Introduction
Percutaneous coronary intervention (PCI) is an
effective treatment for the management of patients with
ST-elevation myocardial infarction (STEMI) (1). However, PCI is not bereft of
complications. Clinical studies have demonstrated that PCI
treatment may be associated with the development of
contrast-induced nephropathy (CIN) (2), due to either contrast anaphylaxis or
renal hypoperfusion (3,4). The development of CIN is associated
with poor patient-associated outcomes, including prolonged hospital
stay and increased mortality (5,6).
Furthermore, the risk of CIN with PCI is higher in patients with
STEMI as compared to other patients requiring contrast
administration. It was also indicated that no therapy is able to
effectively attenuate CIN-related symptoms (7). Thus, there is a need to understand the
risk factors associated with CIN in patients with STEMI undergoing
PCI.
Studies have indicated that pump failure is an
important risk factor for renal injury in patients with STEMI
(8,9). Due to decreased cardiac function,
patients with STEMI and pump failure are prone to develop CIN after
PCI (10). Furthermore, PCI has
also been characterized as a particular risk factor for the
development of CIN, probably due to the urgency of primary PCI
(PPCI) to prevent pump failure or congestive heart failure
(11). To reduce CIN, clinicians
have used drug-based preventive strategies prior to PCI contrast
administration and results have indicated a renal benefit for
patients with STEMI, including improved renal function and
decreased CIN event rates (12).
However, such preventive therapies are frequently used in patients
undergoing elective PCI (EPCI) rather than in patients undergoing
PPCI (13). Furthermore, the CIN
risk factors in patients with STEMI and pump failure have remained
currently elusive and it should be clarified whether there are any
differences in the risk between PPCI and EPCI.
Improving Care for Cardiovascular Disease in China
(CCC) is a collaborative project between the American Heart
Association and the Chinese Society of Cardiology (14). It is an ongoing registry and quality
improvement project focusing on the quality of care for patients
with acute coronary syndrome (ACS). The present retrospective study
(based on this CCC-ACS project) on patients with STEMI and pump
failure undergoing either PPCI or EPCI aimed to explore clinical
risk factors for CIN. The aim was to clarify pump
failure-associated risks based on Killip classes for patients with
STEMI and pump failure undergoing PCI.
Materials and methods
Patients
Data from 40,343 patients with STEMI who had
undergone PCI (EPCI or PPCI) within the CCC-ACS project were
retrospectively collected (14).
Ethical approval was provided by the institutional review board of
the First Affiliated Hospital of the University of Science and
Technology of China (USTC; Hefei, China).
For the study, STEMI was defined as per the 2010
guidelines issued by the Chinese Society of Cardiology (15). Patients fulfilling the following
criteria were included in the study: i) Presenting within 12 h of
the onset of symptoms (typical chest pain lasting for >30 min);
ii) presenting with ST-segment elevation ≥1 mm in at least two
consecutive leads; and iii) treated with stent deployment.
Exclusion criteria of the study were as follows: i)
Patients who did not undergo stent deployment and those who had
undergone surgical revascularization procedures or biodegradable
stent implantation; ii) patients who had serum creatinine levels
>2.0 mg/dl; iii) patients with post-procedural thrombolysis in
myocardial infarction flow grade; iv) patients with pump failure
Killip I class; and v) patients on dialysis or with end-stage
kidney disease.
Data collection
The web-based data collection platform managed by
each participating hospital was used for the collection of data.
For creatinine measurements, reports of biochemical laboratory
analyses for blood samples taken on admission and after the first
72 h of hospitalization were used. CIN was defined as an increase
in serum creatinine by 0.5 mg/dl or 25% within 72 h of PCI
(13).
For other variables (except for lipid profiles and
glucose levels), reports of admission blood samples were used. For
lipid profiles, results were obtained from fasting blood samples
collected within the first 24 h of hospitalization. Total
cholesterol, high-density lipoprotein cholesterol and triglyceride
levels were measured enzymatically (Architec c-Systems; Abbott
Laboratories) and low-density lipoprotein cholesterol levels were
calculated from these lipid parameters using the Friedewald
formula. Complete blood count analyses were performed using
standard clinical laboratory methods (Coulter LH 780 Hematology
Analyzer; Beckman Coulter) and hemoglobin and glycated hemoglobin
(HbA1c) were determined.
Coronary angiography data and Killip
grading
Angiographic PPCI or EPCI data obtained directly
from the cardiac catheterization laboratory records were examined
by two independent researchers (HC and XY), who were blinded to the
patient data. When there was a difference of opinion, we discussed
together and came to a unanimous conclusion. The Killip
classification (16,17) was used for grading pump failure as
follows: i) Killip I: Absence of heart failure symptoms but
increased pulmonary capillary wedge pressure; ii) Killip II: Mild
to moderate heart failure, lung rales in <50% of the two lungs.
X-ray characteristics of pulmonary venous plethora; iii) Killip
III: Severe heart failure with acute pulmonary edema. Lung rales
present in >50% of the two lungs; iv) Killip IV: Cardiogenic
shock.
Statistical analysis
All continuous variables were expressed as the mean
± standard deviation and all categorical variables as n (%). The
assumption of a normal distribution was tested for continuous
variables using a Kolmogorov-Smirnov analysis. Differences in
continuous variables between groups were assessed using Student's
t-test or the Mann-Whitney U test and categorical variables were
compared using Pearson's Chi-square test or Fisher's exact test.
Logistic regression analyses were performed to investigate the
univariable and multivariable predictors with 95% CI. P<0.05 was
considered to indicate statistical significance. Variables with
P<0.10 and the other variables that have been reported to be
associated with contrast-induced nephropathy in patients with STEMI
and pump failure were included in the univariate analysis of the
multivariable logistic regression model. Included variables were
age, male sex, Killip grade, hypertension, primary PCI, chronic
heart failure, chronic kidney failure, smoking, old myocardial
infarction, post-PCI, post-CABG, diabetes mellitus, family history
of CHD, hyperlipemia. All statistical analyses were performed using
the Statistical Package for Social Sciences software (SPSS 20.0 for
Windows; IBM Corp.).
Results
Patients
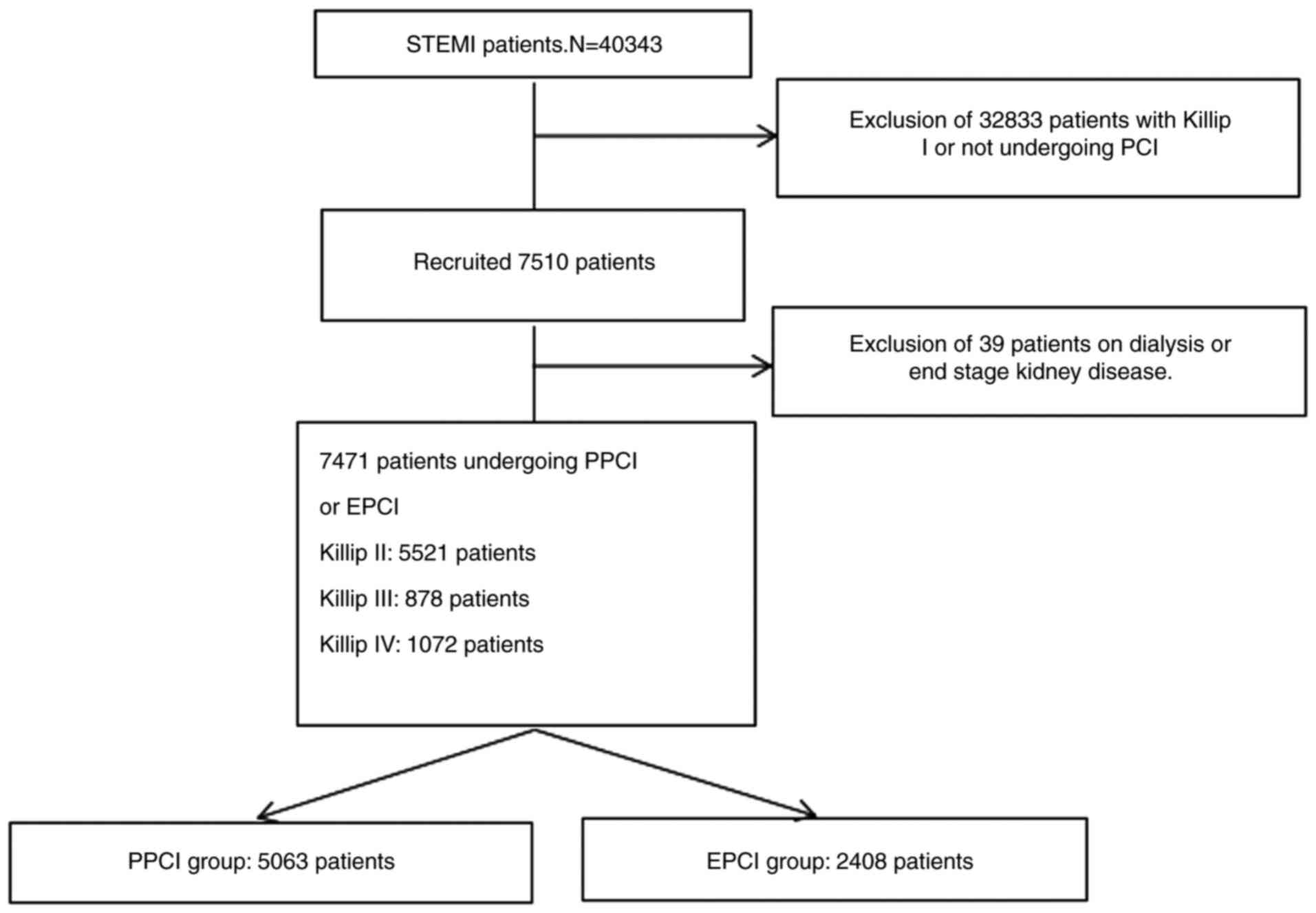
A total of 7,471 patients fulfilled the inclusion
criteria for the analysis (5,521 with Killip grade II, 878 with
Killip III and 1,072 with Killip IV). Patients were further divided
into two groups, with 5,063 patients in the PPCI group and 2,408 in
the EPCI group (Fig. 1). The mean
age of the patients in the PPCI and EPCI group was 63.6±12.5 and
64±11.6 years, respectively. A total of 78.2% of patients in the
PPCI group and 76.2% in the EPCI group were male.
Baseline variables
Details of the baseline characteristics of the study
groups are presented in Table I.
There were no statistically significant differences in terms of
sex, age, body mass index, hypertension, hyperlipemia, diabetes
mellitus, ongoing myocardial infarction, post-PCI, post-coronary
artery bypass graft, heart rate, triglyceride and glycated
hemoglobin between the two groups. The percentage of patients with
family history of congestive heart disease and that of smokers was
significantly higher in the PPCI group, while the percentage of
patients with chronic heart failure was significantly higher in the
EPCI group (P<0.05). Comparison of cardiac arrest rates and
related variables indicated that the incidence of cardiac arrest
was higher in the PPCI group (5.3%) compared to the EPCI group
(3.2%; P<0.001; Table I).
Furthermore, the mean systolic (P<0.001) and diastolic
(P<0.01) blood pressures were significantly lower in the PPCI
group as compared with that in the EPCI group, providing a
mechanism for the increased cardiac arrest rates. In addition,
cholesterol levels related to cardiac arrest onset were also higher
in the PPCI group (P<0.001). The above results demonstrated that
the patients in the PPCI group, as expected, exhibited emergency
features in line with the emergency treatment needed in this
group.
 | Table IComparison of baseline data between
the PPCI and EPCI groups. |
Table I
Comparison of baseline data between
the PPCI and EPCI groups.
| Variable | Total (n=7,471) | PPCI (n=5,063) | EPCI (n=2,408) | P-value |
|---|
| Male sex | 5,792 (77.5) | 3,958 (78.2) | 1,834 (76.2) | 0.051 |
| Age (years) | 63.7±12.2 | 63.6±12.5 | 64.0±11.6 | 0.233 |
| BMI | 24.2±3.3 | 24.2±3.2 | 24.2±3.6 | 0.699 |
| Smoking | 3,437 (46.0) | 2,372 (46.8) | 1,065 (44.2) | 0.034 |
| Hypertension | 3,681 (49.3) | 2,486 (49.1) | 1,195 (49.6) | 0.671 |
| Hyperlipemia | 424 (5.7) | 284 (5.6) | 140 (5.8) | 0.721 |
| Diabetes
mellitus | 1,592 (21.3) | 1,050 (20.7) | 542 (22.5) | 0.081 |
| Family history of
CHD | 151 (2.0) | 116 (2.3) | 35 (1.5) | 0.016 |
| Chronic heart
failure | 91 (1.2) | 50 (1.0) | 41 (1.7) | 0.008 |
| Chronic kidney
failure | 71 (1.0) | 48 (0.9) | 23 (1.0) | 0.976 |
| OMI | 411 (5.5) | 271 (5.4) | 140 (5.8) | 0.414 |
| Post-PCI | 352 (4.7) | 247 (4.9) | 105 (4.4) | 0.323 |
| Post-CABG | 18 (0.2) | 13 (0.3) | 5 (0.2) | 0.686 |
| HR (bpm) | 80.1±18.6 | 80.4±19.2 | 79.6±17.2 | 0.074 |
| HbA1c (%) | 6.71±1.70 | 6.67±1.70 | 6.80±1.70 | 0.077 |
| TG (mmol/l) | 1.66±1.19 | 1.66±1.23 | 1.66±1.12 | 0.903 |
| Cardiac arrest | 344 (4.6) | 266 (5.3) | 78 (3.2) | <0.001 |
| DBP (mmHg) | 75.4±15.5 | 75.1±16.1 | 76.1±14.1 | 0.009 |
| SBP (mmHg) | 123.5±24.9 | 122.7±25.8 | 125.2±22.9 | <0.001 |
| TC (mmol/l) | 4.46±1.25 | 4.54±1.26 | 4.28±1.23 | <0.001 |
| LDL-C (mmol/l) | 1.11±0.43 | 2.87±1.00 | 2.67±0.90 | <0.001 |
| HDL-C (mmol/l) | 2.81±0.97 | 1.13±0.45 | 1.07±0.39 | <0.001 |
Culprit arteries and myocardial injury
during PCI treatment
Data on the frequencies of culprit arteries and
myocardial injury were analyzed from the patients' records. The
culprit artery distributions varied depending on the group. The
proportions of left main coronary artery and right circumflex
artery were both higher in the PPCI group, while those of left
anterior descending, left circumflex artery and saphenous venous
graft lesions were smaller than those in the EPCI group (P<0.05;
Table II). In addition, the
incidence of anterior myocardial infarction in the PPCI group (60%)
was significantly lower than that in the EPCI group (61.2%;
P<0.001; Table II), while
simultaneous treatment of non-culprit arteries was less common in
the PPCI group (6.6%) than in the EPCI group (11.8%; P<0.001;
Table II).
 | Table IIComparison of culprit artery and
related infarction area. |
Table II
Comparison of culprit artery and
related infarction area.
| Variable | Total
(n=7,471) | PPCI (n=5,063) | EPCI (n=2,408) | P-value |
|---|
| Culprit artery | | | | 0.001 |
|
LM | 130 (1.7) | 102 (2.0) | 28 (1.2) | |
|
LAD | 4,379 (58.6) | 2,934 (57.9) | 1,445 (60.0) | |
|
LCX | 850 (11.4) | 552 (10.9) | 298 (12.4) | |
|
RCA | 2,030 (27.2) | 1,427 (28.2) | 603 (25.0) | |
|
SVG | 19 (0.3) | 10 (0.2) | 9 (0.4) | |
|
Others | 63 (0.8) | 38 (0.8) | 25 (1.0) | |
| Simultaneous
treatment of non-culprit artery | 616 (8.2) | 333 (6.6) | 283 (11.8) | <0.001 |
| Anterior myocardial
infarction | 4,509 (60.4) | 3,036 (60.0) | 1,473 (61.2) | 0.001 |
Incidence of CIN
Clinical parameters of renal factors, including
pre-PCI creatinine and pre-PCI estimated glomerular filtration
rate, were not significantly different between the PPCI and EPCI
groups (P>0.05; Table III).
After PCI treatment, the patients in the PPCI group had
significantly higher post-PCI maximum creatinine levels (P<0.05)
as compared to the patients in the EPCI group. In addition, the
incidence of CIN was significantly higher in the PPCI group (17%)
as compared to the EPCI group (P<0.05). Further subgroup
analyses based on pump failure demonstrated that only patients with
Killip II pump failure had a statistically significant increase in
the incidence of CIN in the PPCI group as compared to the EPCI
group (P<0.05). No such difference was noted in patients with
Killip III and IV pump failure.
 | Table IIIComparison of CIN between the PPCI
and EPCI groups. |
Table III
Comparison of CIN between the PPCI
and EPCI groups.
| Variable | Total
(n=7,471) | PPCI (n=5,063) | EPCI (n=2,408) | P-value |
|---|
| Pre-PCI Cr
(mmol/l) | 86.7±37.4 | 86.4±37.3 | 87.2±37.7 | 0.423 |
| Pre-PCI eGFR
(ml/min) | 96.78±50.05 | 97.12±49.97 | 96.08±50.23 | 0.403 |
| Maximum Cr
(mmol/l) | 105.60±63.99 | 106.88±67.82 | 102.92±55.95 | 0.042 |
| CIN incidence | 1,212 (16.2) | 860 (17.0) | 352 (14.6) | 0.009 |
| Killip grade |
|
II | 824 (14.9) | 580 (15.7) | 244 (13.4) | 0.029 |
|
III | 175 (19.9) | 112 (21.3) | 63 (17.9) | 0.230 |
|
IV | 213 (19.9) | 168 (20.2) | 45 (18.8) | 0.622 |
Logistic regression analysis indicated that age,
sex, the Killip classification, hypertension, PPCI vs. EPCI,
presence of chronic heart failure and chronic renal failure were
the major independent variables predicting post-PCI CIN (Table IV). Specifically, Killip
classification was positively associated with an increased risk of
CIN after PCI with an odds ratio of 1.160 (95% CI,
1.069-1.259).
 | Table IVLogistic regression analysis for
contrast-induced nephropathy. |
Table IV
Logistic regression analysis for
contrast-induced nephropathy.
| Variable | Unadjusted OR (95%
CI) | P-value | Adjusted OR (95%
CI) | P-value |
|---|
| Age (per unit
increase in years) | 1.024
(1.019-1.030) | <0.001 | 1.019
(1.013-1.025) | <0.001 |
| Sex (male vs.
female) | 0.651
(0.567-0.747) | <0.001 | 0.805
(0.689-0.941) | 0.006 |
| Killip class (per
unit increase in grade) | 1.214
(1.121-1.315) | <0.001 | 1.160
(1.069-1.259) | <0.001 |
| Hypertension
(present vs. absent) | 0.747
(0.660-0.845) | <0.001 | 0.840
(0.739-0.955) | 0.008 |
| Type of PCI (PPCI
vs. EPCI) | 1.195
(1.044-1.368) | 0.010 | 1.198
(1.044-1.373) | 0.010 |
| Chronic heart
failure (present vs. absent) | 0.453
(0.288-0.714) | 0.001 | 0.579
(0.357-0.939) | 0.027 |
| Chronic kidney
failure (present vs. absent) | 0.276
(0.171-0.444) | <0.001 | 0.335
(0.206-0.547) | <0.001 |
| Smoking (present
vs. absent) | 1.377
(1.215-1.561) | <0.001 | 1.093
(0.924-1.294) | 0.300 |
| OMI (present vs.
absent) | 1.013
(0.773-1.328) | 0.926 | 1.148
(0.720-1.828) | 0.562 |
| Post-PCI (present
vs. absent) | 1.002
(0.750-1.340) | 0.988 | 1.189
(0.725-1.951) | 0.493 |
| Post-CABG (present
vs. absent) | 0.677
(0.222-2.060) | 0.492 | 1.022
(0.216-4.84) | 0.978 |
| Diabetes mellitus
(present vs. absent) | 0.813
(0.703-0.939) | 0.005 | 0.951
(0.789-1.145) | 0.593 |
| Family history of
CHD (present vs. absent) | 0.975
(0.632-1.505) | 0.911 | 1.050
(0.604-1.828) | 0.862 |
| Hyperlipemia
(present vs. absent) | 0.944
(0.727-1.225) | 0.663 | 0.816
(0.596-1.117) | 0.204 |
Discussion
The present results indicated that the incidence of
CIN in patients with STEMI undergoing PPCI with Killip grade II
pump failure is higher as compared to those undergoing EPCI. This
difference is not apparent in other Killip classes. In addition,
the present analysis demonstrated that the Killip classification is
positively associated with post-PCI CIN onset for patients with
STEMI and pump failure.
PPCI is the gold standard treatment for patients
with STEMI, particularly for those with pump failure. On the other
hand, pump failure is an important predictor for CIN (18). For efficient management of patients
with pump failure, coronary artery disease, acute coronary syndrome
or STEMI, risk factors for CIN must be recognized early so that
appropriate management protocols are followed (19). The present study was focused on the
subgroup of patients with STEMI and pump failure, which is known to
be significantly affected by CIN (18). Studies have demonstrated that
oxidative stress, inflammation and renal ischemia/reperfusion are
the major potential pathophysiological mechanisms of CIN, while
perfusion markers (including the Killip grade) have been indicated
to predict the risk of CIN (20,21).
On the other hand, impaired renal function is a risk factor for
cardiovascular diseases and pre-admission renal parameters or
worsening of renal function during hospitalization have been
reported to indicate the risk for adverse events in patients with
STEMI (22,23).
Similar to those of a previous study (24), the present results indicated a
positive correlation between the development of CIN and PPCI
treatment. The present retrospective analysis also demonstrated a
higher incidence of cardiac arrest events, lower SBP values and
higher cholesterol levels in the PPCI group as compared with those
in the EPCI group. These results are consistent with those of
previous studies focusing on patients with PPCI (25,26).
In addition, the incidence of anterior myocardial infarction in the
PPCI group was significantly lower than that in the EPCI group,
while simultaneous treatment of non-culprit arteries was less
frequent in the PPCI group. Of note, the simultaneous treatment of
non-culprit arteries has been reported as a protective factor
against CIN onset (27), which may
partially explain the difference in CIN incidence rates between the
groups of the present study. In the present study, patients in the
PPCI group had a higher incidence of CIN than those in the EPCI
group. Similar results have been reported previously (28).
The effects of pump failure on CIN remain to be
fully elucidated. More specifically, the association between the
Killip grade and the development of CIN in patients with STEMI
after PPCI has remained to be explored. The regression analysis of
the present study demonstrated that failing pump function was
significantly associated with an increased risk of CIN.
Furthermore, patients with Killip grade II in the PPCI group had a
significantly higher incidence of CIN as compared with those in the
EPCI group. However, there was no significant difference in the
incidence of PCI among the Killip III and IV subgroups, despite the
greater severity of pump failure in these patients. The lack of
significance in the incidence of CIN between the PPCI and EPCI
patients with Killip III or IV with pre-PCI renal hypoperfusion may
be attributed to their prior treatment for heart failure (before
PPCI), thereby restoring their renal reperfusion and diminishing
renal injuries after contrast administration. Thus, patients with
Killip II without severe renal dysfunction, who are not pretreated
before the PPCI, may develop ischemia-reperfusion renal injury more
frequently as compared to patients with more severe pump
failure.
As for contrast dosage and type, previous studies
have demonstrated that the contrast dosage is associated with the
post-PCI CIN incidence in patients with STEMI (29,30).
In addition, hypotonic and hyperosmotic contrasts display similar
risk profiles for CIN (31).
Therefore, the influence of contrast media on CIN was not analyzed
in the present study.
The limitations of the present study should be
mentioned. The retrospective nature of the analysis prevents us
from drawing a causal association between the presence of CIN and
the development of pump failure. Only randomized clinical trials
are able to firmly establish such an association. In addition, the
establishment of an animal model will improve our understanding of
the detailed mechanisms.
In conclusion, the Killip classification was
positively associated with post-PCI CIN events in patients with
STEMI and pump failure. The present results also indicate that
patients with Killip II grade pump failure undergoing PPCI are at a
higher risk of CIN as compared to those undergoing EPCI and there
is a need for adequate preventive measures to avoid the development
of CIN in such individuals. Since our conclusions are derived from
a retrospective cohort, there is a need for further prospective
studies to confirm the present results.
Acknowledgements
Not applicable.
Funding
This study was supported by the CCC-ACS project; the
Open Research Fund of Anhui Institute of Cardiovascular Diseases
(grant no. KF2018007) and ‘Borrow to transfer to supplement’
project of Hefei independent innovation policy (grant no.
J2019Y02).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HC, XY and LM conceived and designed the study. HC
and XY were involved in data collection, interpretation and
analysis, and in writing of the manuscript. LM was involved in the
editing of the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The Ethics Committee of the First Affiliated
Hospital of USTC approved this study (no. 2020-P-053). Informed
consent was waived due to the retrospective nature of the study and
the use of anonymized clinical data.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Keeley EC, Boura JA and Grines CL: Primary
angioplasty versus intravenous thrombolytic therapy for acute
myocardial infarction: A quantitative review of 23 randomised
trials. Lancet. 361:13–20. 2003.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Turak O, Ozcan F, Isleyen A, Tok D, Sokmen
E, Buyukkaya E, Aydogdu S, Akpek M and Kaya MG: Usefulness of the
neutrophil-to-lymphocyte ratio to predict bare-metal stent
restenosis. Am J Cardiol. 110:1405–1410. 2012.PubMed/NCBI View Article : Google Scholar
|
|
3
|
De Luca G, Dirksen MT, Spaulding C,
Kelbaek H, Schalij M, Thuesen L, van der Hoeven B, Vink MA, Kaiser
C, Musto C, et al: Drug-Eluting Stent in Primary Angioplasty
(DESERT) Cooperation: Drug-eluting vs bare-metal stents in primary
angioplasty: A pooled patient-level meta-analysis of randomized
trials. Arch Intern Med. 172:611–622. 2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Jukema JW, Verschuren JJW, Ahmed TAN and
Quax PHA: Restenosis after PCI. Part 1: Pathophysiology and risk
factors. Nat Rev Cardiol. 9:53–62. 2011.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Li J-J, Ren Y, Chen K-J, Yeung AC, Xu B,
Ruan XM, Yang YJ, Chen JL and Gao RL: Impact of C-reactive protein
on in-stent restenosis: A meta-analysis. Tex Heart Inst J.
37:49–57. 2010.PubMed/NCBI
|
|
6
|
Bolca O, Güngör B, Özcan KS, Karadeniz FÖ,
Sungur A, Köroğlu B, Bakhshyaliyev N, Yelgeç NS, Karataş B, İpek G,
et al: The neutrophil-to-lymphocyte ratio is associated with
bare-metal stent restenosis in STEMI patients treated with primary
PCI. Coron Artery Dis. 26:402–408. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
AlFaleh HF, Alsuwaida AO, Ullah A, Hersi
A, AlHabib KF, AlNemer K, AlSaif S, Taraben A, Kashour T, Balghith
MA, et al: The prognostic impact of in-hospital worsening of renal
function in patients with acute coronary syndrome. Int J Cardiol.
167:866–870. 2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Amin AP, Spertus JA, Reid KJ, Lan X,
Buchanan DM, Decker C and Masoudi FA: The prognostic importance of
worsening renal function during an acute myocardial infarction on
long-term mortality. Am Heart J. 160:1065–1071. 2010.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Goldberg A, Hammerman H, Petcherski S,
Zdorovyak A, Yalonetsky S, Kapeliovich M, Agmon Y, Markiewicz W and
Aronson D: Inhospital and 1-year mortality of patients who develop
worsening renal function following acute ST-elevation myocardial
infarction. Am Heart J. 150:330–337. 2005.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Stefanini GG, Taniwaki M, Kalesan B, Räber
L, Stortecky S, Pilgrim T, Onuma Y, Silber S, Serruys PW, Meier B,
et al: The impact of renal impairment on long-term safety and
effectiveness of drug-eluting stents. PLoS One.
9(e106450)2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Cassese S, Byrne RA, Tada T, Pinieck S,
Joner M, Ibrahim T, King LA, Fusaro M, Laugwitz KL and Kastrati A:
Incidence and predictors of restenosis after coronary stenting in
10 004 patients with surveillance angiography. Heart. 100:153–159.
2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Best PJM, Berger PB, Davis BR, Grines CL,
Sadeghi HM, Williams BA, Willerson JT, Granett JR and Holmes DR Jr:
PRESTO Investigators. Impact of mild or moderate chronic kidney
disease on the frequency of restenosis: Results from the PRESTO
trial. J Am Coll Cardiol. 44:1786–1791. 2004.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Marenzi G, Lauri G, Assanelli E,
Campodonico J, De Metrio M, Marana I, Grazi M, Veglia F and
Bartorelli AL: Contrast-induced nephropathy in patients undergoing
primary angioplasty for acute myocardial infarction. J Am Coll
Cardiol. 44:1780–1785. 2004.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hao Y, Liu J, Liu J, Smith SC Jr, Huo Y,
Fonarow GC, Ma C, Ge J, Taubert KA, Morgan L, et al: CCC-ACS
Investigators: Rationale and design of the Improving Care for
Cardiovascular Disease in China (CCC) project: A national effort to
prompt quality enhancement for acute coronary syndrome. Am Heart J.
179:107–115. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Shen W and Gao R: Chinese Society of
Cardiology. Guideline for diagnosis and treatment of patients with
ST-elevation myocardial infarction. China J Cardiol. 38:675–690.
2010.PubMed/NCBI
|
|
16
|
Killip T III and Kimball JT: Treatment of
myocardial infarction in a coronary care unit. A two year
experience with 250 patients. Am J Cardiol. 20:457–464.
1967.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Khot UN, Jia G, Moliterno DJ, Lincoff AM,
Khot MB, Harrington RA and Topol EJ: Prognostic importance of
physical examination for heart failure in non-ST-elevation acute
coronary syndromes: The enduring value of Killip classification.
JAMA. 290:2174–2181. 2003.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Yamaguchi J, Kasanuki H, Ishii Y, Yagi M,
Nagashima M, Fujii S, Koyanagi R, Ogawa H, Hagiwara N, Haze K, et
al: HIJC Investigators: Serum creatinine on admission predicts
long-term mortality in acute myocardial infarction patients
undergoing successful primary angioplasty: Data from the Heart
Institute of Japan Acute Myocardial Infarction (HIJAMI) Registry.
Circ J. 71:1354–1359. 2007.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Halkin A, Mehran R, Casey CW, Gordon P,
Matthews R, Wilson BH, Leon MB, Russell ME, Ellis SG and Stone GW:
Impact of moderate renal insufficiency on restenosis and adverse
clinical events after paclitaxel-eluting and bare metal stent
implantation: Results from the TAXUS-IV Trial. Am Heart J.
150:1163–1170. 2005.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wang C-H, Zhang S-Y, Fang Q, Shen ZJ, Fan
ZJ, Jin XF, Zeng Y, Liu ZY and Xie HZ: Renal Dysfunction and hsCRP
Predict Long-term Outcomes of Percutaneous Coronary Intervention in
Acute Myocardial Infarction. Am J Med Sci. 349:413–420.
2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zhang RY, Zhu ZB, Zhang Q, Yang ZK, Hu J,
Lv AK, Zhang JS and Shen WF: Impact of moderate or severe renal
insufficiency on long-term outcomes in patients undergoing
drug-eluting stent based coronary intervention. Int J Cardiol.
136:72–79. 2009.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Garg P, Charytan DM, Novack L, Cutlip DE,
Popma JJ, Moses J, Leon MB, Schofer J, Breithardt G, Schampaert E,
et al: Impact of moderate renal insufficiency on restenosis and
adverse clinical events after sirolimus-eluting and bare metal
stent implantation (from the SIRIUS trials). Am J Cardiol.
106:1436–1442. 2010.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Sahin I, Gungor B, Can MM, Avci II, Guler
GB, Okuyan E, Biter H, Yildiz SS, Ayca B, Satilmis S, et al: Lower
blood vitamin D levels are associated with an increased incidence
of contrast-induced nephropathy in patients undergoing coronary
angiography. Can J Cardiol. 30:428–433. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Seyfarth M, Kastrati A, Mann JFE, Ndrepepa
G, Byrne RA, Schulz S, Mehilli J and Schömig A: Prognostic value of
kidney function in patients with ST-elevation and non-ST-elevation
acute myocardial infarction treated with percutaneous coronary
intervention. Am J Kidney Dis. 54:830–839. 2009.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Rubartelli P, Niccoli L, Verna E, Giachero
C, Zimarino M, Fontanelli A, Vassanelli C, Campolo L, Martuscelli E
and Tommasini G: Stent implantation versus balloon angioplasty in
chronic coronary occlusions: Results from the GISSOC trial. Gruppo
Italiano di Studio sullo Stent nelle Occlusioni Coronariche. J Am
Coll Cardiol. 32:90–96. 1998.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Sahin I, Karabulut A, Avci II, Okuyan E,
Biter HI, Yildiz SS, Can MM, Gungor B, Dinckal M and Serebruany V:
Contribution of platelets indices in the development of
contrast-induced nephropathy. Blood Coagul Fibrinolysis.
26:246–249. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Börekçi A, Gür M, Türkoğlu C, Çaylı M,
Selek Ş, Kaypaklı O, Uçar H, Coşkun M, Şeker T, Koç M, et al:
Oxidative stress and paraoxonase 1 activity predict
contrast-induced nephropathy in patients with ST-segment elevation
myocardial infarction undergoing primary percutaneous coronary
intervention. Angiology. 66:339–345. 2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Mizuguchi Y, Shibutani H, Hashimoto S,
Yamada T, Taniguchi N, Nakajima S, Hata T and Takahashi A:
Examination of the appropriate timing of reperfusion therapy for
recent myocardial infarction: A Japanese single-center
retrospective study. Indian Heart J. 70:4–9. 2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Caspi O, Habib M, Cohen Y, Kerner A,
Roguin A, Abergel E, Boulos M, Kapeliovich MR, Beyar R, Nikolsky E,
et al: Acute Kidney Injury After Primary Angioplasty: Is
Contrast-Induced Nephropathy the Culprit? J Am Heart Assoc.
6(6)2017.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Velibey Y, Tanik O, Oz A, Guvenc TS,
Kalenderoglu K, Gumusdag A, Guzelburc O, Tekkesin AI, Uzun AO,
Alper AT, et al: Off-Hour Primary Percutaneous Coronary Angioplasty
Does Not Affect Contrast-Induced Nephropathy in Patients With
ST-Segment Elevation Myocardial Infarction. Angiology. 68:807–815.
2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Marrón B, Ruiz E, Fernández C, Almeida P,
Horcajada C, Navarro F and Caramelo C: Systemic and renal effects
of preventing contrast nephrotoxicity with isotonic (0.9%) and
hypotonic (0.45%) saline. Rev Esp Cardiol. 60:1018–1025.
2007.PubMed/NCBI View
Article : Google Scholar : (In Spanish).
|