Introduction
Despite the advances in fetal monitoring during
labor, one of the most critical causes of neonatal death and
neurologic injuries remains intrapartum asphyxia (IA) (1-4).
During labor and birth, IA leads to hypoxia and fetal acidosis.
Thus, a reliable method for detecting acidosis can be a useful tool
for predicting adverse neonatal outcome due to IA (2,5-7).
Acidosis can be evaluated and it is defined as low
umbilical cord pH or high umbilical base deficit (expressed as
negative base excess, BE) at birth (7-9).
Hypoxia due to impaired blood supply to the fetus leads in the
early stages to respiratory acidosis that is characterized by a
decrease in pH but normal BE. Following these initial events, if
hypoxia continues there will be a shift to anaerobic metabolism,
resulting in the formation of lactic acid and increase in BE
(6,8,9). Thus,
high cord blood lactate levels can be correlated with fetal
acidosis and asphyxia (10,11).
Some studies suggest that neonatal complications are
associated with metabolic acidosis, rather than respiratory
acidosis, thus a distinction between the two is important for
predicting those neonate at risk for morbidity and mortality
(6,12). Because lactate is a direct end
product of anaerobic metabolism it can be used to differentiate
between metabolic and respiratory acidosis. Furthermore, some
studies suggest that the measurement of umbilical cord blood
lactate is more accurate than pH measurements in predicting
neonatal outcome (10,13). Since labor and birth can be
complicated by a wide variety of events such as retroplacental
hematoma, prematurity, and dystocia, it is important to be able to
objectively confirm or infirm intrapartum hypoxia (12-14).
Perinatal hypoxia is difficult to predict and avoid,
as it can be the result of fetal malformations, prematurity, labor
dystocia or unexpected events such as retroplacental hematoma
(14,15). In addition, in some cases even less
severe pathologies such as thrombophilia can be an important risk
factor for perinatal hypoxic events (16-18).
Thus, an objective mean of assessing fetal hypoxia is important for
confirming or excluding intrapartum asphyxia and predicting
neonatal long term morbidity and mortality (19,20).
We conducted a retrospective, multicenter study to
evaluate umbilical cord blood pH and lactate as a mean of
evaluating the degree of intrapartum hypoxia and also to establish
which of the two is more reliable in predicting morbidity in term
neonates. This study continues and extends the research previously
carried out by Mogos et al at a single center (7).
Patients and methods
Newborns
Our study included newborns born between 2010 and
2012 in three hospitals in Romania: INSMC ‘Alessandrescu Rusescu’,
Bucur Maternity Hospital and Craiova Emergency Hospital. The
information was gathered from the archived patient medical records
and included gestation age, fetal heart rate monitoring during
labor, birth weight, Apgar score, umbilical blood gases (pH and
lactate) and neonatal outcome. The data collected retrospectively
did not contain personal information and only the agreements of the
ethics committee of the participant hospitals were required and
obtained without the need of informed consent or the consent of the
patient/legal representative in the case of minors.
We included in the intrapartum asphyxia group (IA)
all newborns from term singleton births with markers of a severe
hypoxic event during labor defined as the presence of at least one
of the following: Severe changes in fetal heart rate (<100,
>160), meconium staining and in the presence of at least one of
the following: Low Apgar score (≤3 in the first minute or ≤5 after
5 min); respiratory failure (defined/characterized as absence of
spontaneous breathing after more than 5 min or mechanical
ventilation for more than 10 min); the need for intensive care unit
admission for more than 24 h.
The exclusion criteria for the IA group were:
Encephalopathy determined by causes other than IA, congenital
malformations, congenital metabolic diseases, viral infection,
septic shock, major organ failure, or fetal trauma during
birth.
A control group of 150 healthy newborns from term
singleton births, that did not meet any of the above criteria (IA
or exclusion), and that had information regarding umbilical cord
gases, was randomly selected from the newborn that were registered
between 2010 and 2012.
Term pregnancy was defined as a gestational age of
37 weeks or greater and only singleton pregnancies were
selected.
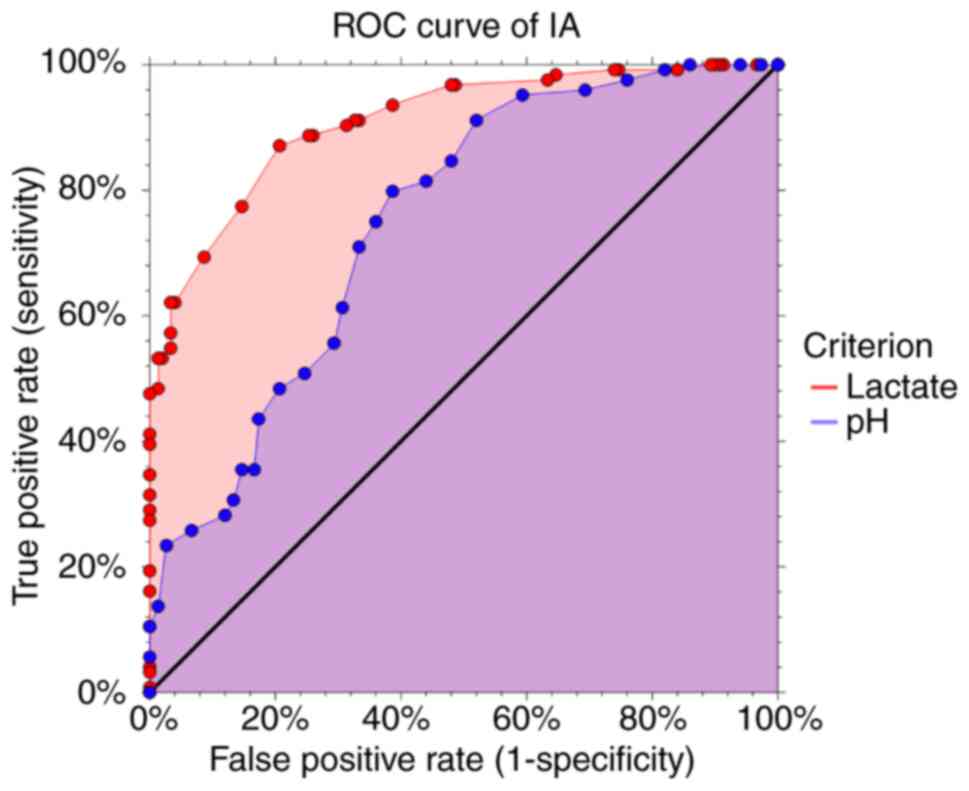
Receiver operating characteristics (ROC) curves were
constructed to evaluate the predictive value of pH and lactate for
fetal asphyxia and neonatal death. To objectively compare the
predictive characteristic of pH and lactate we used the maximal
Youden index to determine the ‘optimal’ cutoff value for each
variable. The Youden index takes into account sensitivity and
specificity and it is used to estimate the diagnostic effectiveness
of different cutoff values (19).
Statistical analysis
The data were collected using Office-Excel version
14.7.7 and for the statistical analysis NCSS 2019 Statistical
Software (2019) (NCSS, LLC.; ncss.com/software/ncss) was used. The characteristics
for each group were calculated using ‘Descriptive statistics’. The
variables were compared using two sample t-test. The results were
analyzed and interpreted according to the obtained P-value;
P<0.05 was considered to be statistically significant.
Results and discussion
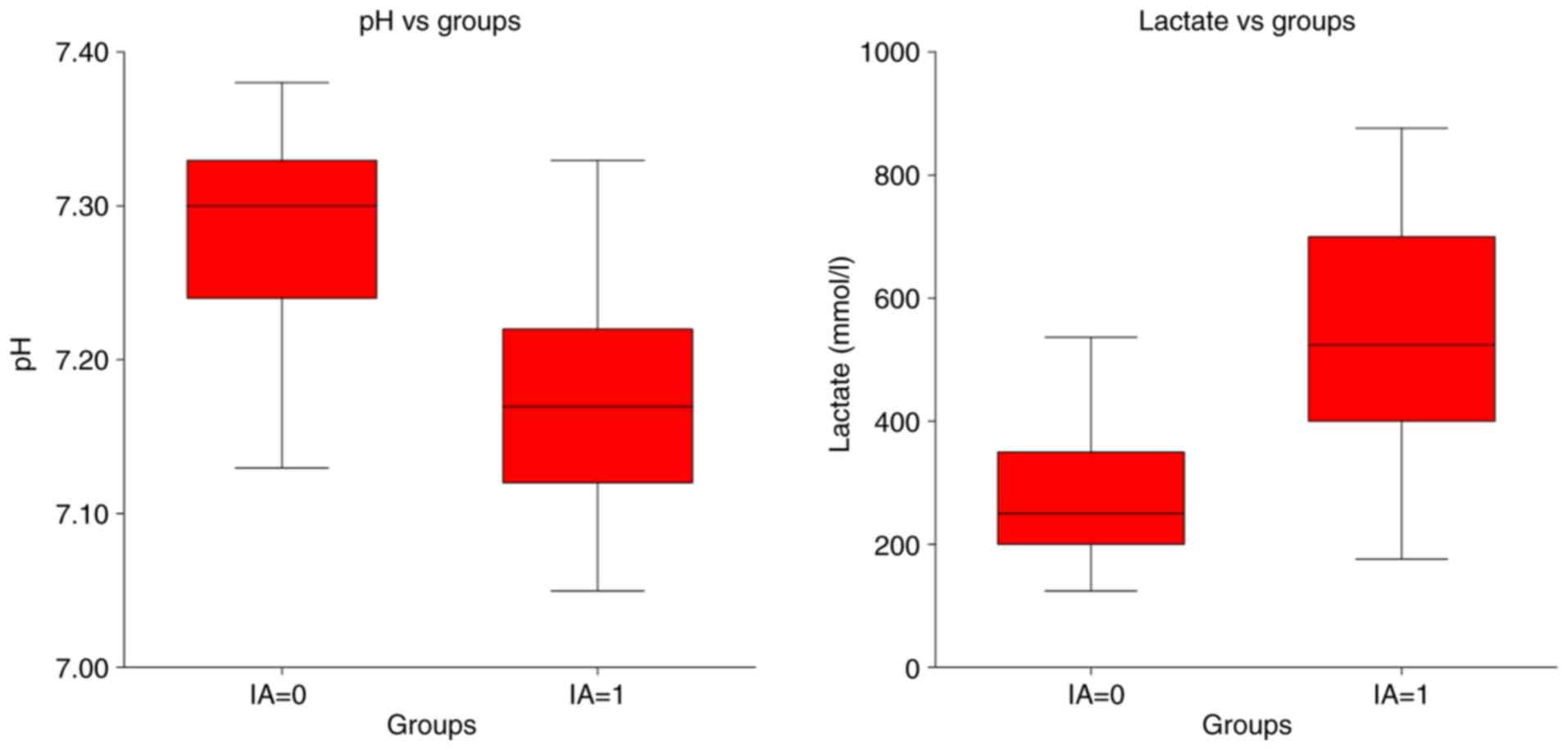
During the period 2010-2012 there were 21,224
births; a total of 124 cases met our criteria for IA. The umbilical
cord pH was significantly lower (P<0.001) in the IA group, with
a mean of 7.17 with values ranging between 7.05 and 7.32, compared
to a mean of 7.28 for the Control group (Table I, Fig.
1). In addition, the lactate values were significantly higher
(P<0.001) for the IA group, with a mean of 5.34 mmol/l and
values ranging between 2.35 and 8.75 mmol/l, compared to a mean of
2.78 mmol/l for the Control group (Table I, Fig.
1).
 | Table IpH and lactate values in the IA and
control groups. |
Table I
pH and lactate values in the IA and
control groups.
| Variable | IA group (n=124) | Control group
(n=150) |
|---|
| pH | 7.17±0.07
(7.05-7.32) | 7.28±0.06
(7.13-7.38) |
| Lactate (mmol/l) | 5.34±1.5
(2.35-8.75) | 2.78±0.7
(1.25-4.35) |
The ROC curves for lactate and pH for evaluating IA
are shown in Fig. 2. The pH had a
ROC curve area of 0.75, while the lactate had a ROC curve area of
0.92; thus, lactate was significantly more accurate in predicting
IA. Judging by the maxim Youden index, the optimal cutoff value was
7.24 for pH with an index of 0.62 and 3.75 mmol/l for lactate with
an index of 0.70 (Table II). Both
sensitivity and specificity were higher for lactate compared to pH
(87.1 and 83.2% compared to 86.3 and 74.0%).
 | Table IISensitivity and specificity of the
different cutoff values for pH and lactate for evaluating IA. |
Table II
Sensitivity and specificity of the
different cutoff values for pH and lactate for evaluating IA.
| Variable | Sensitivity (95%
CI) | Specificity (95%
CI) |
|---|
| pH | | |
|
≤7.12 (10th
percentile) | 31.4%
(23.4-40.4) | 99.9% (97.5-100) |
|
≤7.17 (mean
IA value) | 50.8%
(41.6-59.8) | 93.3%
(88.1-96.7) |
|
≤7.24
(‘optimal cutoff’ from the ROC curve) | 86.3%
(78.9-91.8) | 74.0%
(66.2-80.8) |
| Lactate (mmol/l) | | |
|
≥7.00 (90th
percentile) | 27.4%
(19.7-36.1) | 99.9% (97.5-100) |
|
≥5.35 (mean
IA value) | 48.4%
(39.3-57.5) | 98.6%
(95.2-99.8) |
|
≥3.75
‘optimal cutoff’ from the ROC curve | 87.1%
(79.8-92.4) | 83.2%
(76.3-87.5) |
Umbilical cord gases represent one of the most
objective ways to evaluate newborn metabolic status and rule out
perinatal asphyxia (21,22). In our study, the results confirm
that increased umbilical cord blood lactate is an accurate
predictor of neonatal morbidity due to intrapartum asphyxia. By
comparing the ROC curve areas, lactate proved to be superior to pH
in predicting poor neonatal outcome. In addition, although there
are numerous proposals for cutoff values of pH and lactate to be
used for confirming IA and predicting a poor outcome (23,24),
the greatest sensitivity and specificity were achieved in our study
by using a cutoff value of 7.24 for pH and 3.75 mmol/l for lactate
(Table II).
There are two possible explanations for which
lactate appears to be superior in predicting neonatal morbidity and
mortality. First of all, lactate is a direct product of anaerobic
metabolism; thus, it is produced earlier during hypoxia. Therefore,
changes in its value occur and can be detected more rapidly than
low pH (25,26). Secondly, high umbilical cord blood
lactate is a specific marker of metabolic acidosis which is
associated with more neonatal complications than respiratory
acidosis (6,12).
As with premature births, we are still far from
being able to predict and avoid intrapartum asphyxia, despite the
efforts made over the last decades (27). As technology progresses, probably
more and more sensors and intelligent textiles will be developed,
that will be able to detect fetal hypoxia and distress before
severe lesions occur. Yet, until that time, evaluating cord blood
gases remains one of the most reliable ways of detecting but also
excluding fetal hypoxia (20,28,29).
Moreover, in today's era of defensive medicine and prenatal
diagnostics, it is important to rule out IA as a contributing cause
for the poor neurological outcome of neonates diagnosed prenatally
with complex malformations such as holoprosencephaly, Galen vein
aneurism or other brain anomalies (30-35).
In 2014, the American College of Obstetricians and
Gynecologists compiled a summary of all specified signs present in
the neonatal period and all the factors that suggest or lead to a
diagnosis as early as possible of an acute perinatal
hypoxic-ischemic event (36). The
first neonatal sign is an Apgar score below 5 at 5 and 10 min,
which then is followed by fetal acidemia in the umbilical artery
with a pH <7.0 or the presence of base deficit ≥12 mmol/l,
separately or together. Furthermore, the impact of IA can be
observed by imaging trough magnetic resonance imaging or
spectroscopy where acute brain injuries can be noted (37,38).
The next sign of certainty is the presence of hypoxic-ischemic
encephalopathy and multisystem organ failure. Early detection of
these signs may limit the progression to irreversible consequences
(39).
One limitation of our study was that it included
only term neonates thus the results may not be valid for preterm
births. Moreover, only short-term outcome was taken into
consideration. Thus, future studies may be needed to assess the
predictive ability of pH and lactate for long-term outcomes and in
cases of premature birth.
In conclusion, both umbilical cord lactate and pH
can be used as accurate predictors of neonatal morbidity caused by
intrapartum hypoxia, as it has been showed in numerous studies. Our
study confirmed that lactate is superior to pH in predicting
adverse neonatal outcome. The greatest sensitivity and specificity
in predicting IA were achieved in our study by using a cutoff value
of 3.75 mmol/l for lactate and 7.24 for pH. For these cutoff
values, the sensitivity and specificity for lactate were 87.1 and
83.2%, while for pH they were 86.3 and 74.0%.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AN, REB and CGH collected, analyzed and interpreted
the patient data. SV, MCTD and LP collected the data and had
substantial contribution to the conception of the research and
statistical analysis. ADB, LN and NB substantially contributed to
the conception of the study, the interpretation of the data and the
writing of the manuscript. LIC and RGI contributed to the
literature retrieval and manuscript modification. AN, REB and FF
supervised and designed the present study and contributed to the
approval of the final version of the manuscript. All authors read
and approved the final version of the manuscript.
Ethics approval and consent to
participate
The data collected retrospectively did not contain
personal information and only the agreement of the ethics committee
of INSMC ‘Alessandrescu Rusescu’ Bucharest, Bucur Maternity
Hospital Bucharest and Craiova Emergency Hospital were required and
obtained without the need of informed consent or the consent of the
patient/legal representative in the case of minors.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Freeman JM and Nelson KB: Intrapartum
asphyxia and cerebral palsy. Pediatrics. 82:240–249.
1988.PubMed/NCBI
|
|
2
|
Omo-Aghoja L: Maternal and fetal acid-base
chemistry: A major determinant of perinatal outcome. Ann Med Health
Sci Res. 4:8–17. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Schifrin BS and Ater S: Fetal hypoxic and
ischemic injuries. Curr Opin Obstet Gynecol. 18:112–122.
2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ahearne CE, Boylan GB and Murray DM: Short
and long term prognosis in perinatal asphyxia: An update. World J
Clin Pediatr. 5:67–74. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Graham EM, Ruis KA, Hartman AL,
Northington FJ and Fox HE: A systematic review of the role of
intrapartum hypoxia-ischemia in the causation of neonatal
encephalopathy. Am J Obstet Gynecol. 199:587–595. 2008.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ross MG and Gala R: Use of umbilical
artery base excess: Algorithm for the timing of hypoxic injury. Am
J Obstet Gynecol. 187:1–9. 2002.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Mogos M, Herghelegiu CG, Ioan RG, Cringu
AI and Neacsu A: Determining an umbilical cord pH cutoff value for
predicting neonatal morbidity related to intrapartum hypoxia. Rev
Chim. 70:605–607. 2019.
|
|
8
|
Fahey J and King TL: Intrauterine
asphyxia: Clinical implications for providers of intrapartum care.
J Midwifery Womens Health. 50:498–506. 2005.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Victory R, Penava D, da Silva O, Natale R
and Richardson B: Umbilical cord pH and base excess values in
relation to adverse outcome events for infants delivering at term.
Am J Obstet Gynecol. 191:2021–2028. 2004.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Gjerris AC, Stær-Jensen J, Jørgensen JS,
Bergholt T and Nickelsen C: Umbilical cord blood lactate: A
valuable tool in the assessment of fetal metabolic acidosis. Eur J
Obstet Gynecol Reprod Biol. 139:16–20. 2008.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Bohîlțea RE, Zugravu CA, Neacsu A, Navolan
D, Berceanu C, Nemescu D, Bodean O, Turcan N, Baros Al and Cîrstoiu
MM: The prevalence of vitamin D deficiency and its obstetrical
effects. A prospective study on Romanian patients. Rev Chim.
70:1228–1233. 2019.
|
|
12
|
Goldaber KG, Gilstrap LC III, Leveno KJ,
Dax JS and McIntire DD: Pathologic fetal acidemia. Obstet Gynecol.
78:1103–1107. 1991.PubMed/NCBI
|
|
13
|
Tuuli MG, Stout MJ, Shanks A, Odibo AO,
Macones GA and Cahill AG: Umbilical cord arterial lactate compared
with pH for predicting neonatal morbidity at term. Obstet Gynecol.
124:756–761. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Brăila AD, Krastev BM, Mihai-Zamfir E,
Caraveţeanu DC, Al Krayem N, Brăila M, Velea R and Neacşu A:
Uteroplacental apoplexy associated with invasive cervical neoplasm.
Rom J Morphol Embryol. 58:1465–1470. 2017.PubMed/NCBI
|
|
15
|
Brăila AD, Gluhovschi A, Neacşu A,
Lungulescu CV, Brăila M, Vîrcan EL, Cotoi BV and Gogănău AM:
Placental abruption: Etiopathogenic aspects, diagnostic and
therapeutic implications. Rom J Morphol Embryol. 59:187–195.
2018.PubMed/NCBI
|
|
16
|
AbdelAziz NH, AbdelAzeem HG, Monazea EM
and Sherif T: Impact of thrombophilia on the risk of
hypoxic-ischemic encephalopathy in term neonates. Clin Appl Thromb.
23:266–273. 2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Bohîlțea R, Turcan N, Ionescu C, Toader O,
Nastasia S, Neculcea D, Movileanu I, Munteanu O and Cîrstoiu M: The
incidence of prematurity and associated short-term complications in
a multidisciplinary emergency hospital from Romania. In:
Proceedings of the 5th Romanian Congress of the Romanian Society of
Ultrasound in Obstetrics and Gynecology, pp105-112, 2017.
|
|
18
|
Braila AD, Neacsu A, Musetescu AE, Vircan
EL, Florescu A and Bumbea AM: BIiochemical markers in pregnancy
associated with Sjogren's syndrome and thrombophilia. Rev Chim.
69:2300–2303. 2018.
|
|
19
|
Youden WJ: Index for rating diagnostic
tests. Cancer. 3:32–35. 1950.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Depp R: Perinatal asphyxia: Assessing its
causal role and timing. Semin Pediatr Neurol. 2:3–36.
1995.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Turcan N, Bohiltea RE, Ionita-Radu F,
Furtunescu F, Navolan D, Berceanu C, Nemescu D and Cirstoiu MM:
Unfavorable influence of prematurity on the neonatal prognostic of
small for gestational age fetuses. Exp Ther Med. 20:2415–2422.
2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Turcan N, Bohîlțea R, Neacsu A, Baros Al
and Cîrstoiu MM: The role of anticoagulant therapy in the
prevention of preeclampsia. Pharmacokinetic and pharmacodinamic
mechanisms. Rev Chim. 70:1424–1428. 2019.
|
|
23
|
Bohîlţea RE, Cîrstoiu MM, Ionescu CA,
Niculescu-Mizil E, Vlădăreanu AM, Voican I, Dimitriu M and Turcan
N: Primary myelofibrosis and pregnancy outcomes after low
molecular-weight heparin administration: A case report and
literature review. Medicine (Baltimore). 96(e8735)2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Bohiltea RE, Zugravu CA, Nemescu D, Turcan
N, Paulet FP, Gherghiceanu F, Ducu I and Cirstoiu MM: Impact of
obesity on the prognosis of hypertensive disorders in pregnancy.
Exp Ther Med. 20:2423–2428. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Hamed HO: Intrapartum fetal asphyxia:
Study of umbilical cord blood lactate in relation to fetal heart
rate patterns. Arch Gynecol Obstet. 287:1067–1073. 2013.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ionescu AC, Popescu I, Banacu M, Matei A,
Bohîlțea R and Dimitriu M: Is it possible to predict stillbirth in
the third trimester? Filodiritto Editore-Proceedings. In:
Proceedings of the 5th Romanian Congress of the Romanian Society of
Ultrasound in Obstetrics and Gynecology, pp194-198, 2017.
|
|
27
|
Engidawork E, Chen Y, Dell'Anna E, Goiny
M, Lubec G, Ungerstedt U, Andersson K and Herrera-Marschitz M:
Effect of perinatal asphyxia on systemic and intracerebral pH and
glycolysis metabolism in the Rat. Exp Neurol. 145:390–396.
1997.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Neacsu A, Calin A, Braila AD, Navolan DB,
Dimitriu M, Stanica CD, Ioan R and Ionescu C: Chemical effects and
predictive factors in premature birth. Rev Chim. 69:1796–1801.
2018.
|
|
29
|
Cummins G, Kremer J, Bernassau A, Brown A,
Bridle HL, Schulze H, Bachmann TT, Crichton M, Denison FC and
Desmulliez MPY: Sensors for Fetal Hypoxia and Metabolic Acidosis: A
Review. Sensors (Basel). 18(2648)2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Onose G, Chendreanu C, Neacsu A, Grigorean
V, Strâmbu V, Toader C, Spânu A, Ioana A, Anghelescu A, Onose L,
Haras M, et al: Smart textiles for noninvasive monitoring of
physiological signals. Ind Textila. 60:124–133. 2009.
|
|
31
|
Herghelegiu CG, Duta SF, Neacsu A, Suciu N
and Veduta A: Operator experience impact on the evaluation of still
images of a first trimester cardiac assessment protocol. J Matern
Neonatal Med. 1–5. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Ionescu CA, Calin D, Navolan D, Matei A,
Dimitriu M, Herghelegiu C and Ples L: Alobar holoprosencephaly
associated with a rare chromosomal abnormality. Medicine
(Baltimore). 97(e11521)2018.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Herghelegiu D, Ionescu CA, Pacu I,
Bohiltea R, Herghelegiu C and Vladareanu S: Antenatal diagnosis and
prognostic factors of aneurysmal malformation of the vein of Galen:
A case report and literature review. Medicine (Baltimore).
96(e7483)2017.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Ionescu CA, Vladareanu S, Tudorache S,
Ples L, Herghelegiu C, Neacsu A, Navolan D, Dragan I and Oprescu
DN: The wide spectrum of ultrasound diagnosis of holoprosencephaly.
Med Ultrason. 21:163–169. 2019.PubMed/NCBI View
Article : Google Scholar
|
|
35
|
Domingues AP, Moura P and Vieira DN:
Obstetric litigation: The importance of the quality of clinical
files and its influence on expertise conclusions. J Obstet Gynaecol
(Lahore). 35:146–149. 2015.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Executive summary: Neonatal encephalopathy
and neurologic outcome, second edition. Report of the American
College of Obstetricians and Gynecologists' Task Force on Neonatal
Encephalopathy. Obstet Gynecol 123: 896-901, 2014.
|
|
37
|
Munteanu O, Cîrstoiu MM, Filipoiu FM,
Bohîlțea R, Brătilă E, Bulescu IA and Berceanu C: Morphological and
ultrasonographic study of fetuses with cervical hygroma. A case
series. Rom J Morphol Embriol. 57:1421–1427. 2016.PubMed/NCBI
|
|
38
|
Iacob RE, Iacob D, Moleriu RD, Tit DM,
Bungau S, Otrisal P, Aleya S, Judea-Pusta C, Cioca G, Bratu OG, et
al: Consequences of analgesics use in early pregnancy: Results of
tests on mice. Sci Total Environ. 691:1059–1064. 2019.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Bohîlțea R, Furtunescu F, Turcan N,
Navolan D, Ducu I and Cîrstoiu M: Prematurity and intrauterine
growth restriction: Comparative analysis of incidence and short
term complication. Proceedings of SOGR 2018. In: Proceedings of the
17th National Congress of The Romanian Society of Obstetrics and
Gynecology 2018, pp708-712, 2019.
|