Introduction
According to the Hepa Health project, a study
conducted in 35 European and 5 Asian countries which is considered
by the European Association for the Study of the Liver (EASL), the
prevalence of liver cirrhosis and other chronic liver disease
increases to some extent from Western European countries to Eastern
European countries. However, the highest prevalence is found in
Central European countries, including Romania and Austria with over
1,100 cases per 100,000 individuals. In addition, the highest
mortality rates for liver disease were identified in Romania (36
deaths per 100,000), Lithuania and Hungary (approximately 20 deaths
per 100,000) (1).
According to a systematic study conducted between
2005 and 2015 by the European Center for Disease Prevention and
Control (ECDC), countries in Southern and Eastern Europe had a
higher prevalence of hepatitis B virus (HBV) and hepatitis C virus
(HCV) than northern and western countries. The prevalence of HBV
ranged from 0.1% in Ireland to 4.4% in Romania. Greece and Romania
have the highest prevalence of 3.3 and 4.4%, respectively, while
the other countries have a prevalence of approximately 1%. The same
countries registered the highest prevalence of HCV (2.2 and 3.2%)
(2).
Spontaneous bacterial peritonitis (SBP) is one of
the most common complications of patients with cirrhosis and
ascites, with an incidence between 10-30% and an estimated
in-hospital mortality rate of 20% (3). According to the European guideline,
the diagnosis is based on a polymorphonuclear leukocyte (PMN) value
in ascites fluid >250 mm3 in the absence of secondary
causes of intra-abdominal infection. There is a variant in which
the PMN value is <250 mm3, but with present culture
called monomicrobial bacterascitis (4). Despite the diagnostic and treatment
recommendations in the guideline, in a retrospective study made in
the USA, only 52.4% of patients diagnosed with SBP met the criteria
and only 67.3% of patients received appropriate treatment (5). The diagnostic challenge lies in the
fact that the symptomatology of patients with SBP varies from
typical symptoms to their partial or complete absence. Therefore, a
prompt diagnosis and effective treatment can reduce the poor
outcome rate (6).
Recent research has focused on identifying
non-invasive parameters useful in SBP prediction. Multiple
laboratory tests and clinical factors have been identified as
predictive factors: international normalized ratio (INR) (7), creatinine, total bilirubin (BT), serum
white blood cells (WBC), prothrombin time (8) C-reactive protein (CRP), total platelet
count (PLT) (9) severe ascites
(7), Child Pugh score (10) and Model for End-Stage Liver Disease
(MELD) score (10,11).
The aim of our study was to identify other
predictive factors in the occurrence of SBP in adult Romanian
population, given that the available data are numerous but
contradictory. There is a high need for an early diagnosis
considering the high mortality rate mentioned above.
Patients and methods
Patients
This study has a retrospective, observational, and
non-interventional design and was approved by the Emergency
Clinical Hospital ‘St. Apostle Andrew’ Constanta Ethics Committee.
Although not mandatory for observational, non-interventional
studies at the Emergency Clinical Hospital ‘St. Apostle Andrew’
from Constanta, a university hospital, all admitted patients signed
informed consent by which they agreed that their data be available
for academic and scientific purposes.
The study included 216 patients with liver cirrhosis
of various etiologies (with a mean age of 61.2±10.67 years, 65.7%
males and 34.3% females), hospitalized at the County Emergency
Clinical Hospital, Constanța, between December 2019 and January
2010. Patients >18 years were divided into two groups: 72
patients with SBP and 144 patients without SBP. The diagnosis of
SBP was performed according to the European guideline, namely a PMN
value >250 mm3 with or without a positive culture.
Patients with intra-abdominal surgical causes of peritonitis or
other infectious causes (respiratory, urinary) were excluded. Data
from the first day of admission regarding age, sex, etiology of
cirrhosis, laboratory blood tests and ascites fluid tests, Child
Pugh score, complications and comorbidities, were recorded from the
medical files. The neutrophil-to-lymphocyte ratio was calculated by
dividing the neutrophil count by the lymphocyte count.
Statistical analysis
The software used was SPSS version 23 (IBM Corp.).
Numerical data were synthesized as mean and standard deviation and
qualitative data were recorded as percentages. Differences between
the two groups were tested using the independent samples t-test,
Mann-Whitney U test, and Pearson's Chi-square test. Univariate
logistic regression analysis was used to compare the two groups.
Multivariate logistic regression analysis was performed to identify
predictive factors for SBP occurrence. In order to test the
diagnostic accuracy of the evaluated markers for SBP diagnosis, we
used the area under the curve (AUC). The optimum cut-off value was
identified using Youden index. For the optimal cut-off value, the
sensitivity, and specificity were calculated. P-values of <0.05
were considered statistically significant.
Results
Patient characteristics
Patient characteristics are described by comparison
between the group of patients with SBP and those without SBP. Of
the 216 patients with cirrhosis, 72 patients (33.3%) had SBP and
144 patients did not have SBP (66.67%). In the group of patients
who had SBP, 33.3% were women and 66.7% were men, with a mean age
of 59.29±11.30 years. Among the patients without SBP 34.7% were
women and 65.3% were men, with a mean age of 62.23±10.25 years.
The most common etiologies of liver cirrhosis in the
group of patients with SBP were represented by: Alcoholic (52.8%),
HCV (16.7%), mixed (13.9%), HBV (12.5%) and others (4.1%).
Regarding the mixed etiology, 6 cases had HCV+alcohol, 4 cases had
HBV+HCV and 3 cases with autoimmune etiology were classified as
others. In the group of patients without SBP, the causes of liver
cirrhosis were represented by: Alcoholic (39.6%), mixed (27.1%),
HCV (19.4%), HBV (11.8%) and others (2.1%). For mixed etiology,
there were 10 cases with HBV+alcohol, 16 cases with HCV+alcohol, 5
cases with HBV+HCV, 8 cases with HBV+HDV and 3 cases were
classified as others (2 cases with autoimmune etiology and 1 case
of cryptogenic etiology). The data are shown in Table I.
 | Table ICharacteristics of the patients with
and without SBP by comparison. |
Table I
Characteristics of the patients with
and without SBP by comparison.
| Category | Total (n=216) | With SBP (n=72) | Without SBP
(n=144) | P-value |
|---|
| Age, years (mean ±
SD) | 61.25±10.67 | 59.29±11.30 | 62.23±10.25 | 0.061 |
| Sex, n/total (%) | | | | |
|
Female | 74/216 (34.3) | 24/72 (33.3) | 50/144 (34.7) | 0.839 |
|
Male | 142/216 (65.7) | 48/72 (66.7) | 94/144 (65.3) | |
| Etiology, n/total
(%) | | | | |
|
Alcoholic | 95/216 (44.0) | 38/72 (52.8) | 57/144 (39.6) | |
|
Viral B | 26/216 (12.0) | 9/72 (12.5) | 17/144 (11.8) | 0.217 |
|
Viral C | 40/216 (18.5) | 12/72 (16.7) | 28/144 (19.4) | |
|
Mixed
(alcoholic+viral B/C, viral B+C, viral B+D) | 49/216 (22.7) | 10/72 (13.9) | 39/144 (27.1) | |
|
Others | 6/216 (2.8) | 3/72 (4.1) | 3/144 (2.1) | |
| Child Pugh, n/total
(%) | | | | |
|
Grade A | 4/216 (1.9) | 2/72 (2.8) | 2/144 (1.4) | |
|
Grade B | 120/216 (55.6) | 19/72 (26.4) | 101/144 (70.1) | <0.001 |
|
Grade C | 92/216 (42.6) | 51/72 (70.8) | 41/144 (28.5) | |
| Serum WBC
(103/µl) | 8.44±4.40 | 12.61±4.24 | 6.36±2.53 | <0.001 |
| PLT
(103/µl) | 137.22354.9 | 115.32±32.56 | 147.07±57.46 | <0.001 |
| Hb (mg/dl) | 10.91±1.54 | 11.09±1.70 | 10.82±1.45 | 0.222 |
| BT (mg/dl) | 3.1±1.97 | 4.45±2.30 | 2.44±1.36 | <0.001 |
| Serum albumin
(g/dl) | 2.62±0.51 | 2.49±0.44 | 2.68±0.54 | <0.001 |
| INR | 1.82±0.62 | 2.24±0.83 | 1.61±0.34 | <0.001 |
| Creatinine
(mg/dl) | 1.31±0.96 | 1.53±1.19 | 1.17±0.69 | <0.001 |
| AST (U/l) | 77.46±37.96 | 78.32±36.68 | 77.03±38.71 | 0.815 |
| ALT (U/l) | 46.15±23.0 | 49.01±23.42 | 44.72±22.82 | 0.198 |
| ESR (mm/h) | 30.61±12.04 | 42.11±12.09 | 24.85±6.76 |
<0.001 |
| NLR | 2.48±1.18 | 3.67±1.13 | 1.87±0.49 | |
| Ascites WBC
(cells/mm3) | 615.94±933.648 | 1611±1060.17 | 117.98±58.73 |
<0.001 |
| PMN
(cells/mm3) | 442.02±826.535 |
1,266.05±1016.55 | 25.40±23.97 |
<0.001 |
| Na (mmol/l) | 132±7.59 | 128.06±9.96 | 133.97±5.07 |
<0.001 |
| AR (mmol/l) | 21.3±4.43 | 19.85±6.02 | 22.02±3.15 | 0.001 |
There was a significant difference in Child Pugh
class B and C scores in patients with SBP and those without SBP
(26.4 vs. 70.1%, 70.8 vs. 28.5%, P<0.001). In contrast, there
were no significant differences in age, sex or etiology of liver
cirrhosis (P=0.061, P=0.839 and P=0.217, respectively) between the
two groups.
Patients in the SBP group had significantly higher
serum WBC, BT, INR, creatinine, erythrocyte sedimentation rate
(ESR), neutrophil-to-lymphocyte ratio (NLR), and PMN than patients
in the non-SBP group (all with P<0.001). In addition, the mean
values of PLT, serum albumin, sodium (Na), and alkaline reserve
(AR) were significantly lower in patients with SBP than those
without SBP (P<0.001 for the first 4 variables, P=0.001 for the
last one). There were no significant differences in the mean values
of hemoglobin (Hb), aspartate aminotransferase (AST), and alanine
aminotransferase (ALT), (P=0.222, P=0.815 and P=0.198,
respectively).
Regarding the complications, there were significant
differences between the group with SBP and the group without SBP
regarding upper gastrointestinal bleeding (UGIB) (66.7 vs. 22.9%,
P<0.001) but not in the case of hepatic encephalopathy (HE),
(34.7 vs. 31.3%, P=0.607). Patients without SBP had a higher
proportion of cardiac comorbidities than patients with SBP (42.4
vs. 25%, P=0.016). There were no significant differences between
the two groups regarding pulmonary (P=0.326), renal (P=0.661),
digestive (P=0.682) or metabolic (P=0.298) comorbidities (Table II).
 | Table IICharacteristics of the patients with
and without SBP regarding complications and comorbidities. |
Table II
Characteristics of the patients with
and without SBP regarding complications and comorbidities.
| Category | With SBP
(n=72) | Without SBP
(n=144) | P-value |
|---|
| Complications,
n/total (%) | | | |
|
UGIB | 48/72 (66.7%) | 33/144 (22.9%) |
<0.001 |
|
HE | 25/72 (34.7%) | 45/144 (31.3%) | 0.607 |
| Comorbidities,
n/total (%) | | | |
|
Pulmonary | 11/72 (15.3%) | 30/144 (20.8%) | 0.326 |
|
Renal | 20/52 (27.8%) | 36/144 (25%) | 0.661 |
|
Digestive | 25/72 (34.7%) | 46/144 (31.9%) | 0.682 |
|
Metabolic | 13/72 (18.1%) | 35/144 (24.3%) | 0.298 |
|
Cardiac | 18/72 (25%) | 61/144 (42.4%) | 0.016 |
Univariate logistic regression for
predictive factors in SBP occurrence
Using univariate analysis, 12 variables were
identified as predictive factors in the occurrence of SBP: Serum
WBC (OR, 1.61), PLT (OR, 0.98), BT (OR, 1.79), serum albumin (OR,
0.46), INR (OR, 6.82), creatinine (OR, 1.52), ESR (OR, 1.30), serum
Na (OR, 0.89), AR (OR, 0.89), NLR (OR, 138.2), UGIB (OR, 6.72), and
cardiac comorbidities (OR, 0.45) (Table III).
 | Table IIIUnivariate logistic regression
analysis of predictive factors for SBP occurrence. |
Table III
Univariate logistic regression
analysis of predictive factors for SBP occurrence.
| Parameters | P-value | OR value | 95% CI |
|---|
| Serum WBC
(103/µl) | <0.001 | 1.61 | 1.42-1.83 |
| PLT
(103/µl) | <0.001 | 0.98 | 0.98-0.99 |
| BT (mg/dl) | <0.001 | 1.79 | 1.49-2.16 |
| Serum albumin
(g/dl) | <0.001 | 0.46 | 0.25-0.82 |
| INR | <0.001 | 6.82 | 3.50-13.29 |
| Creatinine
(mg/dl) | <0.001 | 1.52 | 1.13-2.05 |
| ESR (mm/h) | <0.001 | 1.30 | 1.20-1.40 |
| Na (mmol/l) | <0.001 | 0.89 | 0.85-0.93 |
| AR (mmol/l) | 0.001 | 0.89 | 0.83-0.95 |
| NLR | <0.001 | 138.2 | 26.4-724.2 |
| UGIB | <0.001 | 6.72 | 3.59-12.57 |
| Cardiac
comorbidities | 0.013 | 0.45 | 0.24-0.85 |
Multivariate analysis
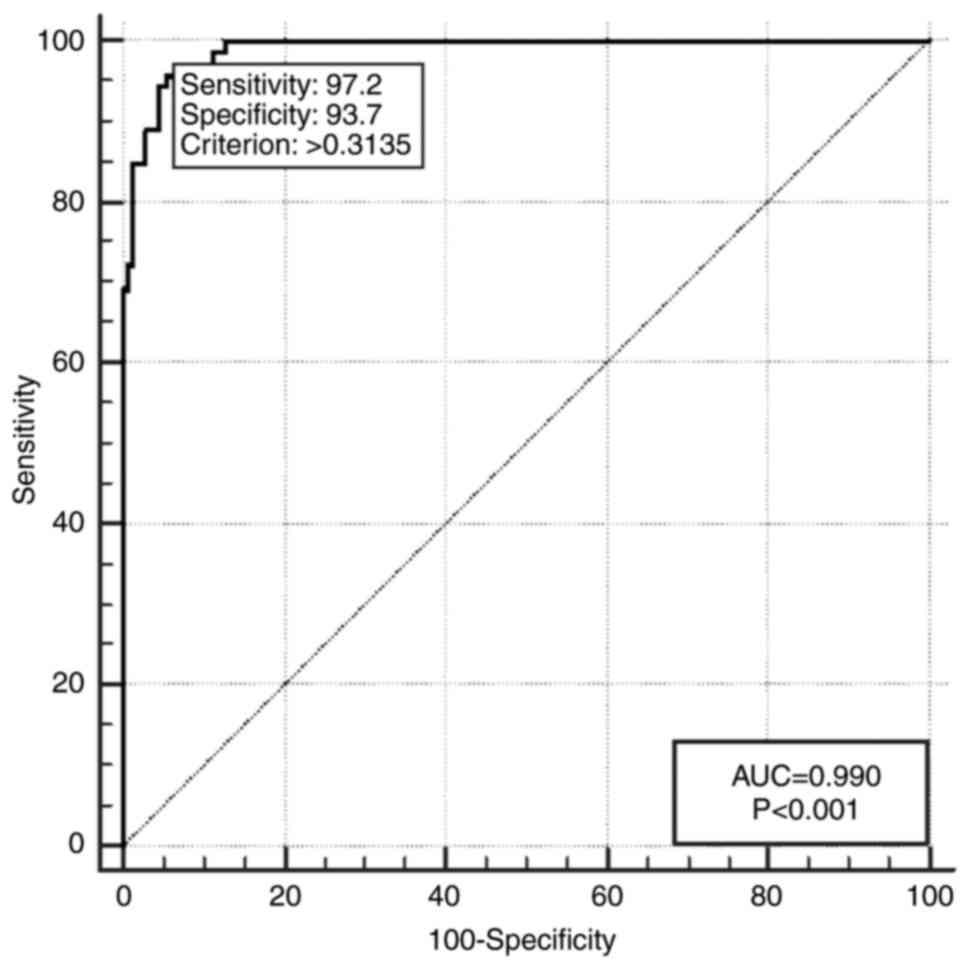
ESR (OR, 1.30) and NLR (OR, 371.36) were identified
as independent predictive factors in the occurrence of SBP. The
logistic regression model obtained from ESR and NLR explains 64.04%
(Cox & Snell R2) to 88.95% (Nagelkerke
R2). In addition, the program reports AUC=0.990; 95% CI,
0.965-0.999 constructed for the combination of independent
variables (Fig. 1 and Table IV).
 | Table IVMultivariate analysis by logistic
regression for SBP prediction. |
Table IV
Multivariate analysis by logistic
regression for SBP prediction.
| Variable | OR | 95% CI | P-value |
|---|
| ESR | 1.3023 | 1.1448-1.4815 | 0.001 |
| NLR | 371.3660 |
26.1400-5275.9269 | <0.001 |
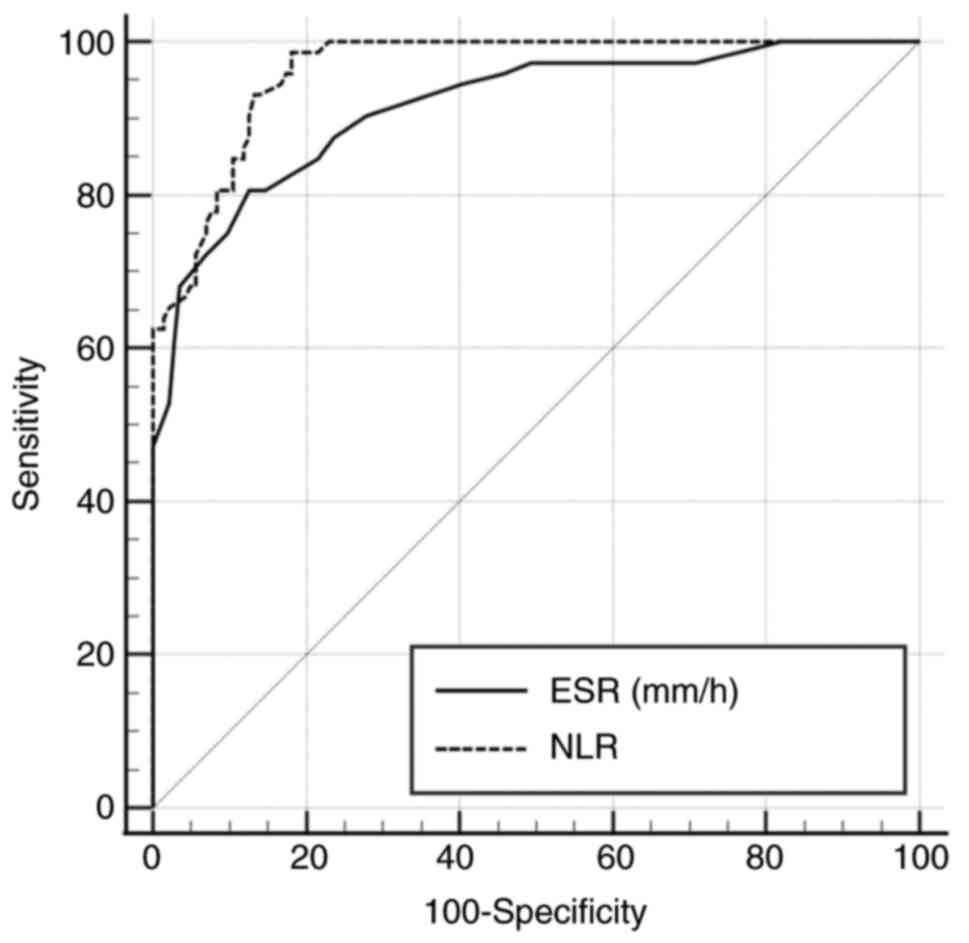
Using receiver operating characteristic (ROC)
statistics, the sensitivity and specificity of ESR, at a cut-off
value of >33 mm/h, for the diagnosis of SBP, were 80.56 and
87.50%, respectively. The sensitivity and specificity of NLR, at a
cut-off value of >2.4, were 98.61 and 81.94%, respectively
(Fig. 2 and Table V).
 | Table VDiagnostic accuracy of ESR and NLR to
predict occurrence of SBP. |
Table V
Diagnostic accuracy of ESR and NLR to
predict occurrence of SBP.
| Variable | AUC | P-value | 95% CI | Cut-off | Sensitivity | Specificity |
|---|
| ESR | 0.916 | <0.001 | 0.870-0.949 | >33 | 80.56 | 87.50 |
| NLR | 0.963 | <0.001 | 0.928-0.984 | >2.4 | 98.61 | 81.94 |
Discussion
Patients with liver cirrhosis are prone to
infections, SBP being among the most common, with a variable
prevalence but with a high mortality rate (6). For this reason, it is necessary to
identify non-invasive, inexpensive, easy-to-achieve factors that
are associated with SBP and have a predictive role.
The etiology of liver cirrhosis varies
geographically. The most common etiology in our study was found to
be alcohol, similar to that in a study by Gonçalves et al
(12) in Brazil. However, our
findings differed in studies from Africa, (7,13)
where leading etiology was HBV.
Our study showed that there was a significant
difference between the mean values of BT, creatinine, INR, serum
WBC, serum albumin and PLT in the SBP group compared to those
without SBP. The mean values of BT, creatinine, INR, and serum WBC
were significantly higher, and the mean PLT was significantly
lower, in a group of 59 patients with SBP from a study with 300
patients with liver cirrhosis (14). But in contrast with our study
results, there was no statistically significant difference in serum
albumin values between the groups. Following the univariate
analysis, in their study, 9 variables were identified as predictive
factors in the occurrence of SBP, namely: age, BT, aspartate
aminotransferase (AST), creatinine, INR, serum leukocytes,
platelets, Model for End-Stage Liver Disease (MELD) score and
C-reactive protein (CRP) (14). Our
univariate analysis did not record age and AST as predictive
factors for SBP but identified albumin as one of them, and data
concerning the MELD score and CRP were not registered.
The results of our study showed that there were
significant differences in the mean value of PMN and ascites
proteins between the SBP and non-SBP groups but no significant
differences between the mean value of Hb, AST, and alanine
aminotransferase (ALT) were registered. Similar to our study
results, Abdel Rahman et al (15) in a study of 80 patients with liver
cirrhosis divided into two equal groups, with and without SBP, the
mean values of Hb, AST and ALT did not differ significantly between
the two groups but the median values of PMN differed significantly.
Contrary to our study, creatinine values were similar in both
groups.
Although the univariate analysis in our study
identified multiple factors involved in the occurrence of SBP
including serum biological parameters (WBC, PLT, creatinine, BT,
serum albumin, Na, alkaline reserve, INR, ESR and NLR), ascites
fluid analysis (WBC and PMN) and clinical parameters [upper
gastrointestinal bleeding (UGIB), cardiac comorbidities] only 2
factors (ESR and NLR) were identified as independent predictive
factors with good accuracy for SBP diagnosis. In contrast, in the
study by Elsadek et al (16)
that included 178 patients with liver cirrhosis, of which 60 with
SBP and 118 without SBP, the diagnostic accuracy of ESR (AUC=0.679;
95% CI, 0.581-0.776) and the cut-off value (27.0 mm/h) were lower
compared to our study.
NLR is a non-invasive marker that can be used to
predict the occurrence of in-hospital infections in patients with
decompensated liver cirrhosis (17). In a study conducted by Piotrowski
et al, an association between NLR and the presence of
infection in patients with liver cirrhosis was identified but with
low diagnostic accuracy (AUC=0.606) (18).
Our study showed that a model consisting of NLR and
ESR has a high accuracy in SBP diagnosis. Moreover, according to
literature data, NLR can be used in combination with other factors
as a predictor in the occurrence of SBP. Abdel-Razik et al
(19) demonstrated that a
combination of age, mean platelet volume (MPV), NLR and CRP, used
as the Mansoura score, can rule out the diagnosis of SBP. Mousa
et al (20) showed that a
combination of NLR and CRP can be used as a simple and non-invasive
test for SBP diagnosis. However, data are contradictory in terms of
the cut-off value.
Our study had several limitations. Namely, it was a
single center retrospective study and did not record data on CRP,
as it was absent from most of the patient medical files.
In conclusion, the present study could be of
clinical utility in predicting SBP, a major cause of mortality in
patients with cirrhosis. The combination of NLR and ESR is an easy
test that can be used to diagnose SBP.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
REP, CFB, AIS and APS conceived and designed the
study. REP, SIM and FV acquired the data; EP, LM, FV, GC and LCP
analyzed the data; CFB, AIS, APS and LCP validated the results. EP,
FV, LM, and SIM were responsible for preparation of the original
draft; REP, CFB, SIM, GC and APS were responsible for the final
manuscript editing. REP, AIS, LM, GC and LCP supervised the
manuscript publication. All authors read and approved the final
manuscript for publication.
Ethics approval and consent to
participate
The present study was approved by the Emergency
Clinical Hospital ‘St. Apostle Andrew’ Constanta Ethics Committee.
Although not mandatory for observational, non-interventional
studies at the Emergency Clinical Hospital ‘St. Apostle Andrew’
from Constanta, a university hospital, all admitted patients signed
informed consent by which they agreed that their data be available
for academic and scientific purposes.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Pimpin L, Cortez-Pinto H, Negro F,
Corbould E, Lazarus JV, Webber L and Sheron N: EASL HEPAHEALTH
Steering Committeey. Burden of liver disease in Europe:
Epidemiology and analysis of risk factors to identify prevention
policies. J Hepatol. 69:718–735. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
European Centre for Disease Prevention and
Control (ECDC): Systematic review on hepatitis B and C prevalence
in the EU/EEA. ECDC, Stockholm, 2016. https://www.ecdc.europa.eu/en/publications-data/systematic-review-hepatitis-b-and-c-prevalence-eueea.
Accessed November 10, 2016.
|
|
3
|
Dever JB and Sheikh MY: Review article:
Spontaneous bacterial peritonitis-bacteriology, diagnosis,
treatment, risk factors and prevention. Aliment Pharmacol Ther.
41:1116–1131. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
European Association for the Study of the
Liver. EASL clinical practice guidelines on the management of
ascites, spontaneous bacterial peritonitis, and hepatorenal
syndrome in cirrhosis. J Hepatol. 53:397–417. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Numan L, Elkafrawy A, Kaddourah O,
Brotherton T, Saeed L, Zafar Y, Tomaw A, Foxworth J and Al-Sayyed
L: Spontaneous bacterial peritonitis: We are still behind. Cureus.
12(e7711)2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Marciano S, Díaz JM, Dirchwolf M and
Gadano A: Spontaneous bacterial peritonitis in patients with
cirrhosis: Incidence, outcomes, and treatment strategies. Hepat
Med. 11:13–22. 2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Duah A and Nkrumah KN: Prevalence and
predictors for spontaneous bacterial peritonitis in cirrhotic
patients with ascites admitted at medical block in Korle-Bu
Teaching Hospital, Ghana. Pan Afr Med J. 33(35)2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Shi KQ, Fan YC, Ying L, Lin XF, Song M, Li
LF, Yu XY, Chen YP and Zheng MH: Risk stratification of spontaneous
bacterial peritonitis in cirrhosis with ascites based on
classification and regression tree analysis. Mol Biol Rep.
39:6161–6169. 2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Wehmeyer MH, Krohm S, Kastein F, Lohse AW
and Lüth S: Prediction of spontaneous bacterial peritonitis in
cirrhotic ascites by a simple scoring system. Scand J
Gastroenterol. 49:595–603. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Paul K, Kaur J and Kazal HL: To study the
incidence, predictive factors and clinical outcome of spontaneous
bacterial peritonitis in patients of cirrhosis with ascites. J Clin
Diagn Res. 9:OC09–OC12. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kraja B, Sina M, Mone I, Pupuleku F,
Babameto A, Prifti S and Burazeri G: Predictive value of the model
of end-stage liver disease in cirrhotic patients with and without
spontaneous bacterial peritonitis. Gastroenterol Res Pract.
2012(539059)2012.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Gonçalves PL, Zago-Gomes Mda P, Marques
CC, Mendonça AT, Gonçalves CS and Pereira FE: Etiology of liver
cirrhosis in Brazil: Chronic alcoholism and hepatitis viruses in
liver cirrhosis diagnosed in the state of Espfrito Santo. Clinics
(Sao Paulo). 68:291–295. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Vento S, Dzudzor B, Cainelli F and Tachi
K: Liver cirrhosis in sub-Saharan Africa: Neglected, yet important.
Lancet Glob Health. 6:e1060–e1061. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Metwally K, Fouad T, Assem M, Abdelsameea
E and Yousery M: Predictors of spontaneous bacterial peritonitis in
patients with cirrhotic ascites. J Clin Transl Hepatol. 6:372–376.
2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Abdel Rahman EM, Attia FA, Alsebaey A,
Elkady MAK, Sayed MM, Awad AR and El-Seidi EA: Ascitic calprotectin
as a useful marker in the diagnosis of spontaneous bacterial
peritonitis in adults. Egypt Liver J. 10:1–6. 2020.
|
|
16
|
Elsadek HM, Elhawari SA and Mokhtar A: A
novel serum index for accurate diagnosis of spontaneous bacterial
peritonitis in cirrhotic patients without other infections. Egypt
Liver J. 10:1–8. 2020.
|
|
17
|
Cai YJ, Dong JJ, Dong JZ, Yang NB, Song M,
Wang YQ, Chen YP, Lin Z and Shi KQ: Neutrophil-lymphocyte ratio
predicts hospital-acquired bacterial infections in decompensated
cirrhosis. Clin Chim Acta. 469:201–207. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Piotrowski D, Sączewska-Piotrowska A,
Jaroszewicz J and Boroń-Kaczmarska A: Lymphocyte-to-monocyte ratio
as the best simple predictor of bacterial infection in patients
with liver cirrhosis. Int J Environ Res Public Health.
17(1727)2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Abdel-Razik A, Mousa N, Abdel-Aziz M,
Elsherbiny W, Zakaria S, Shabana W, Abed S, Elhelaly R, Elzehery R,
Eldars W and El-Bendary M: Mansoura simple scoring system for
prediction of spontaneous bacterial peritonitis: Lesson learnt. Eur
J Gastroenterol Hepatol. 31:1017–1024. 2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Mousa N, Besheer T, Abdel-Razik A, Hamed
M, Deiab AG, Sheta T and Eldars W: Can combined blood neutrophil to
lymphocyte ratio and C-reactive protein be used for diagnosis of
spontaneous bacterial peritonitis? Br J Biomed Sci. 75:71–75.
2018.PubMed/NCBI View Article : Google Scholar
|