Introduction
Giant intracranial aneurysm is a rare entity defined
by a diameter of at least 25 mm, accounting for 5% of all cases of
intracranial aneurysm (1). Giant
intracranial aneurysm of the posterior circulation occurs even more
infrequently and is associated with high morbidity and mortality
rates, even when treated. Due to the small size of the posterior
fossa, unruptured giant posterior circulation aneurysm exerts a
substantial mass effect on the brainstem and the adjacent cranial
nerves, leading to cranial nerve palsy, motor impairment and
hydrocephalus, and may result in variable levels of disability.
Although the treatment of anterior circulation giant aneurysm with
microsurgery and bypass has been moderately successful (2,3), the
treatment of posterior circulation giant aneurysm according to the
same method is associated with poor prognosis, mainly due to
occlusion of the perforating artery, resulting in brainstem
ischemia (4). With regard to giant
and complex intracranial aneurysm that cannot be managed by
surgical strategies, Pipeline with coil embolization is an
alternative treatment (5,6). However, the mortality and morbidity
rates of post-circulation aneurysm treated using flow diversion
devices are much higher compared with those of pre-circulation
aneurysm (7). In the present case
report, contrast agent retention in the aneurysm lumen and the
development of distal blood vessels were evaluated to determine the
influence of bilateral vertebral artery blood flow dynamics on the
aneurysm. Optimal treatment measures were then formulated in order
to achieve the best possible recovery of the patient.
Case report
History and examination
The patient was a 26-year-old female admitted to
Xuanwu Hospital of Capital Medical University (Beijing, China) in
March 2018, who had been experiencing symptoms of neck discomfort
for 1 year and left-sided walking for 1 month. In January 2017, the
patient experienced neck discomfort, dizziness when raising the
head after lowering it and a headache. The patient was first
assumed to have cervical spondylosis and received physical therapy
at a local hospital. However, the headache was not relieved. In
February 2018, the patient experienced left-sided walking, left
hand tremors, dysphagia and slight hoarseness. Local cervical MRI
revealed no obvious signs of cervical disease; however, it did
reveal a large, abnormal signal shadow associated with the
vertebrobasilar artery. Further head MRI and magnetic resonance
angiography (MRA) revealed a large vertebrobasilar aneurysm and
obvious compression of the brain stem. Physical examination
revealed an obvious left-slant tongue extension, hoarseness,
left-hand tremors, Medical Research Council (8) grade 5- muscle strength in
the left-limb and negative bilateral finger-to-nose and
heel-to-knee tibia tests. After admission to the hospital,
high-resolution MRI revealed a thrombus inside the aneurysm and an
enhanced aneurysm wall (Fig. 1).
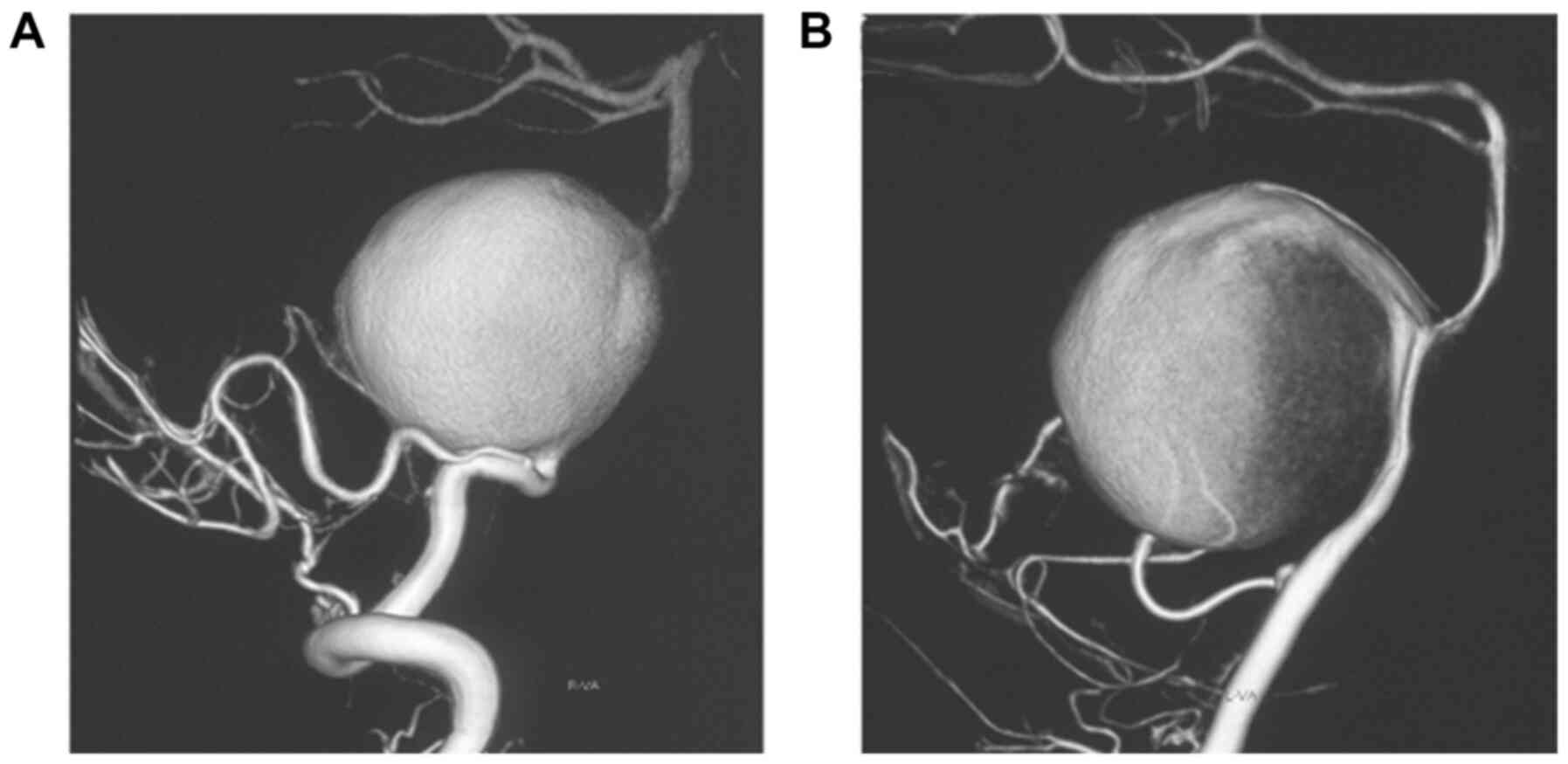
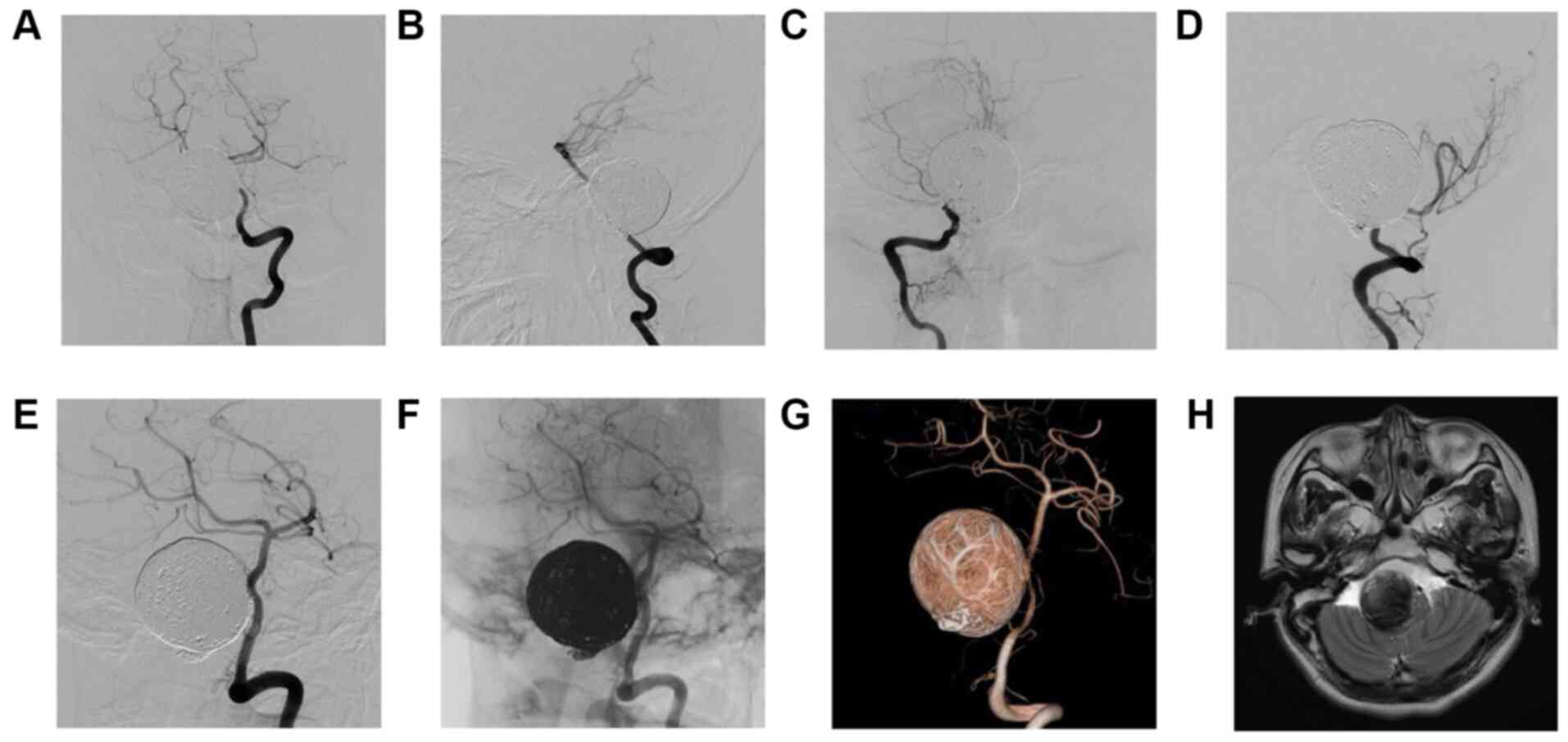
The patient underwent digital subtraction angiography (DSA) at
Xuanwu Hospital (Beijing, China) after 2 days of admission. A giant
spherical aneurysm of the bilateral vertebrobasilar junction (VBJ)
with a maximum diameter of 35 mm was identified during the surgery
(Fig. 2). The neck of the aneurysm
affected the bilateral vertebral arteries (VAs) and the basilar
artery (BA). The right VA was more severely affected, and the
bilateral posterior inferior cerebellar artery (PICA) remained at a
distance from the aneurysm neck. Furthermore, the development of
the posterior cerebral artery was not observed on right VA
arteriography until the capillary phase (Fig. 3A), and the contrast agent was
significantly delayed in the late venous phase (Fig. 3B); however, the development of the
posterior cerebral artery was observed on left VA arteriography
during the artery phase (Fig. 3C),
and the contrast agent was slightly delayed in the same late venous
phase (Fig. 3D).
Treatment strategy and course
Informed consent was provided by the patient and her
relatives prior to endovascular therapy. A treatment plan was
formulated after angiography. First, a microcatheter was placed
through the right VA and the Pipeline was completely released
through the left VA. Subsequently, the aneurysm was relatively
tightly embolized with coils and the right VA was occluded near the
aneurysm neck. Aspirin enteric-coated tablets (100 mg per day) and
clopidogrel (75 mg per day) were administered for 6 days prior to
treatment. At 9 days following hospitalization, the giant aneurysm
of the VBJ was embolized using a Pipeline Flex device (3.5x25 mm;
Medtronic) and coils. A total of 32 coils were used for
embolization, which included 10 Axium detachable 3D coils (25 mm x
50 cm, x4; 22 mm x 50 cm, x3; and 20 mm x 50 cm, x3; Medtronic), 11
HydroFrame coils (18 mm x 50 cm, x3; 16 mm x 44 cm, x2; 14 mm x 45
cm, x2; 13 mm x 47 cm, x2; and 12 mm x 43 cm, x2; MicroVention,
Inc.), 11 Axium detachable Helix coils (12 mm x 40 cm, x2; 10 mm x
30 cm, x4; 9 mm x 30 cm, x3; and 8 mm x 30 cm, x2; Medtronic). The
final intraoperative angiography revealed that the aneurysm body
did not develop and the contrast agent was slightly retained at the
aneurysm neck (Fig. 4). For 2 days
following the endovascular treatment, the patient was listless and
complained of a headache worse than those that had occurred during
the pre-embolization period. Physical examination revealed no new
positive signs. Postoperative fluid administration of 3,000 ml per
day was performed until day 3 after the embolization, and
subsequently, the patient was treated with a dexamethasone sodium
phosphate injection at 10 mg per day and injection of 125 ml 20%
mannitol every 8 h for a total of 7 days. After a further 2 days,
the patient gradually recovered to the preoperative mental state.
Re-examination of the head MRI and MRA on day 8 following
endovascular treatment revealed a small residual aneurysm neck
[Raymond-Roy classification, Class II (9)], and no new infarction in the posterior
circulation area (Fig. 5). The
patient was discharged on day 10 following embolization. The
patient was prescribed dual antiplatelet therapy postoperatively,
with clopidogrel (75 mg/day) administered for 3 months and aspirin
(100 mg/day) administered for 7 months from post-embolization day
1.
Follow-up
A 3-month telephone follow-up revealed that the
patient had increased white phlegm and drool and exhibited a slight
choking cough when drinking water. Furthermore, the patient's
left-limb muscle strength was slightly weakened compared with that
pre-embolization and the patient required help from other
individuals to walk. Three months after embolization,
re-examination of the head MRI and MRA revealed that the aneurysm
was completely occluded [Raymond-Roy classification, Class I
(9)]; however, the brainstem was
markedly compressed (Fig. 6),
similar to the situation encountered during the pre-embolization
stage. At 4 months after embolization, the levels of white phlegm
and drool gradually decreased and the muscle strength of the left
limb recovered. During the patient's second visit 7 months after
the embolization, the patient presented with slow speech, small
strides, no hoarseness in her voice, grade 1 in Kubota drinking
test (10), grade 5 left-limb
muscle strength, normal muscle tension and a negative bilateral
finger-to-nose test. Re-examination of DSA revealed no aneurysm
recurrence [Raymond-Roy classification, Class I (9)] and no stenosis in the parent artery
(Fig. 7). In April 2020 (2 years
after embolization), another video telephone follow-up was
performed (Videos S1 and S2), which revealed that certain
pre-embolization symptoms of the patient, including slow speech,
small strides, hoarseness and choking cough while drinking water,
were completely relieved. However, the patient still experienced
weakness in both lower limbs after walking >1,000 meters. To
date (2 years after the embolization), the modified Rankin scale
score (11) of the patient is 1
point. The major symptoms and outcomes prior to pre-embolization,
during the hospital stay and during the follow-up phase of the
patient are summarized in Table
I.
 | Table IMajor symptoms and outcomes for the
patient prior to EM and during the hospital stay and the follow-up
phase. |
Table I
Major symptoms and outcomes for the
patient prior to EM and during the hospital stay and the follow-up
phase.
| | | | Follow-up after
EM |
|---|
| Item | Pre-EM | In-hospital | 3 months | 4 months | 7 months | 2 years |
|---|
| Dizziness | Moderate | Moderate | Mild | Disappeared | Disappeared | Disappeared |
| Headache | Mild | Mild | Disappeared | Disappeared | Disappeared | Disappeared |
| Hoarseness | Moderate | Moderate | Mild | Mild | Mild | Disappeared |
| Drinking of water
(Kdt score) | 4 | 4 | 3 | 2 | 1 | 1 |
| Left-sided
walking | Mild | Mild | Moderate | Mild | Disappeared | Disappeared |
| Left limb MS (MRC
score) | 5- | 4 | 4- | 5- | 5 | 5 |
| mRS score | 2 | 2 | 4 | 2 | 1 | 1 |
Discussion
Flow diverter devices (FDDs) are increasingly used
in the treatment of intracranial aneurysm. A recent meta-analysis
by Ye et al (7) reported an
aneurysm occlusion rate of 78.8% after an average follow-up of 6.3
months, and neurological morbidity and mortality rates after FDD
treatment were 9.8 and 3.8%, respectively. The rupture rate of
giant, unruptured, posterior circulation aneurysms within 5 years
may be up to 50% (12). The
relevant factors to be considered when treating such complex
aneurysms include the shape, location, vascular architecture and
collateral circulation of the aneurysm's parent artery. Treatment
of these aneurysms has always posed a great challenge for
neurosurgery. Microsurgery and endovascular interventional therapy
are associated with a high incidence of neurological complications
(4,7,13).
Although the complication rate (the number of complications divided
by the number of patients) of complex posterior circulation
aneurysms treated with flow diversion devices is significantly
higher compared with that of anterior circulation aneurysms,
reconstruction of the parent artery with coil embolization is a
suitable alternative when surgical treatment fails.
To date, only a small number of studies have
reported on the treatment of giant aneurysm at the VBJ. Liang et
al (14) described the
endovascular treatment of 99 patients with large or giant aneurysms
of the posterior circulation, 12 of which were located at the VBJ;
3 of those 12 cases were treated by occluding the contralateral VA
with coils, and the bilateral VA was sacrificed in 1 of the 12
cases. However, in the latter case whose VA was sacrificed, the
patient died 3 days after discharge from unknown causes.
Furthermore, the prognosis of the 12 patients was not analyzed
according to subgroups. In the present case study, the aneurysm
neck simultaneously affected the bilateral VAs and the BA. The
bilateral PICAs remained at a distance from the aneurysm neck and
the development of the anterior spinal artery (ASA) was observed on
angiography of the right VA; the right VA was associated with the
development of ASA, which was near the aneurysm neck. In view of
the hemodynamic complexity of this aneurysm, it was crucial to
select a suitable type of treatment in order to reduce the
hemodynamic effect on the aneurysm. On the basis of using the
computational fluid dynamics method, Jing et al (15) discovered that adjunctive coiling
with the placement of a Tubridge flow diverter may significantly
reduce intra-aneurysmal flow velocity and wall shear stress,
promoting thrombosis formation and occlusion of aneurysms. Xiang
et al (16) suggested that
the results of aneurysm occlusion may be predicted with high
fidelity by calculating the intracavitary velocity, inflow rate and
shear force on the wall prior to and after implantation of the flow
device through computer simulation; however, factors associated
with the vascular anatomy must also be considered. Given the
hemodynamic particularity of the aneurysm in the present case, it
was possible to select the VA on the side that exerted the greater
influence on the hemodynamics of the aneurysm for occlusion, and
the Pipeline was able to be placed through the VA on the other
side. In the present case, the development of the posterior
cerebral artery was not observed on right VA arteriography until
the capillary phase and perfusion with the contrast agent was
significantly delayed in the late venous phase; however, the
development of the posterior cerebral artery was observed on left
VA arteriography during the artery phase and perfusion with the
contrast agent was slightly delayed in the same late venous phase.
Therefore, the hemodynamics of the right VA may have a greater
impact on aneurysms, although occluding the right VA may affect the
ASA. Fortunately, the contralateral blood vessels of the patient
were anastomosed with the right ASA. Therefore, it was possible to
place the embolization microcatheter into the aneurysm cavity
through the right VA and the Pipeline was subsequently completely
released through the left VA. Furthermore, the aneurysm was
relatively tightly embolized with coils and the right VA was
finally occluded near the aneurysm neck.
Previous studies have indicated that the combination
of coils and Pipeline for aneurysm treatment may increase the
embolization rate and reduce the risk of bleeding (17,18).
Dense packing of coils may result in a mass effect, whereas loose
packing may cause delayed rupture of the large aneurysm; therefore,
it is important to consider carefully the extent to which coils
should be packed. A single-center study (19) suggested that treatment with Pipeline
and coils resulted in a higher embolization rate compared with
Pipeline alone for aneurysms <10 mm. Peschillo et al
(20) also reported that, for large
and giant carotid aneurysms, treatment with flow-diverter stents in
combination with coils may provide a higher aneurysm occlusion rate
and reduce the requirement for retreatment compared with the use of
flow-diverter stents alone. However, to date, there is no objective
method for determining the appropriate degree of packing coils for
giant aneurysms. Autopsy and histopathological analysis performed
on a patient who died due to delayed rupture of aneurysm 34 days
after treatment with Pipeline and coils suggested that the most
relevant contributing factor in aneurysm rupture was the lack of
thrombus formation in the inflow area, and thrombus coverage in the
outflow area resulted in increased pressure of the aneurysm
(21). Therefore, it may be more
important to reduce the hemodynamic impact on aneurysms by
performing relatively dense embolization for rapid thrombolysis,
since the prognosis is poor following delayed rupture.
Insufficient aneurysm management occurred in the
present case when MRI on day 8 after embolization revealed that the
residual aneurysm neck and mass effect were difficult to treat.
Residual aneurysm neck in a giant aneurysm may increase the risk of
delayed rupture (21). In the
present case, a novel treatment strategy was implemented, which may
lead to improved outcomes through minimizing the flow to the
aneurysm by occlusion of the right VA according to hemodynamics and
the guidance of blood flow by the Pipeline to accelerate the
thrombolysis and endothelialization of the aneurysm neck (14), a procedure that may promote the
complete embolization of aneurysms. Upon analysis of the
hemodynamic influence on the aneurysm of the VBJ, the VA with the
larger shear force on the wall of the aneurysm was selected for
occlusion to simplify the treatment of the aneurysm and to maximize
the probability to achieve recovery, which may be more effective to
treat similar aneurysms.
Supplementary Material
Video follow-up of drinking water 2
years following the operation.
Video follow-up of walking 2 years
following the operation.
Supplementary Data
Supplementary Data
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and methods
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
CLZ and ZHS made substantial contributions to the
design of the study. YHW and PZ made substantial contributions to
the conception and design of the study, and they also contributed
in drafting the manuscript and revising it critically for important
intellectual content, as well as in the collection of data. CLZ
made substantial contributions to the conception of the study, as
well as the acquisition, analysis and interpretation of data. ZZY,
CLD and JMC were involved in the acquisition of data. CLZ and ZHS
contributed in drafting the manuscript and revising it critically
for important intellectual content. All authors read anad approved
the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Medical Ethics
Committee of the 904th Hospital of the People's Liberation Army
(Wuxi, China) and Xuanwu Hospital of Capital Medical University
(Beijing, China). Written informed consent was obtained from the
participant.
Patient consent for publication
The patient provided consent for publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Haemmerli J, Lenga P, Hong B, Kursumovic
A, Maldaner N, Burkhardt JK, Bijlenga P, Rüfenacht DA, Schmidt NO,
Vajkoczy P and Dengler J: Clinical implications and radiographic
characteristics of the relation between giant intracranial
aneurysms of the posterior circulation and the brainstem. Acta
Neurochir (Wien). 161:1747–1753. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Luzzi S, Gallieni M, Del Maestro M,
Trovarelli D, Ricci A and Galzio R: Giant and very large
intracranial aneurysms: Surgical strategies and special issues.
Acta Neurochir Suppl. 129:25–31. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chen J, Zhang C, Li P, Chen L and Wang Y:
High-flow extracranial-intracranial bypass for giant cavernous
carotid aneurysm. J Craniofac Surg. 29:1042–1046. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ota N, Matsukawa H, Noda K, Sato H, Hatano
Y, Hashimoto A, Miyazaki T, Kondo T, Kinoshita Y, Saito N, et al:
Evaluation of microsurgery for managing giant or complex cerebral
aneurysms: A retrospective study. World Neusurg. 115:e190–e199.
2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Griessenauer CJ, Ogilvy CS, Adeeb N,
Dmytriw AA, Foreman PM, Shallwani H, Limbucci N, Mangiaflco S,
Kumar A, Michelozzi C, et al: Pipeline embolization of posterior
circulation aneurysms: A multicenter study of 131 aneurysms. J
Neurosurg. 130:923–935. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Walcott BP, Stapleton CJ, Choudhri O and
Patel AB: Flow diversion for the treatment of intracranial
aneurysms. JAMA Neurol. 73:1002–1008. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ye G, Zhang M, Deng L, Chen X and Wang Y:
Meta-analysis of the efficiency and prognosis of intracranial
aneurysm treated with flow diverter devices. J Mol Neurosci.
59:158–167. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gregson JM, Leathley MJ, Moore AP, Smith
TL, Sharma AK and Watkins CL: Reliability of measurements of muscle
tone and muscle power in stroke patients. Age Ageing. 29:223–228.
2000.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Raymond J, Guilbert F, Weill A, Georganos
SA, Juravsky L, Lambert A, Lamoureux J, Chagnon M and Roy D:
Long-term angiographic recurrences after selective endovascular
treatment of aneurysms with detachable coils. Stroke. 34:1398–1403.
2003.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wu MC, Chang YC, Wang TG and Lin LC:
Evaluating swallowing dysfunction using a 100-ml water swallowing
test. Dysphagia. 19:43–47. 2004.PubMed/NCBI View Article : Google Scholar
|
|
11
|
van Swieten JC, Koudstaal PJ, Visser MC,
Schouten HJ and van Gijn J: Interobserver agreement for the
assessment of handicap in stroke patients. Stroke. 19:604–607.
1988.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wiebers DO, Whisnant JP, Huston J III,
Meissner I, Brown RD Jr, Piepgras DG, Forbes GS, Thielen K, Nichols
D, O'Fallon WM, et al: Unruptured intracranial aneurysms: Natural
history, clinical outcome, and risks of surgical and endovascular
treatment. Lancet. 362:103–110. 2003.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Graziano F, Ganau M, Iacopino DG and
Boccardi E: Vertebro-basilar junction aneurysms: A single centre
experience and meta-analysis of endovascular treatments.
Neuroradiol J. 27:732–741. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Liang F, Zhang Y, Yan P, Ma C, Liang S,
Jiang P and Jiang C: Predictors of periprocedural complications and
angiographic outcomes of endovascular therapy for large and giant
intracranial posterior circulation aneurysms. World Neurosurg.
125:e378–e384. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Jing L, Zhong J, Liu J, Yang X, Paliwal N,
Meng H, Wang S and Zhang Y: Hemodynamic effect of flow diverter and
coils in treatment of large and giant intracranial aneurysms. World
Neurosurg. 89:199–207. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Xiang J, Damiano RJ, Lin N, Snyder KV,
Siddiqui AH, Levy EI and Meng H: High-fidelity virtual stenting:
Modeling of flow diverter deployment for hemodynamic
characterization of complex intracranial aneurysms. J Neurosurg.
123:832–840. 2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lubicz B, Collignon L, Raphaeli G, Pruvo
JP, Bruneau M, De Witte O and Leclerc X: Flow-diverter stent for
the endovascular treatment of intracranial aneurysms: A prospective
study in 29 patients with 34 aneurysms. Stroke. 41:2247–2253.
2010.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Siddiqui AH, Kan P, Abla AA, Hopkins LN
and Levy EI: Complications after treatment with pipeline
embolization for giant distal intracranial aneurysms with or
without coil embolization. Neurosurgery. 71:E509–E513.
2012.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lin LM, Colby GP, Kim JE, Huang J, Tamargo
RJ and Coon AL: Immediate and follow-up results for 44 consecutive
cases of small (<10 mm) internal carotid artery aneurysms
treated with the pipeline embolization device. Surg Neurol Int.
4(114)2013.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Peschillo S, Caporlingua A, Resta MC,
Peluso JPP, Burdi N, Sourour N, Diana F, Guidetti G, Clarençon F,
Bloemsma GC, et al: Endovascular treatment of large and giant
carotid aneurysms with flow-diverter stents alone or in combination
with coils: A multicenter experience and long-term follow-up. Oper
Neurosurg (Hagerstown). 13:492–502. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ikeda H, Lshii A, Kikuchi T, Ando M,
Chihara H, Arai D, Hattori E and Miyamoto S: Delayed aneurysm
rupture due to residual blood flow at the inflow zone of the
intracranial paraclinoid internal carotid aneurysm treated with the
pipeline embolization device: Histopathological investigation.
Interv Neuroradiol. 21:674–683. 2015.PubMed/NCBI View Article : Google Scholar
|