|
1
|
Wu T, Peng J, Meng T, Liu Q, Ao X, Lin W,
Yin H, Chen J, Pu J, Peng Z, et al: Clinicopathological features
and prognostic analysis of 49 cases with crescentic
glomerulonephritis. Exp Ther Med. 18:3984–3990. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Huang L, Zhong Y, Ooi JD, Zhou YO, Zuo X,
Luo H, Chen JB, Wu T, Yang Y, Meng T, et al: The effect of pulse
methylprednisolone induction therapy in Chinese patients with
dialysis-dependent MPO-ANCA associated vasculitis. Int
Immunopharmacol. 76(105883)2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Zhong Y, Pu J, Ao X, Peng W, Peng Z, Li X,
Xiao X, Zhou Q and Xiao P: Investigation of status for vascular
access in hemodialysis patients at Xiangya hospital of Central
South university. Zhong Nan Da Xue Xue Bao Yi Xue Ban.
42:1270–1274. 2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
4
|
Peng Z, Wang J, Yuan Q, Xiao X, Xu H, Xie
Y, Wang W, Huang L, Zhong Y, Ao X, et al: Clinical features and
CKD-related quality of life in patients with CKD G3a and CKD G3b in
China: Results from the Chinese cohort study of chronic kidney
disease (C-STRIDE). BMC Nephrol. 18(311)2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Goodnow CC: Multistep pathogenesis of
autoimmune disease. Cell. 130:25–35. 2007.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Hutton HL, Alikhan MA and Kitching AR:
Inflammasomes in the kidney. Exp Suppl. 108:177–210.
2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Hutton HL, Holdsworth SR and Kitching AR:
ANCA-associated vasculitis: Pathogenesis, models, and preclinical
testing. Semin Nephrol. 37:418–435. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W,
Zhang X, Wang WM, Qiu SJ, Zhou J and Fan J: Systemic
immune-inflammation index predicts prognosis of patients after
curative resection for hepatocellular carcinoma. Clin Cancer Res.
20:6212–6222. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yang R, Chang Q, Meng X, Gao N and Wang W:
Prognostic value of systemic immune-inflammation index in cancer: A
meta-analysis. J Cancer. 9:3295–3302. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
de Joode AA, Sanders JS and Stegeman CA:
Renal survival in proteinase 3 and myeloperoxidase ANCA-associated
systemic vasculitis. Clin J Am Soc Nephrol. 8:1709–1717.
2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hilhorst M, van Paassen P and Tervaert JW:
Limburg Renal Registry. Proteinase 3-ANCA vasculitis versus
myeloperoxidase-ANCA vasculitis. J Am Soc Nephrol. 26:2314–2327.
2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lyons PA, Rayner TF, Trivedi S, Holle JU,
Watts RA, Jayne DRW, Baslund B, Brenchley P, Bruchfeld A, Chaudhry
AN, et al: Genetically distinct subsets within ANCA-associated
vasculitis. N Engl J Med. 367:214–223. 2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Li ZY, Ma TT, Chen M and Zhao MH: The
prevalence and management of anti-neutrophil cytoplasmic
antibody-associated vasculitis in China. Kidney Dis (Basel).
1:216–223. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Jennette JC, Falk RJ, Bacon PA, Basu N,
Cid MC, Ferrario F, Flores-Suarez LF, Gross WL, Guillevin L, Hagen
EC, et al: 2012 revised international chapel hill consensus
conference nomenclature of vasculitides. Arthritis Rheum. 65:1–11.
2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Watts R, Lane S, Hanslik T, Hauser T,
Hellmich B, Koldingsnes W, Mahr A, Segelmark M, Cohen-Tervaert JW
and Scott D: Development and validation of a consensus methodology
for the classification of the ANCA-associated vasculitides and
polyarteritis nodosa for epidemiological studies. Ann Rheum Dis.
66:222–227. 2007.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ma YC, Zuo L, Chen JH, Luo Q, Yu XQ, Li Y,
Xu JS, Huang SM, Wang LN, Huang W, et al: Modified glomerular
filtration rate estimating equation for Chinese patients with
chronic kidney disease. J Am Soc Nephrol. 17:2937–2944.
2006.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Mukhtyar C, Lee R, Brown D, Carruthers D,
Dasgupta B, Dubey S, Flossmann O, Hall C, Hollywood J, Jayne D, et
al: Modification and validation of the birmingham vasculitis
activity score (version 3). Ann Rheum Dis. 68:1827–1832.
2009.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Berden AE, Ferrario F, Hagen EC, Jayne DR,
Jennette JC, Joh K, Neumann I, Noël LH, Pusey CD, Waldherr R, et
al: Histopathologic classification of ANCA-associated
glomerulonephritis. J Am Soc Nephrol. 21:1628–1636. 2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Chen YX, Xu J, Pan XX, Shen PY, Li X, Ren
H, Chen XN, Ni LY, Zhang W and Chen N: Histopathological
classification and renal outcome in patients with antineutrophil
cytoplasmic antibodies-associated renal vasculitis: A study of 186
patients and metaanalysis. J Rheumatol. 44:304–313. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Chang DY, Li ZY, Chen M and Zhao MH:
Myeloperoxidase-ANCA-positive granulomatosis with polyangiitis is a
distinct subset of ANCA-associated vasculitis: A retrospective
analysis of 455 patients from a single center in China. Semin
Arthritis Rheum. 48:701–706. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Yuan Q, Wang J, Peng Z, Zhou Q, Xiao X,
Xie Y, Wang W, Huang L, Tang W, Sun D, et al:
Neutrophil-to-lymphocyte ratio and incident end-stage renal disease
in Chinese patients with chronic kidney disease: results from the
Chinese cohort study of chronic kidney disease (C-STRIDE). J Transl
Med. 17(86)2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Xiao H, Heeringa P, Liu Z, Huugen D, Hu P,
Maeda N, Falk RJ and Jennette JC: The role of neutrophils in the
induction of glomerulonephritis by anti-myeloperoxidase antibodies.
Am J Pathol. 167:39–45. 2005.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Xiao H, Hu P, Falk RJ and Jennette JC:
Overview of the pathogenesis of ANCA-associated vasculitis. Kidney
Dis (Basel). 1:205–215. 2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Ma TT, Huang YM, Wang C, Zhao MH and Chen
M: Coagulation and fibrinolysis index profile in patients with
ANCA-associated vasculitis. PLoS One. 9(e97843)2014.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Willeke P, Kumpers P, Schlüter B, Limani
A, Becker H and Schotte H: Platelet counts as a biomarker in
ANCA-associated vasculitis. Scand J Rheumatol. 44:302–308.
2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
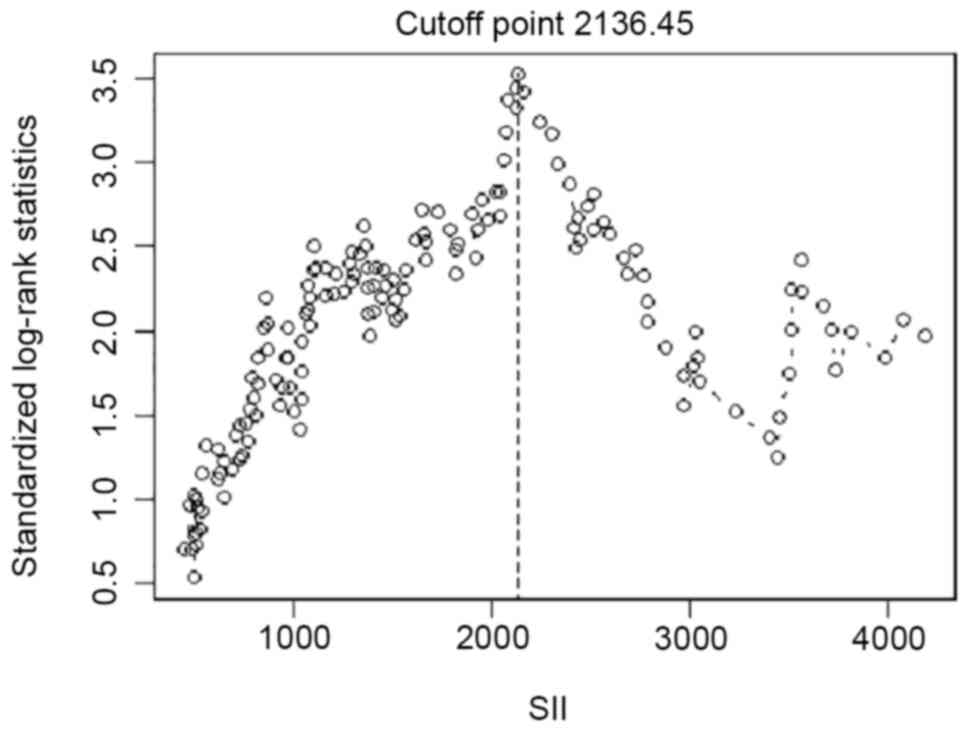
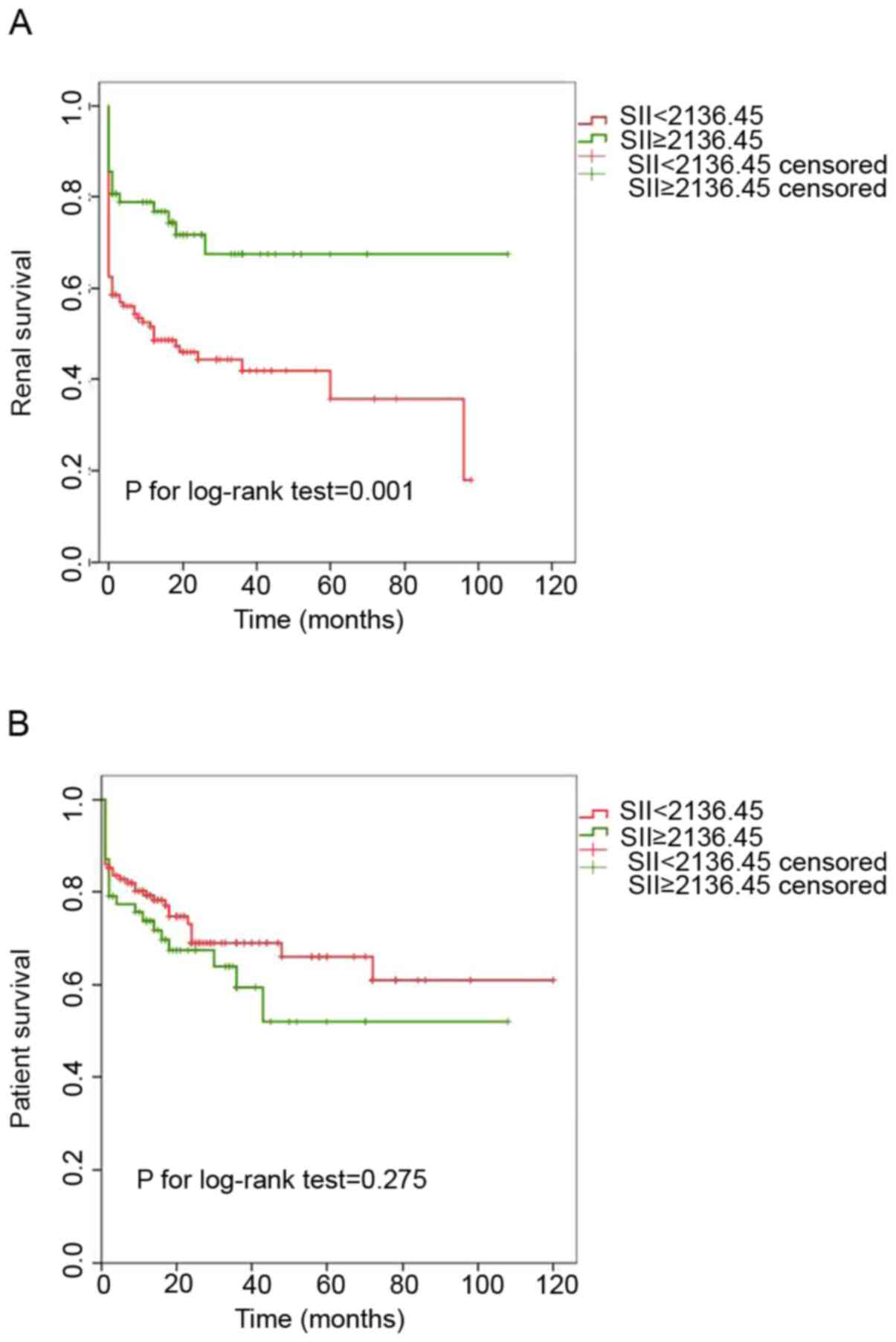
Budczies J, Klauschen F, Sinn BV, Győrffy
B, Schmitt WD, Darb-Esfahani S and Denkert C: Cutoff finder: A
comprehensive and straightforward web application enabling rapid
biomarker cutoff optimization. PLoS One. 7(e51862)2012.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Kim Y, Choi H, Jung SM, Song JJ, Park YB
and Lee SW: Systemic immune-inflammation index could estimate the
cross-sectional high activity and the poor outcomes in
immunosuppressive drug-naive patients with antineutrophil
cytoplasmic antibody-associated vasculitis. Nephrology (Carlton).
24:711–717. 2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Basu N, Karabayas M and Pusey C: Prognosis
and future developments in vasculitis. Best Pract Res Clin
Rheumatol. 32:148–165. 2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Collecchi P, Baldini E, Giannessi P,
Naccarato AG, Passoni A, Gardin G, Roncella M, Evangelista G,
Bevilacqua G and Conte PF: Primary chemotherapy in locally advanced
breast cancer (LABC): Effects on tumour proliferative activity,
bcl-2 expression and the relationship between tumour regression and
biological markers. Eur J Cancer. 34:1701–1704. 1998.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Najafi CC, Korbet SM, Lewis EJ, Schwartz
MM, Reichlin M and Evans J: Lupus Nephritis Collaborative Study
Group. Significance of histologic patterns of glomerular injury
upon long-term prognosis in severe lupus glomerulonephritis. Kidney
Int. 59:2156–2163. 2001.PubMed/NCBI View Article : Google Scholar
|