1. Introduction
In December 2019, a novel coronavirus-induced
pneumonia epidemic began in Wuhan, Hubei, which was officially
termed coronavirus disease-2019 (COVID-19) by the World Health
Organization thereafter (1). By
midnight, March 10, 2020, according to reports from 31 provinces,
including autonomous regions and municipalities directly under the
central government in China, Xinjiang Production and Construction
Corps, there were 16,145 confirmed cases, 4,492 of which were
severe, 61,475 cured and discharged cases, 3,158 deaths, 80,778
confirmed and 285 suspected cases (2). Subsequently, a total of 675,886 those
who came into close contact with those infected were traced, where
14,607 close contacts were placed under medical observation
(2).
During this sudden epidemic, the medical staff are
severely affected. During the COVID-19 epidemic, as the high-risk
group fighting in the front line, a number of medical staff have
been infected. Among the 138 patients diagnosed with COVID-19
continuously admitted to The Zhongnan Hospital of Wuhan University
(Wuhan, China) between January 1 and January 28, 2020, the
proportion of medical professionals was 40% (1). In addition, among the 1,099 patients
with COVID-19 in 552 hospitals across 31 provinces in China, the
proportion of medical staff was 2.09% (3). Dr Yixin Zeng, deputy director of the
National Health Commission, said in a press conference on February
14, 2020, that by midnight on February 11, 2020, a total of 1,716
confirmed cases had been reported by medical staff, accounting for
3.8% of all confirmed cases in China (4). Among those six patients died,
accounting for 0.4% of all COVID-19-associated deaths in China
(4). In addition, Hubei province
reported 1,502 cases confirmed by medical staff, accounting for
87.5% of the total (4). Wuhan
reported 1,102 cases confirmed by medical staff, accounting for
73.4% of the cases confirmed by medical staff in Hubei province
(4). Therefore, reasonable analysis
of risk factors for the occupational exposure to medical staff and
effective prevention measures may reduce the incidence of infection
among medical staff.
Hubei 672 Orthopedics Hospital of Integrated Chinese
and Western Medicine has been designated as one of the hospitals
that has treated a large number of patients with COVID-19 in
January 2020. According to the actual situation in this hospital, a
series of preventative measures have been formulated. The present
study summarizes the relevant experience, risk factors of
occupational exposure and prevention strategies for front-line
medical staff.
2. Risk factors
Insufficient understanding
COVID-19 is an entirely new disease that remains
poorly understood. The majority of the front-line medical staff are
not experts in respiratory and infectious diseases who lack
in-depth understanding (5). Prior
to the development of the national diagnosis and treatment program,
understanding of the route of transmission and severity of this
disease was insufficient.
Lack of early protection
This sudden epidemic caused a severe shortage of
personal protective equipment (PPE), including N95 face masks,
protective clothing and goggles, within the population, especially
in Wuhan (6). This resulted in a
high level of occupational exposure by the medical staff during the
early stages of the epidemic.
Environmental factors
At present, it is considered that the main methods
of coronavirus transmission are respiratory droplets (7), close contact (7) aerosol (7), fecal-oral or urine-oral (3,8) and
ocular mucosa (9) transmission. A
certain amount of virus is present in the respiratory droplets,
vomit and feces of the patients (7). In addition, the airtight environment
in the isolation area leads to a high concentration of virus being
present, which increases the risk of occupational exposure by
medical staff during extended stay.
Routine procedures
A number of routine procedures, including sputum
suction, endotracheal intubation and life nursing (including the
cleaning and hygiene of patients), involve direct contact with
respiratory droplets, vomit, feces and other bodily fluids of the
patients, which increases the risk of coronavirus exposure.
Psychological factors
Emotional tension is manifested as a sense of
powerlessness towards patients who are at the highest risk
(10). These are exacerbated by
long shifts and endocrine disorders due to the shortage of staff,
expectations of overcoming this epidemic, psychological pressure
caused by the diagnosis or death of relatives, colleagues and
peers. This may increase the psychological burden of front-line
medical staff, resulting in the reduction of alertness and
elevation of the risk of occupational exposure.
Other factors
Psychological tension experienced by the patients,
or even minor damage to the PPE worn by the medical staff may also
lead to the accidental occupational exposure to coronavirus.
3. Prevention strategies
Training
Hospital infection office and quality control office
should perform effective professional training on COVID-19
prevention and control in all departments of the hospital,
especially those that are not associated with respiratory medicine
or infection. This training program should include knowledge on the
etiology of COVID-19, hand hygiene, the disinfection process,
prevention and treatment process in case of occupational exposure.
Through training, understanding by the medical staff on how to
prevent and control occupational exposure can be improved with the
assistance of doctors and nurses in charge of infection control.
Staff can then train and practice again in the clinical department
to maintain an appropriate level of knowledge among all staff
within the hospital.
Strengthening the personal protection
of front-line medical staff
It is necessary to prepare a sufficient amount of
PPE and disinfection facilities to strengthen the personal
protection of front-line medical staff. Technical Guidelines for
the Prevention and Control of Novel Coronavirus Infection in
Medical Institutions (First Edition) issued by the National Health
Commission on January 23, 2020, specifies the types of PPE
required, how to wear and remove them, along with a list of
potential issues (11).
Subsequently, Guidelines on the Scope of Use of Common Medical
Protective Equipment (Trial) in The Prevention and Control of
COVID-19, issued by the National Health Commission on January 27,
2020(12), further clarified the
requirements for the use of medical PPE. Standardized and effective
use of PPE is an effective preventive measure for cutting the
transmission of infection (13) and
to prevent infection spreading from patients and carriers to others
(13), which is also a key measure
to ensure the safety of medical staff during diagnosis and
treatment. Therefore, it is necessary to perform effective training
and practical exercises to enhance medical staff proficiency with
the PPE, so that everybody can pass security check before entering
the quarantine area to treat patients.
Rational area layout and regular
disinfection
Hubei 672 Orthopedics Hospital of Integrated Chinese
& Western Medicine controls the source of infection, which is
patients in this case, by establishing the following requirements
of physical isolation: i) Strictly defining the layout of three
areas, namely clean, potentially hazardous and hazardous areas; ii)
two channels of personnel, specifically the medical staff and
patient channel; and iii) two buffer zones, namely between the
clean and the potentially hazardous areas and between the
potentially hazardous and the hazardous area. In addition, the
disinfection system has been improved, where daily disinfection is
performed in the isolation area. The following protocols have been
adopted: i) Air disinfection, where occupied rooms are ventilated
twice a day for ~30 min each time, whilst unoccupied rooms are
irradiated with ultraviolet light once a day for >1 h each time;
ii) surface and floor disinfection, where the surfaces and floors
in the ward are wiped and sprayed daily with 1,000 mg/l chlorine
and wiped with clean water after 30 min. If waste particles that
are visible to the naked eye is present, the waste is first
completely removed, before being covered with 2,000 mg/l chlorine.
Cleaning tools, including rags and mops, are used exclusively for
the designated areas; iii) treatment of medical waste, where the
medical waste of a patient is treated as infectious waste and are
transported in a sealed, double-layered yellow waste bag. This bag
is marked as ‘special infection’ before being transported to the
temporary medical waste storage room immediately after contact by
telephone; and iv) final disinfection. Here, after a patient is
discharged, transferred or has died, a final disinfection is
performed in the ward.
Enhancing the awareness of
occupational protection and standardizing routine procedures
All medical staff should strictly comply with the
routine procedure process, develop good operation practice, raise
awareness of occupational protection, perform all routine
procedures by following the standard prevention principles, stay
alert and avoid the risk of occupational exposure caused by
operational errors. Protective face screen or mask should be worn
when performing daily care procedures, including feeding, sputum
suction and life nursing, which typically involve contact with body
fluids or secreted materials from the patient. Quick-drying hand
sanitizer should be used following every patient contact and the
outer gloves should be replaced after contacting three different
patients to reduce the risk of occupational exposure.
Reasonable scheduling and early
psychological intervention
It is necessary to implement reasonable shift
systems and rest rotation to avoid overworking and ensure
sufficient rest time. This can potentially prevent physical and
mental fatigue and to protect the mental health of medical staff.
Hubei 672 Orthopedics Hospital of Integrated Chinese and Western
Medicine provides a psychological hotline and online consultations
to release psychological pressure. These methods were established
with aims to understand the situation in the family and properly
distribute essential provisions including food, masks and
disinfectant, to the families of medical staff on the frontline to
alleviate additional worries.
Psychological counseling for
patients
Following COVID-19 diagnosis, the immediate reaction
of the patients may include panic, despair, refusal of treatment,
self-injury and attempting to injure others (14). Medical staff should provide timely
and effective psychological counseling to such patients to ensure
that they can accept the reality of their illness and cooperate
with treatment to appropriately release pressure and limit
impulsive behaviors, in turn reducing the risks to occupational
exposure experienced by medical staff caused by violent injury.
4. Treatment after occupational
exposure
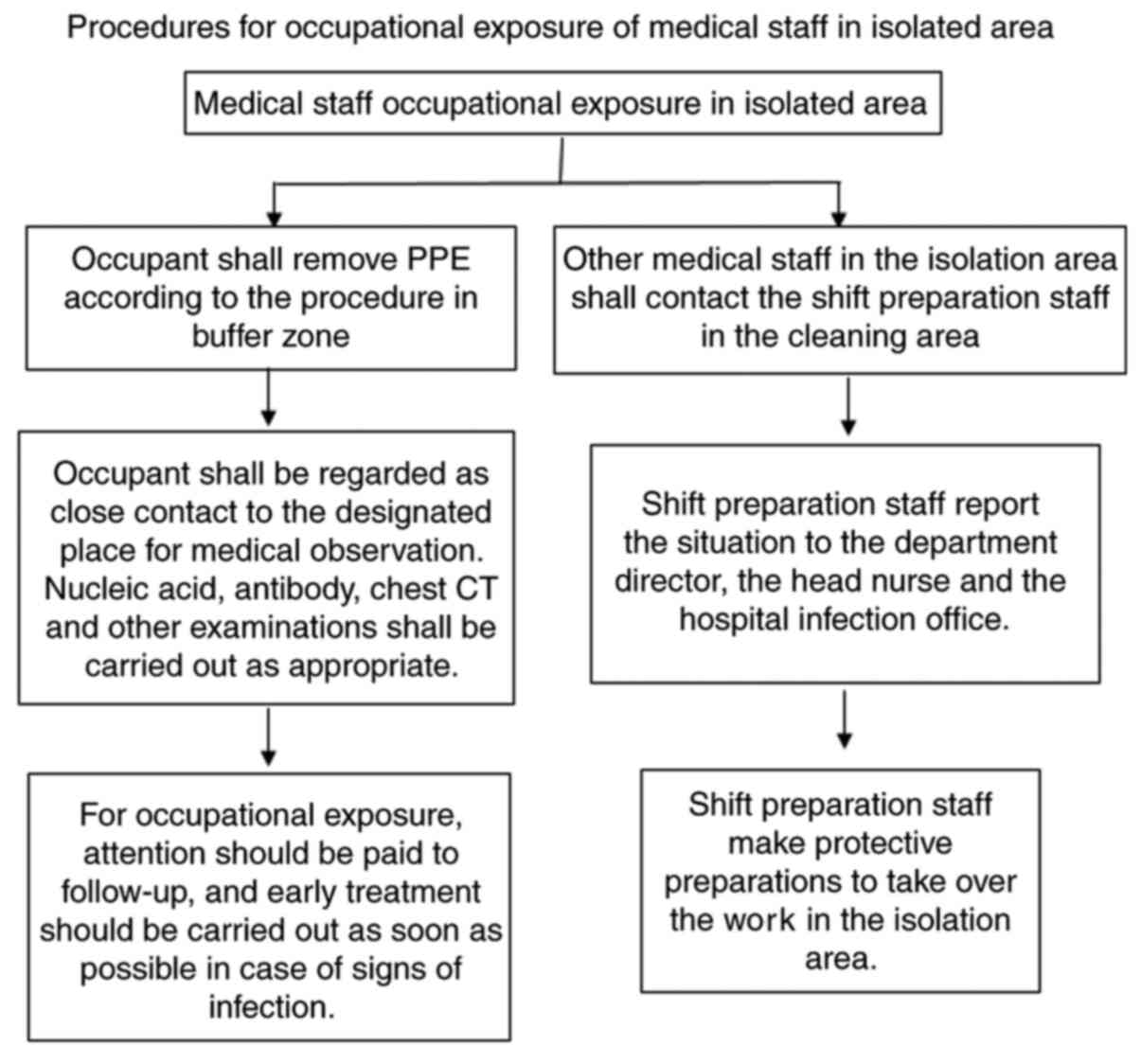
It is necessary to formulate a standardized
contingency plan for occupational exposure. Following occupational
exposure, it should be immediately handled in accordance with this
plan. After occupational exposure, the person should remove PPE
according to the standard procedure. They should be regarded as a
close contact (15) and moved to
the designated area for medical observation. Nucleic acid (16), antibody (16), chest CT and other examinations
should be performed as appropriate. Other medical staff in the
isolation area should also immediately contact the shift
preparation staff in the cleaning area, who should in turn report
the situation to the department director, head nurse and hospital
infection office so that protective preparations can be performed
to take over the work in the isolation area. In addition, following
occupational exposure, staff should be carefully followed up, such
that early treatment should be immediately administered when signs
of infection are observed. A pipeline of this specific process is
presented in Fig. 1.
5. Conclusions
In conclusion, the outbreak of COVID-19 has brought
major challenges to infection control in hospitals around the
world. In particular, occupational exposure has the potential to
adversely affect the health of each member of medical staff.
Therefore, it is necessary to engage everyone in the hospital,
master the relevant knowledge of COVID-19 and use PPEs to protect
the safety of themselves and their colleagues. The present article
summarized the relevant risk factors for occupational exposure and
proposed a number of management strategies for these risks, which
may serve as a referencing point for the prevention and control of
this disease in hospitals.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
JT and XGL contributed to the study conception and
design, the acquisition of data and the analysis and interpretation
of data. YL, QLL, WX, SJZ, YLL and QCZ contributed to drafting the
manuscript and critically revising the manuscript for important
intellectual content. JT prepared the manuscript. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J,
Wang B, Xiang H, Cheng Z, Xiong Y, et al: Clinical characteristics
of 138 hospitalized patients with 2019 novel coronavirus-infected
pneumonia in Wuhan, China. JAMA. 323:1061–1069. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
National Health Commission: Up to 24:00 on
March 10, the latest update on the epidemic situation of
NCP[EB/OL](2020-03-11). (In Chinese). urihttp://www.gov.cn/xinwen/20203/11/content_5489767.htmsimplehttp://www.gov.cn/xinwen/20203/11/content_5489767.htm.
|
|
3
|
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He
JX, Liu L, Shan H, Lei CL, Hui DS, et al: Clinical characteristics
of 2019 novel coronavirus infection in China. medRxiv: Feb 9, 2020
(Epub ahead of print). doi: 10.1101/2020.02.06.20020974.
|
|
4
|
Zhang XT, Wang ZB and Liu WZ: The
theoretical and legal basis for the inclusion of the new
coronavirus pneumonia in the occupational disease classification
catalogue of medical staff. Occup Health Emerg Rescue 38, 2020 (In
Chinese).
|
|
5
|
Chu NJ, Wang J and Jia YD: Protection
against COVID-19 infection among medical staff in designated
hospitals. J Nurs (China). 27:56–60. 2020.(In Chinese).
|
|
6
|
Fu Q, Zhang X and Lishi-Wen : Risk
management strategies for occupational exposure of medical staff
with novel coronavirus infections. Chin J Nosocomiol. 30:801–805.
2020.(In Chinese).
|
|
7
|
National Health Commission: Notice on
issuing COVID-19's diagnosis and treatment Plan (trial Seventh
Edition) [EB/OL]. (2020-03-03). (In Chinese). urihttp://www.gov.cn/zhengce/zhengceku/2020-03/04/content_5486705.htmsimplehttp://www.gov.cn/zhengce/zhengceku/2020-03/04/content_5486705.htm.
|
|
8
|
Holshue ML, DeBolt C, Lindquist S, Lofy
KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural
A, et al: First case of 2019 novel coronavirus in the United
States. N Engl J Med. 382:929–936. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lu CW, Liu XF and Jia ZF: 2019-nCoV
transmission through the ocular surface must not be ignored.
Lancet. 395(e39)2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ma C and Yan XK: Research progress in
psychological stress expression and revention and control strategy
of COVID-19. Journal of Jilin University (Medicine Edition).
46:1–6. 2020.(In Chinese).
|
|
11
|
National Health Commission: Notice of the
general office of the national health commission on the issuance of
technical guidelines for the prevention and control of novel
coronavirus infections in medical institutions (1st edition)
[EB/OL](2020-01-22). (In Chinese). urihttp://www.gov.cn/zhengce/zhengceku/2020-01/23/content_5471857.htmsimplehttp://www.gov.cn/zhengce/zhengceku/2020-01/23/content_5471857.htm.
|
|
12
|
National Health Commission: Guidelines on
the scope of use of common medical protective equipment in the
prevention and control of novel coronavirus infections (trial)
[EB/OL](2020-01-27). (In Chinese). urihttp://www.nhc.gov.cn/xcs/zhengcwj/202001/e71c5de925a64eafbe1ce790debab5c6.shtmlsimplehttp://www.nhc.gov.cn/xcs/zhengcwj/202001/e71c5de925a64eafbe1ce790debab5c6.shtml.
|
|
13
|
Honda H and Iwata K: Personal protective
equipment and improving compliance among healthcare workers in
high-risk settings. Curr Opin Infect Dis. 29:400–406.
2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Yang Y, Li W, Zhang Q, Zhang L, Cheung T
and Xiang YT: Mental health services for older adults in China
during the COVID-19 outbreak. Lancet Psychiatry.
7(e19)2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
National Health Commission: Notice of the
General Office of the National Health Commission on the issuance of
the COVID-19 Prevention and control Programme (4th edition)
[EB/OL](2020-02-06). (In Chinese). urihttp://www.gov.cn/zhengce/zhengceku/2020-02/07/content_5475813.htmsimplehttp://www.gov.cn/zhengce/zhengceku/2020-02/07/content_5475813.htm.
|
|
16
|
Li H, Pan J, Su Y, Wang B and Ge J:
SARS-CoV-2 lgM/lgG antibody detection confirms the infection after
three negative nucleic acid detection. J Cell Mol Med.
24:8262–8265. 2020.PubMed/NCBI View Article : Google Scholar
|