Introduction
Age-related macular degeneration (AMD) is recognized
as a serious and rapidly growing worldwide public health concern
and is the third leading cause of blindness after glaucoma and
cataracts (1). The prevalence of
AMD by 2040 is projected to significantly increase to ~288 million
cases (2). Different factors may
contribute toward AMD, including age, environmental factors and
genetic susceptibility. Ageing may strengthen the problem of visual
difficulty associated with AMD. Patients with AMD have
extracellular deposits called drusen, which are accumulated within
Bruch's membrane (BrM) located between retinal pigment epithelium
(RPE) and the choroid. AMD is classified according to age-related
eye disease study based on the amount of drusen and it includes
early AMD, intermediate AMD and late AMD (3). The late AMD is sub-divided into the
dry non-neovascular type distinguished by the existence of drusen
spreading in the central macula, and the wet neovascular type
characterized by neovascularization within sub-RPE and sub-retinal
space (4). The progression of
neovascular AMD may be decreased by injecting anti-VEGF agents into
the vitreous humour monthly (5).
However, at present, there is no standard medical treatment for dry
non-neovascular AMD. Development of novel therapeutic strategies is
therefore urgently required.
Inflammation serves a vital role in the pathogenesis
of AMD (6). A recent study has
reported that plasma levels of interleukin (IL)-6, IL-8 and tumor
necrosis factor-alpha (TNF) R2 are significantly higher in patients
with dry AMD than in healthy controls (7). Additionally, the IL-6 level is also
associated with the progression of geographic atrophy (7). In wet AMD, IL-1β, IL-6 and TNF-α
levels in plasma are significantly high, compared with healthy
controls (8). Patients with wet AMD
also have an increased expression of inflammation-associated
chemokines (CXCL7, 10, 14, 16 and 22) in the aqueous humor
(9). NLRP3 inflammasome is
upregulated in macular lesions of patients with dry and wet AMD
(10). Analyses of plasma
complement components have demonstrated systemic complement
activation being associated with AMD (11-14).
The RPE is responsible for the maintenance of photoreceptor
function, and RPE dysfunction is the primary cause of AMD.
Inflammation may be induced in the RPE under stress conditions
(6). Recently, it was demonstrated
that oxidative stress-induced inflammation in RPE cells, indicated
by a significant increase in the secretion of IL-1β, IL-6, IL-8,
TNF-α and VEGF (15,16). The RPE is the main cause of drusen
formation, and numerous constituents of drusen deposits are
inflammation mediators (17). For
example, oxidized low-density lipoprotein (oxLDL) may activate
inflammasome and increase secretion of proinflammatory cytokines in
human RPE cells (18,19). 7-ketocholesterol (7KC) is another
component of drusen, which also induces inflammation in human RPE
cells by upregulating the expression of IL-1β, IL-6, IL-8 and TNF-α
(20,21).
Gardenia jasminoides (G. Jasminoides,
‘Zhi Zi’ in Chinese) is an evergreen shrub with fragrant white
flowers, which grows in numerous regions of China and is
predominantly used as an organic yellow dye (22). The fruits of G. Jasminoides
are rich in antioxidant and anti-inflammatory compounds and have
been used as a dietary supplement in Chinese herbal medicine for
many years to treat a variety of human diseases, including
headache, fever, liver disease and hypertension (23). A total of 35 iridoid glycosides and
8 corcin and its derivatives have been identified in G.
Jasminoides fruits. The functions of certain identified
constituents have been characterized and demonstrated to have
antioxidant, anti-inflammatory, anti-diabetic and anticancer
activities (22,24).
We hypothesised that G. Jasminoides extract
(GJE) may have therapeutic potential for AMD. The present study
assessed the efficacy of GJE against inflammation in human RPE
cells in vitro and in Zebrafish embryos. It was found that
GJE decreased lipopolysaccharide (LPS)-induced inflammation in
human RPE cells. It was also demonstrated that GJE inhibited LPS
and CuSO4-induced inflammation in Zebrafish embryos.
Materials and methods
Preparation of G. Jasminoides
extract
The dried fruits of G. Jasminoides were
collected in October 2017 from a local farm in Yueyang, Hunan, P.R.
China. The dried fruits were ground into powder, which was passed
through a 40-mesh sieve. A total of 50 g powder was extracted with
500 ml 75% ethanol by microwave extraction at 60˚C for 30 min. The
obtained extract solutions were filtered and evaporated under a
reduced pressure at 40˚C to remove the solvents. The dried GJE was
dissolved in methanol at 500 µg/ml and filtered through a 0.22 µm
pore size member for further analysis.
High-performance liquid chromatography
(HPLC) analysis
The HPLC separation was performed using a Waters
WATO54275-C18 column (250x4.6 mm, 5 µm, Waters China, Ltd.)
installed on a Waters 2695 HPLC instrument (Waters Corporation).
The mobile phase consisted of 0.1% phosphoric acid (A) and
acetonitrile (B) with a gradient elution: 0-15 min, 4-25% B; 15-20
min, 25-28% B; 20-40 min, 28-38% B; 40-41 min, 95% B; 41-51 min,
95-4% B. The flow rate was 1 ml/min, and the injection volume was
10 µl. The temperature of the column was set at 25˚C. Standard
compounds, including geniposidic acid, deacetylasperulosidic acid,
genipin-1-gentiobioside, geniposide, crocin I and II with >98%
purity were purchased from Shanghai Yuanye Bio-Technology Co.,
Ltd.
Cell viability
ARPE-19 cells (human retina pigment epithelium
cells) were purchased from ATCC (ATCC®
CRL-2302™) and cultured in 96-well plates at a density
of 5x104 cells/well in DMEM/F-12 (Thermo Fisher
Scientific, Inc.) at a final volume of 100 µl at 37˚C in 95% air
and 5% CO2. A total of 24 h later, the cells were washed
twice with 1X PBS and treated with LPS dissolved in water at
different concentrations: 0, 1.0, 2.5, 5.0, 10.0 and 20 µg/ml, with
or without GJE dissolved in methanol at concentrations of 5, 10,
25, 50 and 100 µg/ml for 24 h. Subsequently, the cells were washed
with 1X PBS twice and treated with serum-free medium containing 0.5
µg/ml MTT (Sigma-Aldrich; Merck KGaA) with the final volume of 50
µl per well for 2 h. Next, the MTT solution was removed from the
plate, and 100 µl/well dimethyl sulfoxide was added. The
concentration of formazan was evaluated using an EPOCH microplate
reader at 570 nm. The percentage of live cells was calculated using
the following formula: % of viable cells = (OD of treated cells/OD
of control cells) x100.
Zebrafish embryo treatment
All the animal experimental procedures were approved
by the Animal Ethics and Welfare Committee, Glasgow Caledonian
University (Project License PPL 60/4169). Breeding was set up in
the Animal Unit at Glasgow Caledonian University using adult
wild-type and transgenic zebrafish (Tg:zlyz-EGFP) expressing EGFP
in primitive macrophages to get fertilized embryos, which were
maintained in E3 medium consisting of 5 mM NaCl, 0.17 mM KCl, 0.33
mM CaCl2 and 0.33 mM MgSO4 (25). CuSO4 has been used to
induce acute inflammation, as previously described (26-28).
A total of 24 transgenic zebrafish (Tg:zlyz-EGFP) embryos at 48 h
post-fertilization (hpf) were treated with or without GJE (diluted
in E3 medium, 5 µg/ml) for 24 h (i.e. until 72 hpf). Zebrafish
embryos were further treated with CuSO4 (20 µM) for 1 h to induce
the acute inflammation, by adopting the previously reported
protocol (26,27). Following treatment, embryos were
fixed at room temperature for 2 h in 4% paraformaldehyde, and
macrophage migration to the lateral line was examined using
fluorescent microscopy (magnification, x100). Additionally, the
embryos were collected for further gene expression analysis.
Lipopolysaccharides (LPS) have also been commonly used to
induce inflammation in zebrafish (26-29),
and this method was also used in the present study. Wild-type
zebrafish embryos at 48 hpf were treated with GJE (5 µg/ml) only,
or with GJE plus LPS (5 µg/ml) for 24 h. Following the treatment,
embryos were collected and subjected to gene expression
analysis.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was extracted from treated and control
cells or zebrafish embryos using TRIzol® (Sigma-Aldrich;
Merck KgaA), according to the manufacturer's protocols.
High-capacity cDNA Reverse Transcriptase kit (Thermo Fisher
Scientific, Inc.) was used for cDNA synthesis, according to the
manufacturer's protocols. The RT-qPCR assay was used to quantify
gene expression using 5X HOT FIREPol EvaGreen qPCR Mix Plus (ROX)
kit (Solis Biodyne) with 12.5 mM MgCl2, 10 mM dNTPs,
according to the manufacturer's protocols. Reactions were performed
in triplicates with a total volume of 10 µl consisting of 5.5 µl
nuclease-free water, 2 µl EvaGreen, 0.75 µl 10 µM forward and
reverse primers and 2 µl cDNA (60-120 ng). For the control, all
reagents were used except cDNA, which was replaced with an equal
volume of nuclease-free water. The reaction was performed in the
CFX96 Real-time PCR detection system (Bio-Rad Laboratories, Inc.)
under the following conditions: Denaturation at 95˚C for 2 min; and
40 cycles including denaturation at 95˚C for 15 sec, and annealing
at 60˚C. The fluorescence signals were detected at the end of the
60˚C-step. The relative expression was calculated using the
2-∆∆Cq formula (30).
Primers used for RT-qPCR are listed in Tables SI and SII.
ELISA
Following the exposure of ARPE-19 cells to GJE (5
µg/ml), LPS (5 µg/ml) or GJE (5 µg/ml) with LPS (5 µg/ml) for 24 h,
the culture media were collected and centrifuged at 12,000 x g for
15 min at 4˚C. The IL-1β, IL-6 and TNF-α in the supernatants were
measured using human Mini ELISA development kits for IL-1β (cat.
no. 900-M95), IL-6 (cat. no. 900-M16) and TNF-α (cat. no. 900-M25)
(PeproTech, Inc.).
Statistical analysis
All data are presented as the mean ± standard error
of the mean (n=6). Statistical analysis of the data was performed
using GraphPad Prism software version 8 (GraphPad Software, Inc.)
by one-way analysis of variance, followed by Dunnett's or Tukey's
post hoc test. Linear regression analysis was performed based on
the GraphPad Prism 9 Curve Fitting Guide (GraphPad Software, Inc.).
P<0.05 was considered to indicate a statistically significant
difference.
Results
Analysis of compounds in GJE
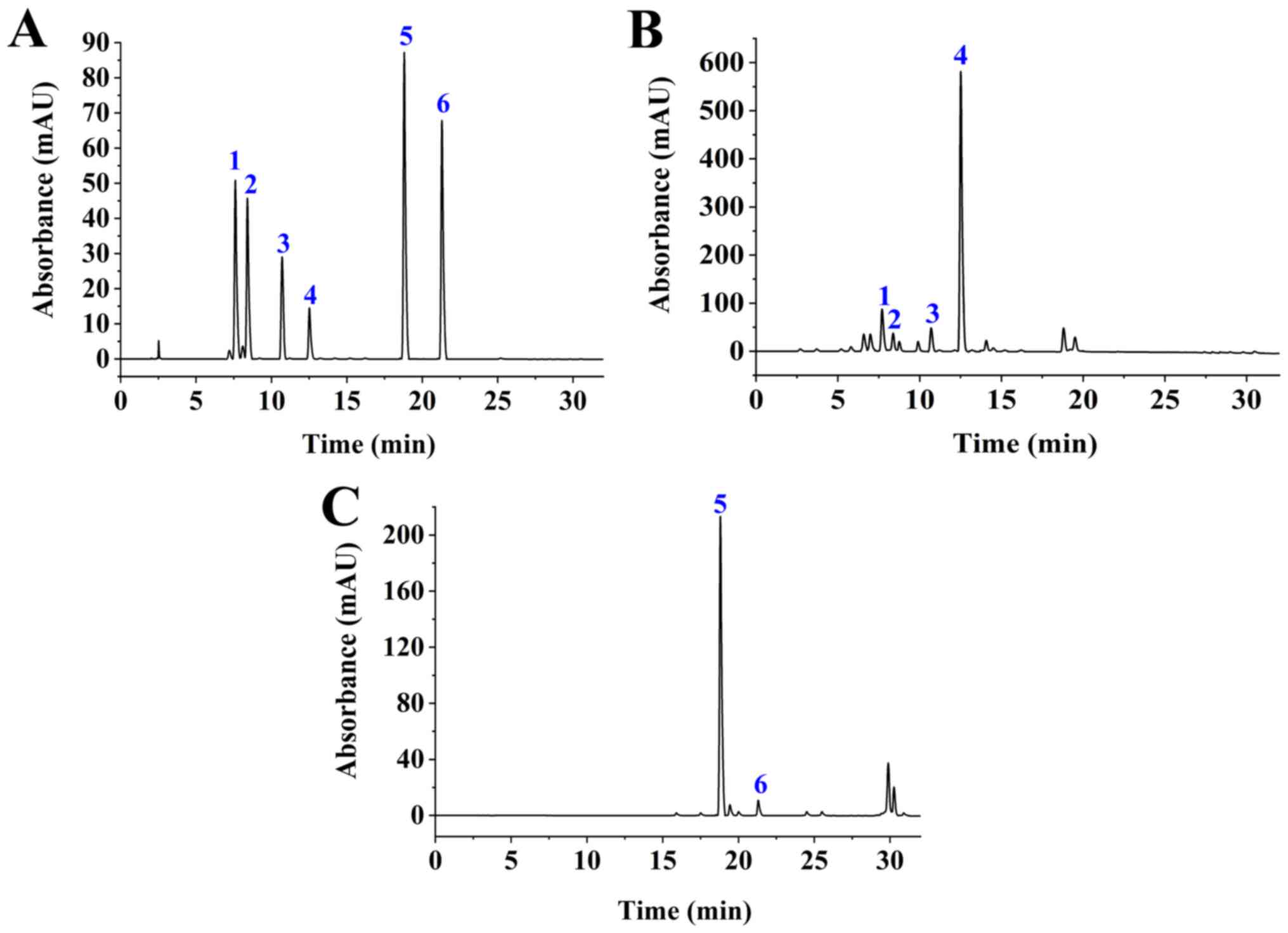
Following microwave-assisted extraction, GJE was
subjected to HPLC analysis. Based on six standards, it was found
that geniposide and Crocin-1 were the major compounds (Fig. 1), which is in agreement with the
results of a recent report (31).
The other four compounds, geniposidic acid, deacetylasperulosidic
acid, genipin-1-gentiobioside and Crocin II, were also identified
in GJE but at low levels. Retention times for geniposide and Crocin
I was 12.85 min and 18.766 min, respectively. Linear regression
analyses were performed on the concentration (X, µg/ml) and the
peak area (Y) of geniposide or Crocin I at different
concentrations. The regression equations for geniposide and Crocin
I were y=19262073.0848 x-14747.0407 (Coefficient, 0.9999) and
y=36463016.7557 x +278758.6821 (coefficient, 0.9992), respectively.
The relative standard deviation for precision was 2.31%
(geniposide) and 1.22% (Crocin I), for repeatability it was 1.59%
(geniposide) and 2.11% (Crocin I), and for stability it was 1.39%
(geniposide) and 1.58% (Crocin I). The average recoveries for
geniposide and Crocin I were 99.62 and 94.94%, respectively. The
contents of geniposide and Crocin I in G. Jasminoides fruits
were 40.88 and 7.72 mg/g, respectively.
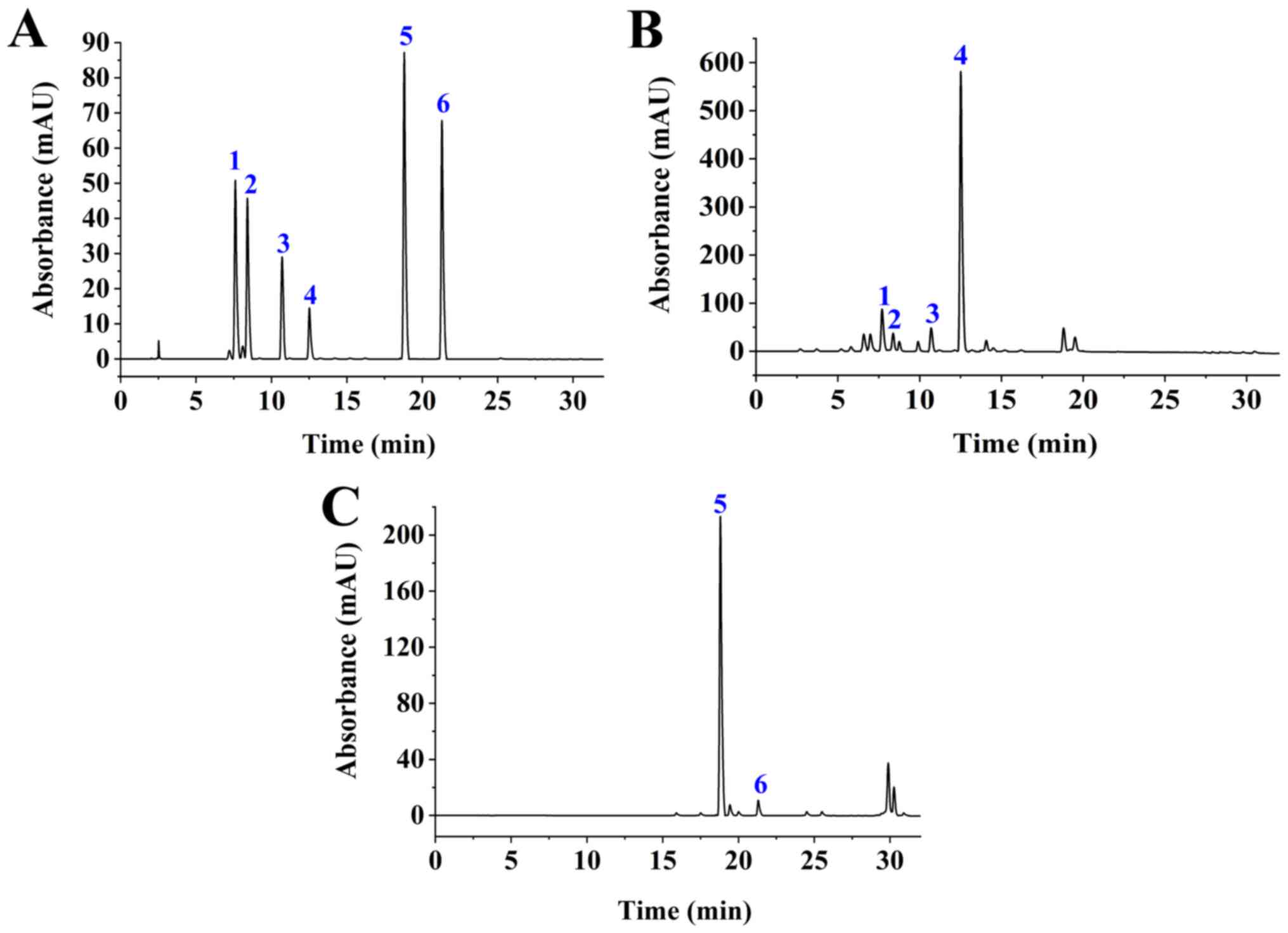 | Figure 1HPLC analysis. (A) HPLC chromatogram
of standard compounds: 1, geniposidic acid; 2,
deacetylasperulosidic acid; 3, genipin-1-gentiobioside; 4,
geniposide; 5, Crocin I; and 6 and Crocin II. (B) HPLC chromatogram
of GJE component: 1, geniposidic acid; 2, deacetylasperulosidic
acid; 3, genipin-1-gentiobioside; and 4, geniposide were identified
with a detection wavelength of 238 nm. (C) HPLC chromatogram of GJE
component: 5, Crocin I; and 6, Crocin II were identified at a
detection wavelength of 440 nm. HPLC, High-performance liquid
chromatography; GJE, Gardenia jasminoides extracts. |
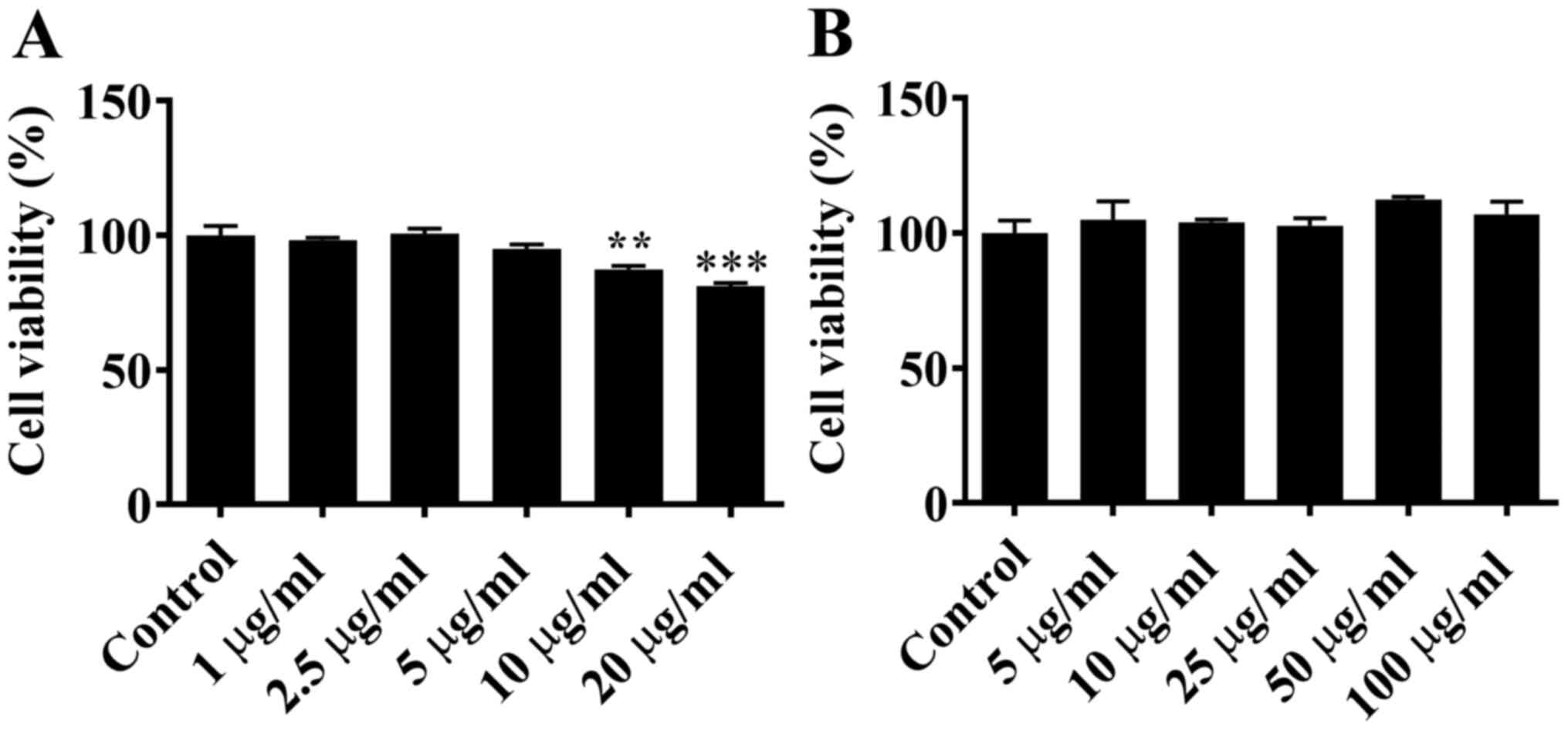
Effects of LPS and GJE on cell
viability
ARPE-19 cells were treated with LPS at
concentrations of 0, 1.0, 2.5, 5.0, 10.0 or 20.0 µg/ml for 24 h.
MTT assay demonstrated that LPS at 1.0, 2.5 or 5.0 µg/ml had no
significant effect on the viability of ARPE-19 cells compared with
control cells. However, LPS at higher concentrations (10.0 or 20.0
µg/ml) was significantly toxic for ARPE-19 cells, and notably
decreased cell viability (Fig. 2A).
When ARPE-19 cells were treated with GJE at concentrations of 0,
5.0, 10.0, 25.0, 50.0 or 100.0 µg/ml, there was no significant
difference in cell viability compared with untreated cells
(Fig. 2B). Based on these data, LPS
at 5.0 µg/ml and GJE at 5.0 µg/ml were selected for further
experiments.
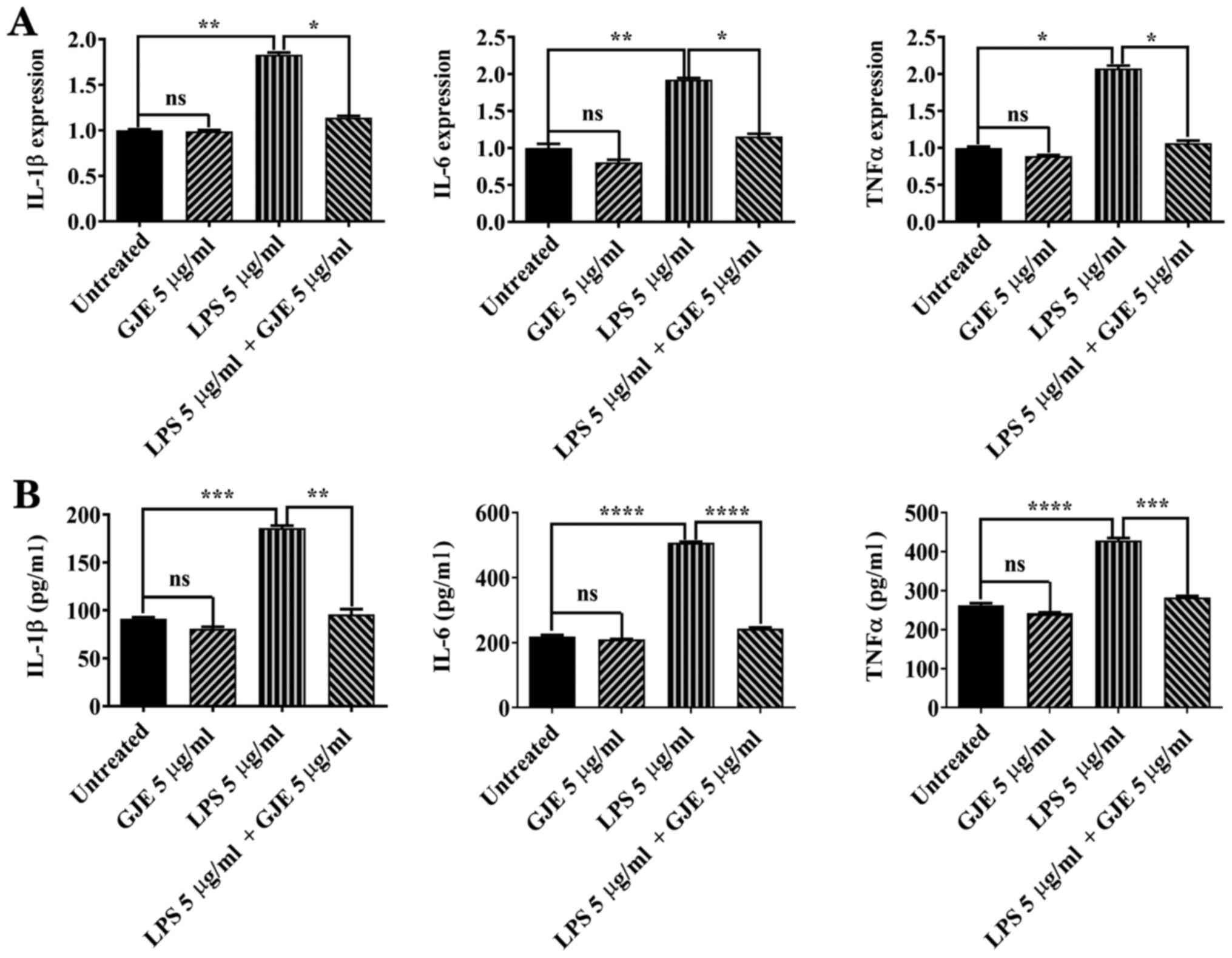
GJZ inhibits LPS-induced inflammation
in ARPE-19 cells
A total of 5 µg/ml LPS has been used to induce
inflammation in AREP-19 cells (32,33).
ARPE-19 cells were treated with GJE, LPS or GJE plus LPS for 24 h
and the expression of proinflammatory cytokines was compared. LPS
significantly increased the expression of IL-1β, IL-6 and TNF-α in
AREP-19 cells compared with control cells, while GJE treatment did
not cause any changes in expression of these inflammatory
mediators. Co-treatment with GJE resulted in markedly decreased
expression of these three cytokine genes compared with cells
treated with LPS alone (Fig. 3A).
Next, ELISA was performed to detect cytokine secretion in control
cells and treated cells. LPS exposure significantly increased
cytokine secretion, while GJE-treated cells secreted cytokines
similarly to control cells. These results suggested that treatment
with GJE reversed LPS-induced cytokine secretion (Fig. 3B).
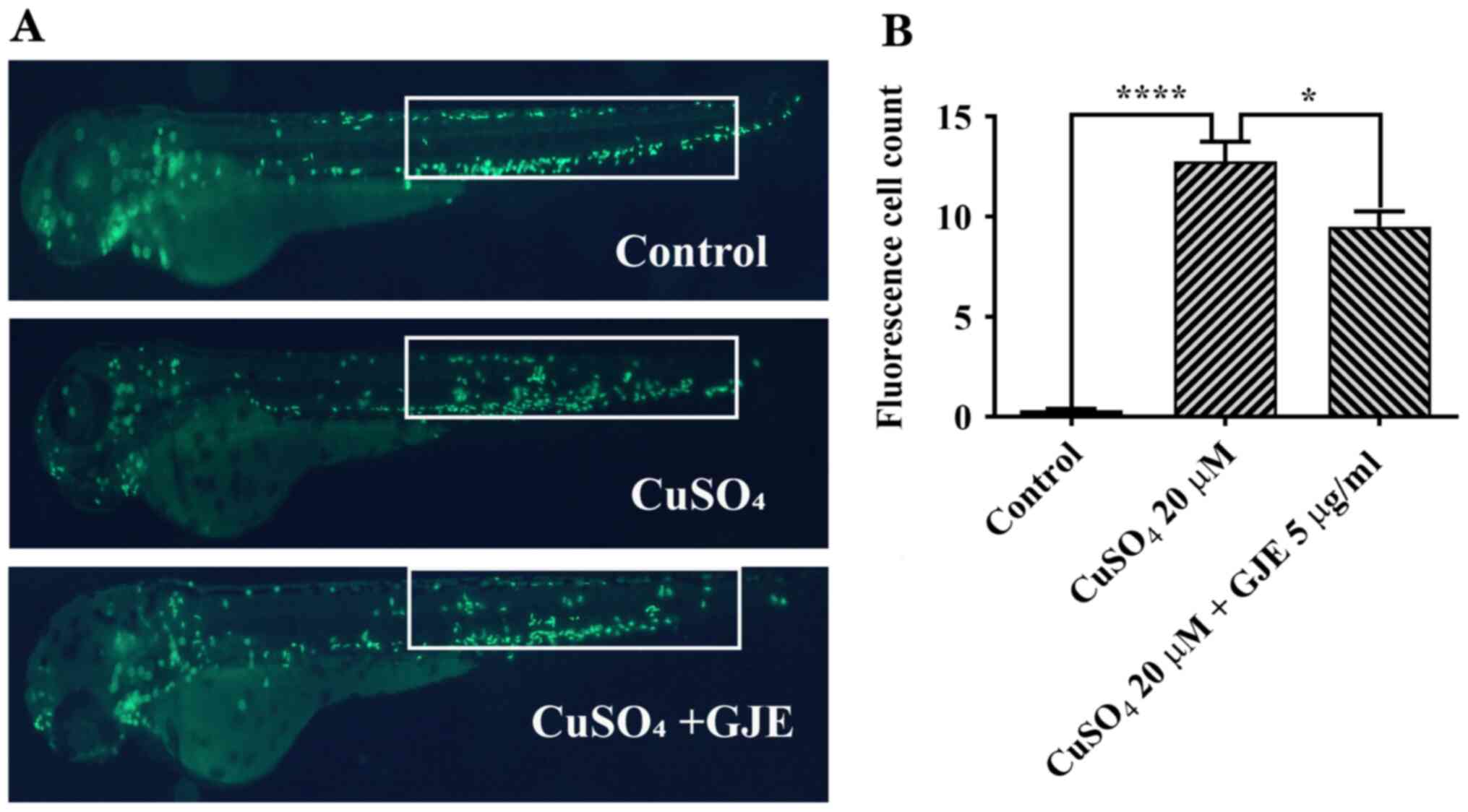
GJE attenuates microphage migration in
zebrafish embryos
Previous reports have demonstrated that
CuSO4 at 20 µM causes primitive macrophage migration to
the lateral line in zebrafish embryos (26-28).
It was also found that the number of migrated macrophages in
treated cells was significantly higher than that in untreated
controls. These results indicated that co-treatment significantly
decreased macrophage migration (Fig.
4).
GJE reduces inflammation in zebrafish
embryos
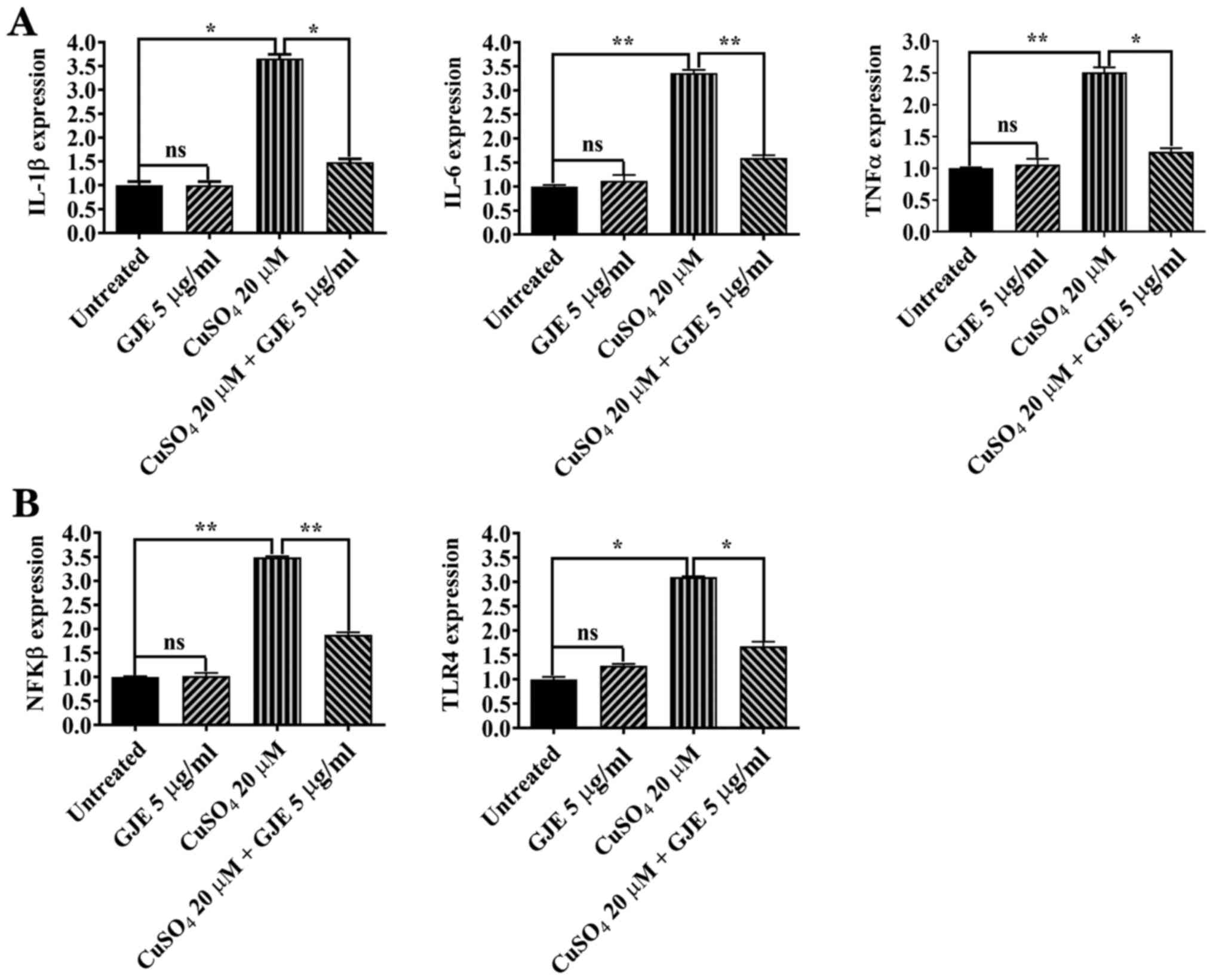
The present study measured the expression of
proinflammatory cytokines in control and treated zebrafish embryos
using RT-qPCR. CuSO4 treatment resulted in significantly increased
expression of IL-1β, IL6 and TNFα cytokines compared with that of
controls, while GJE did not cause any alteration in expression of
these cytokines. The embryos co-exposed to the two compounds had a
significantly decreased expression of cytokines compared with
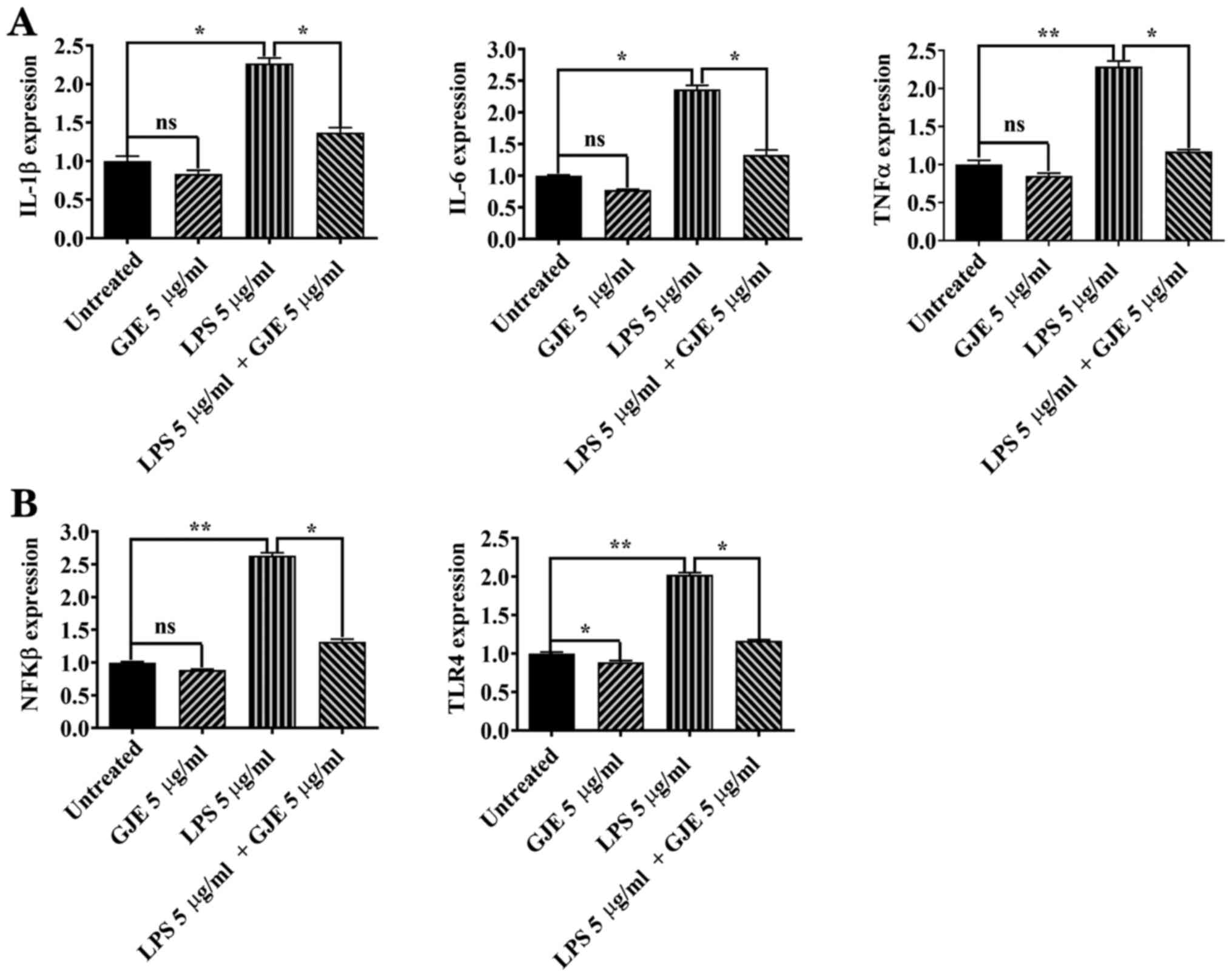
embryos exposed to CuSO4 alone (Fig. 5A). The effects of LPS or LPS plus
GJE were investigated in zebrafish embryos. Similar to the in
vitro results in ARPE-19 cells, LPS significantly increased the
expression of IL-1β, IL-6 and TNFα, while GJE treatment
counteracted LPS-induced effects on the expression of the three
genes (Fig. 6A).
The NFkB signaling pathway serves a central role in
regulating inflammation (34).
Therefore, the present study investigated the NFKB activating
protein (nkap) expression by RT-qPCR. The results of the present
study suggested that CuSO4 and LPS markedly enhanced
nkap expression compared with that of control zebrafish
embryos. Additionally, co-treatment with GJE resulted in
significantly decreased expression of nkap compared with the
embryos exposed to CuSO4 or LPS alone (Figs. 5B and 6B). Finally, activation of the Toll-like
receptor 4 (TLR4) signaling pathway induces the nuclear
translocation of NF-κB and leads to upregulation of proinflammatory
cytokines (35). The present study
found higher expression of tlr4b in CuSO4 or
LPS-treated embryos that were significantly counteracted by
co-treatment with GJE (Figs. 5B and
6B).
Discussion
Inhibition of inflammatory agents represents an
effective therapeutic strategy to treat AMD (36). There are numerous natural products,
which are rich in anti-inflammatory compounds. In GJE, six
predominant compounds, including geniposidic acid,
deacetylasperulosidic acid, genipin-1-gentiobioside, geniposide,
Crocin I and II, were identified and the anti-inflammatory
potential of GJE was confirmed in vitro and in vivo.
The attenuated expression of proinflammatory cytokines is
associated with GJE-evoked inhibition of the TLR4-mediated signal
pathway, given that expression of TLR4 and NKAP were
revealed to be downregulated.
Numerous active compounds have been identified in
G. Jasminoides, including iridoids, iridoid glycosides,
terpenoids and phenolic acids (36). While geniposide and Crocin I were
the predominant compounds in GJE, geniposidic acid,
deacetylasperulosidic acid, genipin-1-gentiobioside and Crocin II
were also detected at a low level in GJE (Fig. 1). The anti-inflammatory
characteristics of the whole GJE and its individual active
components have been widely studied (22,37).
An early study reported the anti-inflammatory capacity of
ethanol-based extracts of G. Jasminoides in inhibiting
carrageenan-induced rat paw oedema and acetic acid-induced vascular
permeability (38). Hwang et
al (39) reported that GJE
decreased vascular inflammation in TNF-α treated human umbilical
vein endothelial cells via preventing NF-kB p65 nuclear
translocation, downregulating adhesion molecule expression and
decreasing monocyte-endothelial cell interaction (39). GJE was also reported to decrease
LPS-induced production of IL-1β, IL-6 and nitric oxide in
microglial BV2 cells through inactivation of the MAPK signalling
pathway (40). Geniposide, the main
functional compound of G. Jasminoides, has shown strong
anti-inflammatory activity in vitro and in vivo. For
example, it significantly decreased the production of IL-1β, IL-6
and TNF-α, decreased expression and translocation of NF-κB p65, and
inhibited the MAPK signalling pathway in rat primary microglia
exposed to oxygen-glucose deprivation (41). Geniposide also showed similar
protective effects in LPS-exposed macrophages and in mice
challenged with LPS (42). Crocin,
another active compound identified in G. Jasminoides, also
showed anti-inflammatory activity by decreasing the expression of
proinflammatory cytokines and decreasing nitric oxide production
(43,44).
In the present study, G. Jasminoides
components demonstrated a protective effect against retinal damage.
Crocin and genipin (a metabolite of geniposide) protect ARPE-19
cells from H2O2-caused oxidative damage by
decreasing the production of reactive oxygen species and inhibiting
Caspase 3-mediated apoptosis via the NRF2 signalling pathway
(45,46). Crocin may decrease
H2O2-induced RGC-5 ganglion cell death by
inhibiting oxidative stress and apoptosis, and reversing NF-κB
activation (47). Crocin may also
increase the survival of rat ganglion cells following
ischemia/reperfusion injury and protect photoreceptors from
blue-light damage in cultured bovine and primate retinas (48-50).
Recently, a clinical trial showed that Crocin (15 mg/day for three
months) resulted in a decrease in glycated haemoglobin (HbA1c) and
in central macula thickness, and result in an improvement of the
best-corrected visual acuity in patients with diabetic maculopathy
(51). Crocetin, another active
compound identified in G. Jasminoides, protected ganglion
cells against H2O2-induced oxidative damage
and prevent photoreceptor degeneration from light-induced damage
(52). Crocetins also inhibit
retinal damage from ischemia/reperfusion injury or from
N-methyl-D-aspartate-induced toxicity via blocking Caspase and NFkB
pathways (53,54). Recently, Nitta et al
(55) reported that crocetin
prevented retinal edema in a laser-induced retinal vein occlusion
mouse model via downregulating the expression of MMP-9 and TNF-α.
Given the multifaceted anti-inflammatory impact of GJE treatment
in vitro and in vivo reported in the present study,
it is likely that the combination of active compounds may evoke
more profound effects than any single-compound treatment. The
optimum dose of these compounds may be even more effective and
require further investigation.
The results of the present study were based on an
in vitro RPE model and zebrafish embryo inflammation models,
which may not be directly relevant to an in vivo AMD study.
Further studies will be required to investigate the
anti-inflammatory role of GJE in preclinical AMD models to further
verify the results of the current study. In addition, it is
valuable to gain more insights into the molecular mechanisms of
GJE's protection in vivo.
In summary, the results of the present study
demonstrated the anti-inflammatory role of GJE in RPE cells and in
zebrafish embryos. Given that it is a natural product with a long
history in Traditional Chinese Medicine, GJE appears to have
therapeutic potential for treating patients with AMD and could be
easily translated to the clinics.
Supplementary Material
Human primers.
Zebrafish primers.
Acknowledgements
Not applicable.
Funding
Funding: The present study was funded by the Department of
Education, Hunan, China (grant no. 19A045); the Hunan Province
‘Help Our Motherland Through Elite Intellectual Resources from
Overseas’ program to ZZ (grant no. 60802); and a Hunan Provincial
Natural Science Foundation of China (grant no. 2020JJ4641) to JC.
The study was partially supported by the Rosetrees Trust (grant
nos. M160, M160-F1 and M160-F2), National Eye Research Centre
(grant no. SAC037) and the Lotus Scholarship Program of Hunan
Province (2019) to XS.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XS and ZZ designed the experiments. JC, GMT, XZ, WT,
FL, ML and CZ performed the experiments. JC, GMT and XZ analyzed
the data. XS and ZZ wrote the manuscript. XS and ZZ confirmed the
authenticity of the raw data. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
All the animal experimental procedures were approved
by the Animal Ethics and Welfare Committee, Glasgow Caledonian
University (Project License PPL 60/4169).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mantel I: Age-related macular
degeneration-a challenge for public health care. Ther Umsch.
73:79–83. 2016.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
2
|
Wong WL, Su X, Li X, Cheung CM, Klein R,
Cheng CY and Wong TY: Global prevalence of age-related macular
degeneration and disease burden projection for 2020 and 2040: A
systematic review and meta-analysis. Lancet Glob Health.
2:e106–e116. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Age-Related Eye Disease Study Research
Group. A randomized, placebo-controlled, clinical trial of
high-dose supplementation with vitamins C and E, beta carotene, and
zinc for age-related macular degeneration and vision loss: AREDS
report no. 8. Arch Ophthalmol. 119:1417–1436. 2001.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Jager RD, Mieler WF and Miller JW:
Age-related macular degeneration. N Engl J Med. 358:2606–2617.
2008.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Yuan A and Kaiser PK: Emerging therapies
for the treatment of neovascular age related macular degeneration.
Semin Ophthalmol. 26:149–155. 2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Datta S, Cano M, Ebrahimi K, Wang L and
Handa JT: The impact of oxidative stress and inflammation on RPE
degeneration in non-neovascular AMD. Prog Retin Eye Res.
60:201–218. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Krogh Nielsen M, Subhi Y, Molbech CR, Falk
MK, Nissen MH and Sørensen TL: Systemic levels of interleukin-6
correlate with progression rate of geographic atrophy secondary to
age-related macular degeneration. Invest Ophthalmol Vis Sci.
60:202–208. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Subhi Y, Krogh Nielsen M, Molbech CR,
Oishi A, Singh A, Nissen MH and Sørensen TL: Plasma markers of
chronic low-grade inflammation in polypoidal choroidal vasculopathy
and neovascular age-related macular degeneration. Acta Ophthalmol.
97:99–106. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Liu F, Ding X, Yang Y, Li J, Tang M, Yuan
M, Hu A, Zhan Z, Li Z and Lu L: Aqueous humor cytokine profiling in
patients with wet AMD. Mol Vis. 22:352–361. 2016.PubMed/NCBI
|
|
10
|
Wang Y, Hanus JW, Abu-Asab MS, Shen D,
Ogilvy A, Ou J, Chu XK, Shi G, Li W, Wang S and Chan CC: NLRP3
upregulation in retinal pigment epithelium in age-related macular
degeneration. Int J Mol Sci. 17(73)2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sivaprasad S, Adewoyin T, Bailey TA,
Dandekar SS, Jenkins S, Webster AR and Chong NV: Estimation of
systemic complement C3 activity in age-related macular
degeneration. Arch Ophthalmol. 125:515–519. 2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Scholl HP, Charbel Issa P, Walier M,
Janzer S, Pollok-Kopp B, Börncke F, Fritsche LG, Chong NV, Fimmers
R, Wienker T, et al: Systemic complement activation in age-related
macular degeneration. PLoS One. 3(e2593)2008.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Reynolds R, Hartnett ME, Atkinson JP,
Giclas PC, Rosner B and Seddon JM: Plasma complement components and
activation fragments: Associations with age-related macular
degeneration genotypes and phenotypes. Invest Ophthalmol Vis Sci.
50:5818–5827. 2009.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Machalińska A, Dziedziejko V,
Mozolewska-Piotrowska K, Karczewicz D, Wiszniewska B and
Machaliński B: Elevated plasma levels of C3a complement compound in
the exudative form of age-related macular degeneration. Ophthalmic
Res. 42:54–59. 2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Alhasani RH, Biswas L, Tohari AM, Zhou X,
Reilly J, He JF and Shu X: Gypenosides protect retinal pigment
epithelium cells from oxidative stress. Food Chem Toxicol.
112:76–85. 2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Tohari AM, Alhasani RH, Biswas L, Patnaik
SR, Reilly J, Zeng Z and Shu X: Vitamin D attenuates oxidative
damage and inflammation in retinal pigment epithelial cells.
Antioxidants (Basel). 8(341)2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kauppinen A, Paterno JJ, Blasiak J,
Salminen A and Kaarniranta K: Inflammation and its role in
age-related macular degeneration. Cell Mol Life Sci. 73:1765–1786.
2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Biswas L, Zhou X, Dhillon B, Graham A and
Shu X: Retinal pigment epithelium cholesterol efflux mediated by
the 18 kDa translocator protein, TSPO, a potential target for
treating age-related macular degeneration. Hum Mol Genet.
26:4327–4339. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Gnanaguru G, Choi AR, Amarnani D and
D'Amore PA: Oxidized lipoprotein uptake through the CD36 receptor
activates the NLRP3 inflammasome in human retinal pigment
epithelial cells. Invest Ophthalmol Vis Sci. 57:4704–4712.
2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Larrayoz IM, Huang JD, Lee JW, Pascual I
and Rodríguez IR: 7-Ketocholesterol-induced inflammation:
Involvement of multiple kinase signaling pathways via NFκB but
independently of reactive oxygen species formation. Invest
Ophthalmol Vis Sci. 51:4942–4955. 2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Yang C, Xie L, Gu Q, Qiu Q, Wu X and Yin
L: 7-Ketocholesterol disturbs RPE cells phagocytosis of the outer
segment of photoreceptor and induces inflammation through ERK
signaling pathway. Exp Eye Res. 189(107849)2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Chen L, Li M, Yang Z, Tao W, Wang P, Tian
X, Li X and Wang W: Gardenia jasminoides Ellis:
Ethnopharmacology, phytochemistry, and pharmacological and
industrial applications of an important traditional Chinese
medicine. J Ethnopharmacol. 257(112829)2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
National Commission of Pharmacopoeia:
Pharmacopoeia of the People's Republic of China, Vol. 1. China
Medical Science and Technology Press, Beijing, pp231, 2010.
|
|
24
|
Song X, Zhang W, Wang T, Jiang H, Zhang Z,
Fu Y, Yang Z, Cao Y and Zhang N: Geniposide plays an
anti-inflammatory role via regulating TLR4 and downstream signaling
pathways in lipopolysaccharide-induced mastitis in mice.
Inflammation. 37:1588–1598. 2014.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Zhang Y, Bai XT, Zhu KY, Jin Y, Deng M, Le
HY, Fu YF, Chen Y, Zhu J, Look AT, et al: In vivo interstitial
migration of primitive macrophages mediated by JNK-matrix
metalloproteinase 13 signaling in response to acute injury. J
Immunol. 181:2155–2164. 2008.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Li JJ, Zhang Y, Han LW, Tian QP, He QX,
Wang XM, Sun C, Han J and Liu KC: Tenacissoside H exerts an
anti-inflammatory effect by regulating the NF-κB and p38 pathways
in zebrafish. Fish Shellfish Immunol. 83:205–212. 2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Zhang Y, Wang C, Jia ZL, Ma RJ, Wang XF,
Chen WY and Liu KC: Isoniazid promotes the anti-inflammatory
response in zebrafish associated with regulation of the
PPARγ/NF-κB/AP-1 pathway. Chem Biol Interact.
316(108928)2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Zhou H, Cao H, Zheng Y, Lu Z, Chen Y, Liu
D, Yang H, Quan J, Huo C, Liu J and Yu L: Liang-Ge-San, a classic
traditional Chinese medicine formula, attenuates acute inflammation
in zebrafish and RAW 264.7 cells. J Ethnopharmacol.
249(112427)2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Zhang Y, Takagi N, Yuan B, Zhou Y, Si N,
Wang H, Yang J, Wei X, Zhao H and Bian B: The protection of
indolealkylamines from LPS-induced inflammation in zebrafish. J
Ethnopharmacol. 243(112122)2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Shan MQ, Wang TJ, Jiang YL, Yu S, Yan H,
Zhang L, Wu QN, Geng T, Huang WZ, Wang ZZ and Xiao W: Comparative
analysis of sixteen active compounds and antioxidant and
anti-influenza properties of Gardenia jasminoides fruits at
different times and application to the determination of the
appropriate harvest period with hierarchical cluster analysis. J
Ethnopharmacol. 233:169–178. 2019.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Ozal SA, Turkekul K, Gurlu V, Guclu H and
Erdogan S: Esculetin protects human retinal pigment epithelial
cells from lipopolysaccharide-induced inflammation and cell death.
Curr Eye Res. 43:1169–1176. 2018.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Tao L, Qiu Y, Fu X, Lin R, Lei C, Wang J
and Lei B: Angiotensin-converting enzyme 2 activator diminazene
aceturate prevents lipopolysaccharide-induced inflammation by
inhibiting MAPK and NF-κB pathways in human retinal pigment
epithelium. J Neuroinflammation. 13(35)2016.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Duan X, Gao S, Li J, Wu L, Zhang Y, Li W,
Zhao L, Chen J, Yang S, Sun G and Li B: Acute arsenic exposure
induces inflammatory responses and CD4+ T cell
subpopulations differentiation in spleen and thymus with the
involvement of MAPK, NF-κB, and Nrf2. Mol Immunol. 81:160–172.
2017.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Vaure C and Liu Y: A comparative review of
toll-like receptor 4 expression and functionality in different
animal species. Front Immunol. 5(316)2014.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Wang L, Schmidt S, Larsen PP, Meyer JH,
Roush WR, Latz E, Holz FG and Krohne TU: Efficacy of novel
selective NLRP3 inhibitors in human and murine retinal pigment
epithelial cells. J Mol Med (Berl). 97:523–532. 2019.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Su Q, Yao J and Sheng C: Geniposide
attenuates LPS-induced injury via up-regulation of miR-145 in H9c2
cells. Inflammation. 41:1229–1237. 2018.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Koo HJ, Lim KH, Jung HJ and Park EH:
Anti-inflammatory evaluation of gardenia extract, geniposide and
genipin. J Ethnopharmacol. 103:496–500. 2006.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Hwang SM, Lee YJ, Yoon JJ, Lee SM, Kang DG
and Lee HS: Gardenia jasminoides inhibits tumor necrosis
factor-alpha-induced vascular inflammation in endothelial cells.
Phytother Res. 24 (Suppl 2):S214–S219. 2010.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Lin WH, Kuo HH, Ho LH, Tseng ML, Siao AC,
Hung CT, Jeng KC and Hou CW: Gardenia jasminoides extracts
and gallic acid inhibit lipopolysaccharide-induced inflammation by
suppression of JNK2/1 signaling pathways in BV-2 cells. Iran J
Basic Med Sci. 18:555–562. 2015.PubMed/NCBI
|
|
41
|
Wang J, Hou J, Zhang P, Li D, Zhang C and
Liu J: Geniposide reduces inflammatory responses of oxygen-glucose
deprived rat microglial cells via inhibition of the TLR4 signaling
pathway. Neurochem Res. 37:2235–2248. 2012.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Fu Y, Liu B, Liu J, Liu Z, Liang D, Li F,
Li D, Cao Y, Zhang X, Zhang N and Yang Z: Geniposide, from
Gardenia jasminoides Ellis, inhibits the inflammatory
response in the primary mouse macrophages and mouse models. Int
Immunopharmacol. 14:792–798. 2012.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Nam KN, Park YM, Jung HJ, Lee JY, Min BD,
Park SU, Jung WS, Cho KH, Park JH, Kang I, et al: Anti-inflammatory
effects of crocin and crocetin in rat brain microglial cells. Eur J
Pharmacol. 648:110–116. 2010.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Yorgun MA, Rashid K, Aslanidis A, Bresgen
C, Dannhausen K and Langmann T: Crocin, a plant-derived carotenoid,
modulates microglial reactivity. Biochem Biophys Rep. 12:245–250.
2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Kassumeh S, Wertheimer CM, Ohlmann A,
Priglinger SG and Wolf A: Cytoprotective effect of crocin and
trans-resveratrol on photodamaged primary human retinal
pigment epithelial cells. Eur J Ophthalmol.
(1120672119895967)2019.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Zhao H, Wang R, Ye M and Zhang L: Genipin
protects against H2O2-induced oxidative
damage in retinal pigment epithelial cells by promoting Nrf2
signaling. Int J Mol Med. 43:936–944. 2019.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Lv B, Chen T, Xu Z, Huo F, Wei Y and Yang
X: Crocin protects retinal ganglion cells against
H2O2-induced damage through the mitochondrial
pathway and activation of NF-κB. Int J Mol Med. 37:225–232.
2016.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Chen L, Qi Y and Yang X: Neuroprotective
effects of crocin against oxidative stress induced by
ischemia/reperfusion injury in rat retina. Ophthalmic Res.
54:157–168. 2015.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Qi Y, Chen L, Zhang L, Liu WB, Chen XY and
Yang XG: Crocin prevents retinal ischaemia/reperfusion
injury-induced apoptosis in retinal ganglion cells through the
PI3K/AKT signalling pathway. Exp Eye Res. 107:44–51.
2013.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Laabich A, Vissvesvaran GP, Lieu KL,
Murata K, McGinn TE, Manmoto CC, Sinclair JR, Karliga I, Leung DW,
Fawzi A and Kubota R: Protective effect of crocin against blue
light- and white light-mediated photoreceptor cell death in bovine
and primate retinal primary cell culture. Invest Ophthalmol Vis
Sci. 47:3156–3163. 2006.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Sepahi S, Mohajeri SA, Hosseini SM,
Khodaverdi E, Shoeibi N, Namdari M and Tabassi SAS: Effects of
crocin on diabetic maculopathy: A placebo-controlled randomized
clinical trial. Am J Ophthalmol. 190:89–98. 2018.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Yamauchi M, Tsuruma K, Imai S, Nakanishi
T, Umigai N, Shimazawa M and Hara H: Crocetin prevents retinal
degeneration induced by oxidative and endoplasmic reticulum
stresses via inhibition of caspase activity. Eur J Pharmacol.
650:110–119. 2011.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Ohno Y, Nakanishi T, Umigai N, Tsuruma K,
Shimazawa M and Hara H: Oral administration of crocetin prevents
inner retinal damage induced by N-methyl-D-aspartate in mice. Eur J
Pharmacol. 690:84–89. 2012.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Ishizuka F, Shimazawa M, Umigai N,
Ogishima H, Nakamura S, Tsuruma K and Hara H: Crocetin, a
carotenoid derivative, inhibits retinal ischemic damage in mice.
Eur J Pharmacol. 703:1–10. 2013.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Nitta K, Nishinaka A, Hida Y, Nakamura S,
Shimazawa M and Hara H: Oral and ocular administration of crocetin
prevents retinal edema in a murine retinal vein occlusion model.
Mol Vis. 25:859–868. 2019.PubMed/NCBI
|