Introduction
The Visian Implantable Collamer Lens (ICL™; STAAR
Surgical) has been used for the correction of high myopia for
>10 years (1-4).
Particularly in recent years, with improvements in surgical
techniques and the update of ICL design, it has been widely used.
This surgical procedure is largely reversible, allowing the lens to
be exchanged when refractive changes and unexpected complications
occur after surgery. The currently used approaches for the
correction of residual refractive error after corneal refractive
surgeries mainly include corneal enhancement surgeries and relaxing
corneal incisions (5-8).
Considering the thinner corneal thickness after corneal refractive
surgery, it is unsafe to perform corneal laser surgery again
without sufficient residual stromal bed thickness. The safety of
repeating corneal laser surgery therefore depends on the residual
stromal bed thickness and the amount of residual correction
required. Particularly in patients with large residual refractive
error, the application of ICL has unique advantages.
Previous studies have demonstrated that ICL V4c
implantation for correcting moderate to high myopia has good
safety, efficacy, predictability and stability after long-term
follow-up (9-11).
Recently, ICL implantation has also been confirmed to perform well
for low and moderate myopia (12,13).
These results provide theoretical support and guidance for the use
of ICL to correct residual refractive errors after corneal
refractive surgery.
In the present study, to evaluate the visual quality
after ICL implantation, an Optical Quality Analysis System (OQAS;
Terrassa, Spain), a device that employs the double-pass technique
to assess the quality of retinal imaging, was used. Previously, it
has been generally used to evaluate the visual quality after ICL
implantation, which allows the detection of possible asymmetries in
retinal images and objective measurement of ocular scatter
(14-16).
In the present study, the safety and efficacy of ICL
implantation for residual refractive errors after corneal laser
surgery were evaluated by measuring the visual acuity and visual
quality.
Materials and methods
Subjects
The present study included a total of 16 eyes from
eight patients (three males and five females) who underwent
implantation of a phakic posterior chamber ICL V4c for residual
refractive error after corneal refractive surgeries between August
2015 and February 2018 at the Shanghai Ninth Hospital Affiliated
with Jiao Tong University (Shanghai, China). Among these, four eyes
of two patients were treated with photorefractive keratectomy (PRK)
20 years ago (June, 1998-October, 1999) and 12 eyes of six patients
were treated with laser in situ keratomileusis (LASIK) 10
years ago (August, 2006-September, 2009). There was no
intraoperative or postoperative complication during the first
operation and the diopters of all patients were stable during the
last 2 years.
All patients underwent a full ophthalmic evaluation
pre-operatively and met the surgical requirements. The uncorrected
visual acuity (UCVA), best-corrected visual acuity (BCVA), manifest
refractive error, intraocular pressure (IOP; non-contact tonometer;
Topcon), anterior chamber depth (ACD; Pentacam; Oculus),
endothelial cell density (ECD; Topcon-SP), corneal topography
(Pentacam), slit-lamp microscopy, funduscopic examination and
visual quality (OQAS; Terrassa) measurements were performed prior
to surgery.
Surgical scheme design
In view of the inherent measurement of refractive
errors in eyes after corneal refractive surgery, the pre-operative
subjective refraction was assessed using the same illumination
conditions by two experienced residents who were trained to measure
refractive errors using a comprehensive refractometer. The patient
underwent small pupil refraction and cycloplegia refraction. In
addition, considering the relatively advanced age of the patients,
the diopters (D) were easily overcorrected after corneal refractive
surgery; therefore, emmetropia was usually selected as the target
refraction in the dominant eye and the target D was adjusted to
retain -0.50 D in the non-dominant eye when the patients were
>45 years of age.
Inclusion criteria
An anterior chamber depth of ≥2.80 mm and an
endothelial cell density >2,000 cells/mm2 were
included in the inclusion criteria in the present study. It
required that patients have a reasonable expectation of surgical
outcomes and patients with keratoconus, cataract or glaucoma and
systemic disease were excluded. The baseline data of all patients
are listed in Table I.
 | Table ICharacteristics of participants who
underwent refractive error adjustment with the collamer lens
implantation (n=16 eyes). |
Table I
Characteristics of participants who
underwent refractive error adjustment with the collamer lens
implantation (n=16 eyes).
| A, General |
|---|
| Variable | | Value |
|---|
| Age (years) | | |
|
Mean ±
SD | | 39.16±7.52 |
|
Range | | 32-47 |
| Sex
(male/female) | | 3/5 |
| Safety
indicesa | | 1.26±0.21 |
| Efficacy
indicesb | | 1.19±0.24 |
| B, Pre- and
post-operative parameters |
| Variable | Pre-operative | Post-operative (6
months) |
| Manifest spherical
equivalent (D) | -4.26±1.55 | -0.53±0.12 |
| Manifest cylinder
(D) | -0.75±0.23 | -0.37±0.09 |
| LogMAR UCVA | 0.68±0.19 | 0.06±0.10 |
| LogMAR BCVA | 0.09±0.08 | -0.02±0.07 |
Surgical procedure
All surgeries were performed by the same experienced
surgeon (JZ). In the present study, the ICL model was ICL V4c with
a 0.36-mm central artificial hole (ICL V4c™; STAAR Surgical). For
ICL V4c implantation, without pre-operative peripheral iridotomy or
intraoperative iridectomy, the procedure was different from the V4
surgery process. On the day of surgery, the pupils of patients were
first enlarged. After topical anesthesia, a model V4c ICL was
inserted into the anterior chamber through a 3-mm temporal clear
corneal incision without sodium hyaluronate injection. When ICL V4c
was injected into the anterior chamber, viscoelastic agent was
injected into the surface of the ICL in the anterior chamber, and
the ICL was then adjusted to enter the posterior chamber.
Afterwards, the viscoelastic surgical agent was easily washed out
of the anterior chamber using automatic irrigation/aspiration.
Postoperative follow-up
All surgeries were uneventful and no intraoperative
complications occurred. After surgery, 0.1% tobramycin
dexamethasone eye drops (Tobradex; Alcon) were prescribed three
times daily for 1 week, after which the dose was tapered off over 2
weeks. Steroidal medication was provided at any time if the IOP
monitoring suggested that it was required. Antibiotic medications
(ofloxacin; Santen) were given four times daily for 1 week and
artificial tears were administered four times daily for 2
months.
Prior to and 6 months after surgery, the UCVA, BCVA,
Spherical equivalent (SE), IOP, ECD, and ACD were checked (Table II). The optical quality assessment
was performed by OQAS, pre-operatively and 1, 3 and 6 months
post-operatively.
 | Table IIComparison pre- and postoperative
parameters in both eyes undergoing implantable collamer lens (ICL)
implantation after corneal refractive surgery. |
Table II
Comparison pre- and postoperative
parameters in both eyes undergoing implantable collamer lens (ICL)
implantation after corneal refractive surgery.
| | OD (8 eyes) | OS (8 eyes) |
|---|
| Parameters | Preoperative | Post 6 months | P-value | Preoperative | Post 6 months | P-value |
|---|
| Mean SE(D) ± SD | -4.40±1.78 | -0.19±0.23 | <0.01 | -4.15±1.61 | -0.13±0.18 | <0.01 |
| Log MAR UCVA | 0.53±0.19 | 0.05±0.09 | <0.01 | 0.44±0.19 | -0.04±0.05 | <0.01 |
| Log MAR BCVA | 0.08±0.14 | 0.01±0.09 | 0.02 | 0.00±0.01 | -0.05±0.05 | 0.03 |
| IOP (mmHg) | 11.95±2.03 | 12.18±1.99 | 0.18 | 11.54±1.58 | 11.90±1.64 | 0.12 |
| ECD
(cell/mm2) | 2,674.25±110.56 | 2,659.13±98.75 | 0.05 | 2,683.00±99.02 | 2,671.00±101.48 | 0.06 |
| ACD (mm) | 3.29±0.22 | 3.31±0.21 | 0.13 | 3.28±0.24 | 3.31±0.23 | 0.11 |
OQAS measurement
The objective scattering index (OSI), the values of
modulation transfer function (MTF) cutoff frequency, the Strehl
ratio (SR) and the OQAS values (OVs) were used to evaluate the
visual performance. The meanings and calculations of the parameters
were reported in several previous studies (14-16).
The determination of the OSI is an objective evaluation of
intraocular scattered light. The index is calculated by evaluating
the amount of light outside the double-pass retinal intensity point
spread function (PSF) image in relation to the amount of light in
the center (14-16).
The MTF cutoff value is the frequency at which the MTF reaches a
value of 0.01. It refers to the frequency, up to which the eye is
able to focus an object on the retina with a significant 1%
contrast. The three OVs are normalized values of three spatial
frequencies, which correspond to MTF values that describe the
optical quality of the eye for three contrast conditions, commonly
used in ophthalmic practice: 100% (OV 100%), 20% (OV 20%) and 9%
(OV 9%). The SR is the ratio of the central maximum of the
illuminance of the PSF in the aberrated eye to the central maximum
that would be expected in a corresponding aberration-free system
(14-16).
Statistical analysis
All statistical analyses were performed using SPSS
version 20.0 (IBM Corp.) and the results are expressed as the mean
± standard deviation. Repeated-measures analysis of variance was
used to analyze the differences in UCVA, BCVA, IOP and ACD as well
as ECD between the eyes prior to and after the operation.
Pre-operative and post-operative visual quality was determined at
different time-points by using repeated-measures analysis of
variance, followed by Tukey's post hoc test. P<0.05 was
considered to indicate statistical significance. Pearson's
correlation coefficient analysis was used to calculate the degree
and significance of correlation between the achieved and predicted
MRSE.
Results
Clinical features of patients. All surgeries
were uneventful and no post-operative complications were observed
during the 6-month follow-up. The pre-operative LogMAR UCVA and
BCVA was 0.68±0.19 and 0.09±0.08, respectively (Table I). After the ICL implantation, the
LogMAR UCVA and BCVA improved significantly, to 0.06±0.10 and
-0.02±0.07, respectively (P<0.001). The mean values of manifest
refractive spherical equivalent (Mean SE) changed from -4.40±1.78 D
pre-operatively to -0.19±0.23 D in the right eye at post-operative
6 months and changed from -4.15±1.61 D pre-operatively to
-0.13±0.18 D in the left eye at 6 months post-operatively (Table II). The parameters of binocular
vision 6 months after surgery were compared and the differences in
UCVA, BCVA and SE prior to and after surgery were statistically
significant, but there was no significant difference in IOP, ECD
and ACD prior to and after surgery (Table II).
Visual outcomes
At 6 months after surgery, none of the examined eyes
exhibited a loss in BCVA of one line or more. Regarding BCVA, four
eyes did not change after surgery, eight eyes gained one line and
four eyes gained two lines (Fig.
1). The safety indices (mean post-operative BCVA/mean
pre-operative BCVA) and the efficacy indices (mean post-operative
UCVA/mean pre-operative BCVA) at 6 months were 1.26±0.21 and
1.19±0.24, respectively (Table
I).
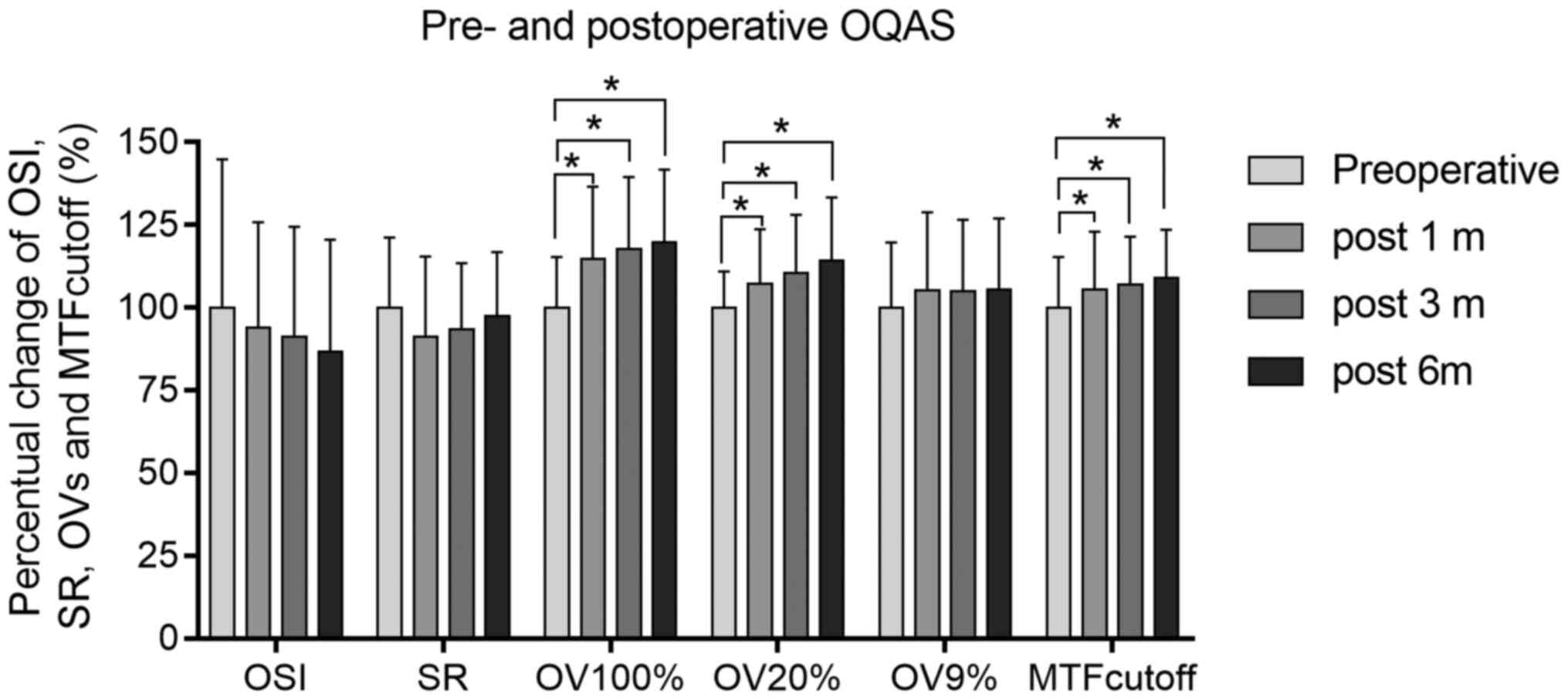
OQAS results
There was no statistically significant difference in
the OSI, SR and OVs at contrasts of 9% at 1, 3 and 6 months after
ICL implantation, respectively. However, there were significant
differences in the MTF cutoff frequency and OVs at contrasts of 100
and 20%, pre-operatively and 1, 3 and 6 months post-operatively
(repeated-measures analysis of covariance; P<0.05). These
results are summarized in Table
III and Fig. 2.
 | Table IIIOptical quality parameters in eyes
subjected to implantable collamer lens implantation after corneal
refractive surgery. |
Table III
Optical quality parameters in eyes
subjected to implantable collamer lens implantation after corneal
refractive surgery.
| | Post-operative | P-value | |
|---|
| OQAS parameter | Pre-operative | 1 month | 3 months | 6 months | Pre-operative vs. 1
month | Pre-operative vs.
post 3 months | Pre-operative vs.
post 6 months |
|---|
| MTF cutoff | 28.739 | 30.274 | 30.738 | 31.294 | <0.001 | <0.001 | <0.001 |
| OSI | 1.550 | 1.516 | 1.469 | 1.399 | 0.165 | 0.153 | 0.142 |
| SR | 0.183 | 0.171 | 0.175 | 0.187 | 0.089 | 0.104 | 0.130 |
| OV100% | 0.890 | 1.021 | 1.048 | 1.066 | <0.001 | <0.001 | <0.001 |
| OV20% | 0.654 | 0.701 | 0.723 | 0.748 | 0.008 | 0.006 | 0.005 |
| OV9% | 0.483 | 0.509 | 0.507 | 0.509 | 0.122 | 0.134 | 0.121 |
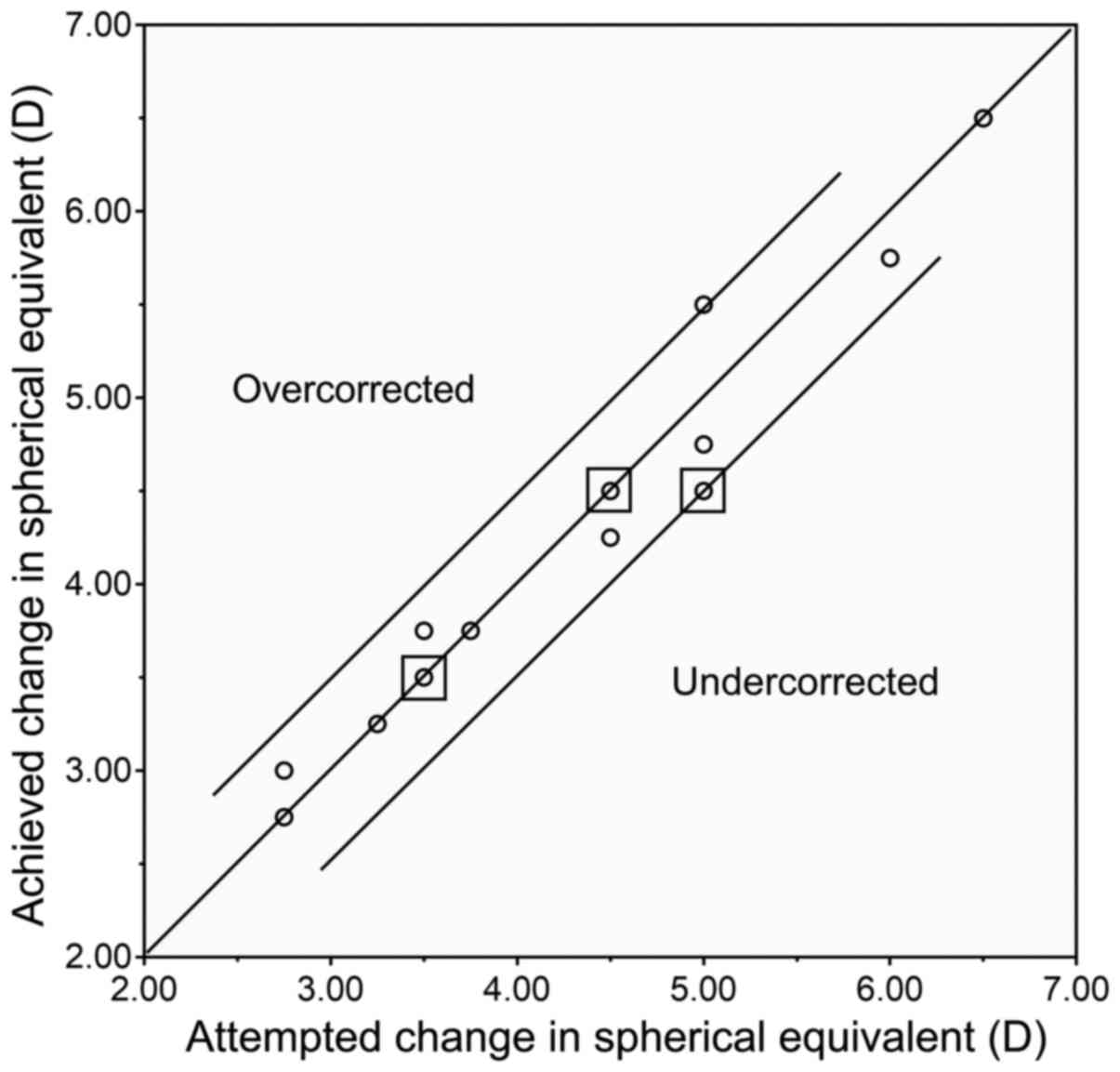
Changes in MRSE
The deviation of the achieved MRSE from the
predicted MRSE was determined. At 6 months, all eyes were within
0.50 D of the target refractive change (Pearson's correlation,
R=0.944; P<0.0001; Fig. 3).
Discussion
Posterior chamber phakic intraocular lens (pIOL)
implantation is a safe and effective refractive surgery that has
been widely accepted. Previous studies have demonstrated that ICL
implantation is better than corneal refractive surgery for the
correction of moderate and high myopia, particularly in terms of
the reduced disturbance of night vision (17-19).
However, data regarding the consequences of ICLs with a central
hole for residual refractive error correction after corneal
refractive surgery are scarce. The aim of the present study was to
evaluate the efficacy, safety, predictability and quality of vision
in patients who underwent posterior chamber ICL V4c implantation
for residual refractive error after corneal refractive surgery.
In the present study, an improvement in UCVA was
obtained after ICL V4c implantation for residual refractive error
correction after corneal refractive surgery, and at 6 months after
the second surgery, all eyes gained a UCVA of 20/20 or better. The
efficacy index was 1.19 at 6 months post-operatively, which was
good, with a BCVA of -0.02±0.07. An effective index greater than or
equal to 1 indicates that the surgery was effective. The safety
index was 1.26. In our study, most eyes maintained the BCVA, and
some gained more lines of BCVA, which was consistent with findings
from previous case reports (18,19). A
safety index ≥1 indicates that the operation is safe and
acceptable. In the follow-up period, none of the eyes lost >1
line of BCVA. The predictability was also high; 100% of eyes were
within ±0.50 D of the predicted refractive change. At
post-operative 6 months, the MRSE of all patients was near
emmetropia (R=0.944).
In agreement with those of previous studies
(20,21), the present study demonstrated good
results obtained with ICL for residual refractive error correction
after corneal refractive surgery and provided a contribution to
accurate pre-operative optometry. In the implantation of
posterior-chamber ICLs, the calculation appeared less dependent on
corneal refractive power but more on precise subjective refraction.
The reliability of autorefractometry after corneal refractive
surgery is influenced by the pre-operative amount of myopia and the
laser optic ablation zone (22).
Since the cornea becomes more flattened after laser surgeries,
there are more possibilities of positive spherical aberration,
which results from different focusing of the beams on the
peripheral and central part of an optical system (23). When increasing the positive
spherical aberration after corneal refractive surgery, higher
refractive power are encountered in the pupil area by peripheral
imaging rays, where the retinal image form appears to be more
myopic compared with subjective refraction (22). In consideration of these factors,
reasonable adjustments were made during the design of the operation
plan according to age and previous surgical history.
Furthermore, the present study indicated that there
was no significant difference in the OSI, SR and the OVs among the
optical quality parameters at contrasts of 9%, pre-operatively and
post-operatively. However, significant changes of the MTF cutoff
frequency were obtained in the present study, as well as OVs at
contrasts of 100 and 20% prior to and after surgery. The OVs at
contrasts of 100% were directly related to the MTF cutoff frequency
(it is the MTF cutoff frequency divided by 30 cycles/degree), which
reflects the patients' vision during the day. In the present study,
there were significant differences in the MTF cutoff frequencies
and OVs at contrasts of 100 and 20%, which indicated that ICL
implantation for correcting residual myopia contributed to good
visual quality mainly during the daytime. ICL implantation does not
involve surgical tissue abstraction and leaves the central cornea
untouched; therefore, the visual quality was essentially improved
post-operatively. However, the night vision loss due to corneal
refractive surgery cannot be improved. In the present study, all
patients had undergone corneal refractive surgeries a few years
earlier and had increased cornea spherical aberration, which partly
contributed to the changes in contrasts of 9% OVs after ICL
implantation. After the corneal refractive surgeries, the corneal
total higher-order aberrations (HOAs) and spherical aberration are
usually increased (24,25), which may lead to greater intraocular
scattering after the second operation and affect the visual quality
at contrasts of 9%. OVs at contrasts of 9% simulate night vision,
which may be disturbed after corneal laser refractive surgery,
including PRK or LASIK, which has been reported to be the main
factor affecting night vision due to increased spherical aberration
(25-27).
Compared with that used in previous studies
(28-30),
a novel type of ICL with a central hole, without pre-operative
peripheral iridotomy, was used in the present study, and good
results were also obtained. It was previously reported that the
presence of a central hole ICL implantation provided an excellent
visual performance almost equivalent to that obtained with
conventional ICLs (14). In
addition, to evaluate the objective visual quality
post-operatively, an OQAS, an advanced tool for quantitatively
evaluating optical quality changes after refractive surgeries, was
used in the present study. According to the present results, the
implantation of ICL with a central hole did not induce a
significant additional change in the subjective intraocular forward
scattering. These results were in agreement with those of previous
studies, which demonstrated that ICL implantation resulted in
almost no interference with the visual quality, as there was no
statistically significant change in OSI after surgery (14,18,31).
Implantation of ICL with central hole significantly improved the
optical quality, including the MTF cutoff frequency and OVs at
contrasts of 100 and 20% in a clinical setting. It is therefore
indicated that this is a good surgical option for the correction of
residual refractive error after corneal refractive surgeries.
There were several limitations to this study. First,
the sample size of the present study was relatively small from a
statistical viewpoint and the follow-up time was short. If the
thickness of the cornea was sufficient, most patients chose laser
surgery for re-correction, so the number of patients who used ICL
implantation for secondary surgery was relatively small. Another
limitation was that the pre-operative and post-operative corneal
total HOAs and spherical aberration, which are important factors
for evaluating quality of vision, were not assessed. In addition,
the subjective quality of vision was not comprehensively evaluated,
e.g. by administering a patient questionnaire for night vision.
In conclusion, the present study demonstrated
significantly improved optical quality parameters, such as the MTF
cutoff frequency, SR, OSI and OVs at contrasts of 100, 20 and 9%,
for patients after corneal refractive surgery undergoing ICL
implantation. These results suggested that ICL implantation
achieved encouraging results in the correction of residual
refractive errors after corneal refractive surgery. Further studies
are required to assess patient satisfaction and evaluate subjects
for longer post-operative follow-up periods to confirm the safety
of the procedure.
Acknowledgements
Not applicable.
Funding
This work was partially supported by the
Cross-disciplinary Research Fund of Shanghai Ninth People's
Hospital, Shanghai Jiao Tong University School of Medicine (grant
no. JYJC201907). The funding body had no role in the design or
conduct of the study, the collection, management, analysis or
interpretation of the data, the preparation, review or approval of
the manuscript or in the decision to submit the manuscript for
publication.
Availability of data and materials
The datasets used and/pr analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XQF analyzed and interpreted the patient data
regarding the patients. FLH and YL performed the ocular
examination. JZ was a major contributor in writing the manuscript
and performed all surgeries. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The present study was approved by the ethics
committee of The Ninth Hospital of Jiao Tong University (Shanghai,
China). It followed the tenets of the Declaration of Helsinki.
Written informed consent was obtained from all patients after the
possible consequences of the study were explained.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Jiménez-Alfaro I, Gómez-Tellería G, Bueno
JL and Puy P: Contrast sensitivity after posterior chamber phakic
intraocular lens implantation for high myopia. J Refract Surg.
17:641–645. 2001.PubMed/NCBI
|
|
2
|
Uusitalo RJ, Aine E, Sen NH and
Laatikainen L: Implantable contact lens for high myopia. J Cataract
Refract Surg. 28:29–36. 2002.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lackner B, Pieh S, Schmidinger G,
Hanselmayer G, Dejaco-Ruhswurm I, Funovics MA and Skorpik C:
Outcome after treatment of ametropia with implantable contact
lenses. Ophthalmology. 110:2153–2161. 2003.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kamiya K, Shimizu K, Igarashi A, Hikita F
and Komatsu M: Four-year follow-up of posterior chamber phakic
intraocular lens implantation for moderate to high myopia. Arch
Ophthalmol. 127:845–850. 2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Moshirfar M, Jehangir N, Fenzl CR and
McCaughey M: LASIK enhancement: Clinical and surgical management. J
Refract Surg. 33:116–127. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Schallhorn SC, Venter JA, Hannan SJ,
Hettinger KA and Teenan D: Flap lift and photorefractive
keratectomy enhancements after primary laser in situ keratomileusis
using a wavefront-guided ablation profile: Refractive and visual
outcomes. J Cataract Refract Surg. 41:2501–2512. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Siedlecki J, Luft N, Kook D, Wertheimer C,
Mayer WJ, Bechmann M, Wiltfang R, Priglinger SG, Sekundo W and
Dirisamer M: Enhancement after myopic small incision lenticule
extraction (SMILE) using surface ablation. J Refract Surg.
33:513–518. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Solaiman KA, Fouda SM, Bor'i A and
Al-Nashar HY: Photorefractive keratectomy for residual myopia after
myopic laser in situ keratomileusis. J Ophthalmol.
2017(8725172)2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sanders DR, Doney K and Poco M: ICL in
Treatment of Myopia Study Group. United States food and drug
administration clinical trial of the implantable collamer lens
(ICL) for moderate to high myopia: Three-year follow-up.
Ophthalmology. 111:1683–1692. 2004.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Alfonso JF, Baamonde B, Fernández-Vega L,
Fernandes P, González-Méijome JM and Montés-Micó R: Posterior
chamber collagen copolymer phakic intraocular lenses to correct
myopia: Five-year follow-up. J Cataract Refract Surg. 37:873–880.
2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Moya T, Javaloy J, Montés-Micó R, Beltrán
J, Muñoz G and Montalbán R: Implantable collamer lens for myopia:
Assessment 12 years after implantation. J Refract Surg. 31:548–556.
2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Dougherty PJ and Priver T: Refractive
outcomes and safety of the implantable collamer lens in young
low-to-moderate myopes. Clin Ophthalmol. 11:273–277.
2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kamiya K, Shimizu K, Igarashi A, Kitazawa
Y, Kojima T, Nakamura T, Oka Y and Matsumoto R: Posterior chamber
phakic intraocular lens implantation: Comparative, multicentre
study in 351 eyes with low-to-moderate or high myopia. Br J
Ophthalmol. 102:177–181. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kamiya K, Shimizu K, Saito A, Igarashi A
and Kobashi H: Comparison of optical quality and intraocular
scattering after posterior chamber phakic intraocular lens with and
without a central hole (Hole ICL and Conventional ICL) implantation
using the double-pass instrument. PLoS One.
8(e66846)2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Güell JL, Pujol J, Arjona M, Diaz-Douton
F and Artal P: Optical quality analysis system; instrument for
objective clinical evaluation of ocular optical quality. J Cataract
Refract Surg. 30:1598–1599. 2004.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Saad A, Saab M and Gatinel D:
Repeatability of measurements with a double-pass system. J Cataract
Refract Surg. 36:28–33. 2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Sanders DR: Matched population comparison
of the visian implantable collamer lens and standard LASIK for
myopia of -3.00 to -7.88 diopters. J Refract Surg. 23:537–552.
2007.PubMed/NCBI
|
|
18
|
Liu HT, Zhou Z, Luo WQ, He WJ, Agbedia O,
Wang JX, Huang JZ, Gao X, Kong M, Li M and Li L: Comparison of
optical quality after implantable collamer lens implantation and
wavefront-guided laser in situ keratomileusis. Int J Ophthalmol.
11:656–661. 2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kamiya K, Shimizu K, Igarashi A and
Kawamorita T: Effect of myopic defocus on visual acuity after
phakic intraocular lens implantation and wavefront-guided laser in
situ keratomileusis. Sci Rep. 5(10456)2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kamiya K and Shimizu K: Implantable
collamer lens for hyperopia after radial keratotomy. J Cataract
Refract Surg. 34:1403–1404. 2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Srinivasan S, Drake A and Herzig S: Early
experience with implantable collamer lens in the management of
hyperopia after radial keratotomy. Cornea. 27:302–304.
2008.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Mirshahi A, Wesemann W, Bühren J and
Kohnen T: Factors influencing the reliability of autorefractometry
after LASIK for myopia and myopic astigmatism. Am J Ophthalmol.
150:774–779. 2010.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Gatinel D, Adam PA, Chaabouni S, Munck J,
Thevenot M, Hoang-Xuan T, Pieger S, Fujieda M and Bains HS:
Comparison of corneal and total ocular aberration before and after
myopic LASIK. J Refract Surg. 26:333–340. 2010.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Sarkar S, Bharadwaj SR, Reddy JC and
Vaddavalli PK: Longitudinal changes in optical quality, spatial
vision, and depth vision after laser refractive surgery for myopia.
Optom Vis Sci. 97:360–369. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Lee K, Ahn JM, Kim EK and Kim TI:
Comparison of optical quality parameters and ocular aberrations
after wavefront-guided laser in-situ keratomileusis versus
wavefront-guided laser epithelial keratomileusis for myopia.
Graefes Arch Clin Exp Ophthalmol. 251:2163–2169. 2013.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Kung JS and Manche EE: Quality of vision
after wavefront-guided or wavefront-optimized LASIK: A prospective
randomized contralateral eye study. J Refract Surg. 32:230–236.
2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Anera RG, Castro JJ, Jiménez JR, Villa C
and Alarcón A: Optical quality and visual discrimination capacity
after myopic LASIK with a standard and aspheric ablation profile. J
Refract Surg. 27:597–601. 2011.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Chen X, Wang XY, Zhang X, Chen Z and Zhou
XT: Implantable collamer lens for residual refractive error after
corneal refractive surgery. Int J Ophthalmol. 9:1421–1426.
2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Lee J, Kim Y, Park S, Bae J, Lee S, Park
Y, Lee J and Lee JE: Long-term clinical results of posterior
chamber phakic intraocular lens implantation to correct myopia.
Clin Exp Ophthalmol. 44:481–487. 2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Pjano MA, Pidro A, Biscevic A, Grisevic S,
Pandzic B and Cerovic V: Refractive outcomes of posterior chamber
phakic intraocular lens implantation for correction of myopia and
myopic astigmatism. Med Arch. 71:93–96. 2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Iijima A, Shimizu K, Yamagishi M, Kobashi
H, Igarashi A and Kamiya K: Assessment of subjective intraocular
forward scattering and quality of vision after posterior chamber
phakic intraocular lens with a central hole (Hole ICL)
implantation. Acta Ophthalmol. 94:e716–e720. 2016.PubMed/NCBI View Article : Google Scholar
|