Introduction
Obesity is a common and costly disease, defined as
abnormal or excessive fat accumulation, usually caused by excessive
food intake, genetic susceptibility, and lack of physical activity.
The body mass index or BMI (weight in kilograms divided by the
square of height in meters) is used in clinical practice to
classify adults as overweight (BMI≥25) or obese (BMI≥30) (1).
The World Health Organization (WHO) warns that
obesity has nearly tripled since 1975. Once considered a
high-income country problem, overweight and obesity are now
increasing in low- and middle-income countries, especially in urban
zones. Worldwide, 39% of adults were estimated to be overweight in
2016, and 13% were obese (1).
Obesity in the adult population in Romania was estimated at 9.4% in
2014, compared to a European average of 15.9% (2).
Obesity is a major risk factor for diabetes,
cardiovascular diseases, obstructive sleep apnea, non-alcoholic
fatty liver disease, osteoarthritis, social stigmatization, and
even cancer (1,3,4).
Literature has focused on the connection between
obesity and gastroesophageal reflux disease (GERD), but there are
limited data available on esophageal motility in obese individuals,
and usually on small cohorts of patients (5). Obesity is a potential risk factor for
GERD and the associated complications including erosive
esophagitis, Barrett esophagus, and esophageal adenocarcinoma as
compared to individuals with a normal BMI (6). Few studies in the literature have
examined motility disorders among the morbidly obese population
outside the context of GERD; most of them focusing on the
relationship between lower esophageal sphincter (LES) pressure and
reflux disease (7).
Patients and methods
We performed a prospective study from January 2017
to July 2020, with a cohort of 79 morbidly obese subjects submitted
for vertical laparoscopic gastrectomy who were evaluated with
high-resolution esophageal manometry before the surgical
intervention, additional to upper gastrointestinal tract endoscopy
and clinical assessment (GERD-HRQL questionnaire). The objective
was to better understand the manometric profile of obesity,
especially regarding esophageal peristalsis, LES basal pressure,
and LES relaxation.
This is part of a larger study approved by the
Ethics and Research Committee of the Carol Davila University
Central Emergency Military Hospital Bucharest, designed to observe
and reduce the prevalence of upper gastrointestinal symptoms and
complications after laparoscopic sleeve gastrectomy. All patients
agreed to be included in the study and signed the informed consent.
The study exclusion criteria were: Other bariatric procedures
(surgical or endoscopically), previous gastric surgery, patients
not willing to sign the informed consent, severe bleeding
disorders, inability to tolerate nasal intubation, or esophageal
obstruction preventing passage of the manometric catheter.
High-resolution esophageal manometry is the current
state-of-the-art diagnostic tool to evaluate esophageal motility
(8). The Chicago Classification
version 3.0 is the latest published esophageal motility disorder
classification by The International High-Resolution Manometry
Working Group, based on high-resolution esophageal pressure
topography, and represents the standard interpretation scheme used
in clinical practice (9).
High-resolution esophageal manometry (HRM) was
performed with a 36-channel High-Resolution Solid-State Catheter
Sierra, by a single examiner, after 6 h of fasting and a previous
upper gastrointestinal endoscopy following the standard protocol: a
baseline phase for resting pressure and a series of 10 wet swallows
of 5 ml of water in the supine position with the interval of a
minimum 30 sec between swallows (10). There were no complications during
the exams.
Drugs that may affect esophageal motility were
discontinued for at least 48 h before the examination (nitrates,
calcium channel blockers, antiemetics, prokinetics, H2 blockers,
antidepressants).
HRM data were analyzed according to the Chicago
Classification version 3.0, using the ManoView ESO software program
(a component of the ManoScan system), providing visual images and
quantitative physiological parameters. The manometric data from the
obese cohort focused on analyzing the LES basal pressure, the
deglutitive LES relaxation (residual pressure), esophageal
peristalsis, and contractility pattern.
The GERD-HRQL questionnaire was used as a
quantitative method for measuring symptom severity of GERD in
morbidly obese. The scale has 15 questions concerning heartburn,
regurgitation, pain, and dysphagia; each item is scored from 0 to
5, and the 16th item is a subjective appreciation of the
present clinical condition. The GERD-HRQL is easy and fast, it
takes only a few minutes to complete, and recently is used also to
measure the quality of life of morbidly obese patients (11). The total score was calculated by
summing the individual scores to questions 1-15, with a highest
possible score (worst symptoms) of 75, and lowest possible score 0.
The heartburn score was obtained by summing the individual scores
to questions 1-6, and the regurgitation score summing 10-15
responses; scores of ≤12 with each question not exceeding 2
indicate heartburn or regurgitation elimination (12).
Statistical analysis
Data are presented as a percentage from the total
(%), mean ± standard deviation (range min-max, where applicable).
Statistical analysis was carried out using SPSS Statistics 25 (IBM
Corp.). Descriptive statistics included measures of central
tendency for quantitative variables, counts, and percentages for
categorical variables and corresponding graphs.
Results
In our study population, females were predominant
[55.70% (44/79 patients)], with 2 peaks of age at 45-50 years and
60 years, probably linked to menopause and hormonal changes. For
men, there were also 2 frequency peaks at 35-40 years and another
one at 50 years. The youngest patient was a 19-year of age female,
struggling from childhood with excess fat, who previously tried a
restrictive diet recommended by the nutritional doctor, as well as
physical exercise, and anorexigenic drugs, and currently she was
proposed for bariatric surgery. Unfortunately, obesity is
increasing also in children not only in adults, and most of them
experience social isolation and stigmatization, anxiety, and low
self-esteem (13).
Approximately 3/4 of the patients (78.48%) were from
the urban zone, and the mean BMI was 46.40±6.0069 kg/m2,
with a maximum of 61 kg/m2.
The mean LES basal pressure was 31.40±18.43 mmHg.
The LES basal pressure was normal in 59.49% of the patients; LES
basal hypertonia was observed in 26.58%, and LES hypotonia in
13.93% of the patients. LES hypotonia may predispose to GERD, but
in our cohort, there was no correlation between LES low pressure
and GERD and erosive esophagitis, based on reflux symptomatology
and upper gastrointestinal endoscopy; yet, one study limitation was
the absence of 24-h esophageal pH monitoring.
The mean integrated relaxation pressure (IRP) was
9.75±10.71 mmHg, with a maximum of 38 mmHg. When the IRP value was
high (>15 mmHg according to the Sierra catheter specifications),
we further analyzed the esophageal contractility to establish a
diagnosis of achalasia or esophagogastric junction (EGJ) outflow
obstruction using the Chicago Classification v3.0.
The esophageal contractility was assessed with
distal contractile integral (DCI) expressed in mmHg-sec-cm, which
means amplitude x duration x length of the contractile wave induced
by wet deglutition test. Mean DCI was 2,693.12±1,919.31
mmHg-sec-cm), with a minimum of 249.7 mmHg-sec-cm and a maximum of
9,373.5 mmHg-sec-cm; the normal values admitted for DCI range
between 450 and 8,000 mmHg-sec-cm.
The distal latency (DL) used to identify premature
contraction (value <4.5 sec) had a mean value of 6.38±1.16 sec
(minimum 4.0, maximum of 9.8 sec). When more than 2 swallows are
premature, with normal IRP the diagnose is distal esophageal
spasm.
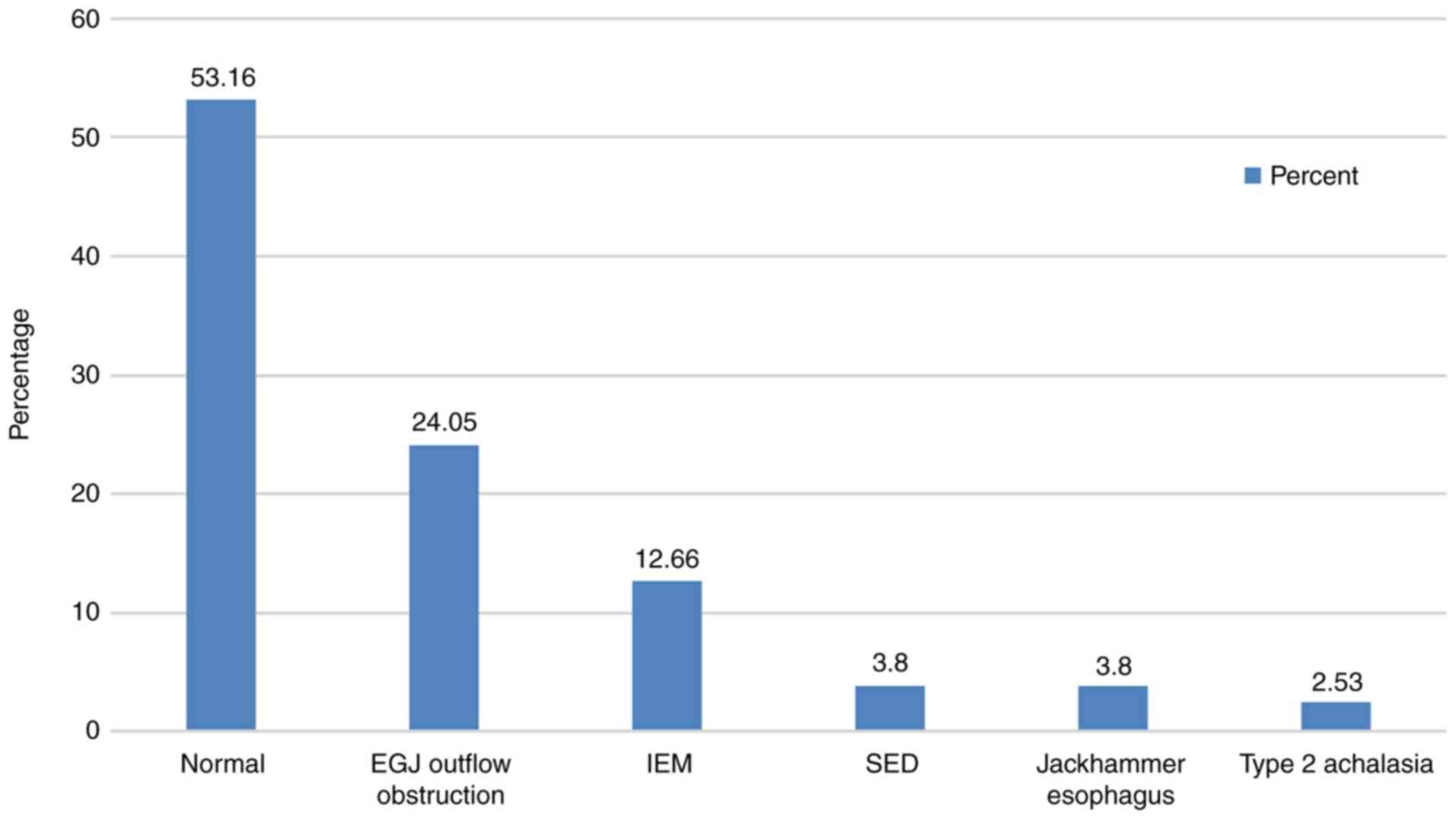
From the obese study group, 46.84% (37/79 patients)
had abnormal manometric findings: 24.05% (19/79 patients) had EGJ
outflow obstruction, 12.66% (10/79 patients) ineffective esophageal
motility (IEM), 3.8% (3 patients) distal esophageal spasm (SED),
3.8% (3 patients) hypercontractile esophagus Jackhammer esophagus,
and 2 cases were suggestive for type 2 achalasia (2.53%) but in
asymptomatic patients (0 points Eckardt score) (Fig. 1). Ineffective esophageal motility
was not associated with diabetes mellitus type 2 or erosive
esophagitis according to our data.
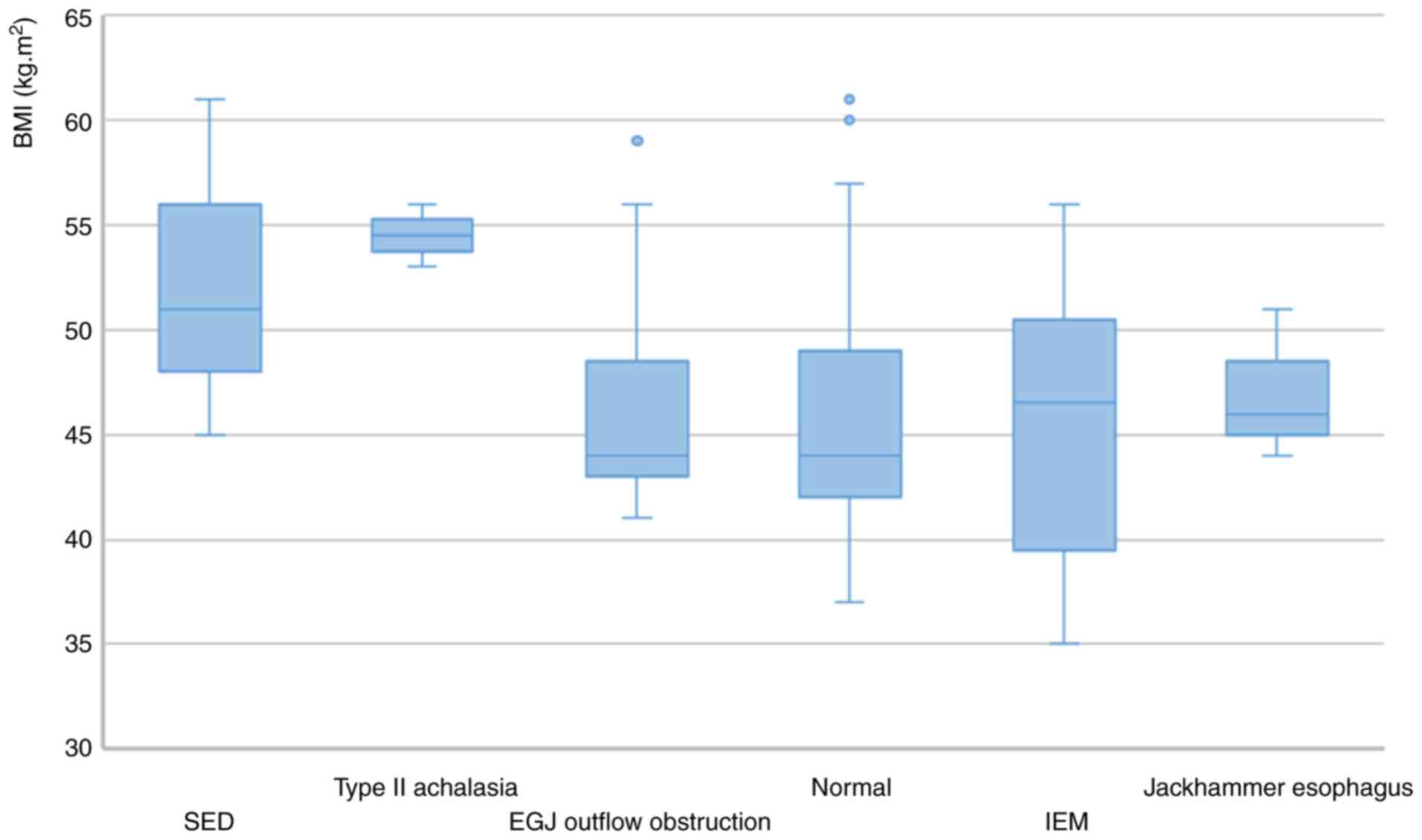
To ascertain whether there is a correlation between
the grade of obesity and specific manometric findings, we analyzed
the BMI values for each manometric diagnosis, and the data that we
obtained are provided in Fig. 2.
Considering the small study cohort, a conclusion on this topic was
difficult. Yet, the research concept can be further materialized as
a research idea in the future, on a larger cohort, to see whether
we can find a model of prediction based on BMI values.
From the total 79 obese patients evaluated for
sleeve gastrectomy, only 6 of them had significant GERD symptoms
(with regurgitation score >12 points, heartburn score >12
points on the GERD-HRQL questionnaire). The heartburn score was
calculable (different from zero) in 19 patients (24.05%), with an
average of 7.89 points; the regurgitation score was similar with an
average of 8.94 points. A positive score for dysphagia (>2
points) was obtained for 3 patients, while for pain 2 patients.
However, 16 patients (20.25%) had erosive esophagitis on upper
gastrointestinal endoscopy (12 grade A and 4 grade B according to
Los Angeles classification), even if only mild reflux symptoms were
present or the patients were asymptomatic. Physiopathologicaly GERD
may be related to the presence of HH, and in our obese group, the
prevalence pof HH was high (29.11%).
Discussion
The present study aimed to determine the manometric
pattern and the prevalence of esophageal dysmotility in morbidly
obese patients. In our obese study population, we observed a female
predominance and high frequency in the five decades of life in both
female and male groups. In additon, the patients were predominantly
from urban regions, in accordance with the literature due to
fast-food consumption, a high-calorie diet, and lack of physical
exercise (14).
The prevalence of manometric abnormalities in the
morbidly obese population was high and included LES basal pressure
alteration, trouble in LES relaxation, disturbance in esophageal
body contractility (ineffective esophageal motility,
hypercontractile esophagus, distal esophageal spasm); yet, the
patients were mostly asymptomatic, thus this may be an accidental
finding or support to the idea that morbidly obese patients may
have abnormal visceral sensation-not always a predictor of the post
gastrectomy evolution (15).
It is known that obese people are predisposed to
GERD (16), HH being one of the
risk factors (17). HH is usually
more frequent in obese individuals because of pressure modification
at the LES due to increased intraabdominal pressure and visceral
fat (18). HH was manometrically
diagnosed in 23 obese patients (29.11%); 16 patients had erosive
esophagitis on upper GI tract endoscopy, although only 6 patients
had significant GERD symptoms on the GERD-HRQL questionnaire. This
might be explained by a high sensitivity threshold of obese to GERD
symptoms. One study limitation is the absence of 24-h esophageal pH
monitoring. The presence of HH is not a contraindication for
laparoscopic sleeve gastrectomy, but it is recommended to be
repaired in the same surgical intervention (19).
Esophageal manometry remains an important tool for
the study of LES continence and esophageal body function and should
be implemented in the evaluation of morbidly obese patients before
bariatric surgery, at least in patients with reflux symptoms or
esophagitis (20). If a patient
presents reflux symptoms and manometry confirms an incompetent LES,
sleeve gastrectomy is probably not the best option and Roux-en-Y
gastric bypass might be a better choice (19). By assessing esophageal motility,
high-resolution manometry helps to select those patients who could
develop postoperative esophageal motor complications (21).
Acknowledgements
Not applicable.
Funding
Funding: No funding was received for preparation of this
article.
Availability of data and materials
Additional information concerning the present study
is available from the corresponding author upon reasonable
request.
Authors' contributions
ALP performed the examination, and was responsible
for the conception and design of the work, and writing of the first
draft. RSC was responsible for data acquisition, analysis, and
interpretation of data. DOC was responsible acquisition, analysis,
interpretation of data for the work, and verifying the final draft.
VDB performed the statistical analysis. MJ carried out the critical
revision for important intellectual content. FIR was responsible
for conception and design of the work. AC was responsible for
acquisition, analysis, interpretation of data for the work. CFB
carried out the final check for all the data and the final approval
of the version to be published. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
This is part of a larger study approved by the
Ethics and Research Committee of the ‘Carol Davila’ University
Central Emergency Military Hospital Bucharest. All patients agreed
to be included in the study and signed the informed consent. All
patients agreed to be included in the study and signed the informed
consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
World Health Organization: Obesity and
overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
Acecessed April 1, 2020.
|
|
2
|
Popa AR, Fratila O, Rus M, Aron RA, Vesa
CM, Pantis C, Diaconu CC, Bratu O, Bungau S and Nemeth S: Risk
factors for adiposity in the urban population and influence on the
prevalence of overweight and obesity. Exp Ther Med. 20:129–133.
2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Zaha DC, Vesa C, Uivarosan D, Bratu O,
Fratila O, Tit DM, Pantis C, Diaconu CC and Bungau S: Influence of
inflammation and adipocyte biochemical markers on the components of
metabolic syndrome. Exp Ther Med. 20:121–128. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Eurostat: European Health Interview
Survey: Almost 1 adult in 6 in the EU is considered obese. Share of
obesity increases with age and decreases with education level. 203,
2016. https://ec.europa.
eu/eurostat/documents/2995521/7700898/3-20102016-BP-EN.pdf/c26b037b-d5f3-4c05-89c1-00bf0b98d646.
Accessed October 20, 2016.
|
|
5
|
Corley DA and Kubo A: Body mass index and
gastroesophageal reflux disease: A systematic review and
meta-analysis. Am J Gastroenterol. 101:2619–2628. 2006.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Hampel H, Abraham NS and El-Serag HB:
Meta-Analysis: Obesity and the risk for gastroesophageal reflux
disease and its complications. Ann Intern Med. 143:199–211.
2005.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Koppman J, Poggi L, Szomstein S, Ukleja A,
Botoman A and Rosenthal R: Esophageal motility disorders in the
morbidly obese population. Surg Endosc. 21:761–764. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Yadlapati R: High-Resolution esophageal
manometry: Interpretation in clinical practice. Curr Opin
Gastroenterol. 33:301–309. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Bredenoord AJ, Fox M, Kahrilas PJ,
Pandolfino JE, Schwizer W and Smout AJ: International High
Resolution Manometry Working Group. Chicago classification criteria
of esophageal motility disorders defined in high resolution
esophageal pressure topography (EPT). Neurogastroenterol Motil.
24:57–65. 2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Weingart V, Lambertz J and Allescher HD:
High-Resolution manometry of the esophagus - Pictorial Atlas and
Textbook. Standard Light GmbH, 2012-2013.
|
|
11
|
Guan XL and Wang H: Quality of life scales
for patients with gastroesophageal reflux disease: A literature
review. Int Journal of Nursing Sciences. 2:110–114. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hunter JG, Trus TL, Branum GD, Waring JP
and Wood WC: A physiologic approach to laparoscopic fundoplication
for gastroesophageal reflux disease. Ann Surg. 223:673–685.
1996.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Puhl RM and Heuer CA: Obesity stigma:
Important considerations for public health. Am J Public Health.
100:1019–1028. 2010.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Nurwanti E, Hadi H, Chang JS, Chao JJ,
Paramashanti BA, Gittelsohn J and Bai CH: Rural-Urban differences
in dietary behavior and obesity: Results of the riskesdas study in
10-18-year-old Indonesian children and adolescents. Nutrients.
11(2813)2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Jaffin BW, Knoepflmacher P and Greenstein
R: High prevalence of asymptomatic esophageal motility disorders
among morbidly obese patients. Obes Surg. 9:390–395.
1999.PubMed/NCBI View Article : Google Scholar
|
|
16
|
El-Serag H: The association between
obesity and GERD: A review of the epidemiological evidence. Dig Dis
Sci. 53:2307–2312. 2008.PubMed/NCBI View Article : Google Scholar
|
|
17
|
El-Serag HB, Graham DY, Satia JA and
Rabeneck L: Obesity is an independent risk factor for GERD symptoms
and erosive esophagitis. Am J Gastroenterol. 100:1243–1250.
2005.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Khan A, Kim A, Sanossian C and Francois F:
Impact of obesity treatment on gastroesophageal reflux disease.
World J Gastroenterol. 22:1627–1638. 2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Garg H, Vigneshwaran B, Aggarwal S and
Ahuja V: Impact of concomitant laparoscopic sleeve gastrectomy and
hiatal hernia repair on gastro-oesophageal reflux disease in
morbidly obese patients. J Minim Access Surg. 13:103–108.
2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Braghetto I, Lanzarini E, Korn O,
Valladares H, Molina JC and Henriquez A: Manometric changes of the
lower esophageal sphincter after sleeve gastrectomy in obese
patients. Obes Surg. 20:357–362. 2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Popescu AL, Costache RS, Bucurica S,
Patrasescu M, Balaban VD, Savulescu FA, Jinga M, Ionita-Radu F and
Fierbinteanu-Braticevici C: Laparoscopic sleeve gastrectomy and
esophageal motility. Rom J Mil Med. 128:190–195. 2020.
|