Introduction
Proto-oncogene CD117 encodes a trans-membrane
tyrosine kinase receptor linked to the PDGF/CSF-1 receptor (c-fms)
subfamily, platelet-derived growth factor (1). The c-Kit receptor is involved in the
growth and development of mast cells and premature stromal cells or
Cajal interstitial cells (2).
Activation of Kit normally occurs when two adjacent receptors are
fused together by a homodimer ligand. Subsequently, a series of
events occur to activate cell signaling cascades, which are
important in regulating proliferation, apoptosis, adhesion and
differentiation in several cell types (3,4). It
plays an important role in the development of several cell types,
including hematopoietic cells, germ cells and melanocytes (4-6).
Regarding malignant melanoma (MM) tumorigenesis,
most tumors appear in the epidermis, in the melanocytes from the
dermo-epidermal junction, being in situ (entirely epidermal)
or invasive (extending from the epidermis into the dermis).
Occasionally, invasive MMs are, however, localized entirely
intradermally at the time of diagnosis. Invasive MM can be:
non-tumorigenic (in the ‘radial growth phase’) or tumorigenic (in
the ‘vertical growth phase’). MM in situ and invasive
non-tumorigenic MM can be divided into: Lentigo maligna,
superficial spreading melanoma, acral lentiginous and lentigo on
the mucosa.
Tumorigenic MM may appear on a pre-existing
non-tumorigenic component of any of the above types, in which case
it is appropriately named. However, tumorigenesis may also occur
‘de novo’, with no evidence of an in situ adjacent or
microinvasive component at the time of detection, in which case it
is called ‘nodular MM’ (7).
However, most of the lesions probably originate through an
intraepidermic nontumorigenic component that fails to develop or
persist while the tumorigenic component evolves.
Important categories of tumorigenic MMs include
desmoplastic MM and neurotropic MM. More rare types of MMs have
been described, such as minimal deviation MM/MM with minus
deviation, balloon cell MM, amelanotic MM, malignant blue nevus,
congenital melanocytic nevus, clear cell sarcoma, melanocytic
malignant schwannoma and approximately 5-10% of MM fall into
‘unclassified’ (NOS) or ‘other’ categories.
As a result, there are two major categories of MM,
which are sequential stages or ‘phases’ of stepping tumor
progression. In non-tumorigenic, radial or horizontal growth,
neoplastic melanocytes are limited to the epidermis (melanoma in
situ) or to the epidermis and papillary dermis, without the
formation of an expansive tumor mass (MM microinvasive). This phase
can be followed, after various time intervals, by the vertical
growth phase. Also, dermal and/or epidermal structures of an
associated nevus can be recognized in some MM.
Recent advances in molecular biology bring
additional information that solves many issues related to MM
tumorigenesis (8,9). It appears that melanocytic stem cells,
in addition to melanocytes, participate in the initiation and
progression of cutaneous MM (10-12).
Basically, most skin MMs start with slow on-site
growth and micro-invasive phase, and patients diagnosed at this
stage have a high rate of healing. Despite a tendency for early
clinical recognition of cutaneous MM, at the time of diagnosis,
most cutaneous MMs have already progressed to the next phase of
growth characterized by rapid growth. In patients diagnosed at this
stage, healing becomes uncertain and the prognosis depends on
certain attributes of the neoplasm and the host (stroma and
immunity). In general, the clinical progression of cutaneous MM is
partly correlated with the expansion of its germ cell (13). Thus, the proportion of cells
involved in the cell proliferation cycle will increase in cutaneous
MM (14,15). In the present study, we analyzed
CD117 (c-Kit), an immunohistochemical marker that evaluates both
tumor progression and prognosis and which may be a therapeutic
target in MM cases.
Patients and methods
Patients and tissue samples
The immunohistochemical study was performed on 55
cases (52% female and 48% male, aged between 23 and 81 years with a
mean age of 62.67) represented by a control group, which included 5
cases of simple nevi and 5 cases of nevi with dysplastic lesions,
as well as a study group consisting of 35 cases of MM primary and
10 metastases (one intestinal, 3 cutaneous - one satellite and two
distant as well as six in the lymph nodes). The study group
included 15 cases of superficial spreading melanoma (SSM), 10 cases
of nodular melanoma (NM), 3 lentigo maligna melanoma (LMM), 3 cases
of acral lentiginous melanoma (ALM) and 4 cases of amelanotic MM.
All biopsies were performed at The Clinical Emergency County
Hospital Craiova, between January 2012 and December 2016.
The study was approved by the Universitary and
Scientific Deontology and Ethics Committee of the University of
Medicine and Pharmacy of Craiova (no. 78 from 27.03.2015), and
informed consent was obtained from each patient.
Immunohistochemical methods
The immunohistochemical study method used to
identify the epitopes of interest was one-time, polymer-specific,
with high sensitivity, high specificity and high affinity. The
characteristics of the antibody and the external controls used are
shown in Table I.
 | Table IAntibody used: clone, dilution,
pretreatment, manufacturer and external control. |
Table I
Antibody used: clone, dilution,
pretreatment, manufacturer and external control.
| Antibody | Clone | Dilution | Pre-treatment | Manufacturer | External
control |
|---|
| CD117 | T595 | 1:50 | Solution citrate pH
6.0 x20 min in microwave | Leica
Microsystemsa | GIST |
From the paraffin blocks, 3-µm series sections were
made, which were inserted into the Leica BOND-MAX self-tester
(Leica Biosystems), and the machining was carried out automatically
according to the manufacturer's specifications. Note that the
sections were incubated with the primary antibody for 1 h and a
Bond Polymer Refine RED Detection System (Leica Biosystems) was
used to detect the primary antibody, visualization of RED
immunoreaction. Contrasting was performed in Mayer's hematoxylin
solution.
Positive external controls were used (Table I) and appropriate negative external
controls throughout the testing process. Negative external controls
were tissue samples from the analyzed cases, to which the primary
antibody was replaced with non-immune Ig serum from the same
species as the primary antibody used. Mast cells were used as an
internal positive control for CD117. Tumor cells showing
cytoplasmic and/or membrane immunoreactivity for CD117 (c-Kit) were
considered positive.
The percentage of positive cells was estimated for
CD117 immunoassay and cases were classified in one of the following
categories: 0 (negative cases, no positive cells), cases with under
10%, between 10-50% and over 50% positive cells. In addition, the
intensity of immunostaining was recorded semi-quantitatively: 0
(negative), +1 (weak), +2 (medium/moderate), +3 (strong).
Methods of statistical analysis
Average values and confidence intervals were used,
as well as comparative tests (Chi-square) for consignments made
using the SPSS 10 software (SPSS, Inc.). The Chi-square test was
used to interpret incidence tables; the data were appreciated from
the point of view of the dependence between the two classification
factors, retaining only the results >5%, considered a sufficient
materiality threshold. This test indicated whether there is a
relationship (mutual influence) between two factors. The commands
used in the software were Analyse, Descriptive Statistics and
CrossTabs. Continuous numeric data was grouped by categories and
plotted as standard ± standard deviations using the Microsoft Excel
package.
Statistical analysis was then performed using the
SPSS package (SPSS, Inc.). For two categories of comparisons, the
Student's-test comparison test was used. For more than two
categories to be compared, a one-way ANOVA test with post-hoc
analysis was used using the Tukey's test to evaluate the
differences between the pairs of categories.
The quantification of the statistical results was as
follows: i) P<0.05, the difference is significant (S); ii)
P<0.01, the difference is highly significant (HS); iii)
P<0.001, the difference is very highly significant (VHS); iv)
P>0.05, the difference is not significant (NS).
Ethical principles
In the course of the study, the ethical principles
underlying the Helsinki Declaration and the University Ethics Code
on the good conduct of the research, along with the codes of
practice established by the Code of Medical Deontology, were
respected.
Results
Of the total of 55 cases selected for the IHC study,
the majority, 76.36% of cases (42 cases) showed positive
immunostaining at CD117. The distribution of CD117 expression (as a
percentage of marker cells and immunostaining intensity) of the
melanocytic lesion studied is shown in Tables II and III.
 | Table IIDistribution of cases according to
the percentage of CD117-positive cells and the type of lesions. |
Table II
Distribution of cases according to
the percentage of CD117-positive cells and the type of lesions.
| | | IHC of CD117 (%
positive cells) |
|---|
| Type of lesions
(N=55) | No. of cases | 0 (negative) | <10% | 10-50% | >50% |
|---|
| Simple nevus | 5 | 5 | 0 | 0 | 0 |
| Dysplastic
nevus | 5 | 0 | 3 | 1 | 1 |
| LMM | 3 | 0 | 0 | 0 | 3 |
| SSM | 15 | 1 | 2 | 5 | 7 |
| NM | 10 | 3 | 4 | 2 | 1 |
| ALM | 3 | 0 | 0 | 1 | 2 |
| Amelanotic MM | 4 | 1 | 1 | 1 | 1 |
| Metastases | 10 | 3 | 2 | 4 | 1 |
 | Table IIIDistribution of the cases according
to percentage of CD117-positive cells and the immunostaining
intensity. |
Table III
Distribution of the cases according
to percentage of CD117-positive cells and the immunostaining
intensity.
| | IHC of CD117 (%
positive cells) |
|---|
| Intensity | 0 (negative) | <10% | 10-50% | Over 50% |
|---|
| 0 (13 cases) | 13 | 0 | 0 | 0 |
| +1 (16 cases) | 0 | 7 | 7 | 2 |
| +2 (16 cases) | 0 | 3 | 5 | 8 |
| +3 (10 cases) | 0 | 2 | 2 | 6 |
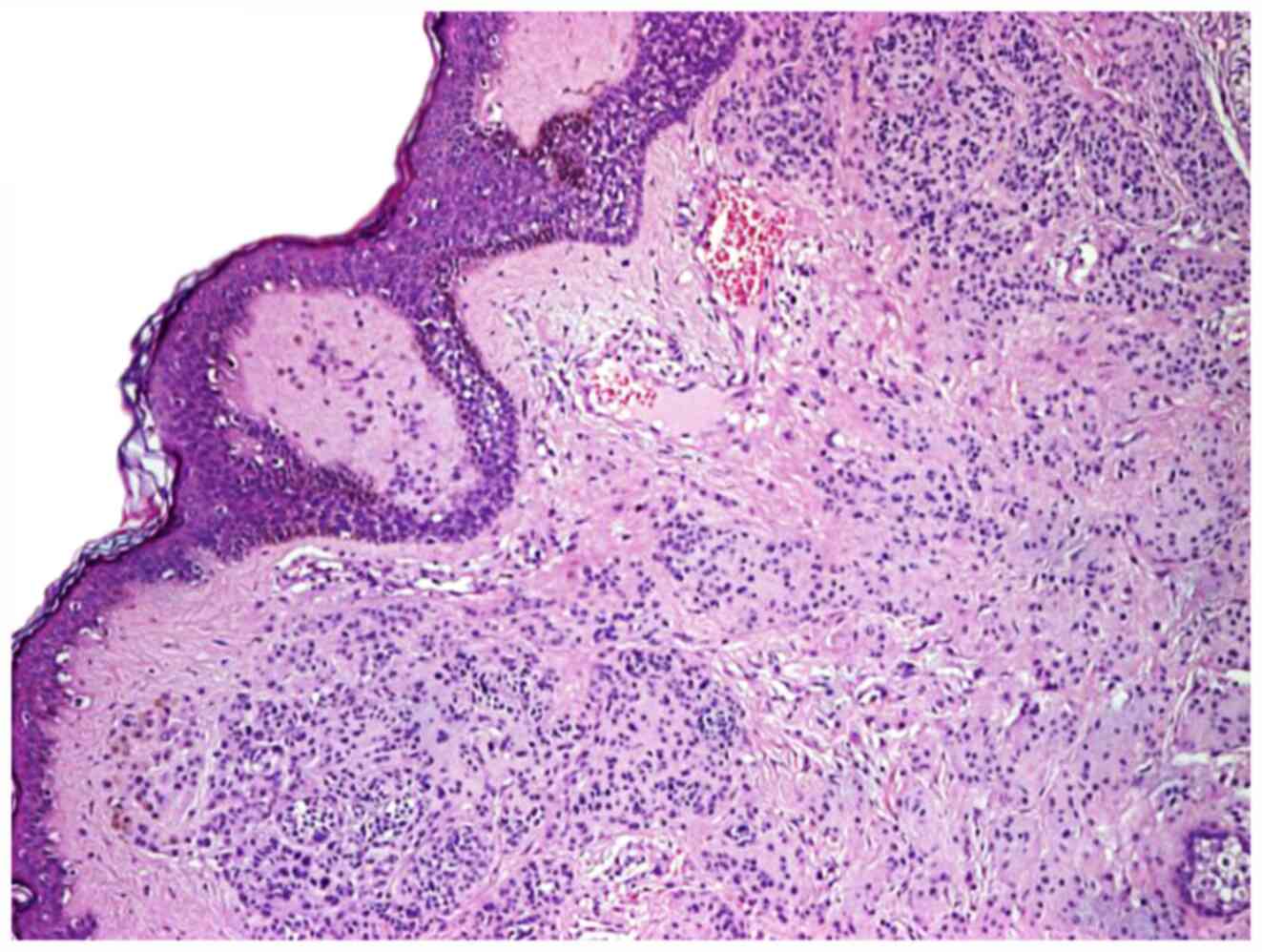
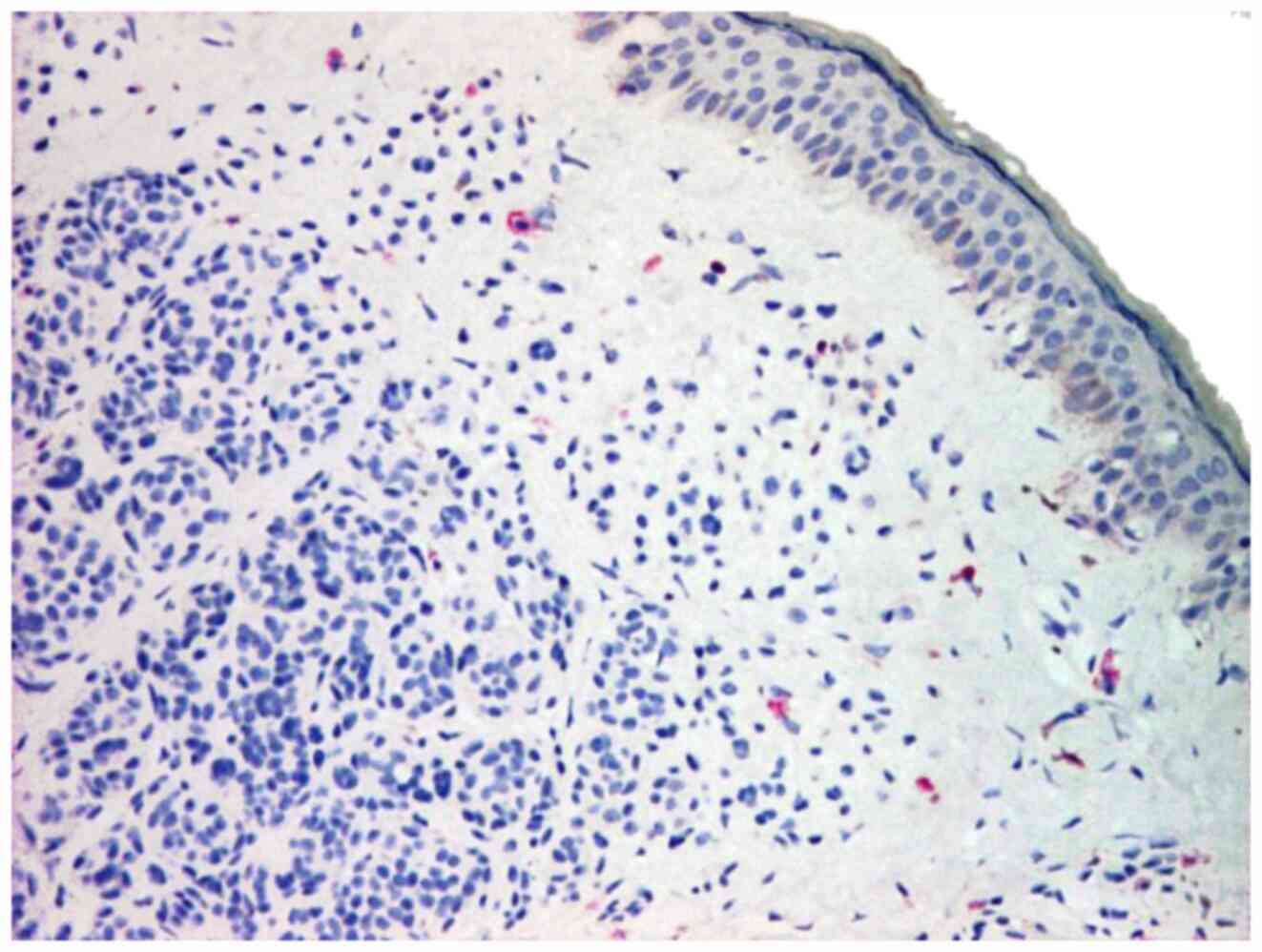
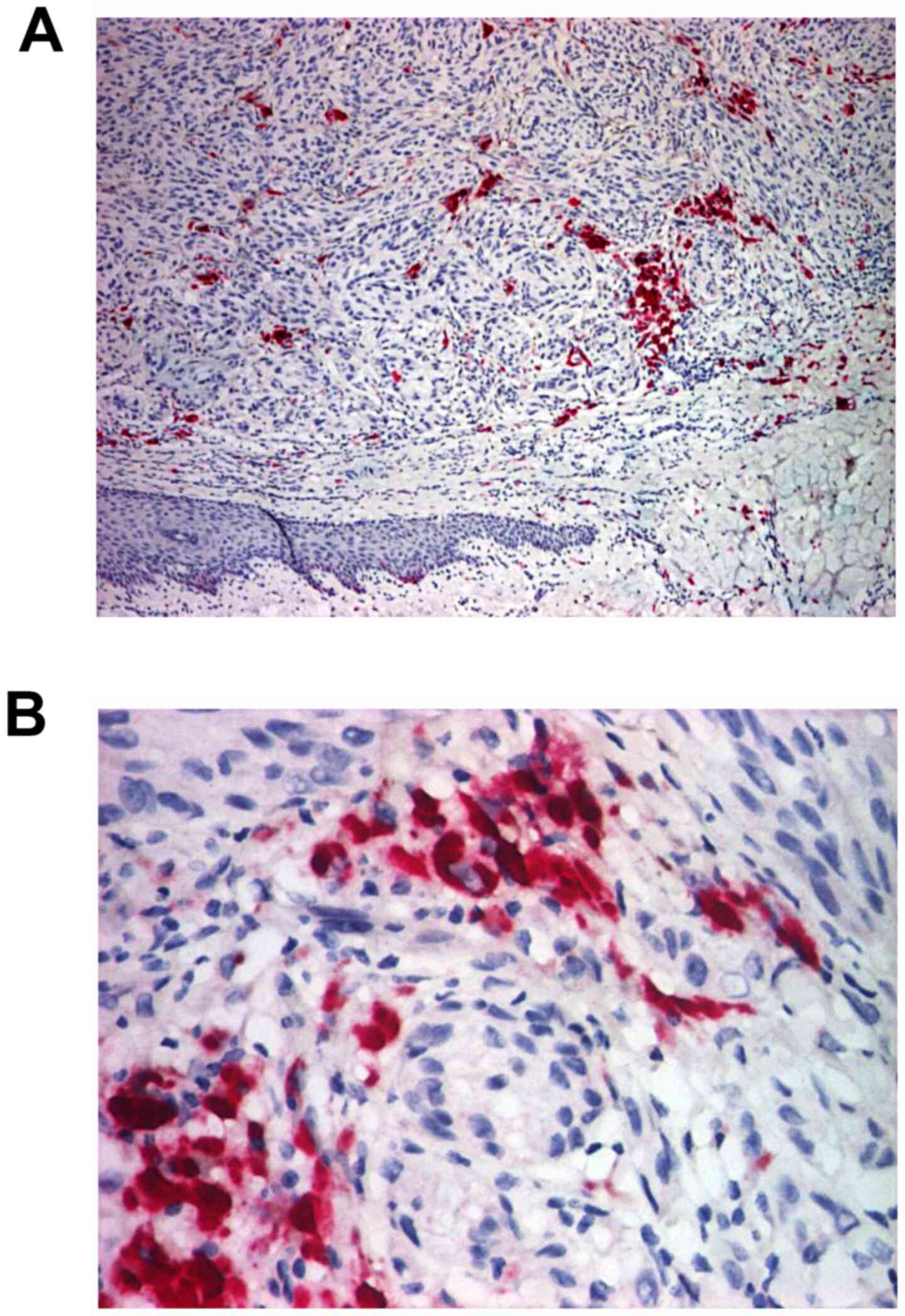
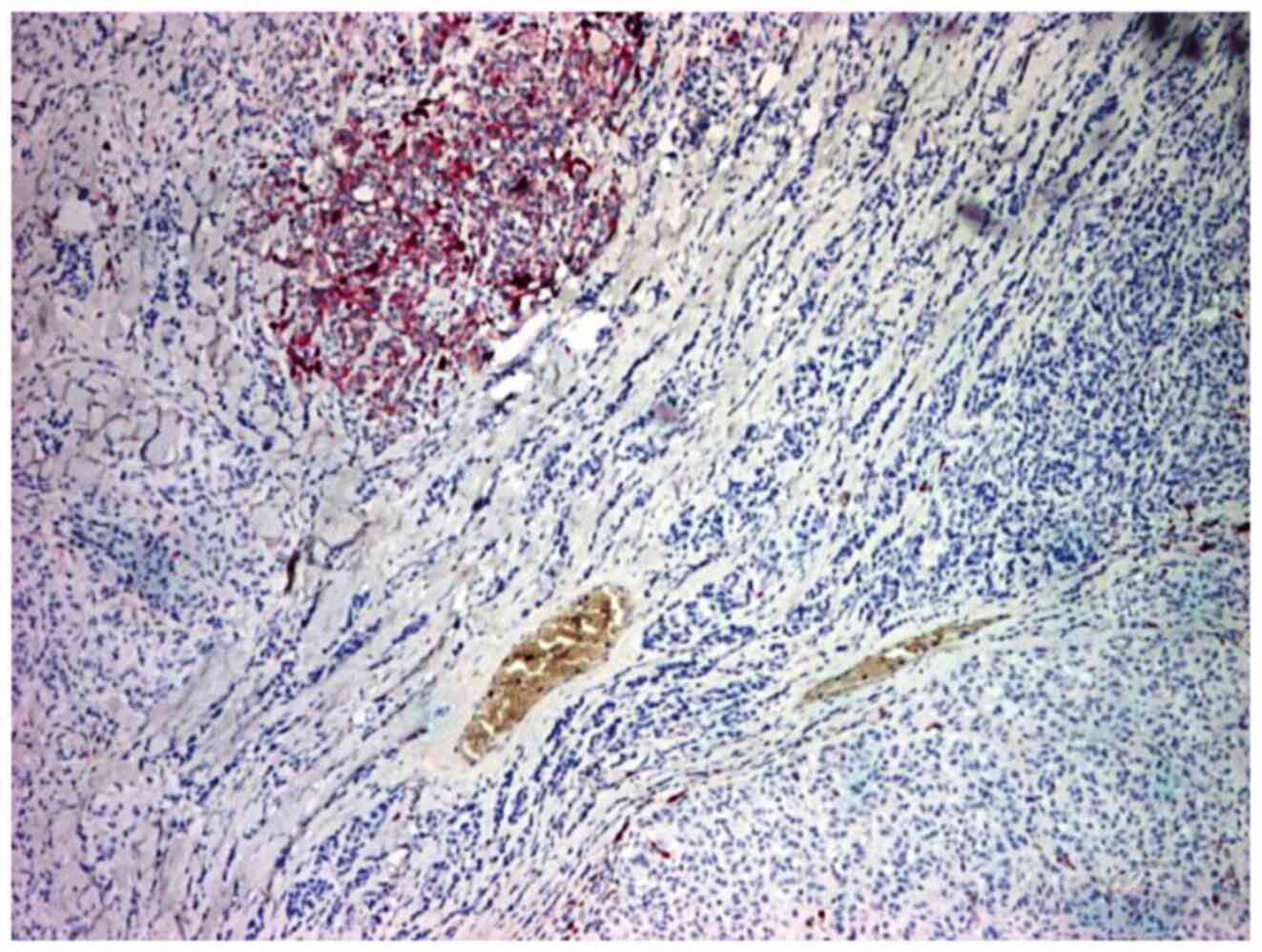
Thus, the vivid nevi did not show immunostaining at
CD117, all cases being negative for this marker (100% negative)
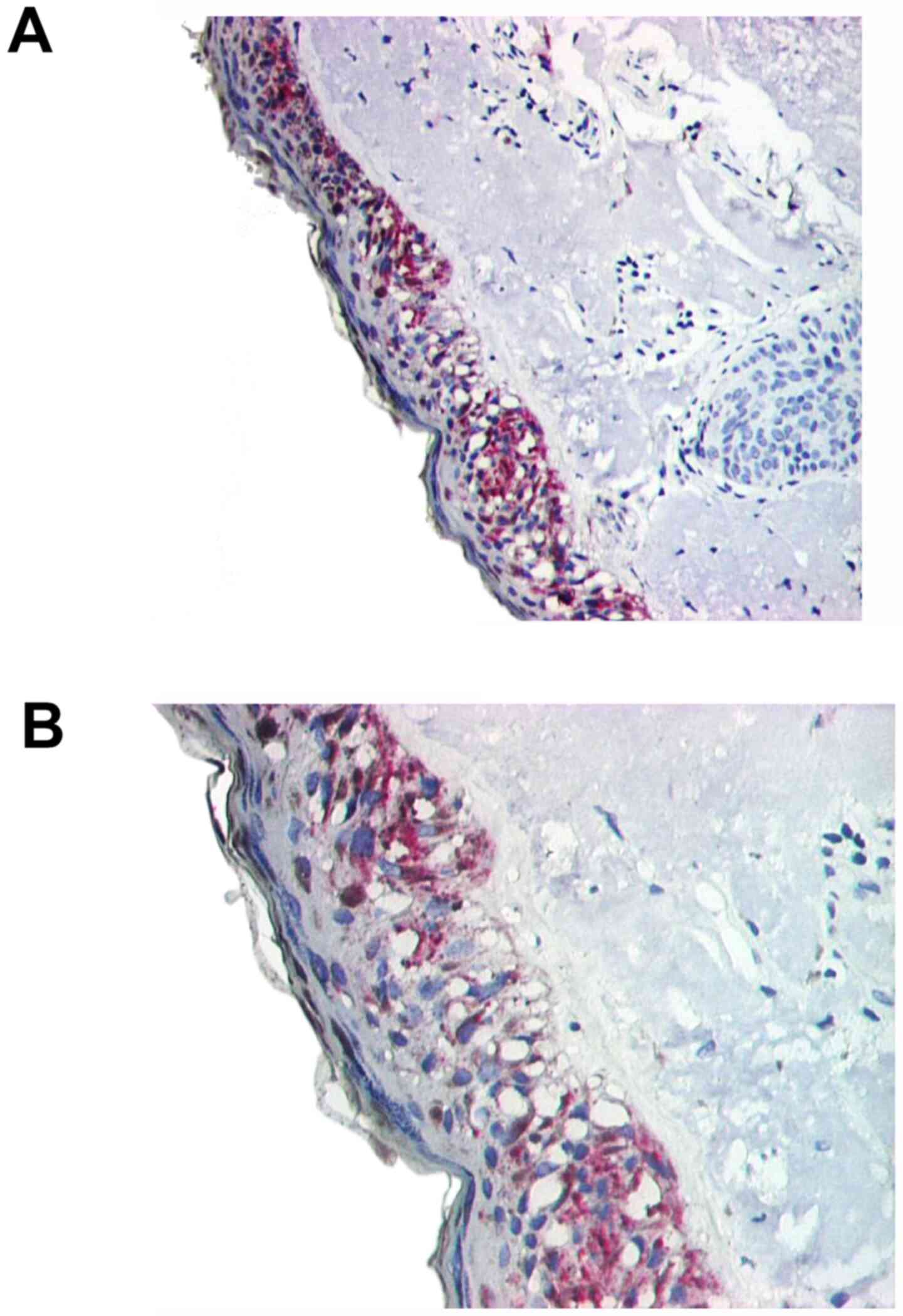
(Figs. 1 and 2), and the dysplastic nevi showed positive
immunostaining in the areas of dysplasia (which are located
superficially at the junction dermal-epidermal) in all cases (100%
positive) (Figs.
3-5). Dysplastic nevi (60%) exhibited under 10% of
CD117-positive cells, 20% of which were positive in 10-50% of tumor
cells and 20% in over 50% of tumor cells, +2 and +3 (Tables II and III).
LMM showed positive immunostaining in all three
cases (100% of positive cases), in over 50% of tumor cells in both
malignant lentigo and melanoma areas (Figs. 6 and 7). The immunomarker intensity was +2 and
+3 and was comparable in the lentigo and melanoma areas (Tables II and III).
SSM was negative in CD117 in one case (6.67%
negative), only 2 cases (13.33%) had immunostaining in below 10% of
tumor cells, 5 cases (33.33%) presenting 10-50% of the marked cells
and the remaining 7 cases (46.67%) were being positive in over 50%
of the tumor cells (Figs.
8-10). The immunomarker intensity was high, with scores of +2
and +3, one case having a +1 score (Tables II and III). A feature of the immunostaining on
CD117 in SSM was that, frequently, the intensity of immunostaining
decreased to the depth of the tumors compared to the
dermo-epidermal junction.
Regarding NM, we observed a relatively high number
of negative cases, 3 cases (30% negative), followed by 4 cases
(40%) with just under 10% positive cells, only 2 cases (20%)
positive between 10-50% of the tumor cells and only 1 case (10%)
was positive in over 50% of the tumor cells (Figs. 11 and 12). The immunomarker intensity was
generally mild and moderate, with scores of +1 and +2, with only
one case of high intensity +3, but in under 10% of tumor cells
(Tables II and III). One aspect noted in the CD117
marker in NM was that, in contrast to SSM, the immunostaining for
CD117 was sometimes more intense in the depth of the tumors, namely
in the tumor invasion front (in 40% of cases, the invasion front
was the only immunostaining of CD117, but in under 20% of total
tumor cells) (Fig. 12).
ALMs were positive in all three cases (100%
positive) with moderate and large (case 2 and 3, two cases); 1 case
showing between 10-50% of stained cells, and 2 cases showing over
50% of marked cells. It should be noted that 2 of the cases were
positive for CD117 only in the epidermal component, the dermal
component being negative. These two cases showed +3 immunostaining.
As a result, the CD117 marker in ALM in the epidermal component was
similar to SSM, and in the dermal component, it was similar to NM
(Tables II and III).
Four cases of amelanotic MMs were observed with one
case each of the categories analyzed in terms of the percentage of
stained cells. CD117 immunostaining intensity in positive cases was
low to moderate, with score 1 and 2, and positivity only at the
invasion front was observed in one case (Tables II and III).
It should also be noted that, in primary MMs with
in situ areas, these areas were strongly positive (intensity
3) to CD117; diffuse positivity was observed in almost all tumor
cells.
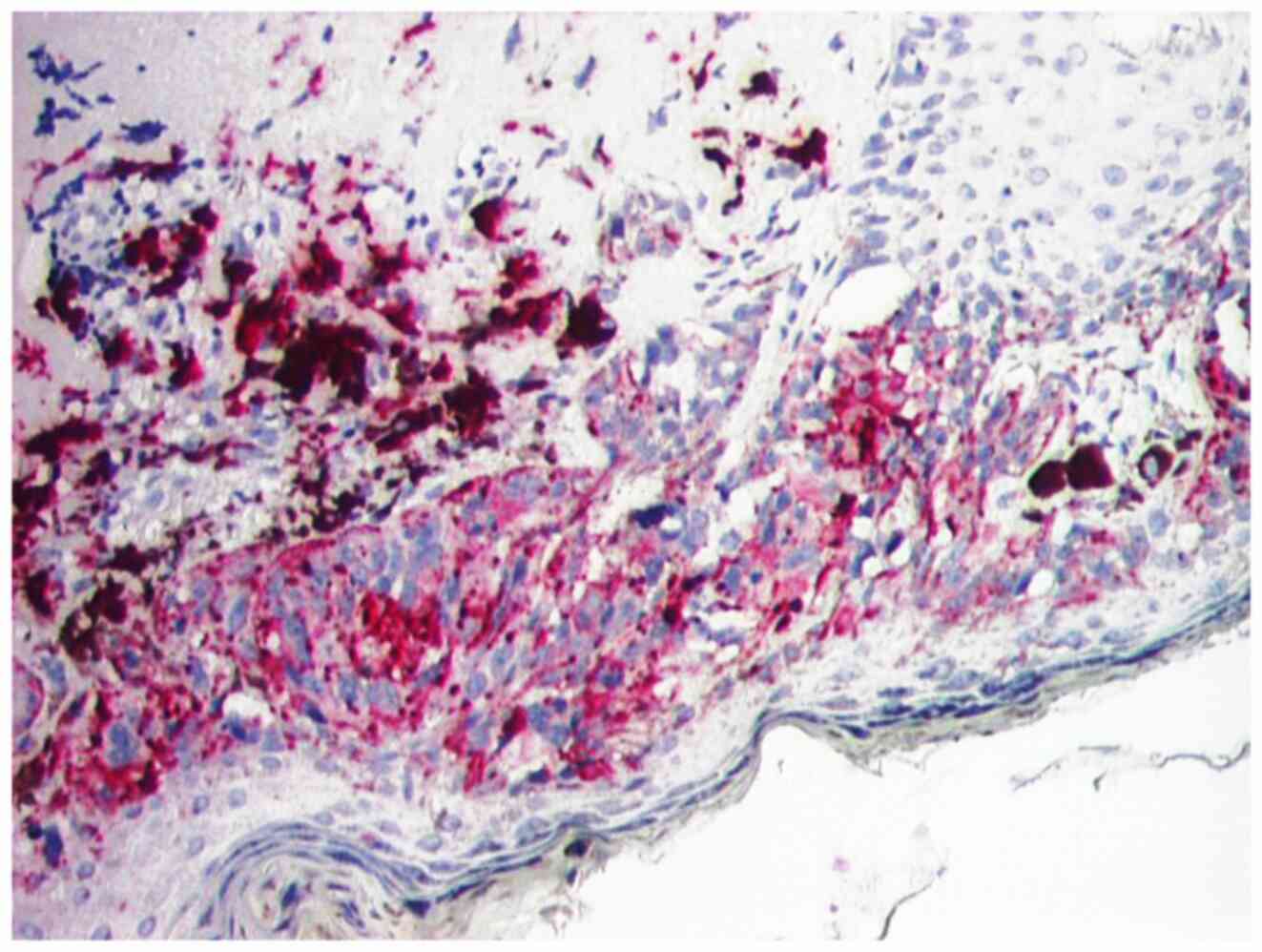
Metastatic MMs (metastases) were considered negative
to CD117 in 30% of cases, positive in 10% of tumor cells in 20% of
cases, between 10-50% of positive tumor cells in 40% of cases and
more than 50% of tumor cells in 10% of cases (Figs.
13-15). The immunomarker intensity in the metastases analyzed
was mild and moderate, with no intensive positive metastases
detected at CD117 (Tables II and
III).
Analyzing the CD117 immunomarker in MM and nevi
cases (simple nevi and dysplastic nevi), we found statistically
significant differences (P=0.01) in the percentage of positive
cells between the two categories; nevi were negative/stained in
under 10% of cells compared to MM, which generally expressed CD117
in over 10% of tumor cells. Thus, CD117 expression in MM was
significantly increased compared to simple or dysplastic nevi
(Table IV). Comparative analysis
between MM and the metastases did not reveal significant
differences (P=0.366), suggesting that MM metastases behave
similarly to their primary tumors in terms of CD117 expression
(Table IV).
 | Table IVDistribution of cases with <10%
and ≥10% of cells stained for CD117 by lesion type. |
Table IV
Distribution of cases with <10%
and ≥10% of cells stained for CD117 by lesion type.
| | IHC of CD117 (%
positive cells) |
|---|
| Lesion type (55
cases) | <10% | ≥10% | P-value |
|---|
| Nevi (10
cases) | 80 | 20 | 0.01 (S) |
| Melanomas (35
cases) | 34.28 | 65.72 | - |
| Metastases (10
cases) | 50 | 50 | 0.366 (NS) |
By comparing all the cases included in the study,
from the point of view of CD117 immunostaining, it was found that
poor/absent immunostaining was significantly more common in cases
expressing CD117 in a reduced cell number, under 10% of cells,
compared to moderate/strong immunostaining that was characteristic
of cases with <10% of positive cells (P=0.000217) (Table V).
 | Table VDistribution of cases with <10%
and ≥10% of cells stained for CD117 depending on the intensity of
the immunostaining. |
Table V
Distribution of cases with <10%
and ≥10% of cells stained for CD117 depending on the intensity of
the immunostaining.
| | | IHC of CD117 (%
positive cells) |
|---|
| Intensity | No. of cases | <10% | ≥10% | P-value |
|---|
| 0/+1 | 29 | 68.96 | 31.04 | 0.000217 (S) |
| +2/+3 | 26 | 19.23 | 80.77 | |
Discussion
The expression of c-Kit has been detected in a
variety of different tumor entities, such as gastrointestinal
stromal tumors (GISTs), malignant melanoma (MM), breast and lung
cancer, colon carcinoma, ovarian, hepatocellular, sarcoma and
mastocytosis (16-20).
Regarding CD117 immunoexpression in MM, Gibson and
Cooper showed that CD117 tends to immunostain strongly the in
situ component of MM, with loss of coloration in deep dermal
components and in NM (21).
This aspect was clearly observed in this study.
Thus, in all LMM cases, areas of lentigo malignant (in situ
lesions) were intensely and diffusely positive to CD117. In
addition, all other primary MM types (SSM, ALM, amelanotic)
associating MM domains in situ, were strongly positive (+3
intensity) for CD117, the positivity being diffused in nearly all
tumor cells of the in situ component.
Furthermore, a decrease in the percentage of marked
cells and the intensity of the immune marker in the deep dermal
component was noted when compared to the dermo-epidermal junction
in most of the analyzed MM types. NM cases lost color to CD177,
being negative or positive in just under 10% of cells, in most
cases (70% of cases). A particular aspect of NM was the presence of
the immunomarker CD117 only at the invasion front (in under 20% of
the tumor cells); this pattern of the marker was probably
correlated with the aggressive infiltrative progression of this
type of MM.
Moreover, the present study showed that all cases of
dysplastic nevi (100% of the positive cases) were scored for CD117
in the dysplasia areas, while the simple nevi were always negative
(100% of the negative cases) to c-Kit.
Consequently, these results suggest that CD117 is
involved in the MM tumorigenesis process, being heavily expressed
in its initial stages (dysplasia, in situ lesion), after
which the expression of CD117 decreases as the tumor progresses
during the growth phase vertical. This involvement of c-Kit in the
tumor transformation process was also supported by the significant
differences observed between CD117 expression in MM compared to
nevi (P=0.01).
It was also noted that the metastases expressed
CD117 comparable to their primary tumors, with no statistically
significant differences in the percentage of c-Kit-positive cells
in primary and metastatic MM (P=0.366). Thus, although the
intensity of the immunostaining in the metastases analyzed was mild
and moderate, with no intensive positive metastases detected at
CD117, MM metastases tended to retain c-Kit expression.
Consequently, the similar expression of CD117 in primary and
metastatic MM may suggest that loss of c-Kit expression by itself
does not have a direct role in the metastatic process in MM, and
other mechanisms are probably involved in this process (22).
This latter aspect was also demonstrated by other
clinical studies on MM cell lines, showing that loss of c-Kit
overexpression in MM cell lines is rather due to alteration in the
expression of transcription factors, such as activating enhancer
binding protein 2 (AP-2), which results in reduced expression of
c-Kit (23).
CD117, a growth factor for melanocyte migration and
proliferation, demonstrated in a previous study differentiated
immunostaining in various benign and malignant melanocytic lesions,
and the metastatic MM staining was lower than the primary MM dermal
staining (24).
By comparing all the cases included in the study,
from the point of view of CD117 immunoassay, it was found that
weak/absent immunostaining is significantly more frequent in cases
expressing CD117 in a reduced cell number, under 10% of cells,
compared to moderate/strong immunostaining, which is characteristic
of cases with over 10% of positive cells (P=0.000217). Similar
results have been reported by other authors (23), suggesting that in MM, when CD117 is
overexpressed, this overexpression is intense and diffuse, and can
be a good screening method for selecting patients who could benefit
from personalized therapy.
KIT changes in malignant tumors are of particular
interest as KIT is one of the therapeutic targets of tyrosine
kinase inhibitors (eg imatinib mesylate, sunitinib, nilotinib and
dasatinib). Imatinib mesylate is a selective inhibitor of certain
tyrosine kinases, including Abelson murine viral oncogene homolog
(ABL), breakpoint cluster region-Abelson (BCR-ABL), Abelson-related
genes (ARG), KIT and factor receptors platelet-derived growth
factor (PDGFR) (25).
Imatinib was initially found to be effective in the
treatment of chronic myeloid leukaemia, where it addresses the
BCR-ABL fusion protein and GIST treatment, where the tyrosine
kinase c-Kit is directed (26,27).
Also, other KIT-positive tumors can benefit from kinase inhibitor
therapy. It has been observed that the response rate can be
particularly high in KIT-expressing tumors and include KIT
activating mutations (28).
Similar findings in primary and metastatic MM
(29-31),
and studies that explored in vitro the sensitivity of
malignant melanocytic cells to this drug, led to the assertion that
imatinib mesylate is only effective in the context of KIT mutations
(32,33). KIT mutations have so far been found
particularly in mucosal ALM or MM, which do not have UV exposure as
a risk factor (34). MM inhibitors
of KIT, imatinib and sunitinib and, more recently, nilotinib and
dasatinib, have been included in MM treatment but were found to be
less effective than in GIST (35,36).
Favorable results were shown for patients with metastatic MM,
especially metastatic ocular MM (37,38);
the reports showed complete remission, lasting up to 1 year
(39,40).
MM with oncogenic mutations in KIT have been
reported in several studies that focused on the role of KIT in
melanocyte transformation (19,34,41).
Some cases of rare metastatic MM having KIT L576P activating
mutation and strong and diffuse KIT expression (42) suggest that MM progression involves
KIT activation and not loss of activity. It has been taken into
consideration the use of tyrosine kinase inhibitors in these cases,
which showed significant results in some studies (43,44).
In a study of Medinger et al, a large series
of solid tumors was immunohistochemically analyzed for c-Kit
expression. The rate of c-Kit expression in solid tumors was low
compared to GIST. However, relatively high c-Kit expression in
sarcomas, MM, renal cell carcinoma, seminoma, and neuroendocrine
carcinoma is interesting and deserves further research (45).
Furthermore, we should be aware that the level of
growth factor receptor expression does not always predict kinase
inhibitor activity in the complex context of intracellular
signaling pathways. Screening tumor samples for expression of
growth factor-specific receptors is, however, very relevant as it
provides valuable information on tumor characteristics, helping us
better understand complex interactions of signal transduction
pathways and guiding us in the development of more specific
therapies (45).
CD117 immunoexpression in MM, significantly
different from nevi (P=0.001), and the increased percentage of
immune-positive MM (65.71%) suggest that tyrosine kinase inhibitors
may be useful in the treatment of cutaneous MM. Similar results
have been reported by Alessandrini et al in a recent study
in patients with conjunctival MM (46).
The role of KIT signaling in melanocyte biology has
been extensively studied. It has been shown that the interaction of
the stem cell factor with the KIT receptor is important for the
survival, proliferation, differentiation and migration of
melanocytes (47).
However, regulation of the KIT pathway is complex
and depends on many other cellular factors (48). While KIT activating mutations are
known to be associated with a variety of malignant human tumors,
such as GIST, seminomas and mastocytosis/mastocytosis leukaemia
(49), the introduction of a KIT
activating mutation into an immortalized murine melanocytic cell
line has been reported to have a more motogenic effect than a
mitogenic one. Therefore, it was speculated that in order to obtain
proliferative advantage and escape epidermal barriers, MM cells
should lose KIT expression (50-52).
This hypothesis was supported by previous
observations and those of a present study, in which KIT expression
in MM is strong in in situ lesions and the junctional
component of invasive lesions, but is lost once MM becomes invasive
and metastatic (23,53).
Recent information on the functional importance of
multiple mutant genes (BRAF, N-RAS, KIT and PTEN) in MM has
fundamentally changed the diagnostic and therapeutic approach.
However, it is not surprising that, in a large number of MM cases,
such single mutations do not clearly delineate the biological
behavior of the tumor at the time of diagnosing a primary MM. In
fact, it seems to be a multitude of biologically distinct MM
entities (54).
Thus, this direct approach is likely to be
insufficient given that in many MM, unknown oncogenes and/or tumor
suppressors can control the fate of tumor cells (55). Most likely, MM approaches, using the
21st-century technology of the genetic profile, will yield
interesting results (56).
However, there are some limitations of our study. We
cannot provide an explanation for the different immunoexpression of
CD117 in different types of melanoma, although some forms have
similar expression levels of CD117 to melanoma metastasis, which is
intriguing and requires further research.
CD117 (c-Kit) is massively involved in the process
of tumorigenesis of cutaneous malignancies, being
immunohistochemically undetectable in benign neural lesions, but
densely expressed in dysplastic lesions (dysplastic nevi) and in
situ melanoma areas.
In invasive cutaneous MM, CD117 expression tends to
decrease as neoplasia progresses and procedes into the tumorigenic,
vertical growth phase, being lower in the profound dermal component
of tumors and in nodular melanomas.
To eliminate the epidermal barriers and gain a
proliferative advantage to allow the transition to the vertical
growth phase, it seems that MM should lose the expression of
c-Kit.
Malignant melanoma cutaneous metastases express
CD117 at a level comparable to their primary tumors, suggesting
that other mechanisms interfere directly with the metastasis
process and not loss of c-Kit expression by itself.
CD117 overexpression in cutaneous melanocytic
lesions (≥10% of tumor cells) correlates significantly with
increased immunostaining intensity (+2/+3), suggesting that the
immunohistochemical evaluation of CD117 may be a good method for
screening patients, who could benefit from a personalized therapy
with tyrosine kinase inhibitors.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AR, CB, MAM and DEB contributed to the study design,
participated in the entire review process and prepared the
manuscript. IŢ, LEB, FDP, GS and DCB contributed to collecting the
relevant literature, data analysis and critical interpretation. GS
and DCB conceived the review and modified the manuscript. All
authors read and approved the final version of the manuscript.
Ethics approval and consent to
participate
The study was approved by the Universitary and
Scientific Deontology and Ethics Committee of the University of
Medicine and Pharmacy of Craiova (no. 78 from 27.03.2015), and
informed consent was obtained from each patient. We complied,
throughout the research, with the ethical standards of the
Declaration of Helsinki, along with the university codes of Good
Research Practice and Medical Ethics.
Patient consent for publication
The patients provided written informed consent for
the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Besmer P, Murphy JE, George PC, Qiu FH,
Bergold PJ, Lederman L, Snyder HW Jr, Brodeur D, Zuckerman EE and
Hardy WD: A new acute transforming feline retrovirus and
relationship of its oncogene v-kit with the protein kinase gene
family. Nature. 320:415–421. 1986.PubMed/NCBI View
Article : Google Scholar
|
|
2
|
Yarden Y, Kuang WJ, Yang-Feng T, Coussens
L, Munemitsu S, Dull TJ, Chen E, Schlessinger J, Francke U and
Ullrich A: Human proto-oncogene c-kit: A new cell surface receptor
tyrosine kinase for an unidentified ligand. EMBO J. 6:3341–3351.
1987.PubMed/NCBI
|
|
3
|
Ashman LK: The biology of stem cell factor
and its receptor C-kit. Int J Biochem Cell Biol. 31:1037–1051.
1999.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ronnstrand L: Signal transduction via the
stem cell factor/c-Kit. Cell Mol Life Sci. 61:2535–2548.
2004.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Arber DA, Tamayo R and Weiss LM: Paraffin
section detection of the c-kit gene product (CD117) in human
tissues: Value in the diagnosis of mast cell disorders. Hum Pathol.
29:498–504. 1998.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Maranduca MA, Branisteanu D, Serban DN,
Branisteanu DC, Stoleriu G, Manolache N and Serban IL: Synthesis
and physiological implications of melanic pigments. Oncol Lett.
17:4183–4187. 2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Blendea A, Georgescu CV, Tolea I,
Brănişteanu DE and Costache A: An unusual cutaneous malignant
melanoma arised de novo: A case report. Rom J Morphol Embryol.
56:1217–1221. 2015.PubMed/NCBI
|
|
8
|
Schatton T, Murphy GF, Frank NY, Yamaura
K, Waaga-Gasser AM, Gasser M, Zhan Q, Jordan S, Duncan LM,
Weishaupt C, et al: Identification of cells initiating human
melanomas. Nature. 451:345–349. 2008.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Reginster MA, Pierard-Franchimont C,
Piérard GE and Quatresooz P: Molecular dermatopathology in
malignant melanoma. Dermatol Res Pract. 2012(684032)2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Klein WM, Wu BP, Zhao S, Wu H,
Klein-Szanto AJ and Tahan SR: Increased expression of stem cell
markers in malignant melanoma. Mod Pathol. 20:102–107.
2007.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Schatton T and Frank MH: Cancer stem cells
and human malignant melanoma. Pigment Cell Melanoma Res. 21:39–55.
2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Rappa G, Fodstad O and Lorico A: The stem
cell-associated antigen CD133 (Prominin-1) is a molecular
therapeutic target for metastatic melanoma. Stem Cells.
26:3008–3017. 2008.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Zurac S, Neagu M, Constantin C, Cioplea M,
Nedelcu R, Bastian A, Popp C, Nichita L, Andrei R, Tebeica T, et
al: Variations in the expression of TIMP1, TIMP2 and TIMP3 in
cutaneous melanoma with regression and their possible function as
prognostic predictors. Oncol Lett. 11:3354–3360. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Quatresooz P, Pierard GE and
Pierard-Franchimont C: Mosan Study Group of Pigmented Tumors:
Molecular pathways supporting the proliferation staging of
malignant melanoma (Review). Int J Mol Med. 24:295–301.
2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Quatresooz P and Piérard GE: Malignant
melanoma: From cell kinetics to micrometastases. Am J Clin
Dermatol. 12:77–86. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Tsuura Y, Hiraki H, Watanabe K, Igarashi
S, Shimamura K, Fukuda T, Suzuki T and Seito T: Preferential
localization of c-kit product in tissue mast cells, basal cells of
skin, epithelial cells of breast, small cell lung carcinoma and
seminoma/dysgerminoma in human: Immunohistochemical study on
formalin-fixed, paraffin-embedded tissues. Virchows Arch.
424:135–141. 1994.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Matsuda R, Takahashi T, Nakamura S, Sekido
Y, Nishida K, Seto M, Seito T, Sugiura T, Ariyoshi Y, Takahashi T,
et al: Expression of the c-kit protein in human solid tumors and in
corresponding fetal and adult normal tissues. Am J Pathol.
142:339–346. 1993.PubMed/NCBI
|
|
18
|
Hornick JL and Fletcher CD:
Immunohistochemical staining for KIT (CD117) in soft tissue
sarcomas is very limited in distribution. Am J Clin Pathol.
117:188–193. 2002.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Went PT, Dirnhofer S, Bundi M, Mirlacher
M, Schraml P, Mangialaio S, Dimitrijevic S, Kononen J, Lugli A,
Simon R and Sauter G: Prevalence of KIT expression in human tumors.
J Clin Oncol. 22:4514–4522. 2004.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Becker G, Schmitt-Graeff A, Ertelt V, Blum
HE and Allgaier HP: CD117 (c-kit) expression in human
hepatocellular carcinoma. Clin Oncol (R Coll Radiol). 19:204–208.
2007.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Gibson PC and Cooper K: CD117 (KIT): A
diverse protein with selective applications in surgical pathology.
Adv Anat Pathol. 9:65–69. 2002.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Fekete GL, Cotoi OS and Fekete JE:
Multiple nodular cutaneous metastases as the first clinical sign of
signet ring cell gastric carcinoma: Case report. Acta
Dermatovenerol Croat. 20:34–37. 2012.PubMed/NCBI
|
|
23
|
Torres-Cabala CA, Wang WL, Trent J, Yang
D, Chen S, Galbincea J, Kim KB, Woodman S, Davies M, Plaza JA, et
al: Correlation between KIT expression and KIT mutation in
melanoma: A study of 173 cases with emphasis on the
acral-lentiginous/mucosal type. Mod Pathol. 22:1446–1456.
2009.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Isabel Zhu Y and Fitzpatrick JE:
Expression of c-kit (CD117) in Spitz nevus and malignant melanoma.
J Cutan Pathol. 33:33–37. 2006.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Heinrich MC, Griffith DJ, Druker BJ, Wait
CL, Ott KA and Zigler AJ: Inhibition of c-kit receptor tyrosine
kinase activity by STI 571, a selective tyrosine kinase inhibitor.
Blood. 96:925–932. 2000.PubMed/NCBI
|
|
26
|
Hochhaus A, Druker B, Sawyers C, Guilhot
F, Schiffer CA, Cortes J, Niederwieser DW, Gambacorti-Passerini C,
Stone RM, Goldman J, et al: Favorable long-term follow-up results
over 6 years for response, survival, and safety with imatinib
mesylate therapy in chronic-phase chronic myeloid leukemia after
failure of interferon-alpha treatment. Blood. 111:1039–1043.
2008.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Demetri GD, von Mehren M, Blanke CD, Van
den Abbeele AD, Eisenberg B, Roberts PJ, Heinrich MC, Tuveson DA,
Singer S, Janicek M, et al: Efficacy and safety of imatinib
mesylate in advanced gastrointestinal stromal tumors. N Engl J Med.
347:472–480. 2002.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Heinrich MC, Corless CL, Demetri GD,
Blanke CD, von Mehren M, Joensuu H, McGreevey LS, Chen CJ, Van den
Abbeele AD, Druker BJ, et al: Kinase mutations and imatinib
response in patients with metastatic gastrointestinal stromal
tumors. J Clin Oncol. 21:4342–4349. 2003.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Alexis JB, Martinez AE and Lutzky J: An
immunohistochemical evaluation of c-kit (CD-117) expression in
malignant melanoma, and results of imatinib mesylate (Gleevec)
therapy in three patients. Melanoma Res. 15:283–285.
2005.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Wyman K, Atkins MB, Prieto V, Eton O,
McDermott DF, Hubbard F, Byrnes C, Sanders K and Sosman JA:
Multicenter Phase II trial of high-dose imatinib mesylate in
metastatic melanoma: Significant toxicity with no clinical
efficacy. Cancer. 106:2005–2011. 2006.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Ugurel S, Hildenbrand R, Zimpfer A, La
Rosée P, Paschka P, Sucker A, Keikavoussi P, Becker JC, Rittgen W,
Hochhaus A and Schadendorf D: Lack of clinical efficacy of imatinib
in metastatic melanoma. Br J Cancer. 92:1398–1405. 2005.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Antonescu CR, Busam KJ, Francone TD, Wong
GC, Guo T, Agaram NP, Besmer P, Jungbluth A, Gimbel M, Chen CT, et
al: L576P KIT mutation in anal melanomas correlates with KIT
protein expression and is sensitive to specific kinase inhibition.
Int J Cancer. 121:257–264. 2007.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Jiang X, Zhou J, Yuen NK, Corless CL,
Heinrich MC, Fletcher JA, Demetri GD, Widlund HR, Fisher DE and
Hodi FS: Imatinib targeting of KIT-mutant oncoprotein in melanoma.
Clin Cancer Res. 14:7726–7732. 2008.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Curtin JA, Busam K, Pinkel D and Bastian
BC: Somatic activation of KIT in distinct subtypes of melanoma. J
Clin Oncol. 24:4340–4346. 2006.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Guo J, Si L, Kong Y, Flaherty KT, Xu X,
Zhu Y, Corless CL, Li L, Li H, Sheng X, et al: Phase II,
open-label, single-arm trial of imatinib mesylate in patients with
metastatic melanoma harboring c-kit mutation or amplification. J
Clin Oncol. 29:2904–2909. 2011.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Carvajal RD, Antonescu CR, Wolchok JD,
Chapman PB, Roman RA, Teitcher J, Panageas KS, Busam KJ,
Chmielowski B, Lutzky J, et al: KIT as a therapeutic target in
metastatic melanoma. JAMA. 305:2327–2334. 2011.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Guerriere-Kovach PM, Hunt EL, Patterson
JW, Glembocki DJ, English JC III and Wick MR: Primary melanoma of
the skin and cutaneous melanomatous metastases: Comparative
histologic features and immunophenotypes. Am J Clin Pathol.
122:70–77. 2004.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Grange JD, Duquesne N, Roubeyrol F,
Branisteanu D, Sandon K, Fleury J, Gerard JP, Chauvel P, Pinzaru G,
Jean-Louis B and Bievelez B: Double irradiation for macroscopic
radioresistance or recurrence of melanomas of the posterior uvea:
Clinical, ballistic, therapeutic and prognostic aspects. Series of
19 cases among 462 patients. J Fr Ophtalmol. 22:1054–1063.
1999.PubMed/NCBI
|
|
39
|
Kim KB, Eton O, Davis DW, Frazier ML,
McConkey DJ, Diwan AH, Papadopoulos NE, Bedikian AY, Camacho LH,
Ross MI, et al: Phase II trial of imatinib mesylate in patients
with metastatic melanoma. Br J Cancer. 99:734–740. 2008.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Ancuceanu R, Dinu M, Neaga I, Laszlo FG
and Boda D: Development of QSAR machine learning-based models to
forecast the effect of substances on malignant melanoma cells.
Oncol Lett. 17:4188–4196. 2019.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Willmore-Payne C, Layfield LJ and Holden
JA: c-Kit mutation analysis for diagnosis of gastrointestinal
stromal tumors in fine needle aspiration specimens. Cancer.
105:165–170. 2005.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Willmore-Payne C, Holden JA, Tripp S and
Layfield LJ: Human malignant melanoma: Detection of BRAF- and
c-kit-activating mutations by high-resolution amplicon melting
analysis. Hum Pathol. 36:486–493. 2005.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Fiorentini G, Rossi S, Lanzanova G,
Bernardeschi P, Dentico P and De Giorgi U: Potential use of
imatinib mesylate in ocular melanoma and liposarcoma expressing
immunohistochemical c-Kit (CD117). Ann Oncol.
14(805)2003.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Lutzky J, Bauer J and Bastian BC:
Dose-dependent, complete response to imatinib of a metastatic
mucosal melanoma with a K642E KIT mutation. Pigment Cell Melanoma
Res. 21:492–493. 2008.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Medinger M, Kleinschmidt M, Mross K,
Wehmeyer B, Unger C, Schaefer HE, Weber R and Azemar M: c-Kit
(CD117) expression in human tumors and its prognostic value: An
immunohistochemical analysis. Pathol Oncol Res. 16:295–301.
2010.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Alessandrini L, Parrozzani R, Bertorelle
R, Valentini E, Candiotto C, Giacomelli L, Midena E and Blandamura
S: C-Kit SCF receptor (CD117) expression and KIT gene mutation in
conjunctival pigmented lesions. Acta Ophthalmol. 91:e641–e645.
2013.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Grichnik JM, Burch JA, Burchette J and
Shea CR: The SCF/KIT pathway plays a critical role in the control
of normal human melanocyte homeostasis. J Invest Dermatol.
111:233–238. 1998.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Grichnik JM: Kit and melanocyte migration.
J Invest Dermatol. 126:945–947. 2006.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Holden JA, Willmore-Payne C and Layfield
LJ: Tyrosine kinase activating mutations in human malignancies:
Implications for diagnostic pathology. Exp Mol Pathol. 85:68–75.
2008.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Alexeev V and Yoon K: Distinctive role of
the cKit receptor tyrosine kinase signaling in mammalian
melanocytes. J Invest Dermatol. 126:1102–1110. 2006.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Ciobotaru OR, Lupu MN, Rebegea L,
Ciobotaru OC, Duca OM, Tatu AL, Voinescu CD, Stoleriu G, Earar K
and Miulescu M: Dexamethasone-chemical structure and mechanisms of
action in prophylaxis of postoperative side effects. Rev Chim
(Bucharest). 70:843–847. 2019.
|
|
52
|
Caruntu C, Boda D, Constantin C, Caruntu A
and Neagu M: Catecholamines increase in vitro proliferation of
murine B16F10 melanoma cells. Acta Endocrinol. 10:545–558.
2014.
|
|
53
|
Buga AM, Docea AO, Albu C, Malin RD,
Branisteanu DE, Ianosi G, Ianosi SL, Iordache A and Calina D:
Molecular and cellular stratagem of brain metastases associated
with melanoma. Oncol Lett. 17:4170–4175. 2019.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Avram S, Coricovac DE, Pavel IZ, Pinzaru
J, Ghiulai R, Baderca F, Soica C, Muntean D, Branisteanu DE,
Spandidos DA, et al: Standardization of A375 human melanoma models
on chicken embryo chorioallantoic membrane and Balb/c nude mice.
Oncol Rep. 38:89–99. 2017.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Kaplan FM, Mastrangelo MJ and Aplin AE:
The wrath of RAFs: Rogue behavior of B-RAF kinase inhibitors. J
Invest Dermatol. 130:2669–2671. 2010.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Wagle N, Emery C, Berger MF, Davis MJ,
Sawyer A, Pochanard P, Kehoe SM, Johannessen CM, Macconaill LE,
Hahn WC, et al: Dissecting therapeutic resistance to RAF inhibition
in melanoma by tumor genomic profiling. J Clin Oncol. 29:3085–3096.
2011.PubMed/NCBI View Article : Google Scholar
|