Introduction
Despite the improved living standards nowadays,
ischemic cerebrovascular disease (ICD), a disease prevalent in the
elderly, is quite common in this increasingly aging society.
Featuring high mortality, recurrence and high disability rate, ICD
poses a serious threat to people's lives (1-3).
ICD can cause temporary blood supply disorder, which leads to
neurological deficits and has a serious impact on patients
(4). ICD onset is often accompanied
by neurological dysfunction (5).
Timely treatment is unavailable due to the sudden onset of ICD,
making the life of patients severely impacted (6).
The prominent clinical treatment for ICD is
intravenous thrombolysis, which can promote the recanalization of
the blocked blood vessels and save the life of patients, because of
the plasminogen activator in the thrombolytic drug which dissolves
the fibrin in the thrombus (7-9).
However, the deficiency is that intravenous thrombolysis only works
within the first 4 h after the onset of the disease and has certain
contraindications for patients (10). Therefore, only a limited number of
patients are suitable for intravenous thrombolysis. Due to the
increasing incidence of ICD, new research and discoveries have been
made. In recent years, neurointervention has been applied in the
treatment of ICD (11).
Neurointervention is a minimally invasive therapy that is based on
a computer to determine the location of arterial stenosis and treat
cerebrovascular disease through intubation. The use of intravenous
thrombolysis in the course of interventional therapy can directly
unblock blood vessels and eliminate infarction (12,13).
Neurointervention compensates for the limitations of intravenous
thrombolysis regarding treatment time and eligibility of patients.
Therefore, the aim of the present study was to combine the two
therapies in order to investigate whether intravenous thrombolysis
combined with neurointervention could improve the ICD
treatment.
The present study explored the efficacy of
neurointervention combined with intravenous thrombolysis in the
treatment of ICD and its influence on neurological function and
prognosis of patients, aiming to provide future reference for the
treatment of ICD.
Patients and methods
General information
A total of 119 patients with ICD admitted to
Xinxiang Central Hospital (Xinxiang, China) from May 2013 to
September 2015 were selected. Among them, 65 patients were enrolled
in the control group and treated with intravenous thrombolysis,
whereas the other 54 patients were enrolled in the observation
group and were treated with intravenous thrombolysis combined with
neurointervention. The control group included 37 males and 28
females, with an average age of 41.3±5.2 years. In the control
group, 18 patients had total anterior circulation infarction, 16
partial anterior circulation infarction, 19 posterior circulation
infarction and 12 lacunar infarction. The observation group
included 28 males and 26 females, with an average age of 42.3±4.7
years. In the observation group, 15 patients had total anterior
circulation infarction, 11 partial anterior circulation infarction,
17 posterior circulation infarction and 11 lacunar infarction. The
study was approved by the Ethics Committee of Xinxiang Central
Hospital. Patients who participated in the study had complete
clinical data and signed written informed consents were obtained
from the patients and/or guardians.
Inclusion and exclusion criteria
The inclusion criteria were the following: patients
with ICD for the first time; patients with treatment indications
for neurointervention; patients admitted to the hospital within 6 h
after the ICD onset; patients diagnosed with ICD by head CT
angiography; and patients with complete clinical data.
The exclusion criteria were the following: patients
with severe inflammation; patients with severe mental disorder;
patients with intracranial hemorrhage; patients with hereditary
diseases; patients with malignant tumors; and patients with other
serious cardiovascular or cerebrovascular diseases.
Treatment methods
Patients in the control group were treated with
intravenous thrombolysis. After admission, patients were treated
with tissue-type plasminogen activator for injection (China FDA
approval no. S20150001; Guangzhou Recomgen Biotech Co., Ltd.). An
intravenous drop of 300,000-500,000 U of urokinase and 20 ml of
saline was firstly administered, followed by an intravenous
injection of 1,000,000 U of urokinase and 100 ml of saline.
In the observation group, patients received
neurointervention treatment right after the intravenous
thrombolysis. Electrocardiography, blood routine tests, liver and
kidney function tests, as well as coagulation function tests were
performed before treatment. Aspirin (China FDA approval no.
H41021076; Henan Fusen Pharmaceutical Co., Ltd.) was orally
administrated at a dose of 50-150 mg/day and clopidogrel [China FDA
approval no. 20180029; Sinofi (Hangzhou) Pharmaceutical Co., Ltd.]
was orally administrated at a dose of 75 mg/day to prevent platelet
aggregation. With the support of the digital subtraction
angiography system, an injection of a small amount of anesthetic
into the inguinal region was administered before puncturing the
femoral artery to place the vascular sheath. A 5F arterial sheath
was inserted. A contrast tube was inserted to the aortic arch under
the guidance of the ultra-sliding guidewire. The blood vessel
direction and position was confirmed by angiography. A total of
200,000 U of urokinase (national medicine standard H22023486) was
added into 20 ml of 0.9% sodium chloride solution for injection.
Next, the solution was pumped in at a rate of 1 ml/min through a
micropump autolysis catheter under the guidance of the micro
guidewire. A stent was placed at the site of arterial stenosis to
determine the unclogging of blocked blood vessels. Antiplatelet
therapy was performed 24 h after surgery.
Outcome measures
Main outcome measures: The National Institutes of
Health Stroke Scale (NIHSS) (14)
scores of the two groups of patients at 1, 3 and 6 months after
treatment were recorded. Kaplan-Meier survival curves were drawn to
assess the patients' survival 1 year after treatment.
Secondary outcome measures: The efficacy of
treatment (Table I) was evaluated
in the two groups. Total effective rate=(cases of marked response +
cases of moderate response)/total no. of cases x100%. In addition,
the vascular recanalization rates (Table II) of the two groups were
calculated. Vascular recanalization rate=(cases of complete
recanalization + cases of partial recanalization)/total no. of
cases x100%.
 | Table IEfficacy evaluation criteria. |
Table I
Efficacy evaluation criteria.
| Items | Criteria |
|---|
| Marked response | ≥45% decrease in
NIHSS score |
| Moderate
response | <45% and ≥18%
decrease in NIHSS score |
| No response | <18% decrease in
NIHSS score |
 | Table IICriteria for vascular
recanalization. |
Table II
Criteria for vascular
recanalization.
| Items | Criteria |
|---|
| Complete
recanalization | The main branches of
the skull are completely recanalized and can be clearly
developed |
| Partial
recanalization | The main branches of
the skull are not clearly developed and the blood vessels in the
posterior part of the embolization are partially recanalized |
| Blocked | The blood vessels at
the back end of the embolization site are blocked and cannot be
developed |
Statistical analysis
Statistical analysis was performed using SPSS 19.0
software (IBM Corp.) and the data were plotted using GraphPad Prism
7 software (GraphPad Software, Inc.). Count data were expressed as
rate (%) and were compared by Chi-square test. Measurement data
were expressed as the mean ± standard deviation (mean ± SD) and
were compared between two groups by the independent samples t-test.
The measurement data were normally distributed. Repeated measures
ANOVA, followed by Bonferroni post hoc test, was used for the
comparison of the data at multiple time points. The 1-year survival
of patients was assessed by Kaplan-Meier survival analysis and
log-rank test was used for the comparison of the survival curves.
P<0.05 was considered to indicate a statistically significant
difference.
Results
General clinical data of patients in
the control and observation groups
As shown in Table
III, no significant difference was observed between the control
and the observation group in terms of age, sex, disease type,
low-density lipoprotein levels, hematological disease, fibrinogen,
triglyceride and total cholesterol levels and alcohol abuse
(P>0.05).
 | Table IIIGeneral clinical data of patients in
the control and observation groups [n (%), mean ± SD]. |
Table III
General clinical data of patients in
the control and observation groups [n (%), mean ± SD].
| Factors | Observation group
(n=54) | Control group
(n=65) | t/χ2 | P-value |
|---|
| Sex | | | 0.306 | 0.580 |
|
Male | 28 (51.85) | 37 (56.92) | | |
|
Female | 26 (48.15) | 28 (43.08) | | |
| Age (years) | 42.3±4.7 | 41.3±5.2 | 1.026 | 0.307 |
| Disease type | | | 0.681 | 0.496 |
|
Total
anterior circulation infarction | 15 (27.78) | 18 (27.69) | | |
|
Partial
anterior circulation infarction | 11 (20.37) | 16 (24.62) | | |
|
Posterior
circulation infarction | 17 (31.48) | 19 (29.23) | | |
|
Lacunar
infarction | 11 (20.37) | 12 (18.46) | | |
| Low-density
lipoprotein (µmol/l) | 2.89±0.87 | 2.81±0.79 | 1.149 | 0.251 |
| Hematological
disease | | | 0.563 | 0.453 |
|
Yes | 18 (33.33) | 26 (40.00) | | |
|
No | 36 (66.67) | 39 (60.00) | | |
| Fibrinogen (g/l) | 6.43±1.25 | 6.26±1.43 | 0.683 | 0.496 |
| Triglyceride
(mmol/l) | 1.35±0.23 | 1.34±0.34 | 0.184 | 0.854 |
| Total cholesterol
(µmol/l) | 4.49±1.04 | 4.48±1.09 | 0.051 | 0.960 |
| Alcohol abuse | | | 0.351 | 0.553 |
|
Yes | 22 (40.74) | 30 (46.15) | | |
|
No | 32 (59.26) | 35 (53.85) | | |
Comparison of neurological deficits
and vascular recanalization between the two groups
NHISS scores before treatment were not statistically
different between the two groups (P>0.05; Table IV). At 1, 3 and 6 months after
treatment, the NHISS scores were lower in the observation group
than those in the control group (P<0.001). In the control group,
the NIHSS scores at 1, 3 and 6 months after treatment were
significantly lower than those before treatment (P<0.05); the
NIHSS score at 1 month after treatment was not significantly
different from that at 3 months after treatment; however, it was
statistically different from that at 6 months after treatment
(P<0.05); the NIHSS score 3 months after treatment was not
different from that at 6 months after treatment. In the observation
group, NIHSS scores at 1, 3 and 6 months after the treatment were
significantly lower those before treatment and those in the control
group after treatment (P<0.05); the NIHSS score at 1 month after
treatment was statistically different from that at 3 and 6 months
after treatment (both P<0.05). As presented in Table V, in the control group, there were
21 cases with complete recanalization, 22 cases with partial
recanalization and 22 cases with no recanalization. In the
observation group, there were 27 cases with complete
recanalization, 23 cases with partial recanalization and 4 cases
with no recanalization. Total vascular recanalization was
significantly better in the observation group than that in the
control group (P<0.001).
 | Table IVComparison of neurological deficits
(NIHSS scores) between the two groups before and after treatment
(mean ± SD). |
Table IV
Comparison of neurological deficits
(NIHSS scores) between the two groups before and after treatment
(mean ± SD).
| Group | Before treatment | 1 month after
treatment | 3 months after
treatment | 6 months after
treatment | F | P-value |
|---|
| Control group
(n=65) | 12.76±2.85 |
10.02±2.91a |
9.24±2.32a |
8.32±2.16a,b | 36.259 | <0.001 |
| Observation group
(n=54) | 12.83±2.57 |
5.23±1.34a |
3.16±1.54a,b |
2.53±0.96a-c | 22.367 | <0.001 |
| t | 0.135 | 11.150 | 16.470 | 18.250 | | |
| P-value | 0.892 | <0.001 | <0.001 | <0.001 | | |
 | Table VVascular recanalization after
treatment in the control and observation groups [n (%)]. |
Table V
Vascular recanalization after
treatment in the control and observation groups [n (%)].
| Items | Control group
(n=65) | Observation group
(n=54) | χ2 | P-value |
|---|
| Complete
recanalization | 21 (32.31) | 27 (50.00) | 3.836 | 0.050 |
| Partial
recanalization | 22 (33.85) | 23 (42.59) | 0.960 | 0.327 |
| Blocked | 22 (33.85) | 4 (7.41) | 12.07 | <0.001 |
| Total vascular
recanalization | 43 (66.15) | 50 (92.59) | 12.07 | <0.001 |
One-year survival rate of the patients
in the two groups after treatment
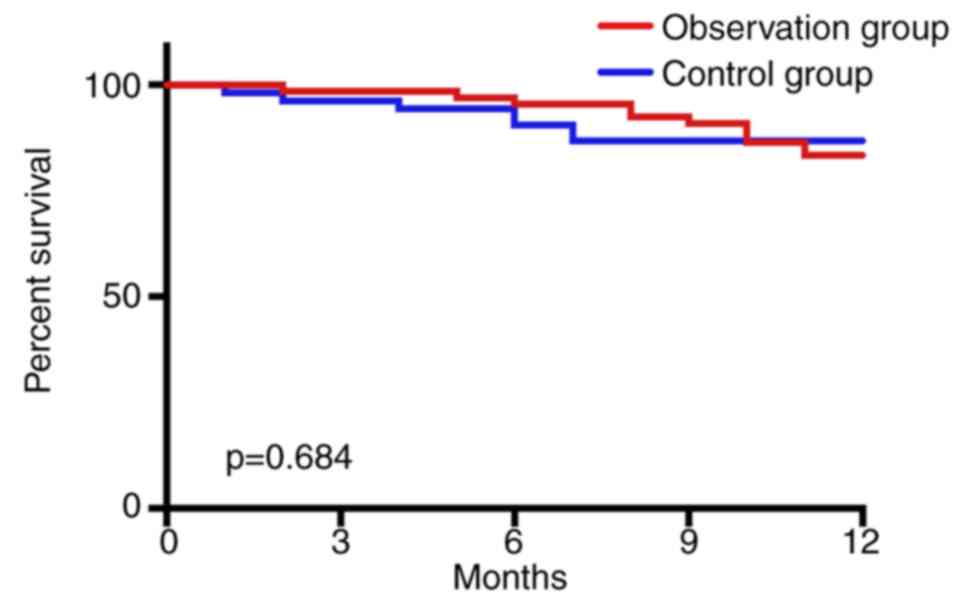
As shown in Fig. 1,
all 119 patients were successfully followed up after treatment to
assess 1-year survival. In the control group, 55 patients survived
and 10 patients died within 1 year after treatment, with a survival
rate of 84.62%. In the observation group, 46 patients survived and
8 patients died within 1 year after treatment, with a survival rate
of 85.19%. According to the Kaplan-Meier survival curve analysis,
the 1-year survival rate after treatment was not statistically
different between the two groups (P=0.684).
Total effective rate after treatment
in the control and observation groups
The rate of marked response was 46.30% in the
observation group and 35.38% in the control group (Table VI). The rate of moderate response
was 42.59% in the observation group and 32.31% in the control
group. The rate of no response was 11.11% in the observation group
and 32.31% in the control group. The observation group had a total
effective rate of 88.89%, significantly higher than the total
effective rate 67.69% in the control group (χ2=9.429,
P=0.002).
 | Table VITotal effective rate after treatment
in the control and observation groups [n (%)]. |
Table VI
Total effective rate after treatment
in the control and observation groups [n (%)].
| Items | Control group
(n=65) | Observation group
(n=54) | χ2 | P-value |
|---|
| Marked
response | 23 (35.38) | 25 (46.30) | 1.459 | 0.227 |
| Moderate
response | 21 (32.31) | 23 (42.59) | 1.339 | 0.247 |
| No response | 21 (32.31) | 6 (11.11) | 9.429 | 0.002 |
| Total effective
rate | 44 (67.69) | 48 (88.89) | 9.429 | 0.002 |
Comparison of complications after
treatment between the control and observation groups
As presented in Table
VII, in the observation group, 2 patients had intracranial
hemorrhage after treatment, 7 airway obstruction, 6
revascularization and 4 arrhythmia. In the control group, 10
patients had intracranial hemorrhage after treatment, 19 airway
obstruction, 18 revascularization and 16 arrhythmia. The
complication rate in the observation group was statistically lower
than that of the control group (P<0.05).
 | Table VIIComparison of complications after
treatment between the control and the observation group [n
(%)]. |
Table VII
Comparison of complications after
treatment between the control and the observation group [n
(%)].
| Complications | Control group
(n=65) | Observation group
(n=54) | χ2 | P-value |
|---|
| Intracranial
hemorrhage | 10 (15.38) | 2 (3.70) | 4.439 | 0.035 |
| Airway
obstruction | 19 (29.23) | 7 (12.96) | 4.571 | 0.033 |
|
Revascularization | 18 (27.69) | 6 (11.11) | 5.037 | 0.025 |
| Arrhythmia | 16 (24.62) | 4 (7.41) | 6.247 | 0.012 |
Comparison of total hospitalization
time between the two groups
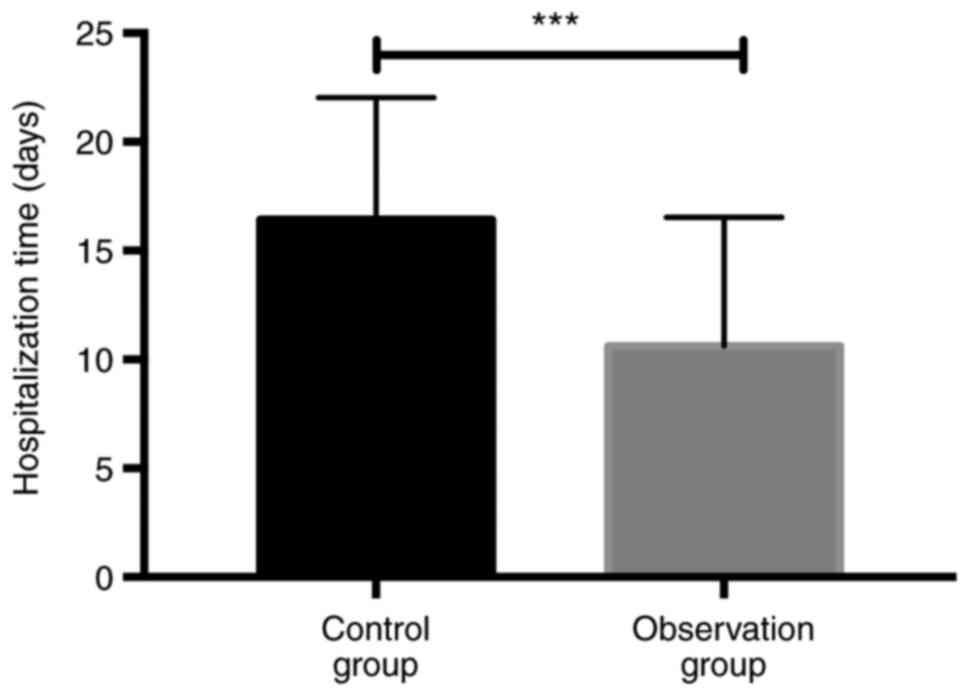
As shown in Fig. 2,
the total hospitalization time in the control group was 16.42±5.62
days, statistically longer than that in the observation group which
was 10.62±5.90 days (t=5.480, P<0.001).
Discussion
ICD is a disease in which cerebrovascular wall
lesions affect the supply of cerebral blood vessels, damaging the
brain tissue of patients to varying degrees, and seriously
affecting the patients' survival and quality of life (6). The impact of ICD on the nerve function
and physical function of patients aggravate the economic burden of
the patients and their families. Therefore, the search for an
effective and safe treatment for ICD is of great significance
(15). Currently, intravenous
thrombolysis is the dominant therapy for treating ICD (16-18).
However, only a limited number of patients are clinically suitable
for intravenous thrombolysis therapy. As studies on cerebrovascular
diseases go deeper, the minimally invasive neurointervention
therapy begins to play a role in the treatment of cerebrovascular
diseases (19-21).
Neurointervention, a safe and highly efficient treatment, with
fewer complications and less damage to the body functions, has
started to be implemented in clinical practice (22).
The present study used the NIHSS score to assess the
neurological function of patients. The NIHSS scores of the two
groups after treatment were lower than those before treatment, and
the NIHSS scores of patients treated with intravenous thrombolysis
combined with neurointervention were significantly lower than those
treated with intravenous thrombolysis only. The clinical treatment
efficacy between the two groups was also compared. The total
effective rate, complications, survival, and vascular
recanalization for patients treated with intravenous thrombolysis
combined with neurointervention were better than those treated with
intravenous thrombolysis alone. A previous study (11) reported that neurointervention
therapy brought a low incidence of complications and a high
recanalization rate. The present study made further progress by
combining intravenous thrombolysis with neurointervention, showing
that intravenous thrombolysis combined with neurointervention can
significantly reduce complications and improve the
revascularization of patients with ICD, with better efficacy. The
speculation is that the high selectivity of neurointervention
compensates for the unspecified targets of intravenous
thrombolysis. Moreover, intravenous thrombolysis can improve the
problem of thrombus shedding resulted from microcirculation
disturbance aroused by neurointervention. Therefore, the
combination of neurointervention and intravenous thrombolysis has
better efficacy, with less bleeding and side effects. Hao et
al (23) explored the clinical
effects of interventional therapy in ICD and showed that the
combination therapy brought better treatment outcomes than the
single use of drugs. Such a result is similar to our findings of
the combination of neurointervention and intravenous thrombolysis
in treating ICD. In the present study, the total hospitalization
time after treatment in the observation group was significantly
shorter than that in the control group. As reported by Coutinho
et al (24), intravenous
thrombolysis combined with thrombectomy was more effective than
intravenous thrombolysis alone, which was similar to the result of
the present study, i.e., that the efficacy of the combination
therapy was better than that of the intravenous thrombolysis alone.
In the present study, the results revealed that the combination
therapy was more efficient leading to reduced hospitalization time.
The combination of intravenous thrombolysis and mechanical
thrombectomy used in Coutinho's et al study is defective
because of the difficulty of the mechanical thrombectomy to be
performed in the tortuous blood vessels. The neurointervention
therapy can directly clear the blood vessels through arterial and
venous intubation, resulting in high recanalization rates, better
safety and treatment efficacy. According to the assessment of the
patients' 1-year survival, the survival rate of the observation
group was 85.19%, whereas that of the control group was 84.62%. No
statistical difference was observed in the survival rate between
the two groups. Although the effect of intravenous thrombolysis
combined with neurointervention is better than that of intravenous
thrombolysis alone, this combination can only recanalize the
established thrombus. Numerous patients with ICD have high levels
of blood lipids, which makes platelets easy to agglutinate into new
thromboses leading to the recurrence of the disease. Unavailability
of timely treatment in case of disease recurrence may lead to
patient death. Therefore, these two treatment methods have no
effect on the patient's survival.
The present study has some limitations. First, the
time for the observation of the efficacy and adverse reactions was
too short to get a clear understanding of the prognosis of
patients, which should be improved in future studies. Second, other
treatment methods were not explored for ICD, which are also needed
to be discussed in subsequent studies. Finally, healthy individuals
were not included in the study, making it unclear whether patients
after treatment present differences from healthy subjects in some
aspects. In future studies, healthy subjects will be enrolled, the
follow-up time will be prolonged, and other treatment options will
be investigated to supplement the deficiencies of the present
study.
In conclusion, neurointervention combined with
intravenous thrombolysis for treating ICD can reduce NHISS score.
In addition, this combination can improve the recanalization rate,
reduce complications and shorten the hospitalization time,
achieving a higher effective rate.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SL wrote the manuscript. SL and XL interpreted and
analyzed the patient data. ZC and CS designed the study and
performed the experiment. HL and JH were responsible for the
analysis and discussion of the data. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Xinxiang Central Hospital (Xinxiang, China). Patients
who participated in the study had complete clinical data. Signed
written informed consents were obtained from the patients and/or
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Powers WJ: Cerebral hemodynamics in
ischemic cerebrovascular disease. Ann Neurol. 29:231–240.
1991.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Singh N, Moody AR, Gladstone DJ, Leung G,
Ravikumar R, Zhan J and Maggisano R: Moderate carotid artery
stenosis: MR imaging-depicted intraplaque hemorrhage predicts risk
of cerebrovascular ischemic events in asymptomatic men. Radiology.
252:502–508. 2009.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chen PP, Lou PA, Zhang P, Qiao C, Li T and
Dong ZM: Trend analysis on the death rate of ischemic heart disease
and cerebrovascular disease among Xuzhou residents from 2011 to
2015. Zhonghua Xin Xue Guan Bing Za Zhi. 45:597–607.
2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
4
|
Li X, Zhang ZW, Wang Z, Li JQ and Chen G:
The role of argon in stroke. Med Gas Res. 8:64–66. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sviridova NK and Yavorsky VV: The
effectiveness of diagnosis and treatment of cerebrovascular
disorders in hypertensive encephalopathy in elderly patients by
studying the characteristics of cerebral hemodynamics and cerebral
perfusion status. Lik Sprava. 41–46. 2015.PubMed/NCBI(In Ukrainian).
|
|
6
|
Liu J, Liu Y, Wang L, Yin P, Liu S, You J,
Zeng X and Zhou M: The disease burden of cardiovascular and
circulatory diseases in China, 1990 and 2010. Zhonghua Yu Fang Yi
Xue Za Zhi. 49:315–320. 2015.PubMed/NCBI(In Chinese).
|
|
7
|
Zivanovic Z, Gubi M, Vlahovic D, Milicevic
M, Jovicevic M, Lucic A, Ruzicka-Kaloci S, Radovanovic B, Zikic TR,
Zarkov M, et al: Patients with acute lacunar infarction have
benefit from intravenous thrombolysis. J Stroke Cerebrovasc Dis.
28:435–440. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Wu C, Wu D, Chen J, Li C and Ji X: Why not
intravenous thrombolysis in patients with recurrent stroke within 3
months? Aging Dis. 9:309–316. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Fan Y, Liao X, Pan Y, Dong K and Wang Y
and Wang Y: Thrombolysis Implementation and Monitor of Acute
Ischemic Stroke in China (TIMS-China) Investigators: Intravenous
thrombolysis is safe and effective for the cryptogenic stroke in
China: Data from the thrombolysis implementation and monitor of
acute ischemic stroke in China (TIMS-China). J Stroke Cerebrovasc
Dis. 28:220–226. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wang MD, Yin XX, Yang TT, Wang Y, Zhu YY,
Zhou YF, Lu ZX and Hu B: Chinese neurologists' perspective on
intravenous thrombolysis for acute ischemic stroke. Brain Behav.
8(e00882)2017.PubMed/NCBI View
Article : Google Scholar
|
|
11
|
Mehta B, Leslie-Mazwi TM, Chandra RV,
Chaudhry ZA, Rabinov JD, Hirsch JA, Schwamm LH, Rost NS and Yoo AJ:
Assessing variability in neurointerventional practice patterns for
acute ischemic stroke. J Neurointerv Surg. 5 (Suppl 1):i52–i57.
2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sacks D, Baxter B, Campbell BCV, Carpenter
JS, Cognard C, Dippel D, Eesa M, Fischer U, Hausegger K, Hirsch
, et al: Multisociety consensus quality improvement revised
consensus statement for endovascular therapy of acute ischemic
stroke: From the American Association of Neurological Surgeons
(AANS), American Society of Neuroradiology (ASNR), Cardiovascular
and Interventional Radiology Society of Europe (CIRSE), Canadian
Interventional Radiology Association (CIRA), Congress of
Neurological Surgeons (CNS), European Society of Minimally Invasive
Neurological Therapy (ESMINT), European Society of Neuroradiology
(ESNR), European Stroke Organization (ESO), Society for
Cardiovascular Angiography and Interventions (SCAI), Society of
Interventional Radiology (SIR), Society of NeuroInterventional
Surgery (SNIS), and World Stroke Organization (WSO). Int J Stroke.
13:612–632. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Blackham KA, Meyers PM, Abruzzo TA,
Albuquerque FC, Fiorella D, Fraser J, Frei D, Gandhi CD, Heck DV,
Hirsch JA, et al: Endovascular therapy of acute ischemic stroke:
Report of the standards of practice committee of the society of
neurointerventional surgery. J Neurointerv Surg. 4:87–93.
2012.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Fischer U, Arnold M, Nedeltchev K,
Brekenfeld C, Ballinari P, Remonda L, Schroth G and Mattle HP:
NIHSS score and arteriographic findings in acute ischemic stroke.
Stroke. 36:2121–2125. 2005.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bondonno CP, Blekkenhorst LC, Prince RL,
Ivey KL, Lewis JR, Devine A, Woodman RJ, Lundberg JO, Croft KD,
Thompson PL and Hodgson JM: Association of vegetable nitrate intake
with carotid atherosclerosis and ischemic cerebrovascular disease
in older women. Stroke. 48:1724–1729. 2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ishida J, Konishi M, Ebner N and Springer
J: Repurposing of approved cardiovascular drugs. J Transl Med.
14(269)2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Cheng NT and Kim AS: Intravenous
thrombolysis for acute ischemic stroke within 3 h versus between 3
and 4.5 h of symptom onset. Neurohospitalist. 5:101–109.
2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Escudero D, Molina R, Viña L, Rodriguez P,
Marqués L, Fernandez E, Forcelledo L, Otero J, Taboada F, Vega P,
et al: Endovascular treatment and intra-arterial thrombolysis in
acute ischemic stroke. Med Intensiva. 34:370–378. 2010.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
19
|
Rahman WT, Griauzde J, Chaudhary N, Pandey
AS, Gemmete JJ and Chong ST: Neurovascular emergencies: Imaging
diagnosis and neurointerventional treatment. Emerg Radiol.
24:183–193. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Yang Y, Liang C, Shen C, Tang H, Ma S,
Zhang Q, Gao M, Dong Q and Xu R: The effects of pharmaceutical
thrombolysis and multi-modal therapy on patients with acute
posterior circulation ischemic stroke: Results of a one center
retrospective study. Int J Surg. 39:197–201. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Radnai P, Szőts M, Rádai F, Horváth G,
Varga C, Fogas J, Szörényi P, Horváth Z, Bajzik G, Moizs M, et al:
Neurointerventional treatment of acute ischemic stroke: Our
experience in kaposvar, Hungary. Ideggyogy Sz. 68:252–257.
2015.PubMed/NCBI(In Hungarian).
|
|
22
|
Loftus CM, Hoffmann M, Heetderks W, Zheng
X and Pena C: Regulation of neurological devices and
neurointerventional endovascular approaches for acute ischemic
stroke. Front Neurol. 9(320)2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Hao Y, Qi Z, Ding Y, Yu X, Pang L and Zhao
T: Effect of interventional therapy on IL-1β, IL-6, and
neutrophil-lymphocyte ratio (NLR) levels and outcomes in patients
with ischemic cerebrovascular disease. Med Sci Monit. 25:610–617.
2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Coutinho JM, Liebeskind DS, Slater LA,
Nogueira RG, Clark W, Dávalos A, Bonafé A, Jahan R, Fischer U,
Gralla J, et al: Combined intravenous thrombolysis and thrombectomy
vs thrombectomy alone for acute ischemic stroke: A pooled analysis
of the SWIFT and STAR studies. JAMA Neurol. 74:268–274.
2017.PubMed/NCBI View Article : Google Scholar
|