Introduction
Cerebral venous sinus thrombosis (CVST) is a rare
cause of stroke with various neurological symptoms, accounting for
~1% of strokes (1). The incidence
of CVST is usually underestimated, as its clinical presentation is
non-specific, including headache, hemiparalysis, aphasia, seizures
and even coma (2). Imaging is
crucial for detecting CVST and associated complications accurately,
which may affect the prognosis and the therapeutic approach
(3,4). Regarding the management of CVST,
anticoagulation therapy is generally considered as the standard
treatment. The majority of the cases have a good prognosis with
standard therapy, but there is a subgroup of patients with CVST who
deteriorate rapidly within a short period of time, with a
potentially fatal outcome. It is necessary to detect the signs of
CVST early, administer standard therapy and adjust the therapy in a
timely manner. Severe clinical manifestation, an age of >65
years, intracranial hemorrhage (ICH), underlying malignancy and
deep CVST are associated with higher mortality rates (5). Certain cases of large and extensive
CVST are refractory to standard anticoagulation therapy and develop
venous obstructive congestive ICH (6). Endovascular intra-arterial application
of thrombolytic agents and/or mechanical thrombectomy for
refractory cases or patients with new ICH on anticoagulation have
been described over the last two decades (7). An increasing number of studies support
individualized treatment for such cases with severe CVST, including
endovascular thrombectomy and thrombolysis, particularly for
hemorrhagic thrombosis (8,9). Local contact thrombolytic therapy may
effectively recanalize the thrombosed cortical veins (10). Severe hemorrhagic CVST (SH-CVST) may
rapidly lead to enlargement of the hematoma, severe cerebral edema
and hernia, which endanger the lives of the patients. Thrombi in
the sinuses in SH-CVST must be removed as soon as possible, as they
are life-threatening. Anticoagulation or thrombolytic therapy alone
may lead to further aggravation of the hematoma in those SH-CVST
cases. Stent retriever thrombectomy combined with long-term local
thrombolysis (SRT-LLT) has been used in certain centers for those
refractory cases or patients with new intracranial hemorrhage
(11-13).
However, to date, no studies have reported on SRT-LLT treatment
specifically for SH-CVST. The aim of the present retrospective
study was to specifically evaluate the effectiveness of SRT-LLT in
SH-CVST. The present study retrospectively analyzed 10 patients
with SH-CVST treated at the Qilu Hospital of Shandong University,
who were initially administered anticoagulant alone. Of those
cases, 8 received SRT combined with LLT when the symptoms
deteriorated further. The aim of the present study was to determine
whether individualized treatment with SRT-LLT may be a potential
effective and safe approach for SH-CVST.
Materials and methods
Patients
The protocol of the present study was approved by
the Ethics Committee of Qilu Hospital Affiliated to Shandong
University (Qingdao, China). Patients or authorized relatives were
informed on the risks and benefits of the operation and provided
written informed consent, including consent for the publication of
CT and digital subtraction angiography (DSA) images. A total of 29
patients with CVST (17 females and 12 males) were encountered at
our center (Qilu Hospital of Shandong University, Qingdao, China)
between December 2013 and November 2018, confirmed by magnetic
resonance venography or DSA. Of these 29 patients, 10 had
hemorrhagic CVST. Their clinical characteristics were recorded and
analyzed, including age, sex, presentation, risk factors, Glasgow
Coma Scale (GCS) score, location of ICH, affected venous sinus,
recanalization status, outcome and complications. Systemic heparin
or low-molecular-weight heparin (LMWH) subcutaneous injection was
the first-line treatment for all patients after admission. LMWH
sodium injection (Qilu Pharmaceutical) was usually administered at
100 IU/kg q12h. The heparin was given via intravenous injection
according to the activated clotting time (ACT) if the patient had
already received heparin injection at another hospital or if there
was a low risk of rebleeding. SRT-LLT was performed on patients
when presenting with the following: i) Failure of first-line
anticoagulation; ii) rapid deterioration of consciousness or
neurological impairment; and iii) significant cortical venous
outflow stasis (arterio-venous circulation time >11 sec; venous
phase >5 sec) (14). In the
present study, 8 patients received endovascular SRT-LLT
therapy.
Procedure
Interventional therapy was performed under general
anesthesia. A 6-Fr and a 5-Fr introducer sheath were placed in the
right femoral vein and left femoral artery, respectively. A 5-Fr
catheter was placed in the left internal carotid artery. DSA
revealed the CVST. Arteriovenous outflow of the cerebral
circulation was detected. A 6-Fr guiding catheter was introduced
into the right or left jugular bulb through the femoral vein route.
Through the guiding catheter, a microcatheter was navigated into
the proximal segment of the thrombosis sinus with a 0.0014-in.
microwire. Subsequently, the Solitaire stent was deployed in the
distal part of the thrombosed sinus and the stent was retracted
after 10 min. The manual aspiration was performed with a 50-ml
syringe, avoiding the clot of thrombus dropping through the guiding
catheter during the retraction. The retraction was repeated up to 3
times. Long-term local thrombolysis was performed following
thrombectomy in order to open the venous sinus and thrombosed
cortical veins as much as possible to avoid further
deterioration.
The 5-Fr catheter and left arterial sheath were
removed. After placing an exchange microwire in the distal part of
the thrombosed sinus, the catheters and introducer sheath were
removed. Subsequently, the microcatheter was again passed through
the sinus. An infusion pump was connected to the microcatheter.
Urokinase (UK; 40,000 U/h) was infused for SRT-LLT. The
microcatheter was fixed to the skin. After the procedure, the
patient was returned to the Intensive Care Unit and was monitored
according to the CVST observation protocol, including vital signs,
GCS score and hemorrhage or thrombosis at the puncture sites. CT
review was usually performed the next day after surgery, unless the
condition changed. The duration of thrombolysis was no more than 7
days and was adjusted according to the improvement of the patient's
condition to reduce the risk of thrombosis around the
microcatheter. Oral anticoagulation treatment was administered
after discontinuing local thrombolysis. Over the next 3-12 months,
warfarin was orally administered. The dose of warfarin was adjusted
according to the monitoring results of the international normalized
ratio every 3 days.
Statistical analysis
The GCS scores at discharge were compared with those
on admission by the paired t-test using SPSS v23 (IBM Corp.).
Results
Baseline characteristics
The mean age of the patients was 39 years (range,
23-65 years). A total of 4 patients (50.0%) were females and 4
(50.0%) were males. A total of 5 patients (62.5%) presented with
acute onset (within 7 days), 1 patient (12.5%) presented with
subacute onset (7-14 days) and the remaining 2 patients (25.0%)
with chronic onset (>14 days). Risk factors of CVST were
reported by 7 patients (87.5%), including puerperium in 2 patients
(25.0%), diarrhea prior to onset in 2 (25.0%), dehydration after
strenuous physical activity in 1 (12.5%), infection of the facial
‘dangerous triangle’ area in 1 (12.5%) and coagulopathy of
eosinophilia in 1 patient (12.5%). No identifiable risk factor was
detected in 1 patient (12.5%). The symptoms at onset included
headache, seizures, nausea, emesis, dizziness, papilledema,
unconsciousness and hemiparalysis. CT scan in all patients revealed
intracranial hemorrhage, including lobe hematoma in 4 patients
(50.0%), subarachnoid hemorrhage in 1 patient (12.5%), multiple
hemorrhages in 1 patient (12.5%), subdural hematoma in 1 patient
(12.5%), and basilar ganglion and thalamus hemorrhage in 1 patient
(12.5%). The median GCS score was 7 (interquartile range, 3-10) at
the time of the intervention. Sinus thrombosis was detected in the
transverse sinus (TS) in 5 of 8 (62.5%) cases, superior sagittal
sinus (SSS) in 7 (87.5%), sigmoid sinus (SigS) in 5 (62.5%) and
straight sinus (SS) in 2 (25.0%) cases. In 7 (87.5%) cases, >2
sinuses were involved. The clinical characteristics of the patients
are summarized in Table I.
 | Table IBaseline characteristics and
outcomes. |
Table I
Baseline characteristics and
outcomes.
| Age (years) | Sex | Symptoms | Risk factors | Onset (days) | GCS on admission | Location of ICH | Affected venous
sinus | Anticoagulation
treatment | Recanalization | Complications | GCS at discharge |
|---|
| 49 | F | Headache | Eosinophilia | 30 | 9 | Left frontal
lobe | SSS+SIGS+TS | Heparin | Partial | None | 14 |
| | | Papilledema | | | | | | | | | |
| | | Hemiplegia | | | | | | | | | |
| 41 | M | Headache | Infection | 120 | 10 | Bilateral
subdural | SSS+ISS+SIGS+
SS+TS | Lmwh | Partial | None | 14 |
| 40 | M | Headache | | | | | | | | | |
| | | Hemiplegia | Dehydrate | 3 | 4 | Right temporal
lobe | SSS+TS+SIGS | Lmwh | Complete | None | 15 |
| | |
Unconsciousness | | | | | | | | | |
| 65 | M | Headache | Diarrhea | 7 | 5 | Multiple
hemorrhage | SSS+SIGS+TS | Lmwh | Partial | Rehemorrhagia | 10 |
| | | Epilepsy | | | | | | | | | |
| | |
Unconsciousness | | | | | | | | | |
| 34 | F | Aphasia | Puerperium | 1 | 8 | Left parietal
lobe | SSS+SIGS+TS | Lmwh | Complete | None | 12 |
| | | Hemiplegia | | | | | | | | | |
| 33 | F | Headache | Puerperium | 6 | 10 | Sah | SSS+SS | Heparin | Complete | None | 13 |
| | | Epilepsy | | | | | | | | | |
| | | Hemiplegia | | | | | | | | | |
| 23 | M | Headache | Diarrhea | 3 | 3 | Thalamus
hemorrhage | SS | Lmwh | Complete | None | 15 |
| | |
Unconsciousness | | | | | | | | | |
| 35 | F | Hemiplegia | Unknown | 8 | 7 | Right temporal
lobe | SSS+LV | Lmwh | Partial | Rehemorrhagia | 11 |
| | | Epilepsy | | | | | | | | | |
| | |
Unconsciousness | | | | | | | | | |
| Total | | | | | 7.2±2.7 | | | | | |
13.0±1.8a |
The initial treatment for SH-CVST with
anticoagulation included administration of heparin (3/8; 37.5%) or
LMWH (5/8; 62.5%). Furthermore, 1 patient underwent immediate
craniotomy for hematoma removal and decompression in another
hospital due to severe cerebral hemorrhage and hernia. All 8
patients deteriorated or did not improve following administration
of first-line anticoagulation treatment.
Endovascular SRT-LLT was performed in these cases,
with successful recanalization of the occluded sinus achieved in
all 8 patients; in 4 patients (37.5%), recanalization was complete
immediately after surgery, whereas the remaining 4 patients with
partial recanalization achieved complete recanalization during the
follow-up evaluation 3-6 months later.
No procedural associated complications were observed
in these cases. ICH expanded in 2 patients (25.0%), detected on
post-interventional CT 7 h post-intervention. Decompressive
hemicraniectomy was performed to relieve the increased intracranial
pressure in 1 patient. At the time of discharge, the patient had
markedly improved with moderate neurological restriction [modified
Ranking scale (mRS) score, 2], without any worsening at 6 months
after discharge. In another patient with enlarged hemorrhage, no
increased edema or intraventricular extension occurred. The patient
did not require further evacuation of the hematoma or decompressive
hemicraniectomy, with moderate neurological restriction (mRS 2) at
discharge and recovery 4 months post-discharge. Recurrence was
defined as the presence of clinical and radiological evidence of
re-thrombosis during follow-up after complete or partial
recanalization. There was no recurrence of CVST in the present
cohort. All patients significantly improved or were cured at
discharge, and the GCS scores at discharge had significantly
improved compared with those on admission. Most patients resumed
their normal activities and none deteriorated or died during a
follow-up period of 6 months to 3 years after discharge.
Representative cases
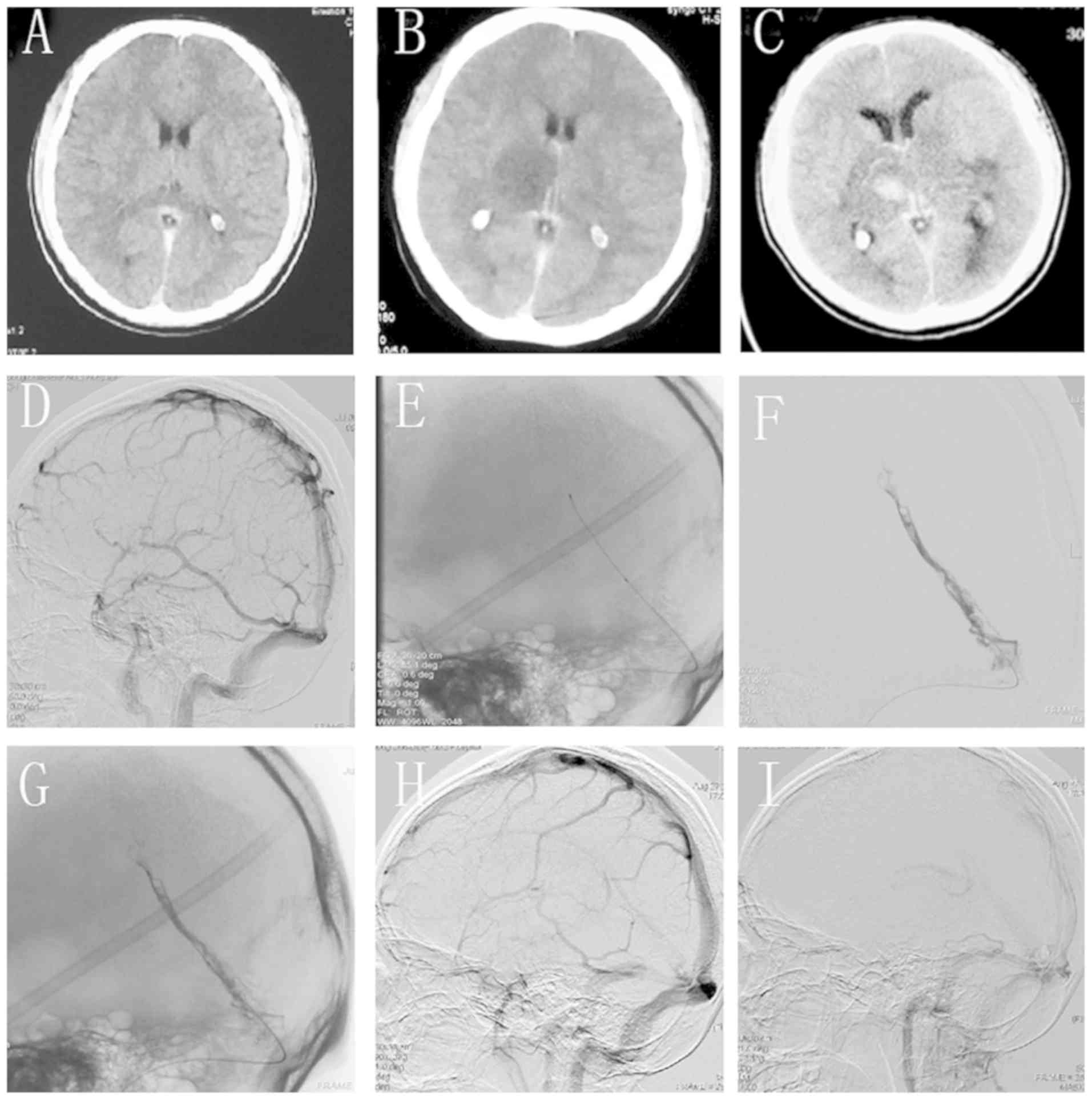
Case one
A 23-year-old right-handed male patient developed
diarrhea after intense exercise and presented with severe headache
on the following day. Scanning images of the case are provided in
Fig. 1. At the local hospital, the
patient was suspected to have subarachnoid hemorrhage based on
non-contrast CT scans, which was later confirmed as CVST (Fig. 1A). The patient was subjected to DSA
and no aneurysms or other abnormalities were identified; however, a
later review confirmed the presence of a thrombus in the straight
sinus (Fig. 1D). At 3 h after DSA
examination, the patient's condition worsened and his consciousness
was impaired, and he was transferred to our hospital within 2 h. On
admission, the patient was in a coma with a GCS score of 6 (E1V1M4)
and had anisocoria with a 5-mm pupil and reactivity to light on the
right side. He underwent another CT scan, which indicated edema in
the right thalamus area and indirect signs of CVST (Fig. 1B). Straight sinus thrombosis was
confirmed by CT and DSA (Fig. 1B
and D). The patient was
administered LMWH as a subcutaneous injection and further
supportive medications; 24 h later, however, he progressively
deteriorated and the GCS score decreased to 3 (E1V1M1). On repeated
CT scans, the patient had hematoma in the right thalamus, with
significant edema in the bilateral thalami and brain stem (Fig. 1C). The patient then received
intervention therapy.
A 6-Fr guiding catheter was introduced into the
right internal jugular vein. The microcatheter (Rebar 27) was then
inserted into the distal part of the thrombosed SS (Fig. 1E). Next, a 6x30-mm Solitaire FR
stent was deployed in the thrombosed segment and the stent was
retracted into the sheath 10 min later; however, the sinus was not
recanalized. The retraction was repeated three times and 300,000 IU
of UK were injected for total thrombolysis. On DSA, partial
recanalization of the thrombosed SS was achieved (Fig. 1F). Over the exchange wire, the Rebar
27 microcatheter was redelivered to the very distal part of the SS
with a 300-cm exchange wire. The infusion pump was then connected
to the microcatheter. UK (40,000 IU/h) was infused by the pump for
SRT-LLT. On the second day after the operation, the patient's state
improved and he was able to follow the doctor's instructions. The
patient improved significantly every day over the following days.
He was fully conscious and his physical activity was good on the
7th postoperative day, with a GCS score of 15. Thrombolysis via the
microcatheter was stopped and oral anticoagulant therapy was
continued. At the 1-month follow-up, the patient had recovered
completely (Fig. 1I) and DSA
re-evaluation revealed complete recanalization of the SS (Fig. 1G and H).
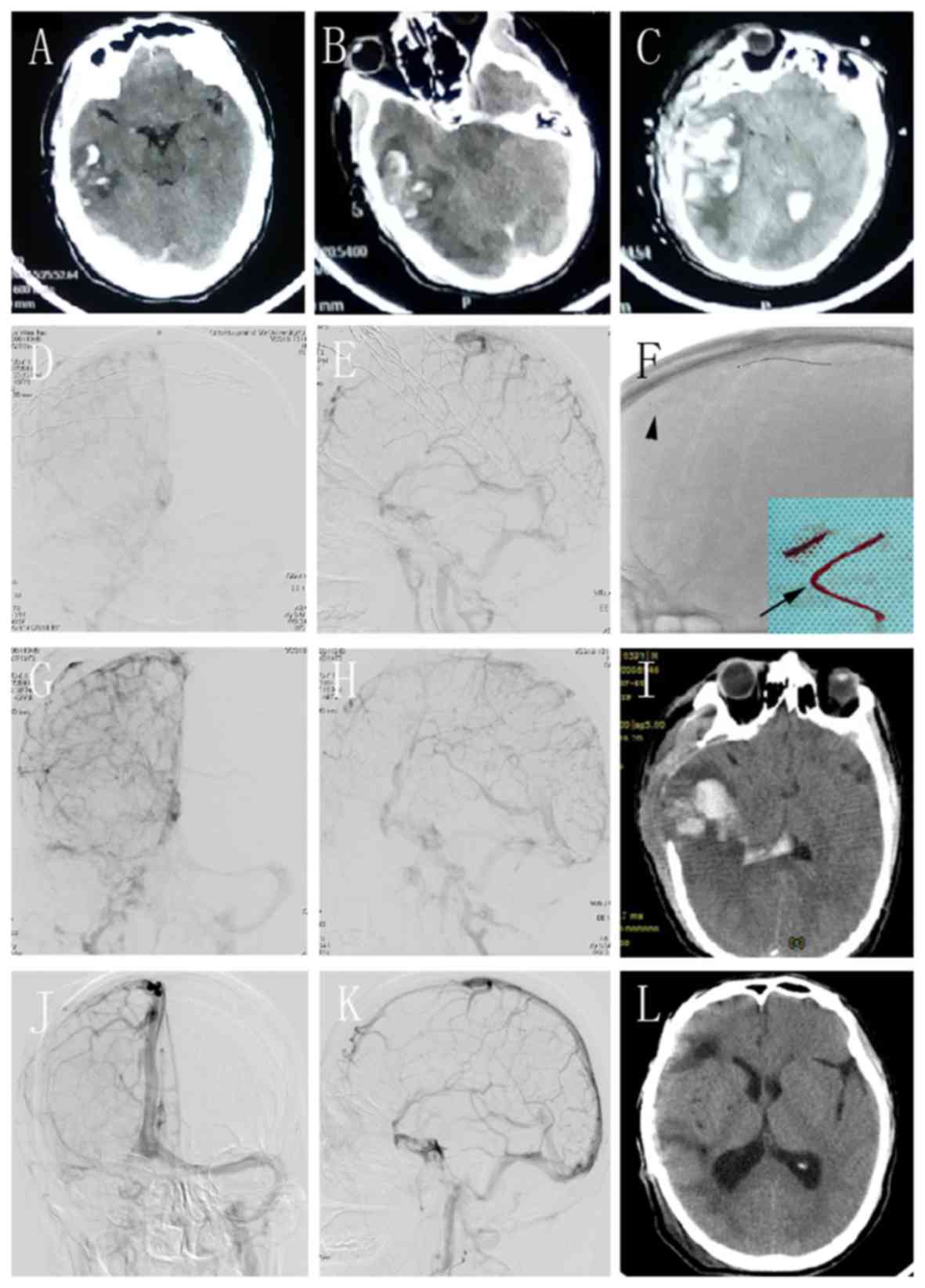
Case two
A 47-year-old right-handed man presented with a
headache after 14 h of driving, which worsened the next day. The
head CT examination performed at the local hospital revealed
hemorrhage in the right temporal lobe (Fig. 2A). The patient was unconscious with
anisocoria in 4 h and the repeat CT revealed an increase in the
size of the hematoma, with midline shift and cerebral herniation
(Fig. 2B). The patient underwent
craniotomy for hematoma removal and decompression. However, his
condition deteriorated and the repeat CT scan revealed re-bleeding
after surgery (Fig. 2C). The
patient was transferred to our hospital with a GCS score of 7
(E1V2M4). The CT image was carefully reviewed and CVST was
confirmed as the cause of the hemorrhage. The patient was
administered anticoagulants and other supportive medications.
However, the treatment was unsuccessful and the GCS score decreased
to 4 (E1V1M2). The patient received intervention therapy. DSA
revealed extensive severe CVST, involving the SSS, bilateral TS,
right SigS and right internal jugular (Fig. 2D and E). A 6-Fr guiding catheter was used, but
any attempts to pass it through the occluded right internal jugular
vein were unsuccessful. Therefore, navigation into the left side
was pursued. A microcatheter (Rebar 27) was placed to reach the
distal part of the SSS. The Solitaire FR stent was deployed and
subsequently retracted 10 min later (Fig. 2F; arrow). Several of the clots were
successfully removed (Fig. 2F;
arrowhead). Angiography revealed that the occluded sinus was
partially recanalized with residual thromboses and the
arteriovenous transit time was shortened (Fig. 2G and H). The patient received the same procedure
as the previous case. UK (40,000 IU/h) was infused for SRT-LLT. The
repeat CT revealed absorption of the hematoma and decrease of the
edema on the 6th day after the operation (Fig. 2I). The thrombolysis was discontinued
and the patient recovered with a GCS score of 15. He was discharged
with fully restored consciousness and no neurological dysfunction
14 days later.
At the 4-month follow-up, the patient's neurological
function was normal. The findings on the CT scan were normal,
except for the cranioplasty (Fig.
2L). The DSA revealed complete recanalization of the SSS, with
normal arteriovenous blood flow in the TS on the left side but
partial occlusion on the right side (Fig. 2J and K). He was prescribed oral anticoagulants
for 1 year.
Discussion
CVST is a rare disease with a potentially fatal
outcome. During recent decades, its incidence has markedly
increased, which may be attributed to advances in imaging
techniques (15). However, CVST may
not be timely diagnosed, as its clinical presentations are atypical
and non-specific (2). Non-contrast
CT scan is only able to reveal indirect signs of CVST and has low
sensitivity and specificity (16).
A number of the patients in the present study were not accurately
diagnosed with CVST at their primary hospital; they were initially
misdiagnosed, e.g. with postpartum reaction, fatigue or simple
diarrhea, which led to rapid aggravation of the symptoms, ICH and
life-threatening complications due to the absence of specific
treatment. The timely and correct treatment for SH-CVST remains
controversial. Systemically administered anticoagulation with
heparin (unfractionated or LMWH) is the standard first-line
treatment for CVST, even in patients with an ICH at baseline
(17). However, a subset of
patients are refractory to standard anticoagulation therapy,
leading to complications, including ischemic and hemorrhagic
stroke, cerebral edema and even death (3). Viegas et al (18) reported that 88% of patients with CVT
recovered following systemic thrombolysis, but 2 patients died due
to intracranial hemorrhage. Systemic thrombolytic therapy,
particularly high-dose thrombolysis, still poses a risk of inducing
bleeding. Gala et al (19)
recommend thrombolytic therapy after failure of anticoagulant
therapy, followed by interventional thrombectomy therapy if the
thrombolysis treatment was unsuccessful. Guo et al (20) reported that 73% of patients with
CVST had a good outcome of intrasinus thrombolytic treatment. The
present study included 10 patients with hemorrhagic CVST who were
first treated with anticoagulation, 8 of whom deteriorated rapidly
in the first 24-48 h. It was decided to perform intervention
therapy directly when the patients deteriorated further even after
receiving anticoagulation treatment. It was considered that
systemic thrombolysis may induce rebleeding in these hemorrhagic
patients, and also that thrombolysis may not act rapidly enough in
patients with a life-threatening condition. Therefore, thrombectomy
combined with local thrombolysis was performed to reduce the risk
of rebleeding.
Endovascular mechanical thrombectomy is considered
to be an effective treatment in addition to systemic
anticoagulation in severe CVST, due to the potential immediate
reestablishment of antegrade venous flow, based on the success of
mechanical clot retrieval in the arterial vasculature for acute
ischemic large-vessel occlusion stroke (21). SRT-LLT achieved complete
recanalization in 50% and partial recanalization in 50% of the
SH-CVST patients who did not respond well to anticoagulation
therapy. Although there were two cases of rebleeding after the
intervention, this was attributed to increased congestion
hemorrhage due to the obstruction of venous reflux by the
thrombosis rather than procedural complications, including injury
of the vessels or the side effects of local thrombolysis. Styczen
et al (8) reported that of
14 patients with CVST undergoing thrombectomy, recanalization was
successful in 86% of cases and complete recanalization was achieved
in 29%. In the present study, complete recanalization was achieved
in 50% of the cases due to combined therapy. Rapid and complete
recanalization may reverse the life-threatening condition in
patients with SH-CVST.
Previous studies reported complete recanalization in
87% and partial recanalization rates in 6% of patients with severe
CVST who were treated with a combination of anticoagulation and
intervention (16,22). Good recanalization rates were
obtained in certain centers with continuous local thrombolysis
after mechanical thrombectomy (23-26).
However, they did not specifically focus on cases with SH-CVST. The
lower rate of complete recanalization in the present study was
probably due to the delayed diagnosis, and there was more severe
thrombosis in the obstructed sinuses compared with that in other
patients with non-hemorrhagic CVST. Acute clots are easier to
completely remove, as they primarily consist of erythrocytes, with
less fibrin cross-linking and collagen deposition. Subacute or
chronic thrombi are more difficult to compress and dissolve due to
the higher collagen and cross-linked fibrin content (27). In the present study, multiple
sinuses were affected, complete recanalization was not achieved by
thrombectomy alone and long-term local thrombolysis was
required.
For cases of CVST with a life-threatening severity,
endovascular intervention, including mechanical thrombectomy,
thromboembolic aspiration or balloon venoplasty, with or without
local thrombolysis, are alternative treatment methods (22,28).
Local thrombolysis during endovascular intervention was first
described in 1988 by Scott et al (29), and it gradually became more popular
and more frequently practiced in the clinical setting. UK is the
most frequently used agent (30).
In most of the previous studies, it was used at doses of
250,000-1,000,000 U in one session during endovascular intervention
(11,13,29,31),
or as a continuous local infusion over several days. Local
thrombolysis further dissolves residual thrombi and cortical venous
thrombosis (10).
As showcased in the second representative case of
the present study, it is dangerous to perform craniotomy blindly
when encountering an atypical cerebral hemorrhage. Intracerebral
hemorrhage or edema in the internal capsule, thalami or basal
ganglia highly suggests the possibility of deep CVST (4,32).
Just as in the second case, it led to rebleeding. Zuurbier also
reported that new hemorrhagic lesions were identified on
post-decompressive craniectomy and/or hematoma evacuation in 4 of
10 patients and tended to be associated with poor outcomes
(33). However, it may be
recommended that all attempts should be made to treat severe cases
by more progressive methods in addition to conservative treatment.
Thrombectomy and thrombolysis may be performed even in cases of
SH-CVST. According to the study by Kulcsár et al (11), thrombectomy and long-term
thrombolysis are complementary without increasing the risk of
rebleeding.
There were certain limitations to the present study.
First, it was not a randomized controlled trial and the number of
cases was too small for a conclusive statistical analysis. It is
most likely due to the low incidence of hemorrhagic CVST that there
are no large-scale prospective clinical studies on interventional
therapy for SH-CVST.
Almost all cases of SH-CVST deteriorated following
an initial mild presentation. It is crucial to evaluate the signs
and the risk factors of CVST and adjust therapy in a timely manner
to avoid progression to a life-threatening condition.
In conclusion, SRT-LLT is feasible, safe and
effective for SH-CVST. It may be applied as a rescue therapy for
the patients with SH-CVST who are refractory to standard medical
treatment.
Acknowledgements
Not applicable.
Funding
The present study was supported by a grant from
Shandong Province Outstanding Young Scientists Fund (grant no.
BS2012YY012).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YW and ZW designed and performed the current study.
CZ and DZ performed analyses. YW, ZW, DZ and BS administered
treatment. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The protocol of the present study was approved by
the Ethics Committee of Qilu Hospital Affiliated to Shandong
University (Qingdao, China). Patients or authorized relatives were
informed on the risks and benefits of the operation and provided
written informed consent.
Patient consent for publication
Informed consent for publication of images was
obtained from all subjects or their relatives.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Silvis SM, de Sousa DA, Ferro JM and
Coutinho JM: Cerebral venous thrombosis. Nat Rev Neurol.
13:555–565. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Linn J, Ertl-Wagner B, Seelos KC, Strupp
M, Reiser M, Bruckmann H and Brüning R: Diagnostic value of
multidetector-row CT angiography in the evaluation of thrombosis of
the cerebral venous sinuses. AJNR Am J Neuroradiol. 28:946–952.
2007.PubMed/NCBI
|
|
3
|
Saposnik G, Barinagarrementeria F, Brown
RD Jr, Bushnell CD, Cucchiara B, Cushman M, deVeber G, Ferro JM and
Tsai FY: American Heart Association Stroke Council and the Council
on Epidemiology and Prevention: Diagnosis and management of
cerebral venous thrombosis: A statement for healthcare
professionals from the American Heart Association/American Stroke
Association. Stroke. 42:1158–1192. 2011.
|
|
4
|
Leach JL, Fortuna RB, Jones BV and
Gaskill-Shipley MF: Imaging of cerebral venous thrombosis: Current
techniques, spectrum of findings, and diagnostic pitfalls.
Radiographics. 26 (Suppl 1):S19–S43. 2006.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Nasr DM, Brinjikji W, Cloft HJ, Saposnik G
and Rabinstein AA: Mortality in cerebral venous thrombosis: Results
from the national inpatient sample database. Cerebrovasc Dis.
35:40–44. 2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Capecchi M, Abbattista M and Martinelli I:
Cerebral venous sinus thrombosis. J Thromb Haemost. 16:1918–1931.
2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ilyas A, Chen CJ, Raper DM, Ding D, Buell
T, Mastorakos P and Liu KC: Endovascular mechanical thrombectomy
for cerebral venous sinus thrombosis: A systematic review. J
Neurointerv Surg. 9:1086–1092. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Styczen H, Tsogkas I, Liman J, Maus V and
Psychogios MN: Endovascular mechanical thrombectomy for cerebral
venous sinus thrombosis: A single-center experience. World
Neurosurg. 127:e1097–e1103. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mokin M, Lopes DK, Binning MJ,
Veznedaroglu E, Liebman KM, Arthur AS, Doss VT, Levy EI and
Siddiqui AH: Endovascular treatment of cerebral venous thrombosis:
Contemporary multicenter experience. Interv Neuroradiol.
21:520–526. 2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mortimer AM, Bradley MD, O'Leary S and
Renowden SA: Endovascular treatment of children with cerebral
venous sinus thrombosis: A case series. Pediatric Neurol.
49:305–312. 2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kulcsár Z, Marosfoi M, Berentei Z and
Szikora I: Continuous thrombolysis and repeated thrombectomy with
the Penumbra System in a child with hemorrhagic sinus thrombosis:
Technical note. Acta Neurochir (Wien). 152:911–916. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Guo XB, Song LJ and Guan S: Endovascular
treatment of chronic, recurrent headache secondary to chronic
cerebral venous sinus thrombosis. J Stroke Cerebrovasc Dis.
23:560–563. 2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Chen C, Li X, Huang L, Zhang J, Chen S, Ye
H, Ye Q, Zhang T, Zhang X, Chen Z, et al: Mechanical thrombectomy
with intraoperative local thrombolysis versus mechanical
thrombectomy with continuous thrombolysis for treatment of cerebral
venous sinus thrombosis: A systematic review of 82 cases. World
Neurosurg. 125:489–497.e14. 2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Chen C, Wang Q, Li X, Lu Z, He J, Fang Q,
Ke X, Duan C and Li T: Stent retriever thrombectomy combined with
local thrombolytic therapy for cerebral venous sinus thrombosis: A
case report. Exp Ther Med. 14:3961–3970. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Coutinho JM, Zuurbier SM, Aramideh M and
Stam J: The incidence of cerebral venous thrombosis: A
cross-sectional study. Stroke. 43:3375–3377. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Dmytriw AA, Song JSA, Yu E and Poon CS:
Cerebral venous thrombosis: State of the art diagnosis and
management. Neuroradiology. 60:669–685. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ferro JM, Bousser MG, Canhao P, Coutinho
JM, Crassard I, Dentali F, di Minno M, Maino A, Martinelli I,
Masuhr F, et al: European Stroke Organization guideline for the
diagnosis and treatment of cerebral venous thrombosis-endorsed by
the European Academy of Neurology. Eur J Neurol. 24:1203–1213.
2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Viegas LD, Stolz E, Canhão P and Ferro JM:
Systemic thrombolysis or cerebral venous and dural sinus
thrombosis: A systematic review. Cerebrovasc Dis. 37:43–50.
2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Gala NB, Agarwal N, Barrese J, Gandhi CD
and Prestigiacomo CJ: Current endovascular treatment options of
dural venous sinus thrombosis: A review of the literature. J
Neurointerv Surg. 5:28–34. 2013.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Guo XB, Guan S, Fan Y and Song LJ: Local
thrombolysis for severe cerebral venous sinus thrombosis. AJNR Am J
Neuroradiol. 33:1187–1190. 2012.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Goyal M, Menon BK, van Zwam WH, Dippel DW,
Mitchell PJ, Demchuk AM, Dávalos A, Majoie CB, van der Lugt A, de
Miquel MA, et al: Endovascular thrombectomy after large-vessel
ischaemic stroke: A meta-analysis of individual patient data from
five randomised trials. Lancet. 387:1723–1731. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Li G, Zeng X, Hussain M, Meng R, Liu Y,
Yuan K, Sikharam C, Ding Y, Ling F and Ji X: Safety and validity of
mechanical thrombectomy and thrombolysis on severe cerebral venous
sinus thrombosis. Neurosurgery. 72:730–738. 2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Chow K, Gobin YP, Saver J, Kidwell C, Dong
P and Viñuela F: Endovascular treatment of dural sinus thrombosis
with rheolytic thrombectomy and intra-arterial thrombolysis.
Stroke. 31:1420–1425. 2000.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Blackham KA: Extensive dural sinus
thrombosis: Successful recanalization with thrombolysis and a novel
thrombectomy device. J Neurosurg. 114:133–135. 2011.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Curtin KR, Shaibani A, Resnick SA, Russell
EJ and Simuni T: Rheolytic catheter thrombectomy, balloon
angioplasty, and direct recombinant tissue plasminogen activator
thrombolysis of dural sinus thrombosis with preexisting hemorrhagic
infarctions. AJNR Am J Neuroradiol. 25:1807–1811. 2004.PubMed/NCBI
|
|
26
|
Dowd CF, Malek AM, Phatouros CC and
Hemphill JC III: Application of a rheolytic thrombectomy device in
the treatment of dural sinus thrombosis: A new technique. AJNR Am J
Neuroradiol. 20:568–570. 1999.PubMed/NCBI
|
|
27
|
Chen H, He X, Xie G, Liang J, Ye Y, Deng
W, He Z, Liu D, Li D, Liu X and Fan Z: Cardiovascular magnetic
resonance black-blood thrombus imaging for the diagnosis of acute
deep vein thrombosis at 1.5 Tesla. J Cardiovasc Magn Reson.
20(42)2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Siddiqui FM, Dandapat S, Banerjee C,
Zuurbier SM, Johnson M, Stam J and Coutinho JM: Mechanical
thrombectomy in cerebral venous thrombosis: Systematic review of
185 cases. Stroke. 46:1263–1268. 2015.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Scott JA, Pascuzzi RM, Hall PV and Becker
GJ: Treatment of dural sinus thrombosis with local urokinase
infusion. Case report. J Neurosurg. 68:284–287. 1988.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Canhao P, Falcao F and Ferro JM:
Thrombolytics for cerebral sinus thrombosis: A systematic review.
Cerebrovasc Dis. 15:159–166. 2003.PubMed/NCBI View Article : Google Scholar
|
|
31
|
D'Alise MD, Fichtel F and Horowitz M:
Sagittal sinus thrombosis following minor head injury treated with
continuous urokinase infusion. Surg Neurol. 49:430–435.
1998.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Poon CS, Chang JK, Swarnkar A, Johnson MH
and Wasenko J: Radiologic diagnosis of cerebral venous thrombosis:
Pictorial review. AJR Am J Roentgenol. 189 (6 Suppl):S64–S75.
2007.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Zuurbier SM, Coutinho JM, Majoie CB, Coert
BA, van den Munckhof P and Stam JJ: Decompressive hemicraniectomy
in severe cerebral venous thrombosis: A prospective case series.
Neurol. 259:1099–1105. 2012.PubMed/NCBI View Article : Google Scholar
|