Introduction
Inguinal hernia represents the entrance of
peritoneal viscera through the inguinal canal. The viscera are
enveloped by the peritoneum forming the hernial sac. The lifetime
risk to develop an inguinal hernia is 27-43% for men and 3-6% for
women. Surgical closure of the hernia sac has become of the most
commonly used procedure in general surgery (1).
The surgical treatment of inguinal hernia can be
performed using a variety of techniques, all based on the treatment
of the hernia sac and its contents, but also the restoration of the
abdominal wall. In the XV-XVI centuries, empirical methods were
used, which were abandoned in the XVIII century, when the first
manuscripts appeared containing information related to the
treatment of hernia (2). The 19th
century marks the beginning of the modern era of hernia surgery
with the appearance of the Cooper and Scarpa manuscripts (3). In 1984, E. Bassini introduced the idea
that the weakness of the posterior wall of the inguinal canal is
responsible for the production of a hernia (4). As a result, he introduced the idea of
strengthening the posterior wall by suturing the lower edge of the
deep abdominal muscles to the femoral arch. For this reason, the
great surgeon Halsted considered Bassini, ‘the father of hernia
surgery’ (5). The revolution in the
treatment of hernias began with the use of the principle of
‘Tension-Free hernioplasty’, in which the tension in the structures
of the inguinal canal disappears, an idea promoted by French
surgeons J. Rives and R. Stoppa (6). They used a polymer mesh for the first
time in the repair of the hernia, placed between the peritoneum and
the transversalis fascia. In 1993, Lichtenstein published the
results of 3,125 hernioplasties, in which he used a polypropylene
mesh placed above the transversalis fascia, a study in which only 4
cases recurred (7).
There are various repair techniques for inguinal and
femoral hernias, classified as classical wide open approaches or
laparoscopic techniques such as: The total extraperitoneal patch
plasty (TEP), transabdominal preperitoneal patch plasty (TAPP), and
Lichtenstein techniques (1,8). The concept of using a mesh to repair
hernias was introduced over 50 years ago and is now standard in
most countries and widely accepted as superior to primary suture
repair. As a result, there has been a rapid growth in the variety
of meshes available and choosing the appropriate one can be an
extremely difficult task (9).
The aim of the present study was the evaluation of
the effectiveness of allograft mesh, as well as the immediate and
long-term complications in textile allografts used in open surgery
of inguinal hernia repair.
Materials and methods
Ethics approval and patient
consent
The present study followed the international
regulations in accordance with the Declaration of Helsinki. The
study was approved by the Ethics Committee of the Sibiu County
Clinical Emergency Hospital. Patient informed consent for
publication of the data/images associated with the manuscript was
obtained.
Materials
The current study includes cases admitted to the
Department of Surgery of Sibiu County Clinical Emergency Hospital
for the period January 2011 to December 2018. The study included
255 patients over a 7-year period, who underwent the modified
Lichtenstein procedure using Premiline Mesh™. Patients from January
2019 to December 2020 were not included due to the Covid-19
pandemic and potential statistical bias. The mesh was constructed
from monofilament polypropylene, which was knitted into a thin and
elastic shape-stable mesh with large pores and low weight (LW).
Statistical analysis was performed using Excel Suite Software.
This type of allograft was selected as it is part of
the LW and large-pore mesh group. The reasons for the choice were:
Easier handling, reduced contact with tissues due to the large
pores of the mesh (which leads to a decrease in the number of
complications related to net rejection, seromas, granulomas) and
the numerous studies performed on swine models whose results have
demonstrated their increased efficacy (10,11).
The meshes used had thinner threads and pores >1
mm. Their specific weight was 33 g/m2. These meshes have
less tissue reaction and are more elastic in behavior. The
elasticity of all LW meshes ranges from 20 to 35% at 16 N/cm.
Modern biomaterials have to be both physical and chemical inert as
the tissue reaction occurs in close relationship with the diameter
of the pores and the amount of foreign material inserted into the
body (12).
Surgical technique description
The technique used in all cases was the Lichtenstein
procedure, a well-known procedure that is not described herein
(13). However, particular aspects
that led to modifying the classical technique include the
following.
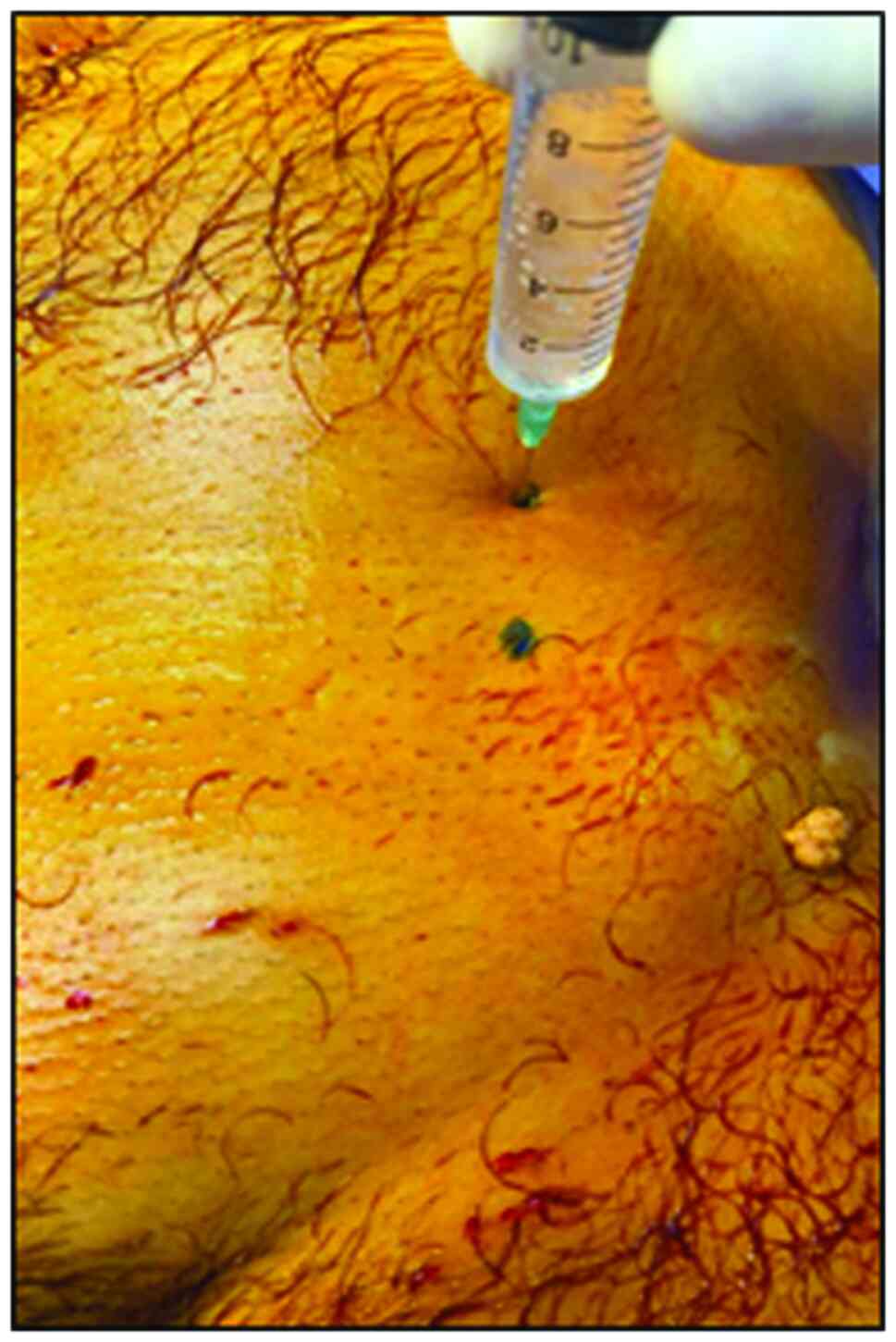
i) The anesthesia used was a combination of
ilioinguinal block, local and intravenous anesthesia. The
ilioinguinal block was calculated as follows: 2 cm were measured
laterally from the iliac spine on the side of the hernia on the
bispinous line, then 2 cm cranially on the perpendicular drawn on
the bispinous line, at the point located at 2 cm (Fig. 1). Local anesthesia was performed by
skin infiltration at the incision site. For intravenous anesthesia,
a general anesthetic from the class of non-barbiturates was
used.
ii) This type of anesthesia associated with the
concept of Fast Track Surgery (FTS) is indispensable in one-day
surgeries. The concept of FTS involves a combination of techniques
used in order to provide a very fast recovery after surgery. It
includes elements of anesthesia, surgery, nutrition, and rapid
postoperative mobilization.
iii) The incision was transverse, parallel to the
bispinous line, but centered on the inguinal canal at half the
distance between the superficial and the deep orifice (Fig. 2).
iv) The allograft used was of the Premiline Mesh
type, with large pores and low weight, which we adapted to the
anatomy of the specific region of each patient.
v) At the end of the intervention, the patient is
woken up on the operating table and helped to walk on their feet to
the postoperative or recovery room-respecting the same concept of
FTS.
vi) The discharge was made 2-3 h after the end of
the surgery (7).
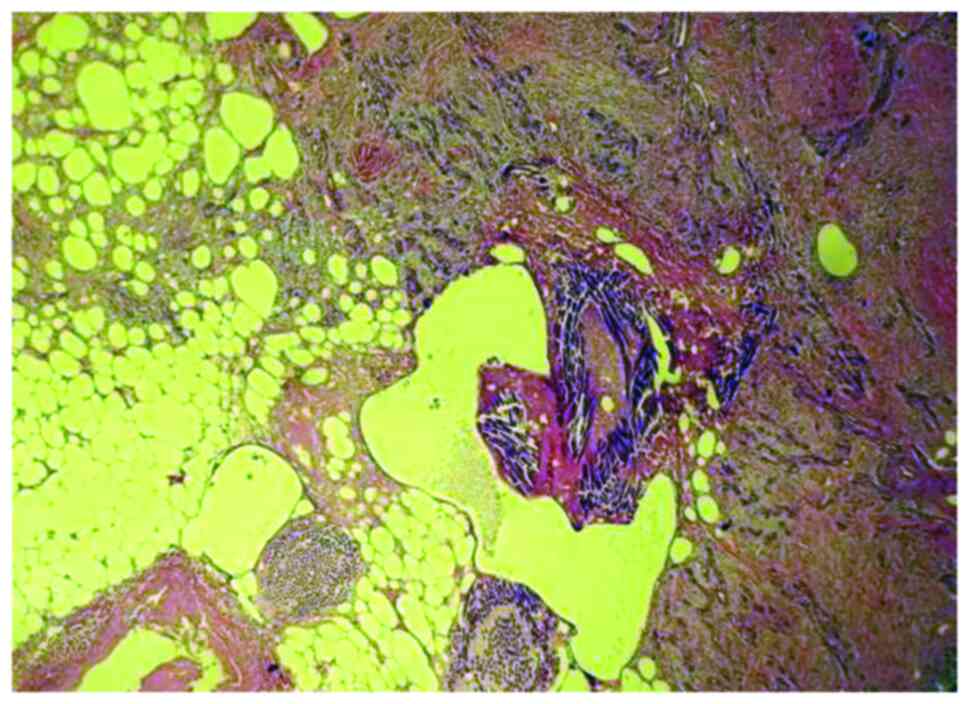
Hematoxylin and eosin staining
To identify any subcutaneous surgical thread
granulomas, tissues were assessed using a conventional brightfield
microscopy. The samples were fixed with 10% formaldehyde, at room
temperature for 24 h. The tissue fragments were dehydrated and
submitted to 3 toluene passages prior to paraffin inclusion. The
sections were 3 microns thick. Hematoxylin and eosin staining was
carried out at room temperature for 1 h. Giant cells were
identified under an optical microscope Viola MC20i microscope using
an SP ARCHO lens.
Statistical analysis
Collected data were compiled and tabulated on a
master sheet. The results obtained were subjected to basic
statistical analysis in Microsoft Excel 16.45 (Microsoft
Corporation). Besides descriptive statistics (mean ± standard
deviation), bivariate analysis was performed using Pearson's
Chi-square and Fisher's exact test for categorical variables as
applicable, and the Student's t-test for continuous variables.
P<0.05 was considered to indicate statistically significant
results.
Results and Discussion
Distribution of patients according to
age
Of the total number of patients included in the
study group, 206 were male and 49 were female. The 255 patients in
this study had a male to female ratio of 81% males and 19% females,
this being in total accordance with the worldwide distribution for
this type of surgical pathology. The patients' age ranged between
20 and 90 years. Regarding the distribution of patients by age
groups, 74 patients were in the 20-40 age group, 85 patients in the
41-61 age group and 96 patients in the 61-90 age group (P=0.09)
(Table I).
 | Table IDistribution of patients according to
age. |
Table I
Distribution of patients according to
age.
| Age group | No. of cases | Percentage |
|---|
| 20-40 | 74 | 29.1 |
| 41-61 | 85 | 33.3 |
| 61-90 | 96 | 37.6 |
| Total | 255 | 100 |
Out of the 255 cases, 51 patients (20%) resided in a
rural environment, while the remaining 204 patients (80%) resided
in an urban environment (P=0.006). This aspect is very important
because untreated minor early complications may lead to subsequent
major problems. Of note, in Romania the residence of the patient
greatly influences the quality of postoperative care and follow up
due to a decreased accessibility to healthcare services in rural
areas. Needless to say disease prevention is decreased, and the
patients tend to postpone the initial consult and present with
advanced pathology stages.
Distribution of patients with
postoperative complications
Postoperative evaluation of the patients is
essential in monitoring both immediate and late complications, as
well as in evaluating the prosthesis. The monitoring of the
patients who were discharged was performed at 2 and 7 days. In
addition, all patients were monitored at 1 and 6 months by
performing an abdominal ultrasound.
At the 2-day check-up, there were only 4 cases
(1.5%) of large postoperative hematoma that required surgical
reintervention, although without removal of the allograft. The
remaining 251 patients included in the study group did not present
immediate complications at the first postoperative evaluation
(P=0.0033) (Table II).
 | Table IIDistribution of patients with early
postoperative complications. |
Table II
Distribution of patients with early
postoperative complications.
| | Immediate
postoperative complications |
|---|
| Check-up | Large hematoma | Small hematoma | Wound seroma |
|---|
| 2 days | 4 | - | - |
| 7 days | - | 9 | 16 |
| Total | 4 | 9 | 16 |
At the 7-day check-up, on which occasion the sutures
were suppressed, complications were observed in 25 patients,
distributed as follows: In 9 patients there were hematomas and in
16 seromas (P=0.04) (Table
II).
In addition, there were no superinfections of the
postoperative wound, probably due to the prophylaxis performed in
each case at the anesthetic induction by intravenous administration
of 1 g amoxicillin.
Late postoperative morbidity was represented by
chronic postoperative pain in 6 patients and cutaneous hypoesthesia
in 14 patients. All 25 cases had a spontaneous resolution.
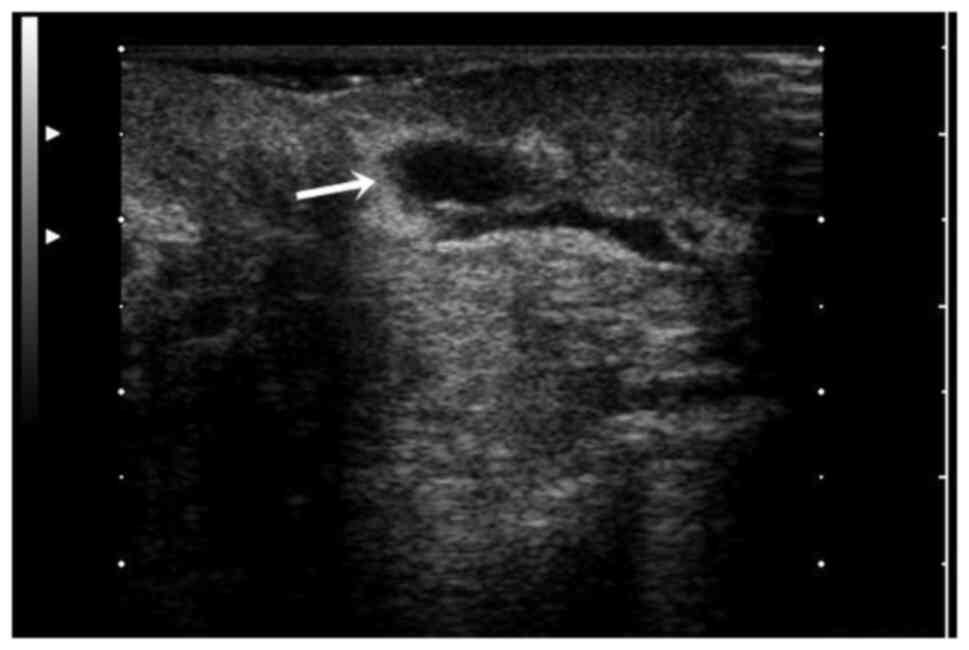
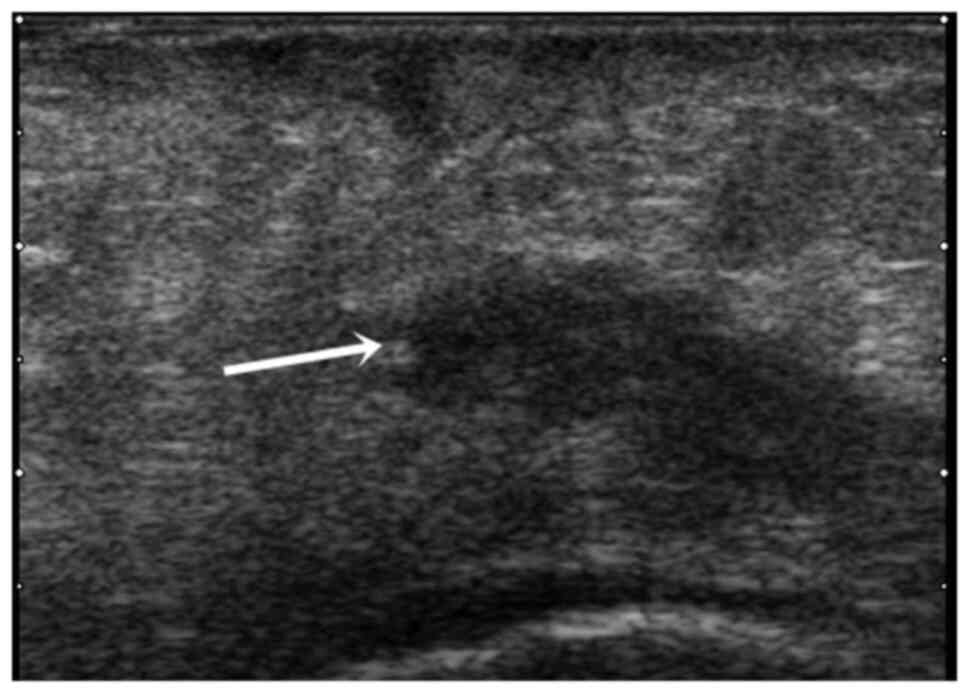
Regarding ultrasound monitoring one month after
discharge, 38 patients developed seroma, 25 patients developed
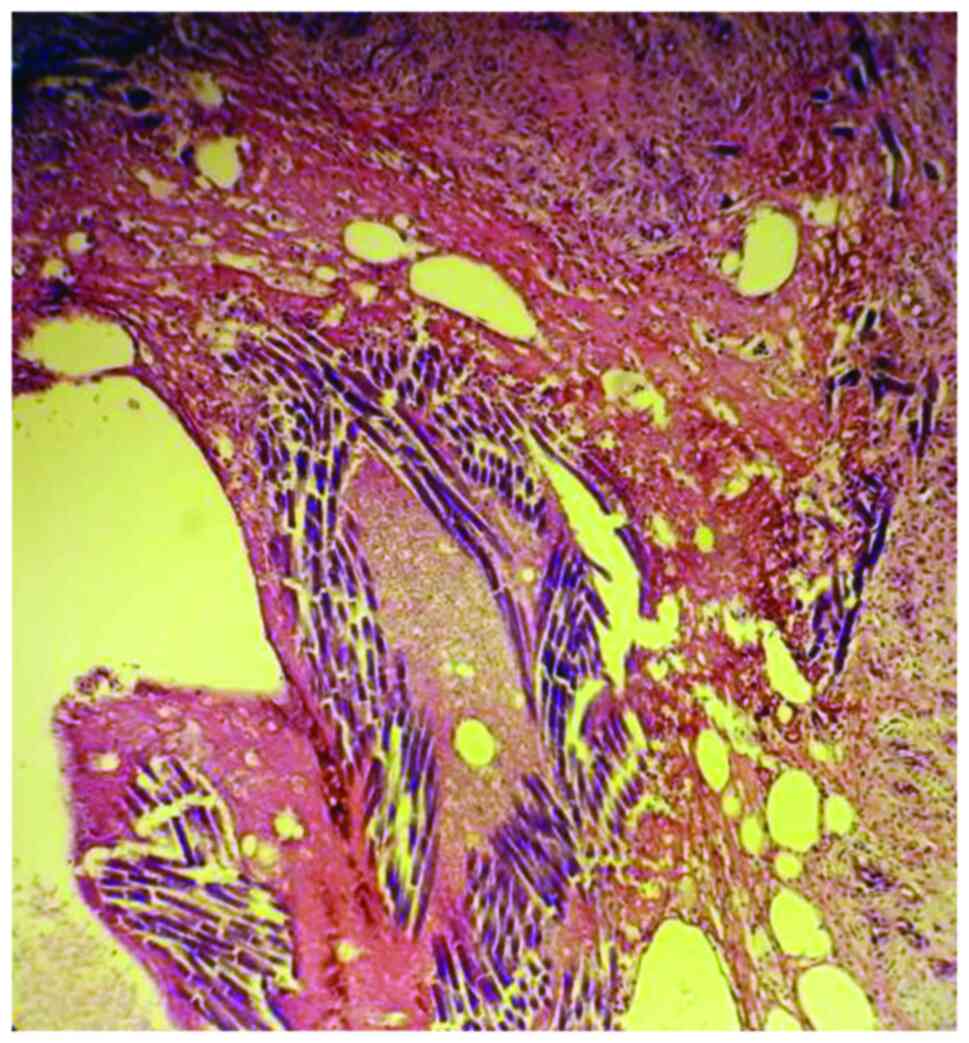
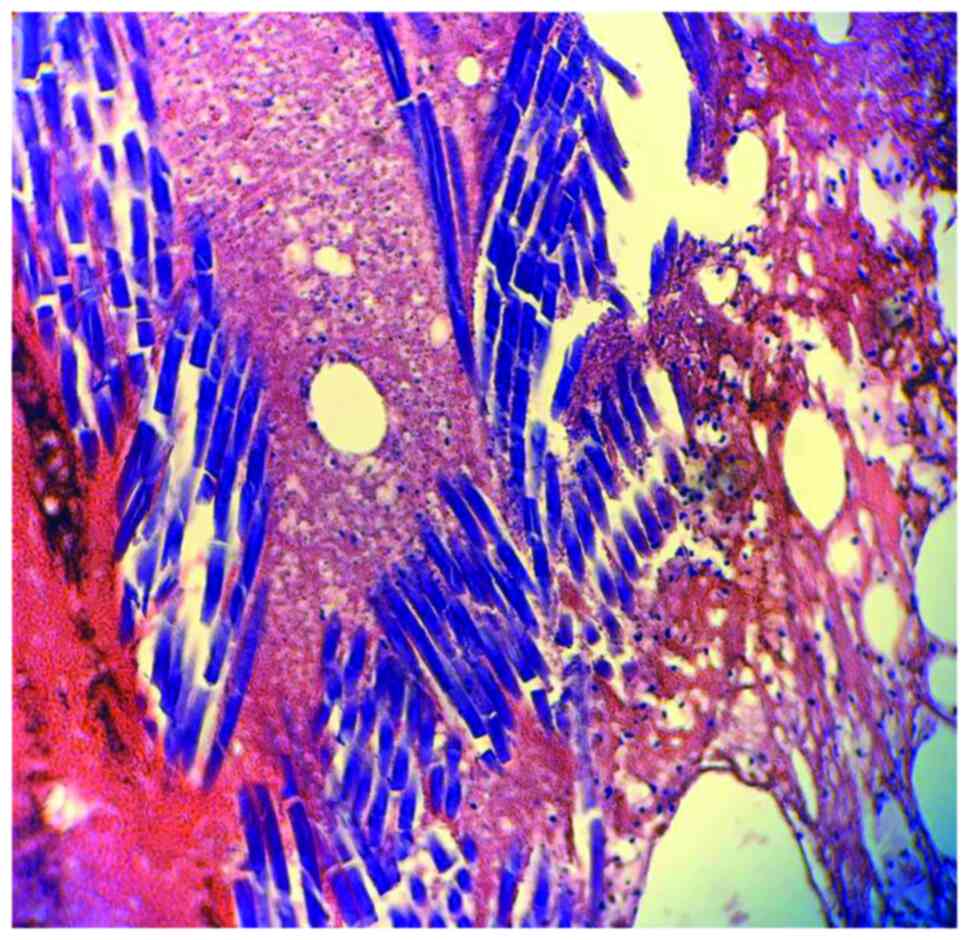
subcutaneous surgical thread granulomas as viewed under a Viola
MC20i microscope using an SP ARCHO lens, 13 patients developed
granulomatous subcutaneous fibrotic band and 8 of them developed
granulomatous over the mesh fibrotic band (Figs. 3 and 4) (P=0.01).
These 84 patients also presented late complications
in the first month, detected using abdominal ultrasound,
representing 33% of the total number of patients included in the
study group (P=0.011).
In a significant number of cases from the present
study, tissue reactivity was identified in the form of granulomas,
seromas or lymph-node reaction. This reactivity can be explained by
the materials used and tissue properties, surgical technique, as
well as by the immune/inflammatory response of each patient. The
body is considered a key factor regarding a complete integration of
the mesh at the tissue level.
Foreign body granuloma occurs through a non-immune
mechanism. It is triggered by exogenous (in our case mesh) or
endogenous foreign bodies. Microscopically, the foreign body
granuloma in the case of the mesh is made up of giant
multinucleated cells, with a disordered nucleus, resulting from the
fusion of macrophages that come to phagocytose the foreign body.
The foreign body is bi-refractive, located in the center of the
granuloma, without necrosis (Figs.
5 and 6).
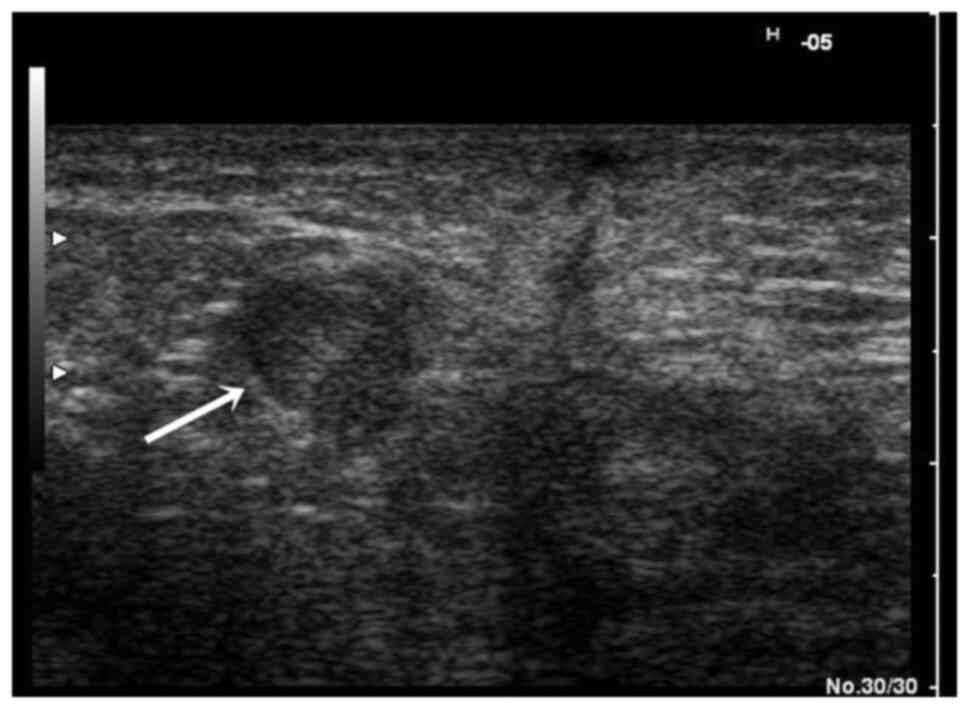
Patient follow-up
The patients who had immediate postoperative
complications were called for a new check-up at 6 months
postoperatively. Furthermore, a soft tissue ultrasound was
performed, which showed the disappearance of the seromas, but in 6
patients, the persistence of inguinal lymphadenopathy was found
(Figs. 7 and 8) (P=0.02). Another important point in the
ultrasound evaluation that was performed at 6 months was the study
of how the mesh was accepted by the host organism. Thus, in only
30% of cases, the allograft was visible on ultrasound examination,
while in the remaining patients it could no longer be highlighted
(P=0.009).
A high percentage of small-sized postoperative
seromas was observed. This could be due to enzymatic activity and
tissue reactivation that is overrun in the immediate postoperative
period. In their composition, lymph, proteins, blood (small
amounts), fibrin, LDH, and white blood cells (WBC) were found. The
presence of WBC with neutrophilia at higher values locally in the
blood stream clearly indicates local tissue activity (14).
The mesh with large pores and low weight was
employed as there was low contact between the allograft and the
body's own tissues, which led to improved acceptance of the
alloplastic material by the host organism. The presence of small
holes in the mesh (<1 mm) pronounced the inflammatory process
and fibrosis, while larger holes provided less fibrotic reaction,
and conserved the elasticity of the inguinal region and lack of
keloid scar (15-17).
Alloplastic mesh with large holes was used
exclusively in the current study. The reasons behind this decision
were the advantages of large-pore LW meshes. Larger pore size leads
to improved integration and biochemical capacity, as well as
increased tissue ingrowth. This type of mesh has a better
integration rate compared to LW meshes with small pores and the
patient is less conscious of the foreign body. A major disadvantage
of this type of mesh is the lack of stability that leads to
shrinkage. The LW small pore mesh was not utilizes as it has a
significantly higher shrinkage rate than any other types of mesh
and also a lower tissue integration rate. Numerous clinical studies
underlined the important of a tension-free placement of the mesh
(18-21).
Effect of mesh
A common complication of the procedures when
dissecting extensively the hernia sac is the development of
seromas. A seroma hinders the attachment of the patch to the
surrounding tissues with rapid fixation and increases the risks of
recurrence and infection (22).
Among the factors leading to seroma formation are
senescence, large hernia volume and scrotum involvement. However, a
recent meta-analysis did not note any difference in the impact of
lightweight vs. heavyweight meshes on the seroma rate after
inguinal hernia repair (23).
Another frequent complication is the development of
hematoma. The risk of hematoma is increased by partially absorbable
mesh, chronic anticoagulation, recurrent hernia procedure, mesh
fixation, larger hernia defect and medial defect localization
(24).
Regarding the formation of hematomas and seromas,
their occurrence is more related to the application of the
technique and the risk factors of each patient than the technique
itself (7).
Needless to say, all 255 cases underwent a complex
differential diagnosis for other possible associated pathology such
as gastro-intestinal carcinomas (25). Other pathology influencing surgical
recovery is diabetes and viral coinfections (26). The fact that we did not encounter a
case with complete immunologic rejection of the mesh is encouraging
(27).
The approach of this type of pathology in a welded
medical-surgical team, with a constant number of cases operated
monthly, leads to decreased operative time, decreased number of
intraoperative and postoperative complications and with improved
immediate and distant results. Using the FTS concept, together with
the use of prostheses, helps increase the patient's chances for a
rapid socio-professional reintegration, with minimal immediate and
late postoperative complications.
Currently, the use of polypropylene mesh represents
the best option to restore the integrity of the abdominal wall in
patients diagnosed with inguinal hernia. In addition, the use of
polypropylene allografts with wide holes has contributed to a
significant reduction of the local inflammatory process, as
indicated in aforementioned literature. Polypropylene has proven
physical, chemical and biological properties, and is currently the
most widely used allograft in the treatment of inguinal
hernias.
The local inflammatory response produced by the
contact between the tissues and the mesh causes a delay in the
complete integration of the tissues, but it is not associated with
the immediate recurrence of the herniated sac and the development
of complications is limited.
Using LW polypropylene allograft with thinner
threads and large pores improved abdominal wall compliance, with
less contraction or shrinkage of the mesh and allowed improved
tissue incorporation.
During the 7-year duration of the study, there were
no cases of recurrence of the hernia sac. This is due both to the
extensive experience in the medical centers included in the study
and to the quality materials used.
Ilioinguinal block anesthesia, together with
intravenous anesthesia, is an important factor in the rapid
recovery of patients. The short duration of hospitalization (<4
h), the quality-price ratio, the good postoperative results, as
well as the rapid socio-professional reintegration, render the
technique very attractive for patients.
The multimodal approach of the patients diagnosed
with inguinal hernia using a series of preoperative workouts
together with the combined anesthesia, the adaptation of the
Lichtenstein technique and a quality mesh, constitutes a step
forward in the modern treatment of inguinal hernia.
Conclusion
Findings of the present study demonstrate once again
the conclusions of literature according to which LW meshes with
large pores are superior to those with small pores, due to an
optimized foreign body reaction based on small amounts of mesh and,
in particular, a significantly low surface area in contact with the
host tissues through the large porous pattern. In addition, an
extremely important feature of this type of mesh is the progressive
decrease of shrinkage on the tissues to which they are fixed,
decreasing the risk of recurrence. In the present study, there was
no case of recurrence at the 6-month check-up. Postoperative
complications related to mesh quality were extremely low, similar
to those in international studies.
Acknowledgements
Professional editing, linguistic and technical
assistance were performed by Irina Radu, Individual Service
Provider.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
CT and AMo contributed substantially to the
conception and design of the study, the acquisition, analysis, and
interpretation of the data, and were involved in the drafting of
the manuscript. AMi and DS contributed substantially to the
analysis and interpretation of the data and were involved in the
drafting of the manuscript. AC and DGB contributed substantially to
the interpretation of the data and were involved in the critical
revisions of the manuscript for important intellectual content. CT,
AMo and DS are responsible for confirming the authenticity of all
the raw data. All authors agreed to be accountable for all aspects
of the work in ensuring that questions related to the accuracy or
integrity of any part of the work are appropriately investigated
and resolved. All authors read and approved the final version of
the manuscript.
Ethics approval and consent to
participate
The study followed the international regulations in
accordance with the Declaration of Helsinki. The study was approved
by the Ethics Committee of the Sibiu County Clinical Emergency
Hospital (approval no. 20200518). Patient informed consent for
publication of the data/images associated with the manuscript was
obtained.
Patient consent for publication
Patient informed consent for publication of the
manuscript was obtained.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Köckerling F and Simons MP: Current
concepts of inguinal hernia repair. Visc Med. 34:145–150.
2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
White JJ and Haller JA: Groin Hernia in
Infants and Children. Nyhus LM and Condon RE (eds). Hernia
Philadelphia, PA, Lippincott, pp101-136, 1978.
|
|
3
|
Rutkow MI: A selective history of groin
hernia surgery in the early 19th century: The Anatomic Atlases of
Astley Cooper, Franz Hesselbach, Antonio Scarpa, and Jules-Germain
Cloquet. Surg Clin North Am. 78:921–940. 1998.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Dørflinger T and Kiil J: Absorbable suture
in hernia repair. Acta Chir Scand. 150:41–43. 1984.PubMed/NCBI
|
|
5
|
Summers JE: Classical herniorrhaphies of
Bassini, Halsted and Ferguson. Am J Surg. 73:87–99. 1947.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Stoppa R, Petit J, Abourachid H, Henry X,
Duclaye C, Monchaux G and Hillebrant JP: Original procedure of
groin hernia repair: Interposition without fixation of Dacron tulle
prosthesis by subperitoneal median approach. Chirurgie. 99:119–123.
1973.PubMed/NCBI(In French).
|
|
7
|
Tanasescu C, Faur M and Sabau D: Day-case
surgery in the context of inguinal hernia repair by the modified
Lichtenstein technique-A single Centre experience. Chirurgia
(Bucur). 114:115–120. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hernia Surge Group. International
guidelines for groin hernia management. Hernia. 22:1–165.
2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Brown CN and Finch JG: Which mesh for
hernia repair? Ann R Coll Surg Engl. 92:272–278. 2010.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Bratu D, Boicean A, Tanasescu C, Sofariu
C, Mihetiu A, Mitariu Cernusca IS, Ognean L, Moldovan C and Boitor
C: Textile polypropylene allografts and their postoperative tissue
reaction in the surgery of inguinal hernia. Mater Plast.
54:119–121. 2017.
|
|
11
|
Cobb WS, Burns JM, Peindl RD, Carbonell
AM, Matthews BD, Kercher KW and Heniford BT: Textile analysis of
heavy weight, mid-weight, and light weight polypropylene mesh in a
porcine ventral hernia model. J Surg Res. 136:1–7. 2006.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Bolocan A, Ion D, Constantinescu S, Luca
AD and Paduraru DN: Randomised trial comparing poly-propylene mesh
and polyvinylidene fluoride mesh in the surgery. Mat Plast.
49:209–211. 2012.
|
|
13
|
Lichtenstein IL, Shulman AG, Amid PK and
Montllor MM: The tension-free hernioplasty. Am J Surg. 157:188–193.
1989.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Wotton FT and Akoh JA: Rejection of
Permacol mesh used in abdominal wall repair: A case report. World J
Gastroenterol. 15:4331–433. 2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kehlet H and Bay Nielsen M: Anaesthetic
practice for groin hernia repair-a nation-wide study in Denmark
1998-2003. Acta Anaesthesiol Scand. 49:143–146. 2005.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Fitzgibbons RJ Jr, Giobbie-Hurder A, Gibbs
JO, Dunlop DD, Reda DJ, McCarthy M Jr, Neumayer LA, Barkun JST,
Hoehn JL, Murphy JT, et al: Watchful waiting vs. re-pair of
inguinal hernia in minimally symptomatic men: A randomised clinical
trial. JAMA. 295:285–292. 2006.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Chicea R, Chicea AL, Mihetiu A, Tantar C,
Cernusca Mitaru MM, Cernusca Mitaru SI, Roman C, Comaneanu RM,
Bratu D and Manea MM: Comparative study between tissues induced
immunohistochemical changes of thread granulomas and textile
allografts. Mater Plast. 55:99–101. 2018.
|
|
18
|
Weyhe D, Cobb W, Lecuivre J, Alves A,
Ladet S, Lomanto D and Bayon Y: Large pore size and controlled mesh
elongation are relevant predictors for mesh integration quality and
low shrinkage-Systematic analysis of key parameters of meshes in a
novel minipig hernia model. Int J Surg. 22:46–53. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Klosterhalfen B, Junge K and Klinge U: The
lightweight and large porous mesh concept for hernia repair. Expert
Rev Med Devices. 2:103–117. 2005.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wolak PK, Strzelecka A, Piotrowska A,
Dąbrowska K, Wolak PP, Piotrowska I and Nowak-Starz G: The
operative time for unilateral inguinal hernia repair in children
performed with Percutaneous Internal Ring Suturing (PIRS) or open
approach method. J Clin Med. 10(1293)2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Sanbhal N, Miao L, Xu R, Khatri A and Wang
L: Physical structure and mechanical properties of knitted hernia
mesh materials: A review. J Industrial Textiles. 48:333–360.
2018.
|
|
22
|
Fang H, Lin R, Lin X, Lu F, Yang Y, Wang
C, Chen Y and Huang H: Drainage decreases the seroma incidence in
laparoscopic transabdominal preperitoneal (TAPP) hernia repair for
large inguinoscrotal hernias. Asian J Surg. 44:544–548.
2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Köckerling F, Bittner R, Adolf D, Fortelny
R, Niebuhr H, Mayer F and Schug-Pass C: Seroma following
transabdominal preperitoneal patch plasty (TAPP): Incidence, risk
factors, and preventive measures. Surg Endosc. 32:2222–2231.
2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Smoot RL, Oderich GS, Taner CB, Greenlee
SM, Larson DR, Cragun EB and Farley DR: Postoperative hematoma
following inguinal herniorrhaphy: Patient characteristics leading
to increased risk. Hernia. 12:261–265. 2008.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Georgescu EF, Mogoantă SŞ, Costache A,
Pârvănescu V, Totolici BD, Pătraşcu Ş and Stănescu C: The
assessment of matrix metalloproteinase-9 expression and
angiogenesis in colorectal cancer. Rom J Morphol Embryol.
56:1137–1144. 2015.PubMed/NCBI
|
|
26
|
Rusu E, Jinga M, Rusu F, Ciurtin C, Enache
G, Dragomir A, Cristescu V, Stoica V, Costache A, Cheta D and
Radulian G: Statin therapy in patients with diabetes and hepatitis
C. Farmacia. 61:1204–1215. 2013.
|
|
27
|
Berghi NO, Dumitru M, Vrinceanu D,
Ciuluvica RC, Simioniuc-Petrescu A, Caragheorgheopol R, Tucureanu
C, Cornateanu RS and Giurcaneanu C: Relationship between chemokines
and T lymphocytes in the context of respiratory allergies (Review).
Exp Ther Med. 20:2352–2360. 2020.PubMed/NCBI View Article : Google Scholar
|