiltration with hyperplasia of the synovial
cell layer in the sham PRF group. However, inflammatory
infiltration of the synovium was reduced in the PRF and steroid
groups, compared with the sham group (Fig. 4). Histopathological score for the
synovium suggested that the PRF and steroid groups tended to have
lower score for synovitis than the sham PRF group, although the
difference among the three groups was not statistically significant
(Table II).
 | Table IIHistopathological scores for the
synovium 2, 4 and 8 weeks after intra-articular PRF administration,
corticosteroid injection (steroid) or sham PRF. |
Table II
Histopathological scores for the
synovium 2, 4 and 8 weeks after intra-articular PRF administration,
corticosteroid injection (steroid) or sham PRF.
| | Histopathological
score at each timepoint |
|---|
| Group | 2 weeks | 4 weeks | 8 weeks |
|---|
| Control | 1.917±0.664 | 1.333±0.401 | 1.917±0.455 |
| Sham PRF |
5.750±1.250a |
6.500±0.000a | 6.250±0.250 |
| PRF |
4.500±1.000a |
5.250±0.750a | 5.250±1.750 |
| Steroid |
4.500±0.500a |
4.750±0.250a |
3.000±0.500a |
Discussion
The present study suggested that both
intra-articular PRF administration and corticosteroid injection may
improve functional walking distance as well as histopathological
results for the distal femurs in an OVA-induced RA rabbit
model.
RA is a common systemic autoimmune disease that
causes chronic inflammation in the joints and other organs,
particularly in the synovial membranes and articular structures
(1). RA pathogenesis typically
involves excess synovial fluid, synovial cell hyperplasia and
formation of a pannus, which can eventually damage the articular
cartilage and cause joint deformities (5,6).
Previous studies have suggested that RA is partly the result of
inflammation within the joint that results in high levels of
proinflammatory cytokines (21,22).
Thus, RA treatment strategies usually include the use of
anti-inflammatory drugs directed at cytokines to prevent the
progression of structural changes within the joint. Although
various oral medications are used, focal joint edema often occurs,
which causes a painful condition in patients with RA. In general,
corticosteroids suppress various inflammatory cytokines and
chemokines, and intra-articular corticosteroid injections are
commonly administered to patients with RA-related pain.
Previous studies have indicated that intra-articular
triamcinolone hexacetonide is effective in reducing synovitis
(15) and joint destruction
(23) in antigen-induced arthritis.
The present study also used an antigen-induced arthritis animal
model of mono-articular disease that affects only the injected
joints. Histopathological findings in this model exhibit
similarities to RA in humans, including synovial hyperplasia,
inflammatory infiltration of lymphatic follicles, pannus formation
and cartilage erosion (24). In the
present study, histopathological features were improved in rabbits
treated with corticosteroids. Nevertheless, the effect of
corticosteroid treatment for RA remains controversial. Although
local corticosteroid treatment has a marked and immediate
ameliorating effect, repeated corticosteroid injections can result
in severe complications, such as septic arthritis (25,26).
Considering the side effects observed with corticosteroid
treatment, the aim of the present study was to determine the
effectiveness of intra-articular PRF administration in RA joints.
The findings of the present study were not notable enough to
consider PRF clearly superior to steroid treatment, since no
significant intergroup difference was determined based on
histopathological scoring of the distal femur 2 and 4 weeks after
treat ment. However, the PRF group displayed improved motion and
histopathological findings for the distal femur, compared with the
sham PRF group.
PRF has initially been used as an alternative to
continuous RF for the treatment of peripheral nerves causing
neuropathic pain (27-29).
Although the mechanisms underlying the effects of PRF stimulation
have not been fully elucidated, it has been suggested that the
electrical field produced by PRF can alter pain signals (30,31).
Van Zundert et al (30)
revealed that c-fos immunoreactive neurons were increased in the
superficial laminae of the spinal dorsal horn after PRF
administration to the dorsal root ganglion. Hagiwara et al
(31) demonstrated that PRF may
actually enhance the descending noradrenergic and serotonergic
inhibitor pathway, which are involved in the neuropathic pain. Due
to its advantages as a minimally neurodestructive approach, PRF is
also used for other types of pain, in addition to neuropathic pain.
For instance, it has been reported that PRF treatment can
effectively relieve discomfort from painful joints if the needle is
placed within the joint (12-14,17,32).
The present study also indicated an improving trend in pain-related
behavior following intra-articular PRF administration, compared
with the sham PRF group. In particular, there was a significant
increase in walking distance at 4 weeks after PRF administration,
compared with the sham PRF group. It was hypothesized that this
difference may be caused by the effect of PRF on the nervous
system. Indeed, joints are innervated by the peripheral nerve
branches entering the joint capsule. Many simple nerve endings are
located at the attachments of joint capsules and are believed to be
terminals of unmyelinated and thinly myelinated nociceptive axons
(33). Moreover, direct influence
of an electric field can inhibit the excitability of
pain-generating nerves or free nerve endings (14,17,27,28,30).
Erdine et al (34) applied
PRF to the afferent axons of the sciatic nerves of rats and
observed the internal ultrastructural components of axons using
electron microscopy. It was found that the axons showed microscopic
damage after PRF exposure. The damage was more pronounced from the
C-fibers to the Aδ fibers to the Aβ fibers following PRF
administration. This result suggested that PRF might have a more
pronounced effect on smaller pain-carrying fibers (C-fiber and Aδ
fibers), and a lesser effect on larger Aβ fibers mediating
non-pain-related sensations (34).
Thus, it may be suggested that intra-articular PRF could disrupt
the synovial lining nociceptive C-fibers, for instance.
Unlike previous clinical studies, the present study
also investigated the differences in histopathological findings
after intra-articular PRF administration, compared with a sham PRF
group, as well as in rabbits receiving corticosteroid treatment.
The histopathological findings demonstrated a significant decrease
in damage to the medial and lateral femoral condyles 2 and 4 weeks
after intra-articular PRF administration or corticosteroid
injection, compared with the sham PRF group. The current findings
supported another possible mechanism of PRF on the immune system
(35,36). The histopathological findings of the
present study suggested decreased damage to the distal femurs.
Although these results were not significant for the synovium, the
microscopic view during the study suggested decreased infiltration
of inflammatory cells into the synovium after treatment in the PRF
and steroid groups compared with the sham PRF group. Although RA
pathogenesis is still poorly understood, activated T cells, B cells
and macrophages invading the joint synovium involved in the
pathogenesis of RA (37). These
inflammatory cells release various proinflammatory cytokines and
mediators, which cause severe tissue damage and secondary
inflammatory injuries in RA (38).
It has been hypothesized that an electric field from a PRF may
affect immune cells, as there are studies that show proinflammatory
cytokines, such as TNFα, are affected by electric fields (35,36).
Fini et al suggested that pulsed electric field delivery
combines a chondrocyte proliferation, matrix synthesis effect and
anti-inflammatory action in osteoarthritis (39). Therefore, the resulting decreased
cytokine levels in the joint microenvironment may, in turn, favor
intrinsic and extrinsic cartilage repair (17).
The limitations of the present study primarily
include the small sample size. Moreover, only the functional and
histopathological manifestations of RA were assessed. To evaluate
pain-related behavior, motion analysis was also conducted, which,
to the best of the authors' knowledge, has not been attempted in
previous studies. Although this analysis allowed adequate
functional assessment of rabbit movements, non-arthritic rabbits
were not included as controls. Moreover, to determine whether PRF
affects the immune system and reduces RA-related inflammation and
cartilage destruction, additional studies involving
immunohistochemical examination are required. Lastly, the lack of
standardized methods for the administration of intra-articular PRF
in rabbits implies that results may have been influenced by the
administration protocol. The present study was designed to apply a
single PRF administration 4 weeks after RA induction. Although the
infiltration of inflammatory cells into the synovium tended to be
decreased in the PRF group compared to the sham PRF group, synovial
hyperplasia was only marginally reduced in the PRF group in
comparison to the sham PRF group. This may suggest that the present
treatment protocol could be modified in order to further improve
the observed effects on synovial hyperplasia.
In conclusion, intra-articular PRF administration
can ameliorate pain-related behavior, delay cartilage destruction
and attenuate synovial inflammation. It is hypothesized that
intra-articular PRF affects the nociceptive nerve fibers of the
synovial lining, inhibits the transfer of pain signals from the
nerves into the joint capsule and reduces the inflammatory response
associated with RA. To the best of the authors' knowledge, the
present study is the first to evaluate the functional and
histopathological effects of intra-articular PRF administration in
a rabbit model of RA. Additional studies involving a larger number
of cases and various PRF administration protocols are required to
address the limitations of the present study.
Acknowledgements
Not applicable.
Funding
The present study was supported by The National
Research Foundation of Korea grant funded by the Korean government
(Ministry of Science and Information and Communications
Technologies; grant no. 2016R1C1B1014185).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HKC conceived the study. HKC, WJS, SGK and WBJ
developed the methodology. SGK analyzed the data. HKC, WJS and WBJ
interpreted the data and drafted the manuscript. HKC and GYP
validated the analysis and reviewed the manuscript. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The present study protocol was approved by the
Animal Research Ethics Committee of Daegu Catholic University
(approval no. DCIAFCR-170131-2-Y).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Alamanos Y and Drosos AA: Epidemiology of
adult rheumatoid arthritis. Autoimmun Rev. 4:130–136.
2005.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Firestein GS: Evolving concepts of
rheumatoid arthritis. Nature. 423:356–361. 2003.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Garnero P, Landewe R, Boers M, Verhoeven
A, Van Der Linden S, Christgau S, Van Der Heijde D, Boonen A and
Geusens P: Association of baseline levels of markers of bone and
cartilage degradation with long-term progression of joint damage in
patients with early rheumatoid arthritis: The COBRA study.
Arthritis Rheum. 46:2847–2856. 2002.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kim KR, Chung TY, Shin H, Son SH, Park KK,
Choi JH and Chung WY: Red ginseng saponin extract attenuates murine
collagen-induced arthritis by reducing pro-inflammatory responses
and matrix metalloproteinase-3 expression. Biol Pharm Bull.
33:604–610. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Rhee DK, Marcelino J, Baker M, Gong Y,
Smits P, Lefebvre V, Jay GD, Stewart M, Wang H, Warman ML and
Carpten JD: The secreted glycoprotein lubricin protects cartilage
surfaces and inhibits synovial cell overgrowth. J Clin Invest.
115:622–631. 2005.PubMed/NCBI View
Article : Google Scholar
|
|
6
|
Cassim B, Shaw OM, Mazur M, Misso NL,
Naran A, Langlands DR, Thompson PJ and Bhoola KD: Kallikreins,
kininogens and kinin receptors on circulating and synovial fluid
neutrophils: Role in kinin generation in rheumatoid arthritis.
Rheumatology (Oxford). 48:490–496. 2009.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Tristano AG: Tyrosine kinases as targets
in rheumatoid arthritis. Int Immunopharmacol. 9:1–9.
2009.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kumar LD, Karthik R, Gayathri N and
Sivasudha T: Advancement in contemporary diagnostic and therapeutic
approaches for rheumatoid arthritis. Biomed Pharmacother. 79:52–61.
2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Manchikanti L: Role of neuraxial steroids
in interventional pain management. Pain Physician. 5:182–199.
2002.PubMed/NCBI
|
|
10
|
Manchikanti L, Boswell MV, Singh V,
Benyamin RM, Fellows B, Abdi S, Buenaventura RM, Conn A, Datta S,
Derby R, et al: Comprehensive evidence-based guidelines for
interventional techniques in the management of chronic spinal pain.
Pain Physician. 12:699–802. 2009.PubMed/NCBI
|
|
11
|
Sluijter ME, Cosman ER, Rittman WB and van
Kleef M: The effects of pulsed radiofrequency fields applied to the
dorsal root ganglion: A preliminary report. Pain Clin. 11:109–117.
1998.
|
|
12
|
Masala S, Fiori R, Raguso M, Morini M,
Calabria E and Simonetti G: Pulse-dose radiofrequency for knee
osteoartrithis. Cardiovasc Intervent Radiol. 37:482–487.
2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Karaman H, Tufek A, Kavak GO, Yildirim ZB,
Uysal E, Celik F and Kaya S: Intra-articularly applied pulsed
radiofrequency can reduce chronic knee pain in patients with
osteoarthritis. J Chin Med Assoc. 74:336–340. 2011.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Schianchi PM, Sluijter ME and Balogh SE:
The treatment of joint pain with intra-articular pulsed
radiofrequency. Anesth Pain Med. 3:250–255. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Wollheim FA, Telhag H, Henricsson A and
Geborek P: Prevention of joint destruction in antigen-induced
arthritis. Clin Immunol Immunopathol. 70:19–21. 1994.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Karasu A, Altug N, Aslan L, Bakir B and
Yuksek N: Evaluation of the anesthetic effects of
xylazine-ketamine, xylazine-tiletamine-zolazepam and
tiletamine-zolazepam using clinical and laboratory parameters in
rabbits. Med Weter. 74:646–652. 2018.
|
|
17
|
Sluijter ME, Teixeira A, Serra V, Balogh S
and Schianchi P: Intra-articular application of pulsed
radiofrequency for arthrogenic pain-report of six cases. Pain
Pract. 8:57–61. 2008.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Park GY, Kwon DR and Lee SC: Regeneration
of full-thickness rotator cuff tendon tear after ultrasound-guided
injection with umbilical cord blood-derived mesenchymal stem cells
in a rabbit model. Stem Cells Transl Med. 4:1344–1351.
2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Cake MA, Read RA, Guillou B and Ghosh P:
Modification of articular cartilage and subchondral bone pathology
in an ovine meniscectomy model of osteoarthritis by avocado and
soya unsaponifiables (ASU). Osteoarthritis Cartilage. 8:404–411.
2000.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Krenn V, Morawietz L, Haupl T, Neidel J,
Petersen I and Konig A: Grading of chronic synovitis-a
histopathological grading system for molecular and diagnostic
pathology. Pathol Res Pract. 198:317–325. 2002.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kastelein RA, Hunter CA and Cua DJ:
Discovery and biology of IL-23 and IL-27: Related but functionally
distinct regulators of inflammation. Annu Rev Immunol. 25:221–242.
2007.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Wilson NJ, Boniface K, Chan JR, McKenzie
BS, Blumenschein WM, Mattson JD, Basham B, Smith K, Chen T, Morel
F, et al: Development, cytokine profile and function of human
interleukin 17-producing helper T cells. Nat Immunol. 8:950–957.
2007.PubMed/NCBI View
Article : Google Scholar
|
|
23
|
Hunneyball IM: Some further effects of
prednisolone and triamcinolone hexacetonide on experimental
arthritis in rabbits. Agents Actions. 11:490–498. 1981.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Choudhary N, Bhatt LK and Prabhavalkar KS:
Experimental animal models for rheumatoid arthritis.
Immunopharmacol Immunotoxicol. 40:193–200. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ostensson A and Geborek P: Septic
arthritis as a non-surgical complication in rheumatoid arthritis:
Relation to disease severity and therapy. Br J Rheumatol. 30:35–38.
1991.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Xing D, Yang Y, Ma X, Ma J, Ma B and Chen
Y: Dose intraarticular steroid injection increase the rate of
infection in subsequent arthroplasty: Grading the evidence through
a meta-analysis. J Orthop Surg Res. 9(107)2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Cho HK, Cho YW, Kim EH, Sluijter ME, Hwang
SJ and Ahn SH: Changes in pain behavior and glial activation in the
spinal dorsal horn after pulsed radiofrequency current
administration to the dorsal root ganglion in a rat model of lumbar
disc herniation: Laboratory investigation. J Neurosurg Spine.
19:256–263. 2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Park HW, Ahn SH, Son JY, Kim SJ, Hwang SJ,
Cho YW and Lee DG: Pulsed radiofrequency application reduced
mechanical hypersensitivity and microglial expression in
neuropathic pain model. Pain Med. 13:1227–1234. 2012.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Choi GS, Ahn SH, Cho YW and Lee DK:
Short-term effects of pulsed radiofrequency on chronic refractory
cervical radicular pain. Ann Rehabil Med. 35:826–832.
2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Van Zundert J, de Louw AJ, Joosten EA,
Kessels AG, Honig W, Dederen PJ, Veening JG, Vles JS and van Kleef
M: Pulsed and continuous radiofrequency current adjacent to the
cervical dorsal root ganglion of the rat induces late cellular
activity in the dorsal horn. Anesthesiology. 102:125–131.
2005.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Hagiwara S, Iwasaka H, Takeshima N and
Noguchi T: Mechanisms of analgesic action of pulsed radiofrequency
on adjuvant-induced pain in the rat: Roles of descending adrenergic
and serotonergic systems. Eur J Pain. 13:249–252. 2009.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Ozyuvaci E, Akyol O, Acikgoz A and
Leblebici H: Intraarticular pulsed mode radiofrequency lesioning of
glenohumeral joint in chronic shoulder pain: 3 cases. Korean J
Pain. 24:239–241. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Chen C, Lu Y, Kallakuri S, Patwardhan A
and Cavanaugh JM: Distribution of A-delta and C-fiber receptors in
the cervical facet joint capsule and their response to stretch. J
Bone Joint Surg Am. 88:1807–1816. 2006.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Erdine S, Bilir A, Cosman ER and Cosman ER
Jr: Ultrastructural changes in axons following exposure to pulsed
radiofrequency fields. Pain Pract. 9:407–417. 2009.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Sluijter ME and Imani F: Evolution and
mode of action of pulsed radiofrequency. Anesth Pain Med.
2:139–141. 2013.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Maretto F, Vennik M, Albers KI and van
Duijn B: TNFα secretion of monocytes exposed to pulsed
radiofrequency treatment: A possible working mechanism of PRF
chronic pain management. Pain Pract. 14:399–404. 2014.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Hu Y, Cheng W, Cai W, Yue Y, Li J and
Zhang P: Advances in research on animal models of rheumatoid
arthritis. Clin Rheumatol. 32:161–165. 2013.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Chun J, Tosun A and Kim YS:
Anti-inflammatory effect of corymbocoumarin from Seseli gummiferum
subsp. corymbosum through suppression of NF-κB signaling pathway
and induction of HO-1 expression in LPS-stimulated RAW 264.7 cells.
Int Immunopharmacol. 31:207–215. 2016.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Fini M, Giavaresi G, Carpi A, Nicolini A,
Setti S and Giardino R: Effects of pulsed electromagnetic fieds on
articular hyaline cartilage: Review of experimental and clinical
studies. Biomed Pharmacother. 59:388–394. 2005.PubMed/NCBI View Article : Google Scholar
|