Introduction
Basal cell carcinoma (BCC) is the most frequent form
of skin cancer and it is characterized by slow progression and
eventually local destruction. Usually, BCC does not have a lethal
outcome, if associated with proper treatment (1). According to recent findings, the risk
of a fair-skin person developing at least one BCC is 30% (1). Moreover, an individual may have
multiple BCCs or a BCC associated with other sun-related skin
neoplasia, and some lesions may recur after treatment (2). Consequently, in countries with mostly
light-skinned individuals, the incidence of BCC is extremely high,
which leads to proportionately increasing burden on the medical
system, both economically and logistically, due to the need for
regular screening.
The diagnosis of BCC is based on clinical findings
and paraclinical investigations, mainly the pathological exam.
Dermoscopy increases the sensitivity to 91.2% and specificity to
95% of the diagnosis in BCC, due to specific dermatoscopic features
(1). Additional diagnostic elements
can be provided by confocal microscopy (3) and ultrasound examination (4).
Localization and tumor size are important risk
factors for recurrence (5). They
contribute to its characterization as high- vs. low-risk tumor. The
concept of the H zone (high risk for recurrence zone) comprises:
Nasolabial fold, nasal, orbital and auricular areas (5). Another factor that has been attributed
to higher recurrence rates is the presence of positive histological
margins, which is more common in the head area (6). Tumors that have even partially
aggressive histologic growth patterns such as micronodular,
infiltrative, and sclerodermiform are more likely to recur compared
to nodular of superficial subtypes (5). Basosquamous BCC is a special category
which has higher recurrence risk and metastasis rates, comparable
to squamous cell carcinoma, rather than with BCC (7).
The gold standard of treatment in BCC is surgical
excision with tumoral-free margins. This can be achieved by
classical surgery or by Mohs micrographic surgery (MMS). For
patients with locally advanced BCCs or with metastasis [which are
very uncommon: 0.0028-0.55% (1)]
that cannot be successfully treated using surgical methods,
radiotherapy or systemic medication are recommended: Hedgehog
inhibitors (vismodegib and sonidegib) (1).
Classical surgery consists of the removal of the
tumor and variable amount of the apparently healthy surrounding
tissue, with a recurrence rate of 2-8% at 5 years (8). Clinically free margins should be
selected as follows: i) for tumors with low risk of recurrence: 3-4
mm; ii) for high-risk tumors, when MMS is not available: 5-15 mm;
iii) in depth, the excision should reach the subcutaneous fat, or,
for cervicofacial area, the excision should be extended to the
muscular fascia, perichondrium or periosteum (1).
MMS is a more expensive and time-consuming surgical
technique. However, this technique allows for a more complete
analysis of the margins, and thus enables better preservation of
the surrounding healthy tissue. MMS is recommended for tumors of
the face especially in the H zone, recurrent tumors or tumors with
aggressive histological features. The reported recurrence rate is
3.9% after 10 years (9).
However, not all dermatologic services have access
to this performant treatment modality. Consequently, doctors may
use classical surgery even for tumors in high-risk areas or with an
aggressive phenotype.
The pathogenesis of BCC is incompletely elucidated.
Many molecules, growth factors and adhesion molecules are involved.
Disruptions of the Hedgehog pathway (Hh) are the most common
alterations in the development of BCC. The signature molecule of Hh
is glioma-associated oncogene homolog 1 (GLI1). The most studied
activation pathway of Hh is through the glycoprotein sonic Hh (SHH)
and this activation pathway has an important role in the
embryological development of various tissues and organs and in
maintaining cell polarity (10). It
was firstly isolated in a glioma, thus the name of
glioma-associated oncogene. Abnormal activation of SHH was reported
in different malignancies such as BCC, medulloblastoma, leukemia,
and carcinomas of the breast, lung, pancreas and prostate (10).
Yes-associated protein (YAP) is essential for the
stem cell population and for BCC proliferation. YAP is a
transcriptional factor of the Hippo signaling pathway, which
controls organ size and tumor inhibition (11). The activation of Hippo leads to the
phosphorylation of YAP and its retention in the cytoplasm. In the
absence of Hippo inhibition, YAP, together with the transcriptional
coactivator with PDZ-binding motif (TAZ) are translocated to the
nucleus where they induce the expression of genes responsible for
proliferation, cell growth, epithelial-mesenchymal transformation
and the inhibition of apoptosis (12).
YAP's interaction with the surrounding
microenvironment is through connective tissue growth factor (CTGF)
(13). CTGF, also known as CCN2, is
part of the CCN family of proteins. The main purpose of CTGF is to
promote cell adhesion through heparin and other integrins depending
on tissue (14). CTGF also has a
role in migration processes, cell proliferation, angiogenesis,
tissue repairing, fibrosis and others (15).
E-cadherin belongs to the cadherin group of
molecules responsible for calcium-dependent cell-to-cell adhesion.
The intercellular adhesions are mediated by the extracellular
domains of these cadherins, while their intracellular part is bound
to numerous adaptor or signaling proteins. YAP is regulated by the
surrounding factors through E-cadherin (16).
Patients with excised BCCs with positive
histological margins may subsequently undergo re-excision,
radiotherapy or adequate clinical assessment and in some cases an
ultrasound exam of the surgical scar. However, patients with
tumoral-free margins are probably less attentively followed up and,
in case of recurrence, may present locally advanced BCCs, which are
more difficult to treat. In addition, patients with a history of
BCC may develop a second BCC or multiple BCCs, some of which may be
less compliant to the use of photoprotection. Thus, the
identification of additional predictive markers for recurrence also
becomes an important concern in skin cancer prevention.
The aim of the present study was to assess the
clinical and histopathological characteristics of the tumors that
become recurrent after classical surgery with initially free
histologic margins. In addition, the expression of GLI1, YAP, CTGF
and E-cadherin was assessed as they have an impact in the
development of BCC and in the attempt to find histological markers
that may be useful for the identification of possible future
recurrences after an initial excision with tumoral-free
margins.
Patients and methods
Participants
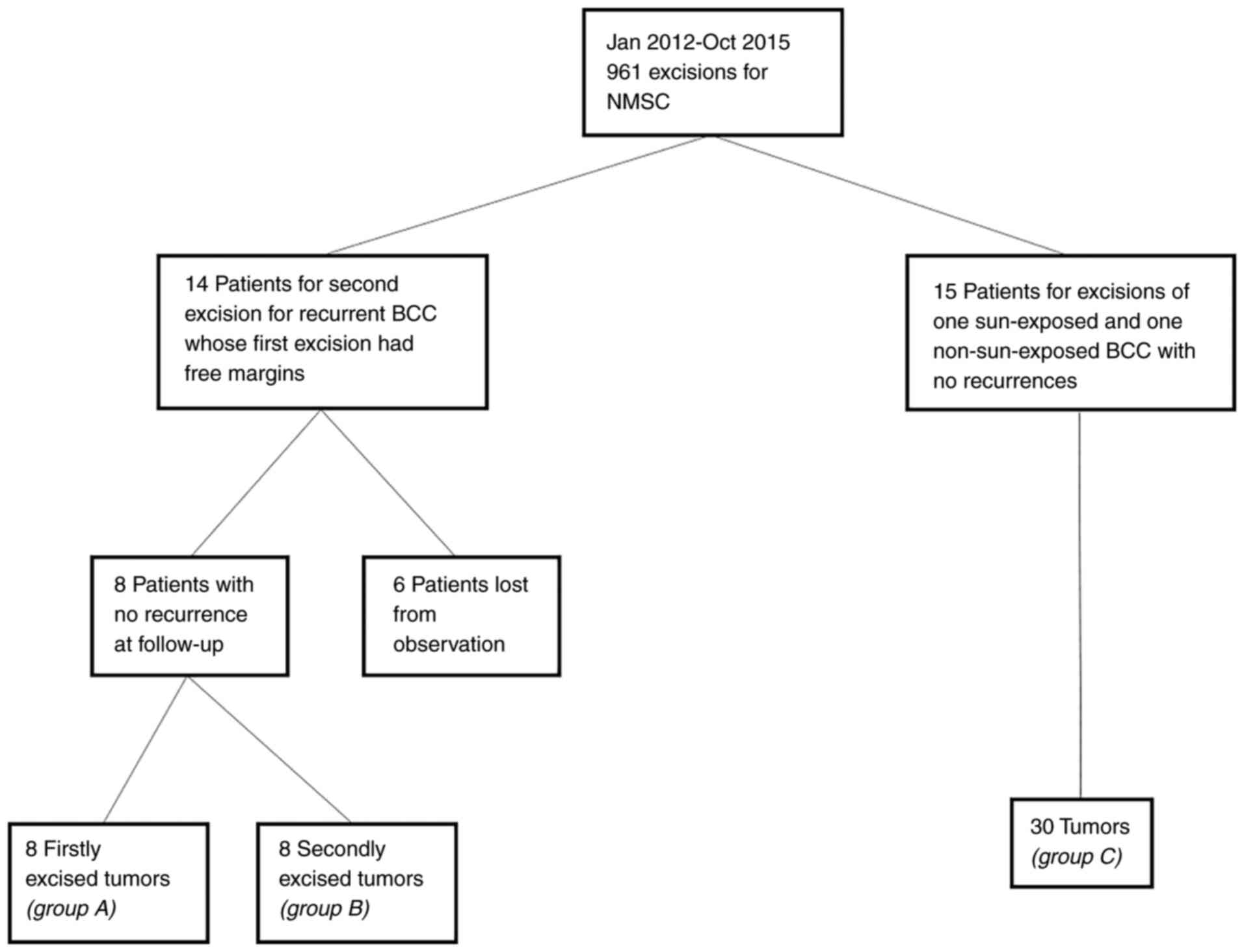
A retrospective observational study in the
Department of Dermatology, Emergency Hospital (Cluj-Napoca,
Romania) was performed. Ethics committee approval (under the number
155/07.04.2017) was obtained as well as informed consent from the
participants. The study included patients whose initial BCCs were
excised with free histological margins, who were readmitted and
underwent a second excision between January 2012 and October 2015
for a recurrence in the Department of Dermatology. The patients
were selected from the 961 admissions for non-melanoma skin cancer
(NMSC) excisions, according to a methodology described in a
previously published study (17)
(Fig. 1).
Inclusion and exclusion criteria
The inclusion criteria were: i) Patients who
underwent classical excision for the first recurrence of a
previously excised BCC; ii) patients whose initially excised tumor
had free histological margins. The exclusion criteria were: i)
patients with squamous cell carcinoma or benign tumors; ii)
patients with initial or recurrent tumor with at least one positive
histological margin; iii) patients with initial or recurrent tumor
of basosquamous subtype or with perineural invasion; iv) patients
treated by Mohs surgery; v) patients who presented re-recurrence
after the second excision; vi) patients who did not present for
follow-up between November 2017 and November 2018. A total of 14
patients met the inclusion criteria, while 6 patients were
excluded. From the remaining 8 patients the initial BCCs (group A:
Recurred tumors, case group) and the recurrent BCCs (group B:
Non-recurred tumors, part of the control group) were analyzed.
Additionally, the control group included tumors from
patients with multiple BCCs, with the following inclusion criteria:
i) patients who underwent surgery for both a tumor in a sun-exposed
area (nose, paranasal area, ear, preauricular area, the rest of the
face, neck, scalp, anterior and posterior thorax, superior limbs)
and a tumor in a non-sun-exposed area (retroauricular area,
inferior limbs, abdomen, lumbar zone, genitalia) concomitantly or
in consecutive steps; ii) patients who underwent both surgeries
between January 2012 and October 2015. The exclusion criteria were:
i) patients who presented recurrence at follow-ups; ii) patients
treated by Mohs surgery; iii) patients with tumors of basosquamous
subtype or with perineural invasion; iv) patients who had more than
two BCCs excised; v) patients who did not present for follow-up in
November 2017 to November 2018. From 961 admissions, 15 patients
with 30 tumors (group C) met the inclusion criteria.
Factors and classification
For the selected tumors, the following
characteristics were recorded: time passed from the initial
excision (years), time until recurrence appearance (years),
localization, dimension (cm), main morphology ranked according to
aggressiveness: infiltration (also including the micronodular
subtype), sclerodermiform, nodular, superficial, cystic.
Additionally, the Breslow index and Clark level were recorded, as
well as the extension of tumoral cells in lateral and deep margins
(mm).
Taking into consideration their location, tumors
were divided into one of three risk localization categories: i)
high risk: nose and paranasal (including the nasolabial fold),
auricular and periauricular; ii) medium risk: rest of the face,
neck, scalp; iii) low risk: trunk, limbs. Regarding the risk of
recurrence, the tumors were divided in 2 categories: i) high risk
(tumors with high risk localization, or medium risk localization
and dimension ≥1 cm, or low risk localization and dimension ≥2 cm,
or histologically diagnosed as infiltrative or sclerodermiform); or
ii) low risk: the other types of tumors.
Immunohistochemistry
For the immunohistochemical analysis, the selected
tumors were formalin-fixed, paraffin-embedded and 5-µm tissue
sections were used in the most representative areas, where the
malignant tumor was predominant. The sections were stained with
antibodies for E-cadherin (Clone EP700Y; Roche, Ventana; BenchMark
Ultra, CC1 standard, 16 min incubation with primary antibody,
OptiView amplification); anti-YAP (rabbit monoclonal EP1675Y'
Abcam, 1:200 dilution), GLI1 (rabbit polyclonal; Thermo Fischer
Scientific, Inc, 5 µg/ml), CTGF/CCN2 (rabbit polyclonal' Novus
Biologicals; 1:50 dilution) and the slides were analyzed under x100
and x400 magnification, using an Olympus microscope BX43.
Immunostaining was assessed by the same pathologist both as a
percentage (with an average of 5 HPF) and staining intensity (0,
none; 1, low; 2, medium; or 3, high).
Statistical analysis
Statistical analysis was performed using the
MedCalc® Statistical Software version 19.6 (MedCalc
Software Ltd., Ostend, Belgium; https://www.medcalc.org; 2020). Quantitative variables
were tested for normality of distribution using the Shapiro-Wilk
test and were expressed as median and 25-75 percentiles.
Qualitative variables were characterized by frequency and
percentage. Comparisons between groups were carried out using the
Mann-Whitney test or Chi-square test, whenever appropriate. The
area under the receiver operating characteristic (ROC) was used to
identify the ability of a quantitative variable to predict the
recurrence. P<0.05 was considered to indicate statistical
significance.
Results
In total, 8 recurrent tumors (group A) and 38
non-recurrent tumors (groups B and C) were clinically and
immunopathologically assessed. Due to the small number of patients
with recurrent tumors, the comparison between recurrent and
non-recurrent tumors harvested from the same patient was not
possible. None of the 23 patients had metastatic BCC.
Results of clinical and pathological
assessment
The tumors were situated predominantly in the head
and neck: 28 tumors (60.9%), compared with the trunk and abdomen:
17 tumors (36.9%) and only one (2.2%) tumor was located on the
extremities (P=0.45) (Table I). All
the recurrent tumors were located in the head and neck areas.
Regarding the categories of risk according to localization, 62.5%
of recurrences occurred in high-risk zones, 37.5% in medium-risk
zones, and none in low-risk zones. By contrast, non-recurrent
tumors were evenly distributed in the three categories: 9 (23.7%)
high risk, 11 (28.9%) medium risk, 18 (47.4%) low risk
(P=0.04).
 | Table IClinical and pathological features of
the assessed BCC tumors. |
Table I
Clinical and pathological features of
the assessed BCC tumors.
| | Non-recurrent
(n=38) | Recurrent
(n=8) | All tumors | P-value |
|---|
| Localization, n
(%) | | | | | | | | |
|
Nose | 0 (0) | 0 (0) | 0 (0) | Head and neck | 0.45 |
|
Paranasal | 2 (5.3) | 3 (37.5) | 5 (10.9) | 28 (60.9) | |
|
Retroauricular | 4 (10.5) | 0 (0) | 4 (8.7) | | |
|
Ear and
periauricular | 3 (7.9) | 2(25) | 5 (10.9) | | |
|
Rest of the
face | 5 (13.2) | 1 (12.5) | 6(13) | | |
|
Scalp | 5 (13.2) | 2(25) | 7 (15.2) | | |
|
Neck | 1 (2.7) | 0 (0) | 1 (2.2) | | |
|
Anterior
thorax | 4 (10.5) | 0 (0) | 4 (8.7) | Trunk 17
(36.9) | |
|
Posterior
thorax | 3 (7.9) | 0 (0) | 3 (6.5) | | |
|
Abdomen and
lumbar area | 10 (26.3) | 0 (0) | 10 (21.7) | | |
|
Superior
limbs | 0 (0) | 0 (0) | 0 (0) | Limbs 1 (2.2) | |
|
Inferior
limbs | 1 (2.7) | 0 (0) | 1 (2.2) | | |
|
High
risk | 9 (23.7) | 5 (62.5) | 14 (30.4) | | 0.04 |
|
Medium
risk | 11 (28.9) | 3 (37.5) | 14 (30.4) | | |
|
Low
risk | 18 (47.4) | 0 (0) | 18 (39.1) | | |
|
Size
(cm) | 0.9
(0.6-0.9)b | 1
(0.63-1.38)b | - | | 0.82 |
| High risk for
recurrence, n (%) | 20 (52.6) | 8(100) | 28 (60.9) | | 0.01a |
| Pathological
morphology |
|
Superficial | 3 (7.9) | 0 (0) | 3 (6.5) | | 0.08 |
|
Nodular | 31 (81.6) | 4(50) | 35 (76.1) | | |
|
Infiltrative | 2 (5.3) | 4(50) | 6(13) | | |
|
Sclerodermiform | 1 (2.6) | 0 (0) | 1 (2.2) | | |
|
Cystic | 1 (2.6) | 0 (0) | 1 (2.2) | | |
|
Pigmentation | 6 (15.8) | 0 (0) | 6(13) | | 0.57 |
|
Ulceration | 23 (60.5) | 6(75) | 29(63) | | 0.12 |
| Pathological
predictive factors | Non-recurrent
(n=38) | Recurrent
(n=8) | All tumors | P-value | Cut-off value | Se | Sp | P-value |
|
Breslow
index (mm) | 1.8
(1.0-2.5)b | 2.2
(2.1-2.3)b | - | 0.05 | >2 | 100% | 67.5% | 0.008a |
|
Clark
level | 4
(3-4)b | 4
(4-4)b | - | 0.02a | >3c | 100% | 47.5% |
<0.001a |
|
Lateral
margins (mm) | 1.09
(1.0-2.0)b | 0.95
(0.13-1)b | - | 0.05 | <1 | 87.5% | 60.0% | 0.04a |
|
Deep margin
(mm) | 1.85
(1.2-2.6)b | 0.8
(0.2-1.4)b | - | 0.009a | <1 | 75.0% | 82.5% |
<0.001a |
The macroscopic size of the tumors was similar in
both groups 1.0 cm (0.63-1.38) for recurrences and 0.9 cm (0.6-0.9)
for non-recurrent tumors (P=0.82).
Morphologically, recurrent tumors were 50% nodular
and 50% infiltrative. Non-recurrent tumors were: 31 nodular
(81.6%), 2 infiltrative (5.3%), 3 superficial (7.9%), 1
sclerodermiform (2.6%), and 1 cystic (2.6%) (P=0.08). Pigmentation
was found in 15.8% of non-recurrent tumors, while none of the
recurrent tumors showed pigmentation (P=0.57). Ulceration was found
in 6 (75%) recurrent tumors compared to 23 (60.5%) primary tumors
(P=0.12).
All recurrent tumors were in the category of high
risk for recurrence, whereas 20 non-recurrent tumors (52.6%) were
also in the high-risk category (P=0.01) (Table I).
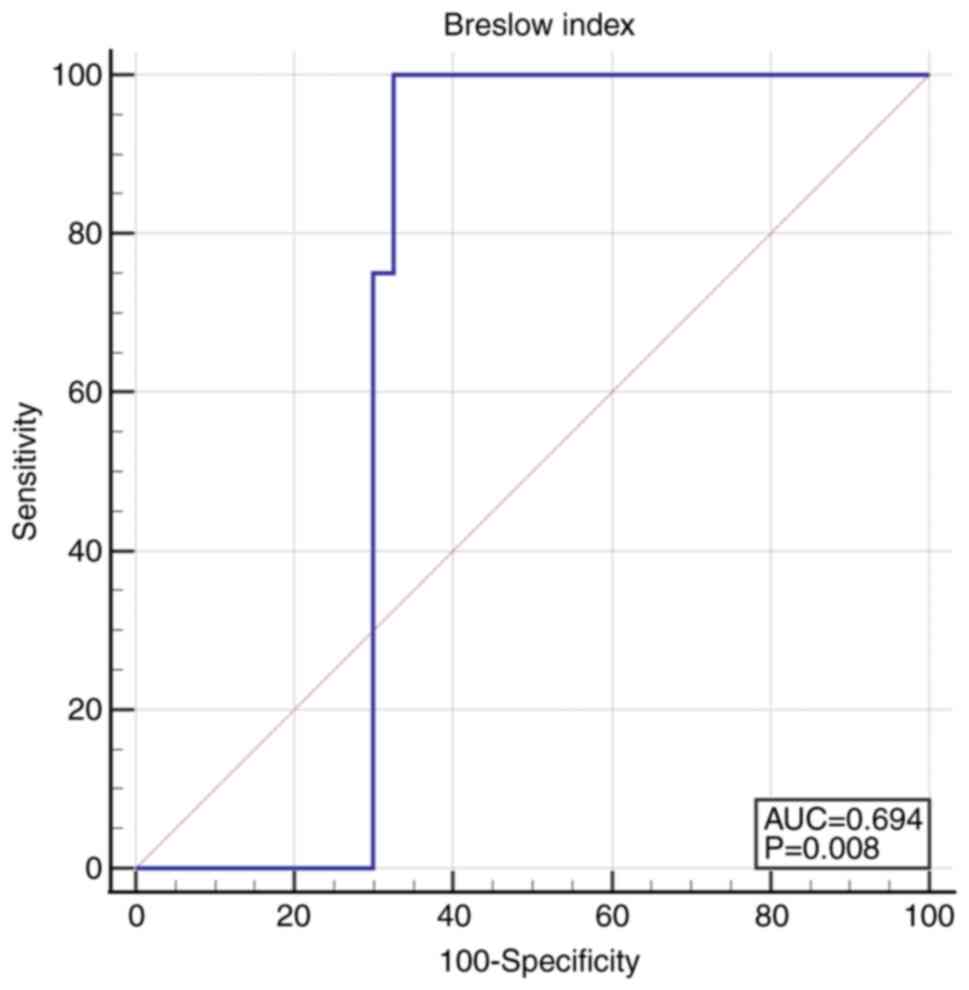
Breslow index was significantly lower in
non-recurrent tumors, 1.8 (1.0-2.5) compared to 2.2 (2.1-2.3) in
recurrent tumors (P=0.05). The cut-off value for recurrence of
Breslow index was higher than 2.0015: AUC 0.694 (95% CI
0.544-0.819), Se 100.0 (95% CI 63.1-100.0), Sp 67.5 (95% CI
50.9-81.4), P=0.008 (Fig. 2).
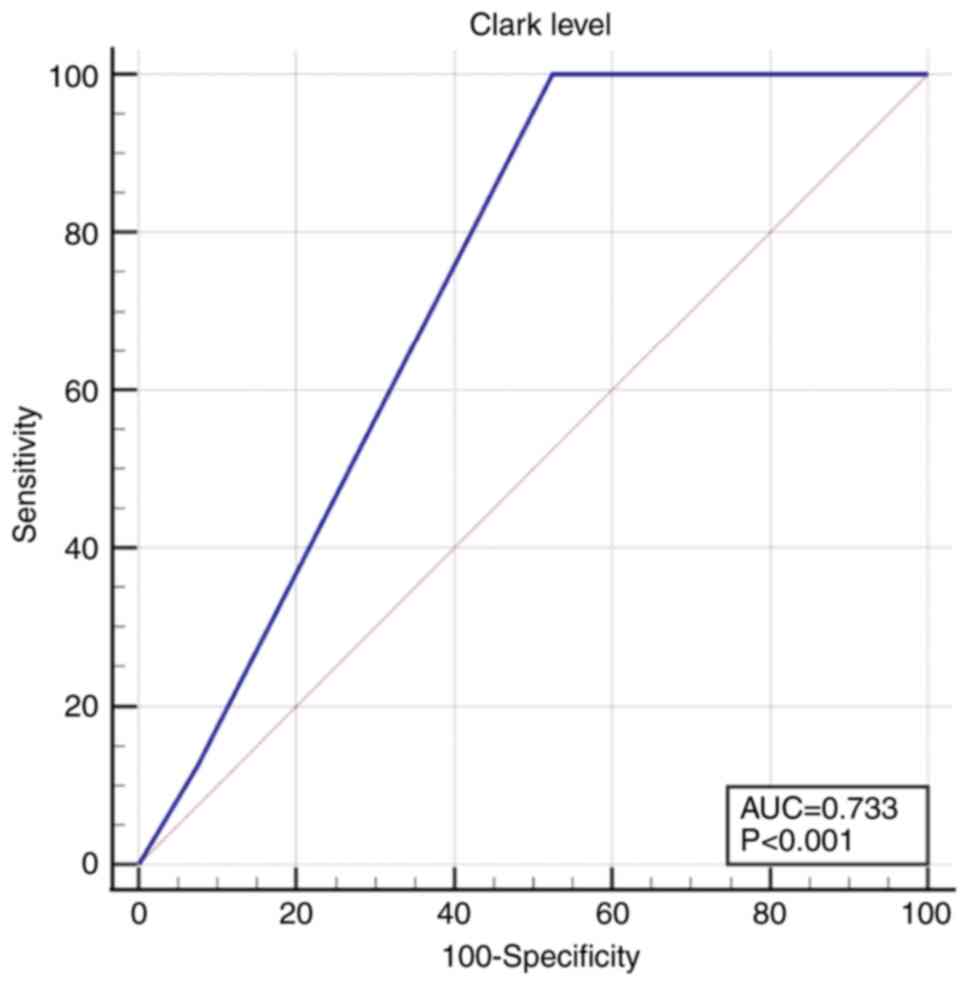
The Clark level was also significantly lower in
non-recurrent tumors 4 [3-4] compared to 4 [4-4] in recurrent
tumors (P=0.02). For the Clark level a cut-off value of 3 was
calculated, above which the risk of recurrence increased: AUC 0.733
(95% CI 0.585-0.850), Se 100.0 (95% CI 63.1-100.0), Sp 47.5 (95% CI
31.5-63.9), P<0.001 (Fig.
3).
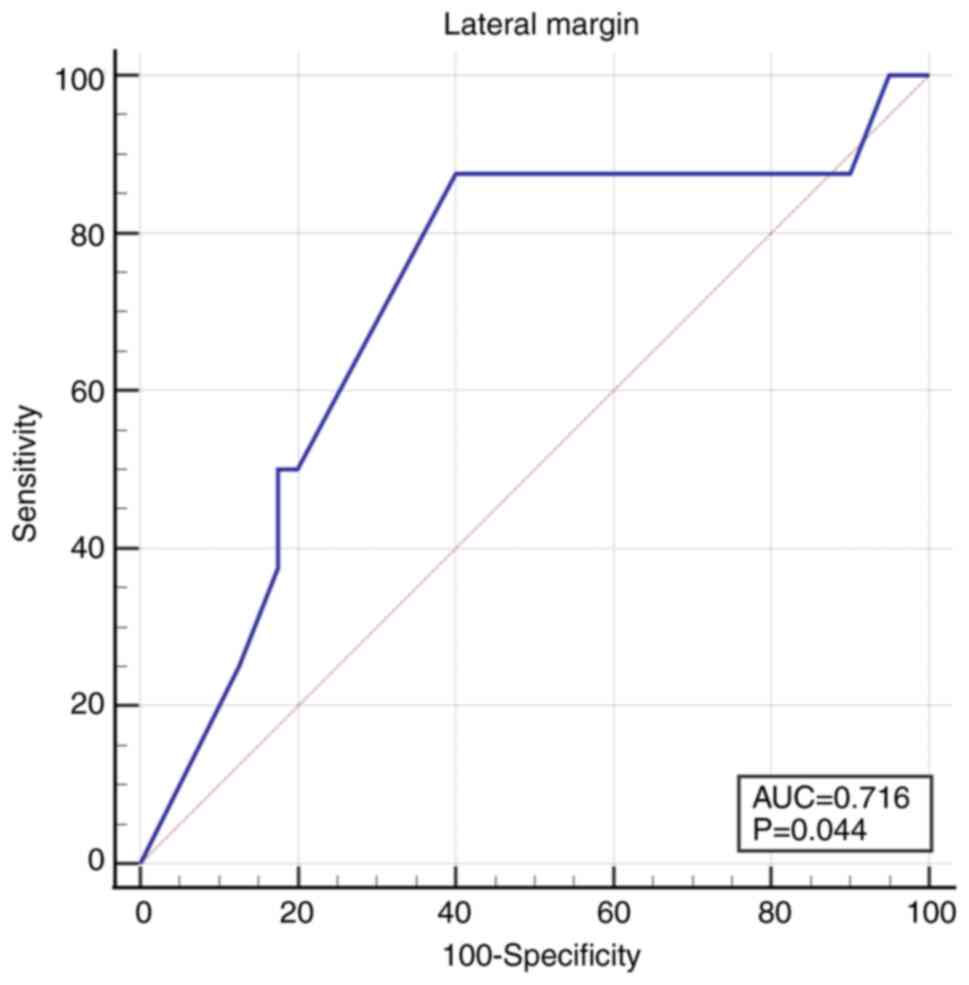
The lateral margins were more distant from the tumor
in non-recurrent tumors 1.09 mm (1.0-2.0) compared to recurrent
tumors 0.95 mm (0.13-1) (P=0.05). The cut-off value under which the
recurrence rate increased was 1 mm: AUC 0.716 (95% CI 0.567-0.836),
Se 87.5 (95% CI 47.3-99.7), Sp 60.0 (95% CI 43.3-75.1), P=0.04
(Fig. 4).
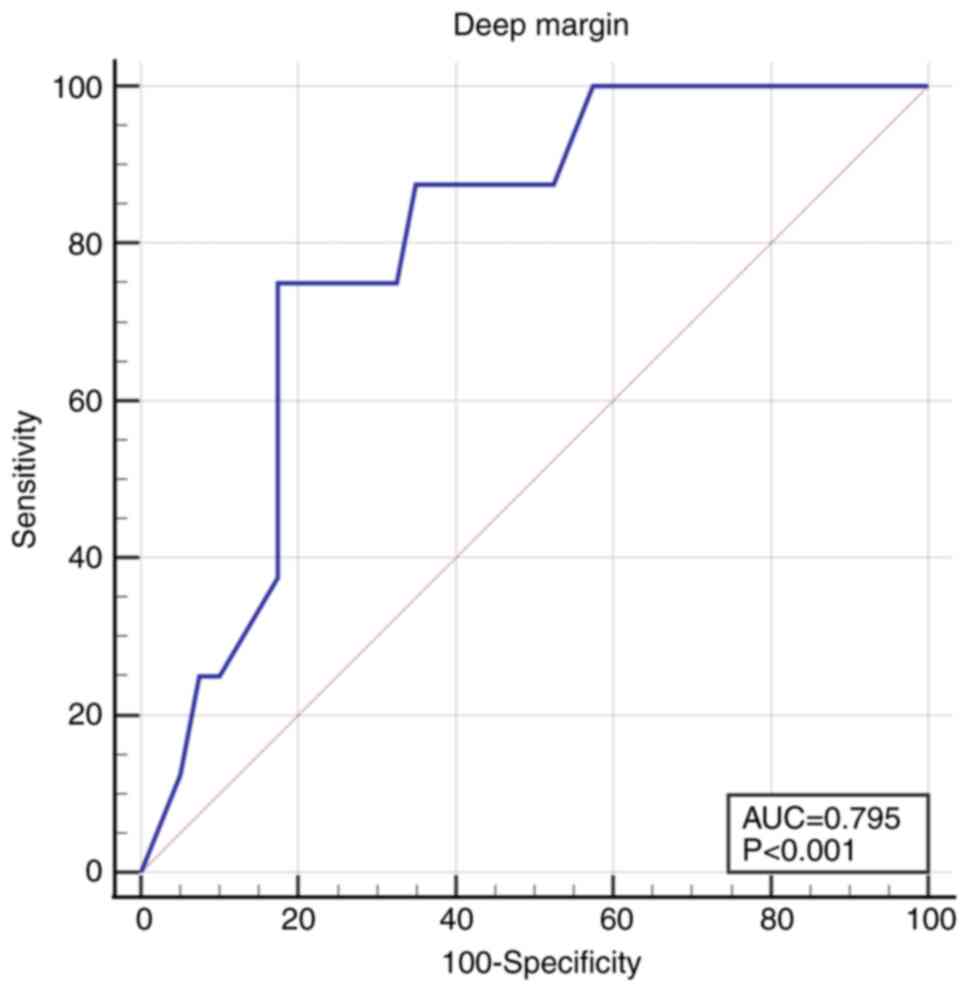
The deep margin was 2-fold deeper in non-recurrent
tumors, 1.85 mm (1.2-2.6) compared to 0.8 (0.2-1.4) in the
recurrent tumors (P=0.009). The cut-off value was 1 mm, under which
the recurrence rate increased: AUC 0.795 (95% CI 0.654-0.898), Se
75.0 (95% CI 34.9-96.8), Sp 82.5 (95% CI 67.2-92.7), P<0.001
(Fig. 5).
The median time from the primary tumor excision to
recurrence appearance was 2 years (1.0-4.0).
Results of the immunohistochemical
analysis
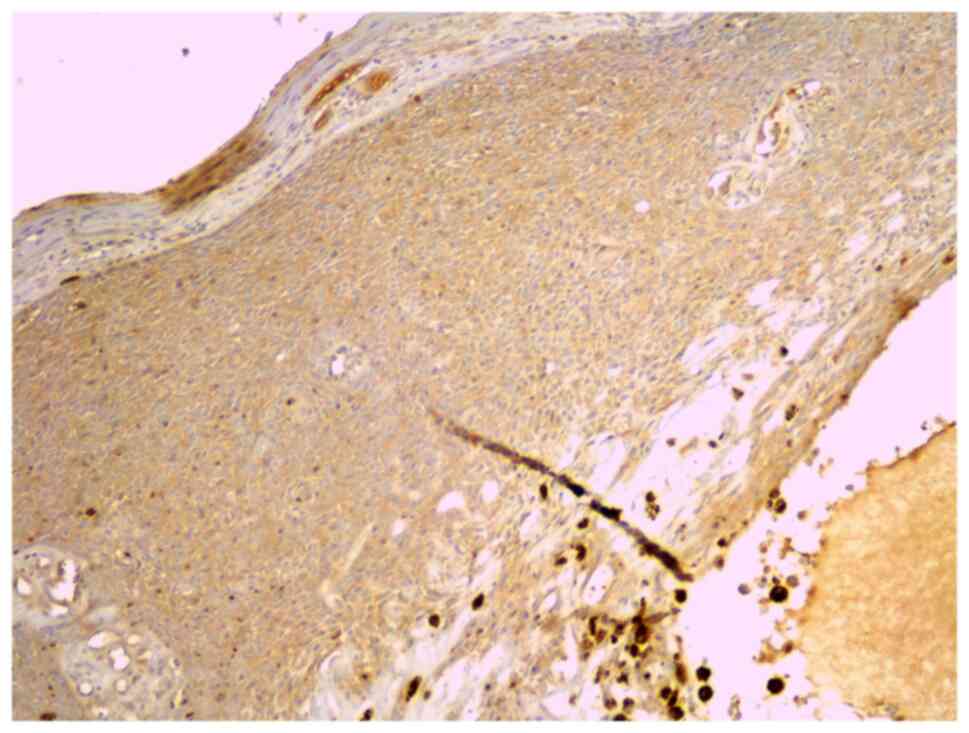
The immunostaining intensity for GLI1 (Fig. 6) was scored 0 in 21.7% of all
tumors, 1 in 58.7%, and 2 in 19.6% of tumors. None of the tumors
showed score 3. GLI1 expression had an intensity of 1 to 2 in 75%
of recurrent tumors and in 78.9% of non-recurrent tumors (P=0.89).
The percentage of positive cells was similar, with a median at 10%
in both recurrent and non-recurrent tumors (Table II) (P=0.84).
 | Table IIImmunohistochemical features of the
assessed tumors. |
Table II
Immunohistochemical features of the
assessed tumors.
| | Recurrent
tumors | Non-recurrent
tumors | |
|---|
| | Intensity | | Intensity | |
|---|
| | 0 | 1 | 2 | 3 | Median percentage
% | 0 | 1 | 2 | 3 | Median percentage
% | P-value for
intensity | P-value for
percentage |
|---|
| GLI1 | 2 (25%) | 5 (62.5%) | 1 (12.5%) | 0 (0%) | 10% (1.25-40) | 8 (21%) | 22 (57.9%) | 8 (21%) | 0 (0%) | 10% (2-30) | 0.89 | 0.84 |
| YAP | 0 (0%) | 0 (0%) | 3 (37.5%) | 5 (62.5%) | 80% (70-100) | 0 (0%) | 5 (13.2%) | 14 (36.8%) | 19 (50%) | 100% (80-100) | 0.55 | 0.31 |
| CTGF | 0 (0%) | 5 (62.5%) | 3 (37.5%) | 0 (0%) | 20%
(6.25-78.75) | 0 (0%) | 8 (21%) | 21 (55.3%) | 9 (23.7%) | 75% (30-90) | 0.05 | 0.09 |
| E-cadherin | 0 (0%) | 4 (50%) | 4 (50%) | 0 (0%) | 15% (10-28.75) | 1 (2.6%) | 13 (34.2%) | 18 (47.4%) | 6 (15.8%) | 20% (10-40) | 0.57 | 0.59 |
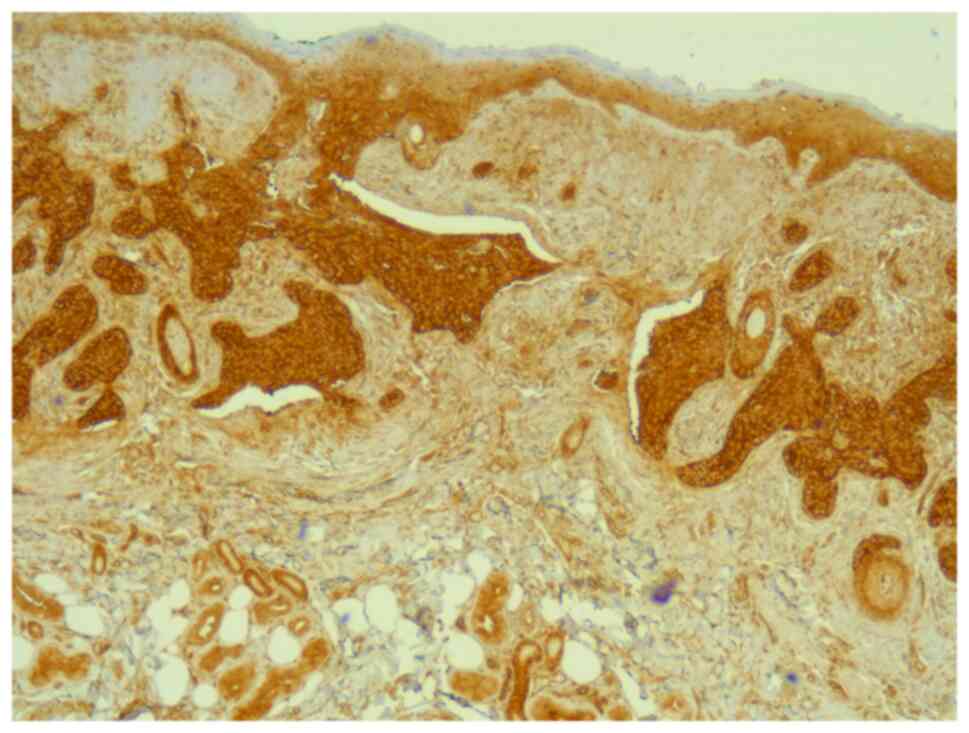
All tumors were immunopositive for YAP (Fig. 7). The immunostaining intensity for
YAP was 1 in 10.9% of all tumors and 2 to 3 in 89.1% of all tumors.
There was no difference between recurrent and non-recurrent tumors;
all recurrent tumors and 86.8% of the non-recurrent tumors had an
intensity of 2 to 3 (P=0.55). YAP was expressed in most cells, both
in recurrent and non-recurrent tumors, at a percentage of 80%
(70-100) and 100% (80-100) respectively, with no statistical
significance (Table II)
(P=0.31).
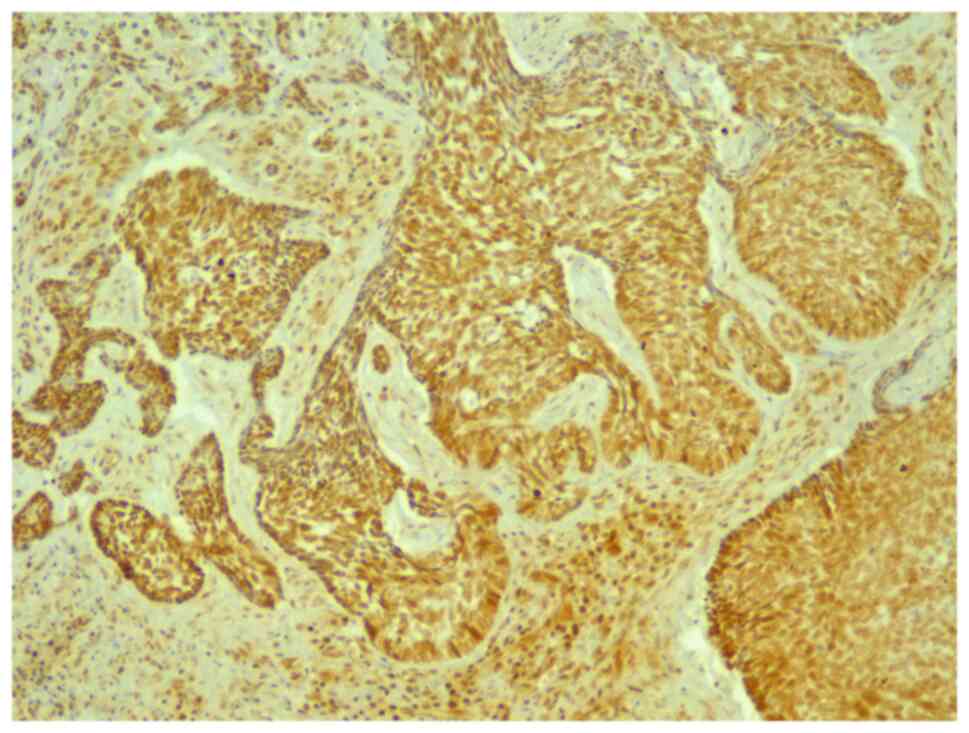
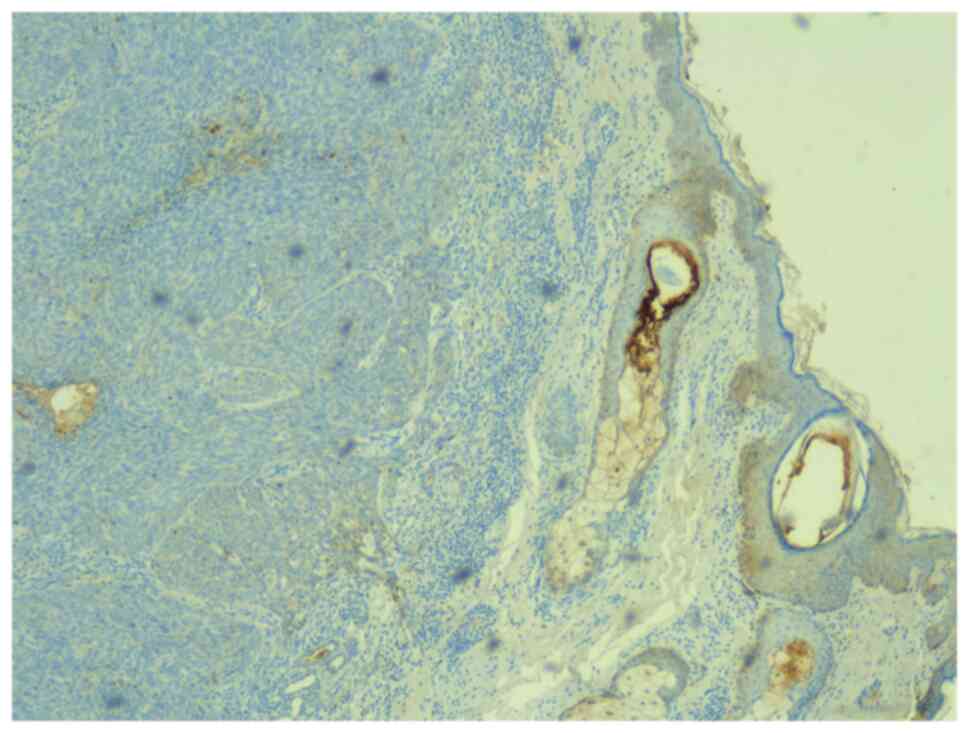
All tumors were immunopositive for CTGF (Fig. 8). The intensity score was 1 to 2 in
80.4% of all tumors and 3 in 19.6% of tumors. CTGF was less
expressed in recurrent tumors compared to the non-recurrent tumors.
The intensity score was 1 in 62.5% of recurrences vs. 21% of
non-recurrences, and score 2 in 37.5% of recurrences vs. 55.3% of
non-recurrences (P=0.05). Regarding the percentage of immunostained
cells, CTGF was expressed less in recurrent tumors, 20%
(6.25-78.75) compared to non-recurrent tumors, 75% (30-90)
(Table II) (P=0.09).
The staining intensity for E-cadherin (Fig. 9) was 0 in only one tumor (2.2%).
Scores 1 and 2 were found in 84.8% of tumors. A score of 3 was
found in 13% of all tumors. The intensity score 3 was found in
15.8% of the non-recurrent tumors, but in none of the recurrent
tumors (P=0.57). The percentage of E-cadherin-positive cells was
15% (10-28.75) in recurrent tumors and 20% (10-40) in non-recurrent
tumors (Table II) (P=0.59).
Discussion
BCC is a cutaneous tumor with slow progression and
complete cure when treated adequately. The gold standard of
treatment in BCC is surgical excision. For high-risk BCCs such as
those located in critical anatomical areas, recurrent BCCs, or
large tumors, MMS is recommended as it allows a much more precise
evaluation of resection margins (18).
The aim of the current study was to identify
clinical and pathological predictive factors for the risk of
recurrence of BCCs excised with negative histological margins
especially those located in high-risk areas, because these patients
might be less compliant to the long-term follow-up.
The results showed that, the pathological predictive
factors for the risk of recurrence were: Breslow index >2, Clark
level >3, and lateral or deep margins closer than 1 mm. Results
of the present study are supported by Girardi et al who
considered, in their study, that the positive margins or
submilimetrical negative margins were inadequate. They also showed
that the Clark level and the depth of invasion (Breslow index) were
independent risk factors for insufficiently safe margins. Thus, in
their study, tumors with inadequate margins had a Clark level of 4
to 5, and the median of Breslow index was at 2, similar to our
results (19).
The European guideline for BCC 2019 does not clearly
define the optimal histological margins and it uses terms such as
‘incompletely excised’ and ‘not optimal’ (1). Our results showed that lateral or deep
margins narrower than 1 mm increase the risk of recurrence of
excised BCCs. From our point of view, limited by the small number
of patients included in the study, it is deemed that free margins
of 1 mm or more would decrease this risk.
Most recurrences appear within the first 3 years
after the initial excision, most of them being located in the head
and neck area (20). This
observation supports the period of time chosen for follow up of the
patients at a minimum 3 years after the excision. All the recurrent
tumors in our study were located in the head and neck area as
expected, similar to the results reported by Bartoš et al
(20) and Saabye Bøgelund et
al (21). In the current case,
the median time of recurrence was 2 years; however, in some of the
studied cases tumors recurred even after more than 3 years. Thus,
patients diagnosed with a BCC, even though it was excised with
histologically free margins should be evaluated at least annually
for the remainder of patients' lives to diagnose other metachronous
malignant skin tumors that may occur and to advise on
photoprotection.
Other than clinical and histopathological parameters
observed in hematoxylin and eosin staining, we assessed the
influence of some molecules that are studied for their involvement
in the carcinogenesis of BCC but not yet related to their clinical
behavior. The aim was to evaluate their predictive value regarding
the risk of recurrence after surgical excision. There were no
statistically significant differences between tumors that recurred
and tumors that did not recur, but some important differences were
found for CTGF.
Few data exist in the literature regarding the role
of GLI1 in cutaneous carcinogenesis. Its implication in the
recurrence of BCC is not known. The development of BCCs and other
hair follicle-derived tumors (trichoepiteliomas, cylindromas,
trichoblastomas) was observed in transgenic mice with enhanced GLI1
expression in the basal layer of the epidermis and in the hair
follicle. This suggests that overexpression of GLI1 is sufficient
for tumor formation (22). The
current results showed that GLI1 had a low-to-medium expression
both in recurrent and non-recurrent tumors, which confirms the
abnormal activation of Hh in BCCs. With the limits of a pilot
study, with a reduced number of patients that does not permit
statistical significance, GLI1 may have a role in the recurrence of
tumors as indicated in studies on other types of cancer. The
expression of GLI1 in squamous carcinomas of the lung was
associated with lymphatic metastasis and poor prognosis (23). Additionally, inhibition of Hh
reduced tumor progression and recurrences in small cell lung cancer
(24).
The role of YAP in the pathogenesis of BCC remains
to be sufficiently elucidated. Previous findings showed that in
BCC, YAP is essential for tumor progression. In transgenic mice,
the deletion of YAP and TAZ resulted in the prevention of tumor
formation (25). Our results
indicated a medium-high expression of YAP, throughout the entire
tumor. The limited data of the present study support the essential
role of YAP for tumor progression. Additionally, overexpression of
YAP was correlated with poor prognosis in patients with
hepatocellular (26), mammary
(27) and prostatic carcinoma
(28).
In BCC, after YAP activation, the tumor stroma is
remodeled through CTGF (13). The
role of CTGF in carcinogenesis and oncogenic behavior is
controversial. The high expression of CTGF was associated with poor
prognosis in ovarian epithelial carcinoma (29). However, a low expression of CTGF was
associated with lymphatic metastasis, recurrences and low survival
rate in colorectal cancer (30). In
the present study, this marker had a low-medium overall expression
which may explain the low metastatic rate of BCC knowing the
dependence of tumoral cells to the surrounding stroma. In this
study, CTGF had a tendency to be lower both as intensity of
staining and percentage of positive cells in tumors that eventually
recurred compared to tumors that did not recur, without significant
differences.
The role of E-cadherin in BCC was more studied than
that of GLI1, YAP or CTGF. Some authors reported the decrease of
E-cadherin expression in morpheaform and recurrent BCCs compared to
nodular, cystic and superficial subtypes (31). In the present study, E-cadherin was
expressed at low-medium levels in most of the tumors. The lower
expression in recurrent tumors, even without statistical
significance is similar to previously published studies. Its low
expression is an indicative of aggressiveness in other epithelial
carcinomas. The expression of E-cadherin was decreased at the tumor
invasive front and also in recurrences and metastasis of oral
squamous cell carcinoma (32). A
meta-analysis reported that reduced or dysfunctional E-cadherin
expression was correlated with poor prognosis in head and neck
squamous cancers (33). Moreover,
in urothelial carcinoma, the low expression of E-cadherin was
related to a high risk of recurrences (34).
Although, in most cases, BCC is not an aggressive
tumor with a life-threatening potential it is important for it to
be diagnosed and treated appropriately. In Romania, the
addressability of the population to medical services for the
diagnosis and treatment of BCC is growing. This also increases the
number of surgical excisions, especially through classical surgery.
For tumors with high risk of recurrence, the patients are referred
to medical centers which have access to MMS. An attentive follow-up
after the excision, even if the resection margins are free form
tumoral cells, is important both for the patient and for the
physician. This underlines the need for tools as predictive factors
to estimate the risk of recurrence. If for a patient with positive
histological margins, the doctor's attention is obviously present,
patients with tumoral-free margins should not be forgotten. We
identified Breslow index over 2, Clark level over 3, lateral or
deep margins below 1 mm as predictive factors for BCC recurrence
and studied the immunostaining of GLI1, YAP, CTGF and E-cadherin as
they are regarded as being important in carcinogenesis.
The study's limitations include the low number of
cases analyzed because most recurrences appear in BCCs with
positive histological margins. Moreover, the number of cases was
limited due to patients who did not present for follow up, hence
the impossibility of assessing the postoperative scar. For this
reason, follow up visits are crucial both for the dermatologist and
patient.
In summary, in the context of increasing incidence
of BCC in the fair-skinned elderly population, it is important to
have tools as predictive factors for the behavior of the tumors.
Locally advanced tumors, with Clark level >3 and Breslow index
>2 have an increased risk to become recurrent. Additionally, the
risk of recurrence is increased in tumors with submilimetrical
histologic margins. Thus, re-excision of such tumors, especially if
they are in the high-risk category must be taken into
consideration. Follow-up should continue even after the 3 years
recommended in the current literature. In our opinion,
observational screening is important concerning both the
identification of recurrences and the diagnosis of other possible
skin neoplasia.
In the future, immunohistochemical analysis resulted
from molecules implicated in the development and progression of BCC
may be employed as a supplementary tool for evaluation of the
aggressiveness and the risk of recurrence. In the current pilot
study, GLI1, YAP and E-cadherin did not prove to be important in
predicting the recurrence of BCC. The low expression of CTGF
potentially indicates a tumor with higher aggressiveness.
Acknowledgements
Not applicable.
Funding
Funding: The study was partially supported by the project PCD
1300/72/13 January 2017 of ‘Iuliu Hațieganu’ University of Medicine
and Pharmacy Cluj-Napoca.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
CV, NIB, SCS and CMM contributed to the design of
work. CV, SCS, ABB, DNC, CSM and CMM were responsible for
literature search and manuscript preparation. CV, SCS, NIB, SCV,
AAB, DNC, CSM, OS and CMM contributed to design of study, data
collection, literature search, manuscript preparation, and critical
revision of manuscript for important intellectual content. CV and
SCS confirm the authenticity of all the raw data. All authors read
and approved the final version of manuscript.
Ethics approval and consent to
participate
Ethics committee approval was obtained from the
‘Iuliu Hatieganu’ University of Medicine and Pharmacy Cluj-Napoca
(approval no.: 155/07.04.2017). All the participants signed an
informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Peris K, Fargnoli MC, Garbe C, Kaufmann R,
Bastholt L, Seguin NB, Bataille V, Marmol V del, Dummer R, Harwood
CA, et al: Diagnosis and treatment of basal cell carcinoma:
European consensus-based interdisciplinary guidelines. Eur J
Cancer. 118:10–34. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Verkouteren JAC, Ramdas KHR, Wakkee M and
Nijsten T: Epidemiology of basal cell carcinoma: Scholarly review.
Br J Dermatol. 177:359–372. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Weedon D: Tumors of the epidermis. In:
Skin Pathology, 3rd edition. Elsevier, pp668-703, 2010.
|
|
4
|
Wortsman X: Sonography of facial cutaneous
basal cell carcinoma. J Ultrasound Med. 32:567–572. 2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
National Comprehensive Cancer Network
(NCCN): Basal Cell Skin Cancer (version 1.2020). Available from:
https://www.nccn.org/professionals/physician_gls/pdf/nmsc.pdf.
|
|
6
|
Lara F, Santamaría JR and Garbers LE:
Recurrence rate of basal cell carcinoma with positive
histopathological margins and related risk factors. An Bras
Dermatol. 92:58–62. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Lima NL, Verli FD, De Miranda JL and
Marinho SA: Basosquamous carcinoma: Histopathological features.
Indian J Dermatol. 57:382–383. 2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Trakatelli M, Morton C, Nagore E, Ulrich
C, Del Marmol V, Peris K and Basset-Seguin N: BCC subcommittee of
the Guidelines Committee of the European Dermatology Forum. Update
of the European guidelines for basal cell carcinoma management. Eur
J Dermatol. 24:312–329. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Van Loo E, Mosterd K, Krekels GA,
Roozeboom MH, Ostertag JU, Dirksen CD, Steijlen PM, Neumann HA,
Nelemans PJ and Kelleners-Smeets NW: Surgical excision versus Mohs'
micrographic surgery for basal cell carcinoma of the face: A
randomised clinical trial with 10 year follow-up. Eur J Cancer.
50:3011–3020. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mastrangelo E and Milani M: Role and
inhibition of GLI1 protein in cancer. Lung Cancer (Auckl). 9:35–43.
2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Pan D: The hippo signaling pathway in
development and cancer. Dev Cell. 19:491–505. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Szelachowska J, Donizy P,
Ratajczak-Wielgomas K, Halon A, Zielecka-Debska D, Lichon K,
Maciejczyk A, Lata-Wozniak E, Piotrowska A and Matkowski R: The
effect of YAP expression in tumor cells and tumor stroma on the
prognosis of patients with squamous cell carcinoma of the oral
cavity floor and oral surface of the tongue. Oncol Lett.
18:3561–3570. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Quan T, Xu Y, Qin Z, Robichaud P, Betcher
S, Calderone K, He T, Johnson TM, Voorhees JJ and Fisher GJ:
Elevated YAP and its downstream targets CCN1 and CCN2 in basal cell
carcinoma: Impact on keratinocyte proliferation and stromal cell
activation. Am J Pathol. 184:937–943. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Chu CY, Chang CC, Prakash E and Kuo ML:
Connective tissue growth factor (CTGF) and cancer progression. J
Biomed Sci. 15:675–685. 2008.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hall-Glenn F and Lyons KM: Roles for CCN2
in normal physiological processes. Cell Mol Life Sci. 68:3209–3217.
2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kim NG, Koh E, Chen X and Gumbiner BM:
E-cadherin mediates contact inhibition of proliferation through
Hippo signaling-pathway components. Proc Natl Acad Sci USA.
108:11930–5. 2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Vornicescu C, Șenila SC, Bejinariu NI,
Vesa SC, Boșca BA, Chirilă DN, Melincovici CS, Sorițău O and Mihu
CM: The role of GLI1, YAP, CTGF and E-cadherin in the pathogenesis
of basal cell carcinoma - our preliminary results. HVM Bioflux.
13:25–32. 2021.
|
|
18
|
Totonchy M and Leffell D: Emerging
concepts and recent advances in basal cell carcinoma.
F1000Research. 6(2085)2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Girardi FM, Wagner VP, Martins MD,
Abentroth AL and Hauth LA: Factors associated with incomplete
surgical margins in basal cell carcinoma of the head and neck. Braz
J Otorhinolaryngol: Apr 8, 2020 (Epub ahead of print). doi:
10.1016/j.bjorl.2020.02.007.
|
|
20
|
Bartoš V, Pokorný D, Zacharová O, Haluska
P, Doboszová J, Kullová M, Adamicová K, Péč M and Péč J: Recurrent
basal cell carcinoma: A clinicopathological study and evaluation of
histomorphological findings in primary and recurrent lesions. Acta
Dermatovenerol Alp Pannonica Adriat. 20:67–75. 2011.PubMed/NCBI
|
|
21
|
Saabye Bøgelund F, Ashlede Philipsen P and
Gniadecki R: Factors affecting the recurrence rate of basal cell
carcinoma. Acta Derm Venereol. 87:330–334. 2007.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Nilsson M: Induction of basal cell
carcinomas and trichoepitheliomas in mice overexpressing GLI-1.
Proc Natl Acad Sci USA. 97:3438–3443. 2000.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Cui Y, Cui CA, Yang ZT, Ni WD, Jin Y and
Xuan YH: Gli1 expression in cancer stem-like cells predicts poor
prognosis in patients with lung squamous cell carcinoma. Exp Mol
Pathol. 102:347–353. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Park KS, Martelotto LG, Peifer M, Sos ML,
Karnezis AN, Mahjoub MR, Bernard K, Conklin JF, Szczepny A, Yuan J,
et al: A crucial requirement for Hedgehog signaling in small cell
lung cancer. Nat Med. 17:1504–1508. 2011.PubMed/NCBI View
Article : Google Scholar
|
|
25
|
Debaugnies M, Sánchez-Danés A, Rorive S,
Raphaël M, Liagre M, Parent M-A, Brisebarre A, Salmon I and
Blanpain C: YAP and TAZ are essential for basal and squamous cell
carcinoma initiation. EMBO Rep. 19(e45809)2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Xu MZ, Yao TJ, Lee NP, Ng IO, Chan YT,
Zender L, Lowe SW, Poon RT and Luk JM: Yes-associated protein is an
independent prognostic marker in hepatocellular carcinoma. Cancer.
115:4576–4585. 2009.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Guo L, Chen Y, Luo J, Zheng J and Shao G:
YAP1 overexpression is associated with poor prognosis of breast
cancer patients and induces breast cancer cell growth by inhibiting
PTEN. FEBS Open Bio. 9:437–445. 2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Marx A, Schumann A, Höflmayer D, Bady E,
Hube-Magg C, Möller K, Tsourlakis MC, Steurer S, Büscheck F,
Eichenauer T, et al: Up regulation of the Hippo signalling effector
YAP1 is linked to early biochemical recurrence in prostate cancers.
Sci Rep. 10(8916)2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Shimbo A, Kajiyama H, Tamauchi S,
Yoshikawa N, Ikeda Y, Nishino K, Suzuki S, Niimi K, Sakata J and
Kikkawa F: Expression of connective tissue growth factor as a
prognostic indicator and its possible involvement in the aggressive
properties of epithelial ovarian carcinoma. Oncol Rep.
42:2323–2332. 2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Lin BR, Chang CC, Che TF, Chen ST, Chen
RJC, Yang CY, Jeng YM, Liang JT, Lee PH, Chang KJ, et al:
Connective tissue growth factor inhibits metastasis and acts as an
independent prognostic marker in colorectal cancer.
Gastroenterology. 128:9–23. 2005.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Vanjaka-Rogošić L, Puizina-Ivić N, Mirić
L, Rogošić V, Kuzmić-Prusac I, Babić MS, Vuković D and Mardešić S:
Matrix metalloproteinases and E-cadherin immunoreactivity in
different basal cell carcinoma histological types. Acta Histochem.
116:688–693. 2014.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Bánkfalvi A, Kraßort M, Buchwalow IB, Végh
A, Felszeghy E and Piffkó J: Gains and losses of adhesion molecules
(CD44, E-cadherin, and β-catenin) during oral carcinogenesis and
tumour progression. J Pathol. 198:343–351. 2002.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Yazdani J, Ghavimi MA, Jabbari Hagh E and
Ahmadpour F: The role of E-cadherin as a prognostic biomarker in
head and neck squamous carcinoma: A systematic review and
meta-analysis. Mol Diagnosis Ther. 22:523–535. 2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Balci MG and Tayfur M: Loss of E-cadherin
expression in recurrent non-invasive urothelial carcinoma of the
bladder. Int J Clin Exp Pathol. 11:4163–4168. 2018.PubMed/NCBI
|