Introduction
Segmental breast surgery is one of the common
methods in treating breast diseases. Clinically, general anesthesia
is the main anesthesia method for breast segmental surgery, which
can relieve pain, fear, anxiety and other negative emotions of
patients. It is an important part of clinical study to ensure the
anesthetic effect while shortening the postoperative recovery time
and reducing anesthesia-related complications. Intravenous
anesthesia has advantages such as rapid onset, strong efficacy,
reversible anesthetic effect, and full variety of drugs. Compared
with inhalation anesthesia, it does not burn, explode or pollute
the operating room environment. Intravenous anesthesia has
gradually become the mainstream technique of clinical anesthesia
(1).
The effect of general anesthesia drugs on oxidative
stress (OS) and hemodynamics of patients during anesthesia is
currently a hot issue. Therefore, it is of great significance to
compare the perioperative OS response of patients from the
perspective of general anesthesia drugs for the selection of
clinical anesthesia drugs. Intravenous anesthesia effectively
maintains the stability of patients' hemodynamics, reduce the
anesthetic dosage, inhibits the occurrence of OS with higher
efficacy, and helps patients wake up quickly and safely from
anesthesia (2). OS reaction refers
to the oxidative damage process in vivo or in cells, which
is caused by the imbalance between the generation and elimination
of oxygen radicals in vivo or in cells, resulting in
accumulation of reactive oxygen species (ROS) and reactive nitrogen
species (RNS) (3). Recent studies
have shown that DNA damage and genetic mutation are all related to
OS. It can also promote and lead to the occurrence of tumors
(4-7).
Moreover, OS reaction is also regarded as an important factor
leading to aging and diseases, because of a series of negative
effects produced by free radicals in vivo or in cells
(8). Because of the strong
oxidizing ability, ROS could easily form negative ions by combining
with one electron. According to different sources, ROS can be
roughly divided into exogenous and endogenous ROS (9). Excessive ROS in the body would
accelerate the aging of the body, while endogenous antioxidant
enzymes [superoxide dismutase (SOD), catalase (CAT), glutathione
peroxidase (GSH-Px)] are the natural barriers between cells and
plasma, which can promote the reactions of various proteins,
microorganisms and enzymes in the body, and inhibit or transform
the generation of ROS (10,11).
This study investigated the clinical efficacy of
intravenous anesthesia on breast segmental surgery and its effects
on hemodynamics by detecting hemodynamic parameters [systolic blood
pressure (SBP), diastolic blood pressure (DBP), heart rate (HR)],
OS response indicator and other data of patients in the two groups
with breast segmental surgery under intravenous anesthesia and
inhalation anesthesia.
Patients and methods
General information
A total of 267 patients were selected, who underwent
breast segmental surgery in Chun'an First People's Hospital
(Hangzhou, China) from March 2015 to September 2018. Among them,
137 patients under intravenous anesthesia were the research group,
with an average age of 40.75±6.88 years. There were 62 patients
with hypertension, 55 patients with hyperlipidemia, 31 cases with
breast cancer, 36 cases of breast fibroids, 37 cases with benign
breast masses and 33 cases of localized cystic hyperplasia of the
breast. The 130 patients who received inhalation anesthesia were
the control group, with an average age of 39.87±6.31 years. There
were 58 patients with hypertension, 60 patients with
hyperlipidemia, 29 cases of breast cancer, 34 cases of breast
fibroids, 36 cases of benign breast masses and 31 cases of
localized cystic hyperplasia of the breast.
Inclusion criteria: Patients accompanied by family
members upon admission, patients aged between 30 and 50 years,
those with education level of primary school or above, complete
clinical data and good compliance, and voluntary cooperation on
follow-up investigation; patients in Grades I-II of the American
Society of Anesthesiologists (ASA), with the operation time between
30 to 50 min.
Exclusion criteria: Patients with unconsciousness;
patients allergic to narcotic drugs; patients with severe organic
diseases, patients who were unable to cooperate with the
examination due to other factors such as aphasia, dysphoria and
other communication disorders.
This study was approved by the Ethics Committee of
the Chun'an First People's Hospital. All patients and their
families were informed prior to the study and provided a signed
complete informed consent.
Anesthesia methods
Patients fasted for 8 h before surgery and were
forbidden to drink 6 h before surgery. Before anesthesia, the
venous access on one side of the patient was normally opened, and
routine items such as electrocardiogram (ECG), respiratory rate
(RR), (SpO2), SBP, DBP, and HR were monitored without any
pre-anesthesia drugs. Propofol (Shanghai Yuanye Biotechnology Co.,
Ltd.; B33792-100 mg) 1-2 mg/kg combined with remifentanil (Shanghai
KE WEI CHEM; R143501) 0.5 µg/kg was used to induce anesthesia in
the research group, and propofol 4 mg/kg/h combined with
remifentanil 12 µg/kg/h was used for anesthesia maintenance. The
control group was anesthetized with 6% sevoflurane (YKPPSJ-009985)
volatilization tank and 6 l/min oxygen flow rate, and anesthesia
was maintained with 2-4% sevoflurane volatilization tank and 1-2
l/min oxygen flow rate. Then the position of laryngeal mask was
determined and inserted, the respiratory frequency was adjusted to
12-16 times/min and the tidal volume to 6-10 ml/kg. After surgery,
the extubation time was recorded, and then the patients were sent
to PACU for awakening. The awakening time of patients, the number
of dysphoria in the awakening period and eye-opening time were
recorded. If the patient had hypotension during surgery, 6 mg
ephedrine was given intravenously, and 0.5 mg atropine was given
intravenously for bradycardia.
Assay methods
Enzyme activity determination: 5-8 ml central venous
blood was extracted from patients at different time points, T
before surgery, T6, T24, T48 and T72 h after surgery. The collected
venous blood was placed in heparin sodium blood collection vessel,
centrifuged at 1,369.55 x g, at 4˚C for 8 min to separate serum,
and the separated serum was stored at -80˚C for later testing. SOD,
CAT and GSH-Px activities were determined. The determination method
was in accordance with the description in the kit (WST-1 method was
used to determine SOD activity, visible spectrophotometry was used
to determine CAT activity, and colorimetry was used to determine
GSH-Px activity). SOD kit: Shanghai Yubo Biotechnology Co., Ltd.,
IC-SOD-Ra; CAT kit: Shanghai Jingkang Bioengineering Co., Ltd.,
JKSJ-1907; GSH-Px kit: Shanghai Jingkang Bioengineering Co., Ltd.,
JK-EA00285.
Main instruments and equipment
Main instruments and equipment were as follows:
Multi-functional ECG monitor (Shanghai Hanfei Medical Equipment
Co., Ltd.; BSM-3763), anesthesia machine (Beijing First Product
Condar RE902-C6 06), full-automatic blood gas analyzer (Shanghai
Yuyan Scientific Instrument Co., Ltd.; 57984), 96-well plate
(Beijing ZEPING Bioscience & Technologies Co., Ltd.; Nunc 003),
high-speed and low-temperature centrifuge (Sichuan Shuke Instrument
Co., Ltd.; TGL-16), Enzyme reader (Wuhan ESCN KIT INC. SMR16.1),
vortex mixer (Shenzhen Cygen Biotechnology Co., Ltd.; S0200-230V),
enzyme-free centrifuge tube (Shanghai Qiming Biological Technology
Co., Ltd.; OX02849).
Observation indicators
The postoperative clinical efficacy, general
conditions and adverse reactions of the two groups of patients were
observed. SBP, DBP and HR were monitored in two groups of patients
before anesthesia induction (T0), before laryngeal mask insertion
(T1), 30 min after anesthesia (T2), and 3 h after surgery (T3). The
mini-mental state examination (MMSE) scores at 1 d before
operation, 1 and 3 d after operation were measured to evaluate the
cognitive function before and after operation. MMSE scale includes
30 single items in five categories: Orientation, memory, attention
and calculation, recall and language. Scores on the MMSE range from
0 to 30, with scores of 27 or higher being traditionally considered
normal. Scores less than 27 generally indicate cognitive
dysfunction: 21-26 points are mild impairment, 10-20 are moderate
impairment, and 0-9 are severe impairment (12). The visual analogue scale (VAS)
scores of the two groups of patients were recorded 1 day before
operation and 1 day after operation. VAS uses 11 numbers from 0 to
10 to indicate the degree of pain. 0, no pain, and 10 the worst
possible pain. The patient chooses one of the 11 numbers to best
describe their current pain. 0 points, no pain; ≤3 points, slight
pain that can be tolerated; 4 points to 6 points, pain that affects
sleep, but still tolerable; 7 points to 10 points, indicates that
the patient has unbearable pain that affects appetite and sleep
(13). The blood samples collected
at T, T6, T24, T48 and T72 h were used to detect the activity of
SOD, CAT and GSH-Px in the serum of patients.
Statistical analysis
SPSS 22.0 (SPSS, Inc.) was used to analyze the data.
GraphPad Prism 7 was used for figures (GraphPad Software, Inc.).
Count data were expressed as [n (%)], and Chi-square test was used
to compare between groups. Measurement data were presented as mean
± SD, and t-test was used to compare two groups. ANOVA (parameter)
and Tukey were used for multiple comparison. P<0.05 was
considered to indicate a statistically significant difference.
Results
Comparison of clinical general
data
The patients between the two groups were compared in
terms of age, body mass index, history of smoking and drinking,
education level and complications (P>0.05), which was comparable
(Table I).
 | Table IComparison of clinical general data
[mean ± SD, n (%)]. |
Table I
Comparison of clinical general data
[mean ± SD, n (%)].
| Characteristics | Research group
(n=137) | Control group
(n=130) | χ2/t | P-value |
|---|
| Average age
(years) | 40.75±6.88 | 39.87±6.31 | 1.09 | 0.28 |
| Body mass index
(kg/m2) | 21.60±2.50 | 21.80±2.30 | 0.68 | 0.50 |
| History of
smoking | | | 0.09 | 0.76 |
|
Yes | 37 (27.01) | 33 (25.38) | | |
|
No | 100 (72.99) | 97 (74.62) | | |
| History of
drinking | | | 0.03 | 0.86 |
|
Yes | 20 (14.60) | 18 (13.85) | | |
|
No | 117 (85.40) | 112 (86.15) | | |
| Education level | | | 0.10 | 0.95 |
|
Primary
school | 22 (16.06) | 19 (14.62) | | |
|
Junior high
school | 82 (59.85) | 79 (60.77) | | |
|
Junior
college or above | 33 (24.09) | 32 (24.62) | | |
| Complications | 117 (85.41) | 118 (90.77) | 1.82 | 0.18 |
|
Hypertension | 62 (45.26) | 58 (44.62) | 0.01 | 0.92 |
|
Hyperlipidemia | 55 (40.15) | 60 (46.15) | 0.98 | 0.32 |
| Time of operation
(min) | 38.81±8.22 | 39.12±7.84 | 1.32 | 0.75 |
| ASA
classification | | | 0.49 | 0.49 |
|
Grade I | 119 (86.86) | 109 (83.85) | | |
|
Grade
II | 18 (13.14) | 21 (16.15) | | |
Comparison of clinical efficacy
Statistical analysis showed that the total effective
rate of the research group (91.24%) was not significantly different
from that of the control group (90.77%) (P>0.05; Table II).
 | Table IIComparison of clinical efficacy [n
(%)]. |
Table II
Comparison of clinical efficacy [n
(%)].
| Group | Cure | Markedly
effective | Effective | Ineffective | Total effective
rate |
|---|
| Research group
(n=137) | 38 (27.74) | 52 (37.96) | 35 (25.55) | 12 (8.75) | 125 (91.24) |
| Control group
(n=130) | 36 (27.70) | 47 (36.15) | 34 (26.15) | 13 (10.00) | 117 (90.00) |
| χ2 | - | - | - | - | 0.06 |
| P-value | - | - | - | - | 0.81 |
Comparison of general conditions
before and after operation
The general conditions of patients in the two groups
before and after surgery were recorded (Table III). The body movement, dysphoria
during the awakening period, eye-opening time and extubation time
in the research group were lower than those in the control group
(P<0.05), there was no significant difference in PONV between
the two groups (P>0.05), while hypotension during surgery in the
research group was significantly higher than that in the control
group (P<0.05).
 | Table IIIComparison of general conditions
before and after surgery [mean ± SD, n (%)]. |
Table III
Comparison of general conditions
before and after surgery [mean ± SD, n (%)].
| Group | Body movement
during surgery | Hypotension during
surgery | Extubation time
(min) | Dysphoria during
the awakening period | Eye-opening time
(min) | PONV |
|---|
| Research group
(n=137) | 8 (5.84) | 20 (14.60) | 9.3±4.2 | 2 (1.46) | 6.2±2.4 | 10 (7.30) |
| Control group
(n=130) | 18 (13.85) | 2 (1.54) | 12.3±4.9 | 14 (10.77) | 8.7±3.5 | 12 (9.23) |
|
χ2/t | 4.87 | 15.05 | 5.38 | 120.26 | 6.84 | 0.33 |
| P-value | 0.03 | <0.01 | <0.01 | <0.01 | <0.01 | 0.57 |
Comparison of hemodynamic
indicators
Before anesthesia, there was no significant
difference in the hemodynamic indicators of the two groups
(P>0.05). The levels of SBP and DBP were significantly lower at
T1 and T2 than those at T0 (P<0.05), and those at T1 were lower
than those at T2 (P<0.05). There was no significant difference
in the levels of SBP and DBP between T3 and T0 (P>0.05), while
the levels of SBP and DBP at T1 and T2 in the control group were
significantly higher than those in the research group (P<0.05).
There was no difference in HR in the control group at T1, T2, T3
and T0 (P>0.05), HR in the research group at T1 and T2 was lower
than that at T0 and corresponding time points of the control group
(P<0.05), and HR at T3 and T0 had no significant difference
(P>0.05; Table IV).
 | Table IVComparison of hemodynamic indicators
at different time points (mean ± SD). |
Table IV
Comparison of hemodynamic indicators
at different time points (mean ± SD).
| Indicators | Group | T0 | T1 | T2 | T3 | F | P-value |
|---|
| SBP (mmHg) | Research group | 121.4±10.7 |
106.5±9.6a |
110.5±9.4a | 119.5±9.1 | 74.88 | <0.01 |
| | Control group | 122.2±10.9 |
115.3±9.2a | 119.9±9.3 | 120.4±9.3 | 11.92 | <0.01 |
| | t | 0.61 | 7.64 | 8.21 | 0.80 | | |
| | P-value | 0.55 | <0.01 | <0.01 | 0.42 | | |
| DBP (mmHg) | Research group | 81.5±8.5 |
73.5±7.4a |
75.9±7.3a | 80.2±7.9 | 31.27 | <0.01 |
| | Control group | 82.6±7.6 |
78.7±6.9a | 81.1±6.4 | 81.3±7.2 | 6.93 | <0.01 |
| | t | 0.11 | 5.93 | 6.18 | 1.19 | | |
| | P-value | 0.27 | <0.01 | <0.01 | 0.24 | | |
| HR (times/min) | Research group | 75.4±7.0 |
69.8±6.5a |
71.8±6.6a | 75.4±6.9 | 23.12 | <0.01 |
| | Control group | 76.0±7.2 | 74.5±7.0 | 75.2±6.9 | 75.8±7.1 | 1.19 | 0.31 |
| | t | 0.69 | 5.69 | 4.12 | 0.47 | | |
| | P-value | 0.49 | <0.01 | <0.01 | 0.64 | | |
Comparison of adverse reactions after
surgery
Comparison of postoperative adverse reactions of
patients (Table V) showed that
adverse reactions of patients in both groups were relieved after
symptomatic treatment, and there was no difference between the
research group and the control group (P>0.05).
 | Table VComparison of postoperative adverse
reactions [n (%)]. |
Table V
Comparison of postoperative adverse
reactions [n (%)].
| Group | Dizziness | Cough | Insomnia | Headache | Rash | Inappetite | Incidence rate of
adverse reactions |
|---|
| Research group
(n=137) | 4 (2.92) | 2 (1.46) | 6 (4.38) | 5 (3.65) | 0 (0.00) | 4 (2.92) | 21 (15.33) |
| Control group
(n=130) | 6 (4.62) | 6 (4.62) | 6 (4.62) | 3 (2.31) | 1 (0.75) | 4 (3.08) | 26 (20.00) |
| χ2 | 0.53 | 2.29 | 0.01 | 0.41 | 1.06 | 0.01 | 1.00 |
| P-value | 0.47 | 0.13 | 0.93 | 0.52 | 0.30 | 0.94 | 0.32 |
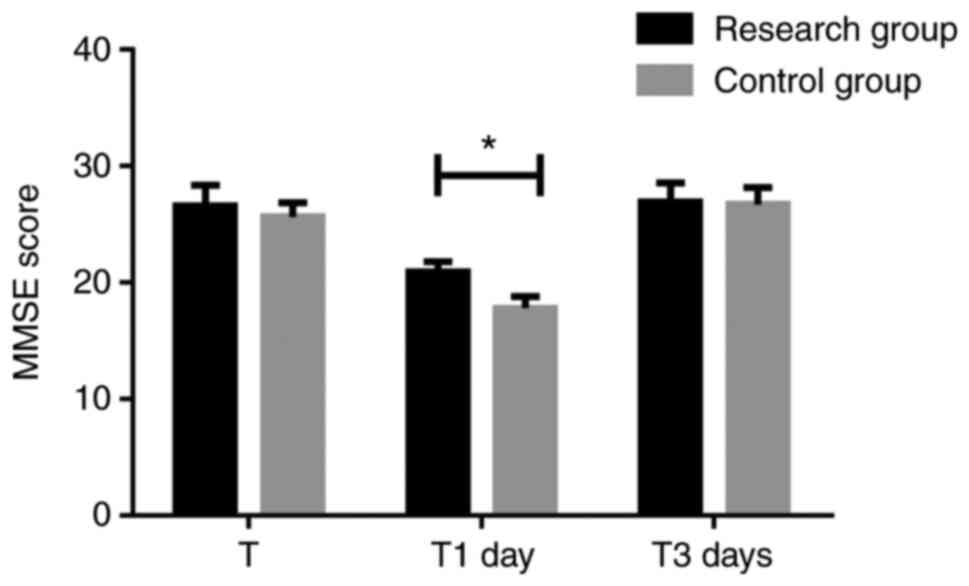
Comparison of MMSE score
According to the MMSE scores of patients in the two
groups (Fig. 1), there was no
significant difference between the research group (26.63±1.74) and
the control group (25.65±1.23) on the first day before surgery
(P>0.05). On the first day after surgery, both groups decreased,
but the score in the research group (20.92±0.88) was higher than
that in the control group (17.83±0.98) (P<0.05). Three days
after surgery, the research group (26.95±1.63) and the control
group (26.70±1.48) returned to normal (P>0.05), there was no
significant difference between the groups (P>0.05).
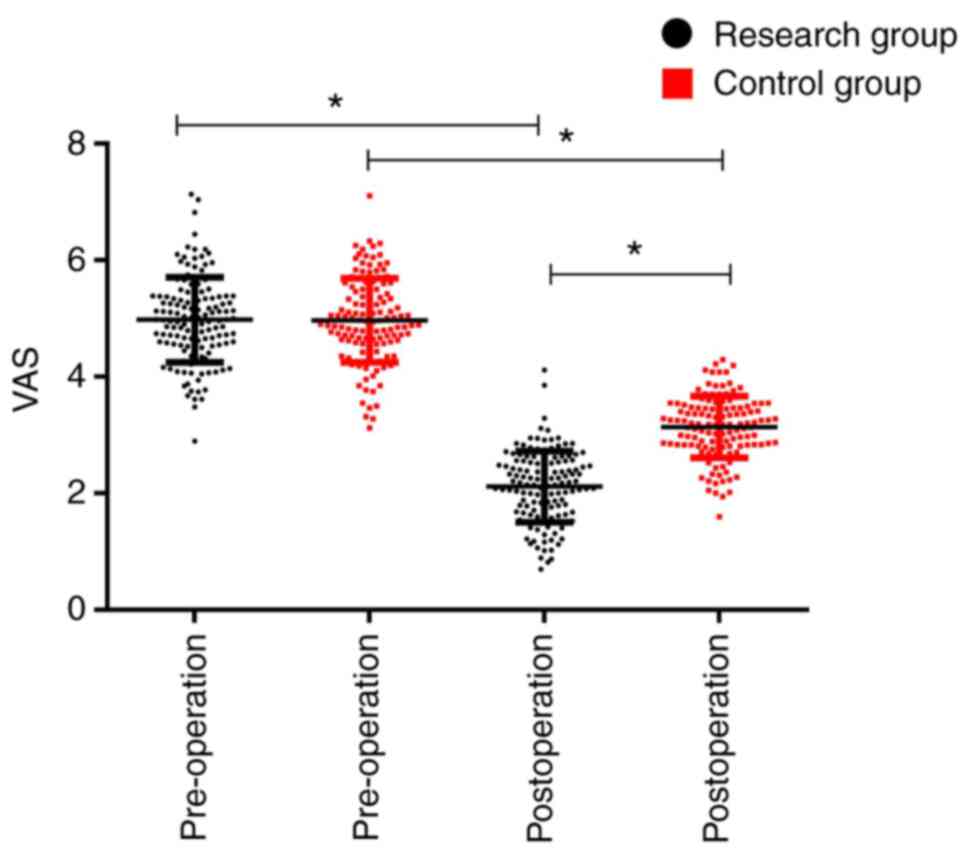
Comparison of VAS score
According to the VAS scores of patients in the two
groups (Fig. 2), there was no
significant difference between the research group (4.89±0.66) and
the control group (4.98±0.70) before surgery (P>0.05); after
surgery, both groups were significantly lower than those before
surgery (P<0.05), while the research group (2.17±0.59) was
significantly lower than that of the control group (3.17±0.59)
(P<0.05).
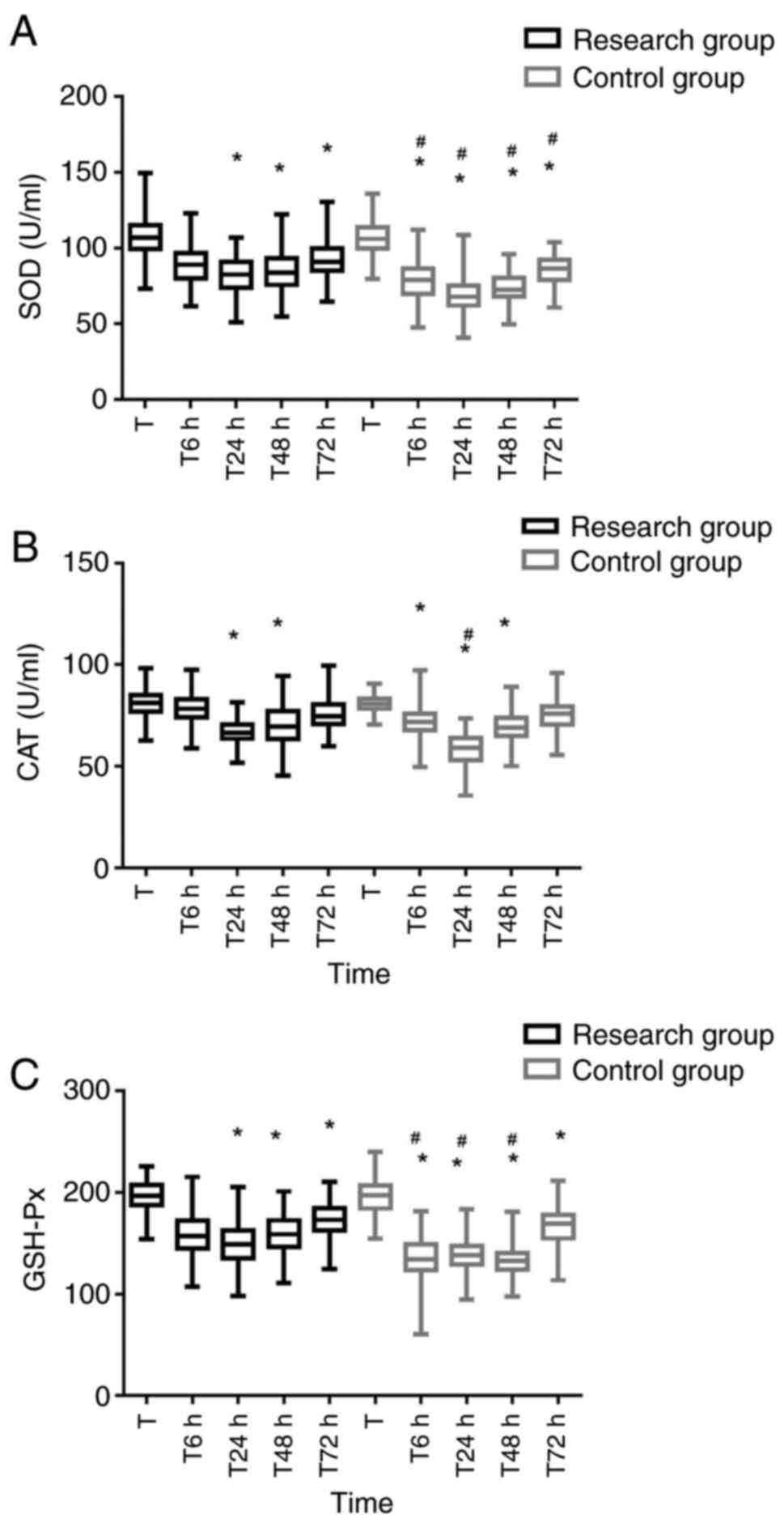
Comparison of serum SOD, CAT and
GSH-Px activities
The activities of SOD, CAT and GSH-Px of patients in
the two groups at T24 and T48 h were lower than those at T
(P<0.05), while the activities of SOD and GSH-Px in the control
group at T72 h were still lower than those at T (P<0.05), and
the CAT activity returned to normal (P>0.05). In the research
group, when SOD at T72 h was lower than those at T (P<0.05), CAT
and GSH-Px activities returned to normal (P>0.05). The
activities of SOD, CAT and GSH-Px in the control group at T6 h were
lower than those at T (P<0.05). When the GSH-Px activity at T6 h
was lower than that at T (P<0.05), SOD and CAT had no
significant difference at T (P>0.05). The SOD activity in the
control group was significantly lower than that in the research
group from T6 to T72 h (P<0.05), while the CAT activity in the
control group was significantly lower than that in the research
group at T24 h (P<0.05). Compared with the research group, the
GSH-Px activity in the control group decreased significantly from
T6 to T48 h (P<0.05; Fig.
3).
 | Figure 3Comparison of serum SOD, CAT and
GSH-Px activities at different time points. (A) Comparison of serum
SOD activities at different time points. (B) comparison of serum
CAT activities at different time points. (C) Comparison of serum
GSH-Px activities at different time points. SOD, CAT and GSH-Px
activities of patients in the two groups were lower at T24 and T48
h than those at T, while SOD and GSH-Px activities in the control
group were still lower at T72 h than those at T. The SOD in the
research group was lower at T72 h than that at T, and the
activities of SOD, CAT and GSH-Px in the control group at T6 h were
lower than those at T. When GSH-Px activity in the research group
was lower at T6 h than that at T, SOD activity in the control group
was significantly lower than that in the research group from T6 h
to T72 h, while CAT activity in the control group was significantly
lower than that in the research group at T24 h (P<0.05). The
GSH-Px activity of the control group decreased significantly from
T6 to T48 h compared with those in the research group (P<0.05).
#P<0.05, compared with the research group at the same
time point; *P<0.05, compared with T0. SOD,
superoxide dismutase; CAT, catalase; GSH-Px, glutathione
peroxidase. |
Discussion
In surgical operations, ideal anesthesia requires
stable hemodynamics and rapid anesthesia induction. Patients should
wake up quickly and completely after withdrawal of drugs, without
dysphoria after surgery, respiratory depression and drug residue
(14). At present, the clinical
application of intravenous anesthesia is gradually paid attention
to. In clinical general anesthesia, propofol combined with
remifentanil is mainly used for drug compatibility, which has the
advantages of rapid anesthesia and postoperative recovery (15,16).
Propofol (17) can be rapidly
removed from the central ventricle through liver metabolism and
renal excretion, while remifentanil (18,19)
can be rapidly degraded by non-specific esterase, which was
advantageous in rapid action, short action time, rapid removal
without accumulation during continuous infusion. Inhalation
anesthesia also has advantages including quick effect and
discharge, little influence on circulation and respiration, and
non-invasive administration. Therefore, intravenous compound
anesthesia is often used in order to give full play to the
characteristics of various drugs and achieve stable anesthesia,
less physiological disturbance and side effects as well as quick
recovery (20).
In this study, it was found that the total effective
rate of the research group (91.24%) was not significantly different
from that of the control group (90.77%) (P>0.05). In the
randomized controlled trial of propofol intravenous anesthesia and
isoflurane inhalation anesthesia by Visser et al (21), the total effective rate of the two
anesthesia methods was not significantly different, which was
similar to our results. Therefore, we speculated that anesthesia
methods had certain influence on clinical efficacy, but the main
influence was still on the condition of patients, operation methods
and other reasons. In this study, the number of hypotension during
surgery in the research group was also significantly higher than
that in the control group (P<0.05). In the research group before
and after surgery, body movement during surgery, dysphoria during
the awakening period, eye-opening time and extubation time were
lower than those of the control group (P<0.05). Kim et al
(22) compared
remifentanil+propofol and remifentanil+sevoflurane, and the results
revealed that the propofol group had a shorter awakening time and
extubation time. In the research of Scott et al (23), it was found that although propofol
and remifentanil had different pharmacodynamic effects, the two
drugs interacted in realizing loss of consciousness and analgesia.
The use of analgesia in total intravenous anesthesia can produce an
effect of saving propofol and possibly minimize the inhibition of
EEG activity. Presumably, the research group used propofol combined
with remifentanil, which had short duration of stay in vivo
and short recovery time after surgery, so the research group had
shorter recovery time than the control group. In a previous study,
the increase of incidence rate of PONV was related to inhalation
anesthetics (24), however, there
was no significant difference in the incidence rate of PONV between
the research group and the experimental group in this study
(P>0.05), and there were certain differences between this study
and their research, which is why further research was needed.
The SBP, DBP and HR of patients all returned to
normal levels 3 h after anesthesia. Mohaghegh et al
(25) compared the effects of
propofol intravenous anesthesia and isoflurane inhalation
anesthesia on postoperative pain of inguinal hernia, and found that
there was no significant difference in SBP, DBP and HR between the
two groups after induction, during intubation, after intubation and
extubation (P>0.05). In our study, although there was no
significant difference in SBP, DBP, HR at T3 and T0 (P>0.05),
there was a significant difference in SBP, DBP in the two groups
between T1, T2 and T0 (P<0.05). HR in the research group at T1
and T2 was lower than those at T0 (P<0.05), it was presumed that
propofol combined with remifentanil was used in the research group,
while Mohaghegh et al (25)
just used propofol, because remifentanil might make hemodynamic
fluctuation more obvious, so further detailed study was needed.
Compared with the control group, the hemodynamic fluctuation of
patients in the research group was more obvious. The levels of SBP
and DBP in the two groups were significantly lower at T1 and T2
than those at T0 (P<0.05), and those at T1 were lower than those
at T2 (P<0.05), while the levels of SBP and DBP at T1 and T2 in
the control group were significantly higher than those in the
research group (P<0.05). HR of research group at T1 and T2 was
lower than that at T0 and corresponding time in control group
(P<0.05). The number of hypotension during surgery was
significantly higher than that of the control group, because both
drugs could inhibit the circulation of the body to a certain
extent, the SBP, DBP and HR in the research group were generally
lower than those in the control group, which was prone to
hypotension during surgery and bradycardia (26).
In this study, there was no difference in adverse
reactions between the research group and the control group
(P>0.05); after symptomatic treatment, the adverse reactions of
patients in both groups were relieved. MMSE scores of patients in
the two groups decreased one day after surgery, but the score was
higher in the research group than that in the control group
(P<0.05). The scores of both groups returned to normal level
three days after surgery (P>0.05). Yu (27) confirmed that the 12 h MMSE scores of
patients 1, 6 and 12 h after surgery were significantly lower than
those before surgery (P<0.05) by analyzing the effect of
propofol and sevoflurane combined anesthesia on cognitive function
of elderly patients undergoing total thoracic surgery. The score of
propofol group was higher than that in the sevoflurane group
(P<0.05), which was consistent with the results of the present
study. However, patients returned to normal after three days of
follow-up, and it was presumed that propofol combined with
remifentanil or sevoflurane would both affect the cognitive
function of patients to a certain extent during surgery, while
propofol combined with remifentanil had relatively little effect on
the cognitive function, but neither anesthesia have permanent
effect on it. In this study, the VAS scores of the two groups were
significantly lower after surgery than those before surgery
(P<0.05), while the score of research group was significantly
lower than that in the control group (P<0.05). Research of
Elbakry et al (28) on the
influence of inhalation (desflurane) and total intravenous
anesthesia (propofol and dexmedetomidine) on postoperative
rehabilitation of morbid obesity patients after laparoscopic sleeve
gastrectomy showed the intravenous anesthesia group had a lower
postoperative VAS (P<0.001), which was consistent with the
results of this study. It indicated that when propofol or
sevoflurane was used during surgery, it could alleviate the need
for postoperative analgesia to a certain extent, as well as the
need for analgesia of patients undergoing propofol anesthesia.
In the present study, the activities of SOD, CAT and
GSH-Px of patients in the two groups were lower at T24 and T48 h
than those at T (P<0.05), while the activities of SOD and GSH-Px
in the control group at T72 h were still lower than those at T
(P<0.05). In the research group, SOD was lower at T72 h than
that at T (P<0.05). The activities of SOD, CAT and GSH-Px in the
control group at T6 h were lower than those at T (P<0.05).
GSH-Px activity in the research group at T6 h was lower than that
at T (P<0.05). SOD activity in the control group was
significantly lower than that in the research group from T6 to T72
h (P<0.05), while CAT activity in the control group was
significantly lower than that in the research group at T24 h
(P<0.05). The GSH-Px activity of the control group decreased
significantly from T6 to T48 h compared with that in the research
group (P<0.05). In a previous study (29) propofol inhibited mitochondrial
dysfunction and OS of liver I/R, propofol instead of sevoflurane
prevented mitochondrial dysfunction and OS by limiting the
activation of HIF-1α in liver ischemia/reperfusion injury. The SOD
activity in the research group was significantly higher than that
in the control group, which was in accordance with the results of
this study, indicating that propofol had stronger inhibition on OS
response of patients compared with sevoflurane. Since there was no
significant difference between the research group and the control
group at T72 h and patients in the two groups gradually recovering
over time, it was presumed that sevoflurane also had certain
antagonism to OS.
This study comprehensively explored the clinical
efficacy of breast segmental surgery under intravenous anesthesia
and inhalation anesthesia and the changes of patients' hemodynamics
and OS response, with the aim to provide certain reference for
clinical research. However, the specific mechanism of intravenous
anesthesia and the influence in different surgeries need to be
further explored, the relationship between clinical pathological
factors and anesthesia methods needs to be analyzed by multiple
factors, and the application of intravenous anesthesia in clinical
practice needs to be further studied, to explore the influence of
various factors on clinical efficacy, to provide reference for more
accurate judgment of patients.
In summary, intravenous anesthesia can reduce the
occurrence of postoperative adverse reactions, improve sedation and
analgesia, and make patients wake up quickly and stably after
surgery, and recover cognitive function and OS rapidly, but it has
a great impact on hemodynamics during surgery. Attention should be
paid to maintaining hemodynamic stability and avoiding occurrence
of hypotension and bradycardia during surgery. Furthermore, it is a
better anesthesia method for breast segmental surgery.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XY, YZ and HH conceived and designed the study, and
drafted the manuscript. XY, XZ, SS and HH collected, analyzed and
interpreted the experimental data. YZ revised the manuscript for
important intellectual content. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Chun'an First People's Hospital (Hangzhou, China). Signed written
informed consents were obtained from the patients and/or
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mahmoud M and Mason KP: Recent advances in
intravenous anesthesia and anesthetics. F1000Res 7: F1000 Faculty
Rev-470 F1000 Faculty Rev-470, 2018.
|
|
2
|
Absalom AR and Mason KP: Total intravenous
anesthesia and target controlled infusions. 2017 doi:
10.1007/978-3-319-47609-4.
|
|
3
|
Poprac P, Jomova K, Simunkova M, Kollar V,
Rhodes CJ and Valko M: Targeting free radicals in oxidative
stress-related human diseases. Trends Pharmacol Sci. 38:592–607.
2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Athar M: Oxidative stress and experimental
carcinogenesis. Indian J Exp Biol. 40:656–667. 2002.PubMed/NCBI
|
|
5
|
Ishii T, Yasuda K, Akatsuka A, Hino O,
Hartman PS and Ishii N: A mutation in the SDHC gene of complex II
increases oxidative stress, resulting in apoptosis and
tumorigenesis. Cancer Res. 65:203–209. 2005.PubMed/NCBI
|
|
6
|
Ray G, Batra S, Shukla NK, Deo S, Raina V,
Ashok S and Husain SA: Lipid peroxidation, free radical production
and antioxidant status in breastcancer. Breast Cancer Res Treat.
59:163–170. 2000.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Saygili EI, Akcay T, Konukoglu D and
Papilla C: Glutathione and glutathione-related enzymes in
colorectal cancer patients. J Toxicol Environ Health A. 66:411–415.
2003.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Höhn A, Weber D, Jung T, Ott C, Hugo M,
Kochlik B, Kehm R, König J, Grune T and Castro JP: Happily (n)ever
after: Aging in the context of oxidative stress, proteostasis loss
and cellular senescence. Redox Biol. 11:482–501. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Tain RW, Scotti AM, Li W, Zhou XJ and Cai
K: Imaging short-lived reactive oxygen species (ROS) with
endogenous contrast MRI. J Magn Reson Imaging. 47:222–229.
2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Davis SM and Pennypacker KR: Targeting
antioxidant enzyme expression as a therapeutic strategy for
ischemic stroke. Neurochem Int. 107:23–32. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ahmed RG: The physiological and
biochemical effects of diabetes on the balance between oxidative
stress and antioxidant defense system. Med J Islamic World Acad
Sci. 15:31–42. 2005.
|
|
12
|
Wong A, Black SE, Yiu SYP, Au LWC, Lau
AYL, Soo YOY, Chan AYY, Leung TWH, Wong LKS, Kwok TCY, et al:
Converting MMSE to MoCA and MoCA 5-minute protocol in an
educationally heterogeneous sample with stroke or transient
ischemic attack. Int J Geriatr Psychiatry. 33:729–734.
2018.PubMed/NCBI View
Article : Google Scholar
|
|
13
|
Le May S, Ballard A, Khadra C, Gouin S,
Plint AC, Villeneuve E, Mâsse B, Tsze DS, Neto G, Drendel AL, et
al: A comparison of the psychometric properties of three pain
scales used in the pediatric emergency department: VAS, FPS-R and
CAS. Pain. 159:1508–1517. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Soleimani A, Heidari N, Habibi MR, Kiabi
FH, Khademloo M, Emami Zeydi A and Sohrabi FB: Comparing
hemodynamic responses to diazepam, propofol and etomidate during
anesthesia induction in patients with left ventricular dysfunction
undergoing coronary artery bypass graft surgery: A double-blind,
randomized clinical trial. Med Arch. 71:198–203. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Masjedi M, Zand F, Kazemi AP and
Hoseinipour A: Prophylactic effect of ephedrine to reduce
hemodynamic changes associated with anesthesia induction with
propofol and remifentanil. J Anaesthesiol Clin Pharmacol.
30:217–221. 2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cho YJ, Kim TK, Hong DM, Seo JH, Bahk JH
and Jeon Y: Effect of desflurane-remifentanil vs.
Propofol-remifentanil anesthesia on arterial oxy genation during
one-lung ventilation for thoracoscopic surgery: A prospective ran
domized trial. BMC Anesthesiol. 17(9)2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Feng AY, Kaye AD, Kaye RJ, Belani K and
Urman RD: Novel propofol derivatives and implications for
anesthesia practice. J Anaesthesiol Clin Pharmacol. 33:9–15.
2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Battershill AJ and Keating GM:
Remifentanil: A review of its analgesic and sedative use in the
intensive care unit. Drugs. 66:365–385. 2006.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kisilcwicz M, Rosenhcrg H and Vaillancourt
C: Remifentanil for procedural sedation; a systematic review of the
literature. Emerg Mcd J. 34:294–301. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Xu R, Zhou S, Yang J, Li H, Zhang Q, Zhang
G, Xu S and Peng Q: Total intravenous anesthesia produces outcomes
superior to those with combined intravenous-inhalation anesthesia
for laparoscopic gynecological surgery at high altitude. J Int Med
Res. 45(246)2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Visser K, Hassink EA, Bonsel GJ, Moen J
and Kalkman C: Randomized controlled trial intravenous anesthesia
with propofol versus inhalation anesthesia with isoflurane-nitrous
oxide. Anesthesiology. 95:616–626. 2001.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kim H, Choi SH, Choi YS, Lee JH, Kim NO
and Lee JR: Comparison of the antitussive effect of remifentanil
during recovery from propofol and sevoflurane anaesthesia.
Anaesthesia. 67:765–770. 2012.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Scott HB, Choi SW, Wong GTC and Irwin MG:
The effect of remifentanil on propofol requirements to achieve loss
of response to command vs. loss of response to pain. Anaesthesia.
72:479–487. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Park SK and Cho EJ: A randomized
controlled trial of two different interventions for the prevention
of postoperative nausea and vomiting; total intravenous anaesthesia
using propofol and remifentanil versus prophylactic palonosetron
with inhalational anaesthesia using sevofluraef-nitrous oxide. J
Int Med Res. 39:1808–1815. 2011.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Mohaghegh T, Yazdi B, Norouzi A, Fateh S,
Modir H and Mohammadbeigi A: Effect of intravenous anesthesia with
propofol versus isoflurane inhalation anesthesia in postoperative
pain of inguinal herniotomy: A randomized clinical trial. Med Gas
Res. 7:86–92. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Oncul S, Gaygusuz EA, Yilmaz M, Terzi H
and Balci C: Comparison of ketamine-propofol and remifentanil in
terms of hemodynamic variables and patient satisfaction during
monitored anaesthesia care. Anasthesiol Intensive Ther. 48:116–121.
2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Yu W: Anesthesia with propofol and
sevoflurane on postoperative cognitive function of elderly patients
undergoing general thoracic surgery. Pak J Pharm Sci. 30:1107–1110.
2017.PubMed/NCBI
|
|
28
|
Elbakry AE, Sultan WE and Ibrahim E: A
comparison between inhalational (Desflurane) and total intravenous
anaesthesia (Propofol and dexmedetomidine) in improving
postoperative recovery for morbidly obese patients undergoing
laparoscopic sleeve gastrectomy: A double-blinded randomised
controlled trial. J Clin Anesth. 45:6–11. 2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Bellanti F, Mirabella L, Mitarotonda D,
Blonda M, Tamborra R, Cinnella G, Fersini A, Ambrosi A, Dambrosio
M, Vendemiale G and Serviddio G: Propofol but not sevoflurane
prevents mitochondrial dysfunction and oxidative stress by limiting
HIF-1α activation in hepatic ischemia/reperfusion injury. Free
Radic Biol Med. 3:323–333. 2016.PubMed/NCBI View Article : Google Scholar
|