Introduction
Since the lower limb is not aligned with the
anatomical axis of the tibia, the inner side of the tibial plateau
is loaded with 70% of the knee joint; the bone is hard and most of
the fractures involved in the medial platform are large condyle
cleavages or collapses (1). Tibial
plateau fractures are closely related to the injury mechanism, and
for its classification, Schatzker typing, Moore typing,
Arbeitsgemeinschaftfür Osteosynthesefragen/Orthopaedic Trauma
Association (AO/OTA) typing, three-column typing and fixation
theory are most widely accepted (2-5).
The correct understanding of the injury mechanism may effectively
guide intra-operative reduction, enabling the accurate choice of
type, location and direction of internal fixators, which is crucial
for fracture prognosis (4,6,7). At
present, 69% of Schatzker IV fractures are posterior coronal
fractures (8), for which the
mechanism of injury is mostly caused by flexion internal force.
Thus, research on typing and subtypes of Schatzker IV type
fractures is intensive (9,10) and there are numerous treatment
methods (11-13).
However, clinical reports on the typing and treatment of extended
tibial plateau fractures are rare (14,15).
Extended tibial plateau fractures cannot be fully explained by
Schatzker typing, Moore typing or AO/OTA typing (16); therefore, these fractures have been
named hyperextension varus bicondylar tibial plateau (HEVBTP)
fractures, the characteristics of which are as follows: Loss of
posterior slope angle (PSA), a posterior cortical tension fracture,
compression of the anterior bone and varus deformity. Fractures of
the tibial plateau are caused by extension or hyperextension,
combined with a force on the varus. The medial column is the side
subjected to pressure, which means that it bears the impact of the
internal condyle of the femur. When subjected to strong forces,
comminuted fracture blocks of the medial and medial anterior border
often occur and the articular surface may be compressed leading to
its collapse; therefore, this type of fracture may involve the
posterior column and even a three-column comminuted fracture. The
articular surface features a backward inclination and may even turn
to a forward tilt, and the medial meniscus is squeezed and may be
damaged or torn. The lateral and posterolateral structure is the
tension side, frequently complicating lateral collateral ligament
or posterolateral complex injury and posterior cruciate ligament
injury (17-20).
As a special type of fracture, tibial plateau
fractures involving the anteromedial margin caused by a
hyperextension varus injury in a clinical setting have rarely been
reported in the literature (16).
This type of fracture is usually caused by serious, violent injury
and is characteristic of endangering the medial column, posterior
column or even the three columns of the tibial plateau, which
complicate the injury of the medial and lateral meniscus,
posterolateral complex and posterior cruciate ligament (14,21).
The key to surgical treatment of tibial plateau fractures involving
the anteromedial margin caused by a hyperextension varus injury is
the accurate reduction of the posterior cortex and the effective
support and fixation of the anterior compression bone, particularly
the reduction and strong fixation of the anteromedial comminuted
bone, which is a difficulty for the treatment of this type of
fracture. If the treatment is improper, it inevitably results in
loss of reduction, thus affecting the stability of fixation and
increasing the incidence of complications. From January 2015 to
June 2017, 27 patients with tibial plateau fractures caused by
hyperextension varus were treated with a self-clipped joint line
plate at Puai Hospital, Tongji Medical College (Wuhan, China).
Among the 27 patients, 2 were lost to follow-up, and 25 had
complete patient data and recovered well throughout the follow-up.
In the present study, a retrospective analysis of the 25 patients
is provided.
Materials and methods
Subjects
The inclusion criteria were as follows: i) Adult
patients with fresh, closed fractures; ii) patients diagnosed as
having a tibial plateau fracture involving the anteromedial margin
caused by a hyperextension varus injury by X-ray films and CT; iii)
patients with normal knee joint motion prior to injury; and iv)
patients with no severe vascular or nerve injuries. Patients with
open fracture, pathological fracture, severe vascular or nerve
injury or complicating osteofascial compartment syndrome were
excluded from the study.
A total of 25 patients were included in the present
study, comprising 13 males and 12 females, aged between 19 and 71
years with a mean age of 45.2 years. All patients had closed
fractures, although 2 patients had fractures with other complicated
parts. The average time from injury to internal fixation was 10.7
days (range, 5 to 17 days). The causes of injury were as follows:
Motor vehicle collision (n=6 cases), high-fall injury (fall from
over standing height, n=5), fall from an electric bicycle (n=9),
fall from a bicycle (n=3) and fall injury (fall from standing
height or less, n=2). The patients' classification based on the
three-column theory was as follows (22): Simple medial column fracture (n=4
cases), fracture of the medial and lateral columns (n=5), fracture
of the medial and posterior columns (n=9) and three-column
fractures (n=7). The classification based on AO/OTA was as follows:
B2.3 (n=4 cases), B3.2 (n=9), C2.3 (n=8) and C3.3 (n=4). The basic
characteristics of the patients are presented in Table SI.
Patients with simple medial column fractures were
treated with a plaster cast prior to the operation and the other
patients were treated with calcaneal traction. All patients
received routine pre-operative swelling treatment and prevention of
deep venous thrombosis of the lower extremities. Pre-operative
three-dimensional CT and MRI examinations were performed to assess
the extent of fracture displacement and comminution, and to assess
ligament and meniscus injury. The blood circulation and
sensory-motor function of the lower limbs was closely monitored
prior to the operation.
The surgical incision types were as follows: Simple
anteromedial incision (n=4 cases); simple posterior medial incision
(n=7); anteromedial and backside inverted ‘L’ incision (n=2);
anterolateral and posterior medial incision (n=10); anterolateral
and backside inverted ‘L’ incision (n=1); and anterolateral and
anteromedial, as well as backside inverted ‘L’ incision (n=1). All
25 patients received a bone graft during the operation, including
autologous iliac bone grafts (n=6 cases), allograft bone grafts
(n=17) and artificial bone grafts, using hydroxyapatite material
(n=2).
Surgical methods
Prior to the operation, proper posture selection,
surgical approach and reset order were carefully planned and
chosen. The supine position was used for patients who required an
anteromedial approach, posterior medial approach or a conventional
internal and external combined approach. The prone position was
taken first after the posterior side inverted ‘L’ incision was
performed. After the internal column and the posterior column were
fixed, the position was changed to a supine position. The
anteromedial and/or anterolateral incision was used to reset and
fix the anteromedial fracture block and the lateral column. For
patients with complex, three-column fractures, the floating
position may be used to observe the intra-operative reduction.
After exposure, the internal and external condyle fractures were
opened and the meniscus was exposed when the knee joint was turned
outward. In reference to pre-operative routine MRI examination, if
there was a meniscus injury, absorbable sutures were first used to
repair the injury. There were 2 cases in which the medial meniscus
margins had a vertical radial rupture and 4 cases in which the
lateral meniscus margins had a vertical longitudinal rupture; all
meniscus ruptures were repaired with absorbable sutures. During
meniscus repair, it is possible to evaluate the height and shape of
the tibial plateau articular surface, which is conducive to the
anatomical reduction of tibial plateau fractures.
The collapsed articular surface was restored using
tools of the periosteum, the top bar was placed through the
fractured window and a bone allograft, autogenous bone or
artificial bone graft was implanted at the collapse site. When the
articular surface was satisfactorily restored, the Kirschner wire
was temporarily fixed to the subchondral bone. After the fixation
was confirmed by the C-arm X-ray machine, proper internal fixation
materials were selected. The rebuilt titanium plate, 1/3 tube
plate, rebuilt titanium locking plate or 3.5 mm proximal tibia
plate (PTP) titanium plate were clipped in accordance with the
prebending of the medial tibia to form the joint line plate, which
was then fixed to the anteromedial margin of the tibia plateau.
According to the fracture conditions, combined with other internal
fixation materials, such as the proximal tibial T-type locking
titanium plate, the distal radius T-type titanium plate, the PTP
titanium plate and the reconstruction titanium plate, final
fixation was completed. For unstable bone fragments involving
articular surface fixation, small hollow lag screws or absorbable
sutures may be used for the fix. After the bone structure was
fixed, the stability of the knee joint ligament was examined. In 2
cases in which an avulsion fracture at the insertion point of the
posterior cruciate occurred, the ligaments were fixed with hollow
screws after reduction. In 4 cases in which the lateral collateral
ligament was avulsed from the fibular head, exposing the fibula
capitulum through the lateral incision, wire anchors were placed
and the avulsion was repaired by suture. No medial collateral
ligament, anterior cruciate ligament or posterior cruciate ligament
rupture were identified in any of the patients. The wound drainage
tube was routinely retained after the operation.
Post-operative treatment and
follow-up
All patients were treated with a cotton pad to
bandage the wound to reduce bleeding after the operation. At the
same time, the affected limb was raised to reduce wound and limb
swelling. Low-molecular-weight heparin was administered 12 h after
the operation to prevent deep vein thrombosis of the lower limb.
After 48 h, the wound drainage tube was removed and knee joint
flexion and extension function exercises were performed under the
protection of braces.
All patients underwent examination immediately after
the operation and at 3, 6 and 12 months after the operation. The
healing time of the fracture was judged by X-ray and clinical
examination, and the time of full weight-bearing walking was
recorded. Any complications after the operation and during
follow-up were recorded. Due to the medial tibial plateau bearing
most of the load of the knee joint, if the fracture block of the
anteromedial platform was seriously crushed, the time of partial
weight load was postponed accordingly. It may be suggested that the
patient should be supported for up to 3 months after the operation.
The time-point of full-weight load-bearing was finally determined
by X-ray according to the degree of fracture grinding and the
healing conditions.
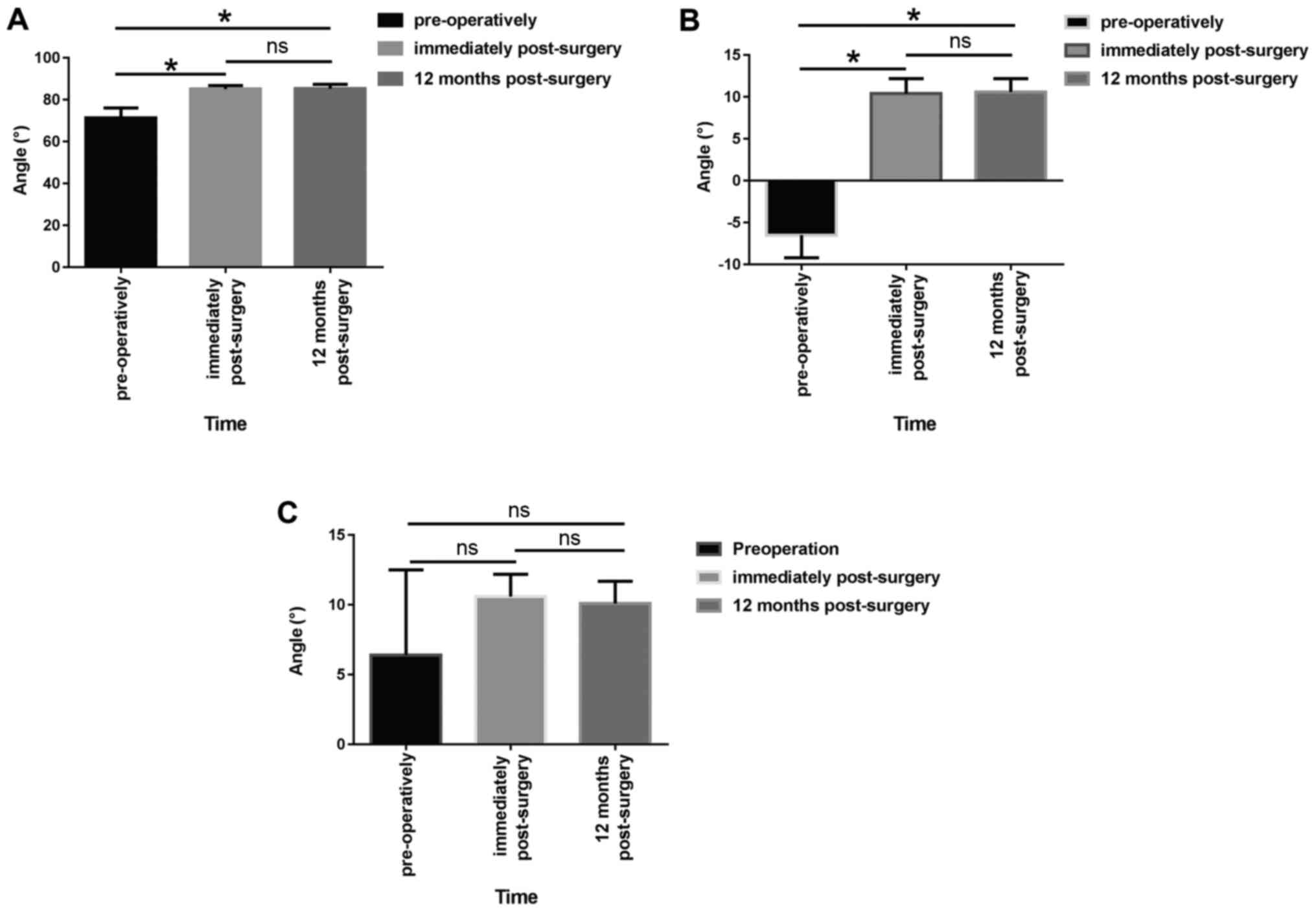
The tibial plateau angle (TPA) and PSA were measured
by X-ray. The TPA and PSA of the tibial plateau prior to operation,
immediately after operation and 12 months after the operation were
compared. Knee joint function of the affected limb was measured 12
months after the operation and was evaluated according to the knee
joint Hospital for Special Surgery (HSS) standard score (23).
Statistical analysis
The statistical software SPSS 19.0 (IBM, Corp.) was
used for statistical analyses. First, the Shapiro-Wilk test was
used to determine whether the measurement data had a normal
distribution. The tibial plateau TPA, the medial PSA (m-PSA) and
the lateral PSA (l-PSA) had normal distribution data, and the
variance was homogeneous; therefore, values were expressed as the
mean ± standard deviation. Comparisons of the tibial plateau TPA
and PSA prior to the operation, immediately after the operation and
12 months after the operation were analyzed by repeated-measures
ANOVA with further pairwise comparisons by the least-significant
difference t-test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Status of fracture healing after the
operation
The 25 patients were followed up for an average of
17.6 months (range, 12-30 months) and it was found that all
fractures had healed. X-ray films revealed that 20 cases achieved
anatomical reduction and 3 cases had articular surface collapse by
<2 mm. The average operation time was 48 min (range, 25-120 min)
and the average blood loss during the operation was 110 ml (range,
15-250 ml). The mean Rasmussen score immediately after the
operation was 15.6 points (range, 12-18 points). Fracture healing
was achieved in all 25 patients. The average time of healing and
full weight-bearing was 12.1 weeks (range, 8-14 weeks) and 15.8
weeks (range, 13-20 weeks), respectively. The HSS scores of all the
patients at 12 months post-operatively averaged 87.6 (range,
68-96), yielding an excellent to good rate of 91.5%. The average
range of motion of the affected knee ranged from 2.3˚ to 125.1˚ 12
months after the operation. The data of the status of fracture
healing after the operation are presented in Table SI.
TPA and posterior slope angle of the
tibial plateau prior to operation and after the operation
The tibial plateau TPA and m-PSA immediately as well
as 12 months after the operation were significantly different from
those prior to the operation (P<0.05; Fig. 1A and B). However, there was no significant
difference in the TPA and m-PSA between the stage immediately after
the operation and 12 months after the operation (P>0.05;
Fig. 1A and B). No significant difference was present
in the pre-operative l-PSA between the stage immediately after the
operation and 12 months after the operation (P>0.05; Fig. 1C). Partial incision necrosis
occurred post-operatively in 1 case, which uneventfully healed
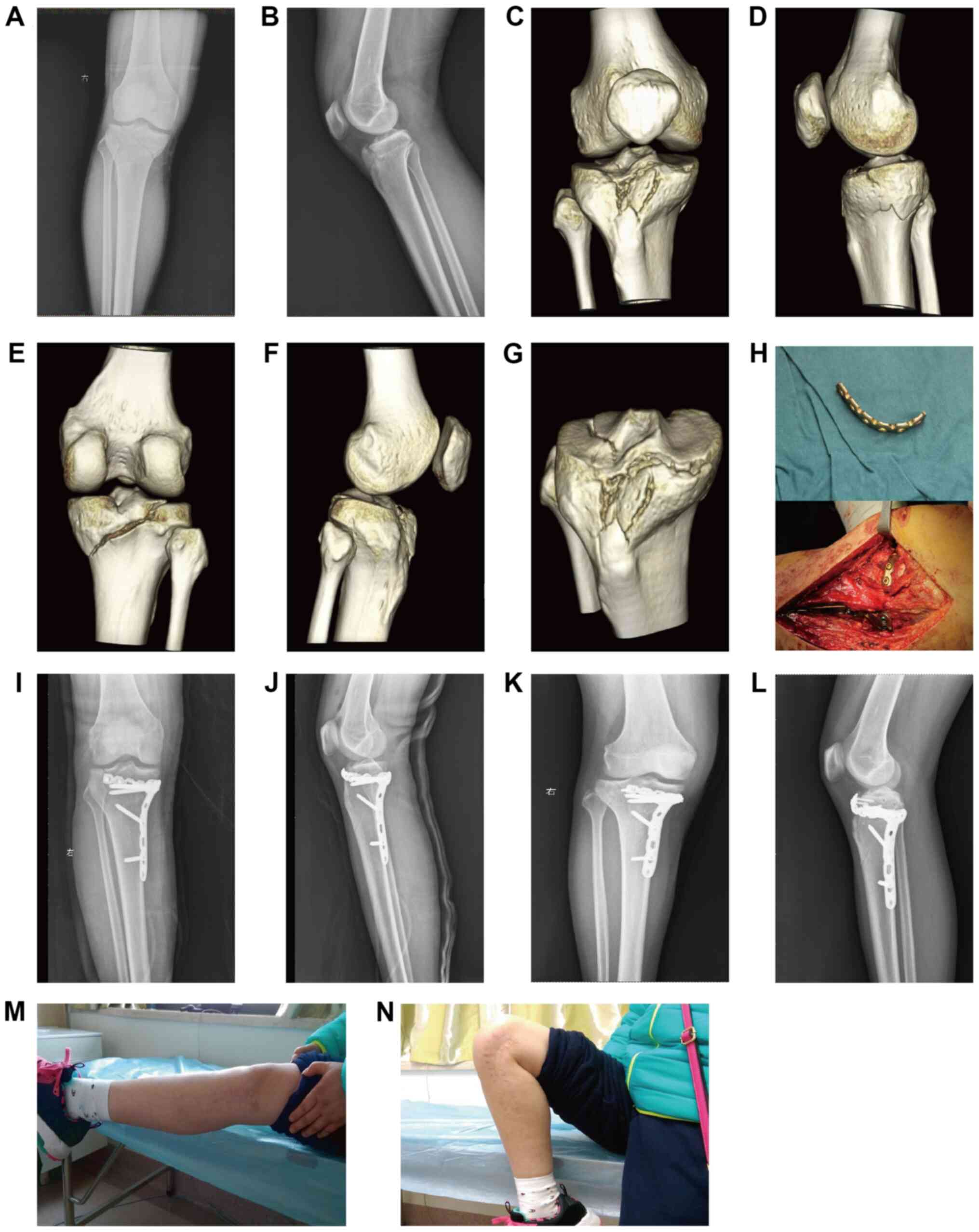
after wound management. Typically, the fractures of a 19-year-old
male with hyperextension varus of tibial plateau fractures
(Schatzker V type) caused by a motor vehicle collision (Fig. 2) and a 33-year-old female with
hyperextension varus of tibial plateau fractures (Schatzker V type)
caused by a high-fall injury (Fig.
3) both were healed, and there was no loss of reduction at 12
months post-surgery. In addition, there were 2 cases complicated
with pre-operative common peroneal nerve injury reported with a
dorsal sense of numbness, which healed after 3 months of
neurotrophic drug administration. No screw loosening, plate
breakage or fixation failure was detected during follow-up.
Discussion
Internal fixation materials commonly used for
clinical medial platform repairs, such as 3.5 or 4.5 mm locking
titanium plates or reconstruction titanium plates cannot be fixed
to the anteromedial margin and cannot form a strong support and
fixation for the broken fracture block of the anteromedial cortex
due to the limited coverage or support area (24-27).
In particular, cases in which the anteromedial cortical bone
fracture extends to the anterolateral side, resulting in the
overall comminuted collapse of the tibial plateau, are lacking
effective fixation, which inevitably results in inadequate
elevation of the medial articular surface of the medial platform,
insufficient recovery of the obliquity, loss of later reduction,
failure of internal fixation, impairment of the stability of knee
joint and an increase in the incidence of complications (28). Therefore, internal fixation and
material selection for anteromedial cortical bone comminuted
fractures are difficult and clinical reports are currently sparse.
As an example, Firoozabadi et al (16) placed 3.5 mm medial T-locking
titanium plates in the anteromedial side as the main supporting
plate, but only to fix the entire medial condyle bone block. As for
a comminuted fracture involving the joint margin, scholars
worldwide have attempted to use various types of internal fixation.
Giordano et al (29) applied
a 1/3 tubular steel plate preflexion and transverse fixation to the
posterior lateral joint in comminuted fractures of the
posterolateral joint margin of the tibial plateau and called it
‘hoop plating’. Lv et al (30) used a 2.4-mm radial distal locking
plate for the treatment of a posterior lateral collapse fracture of
the tibial plateau. The plate was placed closely to the articular
surface, which achieved a satisfactory clinical effect. However,
the 2.4 or 2.7 mm radial distal plate system has low strength and
small coverage, is mostly used for the internal fixation of upper
limb fractures and is not reported for the treatment of comminuted
fractures of the medial tibial medial cortex.
In the present study, the concept of the
circumference line steel plate was proposed: The shape of the
internal fixation material is an arc, semi-ring or even a ring
fixed to the articular cartilage along the joint edge to fix the
broken fracture block. The idea is to fix the comminuted fracture
blocks to the main fracture block or other stable fracture blocks
of the joint surface to form the whole condyle. Through its own
metaphyseal support or other metaphyseal plate bridging, the
condyle was fixed to the diaphysis. At the same time, the plate was
fixed to the anteromedial margin and the screw was located below
the articular surface, particularly with the angle stability of the
locking plate, forming ‘bamboo raft fixation’ technology and the
cross fixation technique for the articular cartilage, which may
provide a powerful mechanical support for the formation of the
comminuted fracture blocks of the anteromedial margin (31).
Giordano et al (29) proposed that the ‘hoop plate’ may
also be used for the joint edge, which may appear the same as the
concept of the joint line plate of the present study, but actually
it is not. The hoop plate is used to treat posterior condyle
fractures of the tibial plateau, of which the 1/3 tube plate is
pre-bent to the posterior side of the tibial plateau to strengthen
the effect of a ‘buttress plate’, meaning that ‘hoop plates’ only
have a fixed function as the collar. The joint line plate is also
placed on the joint edge in the present study of the anteromedial
tibial plateau joint and may also be used for other parts of the
fracture. At the same time, the idea of the joint line plate in
fixing bone fragments of the joint edge is emphasized, similar to
the ‘hoop plate’ or locking plate, which exerts the angle
stabilizing effect of locking screws to form a ‘bamboo raft
fixation’ effect, having a supporting function on the metaphyseal.
At present, there is no such specialized type of joint line plate
used for the anteromedial margin of the tibial plateau. In the
present study, a self-clipped joint line plate was made based on
the size and position of the fracture blocks, including the use of
reconstruction titanium plates (n=6 cases), 1/3 tube type steel
plate fixation (n=5), reconstruction locking plate fixation (n=10)
and a 3.5-mm system PTP titanium plate fixation (n=4). Among the 25
patients included in the follow-up, 20 cases achieved anatomical
reduction and the tibial plateau TPA and PSA recovered
satisfactorily after the operation. At one year after the
operation, the tibial plateau TPA, m-PSA and l-PSA exhibited no
significant changes from the angles immediately after the surgery
and the reduction was not lost. It was proven that with the
fixation of the medial supporting plate, the self-clipped joint
plate was able to meet the requirements of the early functional
exercise of the affected limb and the recovery of the knee joint
function was satisfactory after the operation.
During the operation, the height of the anteromedial
platform fracture should be fully restored, along with the TPA and
PSA, and may be compared with that of healthy limbs. It is crucial
that the bone graft in the bone defect area is sufficient. If there
are certain defects, it is suggested that an autogenous iliac bone
graft may be used, with the advantages of having powerful support,
effects of good bone formation, bone induction and conduction, and
fastening of the fracture during healing (32). During the operation, the medial
collateral ligament, the ‘goose foot’ and other medial stable
structures should be protected to avoid post-operative instability
of the knee joint (33). When
prebending the joint line plate, the plate should be closely
adhered to the bone to reduce irritation to the skin and soft
tissue and the influence of the flexion activity of the knee joint
after the operation. During the operation, if it is necessary to
reduce the dissection of the soft tissue around the incision, the
use of an electric knife and clamping the edge of the skin should
be avoided in order to reduce complications such as incision fat
liquefaction, skin necrosis or wound infection. There may be a
posterolateral complex injury in this type of fracture and
particularly the lateral collateral ligament may be torn or the
fibular head may have an avulsion fracture. Internal and external
stress tests should be performed after the internal fixation of the
intraoperative fracture reduction, the stability of the lateral
collateral ligament should be checked and one-stage surgical repair
should be performed if necessary (34).
Deficits of the present study are that the number of
cases with the application of the joint line plate was limited and
the follow-up time was relatively short. Further studies with more
cases and further follow-up observations are required to acquire
more accurate clinical treatment results. In addition, the
self-clipped joint line plate has no supporting functions on the
epiphysis, which is necessary to cooperate with other internal
fixation materials to complete the final fixation. Therefore,
according to the idea of joint line plating, it is esteemed to
develop an anatomic type of joint line plating to meet clinical
requirements.
Supplementary Material
Baseline characteristics of the
patients.
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by grants from the Health and
Family Planning Commission of Wuhan City for Clinical Medicine
Research Project (grant no. WX16D27).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YCH performed the experiments, analyzed the data and
wrote the paper; JJ contributed to the conception of the study;
WJC, FX and WZ participated in the execution of the experiment; JWW
contributed to analysis and manuscript preparation. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the ethics committee of
the Wuhan Fourth Hospital, Puai Hospital, Tongji Medical College,
Huazhong University of Science and Technology (Wuhan, China). All
patients provided written informed consent.
Patient consent for publication
All patients agreed to publish their images and
scans.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Duan KD and Huang JR: Progress in
diagnosis and treatment of posterior condylar fracture of tibial
plateau. Zhongguo Gu Shang. 32:1173–1176. 2019.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
2
|
Lowe DT, Milone MT, Gonzalez LJ and Egol
KA: Repair of tibial plateau fracture (Schatzker II). JBJS Essent
Surg Tech. 9(e25)2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kfuri M and Schatzker J: Revisiting the
Schatzker classification of tibial plateau fractures. Injury.
49:2252–2263. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Zhang BB, Sun H, Zhan Y, He QF, Zhu Y,
Wang YK and Luo CF: Reliability and repeatability of tibial plateau
fracture assessment with an injury mechanism-based concept. Bone
Joint Res. 8:357–366. 2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ramponi DR and McSwigan T: Tibial plateau
fractures. Adv Emerg Nurs J. 40:155–161. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Graham P: Tibial plateau fracture. Orthop
Nurs. 36:303–305. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Lu C, Ye G, Liu W, Wu H, Wu G and Chen J:
Tibial plateau fracture related to unicompartmental knee
arthroplasty: Two case reports and literature review. Medicine
(Baltimore). 98(e17338)2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Chang SM, Zhang YQ, Yao MW, Du SC, Li Q
and Guo Z: Schatzker type IV medial tibial plateau fractures: A
computed tomography-based morphological subclassification.
Orthopedics. 37:e699–e706. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Chang SM, Hu SJ, Zhang YQ, Yao MW, Ma Z,
Wang X, Dargel J and Eysel P: A surgical protocol for bicondylar
four-quadrant tibial plateau fractures. Int Orthop. 38:2559–2564.
2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Yan B, Yin W, Zhang X, Liu D, Gui K, Sun
J, Chen Y and Ni M: Effectiveness analysis of surgical treatment of
Schatzker type tibial plateau fractures. Zhongguo Xiu Fu Chong Jian
Wai Ke Za Zhi. 31:1305–1310. 2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
11
|
Cherney S and Gardner MJ: Bicondylar
tibial plateau fractures: Assessing and treating the medial
fragment. J Knee Surg. 27:39–45. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
He X, Ye P, Hu Y, Huang L, Zhang F, Liu G,
Ruan Y and Luo C: A posterior inverted L-shaped approach for the
treatment of posterior bicondylar tibial plateau fractures. Arch
Orthop Trauma Surg. 133:23–28. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lu KH, Lu EW, Lin CW, Yang JS and Yang SF:
New insights into molecular and cellular mechanisms of zoledronate
in human osteosarcoma. Pharmacol Ther. 214(107611)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kołodziejczyk K, Kuliński K, Fedorowicz K,
Langner M, Czubak J and Pomianowski S: Difficulties in treating
complex knee injuries with fracture of posterior tibial plateau.
Ortop Traumatol Rehabil. 20:293–300. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Yang X, Xu F, Yin Z and Wang Q: Clinical
observation of 3.5 mm T support plate fixation for simple
posterolateral tibial plateau fracture by posterolateral inverted
L-shaped approach. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi.
31:815–819. 2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
16
|
Firoozabadi R, Schneidkraut J, Beingessner
D, Dunbar R and Barei D: Hyperextension varus bicondylar tibial
plateau fracture pattern: Diagnosis and treatment strategies. J
Orthop Trauma. 30:e152–e157. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Cohen AP, King D and Gibbon AJ:
Impingement fracture of the anteromedial tibial margin: A
radiographic sign of combined posterolateral complex and posterior
cruciate ligament disruption. Skeletal Radiol. 30:114–116.
2001.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Bennett DL, George MJ, El-Khoury GY,
Stanley MD and Sundaram M: Anterior rim tibial plateau fractures
and posterolateral corner knee injury. Emerg Radiol. 10:76–83.
2003.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Chiba T, Sugita T, Onuma M, Kawamata T and
Umehara J: Injuries to the posterolateral aspect of the knee
accompanied by compression fracture of the anterior part of the
medial tibial plateau. Arthroscopy. 17:642–647. 2001.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Yoo JH, Kim EH, Yim SJ and Lee BI: A case
of compression fracture of medial tibial plateau and medial femoral
condyle combined with posterior cruciate ligament and
posterolateral corner injury. Knee. 16:83–86. 2009.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Hong F, Wang N and Chen GJ: Posterior
medial approach inverted L-shaped incision combined with
reconstruction plate for posterior condylar fracture of tibial
plateau. Zhongguo Gu Shang. 29:1027–1032. 2016.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
22
|
Luo CF, Sun H, Zhang B and Zeng BF:
Three-column fixation for complex tibial plateau fractures. J
Orthop Trauma. 24(683)2010.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Insall JN, Ranawat CS, Aglietti P and
Shine J: A comparison of four models of total knee-replacement
prostheses. J Bone Joint Surg Am. 58:754–65. 1976.PubMed/NCBI
|
|
24
|
Dreyfuss D, Allon R, Izacson N and Hutt D:
A Comparison of locking plates and intramedullary pinning for
fixation of metacarpal shaft fractures. Hand (NY). 14:27–33.
2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Wu CM, Chen YA, Liao HT, Chen CH, Pan CH
and Chen CT: Surgical treatment of isolated zygomatic fracture:
Outcome comparison between titanium plate and bioabsorbable plate.
Asian J Surg. 41:370–376. 2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Darrow BG, Weigel JP, Greenacre CB, Xie X,
Liaw PK and Biskup JJ: Ex vivo biomechanical comparison of titanium
locking plate, stainless steel nonlocking plate, and Tie-in
external fixator applied by a dorsal approach on ostectomized
humeri of pigeons (Columba livia). J Avian Med Surg.
33:29–37. 2019.PubMed/NCBI View
Article : Google Scholar
|
|
27
|
Schliemann B, Seifert R, Theisen C,
Gehweiler D, Wähnert D, Schulze M, Raschke MJ and Weimann A: PEEK
versus titanium locking plates for proximal humerus fracture
fixation: A comparative biomechanical study in two- and three-part
fractures. Arch Orthop Trauma Surg. 137:63–71. 2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Maeda H, Noguchi M, Suehiro M, Mihara E
and Chou Z: Analysis of surgical treatment results in patients with
tibial plateau fractures. Orthoped Traumatol. 42:805–809. 2010.
|
|
29
|
Giordano J, Schatzker M and Kfuri M: The
‘Hoop’ plate for posterior bicondylar shear tibial plateau
fractures: Description of a new surgical technique. J Knee Surg.
30:509–513. 2017.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Lv TR, Q C and X. L: Treatment of
posterolateral depression fractures of tibial plateau with improved
postemlateral approach and 2.4 mm distal radiuslocking plate. Chin
J Orthop Trauma. 18:851–856. 2016.
|
|
31
|
G F, ZJ P and H. L: Dual locking plate
fixation for Type C3 tibial plateau fractures involving the
posterior column. Chin J Orthop. 34:695–702. 2014.
|
|
32
|
Naito K, Sugiyama Y, Obata H, Mogami A,
Obayashi O and Kaneko K: Screw fixation and autogenous bone graft
for an irreducible distal ulna fracture associated with distal
radius fracture. J Hand Surg Asian Pac Vol. 22:236–239.
2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Shi Z, Zhang X, Zhang K, Jiang R, Yang W
and C. L: Short-term effect of non-absorbable sutures repairing
iatrogenic medial collateral ligament injury during total knee
arthroplasty. Chin J Bone Joint Surg. 12:126–130. 2019.
|
|
34
|
Mihalko WM, Saleh KJ, Krackow KA and
Whiteside LA: Soft-tissue balancing during total knee arthroplasty
in the varus knee. J Am Acad Orthop Surg. 17:766–774.
2009.PubMed/NCBI View Article : Google Scholar
|