Introduction
Acute myocardial infarction (AMI) is one of the most
severe cardiac emergencies in internal medicine. Because of its
properties of acute onset, quick progression, and high morbidity
and mortality (1,2), AMI has been a research focus for a
long time. However, many recent studies have reported that the
incidence of AMI has started to decrease, and this reduction is
mainly concentrated in the age population greater than 60 years
(3-6).
Considering that elderly individuals are the main population with a
high AMI incidence (7), this
reduced incidence as mentioned above was a delightful change. Yet,
the incidence of AMI among the young population has gradually shown
a rising trend (6,8,9). The
young population who suffers AMI can show many clinical symptoms,
such as ischemic chest pain, and the clinical course is extremely
short. Some patients even experience sudden cardiac death. Although
epidemiological research has determined that various behaviors and
symptoms, including smoking, hypertension, diabetes, and family
history of coronary heart disease (CHD), may be potential risk
factors for AMI occurrence (10-12),
it is still unclear how these factors differ between the young and
old population. Therefore, investigating the epidemiology and
clinical characteristics of AMI occurrence in the young population
is a new future research focus. Through our study, the behavioral
and clinical characteristics of AMI in the young population will be
explored and determined, which will provide significant clues for
explaining the increasing trend of AMI in the young population and
helping to design specific strategies to prevent and treat young
AMI patients.
Patients and methods
Study design
This retrospective, single-center, observational
study was conducted during a 24-month period from January 2014 to
December 2015 at Weifang People's Hospital. Consecutive patients
who were diagnosed with AMI were included in the present study, and
the criteria for enrollment in this study were based on AMI
diagnostic criteria from WHO (https://doi.org/10.1016/S0140-6736(08)61237-4): At
least covering two of the following three features, including
ischemic thoracodynia, ECG dynamic change, and serum biomarkers of
myocardial necrosis. All enrolled patients were divided in two
groups, including a young group (n=114) and an elder group (n=179).
In addition, 60 young volunteers received health checkup and the
same healthy subjects during January 2014 to December 2015 at
Weifang People's Hospital were enrolled as the healthy control
group (age range 18-72 years, with an average age of 42.1±6.3
years). Detailed information is listed in Table I.
 | Table IBaseline characteristics associated
with AMI between the young and elder group. |
Table I
Baseline characteristics associated
with AMI between the young and elder group.
| Factors | Control group n | Young group n
(%) | Elder group n
(%) | P-valuea |
|---|
| Total | 60 | 114 | 179 | |
| Sex | | | | <0.01 |
|
Male | 31 | 108 (94.7) | 115 (64.2) | |
|
Female | 30 | 6 (5.3) | 64 (35.8) | |
| History of
smoking | | | | <0.05 |
|
Yes | 14 | 96 (84.2) | 105 (58.7) | |
|
No | 46 | 18 (15.8) | 74 (41.3) | |
| Hypertension | | | | <0.01 |
|
Yes | 6 | 30 (26.3) | 121 (67.6) | |
|
No | 54 | 84 (73.7) | 58 (32.4) | |
| Hyperlipemia | | | | >0.05 |
|
Yes | 3 | 52 (45.6) | 97 (54.2) | |
|
No | 57 | 62 (54.4) | 82 (45.8) | |
| Obesity | | | | >0.05 |
|
Yes | 12 | 30 (26.3) | 58 (32.4) | |
|
No | 48 | 84 (73.7) | 121 (67.6) | |
| Diabetes | | | | <0.01 |
|
Yes | 2 | 8 (7.0) | 67 (37.4) | |
|
No | 58 | 106 (93.0) | 112 (62.6) | |
| Positive family
medical history | | | | <0.01 |
|
Yes | 5 | 60 (52.6) | 29 (16.2) | |
|
No | 55 | 54 (47.4) | 150 (83.8) | |
| Blood fat level
(mmol/l) | | | | |
|
TC | 3.19±0.39 | 8.19±2.17 | 5.98±1.13 | <0.05 |
|
TG | 0.97±0.26 | 4.71±1.17 | 2.18±0.69 | <0.05 |
|
HDL | 1.93±0.38 | 1.66±0.42 | 1.39±0.21 | >0.05 |
|
LDL | 2.34±0.71 | 3.77±0.85 | 3.14±0.74 | >0.05 |
Data collection
In the present study, three types of information
were collected. Firstly, data of AMI-related risk factors were
collected, which included blood pressure, blood fat, blood glucose,
smoking history, drinking history, body mass index (BMI), family
history of coronary heart disease (CHD), history of hypertension
and diabetes. Among these, blood fat included total cholesterol
(TC), triglyceride (TG), high-density lipoprotein (HDL) and low
density lipoprotein (LDL) levels. BMI was calculated using weight
(kg) and height (m) as (BMI=kg/m2), and BMI >25 was
defined as overweight. TC >5.75 mmol/l and TG >1.7 mmol/l
were defined as being increased. Smoking history was defined as the
smoking of 1 or more cigarettes per day and lasting for over 1
year; smoke 20 or more cigarettes per day and lasting for 10 years
was defined as smoking heavily. Drinking was defined as drinking
wine (>50 g per day); drinking wine (>150 g per day) and
lasting for 10 years was defined as excessive drinking. Then, we
investigated whether patients had angina or not before AMI. We
determined whether thoracodynia was typical or not, and whether
this was combined with complications, including arrhythmia, cardiac
insufficiency, formation of ventricular aneurysm, perforation of
ventricular septum, cardiac shock, and death. Finally, the results
of radiography were also collected. The criteria for judgment was
by means of diameter measurement: Stenosis ≥50% was defined as a
significant lesion. Lesions involved in 1 branch, 2 branches, or 3
branches of left main/anterior descending coronary artery, left
circumflex, and right coronary artery was defined as
1-branch-lesion, 2-branch-lesion, and 3-branch-lesion,
respectively.
Statistical analysis
In the present study, we used SAS 9.2 (SAS
Institute, Inc.) to deal with data cleaning and analysis. Mean ± SD
(standard deviation) was used to reflect the distribution of
measurement data, and t-test was used to compare data from two
groups. χ2 test was used to test the differences of
categorical data from two groups. P<0.05 was defined as
indicative of statistical significance, and all tests were two
sided.
Results
Demographic characteristic
In the present study, we finally enrolled 293 AMI
patients, including 114 young AMI patients (age ≤42 years) assigned
to the young group and 179 elder AMI patients (age ≥60 years)
assigned to the elder group. We also enrolled 60 young volunteers
who received a health checkup as the healthy control group, and
detail information is listed in the Table I. Among the young group, 108 (94.7%)
patients were male and 6 (5.3%) patients were female. The range of
age was from 32 to 44 years and the mean age was 36.6±4.0 years.
Among the elder group, 115 (64.2%) patients were male and 64
(35.8%) patients were female; the maximum age was 81 years and the
minimum was 60 years, with an average age of 69.4±6.2 years.
Analysis of AMI-related factors
between the young and elder group
As documented in Table
I, the compositions of male and female in these two groups
showed a significant difference. In the young AMI group, the males
had a higher rate (94.7%) than that in the elder group (64.2%). The
percentages of males and females in the elder group were much
closer. The young AMI group had a higher percentage of smoking
history compared to the elder group (84.2 vs. 58.7%; P<0.05) and
positive family medical history (52.6 vs. 16.2%); however, the
elder AMI group seemed to be more likely to have hypertension
compared with the young group (67.6 vs. 26.3%; P<0.01) and
diabetes (37.4 vs. 7.0%; P<0.01). For hyperlipemia and obesity,
there were no obvious differences between the two groups
(hyperlipemia: 45.6 vs. 54.2%, P>0.05; obesity: 26.3 vs. 32.4%,
P>0.05). Lipid metabolism in AMI patients is a key point that
requires more attention. In the present study, the blood fat levels
including TC and TG were significantly higher in young group
compared to the elder group (TC: 8.19±2.17 vs. 5.98±1.13,
P<0.05; TG: 4.71±1.17 vs. 2.18±0.69, P<0.05). However, we did
not observed the significant difference in the serum HDL and LDL
levels between these two groups which may due to a relative small
sample size.
Clinical performance comparisons
between the young and elder group
As documented in Table
II, for clinical performances, we found that young AMI patients
had a higher rate of typical thoracodynia which occurred most
suddenly when compared with the elder group (93.0 vs. 68.2%;
P<0.01). However, in the elder patients, they were more likely
to have different types of clinical performances than the young
patients, including premonitory symptom (84.4 vs. 33.3% yes),
arrhythmia (78.2 vs. 52.6% yes), heart failure (41.9 vs. 21.1%
yes), and cardiac shock (37.4 vs. 3.5%, yes).
 | Table IIComparisons of clinical performances
between the young and elder group. |
Table II
Comparisons of clinical performances
between the young and elder group.
| Factors | Young group n
(%) | Elder group n
(%) |
P-valuea |
|---|
| Total | 114 | 179 | |
| Premonitory
symptom | | | <0.01 |
|
Yes | 38 (33.3) | 151 (84.4) | |
|
No | 76 (66.7) | 28 (15.6) | |
| Typical
thoracodynia | | | <0.01 |
|
Yes | 106 (93.0) | 122 (68.2) | |
|
No | 8 (7.0) | 57 (31.8) | |
| Arrhythmia | | | <0.01 |
|
Yes | 60 (52.6) | 140 (78.2) | |
|
No | 54 (47.4) | 39 (21.8) | |
| Heart failure | | | <0.05 |
|
Yes | 24 (21.1) | 75 (41.9) | |
|
No | 90 (78.9) | 104 (58.1) | |
| Cardiac shock | | | <0.01 |
|
Yes | 4 (3.5) | 67 (37.4) | |
|
No | 110 (96.5) | 112 (62.6) | |
Outcomes from coronary angiography
(CAG)
As documented in Table
III, the different age groups had different major lesion sites
and statuses. The lesion per capita in the young AMI group was 1.8,
which was lower than 2.8 in the elder AMI group. The lesions in the
young patients mostly focused on anterior descending coronary
artery, and 62.4% of lesions were one-branch lesion. Comparatively,
the elder patients had more severe conditions. The distributions of
lesion sites were almost equally on left main/anterior descending
coronary artery, left circumflex, and right coronary artery.
Three-branch lesion was the most frequent lesion, followed by
two-branch lesion and one-branch lesion, which was a little
different from that in the young AMI group.
 | Table IIIComparisons of the outcomes of
coronary angiography (CAG) between the young and elder group. |
Table III
Comparisons of the outcomes of
coronary angiography (CAG) between the young and elder group.
| Factors | Young group n
(%) | Elder group n
(%) |
P-valuea |
|---|
| Total | 114 | 179 | |
| Total lesions on
coronary artery | 194 | 465 | |
| Lesions per
capita | 1.8 | 2.6 | <0.01 |
| Lesions on anterior
descending coronary artery | | | <0.01 |
|
Yes | 101 (52.1) | 153 (32.9) | |
|
No | 93 (47.9) | 312 (67.1) | |
| Lesions on right
coronary artery | | | >0.05 |
|
Yes | 42 (21.6) | 112 (24.1) | |
|
No | 152 (78.4) | 353 (75.9) | |
| Lesions on left
circumflex | | | >0.05 |
|
Yes | 40 (20.6) | 103 (22.2) | |
|
No | 154 (79.4) | 362 (77.8) | |
| Lesions on left
main coronary artery | | | <0.01 |
|
Yes | 11 (5.7) | 97 (20.9) | |
|
No | 183 (94.3) | 368 (79.1) | |
| Coronary
angiography lesion (individual) | | | |
|
No
lesions | 6 (5.3) | 2 (1.1) | <0.01 |
|
One-branch
lesion | 71 (62.4) | 44 (24.6) | <0.01 |
|
Two-branch
lesion | 23 (20.1) | 56 (31.3) | <0.01 |
|
Three-branch
lesion | 14 (12.2) | 77 (43.0) | <0.01 |
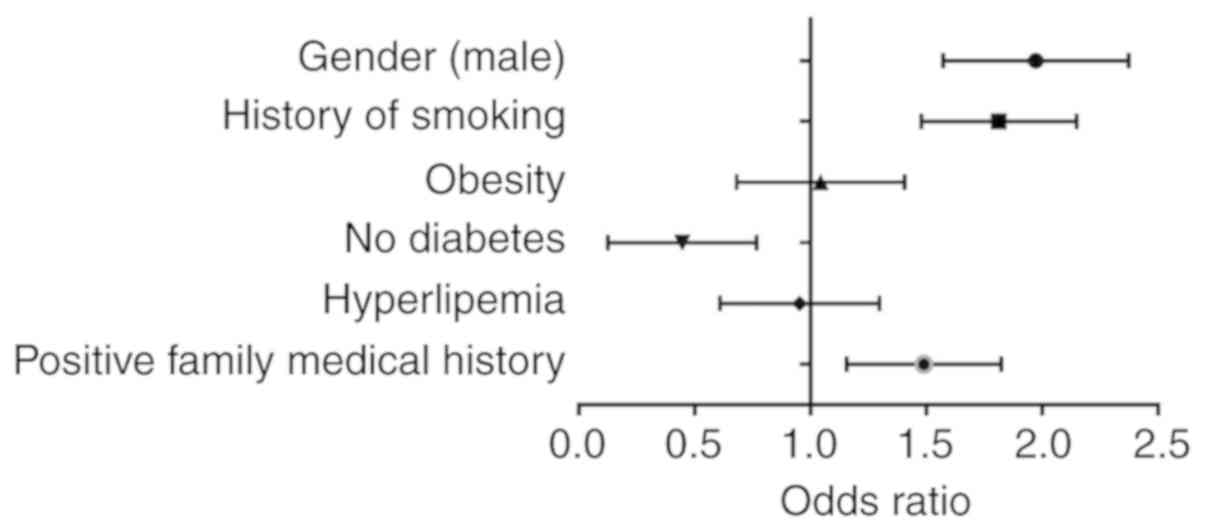
Odds ratios between the young and
elder group
As shown in Fig. 1,
compared with the elderly group, the young males had a history of
smoking and had a positive family medical history of heart disease,
and had higher risk of acute myocardial infarction. However, the
absence of diabetes was found to be a protective factor. Details
are shown in Fig. 1.
Discussion
In this study, we analyzed clinical data collected
from Weifang People's Hospital to evaluate the acute myocardial
infarction (AMI) characteristics in young patients, which could
provide some clues for AMI diagnosis and therapy in different age
subsets in the future.
In the young AMI group (age ≤42 years), the AMI
incidence in males was obviously higher than that of females, which
was consistent with a previous study (13). Estrogen is an important hormone
protecting women from AMI (14),
which involves the regulation of lipometabolism, inhibition of
platelet activation, and suppression of intima proliferation caused
by lesions. After menopause, the estrogen level decreases. Along
with this, the protection from AMI also become weak, even
disappearing, which increases the female AMI incidence (15). Smoking, hypertension, hyperlipemia,
diabetes, and family history of cardiac heart disease (CHD) are
potential risk factors for the occurrence of CHD (16). The present study found that 84.2% of
young patients had a history of smoking, which was higher than that
of the elder group (age ≥60 years). A previous study revealed that
CO2 and nicotine in smoke cause hypoxia in tissues and
the myocardium, which then induced coronary spasm and an increase
in blood viscosity (17). A history
of long-term smoking decreases coronary dilation function, and
increases platelet aggregation (18). Meanwhile, high-density lipoprotein
is decreased and low-density lipoprotein is increased. This change
damages serum antioxidative function (19). Based on the above clinical
situations, coronary atherosclerotic plaque forms, and is
aggravated, which in turn promotes the occurrence and progression
of CHD. Thus, abstinence from smoking is one of the most critical
interventions for CHD prevention, especially for young people
The rate of hypertension and diabetes in the elder
group were higher than that in the young group, which suggests that
the elderly AMI patients were consistently accompanied by certain
chronic diseases (20). At the same
time, the elderly people had a higher frequency of complications,
including arrhythmia, heart failure, and cardiac shock, which were
the significant reasons for the poor prognosis in AMI elder
patients. Noticeably, the rate of hypertension and various
complications in young patients were not low. In the present study,
the incidence of hypertension and hyperlipemia in the young AMI
patients were 26.3 and 45.6%, which were significantly higher than
these percentages in the young health control group, and should be
focused on. The rate of hyperlipemia did not show much difference
between the young and elder groups, but almost half of the patients
had hyperlipemia in the two groups. Some studies have shown that
high levels of serum total cholesterol (TC) and low density
lipoprotein (LDL) are independent risk factors for coronary disease
(21-23).
Therefore, controlling blood fat is an important intervention for
reducing AMI incidence in all populations.
Through the coronary angiography (CAG) results, we
found that the most frequent coronary lesion in young AMI patients
was the one-branch lesion (62.4%), and the secondary injury was
limited. Comparatively, elder AMI patients had more multiple-branch
lesions and calcified lesions, which has serious influences on
cardiac function. Additionally, healthy coronary artery with only
none or mild atherosclerosis, normal coronary angiography and
negative treadmill test was found in a certain proportion of young
AMI patients, which are consistent with previous reports (24,25).
This may be related to the clinical characteristics of the young
AMI patients, who exhibited a short course of disease and fewer
complications of hypertension and diabetes.
After comparing the risk factors and clinical
performances between young AMI patients and elder AMI patients
comprehensively, we found that smoking, hyperlipemia, and positive
family medical history were the most critical factors for young AMI
patients, which may play important roles in increasing AMI
incidence. Interventions for controlling these risk factors will be
important in the future for young patients, including abstinence
from smoking, alcohol consuming limitation, proper exercise and a
rational diet.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JW and LL designed the study and drafted the
manuscript. NM, XZ and YQ were responsible for the collection and
analysis of the experimental data. GF, GL and TZ analyzed
AMI-related factors and compared clinical performance. All authors
read and approved the manuscript and agree to be accountable for
all aspects of the research in ensuring that the accuracy or
integrity of any part of the work are appropriately investigated
and resolved.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
W.F. Maternal and Child Health Hospital, Weifang, Shandong, P.R.
China. Patients who participated in this research, signed the
informed consent and had complete clinical data. Signed written
informed consents were obtained from the patients and/or
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Anderson JL and Morrow DA: Acute
myocardial infarction. N Engl J Med. 376:2053–2064. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Longjian L, Ling A and Xinglong Li:
Analysis of death cause in the total population in Mentougou
district of Beijing from 2006 to 2015. Xian Dai Yu Fang Yi Xue.
44:1823–1826. 2017.
|
|
3
|
Randall SM, Zilkens R, Duke JM and Boyd
JH: Western Australia population trends in the incidence of acute
myocardial infarction between 1993 and 2012. Int J Cardiol.
222:678–682. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Schmidt M, Jacobsen JB, Lash TL, Bøtker HE
and Sørensen HT: 25 year trends in first time hospitalisation for
acute myocardial infarction, subsequent short and long term
mortality, and the prognostic impact of sex and comorbidity: A
Danish nationwide cohort study. BMJ. 344(e356)2012.PubMed/NCBI View
Article : Google Scholar
|
|
5
|
Dégano IR, Salomaa V, Veronesi G,
Ferriéres J, Kirchberger I, Laks T, Havulinna AS, Ruidavets JB,
Ferrario MM, Meisinger C, et al: Twenty-five-year trends in
myocardial infarction attack and mortality rates, and
case-fatality, in six European populations. Heart. 101:1413–1421.
2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wang DZ, Shen CF, Zhang Y, Zhang H, Song
GD, Li W, Xue XD, Xu ZL, Zhang S and Jiang GH: Fifteen-year trend
in incidence of acute myocardial infarction in Tianjin of China.
Zhonghua Xin Xue Guan Bing Za Zhi. 45:154–159. 2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
7
|
Hernandez-Suarez DF, Osterman-Pla AD,
Carrasquillo O, Aranda J, Baez S, Lopez M and Garcia-Rivera EJ:
Epidemiological profile of hispanics admitted with acute myocardial
infarction in Puerto Rico: The Experience of 2007, 2009 and 2011. J
Clin Med Res. 9:528–533. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Guo X, Li Z, Vittinghoff E, Sun Y and
Pletcher MJ: Trends in rate of acute myocardial infarction among
patients aged <30 years. Nat Rev Cardiol. 15(119)2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Liu Y, Han T, Gao M, Wang J, Liu F, Zhou S
and Chen Y: Clinical characteristics and prognosis of acute
myocardial infarction in young smokers and non-smokers (≤45 years):
A systematic review and meta-analysis. Oncotarget. 46:81195–81203.
2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Veeranna V, Zalawadiya SK, Niraj A,
Pradhan J, Ference B, Burack RC, Jacob S and Afonso L: Homocysteine
and reclassification of cardiovascular disease risk. J Am Coll
Cardiol. 58:1025–1033. 2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sailam V, Karalis DG, Agarwal A, Alani F,
Galardi S, Covalesky V and Athanassious C: Prevalence of emerging
cardiovascular risk factors in younger individuals with a family
history of premature coronary heart disease and low Framingham risk
score. Clin Cardiol. 31:542–545. 2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ueshima H, Sekikawa A, Miura K, Turin TC,
Takashima N, Kita Y, Watanabe M, Kadota A, Okuda N, Kadowaki T, et
al: Cardiovascular disease and risk factors in Asia: A selected
review. Circulation. 118:2702–2709. 2008.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Matsis K, Holley A, Al-Sinan A, Matsis P,
Larsen PD and Harding SA: Differing clinical characteristics
between young and older patients presenting with myocardial
infarction. Heart Lung Circ. 26:566–571. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Manson JE, Allison MA, Rossouw JE, Carr
JJ, Langer RD, Hsia J, Kuller LH, Cochrane BB, Hunt JR, Pettinger
MB, et al: Estrogen therapy and coronary-artery calcification. N
Engl J Med. 356:2591–2602. 2007.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sidney S, Petitti DB and Quesenberry CP
Jr: Myocardial infarction and the use of estrogen and
estrogen-progestogen in postmenopausal women. Ann Intern Med.
127:501–508. 1997.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ebrahim S, Taylor F, Ward K, Beswick A,
Burke M and Davey Smith G: Multiple risk factor interventions for
primary prevention of coronary heart disease. Cochrane Database
Syst Rev: Jan 19, 2011 (Epub ahead of print). doi:
10.1002/14651858.CD001561.pub3.
|
|
17
|
Lakier JB: Smoking and cardiovascular
disease. Am J Med. 93 (Suppl 1):S8–S12. 1992.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Cavusoglu Y, Timuralp B, Us T, Akgün Y,
Kudaiberdieva G, Gorenek B, Unalir A, Goktekin O and Ata N:
Cigarette smoking increases plasma concentrations of vascular cell
adhesion molecule-1 in patients with coronary artery disease.
Angiology. 55:397–402. 2004.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Yan S, Xiaopeng Z, Xudong J, Wenzhong Z,
Wei W, Wenming C, Xin Z and Ning L: Potential mechanisms of
oxidative damage mechanisms by smoking. Teratog Carcinog Mutagen.
21:50–53. 2009.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Maosen W, Shengfeng W and Zitian Z:
Clinical characteristics and treatment of old acute myocardial
infarction patients. Contemp Med. 17:56–57. 2011.
|
|
21
|
The Lipid Research Clinics Coronary
Primary Prevention Trial results. II. The relationship of reduction
in incidence of coronary heart disease to cholesterol lowering.
JAMA. 251:365–374. 1984.
|
|
22
|
Sever PS, Dahlöf B, Poulter NR, Wedel H,
Beevers G, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A,
McInnes GT, et al: Prevention of coronary and stroke events with
atorvastatin in hypertensive patients who have average or
lower-than-average cholesterol concentrations, in the
Anglo-Scandinavian Cardiac Outcomes Trial--Lipid Lowering Arm
(ASCOT-LLA): A multicentre randomised controlled trial. Lancet.
361:1149–1158. 2003.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Baigent C, Keech A, Kearney PM, Blackwell
L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, et
al: Efficacy and safety of cholesterol-lowering treatment:
Prospective meta-analysis of data from 90,056 participants in 14
randomised trials of statins. Lancet. 366:1267–1278.
2005.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Wenlin R, Dayi H, Jianjun P, et al:
Clinical analysis of percutaneous coronary intervention in young
AMI patients. Beijing Med J. 26:423–424. 2004.
|
|
25
|
Xuegang Y and Chuanrong C: Analysis of
clinical characteristics and CAG results between old and young AMI
patients. J Clin Cardiol. 13:281–365. 1997.
|