Introduction
Rheumatoid arthritis (RA) is a chronic and
refractory autoimmune joint disease, characterized by the
proliferation of synoviocytes in inflamed synovia and the
expression of inflammatory cytokines and chemokines in synoviocytes
(1). Multiple pro-inflammatory and
inflammatory cytokines have been indicated to participate in the
development of RA. A variety of cytokines and chemokines are
present in the synovium of patients with RA, which have an
important role in the maintenance of the inflammatory response
(2,3). Important pro-inflammatory cytokines,
including IL-33, IL-1β, IL-6, IL-8 and TNF-α, and chemokines such
as MIG and IP-10, are considered markers for the diagnosis of RA
and represent therapeutic targets (3-9).
A complex mechanistic network exists between these cytokines and
chemokines.
IL-33 is a member of the IL-1 family of cytokines
(10). Supporting evidence
regarding the association between IL-33 and pathogenesis of RA has
been provided by Matsuyama et al (11), who reported that IL-33 levels were
elevated in the serum and synovial fluid of patients with RA,
demonstrating a positive association with disease activity. IL-33
is expressed in synovial fluid of patients with RA and released
from fibroblast-like synoviocytes (FLSs) following stimulation with
TNF-α and IL-1β (11,12). IL-33 is able to activate human mast
cells to release IL-8, in patients with RA (13). A study indicated that IL-33 was able
to enhance the expression of MIG and IP-10 in wild-type mice with
colitis (14). IL-33 has an
important role and a complex relationship with cytokines and
chemokines in RA (12,15,16).
However, the role of IL-33 remains controversial, with a number of
studies suggesting that it promotes inflammation (17), while others indicate that the
response is inhibitory (18). A
confounding observation is that high levels of IL-33 may be
detected in the serum or synovial fluid of just one third to half
of all patients with RA, suggesting that IL-33 is widely variable
in RA (11,19,20). A
significant number of patients with RA have low levels of IL-33 in
serum but still exhibit high disease activity (19). Since contrary results are
increasingly observed in RA, the present study hypothesized that
the concentrations of IL-33 and other cytokines and chemokines may
not be linearly correlated, but a more complex polynomial
association should be further investigated. The present study aimed
to establish a correlation curve model of cytokines (IL-8, MIG and
IP-10) and chemokines (IL-1β, TNF-α and IL-6) with IL-33 in serum
and synovia, and to explore the nature of the relationship.
Materials and methods
Patient enrollment
A total of 96 patients with RA who had presented at
the Rheumatology Clinic of Zhujiang Hospital of Southern Medical
University between 1st April 2019 to 1st September 2020 (Guangzhou,
China) were recruited for the study. All patients fulfilled the
2010 RA classification criteria (21) and disease activity score
DAS28-erythrocyte sedimentation rate (ESR) ≥2.6. The disease
activity was graded according to DAS28-ESR: <2.6 (clinical
remission), 2.6-3.1 (low), 3.2-5.0 (moderate activity) and >5.1
(high disease activity) (22).
Patients with remission of RA were excluded. Serum and synovial
fluid samples were collected as appropriate from patients with RA
after obtaining written informed consent.
Human FLS culture
Synovial tissue samples were obtained by knee joint
arthroscopy from the knees of five patients with active RA, with a
DAS28-ESR >5.1. All patients with RA fulfilled the 2010 RA
classification and signed written informed consent. Synovial
tissues were cut into 1-2 mm3 pieces and incubated with
collagenase I for 1-3 h at 37˚C to isolate synoviocytes (RA-FLSs).
Upon reaching 95% confluency, cells were subsequently digested
using 0.25% trypsin, collected, resuspended and plated for
proliferation. Following subculture, RA-FLSs at passages 3-6 were
used for subsequent experiments. RA-FLSs were cultured in DMEM
(Gibco; Thermo Fisher Scientific, Inc.) containing 10% FBS (Gibco;
Thermo Fisher Scientific, Inc.), 100 U/ml penicillin and 100 µg/ml
streptomycin in a humidified atmosphere containing 5%
CO2 at 37˚C. The culture medium was refreshed every 3-4
days. Cells at passage 3 to 6 were used for the experiments.
Individual cell samples from the patients were used in the
assays.
Synovial-cell activation
RA-FLSs were seeded in the wells of 24-well plates
at a density of 2x104 cells/well. After 24 h of culture,
0, 10, 50, 100 or 150 ng/ml human IL-33 (R&D Systems) was
added, followed by incubation for 4 or 24 h in a humidified
atmosphere containing 5% CO2 at 37˚C. Human IL-17 (100
ng/ml; R&D Systems) and TNF-α (100 ng/ml; R&D Systems), two
cytokines known to activate synoviocytes, were used as the positive
controls (23), followed by
incubation for 4 or 24 h in a humidified atmosphere containing 5%
CO2 at 37˚C.
Reverse transcription-quantitative PCR
(RT-qPCR)
Total RNA was isolated from RA-FLSs using
TRIzol® reagent (Invitrogen; Thermo Fisher Scientific,
Inc.) in accordance with the manufacturer's protocols. RT was
conducted using the first-strand cDNA synthesis kit (cat. no.
RR047A; Takara Biotechnology Co., Ltd.) in accordance with the
manufacturer's protocols. Real-time PCR was performed using a SYBR
Premix ExTaq kit (cat. no. RR420A; Takara Biotechnology Co., Ltd.)
to assess the expression of IL-6 in accordance with the
manufacturer's protocols, IL-8, MIG, IP-10, IL-1β and TNF-α. The
PCR reactions were performed on an ABI 7500 Real-Time PCR system
(Applied Biosystems; Thermo Fisher Scientific, Inc.) in accordance
with the manufacturer's protocols. The following thermocycling
conditions were used for the qPCR: Initial denaturation (95˚C, 30
sec, 1 cycle) and dissociation (95˚C for 5 sec; 60˚C for 34 sec; 40
cycles). Relative mRNA expression was calculated using the
2-∆∆Cq method (24), the
∆∆Ct (∆∆Ct=∆Ct sample-∆Ct control) was used to indicate the ratio
of the expression of the target gene in the model group to that of
the control group. The primers were synthesized by Sangon Biotech
Co., Ltd.. Primer sequences are listed in Table I.
 | Table IThe primer sequences used for PCR. |
Table I
The primer sequences used for PCR.
| Gene name | Primer | Sequence (5'-3') |
|---|
| IL-6 | Forward |
ACTCACCTCTTCAGAACGAATTG |
| | Reverse |
CCATCTTTGGAAGGTTCAGGTTG |
| IL-8 | Forward |
TTTTGCCAAGGAGTGCTAAAGA |
| | Reverse |
AACCCTCTGCACCCAGTTTTC |
| MIG | Forward |
CCAGTAGTGAGAAAGGGTCGC |
| | Reverse |
AGGGCTTGGGGCAAATTGTT |
| IP-10 | Forward |
GTGGCATTCAAGGAGTACCTC |
| | Reverse |
TGATGGCCTTCGATTCTGGATT |
| IL-1β | Forward |
CCACCTCCAGGGACAGGATA |
| | Reverse |
AACACGCAGGACAGGTACAG |
| TNF-α | Forward |
GAGGCCAAGCCCTGGTATG |
| | Reverse |
CGGGCCGATTGATCTCAGC |
| GAPDH | Forward |
GCACCGTCAAGGCTGAGAAC |
| | Reverse |
TGGTGAAGACGCCAGTGGA |
ELISA
The concentrations of cytokines and chemokines in
serum and synovial fluid samples were measured using ELISA in
accordance with the manufacturer's protocols, including IL-33 (cat.
no. D3300B; R&D Systems, Inc.), IL-1β (cat. no. DLB50; R&D
Systems, Inc.), TNF-α (cat. no. 88734688; Thermo Fisher Scientific,
Inc.), IL-6 (cat. no. 88706688; Thermo Fisher Scientific, Inc.),
IL-8 (cat. no. 88808622; Thermo Fisher Scientific, Inc.), MIG (cat.
no. EHMIG; Invitrogen; Thermo Fisher Scientific, Inc.) and IP-10
(cat. no. KAC2361; Invitrogen, Thermo Fisher Scientific, Inc.).
After stimulation of 2x104 RA-FLSs with human IL-33 as
described above, the supernatants of the FLS cell cultures were
collected and IL-6, IL-8, MIG, IP-10, TNF-α and IL-1β
concentrations were quantified. The optical density values of each
sample were measured at 450 nm.
Statistical analysis
Statistical analyses were performed using SPSS 24.0
(IBM Corp.) and GraphPad Prism 8.0 (GraphPad Software, Inc.).
Values are presented as the mean ± standard deviation or the median
(interquartile range). Differences between groups were analyzed
using the Kruskal-Wallis test (>2 groups) or a Mann-Whitney U
test (two groups). Mann-Whitney U-test was also used as a post-hoc
test after the Kruskal-Wallis test, and Bonferroni correction was
performed for these data. Second-order polynomial regression
analyses were performed using SPSS 24.0 to quantify the
associations among the variables. All statistical tests and
confidence intervals were two-sided and P<0.05 was considered to
indicate statistical significance.
Results
Baseline clinical and demographic
features
A total of 96 patients with RA were recruited, from
whom 40 serum samples (35 females and 5 males; mean age,
51.80±13.37 years) and 56 synovial samples (43 females and 13
males; mean age, 48.85±13.39 years) were obtained. Patients
characteristics are displayed in Table
II.
 | Table IICharacteristics of the patients with
rheumatoid arthritis and their protein levels. |
Table II
Characteristics of the patients with
rheumatoid arthritis and their protein levels.
| Sample type | n | Gender, M/F | Age, years | IL-33, pg/ml | MIG, pg/ml | IP-10, pg/ml | IL-6, pg/ml | IL-8, pg/ml | TNF-α, pg/ml | IL-1β, pg/ml |
|---|
| Serum | 40 | 5/35 | 51.80±13.37 | 36.46
(16.05,191.92) | 1,081.88
(460.67,1,384.15) | 143.40
(90.50,316.40) | 94.95
(3.33,172.46) | 675.23
(117.55,1,042.17) | 20.17
(12.02,32.53) | 12.85
(10.21,22.73) |
| Synovial fluid | 56 | 13/43 | 48.85±13.39 | 40.45
(22.40,80.36) | 563.59
(404.68,1,176.68) | 201.12
(269.35,606.46) | 34.13
(9.53,222.03) | 14.13
(6.74,44.44) | 9.68
(3.38,16.22) | 8.56
(1.74,9.45) |
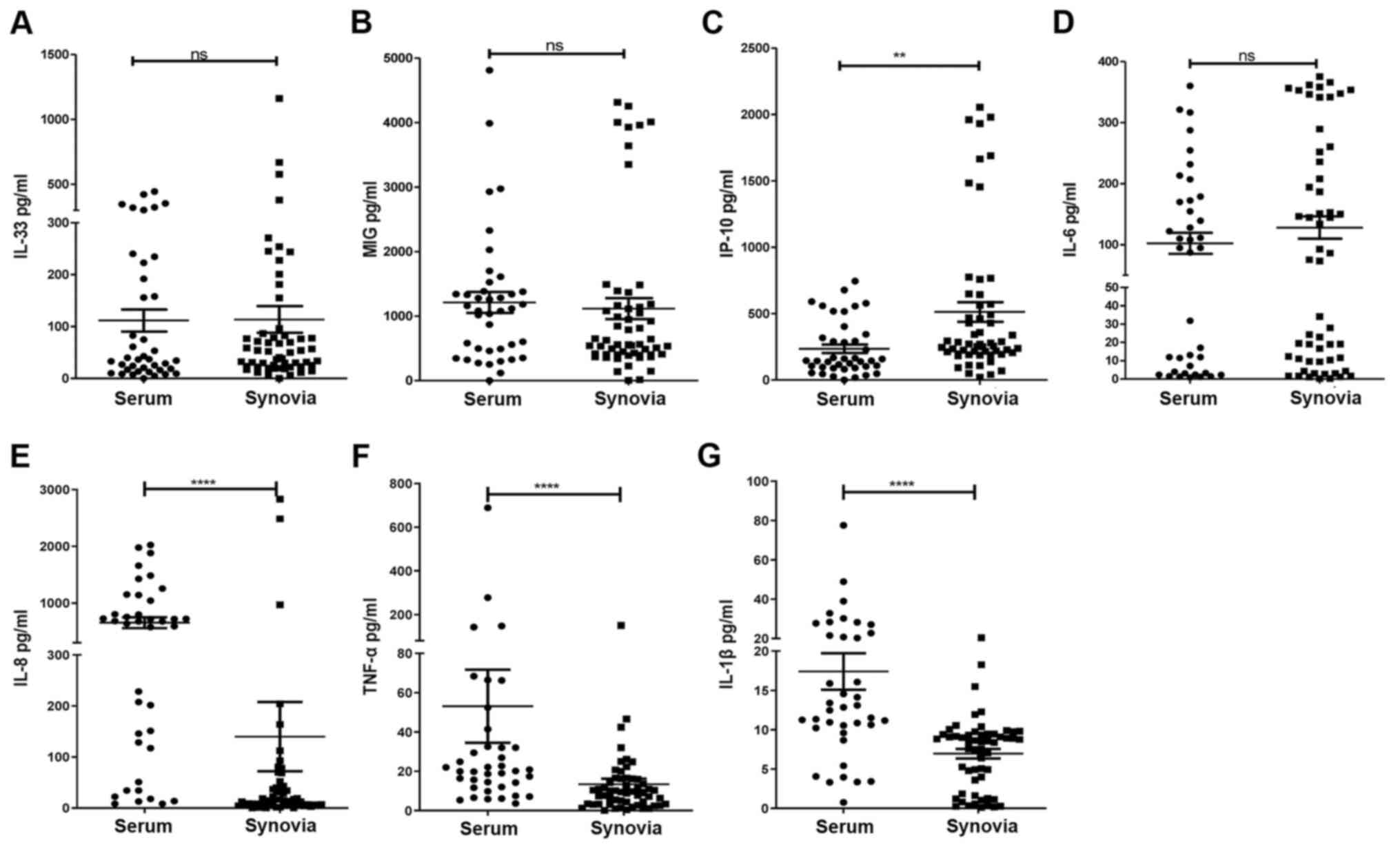
Cytokine and chemokine levels in
patients with RA
At the baseline, there were no differences in IL-33,
MIG and IL-6 concentrations between the synovial and serum samples
of patients with RA (Fig. 1A,
B and D). The IP-10 concentration was
significantly higher in synovial fluid than in serum (Fig. 1C). The IL-8, TNF-α and IL-β
concentrations were significantly higher in serum than in synovial
fluid (Fig. 1E-G).
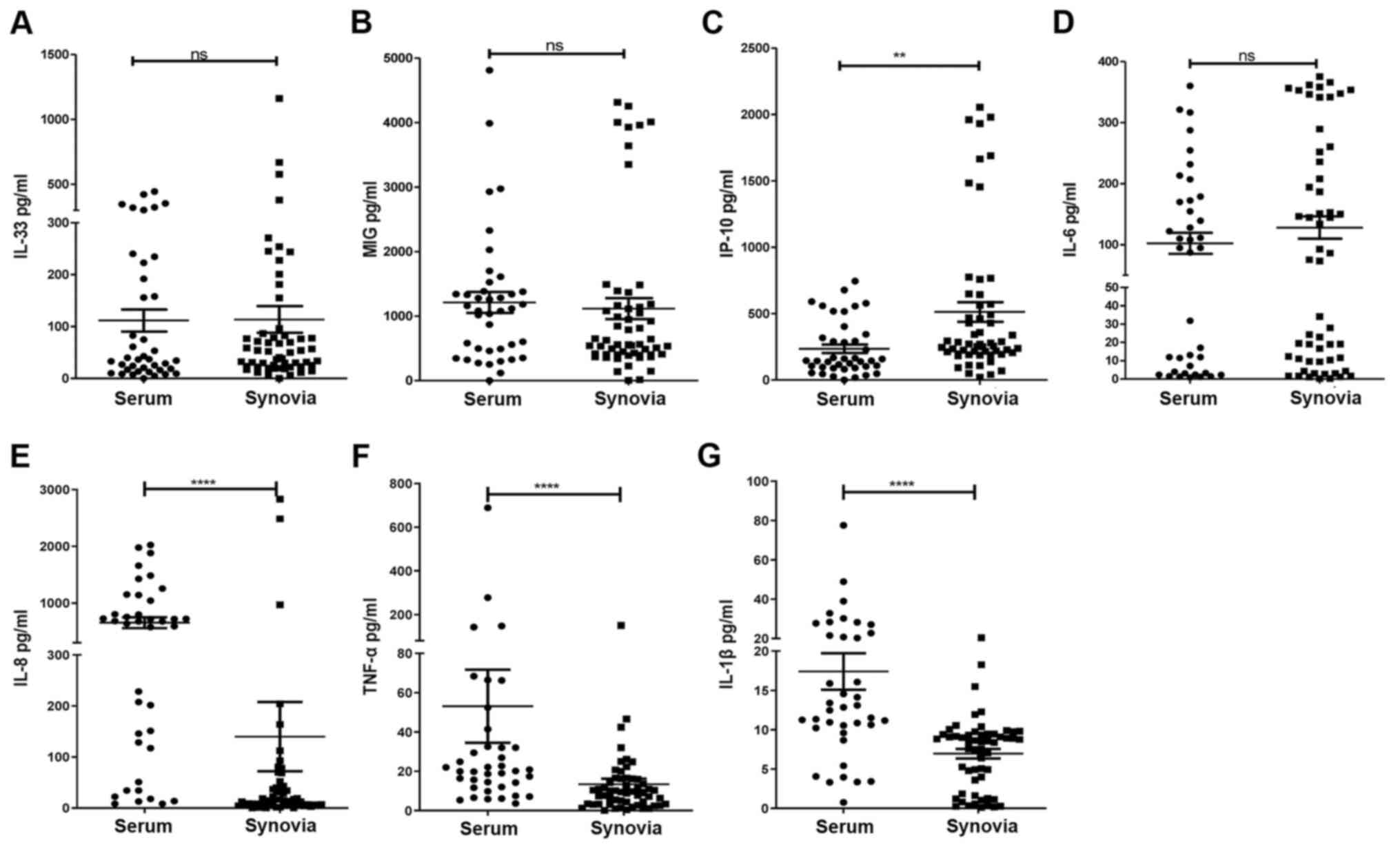 | Figure 1Concentration of cytokines and
chemokines in serum and synovia, measured by ELISA, were obtained
from 96 patients with RA (n=40 serum and 56 synovial samples). (A)
IL-33 (P=0.640), (B) MIG (P=0.183), (C) IP-10 (P=0.001), (D) IL-6
(P=0.376), (E) IL-8 (P<0.001), (F) TNF-α (P<0.001) and (G)
IL-1β (P<0.001) levels were compared between RA synovia and
serum. **P<0.01, ****P<0.001 as
assessed by the Mann-Whitney U-test, as appropriate. Ns, no
significance; RA, rheumatoid arthritis; MIG, monokine-induced by
γ-IFN; IP-10, IFN-γ-induced protein 10. |
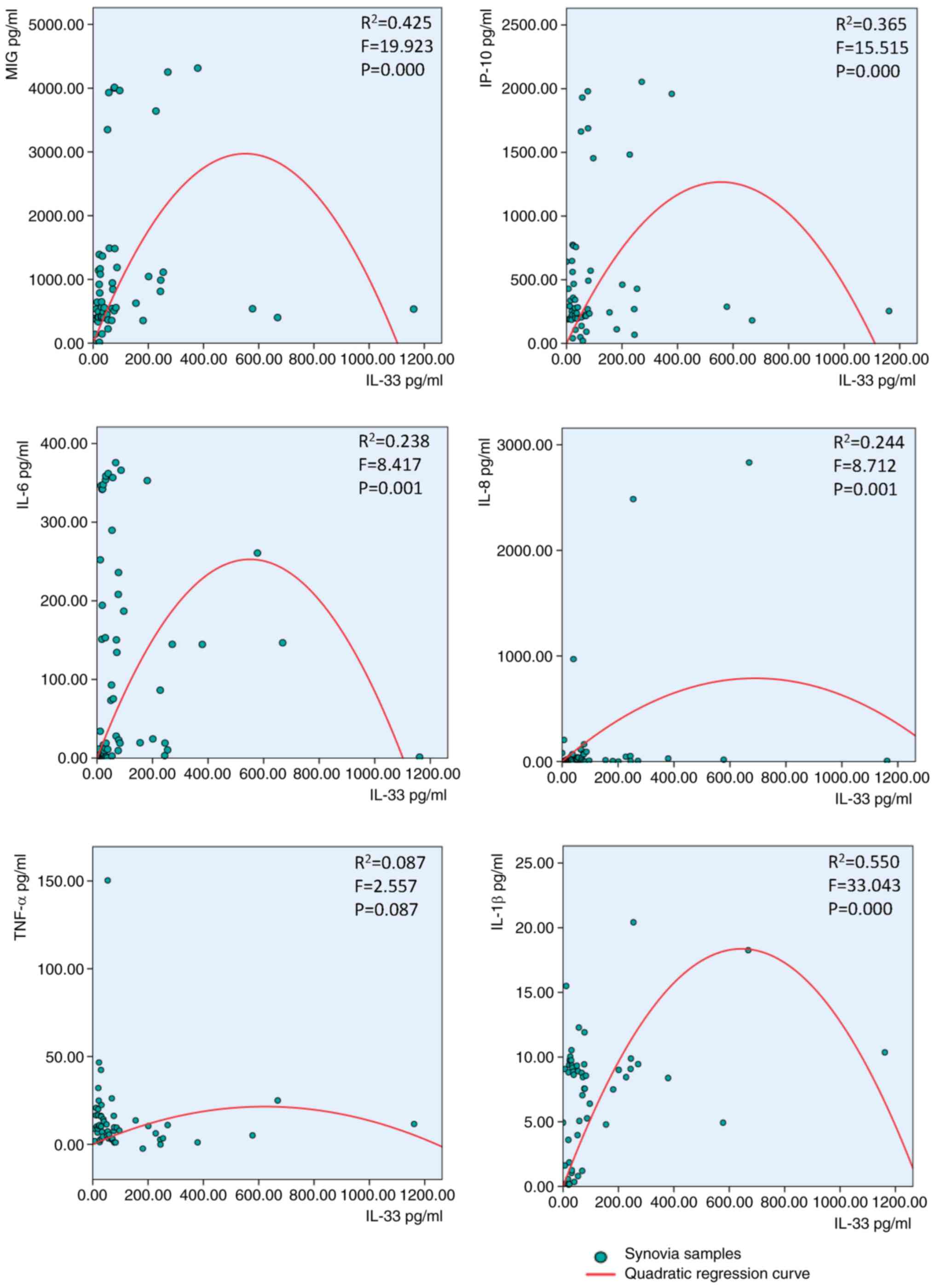
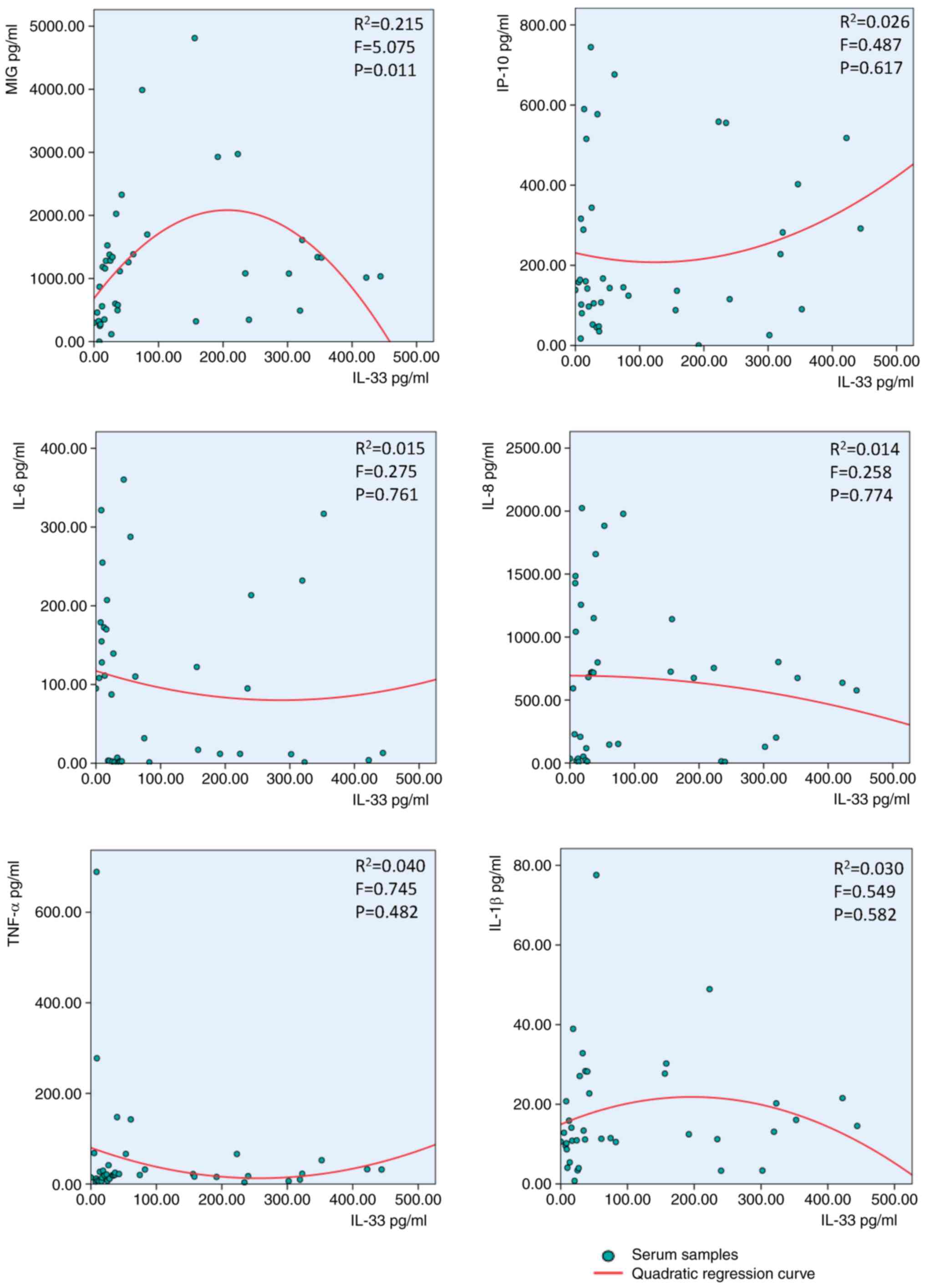
IL-33 concentration follows an
inverted-U-shaped curve in response to cytokines and
chemokines
The IL-33 concentration exhibited an
inverted-U-shaped curve in response to IL-6, IL-1β, IL-8, MIG and
IP-10, but not TNF-α, in synovial fluid of patients with RA
(Fig. 2). The same IL-33
inverted-U-shaped association was observed after treatment with MIG
but notIP-10, TNF-α, IL-6, IL-1β or IL-8 in the serum of patients
with RA (Fig. 3).
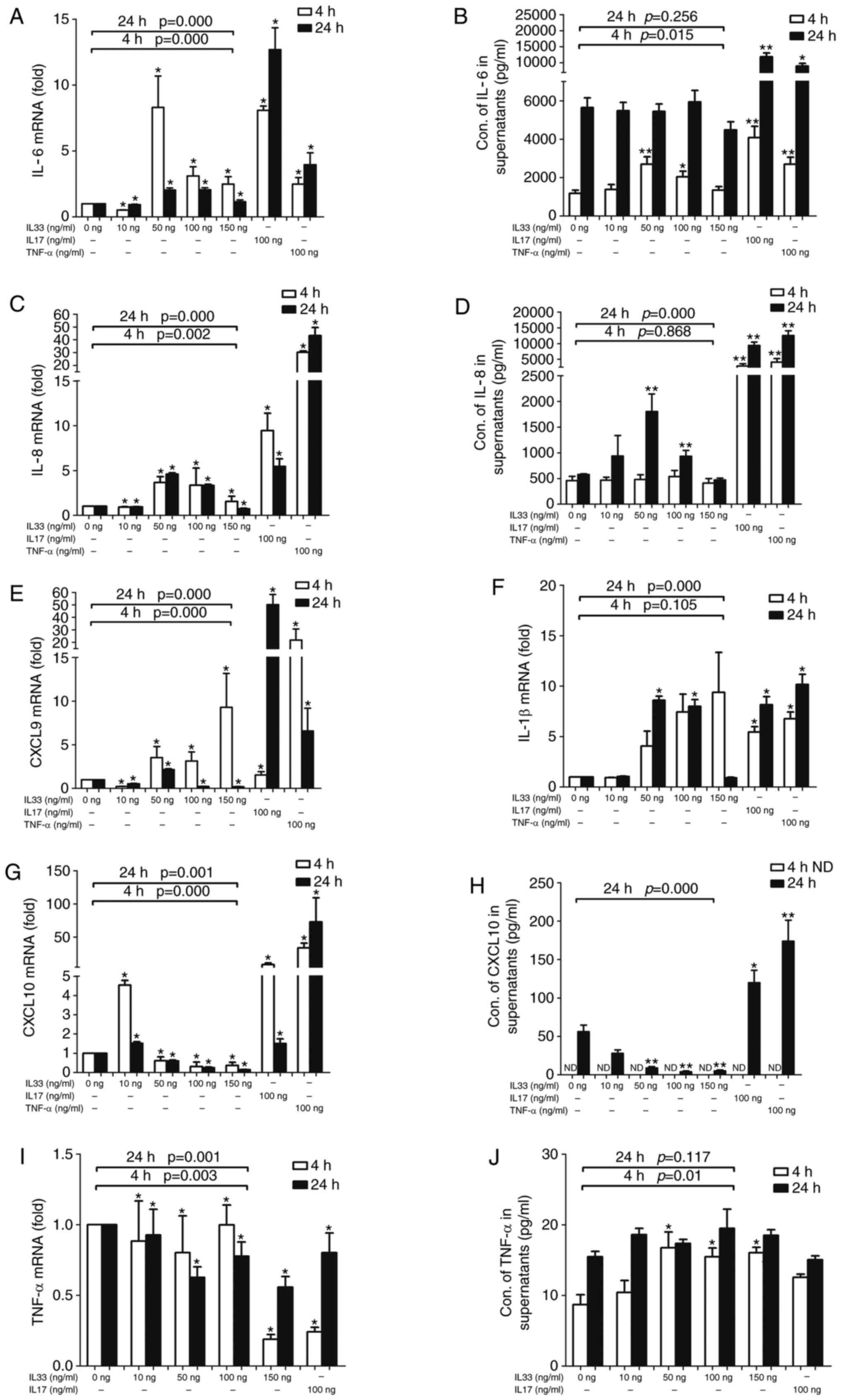
mRNA and protein expression levels of
IL-6, IL-8, MIG, IP-10, IL-1β and TNF-α in FLSs stimulated by
IL-33
As presented in Fig.
4, IL-33 affected the mRNA expression of IL-6, IL-8, MIG,
IP-10, IL-1β and TNF-α in FLS. However, only the protein expression
of IL-6, IL-8, IP-10 and TNF-α was detectable in the supernatants
of the FLS cell culture. IL-33 affected both the mRNA and protein
expression of IL-6 in FLSs. A high response of FLSs at a
concentration of 50 ng/ml IL-33 suggested that it had a narrow
working concentration on FLSs (Fig.
4A). A greater response at 4 h than at 24 h suggested that
IL-33 is effective over a precise time frame in FLSs. Over time,
the effect of IL-33 on IL-6 secretion by FLSs changed (Fig. 4B). Different to IL-6, the expression
of IL-8 reached a peak after 24 h at a concentration of 50 ng/ml of
IL-33 (Fig. 4C and D). MIG mRNA expression was upregulated in
the 50 and 100 ng groups after 4 h, but only in the 50 ng group
after 24 h (Fig. 4E), while MIG
protein could not be detected in the FLS culture supernatant. IL-6,
IL-8 and IL-1β mRNA were detected at high levels in both the 50 and
100 ng IL-33 groups at both time-points, but MIG and IL-1β protein
expression was not detected in the supernatants of FLSs, even at
low levels. (Fig. 4F). IP-10 mRNA
expression was downregulated as the concentration of IL-33
increased (Fig. 4G). The ELISA
results also demonstrated that the protein expression of IP-10
decreased as the concentration of IL-33 increased after 24 h.
Conversely, TNF-α and IL-17 increased the IP-10 mRNA expression in
FLSs (Fig. 4H). TNF-α protein and
mRNA expression was affected by different concentrations of IL-33
or by IL-17, but the obvious inverted-U-shaped regularity was not
observed. (Fig. 4I and J).
Discussion
Previous studies have indicated that IL-33 is
expressed in the synovium of patients with RA, promoting articular
inflammation (12,15,20);
however, the underlying mechanisms have not been fully elucidated
and conflicting experimental results have been observed on numerous
occasions. In vivo, injection of IL-33 has been demonstrated
to exacerbate joint inflammation in a K/BxN serum-transfer mouse
model of arthritis (17). However,
a separate study provided conflicting results, indicating that
injection of IL-33 ameliorated joint inflammation in the same mouse
model (18). Of note, another two
research groups observed similar contradictory results: Biton et
al (25) reported that IL-33
was able to suppress inflammation in collagen-induced arthritis
(CIA) mice, but Xu et al (12) demonstrated that IL-33 was a critical
proinflammatory cytokine causing fibroblast activation in CIA mice.
The contradictory results may be due to the different dosage of
IL-33 injected. Therefore, whether the effect of IL-33 was
proinflammatory or inhibitory may be dependent on its
concentration.
To confirm this hypothesis, an additional series of
experiments was performed. First, the concentrations of a variety
of cytokines and chemokines were measured in synovia and serum. Of
note, the level of IP-10 was considerably higher in synovial fluid
than in serum, indicating that inflamed joints constitute the
primary source of circulating IP-10 in arthritis. Conversely, IL-8,
TNF-α and IL-1β levels were substantially higher in serum than in
synovial fluid. Next, the association of IL-33 with other cytokines
and chemokines in patients with RA was investigated. As expected,
IL-33 was not linearly correlated with other cytokines and
chemokines but exhibited an inverted-U-shaped association. In the
present study, IL-33 exhibited an inverted-U-shaped association
with IL-6, IL-8, IL-1β, MIG and IP-10 in the synovia of patients
with RA. Although the results may reveal the mechanism of IL-33 in
RA, in numerous instances, the data points at the right side of the
x-axis do not map onto the U-shaped fit, hence, U-shaped model may
only have limited applicability in clinical practice. In the cell
model, there appears to be some U-shaped effects of IL-33. This
notion may indeed be valid, but the mathematical U-shaped curve fit
does not seem ideal in serum and synovial fluid samples for the
patient. This fact does make the U-shaped association
insignificant. Therefore, the sample size needs to be expanded to
increase the validity of the results and the conclusions of the
present study. Although there is an inverted-U-shaped association
between synovial IL-33 and MIG, IP-10, IL-6, IL-8, IL-1β in
patients with RA, it may be disproportionately influenced by only a
couple of data points as high concentration points, which limited
the extrapolation of conclusions of the present study. Therefore,
it is of note that in the present study, the datapoints do not
exactly follow the U-shaped curve fit in most cases. Therefore, the
applicability of this mathematical model in clinical practice is
limited.
Although the conclusions are limited, the study
partially illustrates that IL-33 may have a greater effect on
synovial cells and that IL-33 has a more specific role in synovia
than in serum, since this U-shaped association occurs only in
synovia. Synovia is principally produced by synovial cells, and
therefore, the present study aimed to explore the role of IL-33 in
synovial cells. The experiment was designed with various IL-33
concentrations stimulating FLSs. As expected, the most noteworthy
result was that specific concentrations of IL-33 were important in
FLS cultures, with 10 ng/ml being too low to cause an impact on FLS
but 150 ng/ml IL-33 being too high. This response was consistent
with the U-type association between IL-33 and other cytokines
observed in synovial fluid. The most appropriate concentration of
IL-33 was 50 ng/ml for 20,000 FLSs, although its influence was not
comparable with IL-17 and TNF-α, which strongly influenced FLSs. In
another study, negative results were obtained (26), which may be because IL-33 was
effective within a narrow range of working concentrations and the
most appropriate ratio of the IL-33 concentration/cell number was
important in FLS cultures. Time-points were an additional factor
that affected FLS, with the incubation time of 4 h being more
effective than 24 h regarding IL-6 release, suggesting that IL-33
affects FLS over a precise time frame. IL-6 was released earlier
than IL-8, suggesting that different cytokines released by FLSs
were controlled by different mechanisms. A significant
inverted-U-shaped influence on IL-6 and IL-8, but not IP-10 and
TNF-α, was obtained, and therefore, the results imply that
different cytokines released by FLSs were controlled by different
mechanisms. IL-33 regulated the production of IL-1β in FLS in an
inverted U-shaped manner and combined with the results of another
study, which established that IL-1β regulated the production of
IL-33 in FLS (27), it was
demonstrated that IL-33 has a key role in the positive and negative
feedback mechanisms with IL-1β. In the present study, the
association between IL-33 and other cytokines and chemokines was
assessed. Initially, the inverted-U-shaped association between
IL-33 and the chemokines IL-8, MIG and IP-10 in synovia was shown.
These results are important for RA, suggesting that IL-33 has the
potential capability to recruit and regulate inflammatory cells. A
limitation of the present study was that although the U-shaped fit
used appeared to be the best-fitting curve for the present data,
the insufficient number of high-concentration values of IL-33
limited the extrapolation of conclusions. In the future, more
high-concentration value data of IL-33 will be added to strengthen
the current conclusions. In clinical testing, high-concentration
value samples for IL-33 are relatively rare; however, increasing
the sample size may be a suitable solution.
The present study reported that IL-33, a member of
the IL-1 family of cytokines, exhibits an inverted-U-shaped
association with multiple cytokines and chemokines in synovial
fluid, including IL-6, IL-1β, IL-8, MIG and IP-10, but not in
serum. IL-33 also triggered the expression of the pro-inflammatory
cytokines IL-6 and IL-1β and the chemokines IL-8 and MIG in a
U-shaped dose-dependent manner in RA-FLSs.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Natural
Science Foundation of China (grant no. 81601397) and the National
Natural Science Foundation of China (grant no. 81771727).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JW, QL and JXD performed the experiments. JW and QL
conceived the study and analyzed the results. JJZ and QHY designed
the experiments and revised the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Zhujiang Hospital of Southern Medical University (Guangzhou, China;
grant no. 2019-KY-091-01). This was to certify that the research
design and methods are in accordance with the requirements of the
ethical standards of the 2013 Declaration of Helsinki, and
regulations and procedures regarding human subject protection in
Chinese laws. Written informed consent was obtained from all study
participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interest.
References
|
1
|
Nanki T, Nagasaka K, Hayashida K, Saita Y
and Miyasaka N: Chemokines regulate IL-6 and IL-8 production by
fibroblast-like synoviocytes from patients with rheumatoid
arthritis. J Immunol. 167:5381–5385. 2001.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Szekanecz Z, Kim J and Koch AE: Chemokines
and chemokine receptors in rheumatoid arthritis. Semin Immunol.
15:15–21. 2003.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kuan WP, Tam LS, Wong CK, Ko FW, Li T, Zhu
T and Li EK: CXCL 9 and CXCL 10 as sensitive markers of disease
activity in patients with rheumatoid arthritis. J Rheumatol.
37:257–264. 2010.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ruschpler P, Lorenz P, Eichler W, Koczan
D, Hänel C, Scholz R, Melzer C, Thiesen HJ and Stiehl P: High CXCR3
expression in synovial mast cells associated with CXCL9 and CXCL10
expression in inflammatory synovial tissues of patients with
rheumatoid arthritis. Arthritis Res Ther. 5:R241–R252.
2003.PubMed/NCBI View
Article : Google Scholar
|
|
5
|
Pandya JM, Lundell AC, Andersson K,
Nordstrom I, Theander E and Rudin A: Blood chemokine profile in
untreated early rheumatoid arthritis: CXCL10 as a disease activity
marker. Arthritis Res Ther. 19(20)2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Siebert S, Tsoukas A, Robertson J and
McInnes I: Cytokines as therapeutic targets in rheumatoid arthritis
and other inflammatory diseases. Pharmacol Rev. 67:280–309.
2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Brennan FM and McInnes IB: Evidence that
cytokines play a role in rheumatoid arthritis. J Clin Invest.
118:3537–3545. 2008.PubMed/NCBI View
Article : Google Scholar
|
|
8
|
Hueber AJ, Asquith DL, McInnes IB and
Miller AM: Embracing novel cytokines in RA-complexity grows as does
opportunity! Best Pract Res Clin. Rheumatol. 24:479–487.
2010.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mateen S, Zafar A, Moin S, Khan AQ and
Zubair S: Understanding the role of cytokines in the pathogenesis
of rheumatoid arthritis. Clin Chim Acta. 455:161–171.
2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
He R, Yin H, Yuan B, Liu T, Luo L, Huang
P, Dai L and Zeng K: IL-33 improves wound healing through enhanced
M2 macrophage polarization in diabetic mice. Mol Immunol. 90:42–49.
2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Matsuyama Y, Okazaki H, Tamemoto H, Kimura
H, Kamata Y, Nagatani K, Nagashima T, Hayakawa M, Iwamoto M, Yoshio
T, et al: Increased levels of interleukin 33 in sera and synovial
fluid from patients with active rheumatoid arthritis. J Rheumatol.
37:18–25. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Xu D, Jiang HR, Kewin P, Li Y, Mu R,
Fraser AR, Pitman N, Kurowska-Stolarska M, McKenzie AN, McInnes IB
and Liew FY: IL-33 exacerbates antigen-induced arthritis by
activating mast cells. Proc Natl Acad Sci USA. 105:10913–10918.
2008.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Rivellese F, Suurmond J, Habets K, Dorjée
AL, Ramamoorthi N, Townsend MJ, de Paulis A, Marone G, Huizinga TW,
Pitzalis C and Toes RE: Ability of interleukin-33- and immune
complex-triggered activation of human mast cells to down-regulate
monocyte-mediated immune responses. Arthritis Rheumatol.
67:2343–2353. 2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Pushparaj PN, Li D, Komai-Koma M,
Guabiraba R, Alexander J, McSharry C and Xu D: Interleukin-33
exacerbates acute colitis via interleukin-4 in mice. Immunology.
140:70–77. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Palmer G, Talabot-Ayer D, Lamacchia C, Toy
D, Seemayer CA, Viatte S, Finckh A, Smith DE and Gabay C:
Inhibition of interleukin-33 signaling attenuates the severity of
experimental arthritis. Arthritis Rheum. 60:738–749.
2009.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Yuan FL, Li X, Lu WG, Li CW, Xu RS and
Dong J: IL-33: A promising therapeutic target for rheumatoid
arthritis? Expert Opin Ther Targets. 15:529–534. 2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Xu D, Jiang HR, Li Y, Pushparaj PN,
Kurowska-Stolarska M, Leung BP, Mu R, Tay HK, McKenzie AN, McInnes
IB, et al: IL-33 exacerbates autoantibody-induced arthritis. J
Immunol. 184:2620–2626. 2010.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Anthony RM, Kobayashi T, Wermeling F and
Ravetch JV: Intravenous gammaglobulin suppresses inflammation
through a novel T(H)2 pathway. Nature. 475:110–113. 2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Mu R, Huang HQ, Li YH, Li C, Ye H and Li
ZG: Elevated serum interleukin 33 is associated with autoantibody
production in patients with rheumatoid arthritis. J Rheumatol.
37:2006–2013. 2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Talabot-Ayer D, McKee T, Gindre P, Bas S,
Baeten DL, Gabay C and Palmer G: Distinct serum and synovial fluid
interleukin (IL)-33 levels in rheumatoid arthritis, psoriatic
arthritis and osteoarthritis. Joint Bone Spine. 79:32–37.
2012.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Aletaha D, Neogi T, Silman AJ, Funovits J,
Felson DT, Bingham CO III, Birnbaum NS, Burmester GR, Bykerk VP,
Cohen MD, et al: 2010 Rheumatoid arthritis classification criteria:
An American College of Rheumatology/European League Against
Rheumatism collaborative initiative. Arthritis Rheum. 62:2569–2581.
2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Izawa N, Hirose J, Fujii T, Oka H, Uehara
K, Naito M, Matsumoto T, Tanaka S and Tohma S: The utility of
25-question geriatric locomotive function scale for evaluating
functional ability and disease activity in Japanese rheumatoid
arthritis patients: A cross-sectional study using NinJa database.
Mod Rheumatol. 29:328–334. 2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Wu J, Li Q, Jin L, Qu Y, Liang BB, Zhu XT,
Du HY, Jie LG and Yu QH: Kirenol Inhibits the function and
inflammation of fibroblast-like synoviocytes in rheumatoid
arthritis in vitro and in vivo. Front Immunol.
10(1304)2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Biton J, Khaleghparast Athari S, Thiolat
A, Santinon F, Lemeiter D, Hervé R, Delavallée L, Levescot A, Roga
S, Decker P, et al: In vivo expansion of activated Foxp3+
regulatory T cells and establishment of a type 2 immune response
upon IL-33 treatment protect against experimental arthritis. J
Immunol. 197:1708–1719. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Machado CRL, Resende GG, Macedo RBV,
Nascimento VC, Sliva TP, Kakehasi AM and Andrade MVM: AB0028
Fibroblast-like synoviocytes may not be the target of il-33 in the
joint phisiopathology. Ann Rheum Dis. 76 (Suppl 2)(S1056)2017.
|
|
27
|
Lee EJ, So MW, Hong S, Kim YG, Yoo B and
Lee CK: Interleukin-33 acts as a transcriptional repressor and
extracellular cytokine in fibroblast-like synoviocytes in patients
with rheumatoid arthritis. Cytokine. 77:35–43. 2016.PubMed/NCBI View Article : Google Scholar
|