Introduction
In the 16th century, Ambroise Paré was the first to
perform a mastoidectomy, for the same clinical reasons it is
performed today (1). Unfortunately,
medical services at the time were rudimentary and rather
palliative, and were provided mainly in monastic hospitals,
especially for poor people and the anatomic (drainage results)
suffered greatly from lack of sanitary conditions (2). Functional results of the surgery were
still a future concern, and the patient was considered fortunate to
survive the suppurative mastoiditis and only lose the sense of
hearing to the affected ear. In the 19th century, Küster &
Bergmann (1891) were equally credited with describing the first
radical mastoidectomy and from there the surgical technique began
its development (3,4).
The generic term mastoidectomy describes a procedure
that addresses the inflammatory status of the middle ear. A
successful mastoidectomy is expected to deliver a ‘dry, safe,
stable ear, free of disease’. Maintaining or improving hearing is
important but the pursuit of a hearing result should not compromise
this primary aim (5). Restoring
sound transmission to the inner ear through reconstruction of the
ossicular chain is paramount in middle ear surgery (6,7) but
useless without a well performed mastoidectomy. This type of
surgery is notorious for bringing the patient into the operating
room only after the ear discharge has been going on ‘long enough’
to cause concern. It is certain that no one questions the drainage
role of the procedure (cavity cleanliness), but the common belief
is that the functional results are poor (hearing is destroyed or at
least gravely impaired). Mastoidectomy could be considered as
anathema since this procedure requires the patients hearing in
exchange for a dry, safe ear or even to save the patient's life.
But is this conviction founded?
Hearing loss represents one of the most serious
afflictions confronting the world's population, with variable
etiology, of which at least 50% cases are genetic. However, WHO
estimates that between 65 and 330 million individuals suffer from
some form of middle ear suppuration and 50% of them suffer from
hearing impairment (8-10).
Patients and methods
We initiated the retrospective non-controlled study
by conducting a random selection of 200 long-term patients with
both radical canal-wall down (CWD) and modified radical
mastoidectomy (MRM), performed over a 3-year period. The techniques
for both types of surgery are well known and described in the
literature (11-13).
The initial cohort was comprised of 209 patients of which 9 died (8
of causes non-related to middle-ear disease, 1 directly related to
middle-ear disease after otogenic brain abscess). The basic
statistical criteria for the selection was post-operative time
span. Data analysis began in 2004 giving a post-operative follow-up
period of 8.12 years for the entire cohort, from the moment of
surgery and 7.86 years from the time of complete epithelization of
the cavity, which allowed us to consider it as long-term
evaluation. All patients were clinically evaluated (microscope
otoscopy), both before surgery and after surgery. A pre-operative
measurement of the absolute thresholds of hearing (AHT) and bone
conduction threshold (BCT) (between 0.5-2 kHz) was performed and
used as a statistical indicator for functional results of the
mastoidectomy. Audiometric control took place as follows: 2 months
post-operative (corresponding to the moment of complete
epithelization of the cavity for 80% of cases); 1-year
post-operative (complete epithelization of the cavity for all
cases); 2 years post-operative; 3-4 years post-operative and
another 2 times over the next 3 years (starting from the 5th up to
the 8th year).
Our main goal was to define the situations and
factors that influenced hearing results of mastoidectomy and to
provide us with various aspects of the functional prognosis. Based
on the selection criteria of the studied group and by performing
statistical analysis of the correlation of functional results and
statistically significant variables, we were able to formulate
pertinent conclusions regarding the functional success rate of
mastoidectomy.
Although largely clinical, our study also included
minimal statistical analysis including creating Microsoft Excel
databases and attributing codes to facilitate data analysis using
Excel and SPSS version 15.00 (IBM Corp.). Factors such as age of
the patient, presence of cholesteatoma, and stage of disease were
correlated with the functional results of the mastoidectomy. Data
are expressed as percentage, mean values and standard deviation.
The level of statistical significance was set as P≤0.05. Parametric
tests (Student's t-test) or non-parametric tests (Mann-Whitney)
were also applied.
The studied variables Pre-surgery
variables
The pre-surgery variables included: age group: 0-10
years (n=1), 11-20 years (n=4), 21-30 years (n=56), 31-40 years
(n=45), 41-50 years (n=49), 51-60 years (n=27), 61-70 years (n=15),
71-80 years (n=3); and clinical stage of the disease: complicated
(n=45), not complicated (n=155). The type of disease included:
cholesteatoma (n=56) and non-cholesteatoma (n=144), and the type of
tympanic membrane perforation included marginal (n=75) and central
(n=125).
Intraoperative data
The intraoperative data included type of
mastoidectomy: modified radical (n=125), radical (n=75), and
ossicular chain status: absent (n=13), complete and mobile (n=27),
complete and fixed (n=25), interrupted (n=135). Total lesional
score was: 0-19 (n=170), 20-39 (n=13), 40-59 (n=5), 60-79 (n=5),
80-99 (n=4), 100-119 (n=2), 140-159 (n=1).
Follow-up data
The follow-up data included the period for complete
epithelization of the cavity: 2 months, 1 year, 2 years, 3-4 years,
8 years; and cavity self-cleansing: present or absent; as well as
the mastoidectomy result (drainage effect): Failure or success.
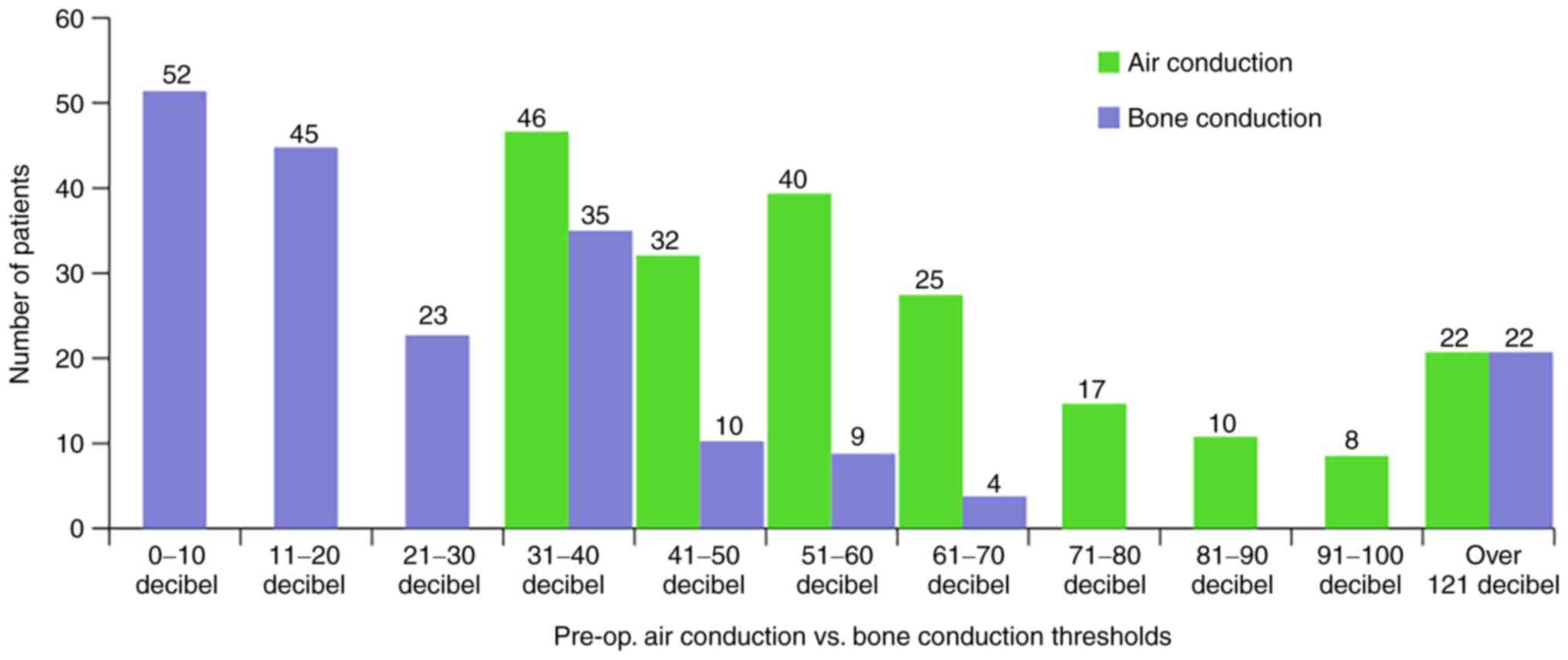
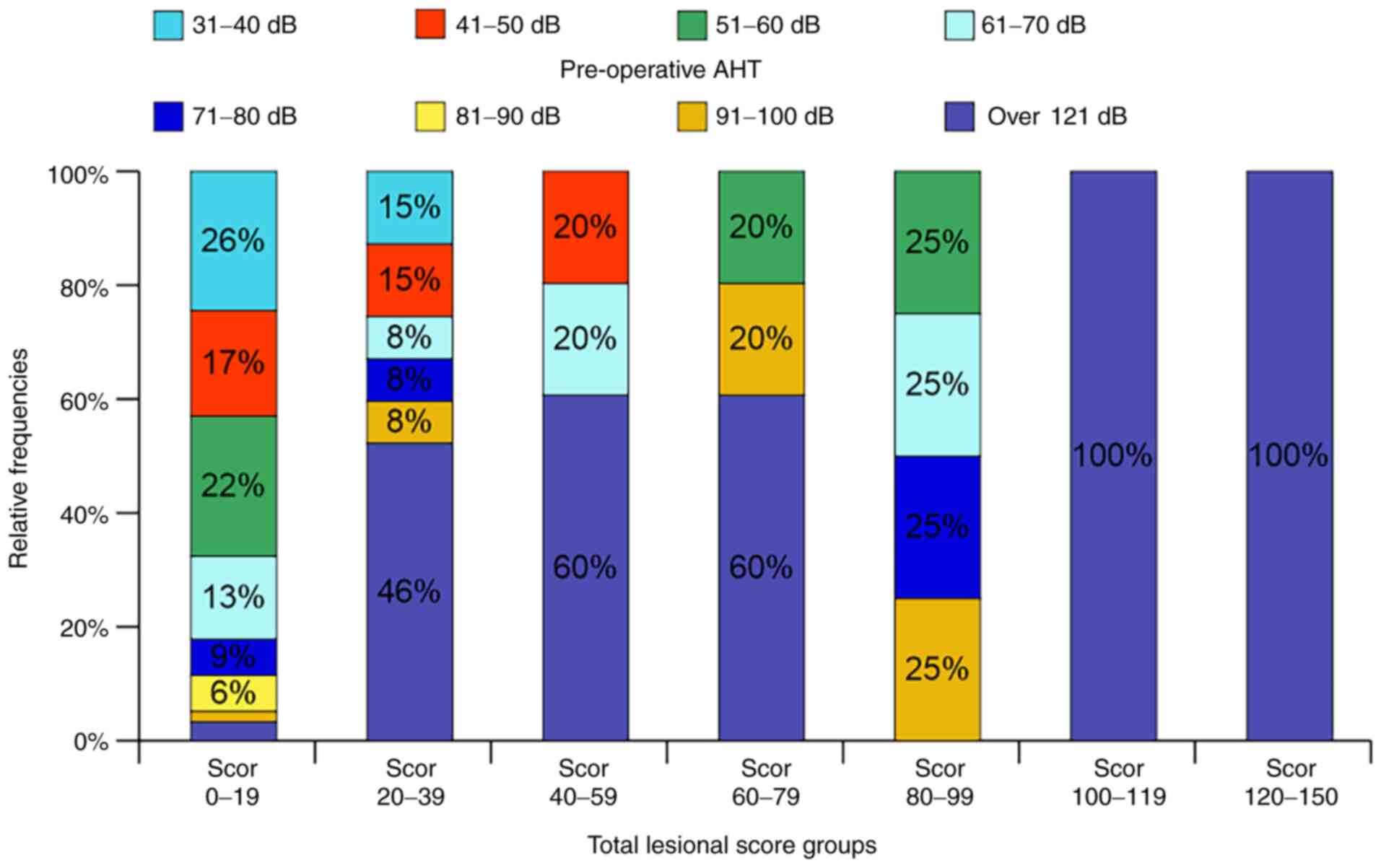
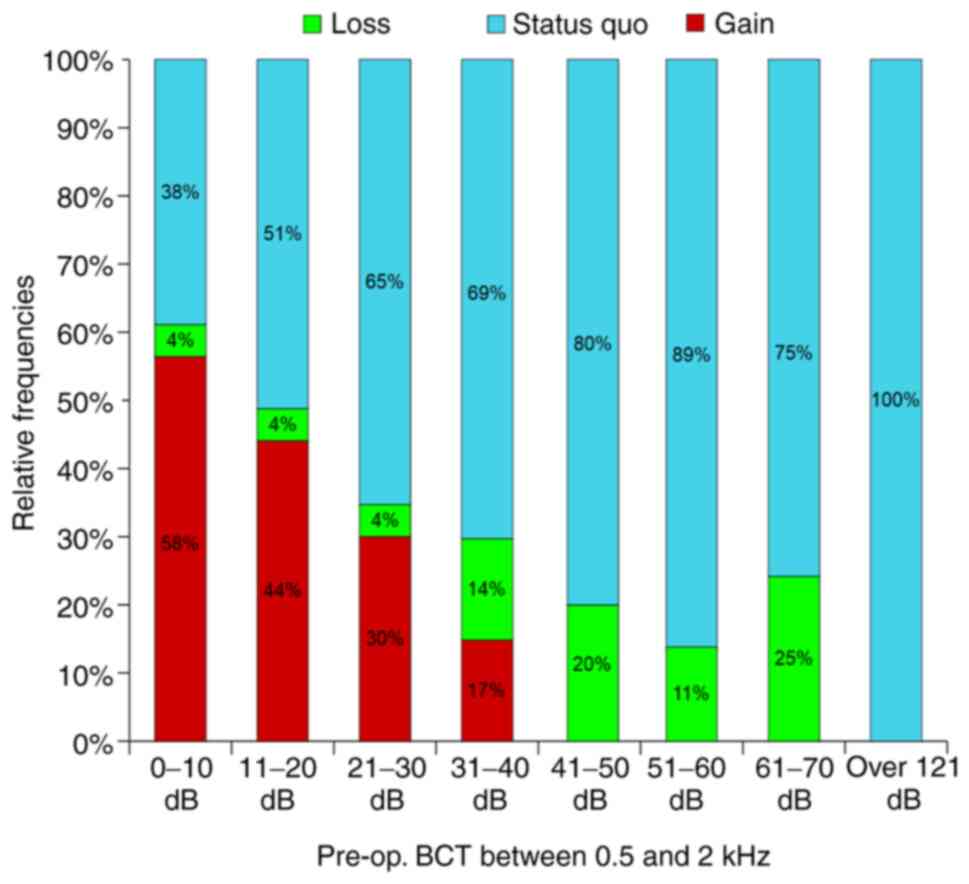
The proportion of severe and profound hearing loss
[71-100 dB SPL (decibel sound pressure level)] was 17%, and the
total hearing loss (>120 dB SPL) was 11% (Fig. 1). The distribution of mild (31-50 dB
SPL) (39%) and moderate hearing loss (51-70 dB SPL) (33%) were also
noted. One could speculate that these values were under the direct
actions of the normal probability law. For pre-operative bone
conduction threshold (BCT), those up to 30 dB represent 60% of the
cases while those between 31-40 dB included 18%. The first group
corresponds to pure conduction type hypoacusis while the second is
shared by conduction and mixed hypoacusis. For groups above 41 dB,
we consider them as part of mixed or sensorineural hypoacusis
(Fig. 1). For well-defined
pre-operative clinical situations, we considered that 0-30 dB
represents a sufficient cochlear reserve for favorable functional
prognosis of the surgery. Above 31 dB, the cochlear reserve is
considered insufficient for functional gain.
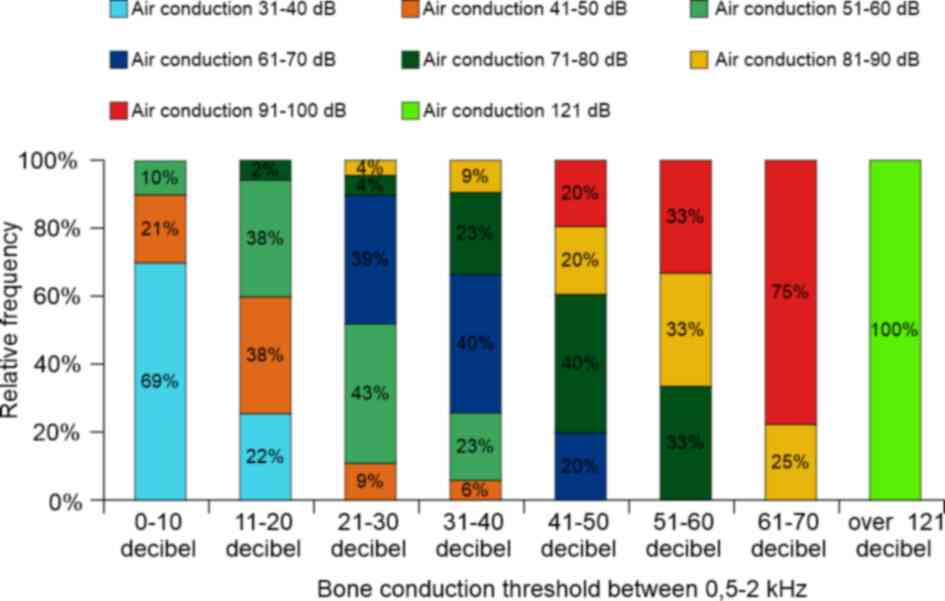
Fig. 2 shows how the
two thresholds interacted within the studied cohort and confirm
that the difference between them was situated within a well-defined
interval (only low BCT allowed for 50-60 dB difference, with an
average of 35 dB). High thresholds allow an under-average
difference but only up to 10-15 dB.
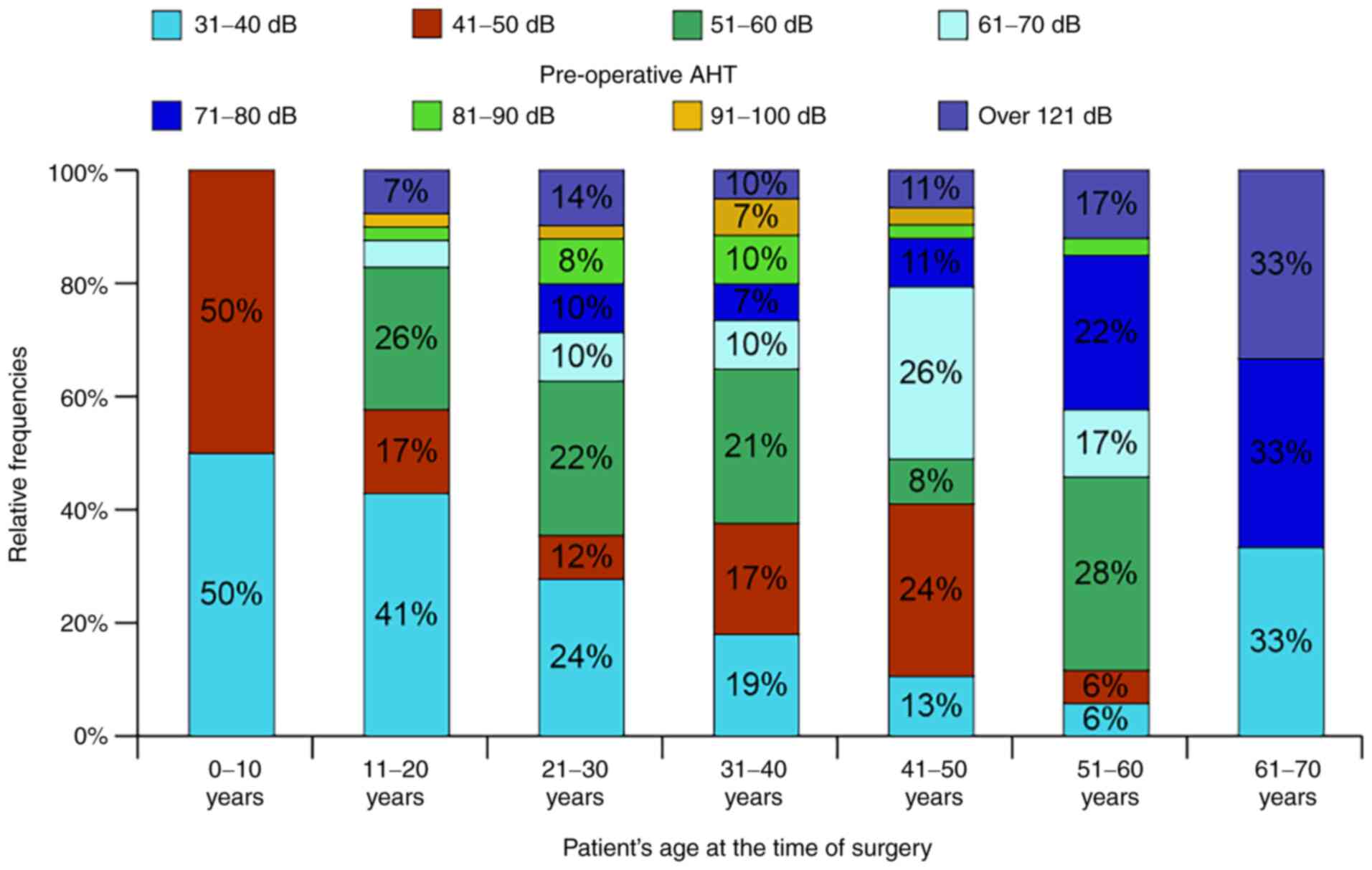
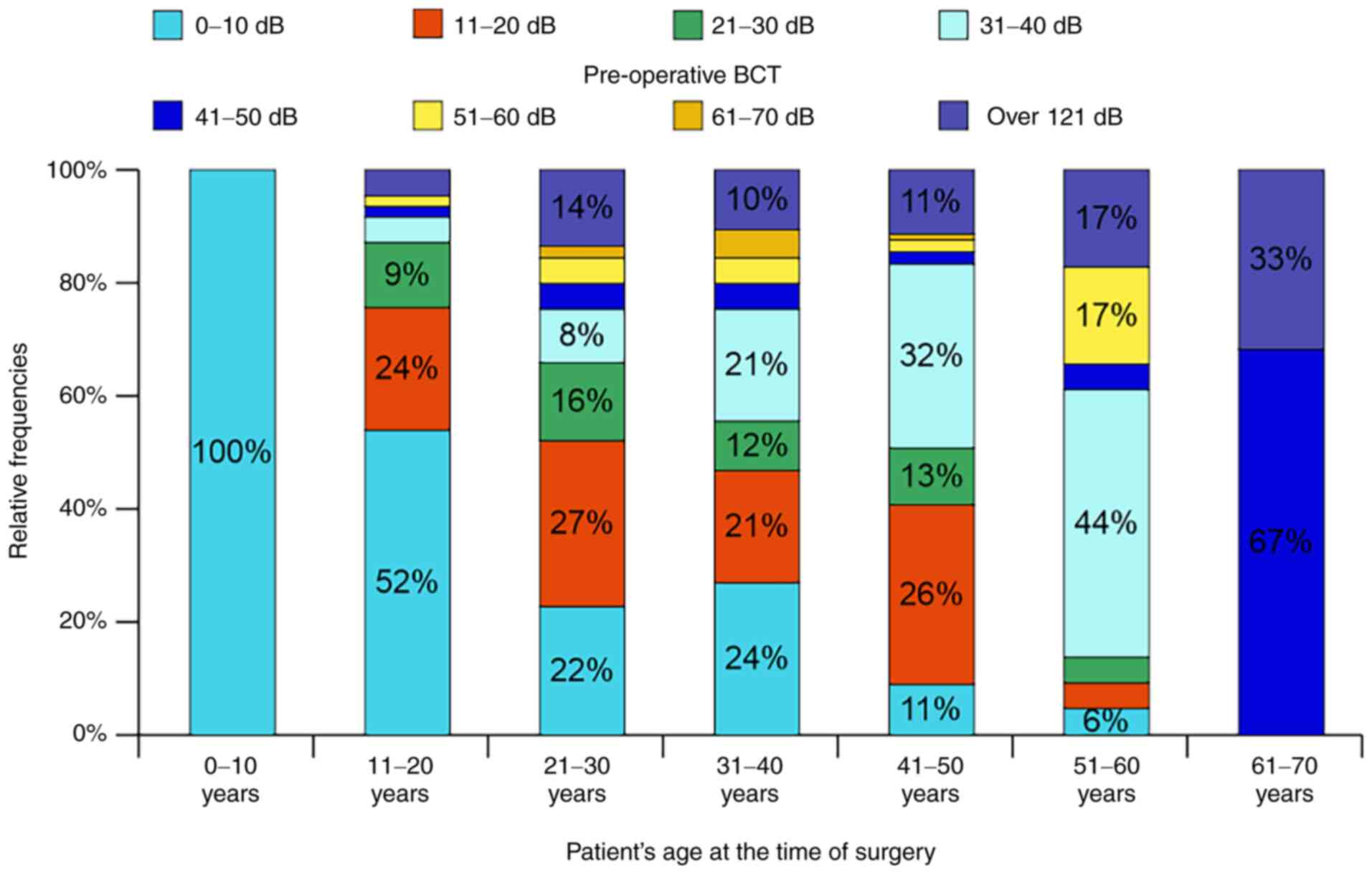
We defined age at the time of surgery as: physical
time, duration of evolution, aging (progressive degradation of
function at different rates), an unstoppable increase in damaged
cell proportion, increase of degree or intensity of disease, rise
of hearing thresholds; all of these being included in a formalized
model (physical-mathematical model). The influence of patient's age
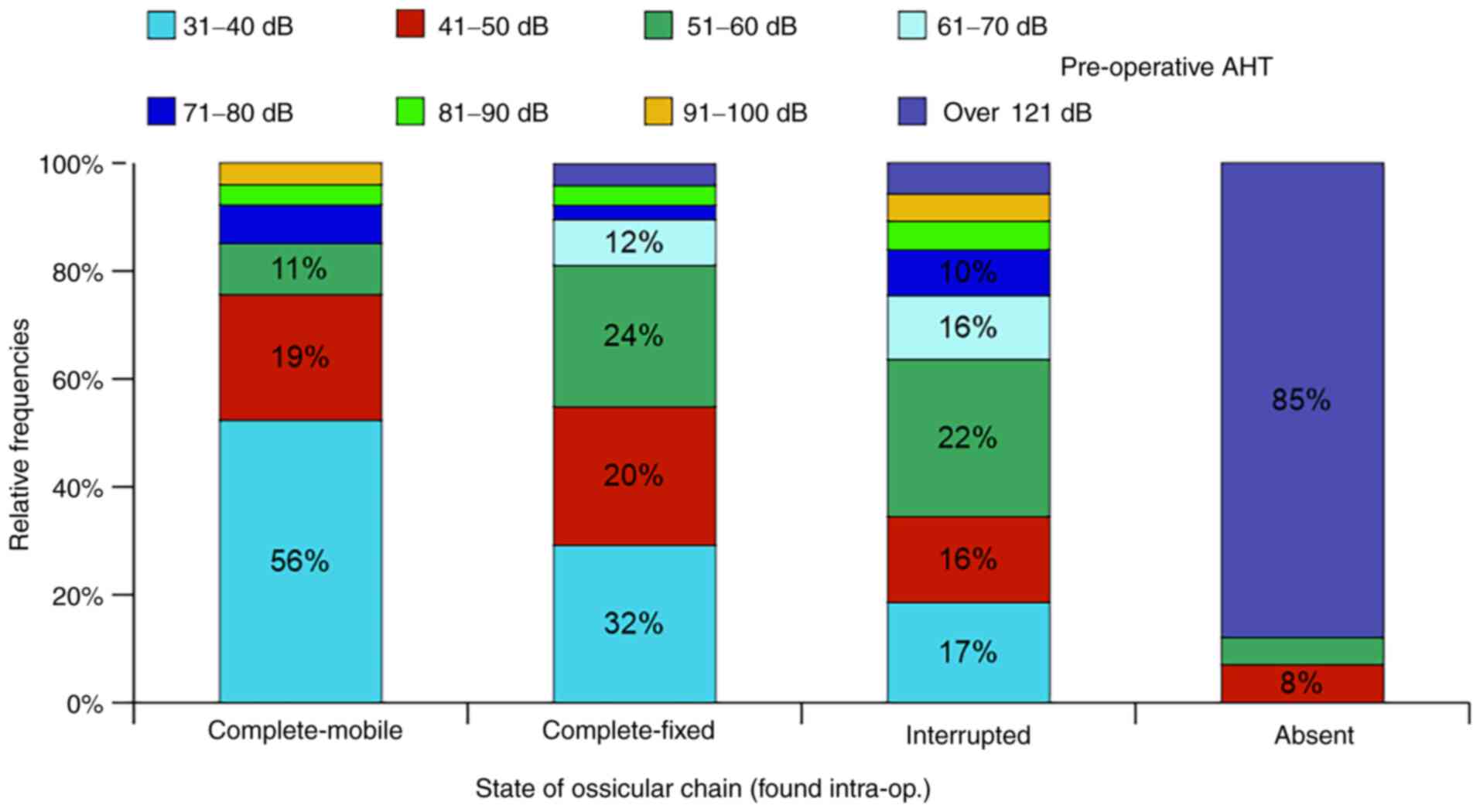
on AHT and BCT are depicted in Figs.
3 and 4. The distribution of
absolute pre-operative hearing thresholds in relation to the state
of the ossicular chain (OC) are presented in Fig. 5 and signify the analytical influence
the physical and functional state of the OC has on hearing results
but cannot entirely explain the intimate mechanisms of normal or
pathological sound transmission. It is surprising that age
(duration of disease evolution) offers an obvious causal connection
as an analytical function to the AHT while the state of the OC
offers an equally obvious connection but of a statistical type. In
other words, for age, the connection is direct as simple, cause →
effect while for OC status the connection is indirect, as cause →
unknown parameters → effect, even more so since the basis of our
discussion is the transmission of sound waves through the ossicular
chain.
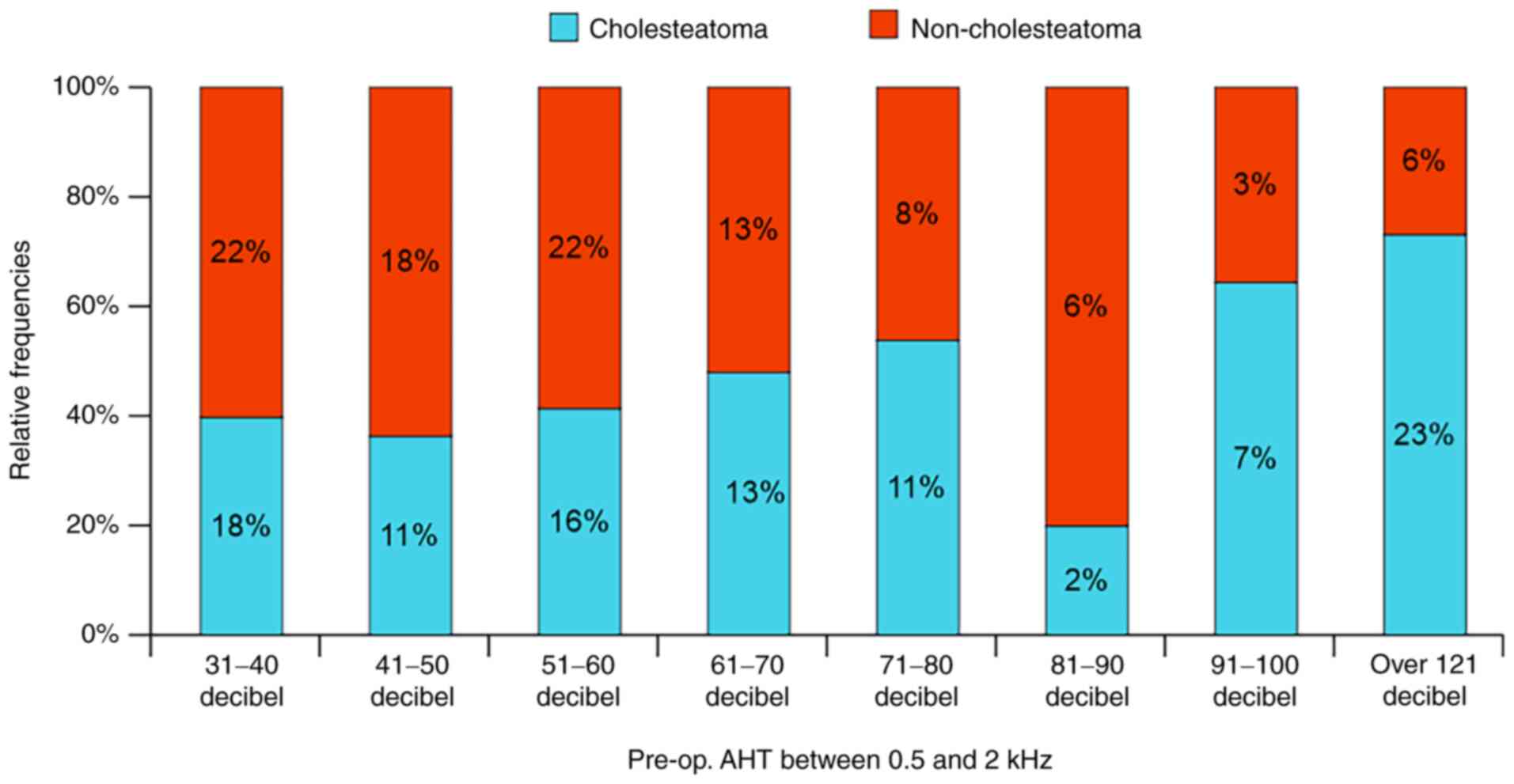
Fig. 6 shows the
distribution of relative frequencies of AHT in relation to the type
of disease and states the negative influence of cholesteatoma. This
statistical information contradicts the common belief that
cholesteatoma tends to preserve hearing for longer periods compared
to non-cholesteatoma middle-ear inflammatory disease.
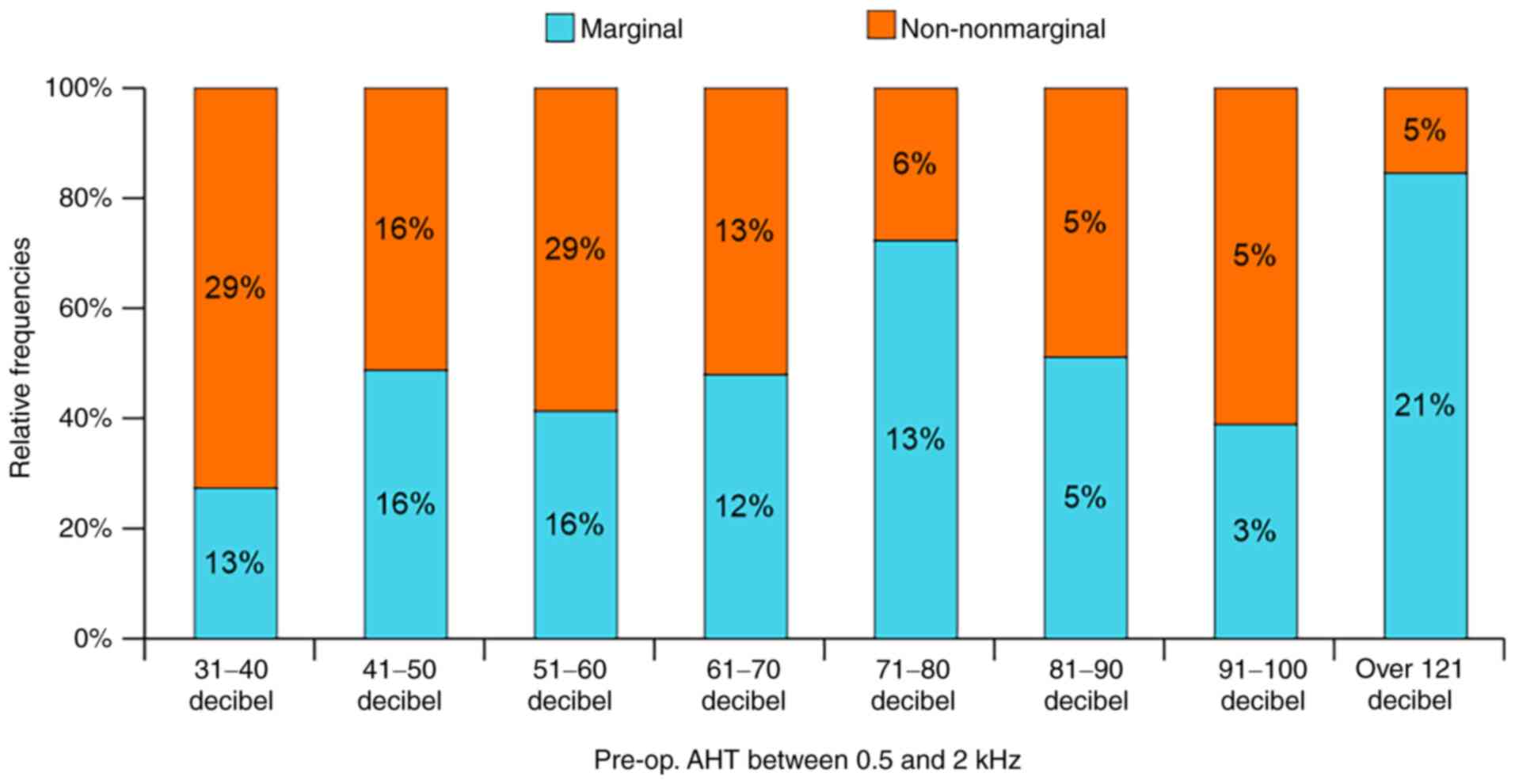
The influence of the type of perforation on hearing
thresholds proved inconsistent and inconsequential (Fig. 7). This indicates that the type of
perforation is wrongly considered as having diagnostic and
prognostic value at least from a functional standpoint if not from
a physical one.
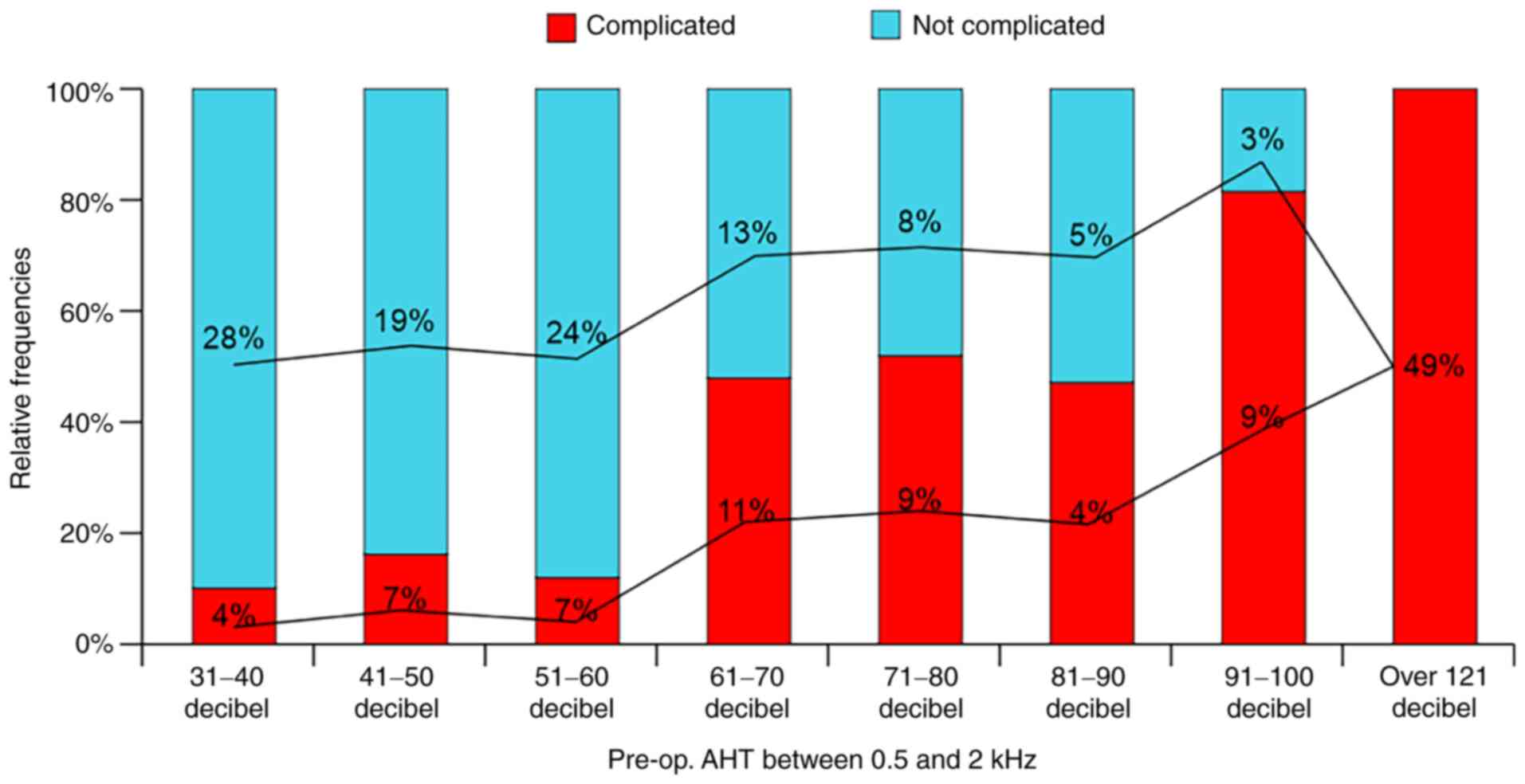
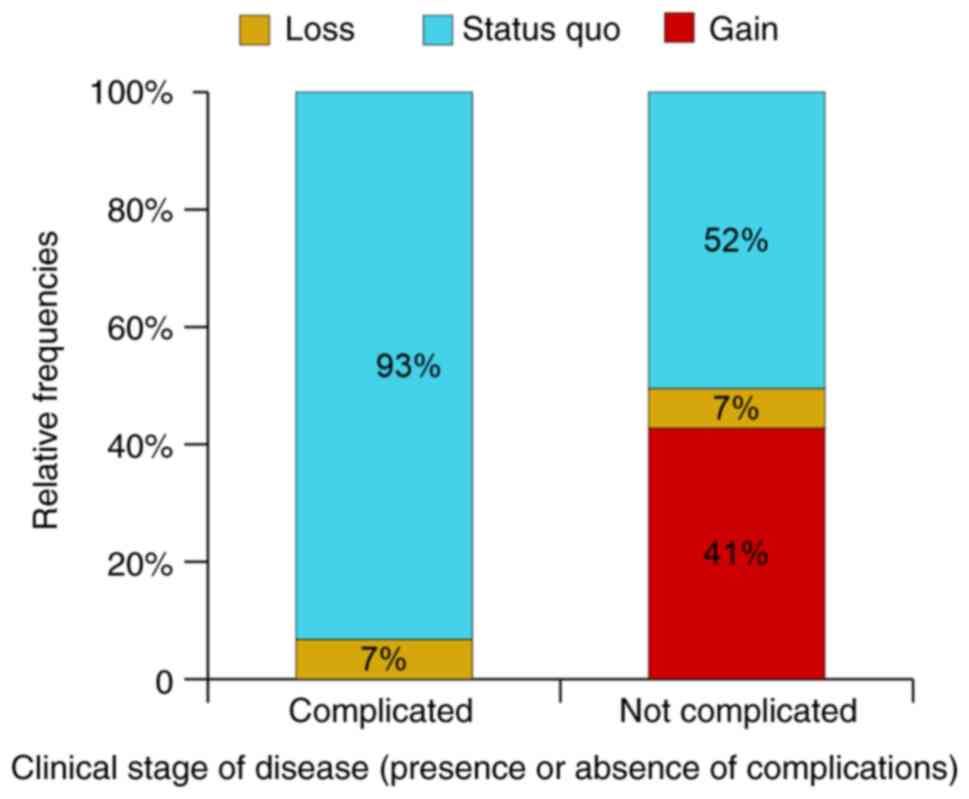
The clinical stage of disease, complicated or not
complicated, proved to have direct analytical function connections
to pre-op AHT distribution. It is obvious that the appearance of a
complication signifies a certain degree of severity of the disease
and therefore a larger number of permanently damaged mastoid cells
(Fig. 8). By connecting the middle
of each column from each series we obtain a graphic representation
of two linear functions of opposing evolution trends.
Since the total lesional score is arbitrary,
including all other lesions except for those of the middle-ear
mucosa (protympanum, tympanic cavity, additus, antrum, mastoid and
petrous cells), the findings shown in Fig. 9 regarding its impact on AHT
distribution become similar to those of Fig. 8.
Results and Discussion
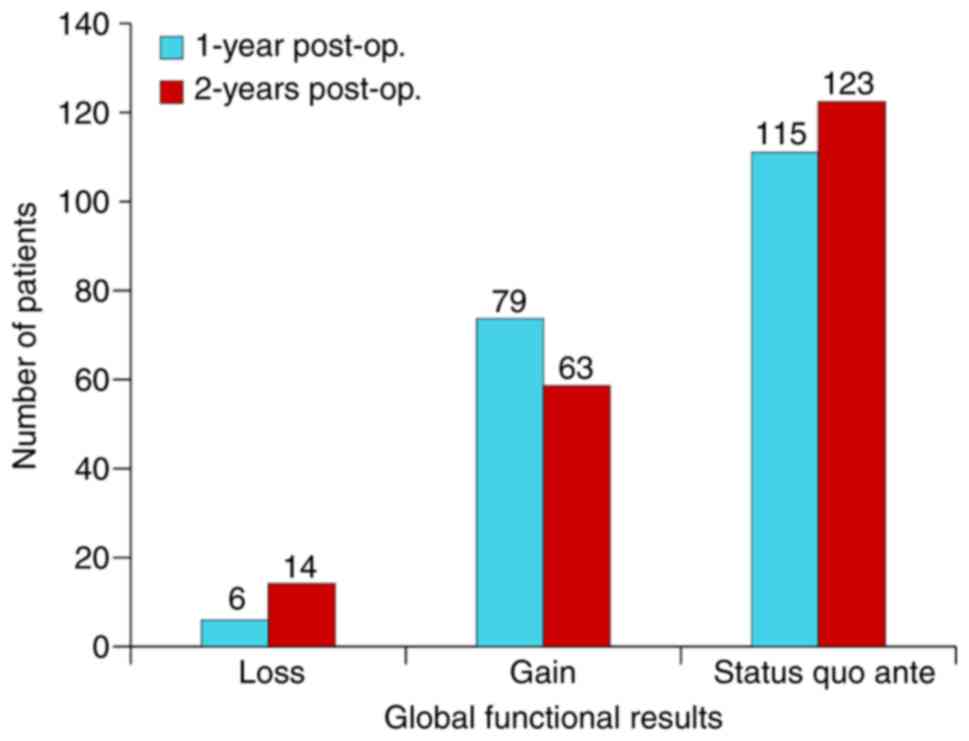
Fig. 10 shows the
global functional results at 1-year and 2 years post-operative,
respectively, and we can observe a 3% loss rate in BC hearing and a
39.5% rate of gain while the rate of unmodified AHT (status quo
ante) is 57.5%. Two years after surgery, the rate of loss
doubled, the rate of gain decreased to 31.5% and the status
quo rate increased to 61.5% (Fig.
10).
It is paramount to note that the results at the end
of the 2nd year remained unchanged for the entire period, up to
8.12 years which leads to the assumption that stable functional
results for a mean period of 8 years could be predicted exclusively
at the end of the cavity epithelization or, better still, 2 years
post-operative. Thus, it becomes extremely useful to inform the
patients and instruct them accordingly. Practically, the audiogram
at 2 months (complete epithelization in 80% of cases) should not be
repeated earlier than 10-22 months post-operative. As for
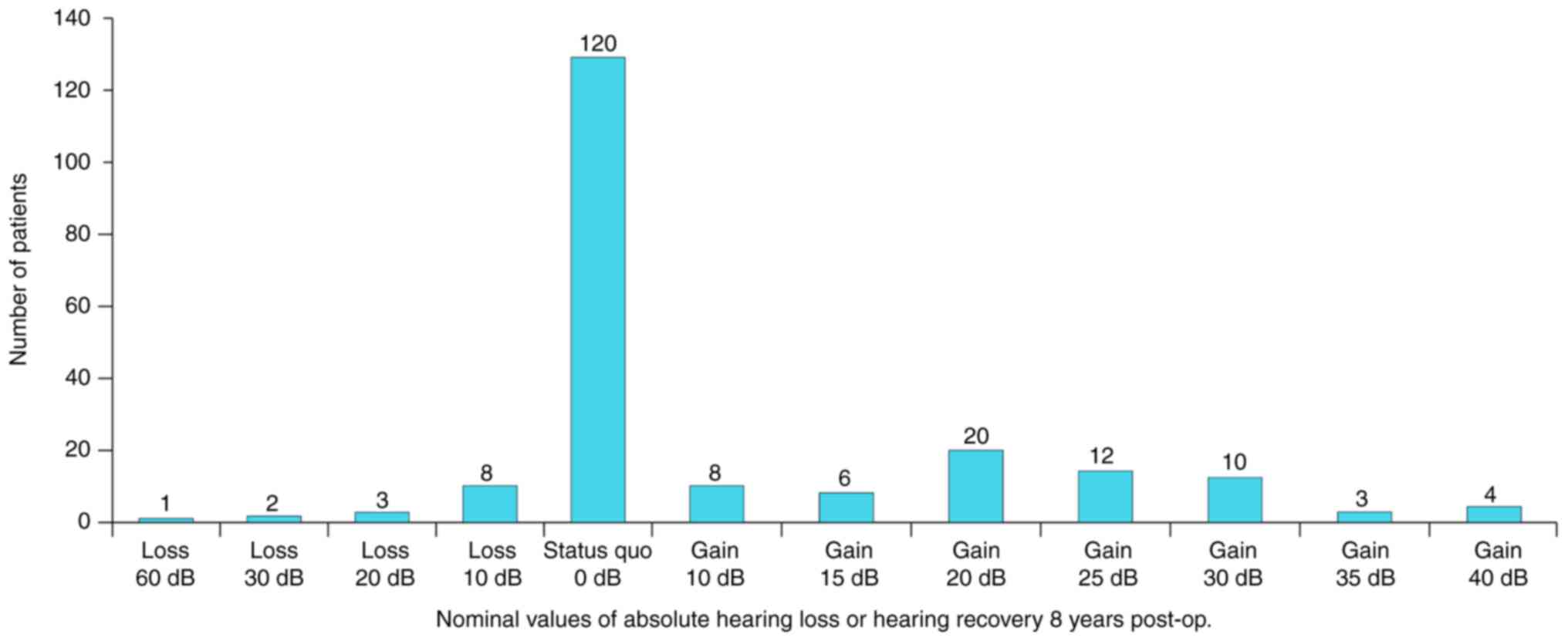
expressing the functional results in absolute values (dB) we can
see from Fig. 11 that the null
value (status quo ante) was observed in 61.5% (n=123) of the
cases, the most drastic loss of 60 dB in 0.5% (n=1), 20-30 dB loss
in 2.5% (n=5), 10 dB loss in 4% (n=8); 10-20 dB gain in 17% (n=34);
25-35 dB gain in 12.5% (n=25) and the best gain of 40 dB in 2%
(n=4) of the patients.
From a practical standpoint, we defined the most
adequate pre- and post-operative terms that could give us
expectancy about the functional results. What can we most
definitely know before surgery?-Age of patient, clinical stage of
disease (complicated, not complicated), type of disease
(cholesteatoma, non-cholesteatoma), type of TM perforation
(marginal, central), radiographic configuration, AHT between 0.5-2
kHz (still, a subjective examination), BCT between 0.5-2 kHz. What
can we discover during surgery?-OC status, total lesional score
(extent of lesions), type of mastoidectomy (radical, modified
radical). Our statistical analysis led us to a number of
conclusions.
For the complicated cases, mastoidectomy did not
lead to hearing threshold gain but provided hearing preservation in
93% of the cases (42 out of the 45 patients). In non-complicated
cases, a gain occurred in 41% (63 of the 155 patients) which was
10% higher than the global gain rate shown in Fig. 10. The status quo ante
occurred in 52% (81 out of 155) of the patients (Fig. 12). Regardless of the state of the
disease, loss of hearing occurred in 7% (3 of 45 and 11 of 155,
respectively). This rate was found to be identical to the mean
global rate of hearing loss (Fig.
10). Of interest, the authors of the present study intend to
publish a subsequent study on the anatomic (drainage) results of
the same cohort, which will further explain the present data.
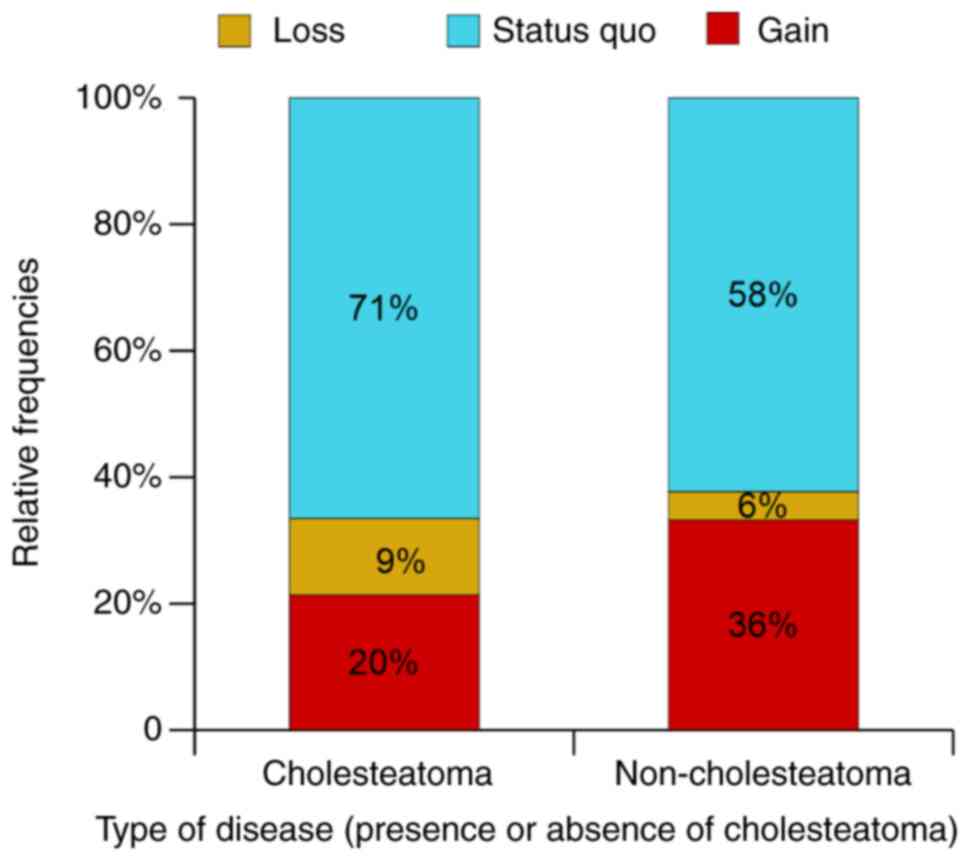
For cholesteatoma, the gain rate was 16% lower than
that for non-cholesteatoma and the hearing loss rate was 2% higher
(and 3% higher than the mean global rate) which provided a
consistent prognostic signification for gain but not for hearing
loss probability (Fig. 13).
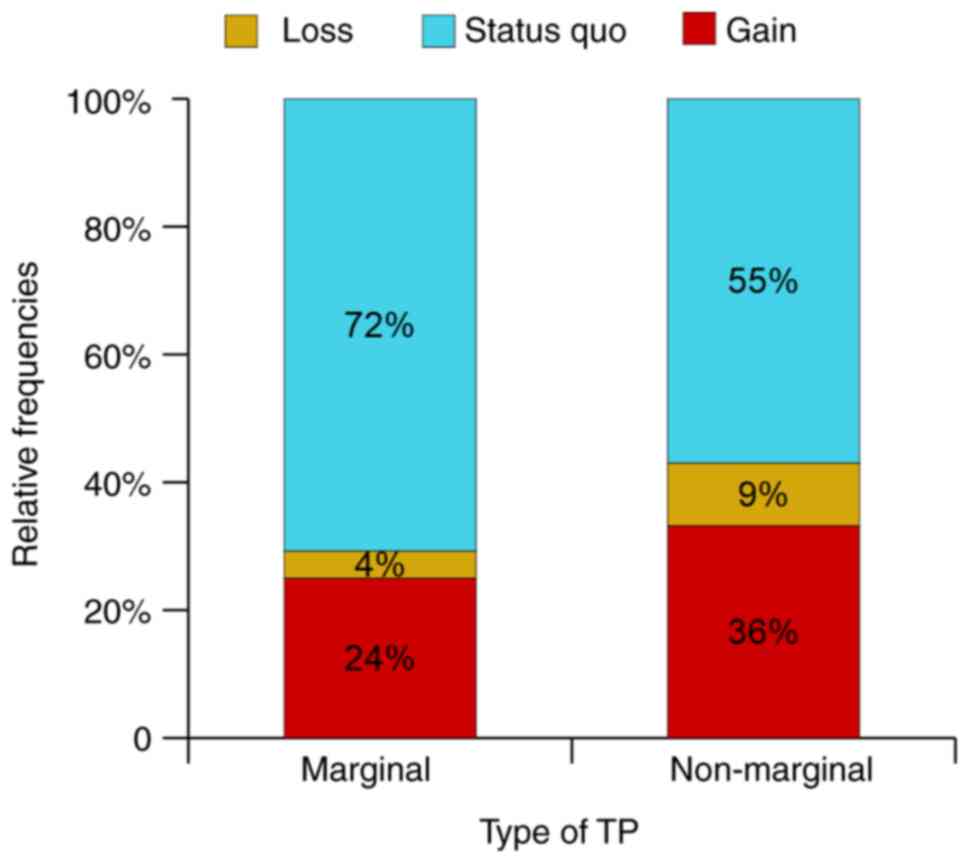
The influence of TM perforation as a predictive
factor was inconsistent and not as clear as for cholesteatoma,
although the numeric values could lead to a negative prognosis in
the case of marginal perforations (Fig. 14).
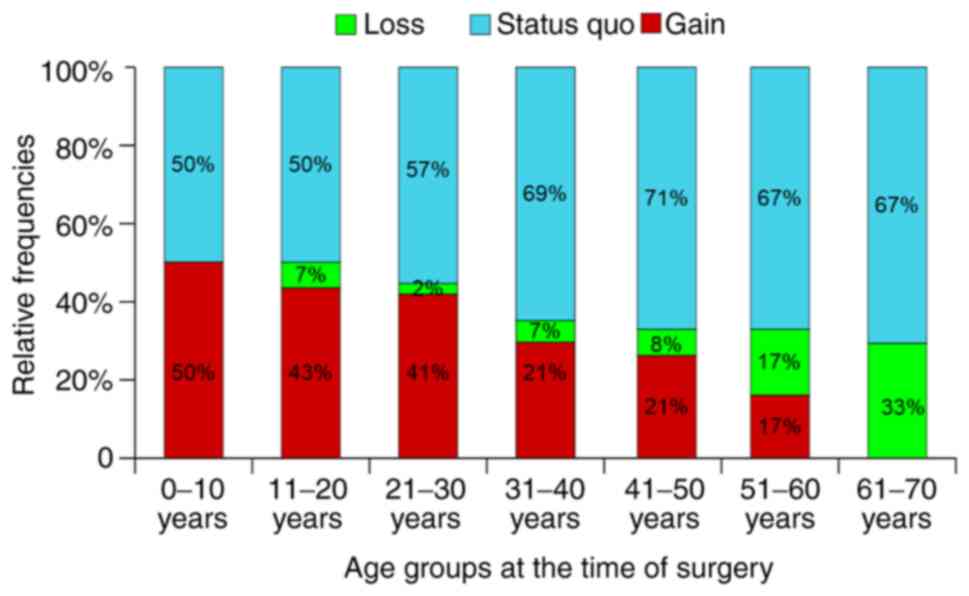
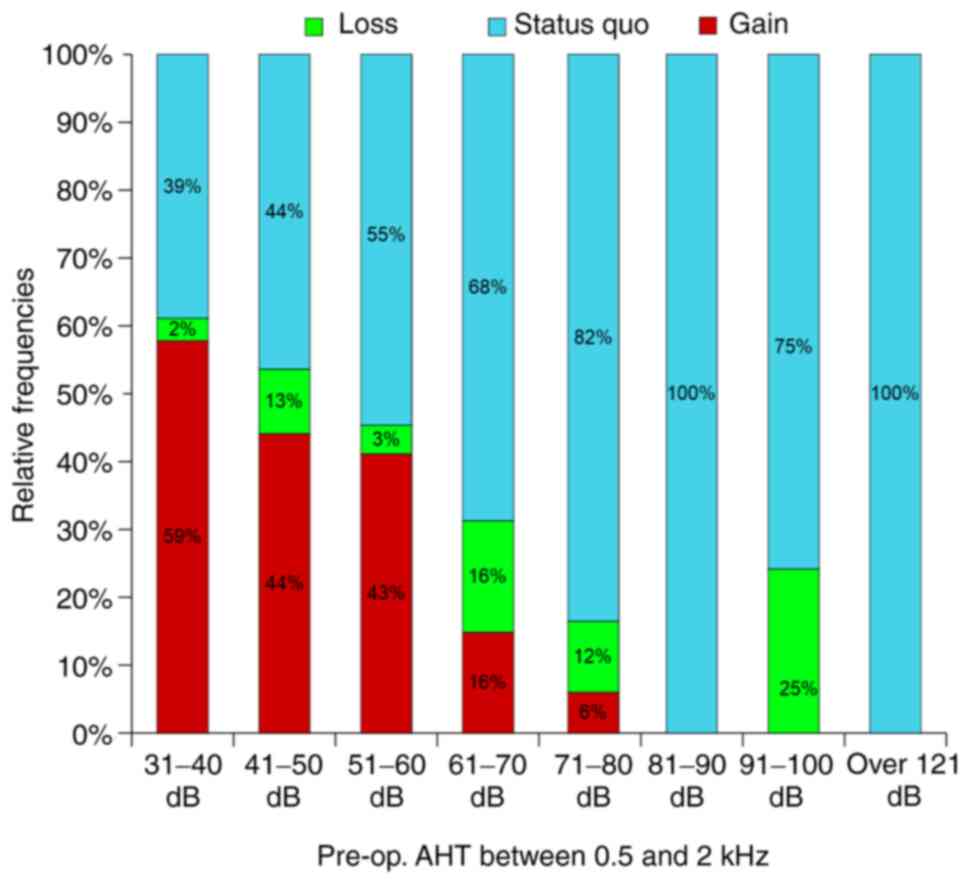
While the connection between the type of disease and
functional results is a statistical one (indirect) in which an
intermediate term could be suspected as dependent on the clinical
forms of disease, the connection to the patient's age and
pre-operative hearing thresholds was direct (cause-effect or
analytical function) (Fig. 15,
Fig. 16 and Fig. 17). We therefore conclude that these
are the fundamental prediction factors for functional results in
mastoidectomy. All three charts show linear analytical functions
with characteristic evolution trends. Thus, positive functional
results were inversely proportional to age and pre-operative
hearing thresholds (descending trend) while the indifferent and
negative results were directly proportional to these parameters
(ascending trend).
This represents an experimental confirmation of
theoretical facts previously stated; to obtain the optimal
functional results, the surgery must take place long before
complications occur or as long as hearing thresholds remain
permissive for gain. Ultimately, the threshold dictates the
prognostic of functional gain.
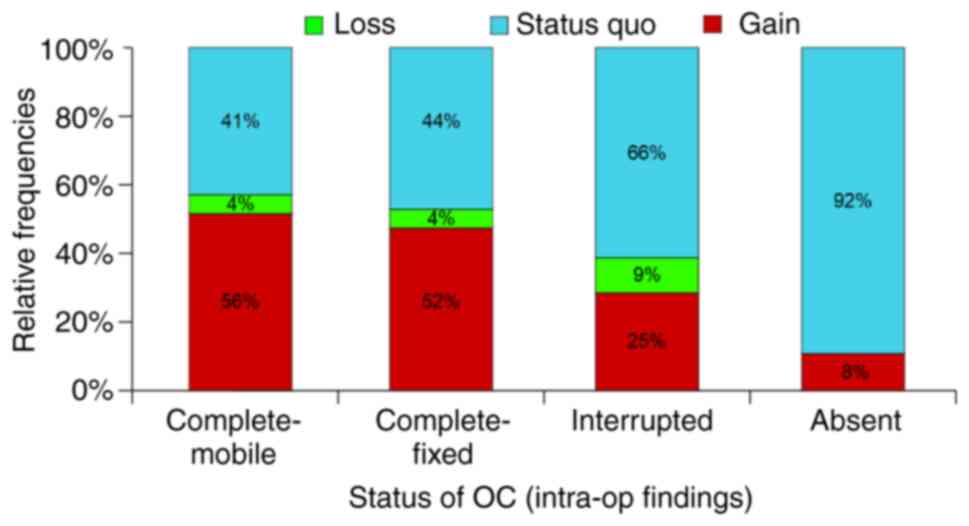
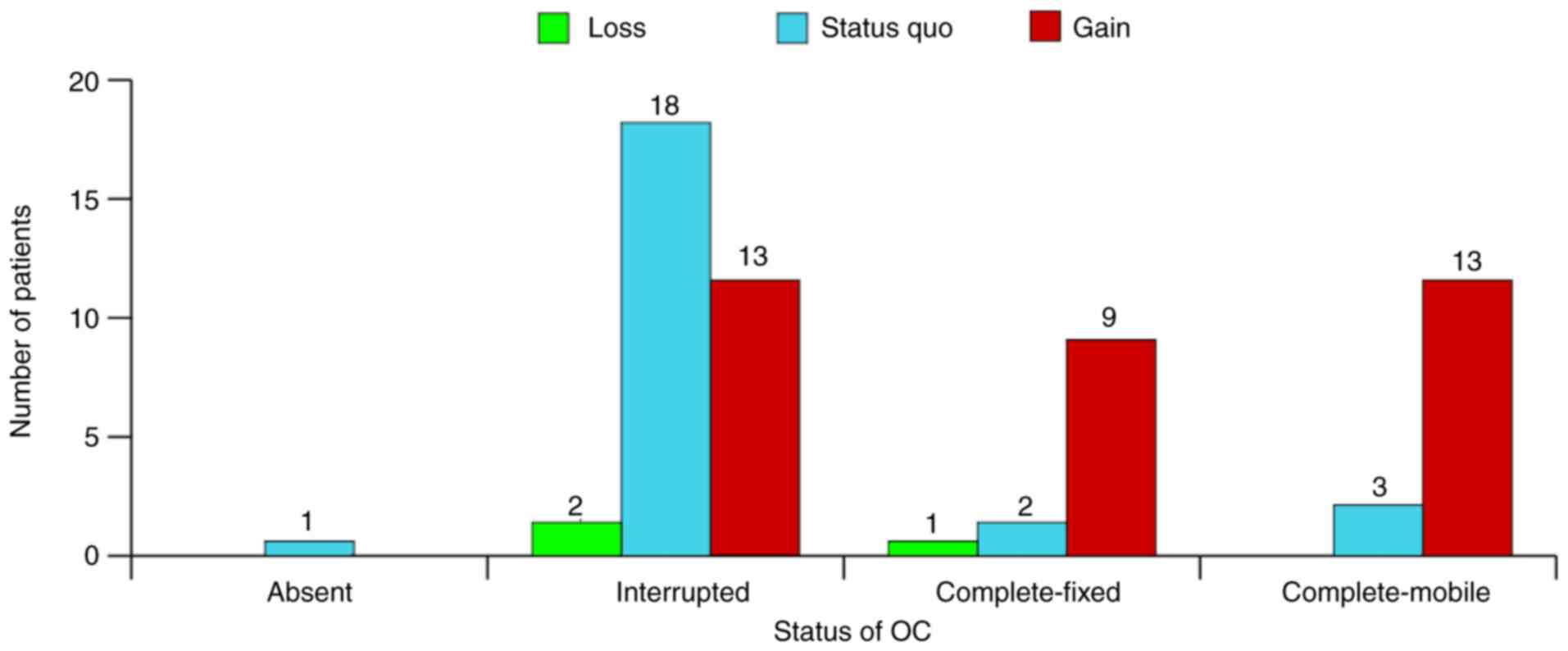
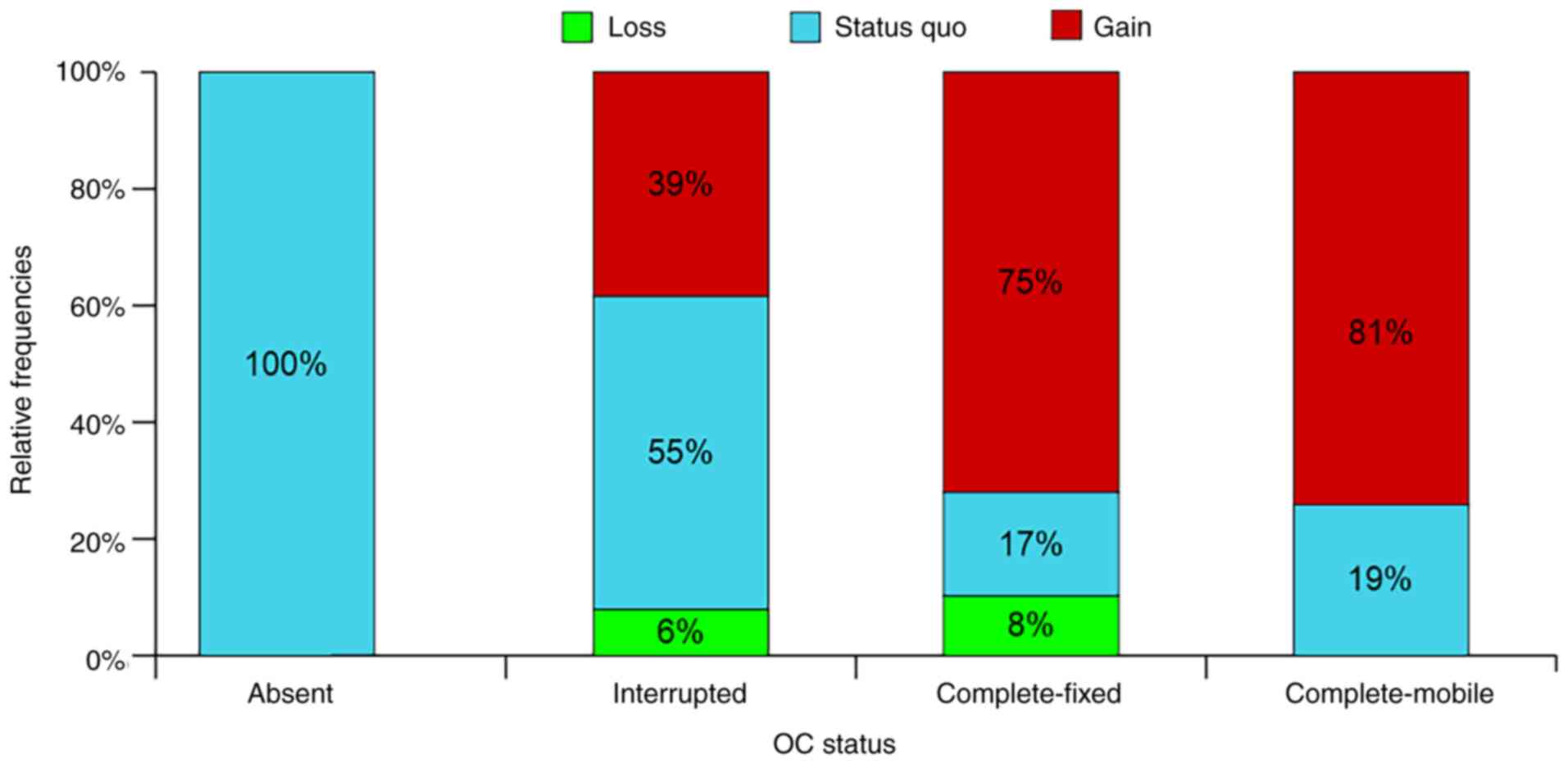
The OC acts as a double standard for prognostic
value since the gain is apparently inexplicably good for
interrupted or missing OC (Fig.
18).
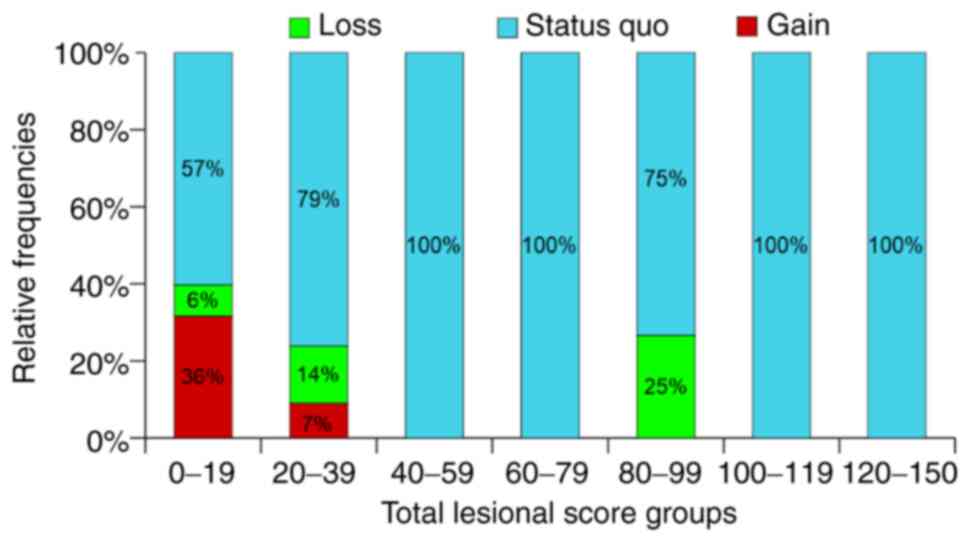
Since the total lesional score has been previously
discussed (14) and is arbitrary,
its influence on functional results is coherent to the theoretical
statement that the intensity of disease is correlated to the
specific weight of the lesional cells (low score mean small
proportion of afflicted cells) (Fig.
19).
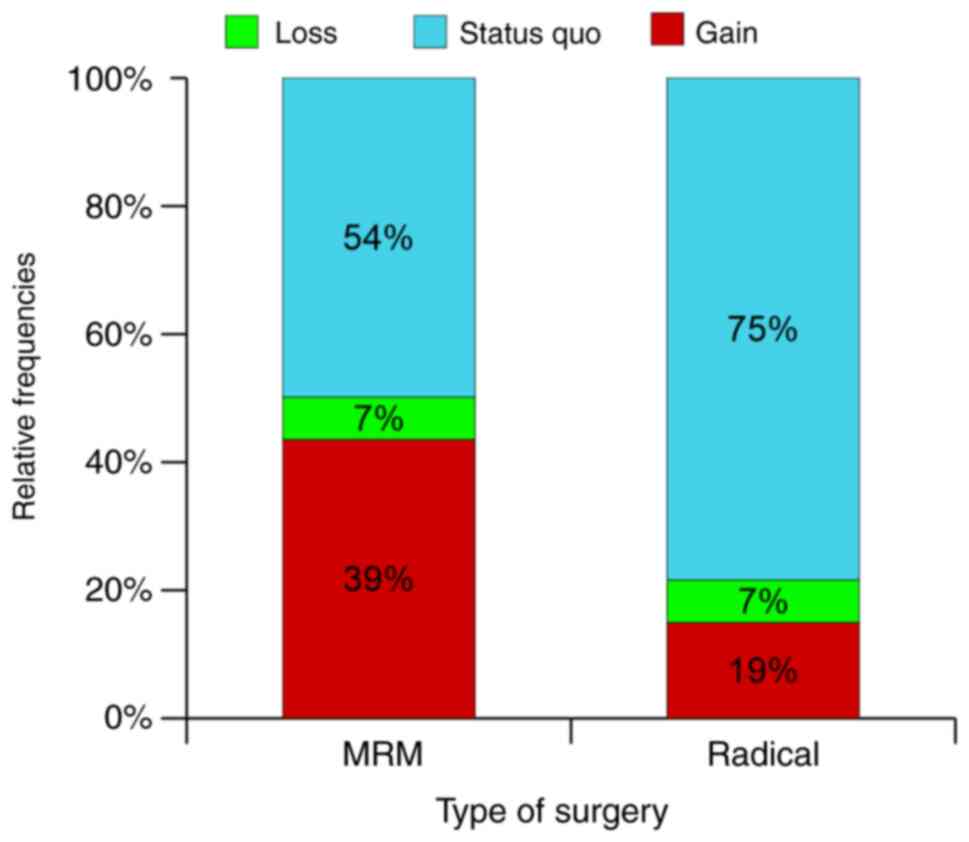
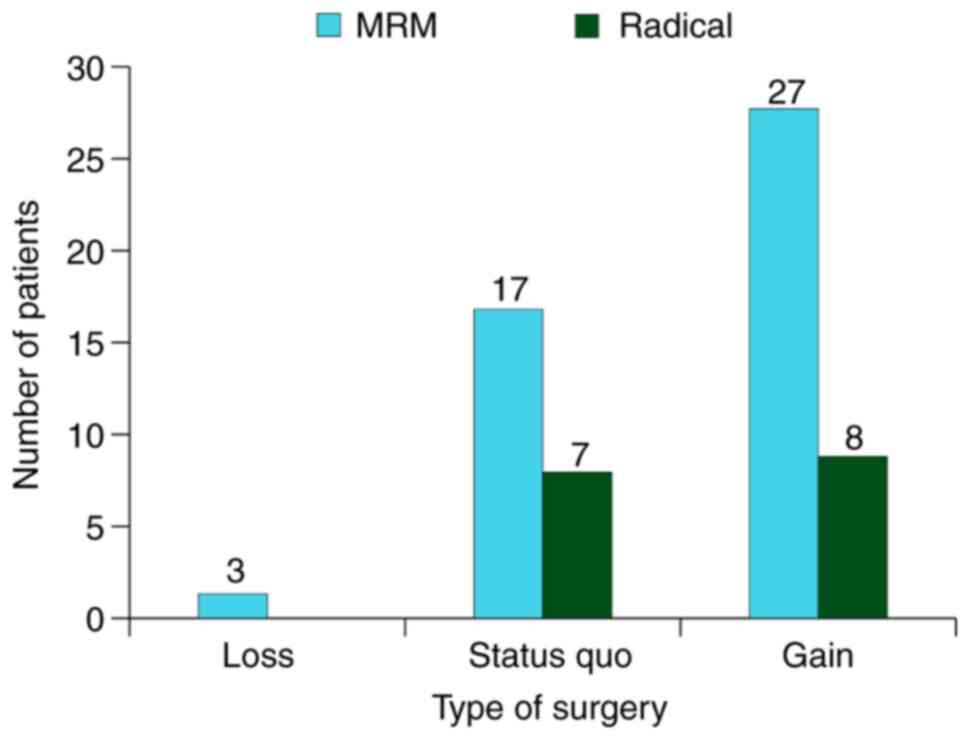
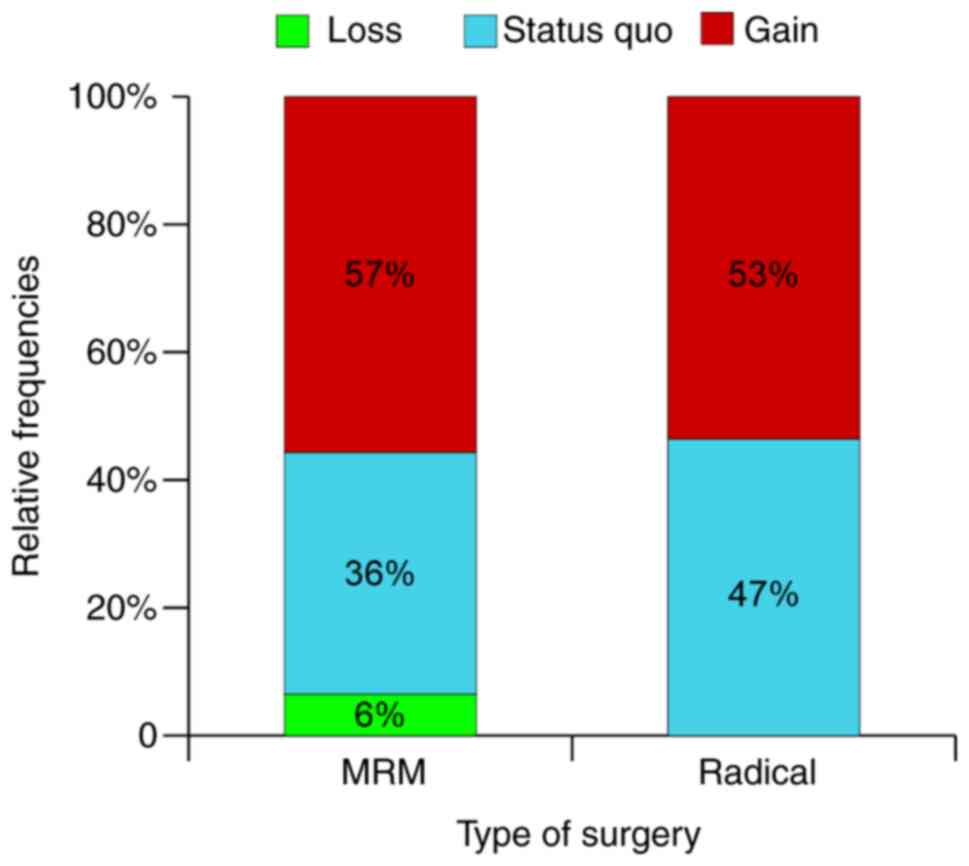
The influence of the type of surgery contradicts
neither theoretical or intuitive considerations and revealed a
double rate of gain for radical modified mastoidectomy compared to
radical mastoidectomy (Fig. 20). A
similar study by Galm et al compared the functional results
[pre- and post-operative air-bone gap (ABG)] for opened and closed
technique mastoidectomy and found no statistically significant
differences. A closed technique has the advantage of preserving the
posterior wall and making the ear ‘water proof’. The post-operative
ABG was ≤20 dB in 41% of patients with closed mastoidectomy and 21%
in patients with opened technique (15). The results were also considered
comparable to those of Stankovic (16) and Lucidi et al (17) as the authors consider it feasible to
achieve good functional results with both techniques. The main
limitation of this study is that it did not benefit from long-term
hearing results.
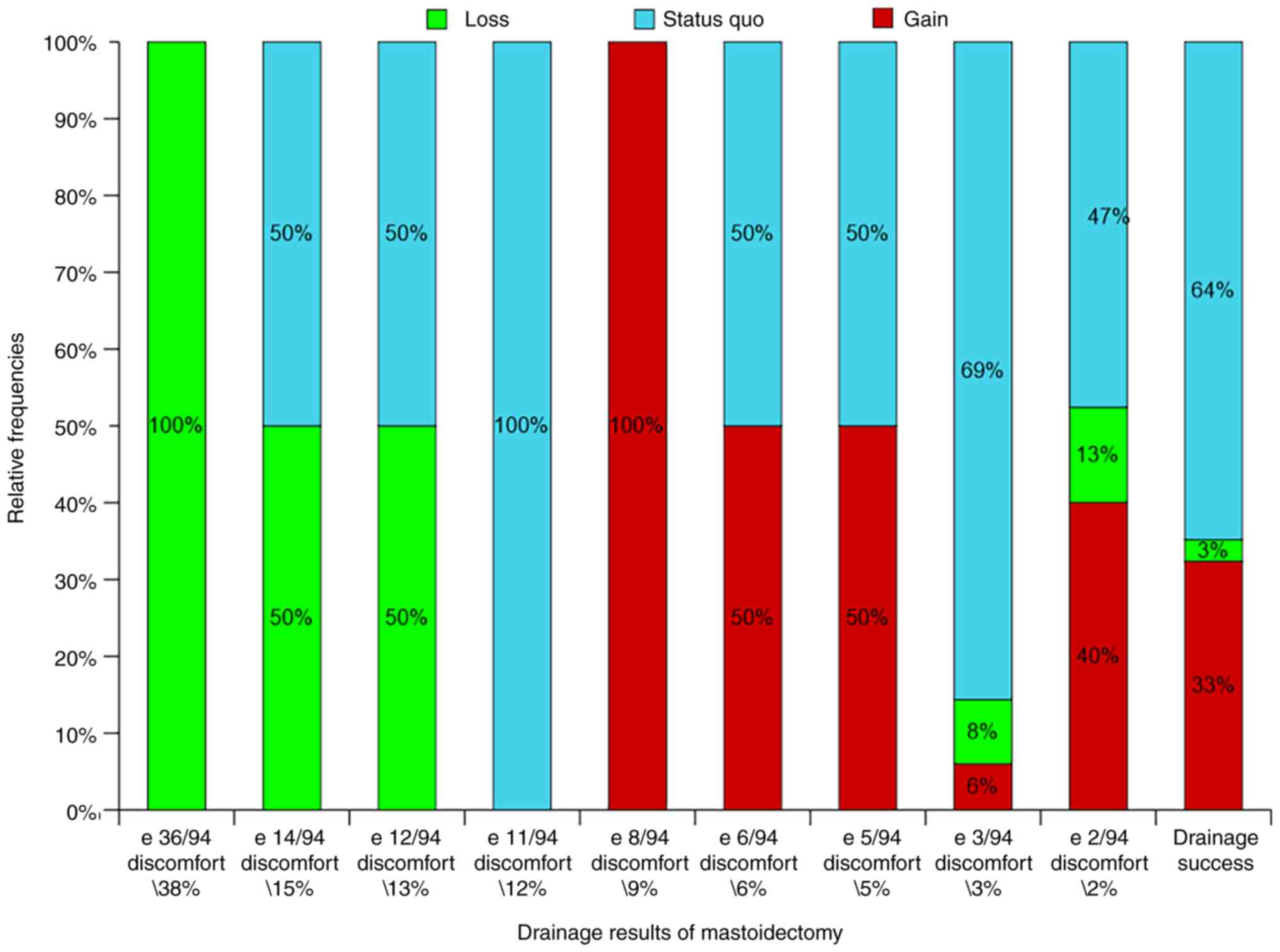
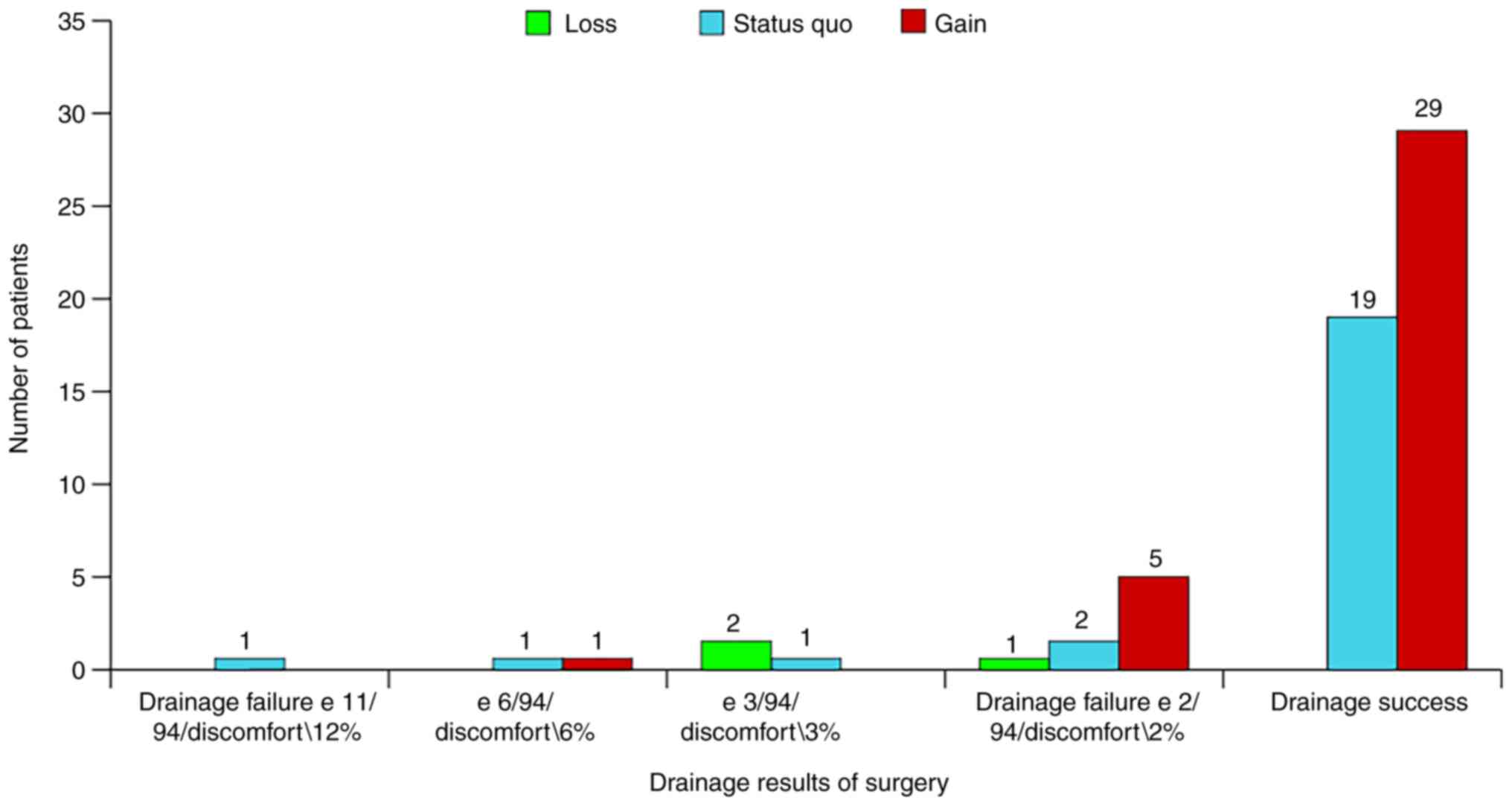
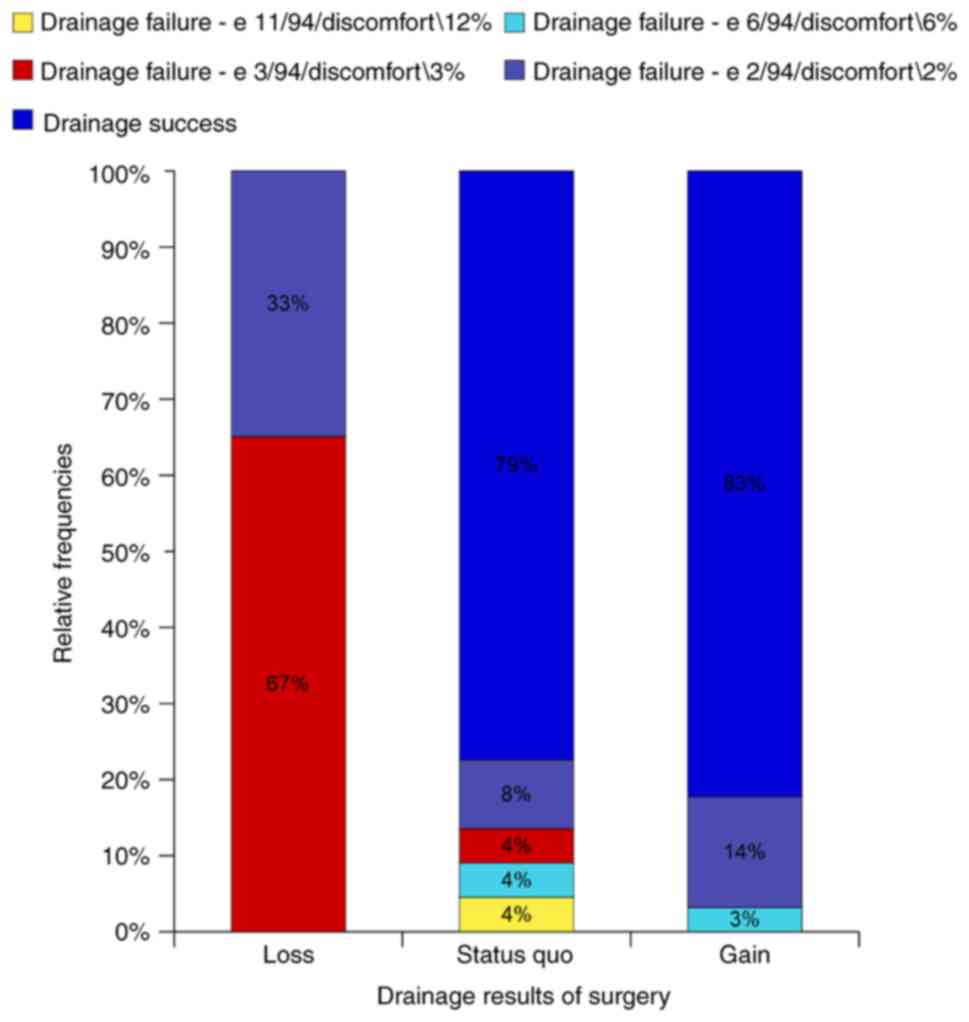
The success rate of the mastoidectomy is the most
important factor for the functional state of an operated ME and is
congruent to the gain rate (Fig.
21). Failed drainage means remnant lesions and therefore poor
functional results. The two types of results (drainage and hearing
gain) are two aspects of the same phenomena. The codes presented in
Fig. 21 represent our own original
quantification of drainage results of mastoidectomy as related to
the number of discharge episodes and therefore to the degree of
comfort/discomfort of the patient. We intend to present our results
in a future article concerning the drainage long-term results of
the same cohort of patients and to further discuss this system of
defining parameters.
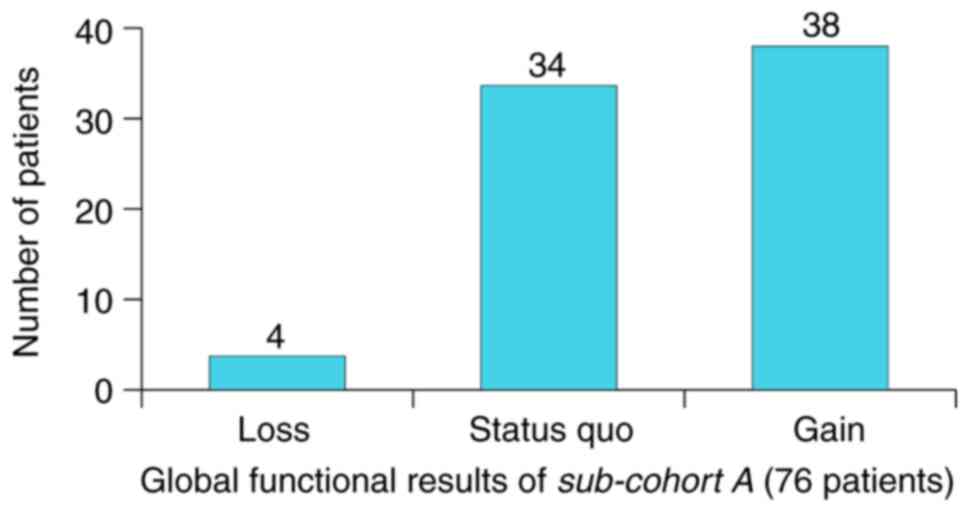
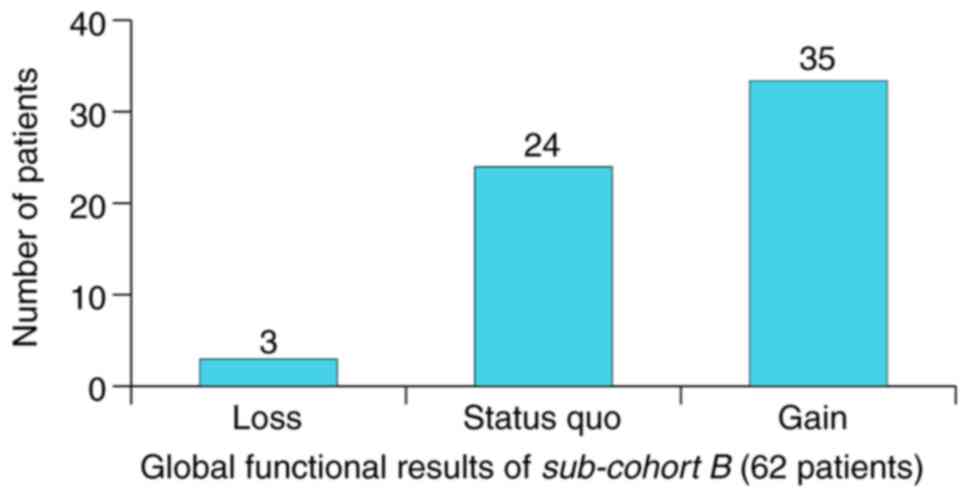
To further confirm our conclusion, we filtered the
analyzed cohort (n=200) by several parameters. First, we filtered
the patients by pre-operative hearing thresholds, the criteria
being AHT up to 50 dB correlated to BCT up to 30 dB. We gathered a
sub-cohort A of 76 patients who showed significant change in
functional results: Gain rate 50%, loss rate 5%, status quo
45% (Fig. 22). The second
criteria, age up to 50, provided us a new sub-cohort B of 62
patients (filtered by both hearing threshold and age) with an
increased gain rate of 56%, an unaltered loss rate of 5% and a
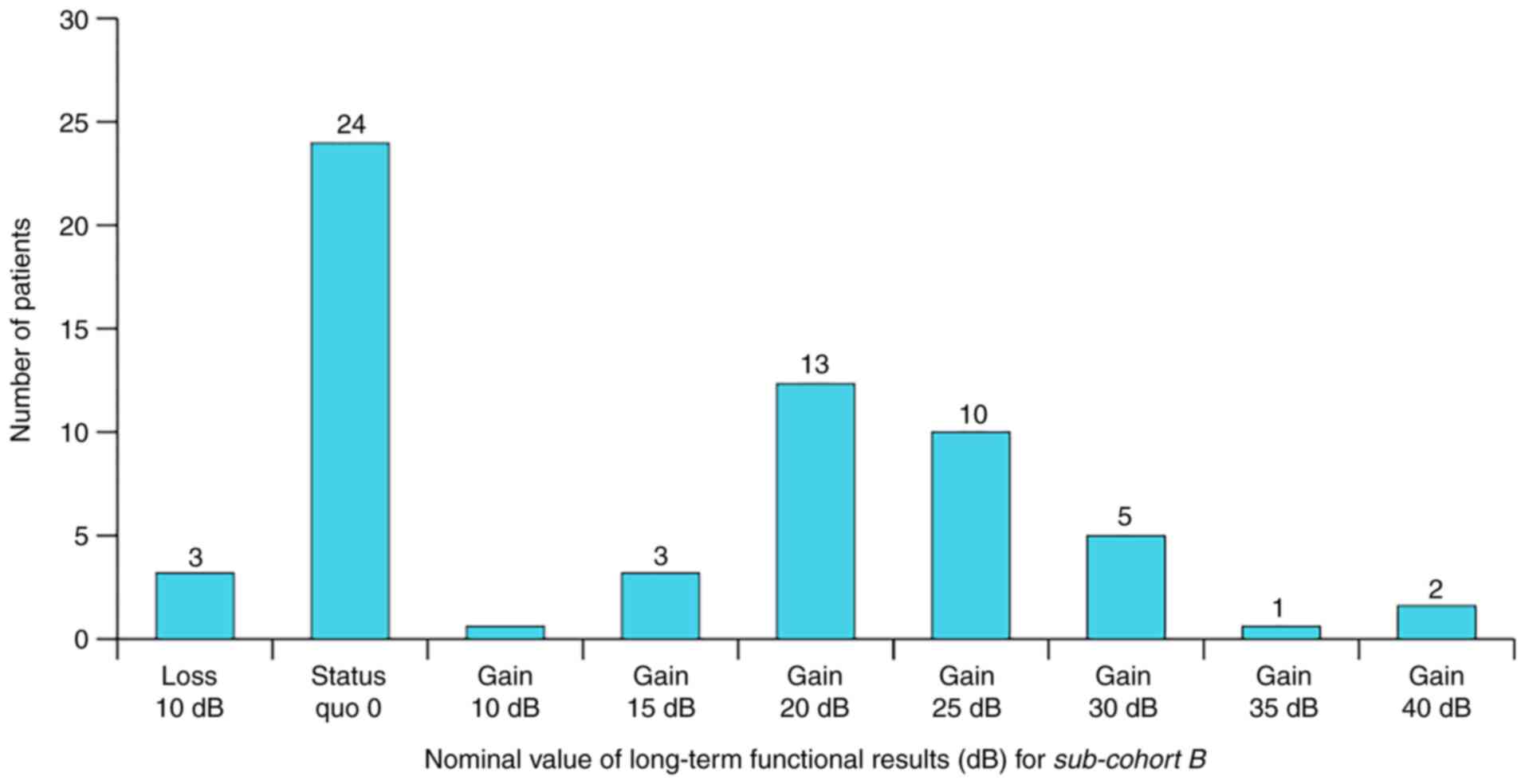
decreased status quo of 39%. Functional results in absolute
values (dB) for sub-cohort B are shown in Fig. 23 where we can observe that the
maximum value for hearing loss (10 dB) is present in 5% of the
patients (n=3), status quo (0 dB) in 39% (n=24) and gain as
follows: 10 dB in 2% (n=1), 15 dB in 5% (n=3), 20 dB in 21% (n=13),
25dB in 16% (n=10), 30 dB in 8% (n=5), 35 dB in 2% (n=1) and 40 dB
in 3% (n=2). We can also note the distribution of recovery results
by the normal law of probability represented by the Gaussian bell
curve with a central axis at the mean value of 20 dB (Fig. 24).
Functional results for the same sub-cohort B
depending on the type of surgery (in absolute and relative
frequencies) are presented in Figs.
25 and 26. For absolute values
(number of patients), the results are apparently paradoxical;
hearing loss appears exclusively in MRM but the explanation is
rather simple since a partial surgery increases the chances of
remnant lesions. For the relative frequencies the distribution was
similar in both types of surgery which signified the intrinsic
property of the surgery to determine well-defined functional
results. All is perfectly explainable from a theoretic and
intuitive point of view since mastoidectomy means exclusion of
lesions and lesions manifest themselves, ultimately, by hearing
loss. The functional results depend on the chance of maximum lesion
exclusion.
The influence of the OC on the functional results
within sub-cohort B were in accordance to our previous results
which state that it can only partially explain the functional
status of the ME. We should however note the high gain rate for
intact OC [81% (n=13)] when mobile and [75% (n=9)] when fixated
(Figs. 27 and 28). This only confirms the statement that
the intensity of the disease is determined by the proportion of
lesions; the OC responds to the presence of disease by fixation and
osteolysis.
The nervus probandi of our entire study is
still the relationship between drainage and the functional results
of mastoidectomy. These are the expression of the same mass random
phenomenon. From this perspective, mastoidectomy represent a direct
intervention in a static population in which stochastic processes
apply. We observed that hearing gain was characterized by a rate of
drainage success of 83% which means that the proportion of remnant
cells with irreversible lesions was contained within the defining
interval of healthy ME mucosa. A status quo was obtained
with a 79% drainage success while loss of hearing was characterized
by a relatively high (67%) degree of drainage failure (3 episodes
of discharge over 94 months; 3% discomfort) (Figs. 29 and 30).
In comparison, Mukherjee et al conducted a
study on 133 MRM patients and published long-term results. Their
conclusions were that MRM allows excellent visualization and has
far lower residual rates than intact canal (ICW) wall procedures. A
total of 61% of the patients had post-operative AC thresholds
within 10 dB of the pre-operative values; 23% showed worsening and
16% improved, which was consistent to our functional results
(5).
A smaller study by Çetinkaya et al reported
the results of 30 patients with various types of mastoidectomies as
follows: 85% hearing gain of 5-35 dB, 10% hearing loss and 3%
status quo ante (3).
The much more extensive study by Kos et al
analysed 259 cases of CWD mastoidectomy by measuring 4-frequency
(0.5, 1, 2 and 4 kHz) average ABG and mean AC threshold. After
revision tympanoplasty, the long-term results were unchanged or
improved for 72% of the patients (18). These results were congruent to those
reported by others (19-27).
A truly similar study is one performed by Pareschi
et al that reported long-term functional results (10-year
follow-up) and used the pure-tone average air conduction threshold
(aPTA) instead of ABG that provides no information on the real
hearing status (28). The
functional results reported were 36.4% with aPTA <30 dB, similar
to Vartiainen (29) with 38.8% aPTA
<40 dB at 10 years (not accounting for the 4 kHz region) and to
other studies with aPTA ranging from 31.2 to 42.4 dB with only 5
years post-operative (29-32).
In conclusion, good functional results cannot be
achieved without good drainage results of the surgery. Even more, a
successful drainage ensures long-term stability of hearing. The two
types of results (drainage and functional) of mastoidectomy are
expressions of the same phenomenon defined as a conversion of a
static population by binary division in respect to the spatial
distribution of its constituting units.
Functional results are linked by an analytical
function to the intensity of the disease (pre-operative AHT and
BCT) and length of evolution (age of patient). These parameters
vary inversely proportional and can be considered as complete and
precise analytical instruments for both functional and drainage
results of mastoidectomy.
The global rate of hearing loss after surgery was
7%, the global rate of gain was 32% and the rate of status quo
ante was 61%.
The favorable prognostic terms for good functional
results include: AHT under 50 dB, BCT under 30 dB and age under 50.
When all these are present, the gain rate increased to 56% and the
hearing loss rate decreased to 5% with a nominal value of 10 dB.
The maximum rate of gain was 81% and of loss was 0%.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
HM and MR contributed equally to this work and
should, therefore, both be considered first authors of this
article. HM and MR were responsible for the original idea,
conception, patient selection and care, operations, data collection
and editing structure. AIM, AB and GC assisted with patient care
and follow-up, gathered the medical information and provided a
final view of the article. MAS was responsible for the data
analysis and graphical representation of the results and provided a
final view of the article. All authors read and approved the final
manuscript for publication.
Ethics approval and consent to
participate
For this study, agreement was obtained from the
Research Ethics Committee of the Faculty of Medicine, Titu
Maiorescu University (resolution 1/25.05.2021). All patients
provided informed consent and approved the publication of data.
Patient consent for publication
Not applicable.
Authors' information
Horia Mocanu: ORCID: 0000-0002-9708-8285;
Adela-Ioana Mocanu: ORCID: 0000-0003-0725-2131; Alexandru Bonciu:
ORCID: 0000-0002-5251-4594; Gabriella Coadă: ORCID:
0000-0003-4104-8716; Mihai-Adrian Schipor: ORCID:
0000-0002-2677-9353; Marian Rădulescu: ORCID:
0000-0002-4029-7721.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Millstein S: The history of mastoid
surgery. Am J Otol. 1:174–178. 1980.PubMed/NCBI
|
|
2
|
Alecu I, Mocanu H and Călin IE:
Intellectual mobility in higher education system. Rom J Mil Med.
120:16–21. 2017.
|
|
3
|
Çetinkaya EA, Çukurova I, Olgun L and
Kabakçi R: Long-term outcomes of functional surgery for attic
cholesteatoma. ENT Updates. 6:29–33. 2016.
|
|
4
|
Bento RF and Fonseca AC: A brief history
of mastoidectomy. Int Arch Otorhinolaryngol. 17:168–178.
2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Mukherjee P, Sauders N, Liu R and Fagan P:
Long-term outcome of modified radical mastoidectomy. J Laryngol
Otol. 118:612–616. 2004.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Neudert M, Bornitz M, Mocanu H,
Lasurashvili N, Beleites T, Offergeld C and Zahnert T: Feasibility
study of a mechanical real-time feedback system for optimizing the
sound transfer in the reconstructed middle ear. Otol Neurotol.
39:e907–e920. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Mocanu H, Bornitz M, Lasurashvili N and
Zahnert T: Evaluation of Vibrant® Soundbridge™ positioning and
results with laser doppler vibrometry and the finite element model.
Exp Ther Med. 21(262)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Mocanu H and Oncioiu I: The influence of
clinical and environmental risk factors in the etiology of
congenital sensorineural hearing loss in the Romanian population.
Iran J Public Health. 48:2301–2303. 2019.PubMed/NCBI
|
|
9
|
Mocanu H: The role of perinatal hearing
screening in the normal development of the infant's language. In:
Debating Globalization. Identity, Nation and Dialogue. 4th edition.
Boldea I and Sigmirean C (eds). Arhipeleag XXI Press, Tirgu Mures,
pp562-569, 2017.
|
|
10
|
Mocanu H: The economic impact of early
diagnosis of congenital hearing loss. In: Debating Globalization.
Identity, Nation and Dialogue. 4th edition. Boldea I and Sigmirean
C (eds). Arhipeleag XXI Press, Tirgu Mures, pp556-561, 2017.
|
|
11
|
Cook JA, Krishnan S and Fagan PA: Hearing
results following modified radical versus canal-up mastoidectomy.
Ann Otol Rhinol Laryngol. 105:379–383. 1996.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Fagan PA: Modified radical mastoid surgery
for chronic ear disease. Ann Acad Med Singap. 20:665–673.
1991.PubMed/NCBI
|
|
13
|
Perez de Tagle JR, Fenton JE and Fagan PA:
Mastoid surgery in the only hearing ear. Laryngoscope. 106:67–70.
1996.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Mocanu H, Mocanu AI, Drăgoi AM and
Rădulescu M: Long-term histological results of ossicular chain
reconstruction using bioceramic implants. Exp Ther Med.
21(260)2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Galm T, Martin TP and Raut V: Open and
closed cavity mastoid operations: Comparing early hearing results.
Eur Arch Otorhinolaryngol. 270:77–80. 2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Stankovic MD: Audiological results of
surgery for cholesteatoma; Short- and long-term follow-up of
influential factors. Otol Neurotol. 29:933–940. 2008.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lucidi D, De Corso E, Paludetti G and
Sergi B: Quality of life and functional results in canal wall down
vs canal wall up mastoidectomy. Acta Otorhinolaryngol Ital.
39:53–60. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kos MI, Castrillon R, Montandon P and
Guyot JP: Anatomic and functional long-term results of canal
wall-down mastoidectomy. Ann Otol Rhinll Laryngol. 113:872–876.
2004.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Veldman JE and Braunius WW: More than 10
years of revision-cleaning and revision-reconstructive ear surgery
in chronic otitis media; good long-term results. Ned Tijdschr
Geneeskd. 141:1563–1567. 1997.PubMed/NCBI(In Dutch).
|
|
20
|
Tran Ba Huy P, Chaar I, Fouda A, Almorad
M, Brette MD and Freyss G: Anatomical and functional evaluation,
after 3 and 5 years, of 94 cases of chronic cholesteatomatous
otitis media. Clinical and therapeutic implications. Ann
Otolaryngol Chir Cervicofac. 105:29–38. 1988.PubMed/NCBI(In French).
|
|
21
|
Brown JS: A ten-year statistical follow-up
of 1142 consecutive cases of cholesteatoma: The closed vs the open
technique. Laryngoscope. 92:390–396. 1982.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Harvey SA and Fox MC: Relevant issues in
revision canal wall-down mastoidectomy. Otolaryngol Head Neck Surg.
121:18–22. 1999.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Weiss MH, Parisier SC, Han JC and
Edelstein DR: Surgery for recurrent and residual cholesteatoma.
Laryngoscope. 102:145–151. 1992.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Austin DF: Staging in cholesteatoma
surgery. J Laryngol Otol. 103:143–148. 1989.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Nyrop M and Bonding P: Extensive
cholesteatoma: Long-term results of three surgical techniques. J
Laryngol Otol. 111:521–526. 1997.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Portmann M, Crovetto MA, Valles J and
Aguayo F: Anatomical and functional results of the ‘small tympanic
cavity’ in total petromastoid excision for cholesteatoma. Rev
Laryngol Otol Rhinol (Bord). 108:161–164. 1987.PubMed/NCBI(In French).
|
|
27
|
Parisier SC, Hanson MB, Han JC, Cohen AJ
and Selkin BA: Pediatric cholesteatoma: An individualized,
single-stage approach. Otolaryngol Head Neck Surg. 115:107–114.
1996.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Pareschi R, Lepera D and Nucci R: Canal
wall down approach for tympano-mastoid cholesteatoma: Long-term
results and prognostic factors. Acta Otorhinolaryngol Ital.
39:122–129. 2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Vartiainen E: Ten-year results of canal
wall down mastoidectomy for acquired cholesteatoma. Auris Nasus
Larynx. 27:227–229. 2000.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Aslan Felek S, Islam A, Celik H, Demirci
M, Samim E and Kose SK: The functional and anatomical results of
the canal wall down tympanoplasty in extensive cholesteatoma. Acta
Otolaryngol. 129:1388–1394. 2009.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Göçmen H, Kiliç R, Ozdek A, Kizilkaya Z,
Safak MA and Samim E: Surgical treatment of cholesteatoma in
children. Int J Pediatr Otorhinolaryngol. 67:867–872.
2003.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Kim MB, Choi J, Lee JK, Park JY, Chu H,
Cho YS, Hong SH and Chung WH: Hearing outcomes according to the
types of mastoidectomy: A comparison between canal wall up and
canal wall down mastoidectomy. Clin Exp Otorhinolaryngol.
3:203–206. 2010.PubMed/NCBI View Article : Google Scholar
|