Introduction
Trochanteric fractures occurring in adults represent
a challenging pathology from an orthopedic point of view. Most of
these patients are old, with associated comorbidities and sometimes
with fractures resulting from high intensity trauma. Mechanical
complications are in general less frequent than systemic ones. Some
of the truly elderly patients or the ones with various lytic tumors
present at the emergency room with pertrochanteric fractures
resulting from low-level trauma. Most complications are due to
severe osteoporosis or malposition of the implant. Although
rheumatological research is still in progress, osteoporosis
treatment has not yet succeeded to reduce the complications of
trochanteric fractures, which are increasing in older patient
groups (1). The poor compliance of
patients undergoing rheumatological treatments may be one of the
causes for pertrochanteric fractures (2,3).
Increasing life expectancy in Romania (75.31 years, data from
TheWorldBank.com) also may be a factor for this
increasing pathology.
Elderly patients, unless operated rapidly, may lose
the will to resume walking; therefore, a conservative, non-surgical
treatment is not desirable. Studies in literature showed a higher
mortality rate and poor functional results after conservative
approach.
The most frequent types of surgical treatment used
in this pathology are those of reduction and osteosynthesis with
intramedullary nails, DHS, as extramedullary osteosynthesis
(4,5).
Our method of choice in treating this pathology is
the reduction and internal fixation with a titanium made gamma-nail
system. Due to some complications encountered during our practice,
we decided to make an ample review of literature, an adequate
analysis of our complicated cases and a mechanical test of the
implant we used, in order to identify the factor that influences
the breakage point.
Trochanteric fractures are fractures that affect the
proximal 1/3 of the femur, starting from the base of the femoral
neck up to 5 cm below the small trochanter (6).
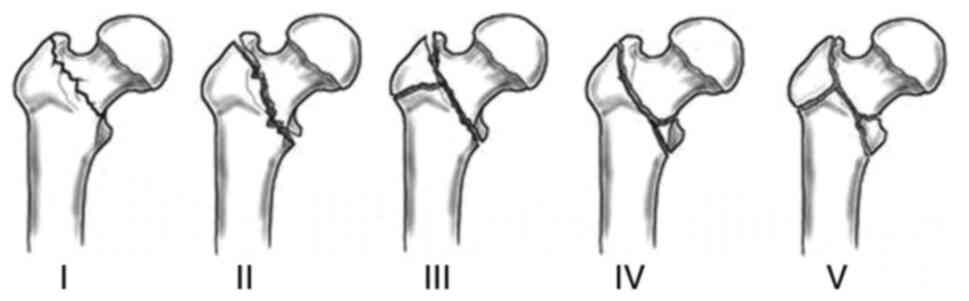
Although there are several classifications used for
this anatomical region based on various factors, the most common
are those based on the fracture path (7,8) and
the degree of comminution. In this study, we used the Evans
Classification, which is divided into five types, starting with the
first one (non-displaced with 2 fragments) and ending with the V
degree, where comminution is high (Fig.
1) (9). The classifications of
pertrochanteric fractures, like all classifications, have their
limitations regarding reproducibility. The main challenge is to
achieve a satisfactory reduction, before surgery, under C-Arm
X-rays.
An increasing number of cases of pertrochanteric
fractures affecting the elderly were reported in hospitals across
Romania. Pertrochanteric fractures are associated with increased
bone fragility, with falls from the same level or with psychiatric
or heart problems, in some patients (10).
The diagnosis of trochanteric fracture is made
clinically, the affected limb being shortened and in adduction plus
external rotation. Although the diagnosis is clinical in most
cases, type 1 trochanteric fractures in the Evans classification do
not display an external rotation and the diagnosis cannot be
complete without an X-ray in the anteroposterior and lateral
incidence, since imaging is crucial in determining the
classification (Fig. 2). The X-ray
exposure can be completed with a CT in cases where a fracture is
suspected on pathological background.
Trochanteric fractures are common in patients over
70 years of age who have various comorbidities, among which
malnutrition and severe osteoporosis (11).
In patients aged 70 years, the immediate
postoperative complications are represented by the loss of the
ability to walk, as well as the failure to cope psychiatrically and
emotionally. Rehabilitation has a crucial role and it is sometimes
hard to exert.
The treatment of this pathology must be quick, with
limited blood loss and a fast recovery of walking. Theoretically,
the patient should be encouraged to walk immediately after surgery,
even at the risk of full weight bearing on the fractured limb.
Regardless of the chosen treatment, the complications that may
occur pre- or postoperatively, the treatment of pain, the
prevention of pulmonary thromboembolism and the maintenance of an
adequate musculature must be taken into account.
From the analysis of cases with failed mechanical
device stability, we aimed to identify the causes that lead to
reintervention and sometimes death from a scientific point of
view.
Materials and methods
During surgery, we follow the international
guidelines and the manufacturer's implanting technique. In all
cases, we struggle to achieve a close-to-perfect preoperative
fracture reduction. The positioning of the patient is important.
The orthopedic Table is used and the fracture is reduced, a
maneuver that later helps us when implanting the nail in the ideal
position. The maneuver of reduction on the orthopedic Table is
performed under radiological control.
Small incisions are performed and the nail is
implanted intramedullary and stabilized. X-rays are used on all
patients to verify the correct position. The ideal position for the
lag screw is inferior and posterior in the femoral head (12). For all our patients, Gamma nail
implants made of titanium were used, from the same manufacturer.
The implant had cervical-diaphyseal angle of 125̊, a distal
diameter of 10 mm, a U-lag screw, and a distal static screw. Since
we encountered one case with a broken implant, we decided to
analyze in laboratory conditions in order to identify what are the
factors that influenced its durability. Patients with severe
osteoporosis were included in this study to verify the efficiency
of fast rehabilitation program with immediate full weight bearing.
Patients with non-consolidation were included and also one patient
with implant failure, due to septic complications.
Stress testing on the implant was done in a
different center. Extremely interesting findings led us to a close
check on the nail's surgical tray for accuracy and measurement
tolerances. Results will be discussed later in the report.
The study was approved by the Ethics Committee of
‘Foişor’ Orthopedics-Traumatology and Osteoarticular TB Hospital
(Bucharest, Romania). All patients provided a signed informed
consent.
Twenty-three patients with previous osteoporosis
were included in the study, 10 were not allowed for full weight
bearing until 6 weeks after surgery, and 12 were following a fast
recovery program, with early walking. Osteoporosis was diagnosed
for all before surgery, and all the patients were under treatment
for this pathology. T-score was recorded for each patient.
One patient, operated in another clinic, was
admitted in our hospital, in the emergency room, with severe
sepsis. A failed and displaced implant was identified on the
X-rays. The CT scan was necessary in order to examine any secondary
septic determinations.
One patient operated in another emergency clinic
with a DCS system for a right hip fracture needed second surgery.
The gamma nail that we used failed after one year. A full set of
blood tests were performed for all patients.
Results
Titanium and titanium alloys, which have been used
widely as biomedical implant materials since the 1970s, possess the
desired properties or biomedical applications, such as excellent
biocompatibility, good corrosion resistance, and high ratio
strength (13-15).
In this study, we only used the same brand of titanium nails.
Twenty-three patients with osteoporosis were
included in the study. Follow-up was at 6 months, until fracture
healing. The average T-score was 2.6 for the whole group. Randomly
assigned, by means of the operating surgeon, 10 patients were not
allowed for full weight bearing rehabilitation (NFWB group). Their
average T-score was 2.7. The other 13 patients had an average
T-score of 2.5 (FWB group). None of these patients had major
comorbidities. All the patients were over 70 years old. No septic
complications were recorded. The body mass index (BMI) was between
26-31. No significant influence was identified; therefore, the
topic was not addressed.
The average T-score was not statistically
significant (P>0.01), small differences in the T-score did not
change the postoperative results. The only difference in the
rehabilitation program, between the two groups, was the full weight
bearing indication. NFWB group had 1 case of screw cut-out that
needed reintervention. Lag screw was malpositioned. Weight bearing
was possible, but with moderate pain. The patient had a
reintervention, with total hip arthroplasty with revision stem. 10%
of this group had cut-out complications.
In the FWB group, 3 patients had cut-out screws,
with gradual moderate pain. One patient had a small screw
displacement, but without cut-out. Twenty-three percent of these
patients encountered mechanical complications during the first 3
months. Statistically, early weight bearing does not benefit from
the postoperative results, increasing the number of osteoporotic
patients with mechanical failures (P<0.01). Taking into
consideration that one of these cases had the lag screw positioned
in a non ideal location, statistically, it seems that faster
rehabilitation does not increase the chance of screw cut-out with a
big percent, but in fact, the screw position is the most
important.
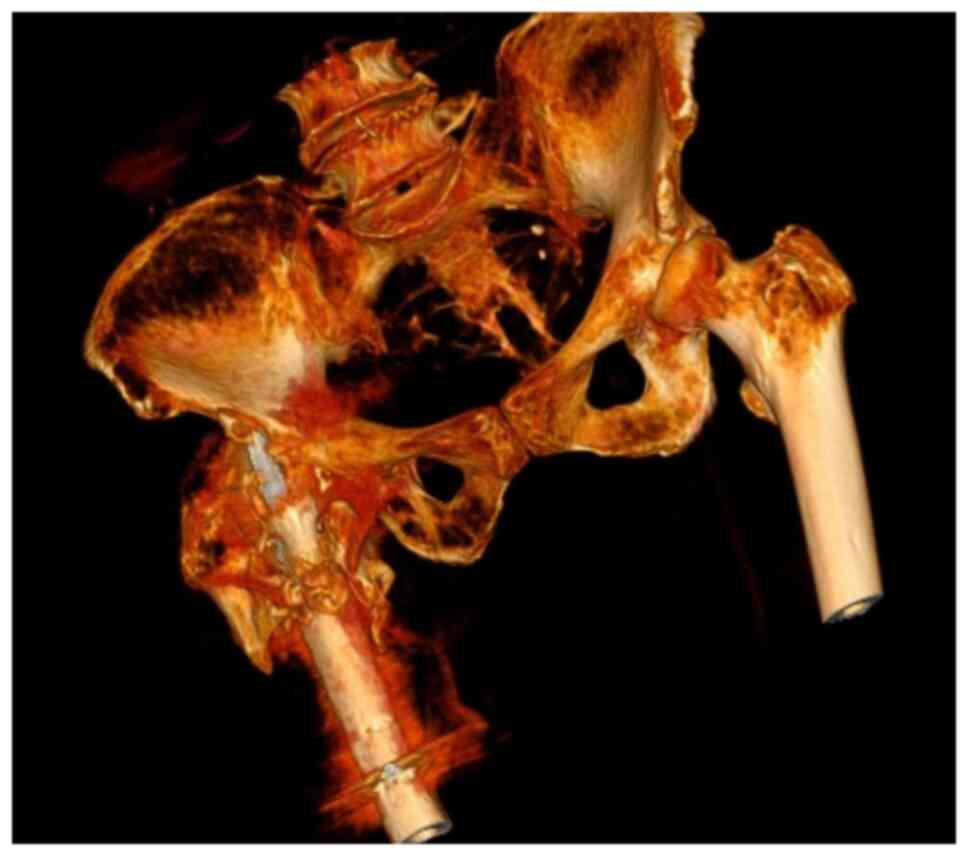
The second aspect of this study is represented by a
patient with bilateral hip fractures (~2 years distance between
fractures), operated in another emergency clinic with a DCS system.
We changed the implant with an intramedullary nail. The right hip
is of interest for this research. We applied the same method, but
this time the nail broke after 6 months. The screw position was
optimal. The insufficient restore of lateral femoral cortical bone
was identified as the cause. The stress shielding forces were high
and the bone healing was incomplete. The nail broke in the proximal
part. A good solution was bone grafting and a longer nail. The same
screw position was used the second time. Pain levels were low and
the patient was able to walk. No follow-up was possible (Figs. 3 and 4). No sign of infection was identified.
There were no skin complications and the bacterial cultures were
negative.
An 83 years old patient, female, with diabetes,
represents the third part of this report. She presented at the
emergency room with pain. Weight bearing was impossible. She had a
pertrochanteric fracture operated a year before in another service.
The implant was compromised with no signs of callus. Blood sugar
levels were uncontrolled and at the clinical exam, we identified
multiple sacral sores. Clinical signs of shoulder arthritis were
present. The affected thigh was 12 cm larger in diameter, hot and
associated with redness. We decided to perform surgery and
drainage. The following day, the patient was in a semicomatose
state. During surgery, an extremely large quantity of pus was
extracted.
During the same night, the patient went into septic
shock with high potassium levels and anuria. She was unresponsive
to norepinephrine and epinephrine. Death was recorded in the same
night. Slow evolving sepsis, associated with comorbidities and a
failed implant, all collaborated to the occurrence of the septic
shock.
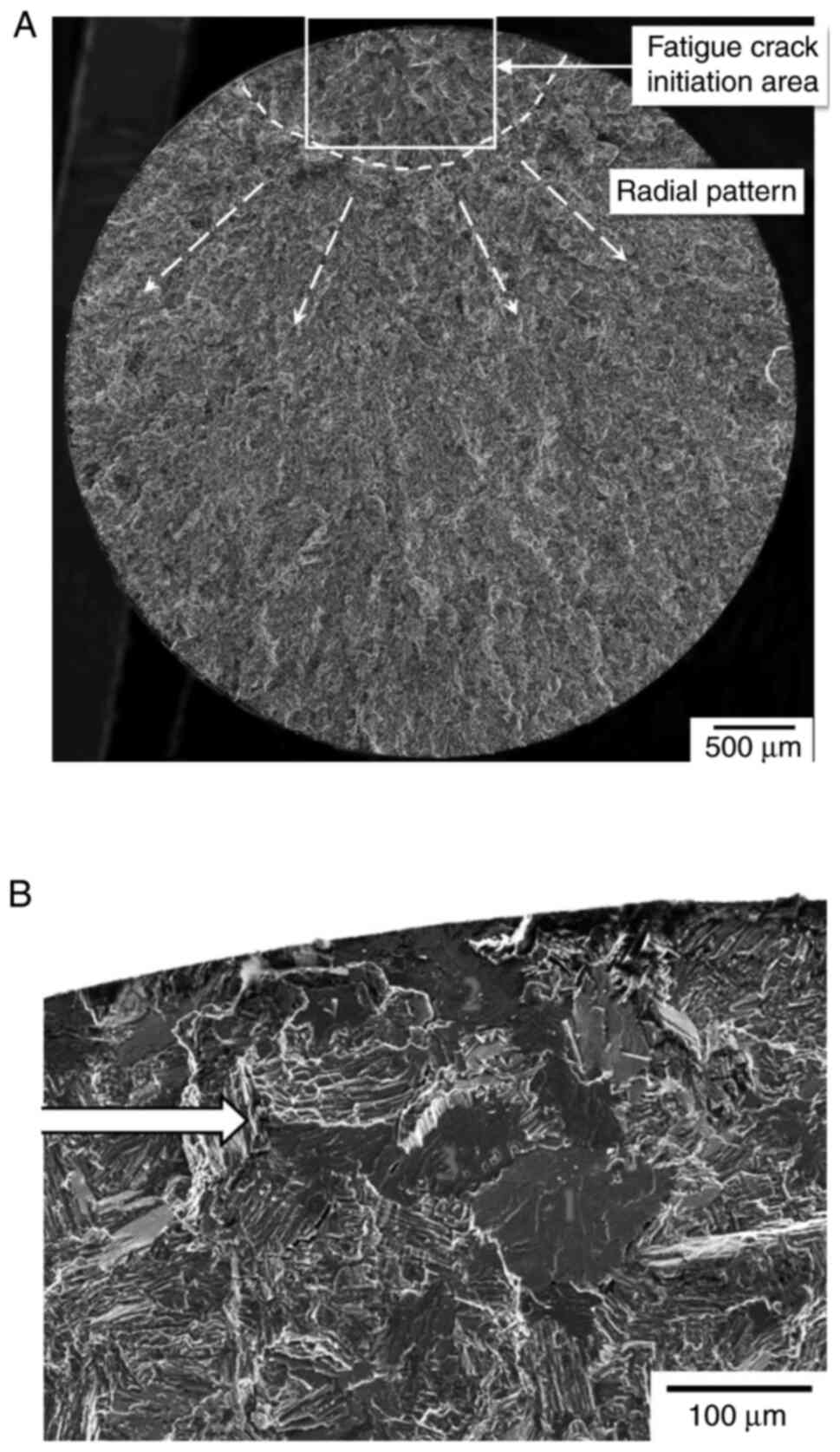
The proximal part of the broken nail was sent for
analysis. Metallurgic tests and scanning with an electronic
microscope were performed. Fatigue zones were identified at the
contact between the nail and the screw. It is well-known that most
of the fatigue cracks initiate at free surface. This phenomenon
occurs only in special cases when a very high cycles fatigue test
is performed (Fig. 5A and B) (16).
This type of changes in the structure were not
confirmed at low-cycle or high-cycle fatigue tests for
TIAl6V4(17). We suspected that
nonunion of the fracture was not the only cause of breakage. High
tolerances of the lag screw guide (from multiple uses) led to small
errors in the screw placement. Small dents were seen under
microscope at the beginning of the primary fissure. The rigidity of
the implant (titanium alloy) may eliminate micro-motions in the
axial plane at the fracture site (producing delayed healing),
causing extra load relative to the femur, that further causes
stress shielding. Our theory is also confirmed by other articles.
It took over 6 month for the nail to break. We found an average
duration until failure of over 10 months in most studies (18-20).
Checking the guide for the lag screw, we identified
an average of 1.4 mm error, from 10 tests. The cause for this error
was the locking hex screw that locks the guide to the nail and also
the threaded kirschner wire, used as a guide. That allows small
errors at the passing of the drill through the nail. Small
scratches on the coating and inside the nail's hole were
observed.
The last case was an extremely misplaced implant
with associated severe sepsis and non-union (Figs. 6 and 7). In this particular case, there was a
drastic error in the reduction of the fracture, associated with
life threatening comorbidities.
Discussion
The number of patients with peritrochanteric
fractures is increasing, most likely due to the increase of average
life span. Considering the gravity of this traumatic event, it is
important to determine the factors that contribute and are
associated with the failure of implant fixation. We tried to
approach this subject from a different point of view. We focused on
some particular cases that could lead us to some new presumption of
why these systems sometimes fail. There are few publications on
this topic and sometimes data are incomplete.
Peritrochanteric fractures represent a major issue
of public health, as they are responsible for morbidity, increased
mortality and high costs. Usually, after this type of surgery, the
rehabilitation period is very long.
There is a constant debate about fast rehabilitation
associated with weight bearing, as well as non-weight bearing
protocols. Could this be the primary factor of gamma nail system
fail? Osteoporosis has a prevalence of ~10% in the USA. This number
is considered very high, in an age were physical activity is
decreasing and people's average life span is increasing (21). Most patients that were hospitalized
with hip fractures are also suffering from osteoporosis or at least
osteopenia. In the 23 patients with pre diagnosed osteoporosis and
associated perthrocanteric fractures were included in our study,
resulted from falls from ground level. We excluded lytic bone
lesions as cause of these fractures. The two groups were divided
randomly by the surgeon who performed the operations. In one group,
there was a preference of very fast rehabilitation with weight
bearing (FWB). We observed a very high cut-out rate for these small
group (23%). On the non-weight bearing group, only one case had a
cut-out, but this incident was caused by lag screw
misplacement.
Regarding BMI, there was no statistical correlation
between these groups. The T-score was not relevant either. What we
did note was that the weight bearing indication plays a crucial
role in the outcome of the surgery. In osteoporotic patients, full
weight bearing should be restricted to at least 6 weeks after
surgery. Partial weight bearing can be allowed, but no more than
15% of the body weight. It is important to mention that this
finding is relevant only to patients diagnosed with osteoporosis
(22-24).
Based on our clinical experience, fast
rehabilitation protocols associated with weight bearing decrease
the recovery period after surgery, increase patient satisfaction,
decrease the cost of the medical act and also augment the personal
independence. According to our findings, this approach should be
restricted to patients that have acceptable bone stock accompanied
by an adequate surgical technique. Screw placement plays a crucial
role in the outcome of this type of surgery (22).
One patient that we identified was a 61-year old
woman, with a BMI of 29. She had been operated in our clinic after
a failed DCS system (performed in another regional hospital), used
for a peritrochanteric left hip fracture. The situation on the
right leg was identical. We performed the second surgery, using a
gamma nail fixation. After 6 months, the implant broke. We took
into consideration inadequate reduction and insufficient restore of
the lateral femoral wall as primary causes of failure. Consulting
data from literature, we noted an average duration of over 10
months after nail breakage (18-20).
This finding led us to further investigate the
broken implant, after extraction. On a microscopic view, we
observed small cracks and dents produced by the lag screw in the
hole of the nail. Titanium is an extremely stiff material,
resilient to bending. It tends to increase stress shielding on
fracture level. Small scratches in the weakest point of the nail
can determine a decrease in resistance. In this particular case,
this was the second surgery, so bone healing was slower. Could
small errors in the guiding system cause a decrease of the nail
resistance? We identified up to 1.4 mm of error in the system
guiding instruments tray, caused by multiple use and perhaps also
being inadequate (Fig. 8).
Several cases in literature have reported failed
titanium or titanium alloy implants, specially gamma nails
(19). Nonetheless, the overall
long-term results for this type of material are still extremely
good (25-30).
Most frequently, failure takes place as a result of
high tensile stresses around notches, holes or small indentations.
Exceeding the stress forces within the very thin 1.8-17 nm of
protective coating (titanium oxide TiO2) can produce
small/micro cracks followed by repassivation (31).
This effect is constant and is augmented by the
corrosive environment (oxidative wear). Physiological loading
induces unexpected, high cyclic stress during daily activity,
weight bearing until fracture healing is complete. It is clear that
none of these forces exceed the material's critical breaking point
on one exposure, but it is a relevant issue after a high number of
cycles. Microcracks in the material grow at a slow per-cycle
velocity and can propagate to implant breakage until bone heals
(32). The same principle of
titanium alloy implants breakage was noticed in the modular
systems. Due to small micromotions, the protective titanium oxide
coating was destroyed and the implant failed due to increased
fretting corrosion at the modular interface (33). In our case, the disruption of the
titanium protective coating was iatrogenic. The drill for the
lag-screw, due to small errors in the guiding system produces small
scratches in the protective coating. The fracture site had a slow
healing rate with high stress forces at this level. All led to a
very fast implant breakage. It seems that this error severely
decreased the implant's lifetime.
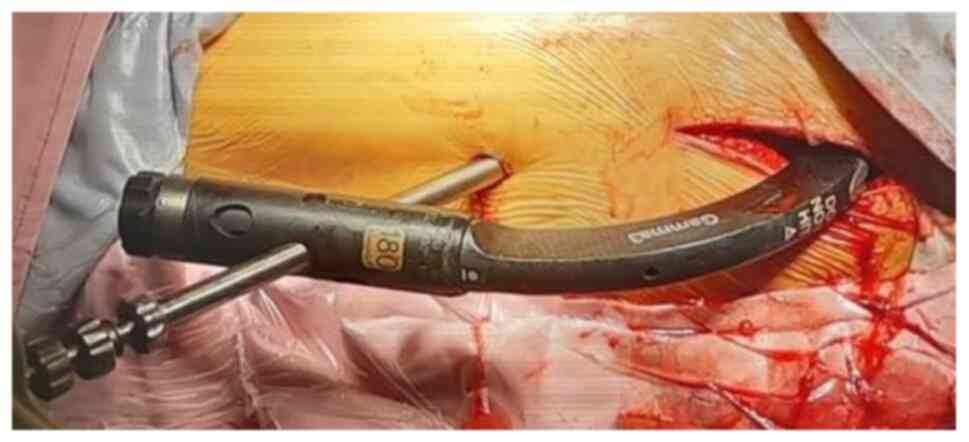
The next case that we analyzed was a failed gamma
nail due to multiple causes. When including this case in the study,
we wanted to advocate the fast reintervention for this type of
patients. An 83-year old diabetic patient presented to our
emergency room with clinical sepsis, with a malpositioned nail,
without fracture reduction, 8 months after surgery in another
hospital. She did not address another hospital services and no
follow-up information was available during this period of time.
Septic signs appeared one month before presenting to our clinic
(family anamnesis, patient had a semicomatose status). At the
clinical exam, we identified a right shoulder arthritis. Since the
patient's status was rapidly declining, we decided to perform
extraction of the implant and debridement (Fig. 9). Unfortunately, during surgery, the
patient went into septic shock.
Failed gamma nails should be addressed rapidly.
Peritrochanteric fractures increase morbidity and in conjunction
with comorbidities can have a very high mortality rate. Septic
complications can lead to sepsis or even shock. We analyzed this
extreme case only to underline the fact that care must be exercised
in fracture preoperative reduction and adequate nail and screw
placement, since implant failing can sometimes lead to death.
Failure of gamma nail implants is not frequent, but
still it must be avoided as much as possible. Such events lead to
additional surgical procedures. In literature, the rate of breakage
is reported in variable proportions; however, it is generally below
5.6% (19,34,35).
There are many causes that may determine this complication.
The aim of this report was to identify lesser-known
facts that can lead to surgical reintervention. According to our
data, some patients have pre-existent osteoporosis. This
comorbidity increases the percentage of implant failure. It is safe
to say that full weight bearing should be allowed 6 weeks after or
to patients that have good bone stock. Faster mobilization after
surgery cannot always lead to good results, especially in old
people with fragile bones. Lag screw placement and preoperative
adequate fracture reduction are critical aspects that greatly
influence the surgical outcome. A displaced implant associated with
fractured delayed healing or cut-out should be addressed rapidly,
since it can increase morbidity and sometimes lead to fatal
complications.
In our study and after a thorough review of major
publications, we have identified a novel factor of gamma nail
failure. Breakage of the nail at the lag-screw level can be
determined by errors in the guiding instruments. These high
tolerances can cause dents or scratches in the protective titanium
coating. This can lead to early implant breakage due to stress
forces in a high-cycles environment. Extra care should be promoted
to fracture reduction and adequate use of the gamma instruments
tray. It is obvious that the forces exerted at this level do not
meet the critical level of implant breaking point, but after a high
number of cycles with a lower stress level, the lifetime and
resistance of titanium alloy components are greatly reduced. This
theory was also observed in other modular systems, used in the
orthopedic field.
The gamma nail system remains one of the best
solutions in the surgical treatment of pertrochanteric fractures,
even though it may sometimes be associated with postoperative
complications (36).
Acknowledgements
Professional editing, linguistic and technical
assistance performed by Irina Radu, Individual Service Provider,
certified translator in Medicine and Pharmacy (certificate
credentials: Series E no. 0048).
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
SD planned the clinical study, performed the
surgical procedures, contributed to the conception and design of
the study, and the acquisition, analysis and interpretation of the
data. CDMD contributed to the conception and design of the study,
analysis of data, the drafting of the manuscript and its critical
revision for important intellectual content. DCC contributed to the
analysis and interpretation of the data and the critical revision
for important intellectual content. CID and HTS contributed to the
conception and design of the study and the critical revision of the
manuscript for important intellectual content. CIS contributed to
the conception and design of the study, the interpretation of the
data and the critical revision of the manuscript for important
intellectual content. All authors read and approved the final
version of the manuscript and agreed to be accountable for all
aspects of the study.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
‘Foişor’ Orthopedics-Traumatology and Osteoarticular TB Hospital
(Bucharest, Romania). All patients provided a signed informed
consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
White SM and Griffiths R: Projected
incidence of proximal femoral fracture in England: A report from
the NHS hip fracture anaesthesia network (HIPFAN). Injury.
42:1230–1233. 2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Gillespie WJ, Gillespie LD and Parker MJ:
Hip protectors for preventing hip fracures in older people.
Cochrane Database Syst Rev. 6(CD001255)2010.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Cameron ID, Kurrle SE, Quine S, Sambrook
PN, March L, Chan DK, Locwood K, Cook B and Schaafsma FF: Improving
adherence with the use of hip protectors among older people living
in nursing care facilities: A cluster randomized trial. J Am Med
Dir Assoc. 12:50–57. 2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Bjorgul K, Novicoff WM and Saleh KJ:
Learning curves in hip fracture surgery. Int Orthop. 35:113–119.
2011.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Biber R, Gruninger S, Singler K, Sieber CC
and Bail HJ: Is proximal femoral nailing a good procedure for
teaching in orthogeriatrics? Arch Orthop Trauma Surg. 132:997–1002.
2012.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Loizou CL, McNamara I, Ahmed K, Pryor GA
and Parker MJ: Classification of subtrochanteric femoral fractures.
Injury. 41:739–745. 2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ramadier J, Duparc J, Rougemont D and De
Ferrari G: Surgical treatment of trochanteric and
juxta-trochanteric fractures. Rev Chir Orthop Reparatrice Appar
Mot. 42:759–786. 1956.(In French). PubMed/NCBI
|
|
8
|
Decoulx P and Lavarde G: Fractures of the
trochanteric region. A statistical study of 2,612 cases. J Chir
(Paris). 98:75–100. 1969.(In French). PubMed/NCBI
|
|
9
|
Evans EM: The treatment of trochanteric
fractures of the femur. J Bone Joint Surg Br. 31B:190–203.
1949.PubMed/NCBI
|
|
10
|
Grigorie D, Sucaliuc A, Ciutan M and
Vladescu C: Incidence and time trend of hip fractures in Romania: A
nationwide study from 2008 to 2018. Acta Endocrinol (Buchar).
15:505–512. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mizrahi E, Fleissig Y, Arad M, Blumstein T
and Adunsky A: Rehabilitation outcome of hip fracture patients: The
importance of a positive albumin gain. Arch Gerontol Geriatr.
47:318–326. 2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kuzyk PR, Zdero R, Shah S, Olsen M,
Waddell JP and Schemitsch EH: Femoral head lag screw position for
cephalomedullary nails: A biomechanical analysis. J Orthop Trauma.
26:414–421. 2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Niinomi MJ: Mechanical biocompatibilities
of titanium alloys for biomedical applications. J Mech Behav Biomed
Mater. 1:30–42. 2008.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Elias CN, Lima JHC, Valiev R and Meyers
MA: Biomedical applications of titanium and its alloys. JOM.
60:46–49. 2008.
|
|
15
|
Black J: Biologic performance of tantalum.
Clin Mater. 16:167–173. 1994.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Zuo JH, Wang ZG and Han EH: Effect of
microstructure on ultra-high cycle fatigue behaviour of Ti-6Al-4V.
Mater Sci Eng A. 473:147–152. 2008.
|
|
17
|
Wagner L and Lutjering G: Microstructural
influences on propagation of short cracks in an (α+β) Ti-alloy. Z
Metallkde. 87:369–375. 1987.(In German).
|
|
18
|
Willeumier JJ, Kaynak M, van der Zwaal P,
Meylaerts SAG, Mathijssen NMC, Jutte PC, Tsagozis P, Wedin R, van
de Sande MAJ, Fiocco M and Dijkstra PDS: What factors are
associated with implant breakage and revision after intramedullary
nailing for femoral metastases? Clin Orthop Relat Res.
476:1823–1833. 2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Iwakura T, Niikura T, Lee SY, Sakai Y,
Nishida K, Kuroda R and Kurosaka M: Breakage of a third generation
gamma nail: A case report and review of the literature. Case Rep
Orthop. 2013(172352)2013.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Johnson NA, Uzoigwe C, Venkatesan M,
Burgula V, Kulkarni A, Davison JN and Ashford RU: Risk factors for
intramedullary nail breakage in proximal femoral fractures: A
10-year retrospective review. Ann R Coll Surg Engl. 99:145–150.
2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wright NC, Looker AC, Saag KG, Curtis JR,
Delzell ES, Randall S and Dawson-Hughes B: The recent prevalence of
osteoporosis and low bone mass in the United States based on bone
mineral density at the femoral neck or lumbar spine. J Bone Miner
Res. 29:2520–2526. 2014.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Sharma V and Babhulkar S and Babhulkar S:
Role of gamma nail in management of pertrochanteric fractures of
femur. Indian J Orthop. 42:212–216. 2008.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Halder SC: The gamma nail for
peritrochanteric fractures. J Bone Joint Surg Br. 74:340–344.
1992.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kempf I, Grosse A, Taglang G and Favreul
E: Gamma nail in the treatment of closed trochanteric fractures,
results and indications apropos of 121 cases. Rev Chir Orthop
Reparatrice Appar Mot. 79:29–40. 1993.(In French). PubMed/NCBI
|
|
25
|
Busch CA, Charles MN, Haydon CM, Bourne
RB, Rorabeck CH, Macdonald SJ and McCalden RW: Fractures of
distally-fixed femoral stems after revision arthroplasty. J Bone
Joint Surg Br. 87:1333–1336. 2005.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Dangles CJ and Altstetter CJ: Failure of
the modular neck in a total hip arthroplasty. J Arthroplasty.
25:1169.e5–e7. 2010.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Lakstein D, Eliaz N, Levi O, Backstein D,
Kosashvili Y, Safir O and Gross AE: Fracture of cementless femoral
stems at the mid-stem junction in modular revision hip arthroplasty
systems. J Bone Joint Surg Am. 93:57–65. 2011.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Magnissalis EA, Zinelis S, Karachalios T
and Hartofilakidis G: Failure analysis of two Ti-alloy total hip
arthroplasty femoral stems fractured in vivo. J Biomed Mater Res B
Appl Biomater. 66:299–305. 2003.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Patel A, Bliss J, Calfee RP, Froehlich J
and Limbird R: Modular femoral stem-sleeve junction failure after
primary total hip arthroplasty. J Arthroplasty. 24:1143.e3–e5.
2009.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Sotereanos NG, Sauber TJ and Tupis TT:
Modular femoral neck fracture after primary total hip arthroplasty.
J Arthroplasty. 28:196.e7–e9. 2013.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Sul YT, Johansson CB, Petronis S, Krozer
A, Jeong Y, Wennerberg A and Albrektsson T: Characteristics of the
surface oxides on turned and electrochemically oxidized pure
titanium implants up to dielectric breakdown: The oxide thickness,
micropore configurations, surface roughness, crystal structure and
chemical composition. Biomaterials. 23:491–501. 2002.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Ritchie RO, Davidson DL, Boyce BL,
Campbell JP and Roder O: High-cycle fatigue of Ti-6Al-4V. Fatigue
Fract Engng Mater Struct. 22:621–631. 1999.
|
|
33
|
Gilbert JL, Buckley CA and Jacobs JJ: In
vivo corrosion of modular hip prosthesis components in mixed and
similar metal combinations. The effect of crevice, stress, motion,
and alloy coupling. J Biomed Mater Res. 27:1533–1544.
1993.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Abram SG, Pollard TC and Andrade AJ:
Inadequate ‘three-point’ proximal fixation predicts failure of the
gamma nail. Bone Joint J. 95-B:825–830. 2013.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Eberle S, Bauer C, Gerber C, von Oldenburg
G and Augat P: The stability of a hip fracture determines the
fatigue of an intramedullary nail. Proc Inst Mech Eng H.
224:577–584. 2010.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Liu M, Yang Z, Pei F, Huang F, Chen S and
Xiang Z: A meta-analysis of the gamma nail and dynamic hip screw in
treating peritrochanteric fractures. Int Orthop. 34:323–328.
2010.PubMed/NCBI View Article : Google Scholar
|