Introduction
Atherosclerosis primarily refers to the deposition
of fatty streaks and lipid spots in large elastic arteries,
including medium-sized elastic arteries (cerebral and coronary
arteries) and aortas in the blood circulatory system, which results
in the development of fibrous atherosclerotic plaque and
atheromatous lesions. Some of these changes may deteriorate the
elasticity of the arterial wall, block the lumen and induce
cardiocerebrovascular diseases, such as coronary heart disease and
cerebral infarction (CI) (1).
Carotid atherosclerotic plaque (CAP) is an independent risk factor
for cardiocerebrovascular events (2). Chen et al (3) observed atherosclerosis in patients
with CI using high-resolution MRI, and the results showed that the
proportion of severe stenosis of offending vessels and plaque load
in patients with recurrent CI were higher than those in patients
with primary CI; logistic regression analysis also showed that
severe lumen stenosis was a risk factor for the recurrence of CI.
Tang and Luo (4) pointed out that
the incidence of moderate carotid artery stenosis, plaque detection
rate, and incidence of soft plaques in patients with myocardial
infarction and hypertension were higher than those in the control
group without myocardial infarction and hypertension, and the
degree of carotid atherosclerotic vascular stenosis and plaque
stability can reflect the risk of cardiovascular disease in
patients to a certain extent, thus the degree of carotid
atherosclerosis can be used as a predictor of cardiovascular
diseases, including myocardial infarction. Therefore, early
diagnosis and treatment of atherosclerotic plaques via promotive
and effective measures are clinically significant in preventing the
development of severe cardiocerebrovascular diseases.
Previous studies have revealed that regular oral
administration of lipid-lowering agents, such as statins,
effectively reduces blood lipid levels, and consequently, the
incidence of cardiocerebrovascular events in patients with CAP
(5). Simvastatin is commonly used
in clinical practice to lower blood lipid levels, improve vascular
endothelial function and stabilize atherosclerotic plaques in
patients with hyperlipidemia (6).
Zhang et al (7) found that
the effective rate of simvastatin in the treatment of patients with
atherosclerosis was 89.80%, which was equivalent to that of
atorvastatin calcium, but that the serum high-sensitivity
C-reactive protein (hs-CPR), carotid intima-media thickness (IMT),
cystatin C, triglyceride (TG), total cholesterol (TC) and
low-density lipid cholesterol (LDL-C) in simvastatin group were
significantly lower than those in the atorvastatin calcium group,
suggesting that simvastatin has a significant effect on patients
with atherosclerosis. Compared with other statins, simvastatin is
primarily characterized by mild adverse reactions and better
tolerance in patients. To further validate the therapeutic effect
of simvastatin on CAP, the present study was designed to
investigate the efficacy of simvastatin in the treatment of elderly
patients with carotid atherosclerosis, and to further observe the
effect of simvastatin on serum inflammatory factors and
cardiocerebrovascular events.
Materials and methods
General characteristics
A total of 130 elderly patients diagnosed with CAP
in the outpatient department of Baoji City People's Hospital
(Baoji, China) were included. The inclusion criteria were as
follows: i) Patients with soft CAP as evidenced by carotid artery
color Doppler ultrasound, with <70% arterial luminal stenosis;
ii) those who met the diagnostic standards for CAP revised by the
Fourth National Academic Conference for Cerebrovascular Diseases
(8); iii) those who were willing to
follow the doctor's advice and adhere to long-term medication
without drop-out cases midway; and iv) those who signed informed
consent and volunteered to participate in the present study.
Patients with the following conditions were excluded: i) Previous
treatment using statins or other lipid-lowering agents 1 month
before enrollment in the study; ii) severe carotid stenosis with a
carotid stenosis rate of >70%; iii) statin allergy, uncontrolled
hypertension, familial hypercholesterolemia or secondary
hypercholesterolemia; iv) infectious diseases, severe
gastrointestinal (GI) diseases, or history of GI surgery that may
affect drug absorption; v) severe liver and kidney dysfunction or
heart failure; and vi) malignant tumors or bleeding within plaques.
The present study was approved by the Medical Ethics Committee of
Baoji City People's Hospital (Baoji, China). Patients were randomly
divided into control and observation groups (n=65 per group).
Treatment plan
Functional indicators of the heart, liver, and
kidney were measured for each patient before enrollment. If
necessary, antihypertensive and hypoglycemic agents were
administered to patients, and dietary therapy was administered to
control blood lipid levels. In the present study, the control group
was administered 75 mg oral aspirin enteric-coated tablets daily
(Harbin Tiandi Pharmaceutical Co., Ltd.; National Medicine
Permission no. H23023503; drug specification, 0.25 g) and, based on
the treatment administered to the control group, the observation
group was administered additional 20 mg oral simvastatin tablets
every night (Shanghai Xinyi Wanxiang Pharmaceutical Co., Ltd.;
National Medicine Permission no. H19980174; drug specification, 5
mg). Both groups were treated continuously for 12 months.
Outcome measurements Determination of
blood lipid
In total, 5 ml fasting venous blood in the early
morning was collected from all patients before and 12 months after
treatment. TC and TG levels were determined using the oxidase
method; high-density lipid cholesterol (HDL-C) and LDL-C levels
were determined using the endpoint method.
Detection of carotid ultrasound
indexes
The shape and internal echo of the bilateral common
carotid, internal carotid, external carotid and vertebral arteries,
as well as the length, thickness (IMT) and number of arterial
plaques were measured and compared before and 12 months after
treatment using HPSONOS-5500 color ultrasound Doppler instrument
(Hewlett-Packard) with high-frequency L-7540 probes at a frequency
of 4-100 mHz. The transverse and longitudinal ultrasound imaging of
the common carotid artery and the posterior wall of the common
carotid artery is shown as two parallel lines separated by lower
echo, and the distance between the two lines was recorded as IMT.
The image 1 cm below the carotid sinus was frozen and measured 5
times in total, and the average value of the left and right side of
10 measurements was recorded as the final IMT.
The criteria for efficacy evaluation were as follows
(9). Significant response, ≥90%
plaque reduction or shrinkage or disappearance; response, 30-89%
plaque reduction or shrinkage; non-response, <30% plaque
reduction or shrinkage or occurrence of cardiocerebrovascular
events. Overall response rate (ORR)=(significant response +
response)/65x100%.
Measurement of inflammatory
factors
Additionally, 3 ml fasting venous blood before and
12 months after treatment was collected from all patients, and
serum was separated by centrifugation at 1,000 x g for 5 min at
4˚C. hs-CRP, tumor necrosis factor-α (TNF-α) and interleukin-6
(IL-6) levels were determined using enzyme-linked immunosorbent
assay (ELISA) kits (R&D Systems, Inc.) of hs-CRP (cat. no.
2119), TNF-α (cat. no. 1576), and IL-6 (cat. no. 3166). All
operations strictly followed the manufacturer's instructions.
Detection of nitric oxide (NO),
D-dimer and fibrinogen
5 ml venous blood before and 12 months after
treatment was collected from all patients. NO level was determined
using an ELISA kit (cat. no. 7945; Roche Diagnostics), and plasma
D-dimer and fibrinogen levels were determined using thrombin
turbidimetry with a Sysmex CA-7000 automatic coagulation analyzer
(Sysmex Shanghai Ltd.) with default parameters. All operations
strictly followed the manufacturer's instructions.
Detection of microemboli
The inspection instrument used was Multi-Dop X4 TCD
instrument (DWL) with 2-MHz pulse wave-measuring probes. Patients
were informed to maintain the supine position, and the probes were
placed on both sides of their head to obtain the optimal blood flow
signal of the middle cerebral artery. The parameters were set to
45-38 mm in depth, 5 mm in spacing and 8 ml in volume. After
monitoring for 30 min, the spectrum and audio frequency of
microemboli were analyzed using transcranial Doppler emboli
detection software (version 8.00) (DWL). The diagnostic criteria
for positive microemboli included the following: i) duration
<300 ms; ii) ≥6 dB of signal intensity higher than background
Doppler blood flow spectrum; iii) single-phase microembolic signal
and above the baseline; iv) a ‘tweet’-like audio signal; and v)
random appearance during the cardiac cycle.
Record of cardiocerebrovascular
events
The incidence of cardiocerebrovascular events during
treatment was recorded. The data were collected during the
treatment period, which was the incidence during 12 months of
continuous treatment.
Statistical analysis
Data were analyzed using SPSS 23.0 (IBM Corp.). The
mean between the two groups was compared using two independent
samples t-test, and paired t-test was used to compare the mean
before and after intervention within the same group. A mixed
two-way ANOVA followed by Bonferroni's correction was used for
within-group and between-group comparisons. Numerical data are
presented as rates or percentages and analyzed using the
χ2 test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Comparison of baseline data between
the two groups
No significant differences were found in terms of
sex, age, primary diseases and original medication between the two
groups, indicating comparability between them (P>0.05; Table I).
 | Table IComparison of general data between the
observation (n=65) and control (n=65) groups. |
Table I
Comparison of general data between the
observation (n=65) and control (n=65) groups.
| | Sex | | Primary disease | Original
medication |
|---|
| Group | M | F | Mean age (years) | CHD | Hypertension | Diabetes | CI | Aspirin | Calcium
antagonist | ACEI | β-Blocker | Nitrate ester |
|---|
| Observation | 35 | 30 | 74.71±5.12 | 17 | 22 | 15 | 20 | 16 | 15 | 21 | 20 | 28 |
| Control | 37 | 28 | 73.88±5.86 | 20 | 24 | 13 | 18 | 17 | 13 | 23 | 17 | 25 |
Simvastatin improves CAP in elderly
patients
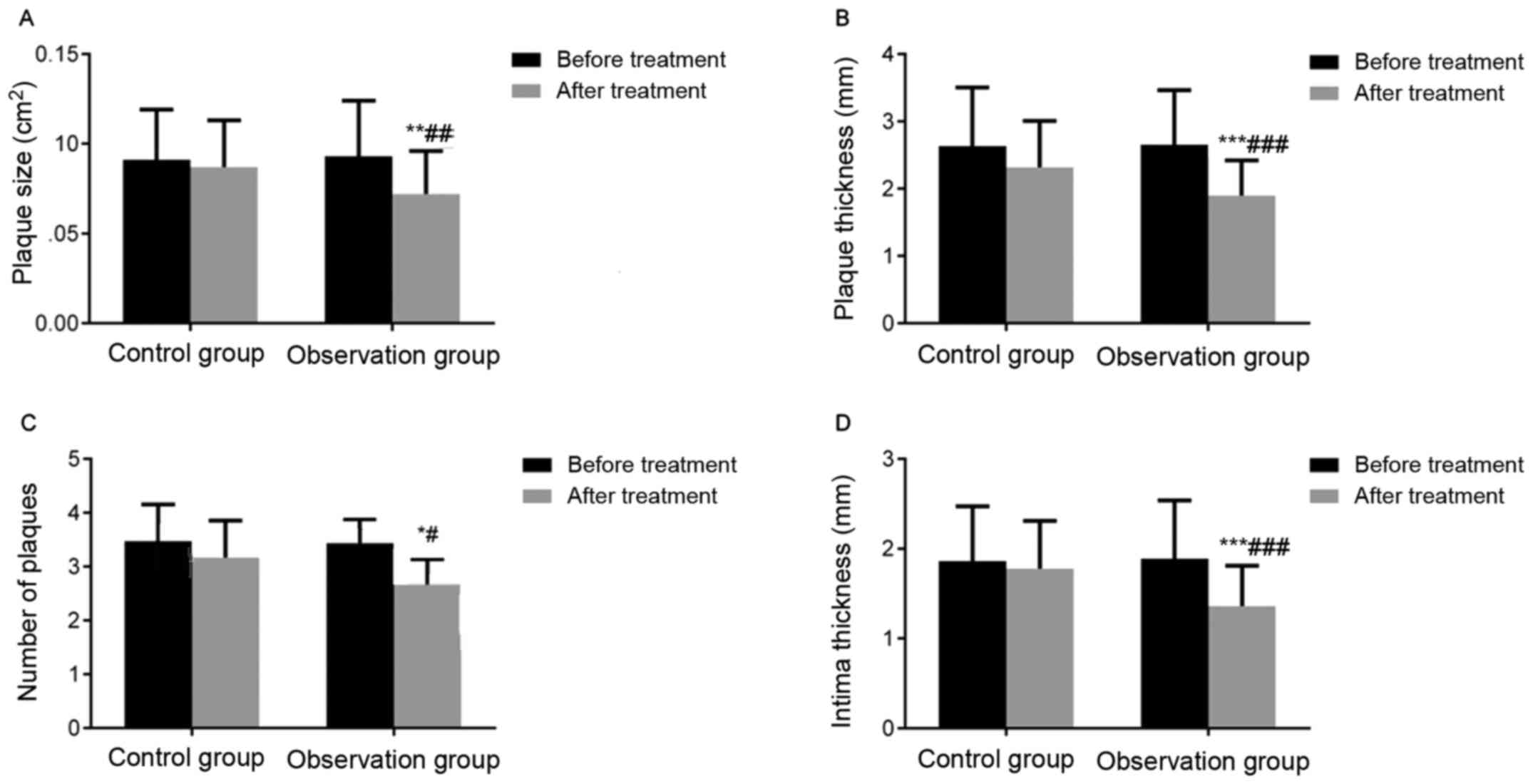
Before treatment, there was no statistically
significant difference in the size, thickness, and number of CAP
and IMT between the two groups (P>0.05). In the observation
group, intragroup comparison showed that the size (P<0.01),
thickness (P<0.001), and number of CAP (P<0.05) and IMT
(P<0.001) significantly decreased after treatment, compared with
before treatment. However, no significant differences were noted in
these indices in the intragroup comparison of the control group
before and after treatment, suggesting that simvastatin improved
CAP in elderly patients in terms of the size and thickness of CAP
and IMT (Fig. 1).
Simvastatin improves blood lipid
levels in elderly patients with CAP
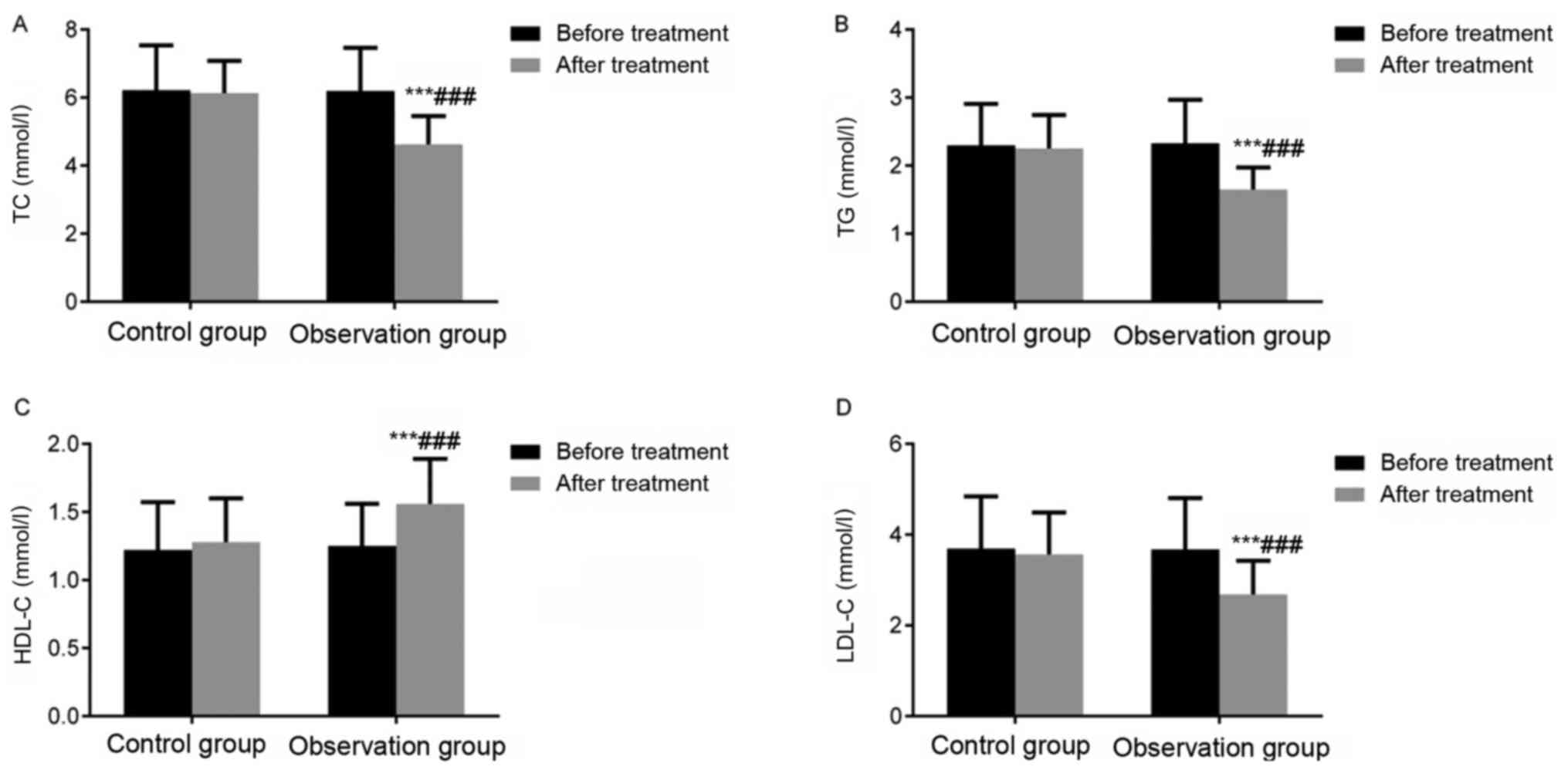
Intragroup comparison of the observation group
revealed that TC, TG and LDL-C levels significantly decreased, and
HDL-C level significantly increased after treatment compared with
before treatment (P<0.001). However, no significant differences
were found in these indices in the intragroup comparison of the
control group before and after treatment. These results suggested
that simvastatin improved blood lipid levels in elderly patients
with CAP (Fig. 2).
Clinical efficacy
ORR of the observation group was 93.85%, which was
significantly higher than that of the control group (80.00%;
P<0.05), suggesting that simvastatin improved the
characteristics of the indices of arterial plaques in elderly
patients with CAP (Table II).
 | Table IIComparison of clinical efficacy
between the observation (n=65) and control (n=65) groups. |
Table II
Comparison of clinical efficacy
between the observation (n=65) and control (n=65) groups.
| Group | Significant
response | Response | Non-response | Overall response
rate |
|---|
| Control group | 30 (46.15) | 22 (33.85) | 13 (20.00) | 52 (80.00) |
| Observation
group | 36 (55.38) | 25 (38.46) | 4 (6.15) | 61
(93.85)a |
Simvastatin reduces serum inflammatory
factor levels in elderly patients with CAP
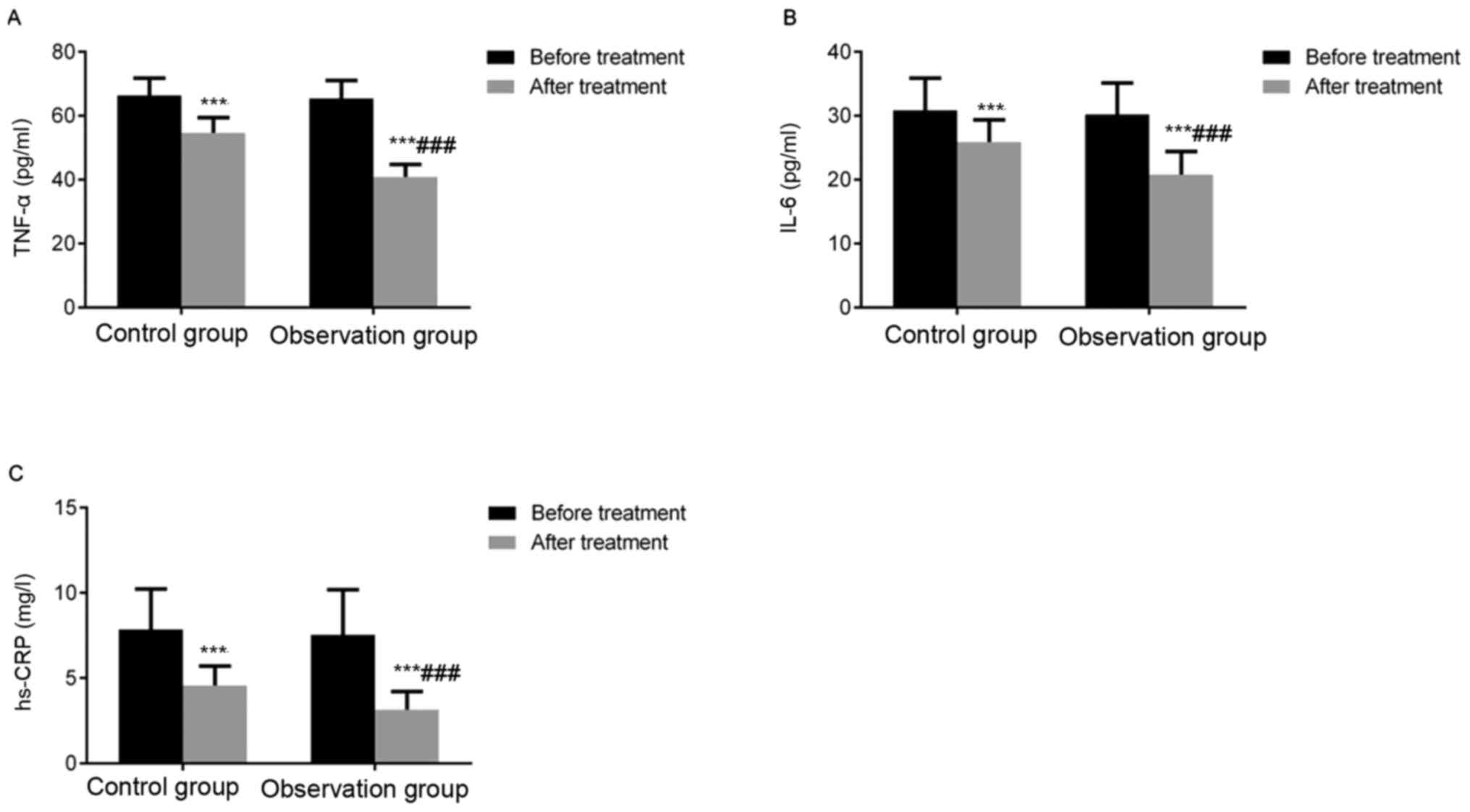
Intergroup comparison revealed no significant
differences in TNF-α, IL-6 and hs-CRP levels before treatment
(P>0.05). Intragroup comparison of both groups indicated that
TNF-α, IL-6 and hs-CRP levels significantly decreased after
treatment compared with before treatment (P<0.001). Intergroup
comparison after treatment revealed that TNF-α, IL-6 and hs-CRP
levels were significantly lower in the observation group than in
the control group (P<0.001). These results indicate that
simvastatin reduces inflammatory factor levels in elderly patients
with CAP (Fig. 3).
Simvastatin increases NO levels and
decreases D-dimer and fibrinogen levels in elderly patients with
CAP
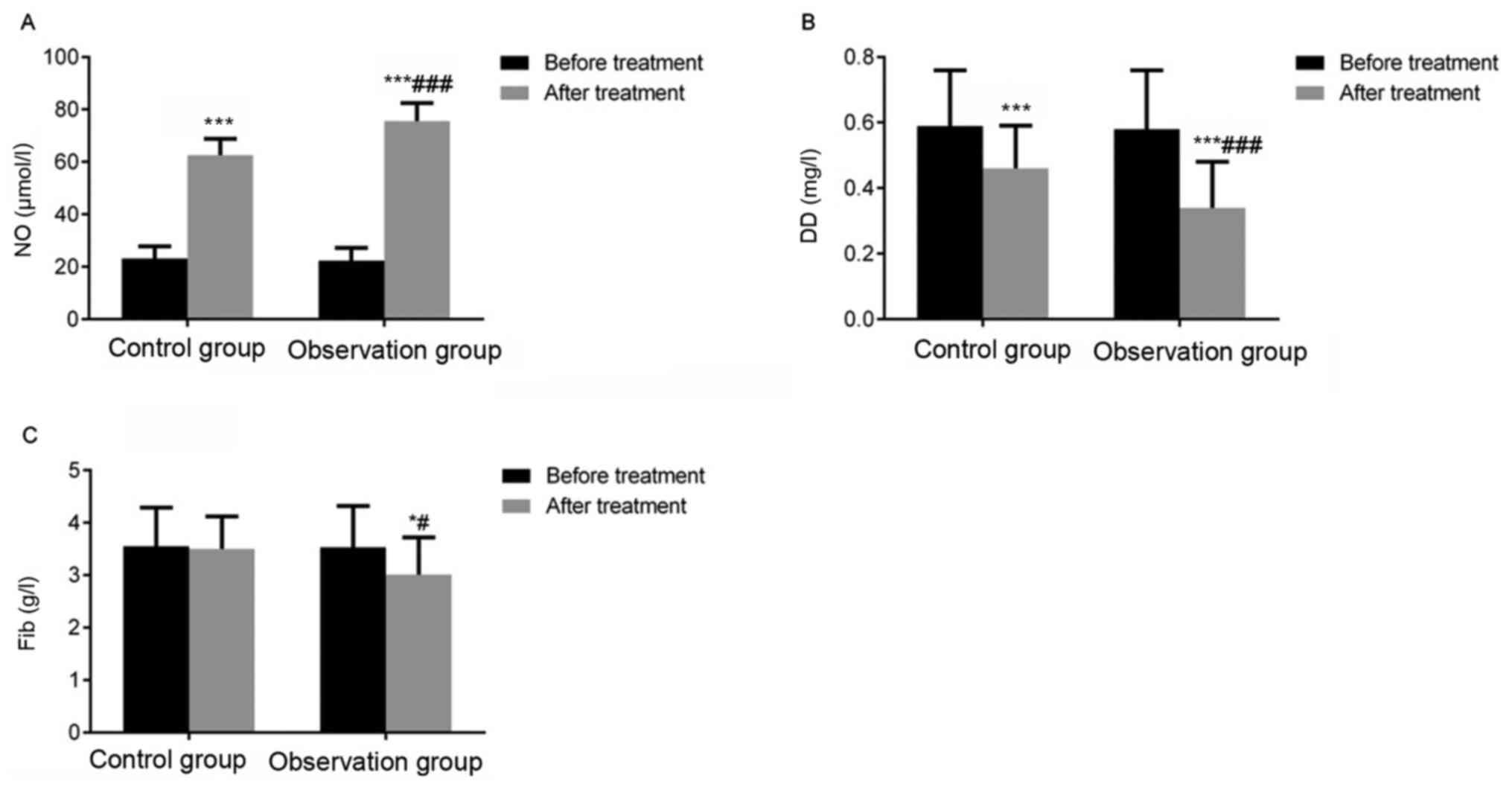
Before treatment, there was no statistically
significant difference in NO, D-dimer, and fibrinogen levels
between the two groups (P>0.05). Intragroup comparison of the
observation group revealed that NO level significantly increased
(P<0.001), and D-dimer (P<0.001) and fibrinogen (P<0.05)
levels significantly decreased after treatment compared with before
treatment (P<0.05). However, no significant differences were
noted in terms of NO, D-dimer and fibrinogen levels in the control
group before and after treatment (P>0.05), suggesting that
simvastatin improves NO, D-dimer and fibrinogen levels in elderly
patients with CAP (Fig. 4).
Simvastatin reduces microemboli
formation in elderly patients with CAP
The rate of microemboli positivity in the
observation group after treatment was significantly lower than that
before treatment and in the control group (P<0.01), suggesting
that simvastatin reduced microemboli formation in elderly patients
with CAP (Table III).
 | Table IIIComparison of microemboli count
between the observation (n=65) and control (n=65) groups. |
Table III
Comparison of microemboli count
between the observation (n=65) and control (n=65) groups.
| | Before treatment | After treatment |
|---|
| Groups | n | % | n | % |
|---|
| Control group | 27 | 41.54 | 20 | 30.77 |
| Observation
group | 25 | 38.46 | 6 | 9.23a,b |
Simvastatin reduces the incidence of
acute cardiocerebrovascular events in elderly patients with
CAP
The incidence of acute cardiocerebrovascular events
was significantly lower in the observation group than in the
control group (P<0.01), suggesting that simvastatin reduces the
incidence of acute cardiocerebrovascular events in elderly patients
with CAP (Table IV).
 | Table IVComparison of acute
cardiocerebrovascular events between the observation (n=65) and
control (n=65) groups. |
Table IV
Comparison of acute
cardiocerebrovascular events between the observation (n=65) and
control (n=65) groups.
| Outcomes | Observation
group | Control group | P-value |
|---|
| All-cause
death | (0) | 2 (3.08) | >0.01 |
| Myocardial
infarction | 1 (1.54) | 6 (9.23) | <0.01 |
| Stroke | 1 (1.54) | 6 (9.23) | <0.01 |
| Overall incidence
of acute cardiocerebrovascular events | 2 (3.08) | 14 (21.54) | <0.01 |
Discussion
Atherosclerosis is a chronic systemic disease
commonly found in the medium-aged and elderly population, and it is
reported that the detection rate of atherosclerosis in individuals
aged 40-49 years is 58.36%, and its incidence increases with age
(10). Carotid arteries, including
bilateral common carotid arteries, bifurcation of the common
carotid artery and extracranial segment of the internal carotid
artery, are the common sites involved in atherosclerosis;
furthermore IMT of ≥1.3 mm at any site is defined as a plaque,
which can result in carotid stenosis and affects peripheral blood
supply, causing adverse cardiocerebrovascular events (11). Factors responsible for CAP formation
are complicated, and CAP is generally believed to be attributed to
varying pathogeneses. The recognized mechanisms include mechanical
(such as hypertension and carotid pulse pressure), inflammatory and
physicochemical) factors (including lipid metabolism disorders and
elevated fibrinogen) (12). An
elevated cholesterol level caused by impaired lipid metabolism is
considered the initiating factor for atherosclerosis, and chronic
inflammation is critical for its continuous development (13). Therefore, regulating lipids,
reducing the inflammatory response and decreasing fibrinogen levels
may be key in improving disease-related symptoms and prognostic
outcomes during the treatment of elderly patients with CAP.
Simvastatin is a member of the statin family.
Numerous animal experiments and clinical trials have reported that
statins have potent anti-atherosclerotic effects, and the
underlying mechanisms may involve lipid-regulation and
lipid-lowering effects, antiplatelet aggregation and thrombosis,
maintenance of plaques, and improvement of endothelial function
(5,14,15).
During lipid lowering, simvastatin effectively reduces the TC
concentration in the blood and prevent lipid production, including
TC, TG and LDL production, by lowering the reductase level of
hydroxymethylglutaryl coenzyme A and blocking cholesterol synthesis
(16). Relevant basic experiments
and clinical studies have confirmed that simvastatin effectively
reduces and eliminates CAPs, and consequently decreases the
incidence of acute cardiocerebrovascular events to improve the
prognosis of patients (17). In
addition, simvastatin exhibits an anti-inflammatory effect
primarilu via mechanisms such as reduction of inflammatory
infiltrating cell count, inhibition of adhesion molecule function
on isopentenylated G protein and integrin, and reduction of CRP
level (18). Currently, simvastatin
is widely used in the clinical treatment of diseases such as
cardiocerebrovascular diseases, atherosclerosis and myocardial
ischemia (19). In the present
study, the clinical control design was used to compare the effects
of conventional therapy vs. simvastatin on CAP in elderly patients.
The results indicated that the size, thickness and number of CAP
and IMT were significantly decreased, TC, TG and LDL-C levels were
significantly decreased, and HDL-C level was significantly
increased in the observation group after treatment, compared with
those in the control group. Furthermore, simvastatin treatment can
reduce the size and number of CAPs with its lipid-lowering effect,
thus producing a definite effect on CAP.
Chronic inflammatory response is one of the major
mechanisms involved in carotid atherosclerosis in the elderly.
After vascular endothelial injury, inflammatory response occurs in
the vascular wall resulting in the production of various adhesion
molecules and increased inflammatory factors such as TNF-α, IL-6
and CRP. TNF-α and IL-6, among other inflammatory factors, enhance
the local inflammatory response, resulting in plaque complications
and decreased stability (20).
Unstable plaques are more prone to breakage, shedding and
metastasis, causing vascular embolization at the distal end and
increasing the risk of cardiocerebrovascular events (21). CRP binds lipoproteins to activate
the complement system and produce aggressive complexes by binding
to ligands (apoptotic and necrotic cells, or phosphocholine of
invading pathogens) and terminal protein C, which can induce
vascular damage (22). In addition,
CRP may enhance the inflammatory response and aggravate vascular
inflammation damage. Detection of hs-CRP is more sensitive than
that of CRP, allowing the determination of even low concentrations
of CRP (0.1-10 mg/l) (22). Prior
evidence (23) supports that
patients with diabetes with hs-CRP level of ≥2 mg/l are more likely
to develop carotid atherosclerosis, and hs-CRP level was associated
with the progression of carotid atherosclerosis and plaque count.
In the current study, inflammatory factors (TNF-α, IL-6 and hs-CRP)
levels decreased in the observation group after treatment,
suggesting that simvastatin reduced serum inflammatory factor
levels and consequently the inflammatory response in elderly
patients with CAP.
NO is a commonly used indicator for vascular
endothelial function and is a vasodilator. Decreased NO level is
associated with the degree of vascular endothelial cell injury
(24). D-Dimer is one of the fibrin
degradation products, which may be elevated due to coagulation
dysfunction and microthrombosis (25). In addition, fibrinogen is one of the
independent predictors of atherosclerosis and is primarily produced
in the liver. Fibrinogen promotes platelet aggregation and
thrombosis, which serves an important role in atherosclerotic
lesion formation, and is associated with disease severity (26). The present study demonstrated that
increased NO level and decreased D-dimer and fibrinogen levels in
the observation group were more significant than those in the
control group. Further, the decreased rate of microemboli
positivity in the observation group was more notable than that in
the control group after treatment. The aforementioned findings
support that simvastatin improves serum NO level, protects vascular
endothelium and reduces serum D-dimer and fibrinogen levels, which
consequently improves blood coagulation status and eliminates
microemboli.
Carotid atherosclerosis is the most critical risk
factor for cardiocerebrovascular events and is an important index
reflecting systemic arteriosclerosis due to the superficial
location of the carotid artery and easy identification of CAP
(27). A prospective cohort study
showed that the incidences of all-cause death and
cardiocerebrovascular events in patients with CAP were 5.50 and
3.80%, respectively, which were higher than those in the non-plaque
group (1.50 and 1.40%, respectively) (28). A Cox proportional hazard regression
model determined that CAP was an independent risk factor for
all-cause death and cardiocerebrovascular events with 95%
confidence intervals of (1.160-2.395) and (1.312-2.876),
respectively (28). The present
study showed that the incidences of acute cardiocerebrovascular
events were lower in the observation group than in the control
group following treatment, indicating that simvastatin can prevent
the development of acute cardiocerebrovascular events. This is
possibly attributed to the multiple mechanisms of simvastatin in
regulating lipids, reducing inflammatory response, eliminating
microemboli, protecting vascular endothelium and improving blood
coagulation status, thus facilitating the reduction of mortality
and prevention of acute heart and brain events.
In summary, continuous use of statins may stabilize
and dissolve CAPs in elderly patients and reduce acute
cardiocerebrovascular events by lowering blood lipid levels. It was
demonstrated that simvastatin reduces blood lipid levels, number
and size of plaques, the inflammatory response, microemboli
formation in elderly patients with CAP and the risk of
cardiovascular events, which is the primary novelty of this study.
The present findings suggest that simvastatin treatment for elderly
patients with atherosclerotic plaque can effectively reduce the
risk of cardiocerebrovascular events. The present study was a
preliminary efficacy study, and only the changes in the levels of
inflammatory factors and other indicators between the two groups
were preliminarily observed. Whether there is correlation between
factors, and whether simvastatin primarily functions through that
signaling pathway was not included in the present study, and the
specific signaling pathways mediated by these factors are still
unknown. In addition, the observation time was set to 1 year, and
the research time is relatively short. In future studies, the
research time should be increased, and the main pathway of its
function should be detected. Part of the study on the mechanism is
conjecture, and the correctness of the aforementioned hypotheses
should be verified in a multi-center study with and expanded sample
size and a prolonged observation time.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HZ and QL conceived the study and designed the
experiments. MJ and HH contributed to data collection, performed
data analysis and interpreted the results. HZ and QL confirmed the
authenticity of all the raw data. HZ wrote the manuscript. QL
contributed to the critical revision of article. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Medical Ethics
Committee of Baoji City People's Hospital (Baoji, China) and all
patients signed informed consent and volunteered to participate in
this study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rafailidis V, Chryssogonidis I, Tegos T,
Kouskouras K and Charitanti-Kouridou A: Imaging of the ulcerated
carotid atherosclerotic plaque: A review of the literature.
Insights Imaging. 8:213–225. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kwee R, Oostenbrugge R, Hofstra L, van
Engelshoven J, Mess W, Wildberger J and Kooi ME: Noninvasive
Imaging of Carotid Atherosclerosis, pp497-525, 2011.
|
|
3
|
Chen SX, Hong GX, Li ZH and Yang ZY: High
resolution MRI observation on intracranial atherosclerotic plaque
and risk factors in patients with recurrent cerebral infarction.
Chin J Med Imaging Technol. 36:2020.
|
|
4
|
Tang QH and Luo KQ: Color doppler
ultrasound in detection of carotid atherosclerotic stenosis degree
and plaque distribution in patients with myocardial infarction
associated by hypertension. Med Pharm J Chin PLA. 31:44–47.
2019.
|
|
5
|
Eilenberg W, Stojkovic S, Kaider A,
Kozakowski N, Domenig CM, Burghuber C, Nanobachvili J, Huber K,
Klinger M, Neumayer C, et al: NGAL and MMP-9/NGAL as biomarkers of
plaque vulnerability and targets of statins in patients with
carotid atherosclerosis. Clin Chem Lab Med. 56:147–156.
2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Huang HY and Yan WM: Comparison of the
efficacy and safety of 4 kinds of statins in the treatment of
atherosclerosis. China Pharm. 27:5100–5103. 2016.
|
|
7
|
Zhang N, Ma Y and Wang R: Pharmacoeconomic
evaluation of simvastatin capsules and atorvastatin calcium tablets
in the treatment of patients with atherosclerosis. China J Pharm
Econ. 16:31–34. 2021.
|
|
8
|
Wang WW and Wang XD: Summary of the 6th
national cerebrovascular disease academic conference. Chin J
Neurol. 37:346–348. 2004.
|
|
9
|
Zhao X, Hippe DS, Li R, Canton GM, Sui B,
Song Y, Li F, Xue Y, Sun J, Yamada K, et al: Prevalence and
characteristics of carotid artery high-risk atherosclerotic plaques
in chinese patients with cerebrovascular symptoms: A Chinese
atherosclerosis risk evaluation ii study. J Am Heart Assoc.
6(e005831)2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Cao Y, Sun Y, Zhou B, Zhao H, Zhu Y, Xu J
and Liu X: Atherosclerotic plaque burden of middle cerebral artery
and extracranial carotid artery characterized by MRI in patients
with acute ischemic stroke in China: Association and clinical
relevance. Neurol Res. 39:344–350. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Alloza I, Goikuria H, Idro JL, Triviño JC,
Fernández Velasco JM, Elizagaray E, García-Barcina M,
Montoya-Murillo G, Sarasola E, Vega Manrique R, et al: RNAseq based
transcriptomics study of SMCs from carotid atherosclerotic plaque:
BMP2 and IDs proteins are crucial regulators of plaque stability.
Sci Rep. 7(3470)2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ni T, Chen M, Yang K, Shao J, Fu Y and
Zhou W: Association of CD147 genetic polymorphisms with carotid
atherosclerotic plaques in a Han Chinese population with cerebral
infarction. Thromb Res. 156:29–35. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Schaefer CA, Blatzheim AK, Passon SG,
Pausewang KS, Schahab N, Nickenig G, Skowasch D, Schueler R,
Hammerstingl C and Pingel S: Modulation of carotid strain by statin
therapy in atherosclerosis patients. Vasa. 46:108–115.
2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Natarajan P, Young R, Stitziel NO,
Padmanabhan S, Baber U, Mehran R, Sartori S, Fuster V, Reilly DF,
Butterworth A, et al: Polygenic risk score identifies subgroup with
higher burden of atherosclerosis and greater relative benefit from
statin therapy in the primary prevention setting. Circulation.
135:2091–2101. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kocaman SA, Baysan O, Çetin M, Kayhan
Altuner T, Polat Ocaklı E, Durakoğlugil ME, Erdoğan T and Karaoğuz
MR: An increase in epicardial adipose tissue is strongly associated
with carotid-intima media thickness and atherosclerotic plaque, but
LDL only with the plaque. Anatol J Cardiol. 17:56–63.
2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ahmed AM: Inhibition of inducible nitric
oxide synthase (iNOS) by simvastatin attenuates cardiac hypertrophy
in rats. Folia Morphol (Warsz). 76:15–27. 2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ngo-Metzger Q and Gottfredson R: Statin
Use for the primary prevention of cardiovascular disease in adults.
Am Fam Physician. 96:805–806. 2017.PubMed/NCBI
|
|
18
|
Feng Y, Lei B, Zhang F, Niu L, Zhang H and
Zhang M: Anti-inflammatory effects of simvastatin during the
resolution phase of experimentally formed venous thrombi. J
Investig Med. 65:999–1007. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Środa-Pomianek K, Michalak K, Palko-Łabuz
A, Uryga A, Szczęśniak-Sięga B and Wesołowska O: Simvastatin
strongly augments proapoptotic, anti-inflammatory and cytotoxic
activity of oxicam derivatives in doxorubicin-resistant colon
cancer cells. Anticancer Res. 39:727–734. 2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Stefanutti C, Mazza F, Pasqualetti D, Di
Giacomo S, Watts GF, Massari MS, de Neve J, Morozzi C and Fischer
M: Lipoprotein apheresis downregulates IL-1α, IL-6 and TNF-α mRNA
expression in severe dyslipidaemia. Atheroscler Suppl. 30:200–208.
2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Poredos P, Spirkoska A, Lezaic L, Mijovski
MB and Jezovnik MK: Patients with an inflamed atherosclerotic
plaque have increased levels of circulating inflammatory Markers. J
Atheroscler Thromb. 24:39–46. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Braig D, Nero TL, Koch HG, Kaiser B, Wang
X, Thiele JR, Morton CJ, Zeller J, Kiefer J, Potempa LA, et al:
Transitional changes in the CRP structure lead to the exposure of
proinflammatory binding sites. Nat Commun. 8(14188)2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Pleskovič A, Letonja M, Vujkovac AC,
Nikolajević Starčević J, Gazdikova K, Caprnda M, Gaspar L, Kruzliak
P and Petrovič D: C-reactive protein as a marker of progression of
carotid atherosclerosis in subjects with type 2 diabetes mellitus.
Vasa. 46:187–192. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Jorgensen AL: Contrast-induced
nephropathy: Pathophysiology and preventive strategies. Crit Care
Nurse. 33:37–46. 2013.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Yang N, Hao J and Zhang D: Antithrombin
III and D-dimer levels as indicators of disease severity in
patients with hyperlipidaemic or biliary acute pancreatitis. J Int
Med Res. 45:147–158. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Schreiner PJ, Appiah D and Folsom AR:
Gamma prime (γ') fibrinogen and carotid intima-media thickness: The
atherosclerosis risk in communities study. Blood Coagul
Fibrinolysis. 28:665–669. 2017.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Clarke R, Du H, Kurmi O, Parish S, Yang M,
Arnold M, Guo Y, Bian Z, Wang L, Chen Y, et al: Burden of carotid
artery atherosclerosis in Chinese adults: Implications for future
risk of cardiovascular diseases. Eur J Prev Cardiol. 24:647–656.
2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Li W, Ma F, Jiang YM, Li JJ, Song L, Chen
SH, Liu XM, Li XQ and Wu SL: Association between carotid artery
plaques and all-cause mortality and cardiovascular events. Zhonghua
Xin Xue Guan Bing Za Zhi. 45:1086–1090. 2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|