Introduction
Optical coherence tomography (OCT) can be defined as
a modern imaging investigation technique. This technique is
effective in visualizing the differences in the optical properties
of tissues. OCT has both optical absorption and optical reflection
properties (1).
OCT was introduced into the medical field >20
years ago and was initially used for structural and functional
investigations of the eye by ophthalmologists (2-4).
The use of OCT technologies has increased in recent years in
various medical domains, such as gastroenterology, dermatology and
neurology (5-12).
Recently, OCT has been used in dental medicine and particularly in
orthodontics. There are a multitude of uses for OCT in the field of
dentistry, such as for the anatomical examination of dental and
periodontal structures, for the qualitative and quantitative
evaluation of the resins used in the bonding procedure, for the
examination of the biofilm formed around the brackets, and for the
evaluation of periodontal ligament responses to various orthodontic
forces generated during treatment (13-16).
The most crucial advancements in orthodontics were
made with the introduction of acid etching, followed by the direct
bonding of the brackets on the enamel surface, using an epoxy
resin. This technique was described by Newman in 1965(17). Currently, the adhesive systems used
in orthodontics are based on Bowen's bisphenol A-glycidyl
methacrylate (Bis-GMA) resin. This resin is available in a wide
variety of viscosities for easy penetration into the etched enamel
surfaces (18).
At the end of the orthodontic treatment period with
fixed appliances, a crucial step is the bracket debonding
procedure. During this step, particular attention should be paid to
the removal of all adhesive resin from the enamel surface. The
orthodontist should also aim to restore the tooth surface to its
pre-treatment condition as much as possible.
Bracket debonding is one of several causes of
iatrogenic damage to enamel. The evaluations of this procedure are
commonly performed using an optical microscope; however, this
method ensures that only the enamel surface is analyzed. OCT is a
high-resolution optical technique that allows the minimally
invasive visualization of near-surface alterations in complex
tissues. The applications of OCT in dental medicine are related to
both hard and soft tissue analysis.
Based on low coherence interferometry using
broadband light, the OCT investigation can provide real-time
structural images of the enamel and of the soft parts. Currently,
this imaging technique can be used to detect the morphological
changes of oral tissues in vivo. It is also applicable in
the diagnosis of early tooth lesions, in assessing the progression
of periodontal disease and in detecting oral cancer (19,20).
Materials and methods
The present study was approved by the Ethics
Committee of the University of Medicine and Pharmacy of Craiova,
Romania (approval reference no. 72/07.09.2020), in accordance with
the ethical guidelines for research with human participants of the
University of Medicine and Pharmacy of Craiova, Romania. Written
informed consent was obtained from all subjects involved in the
study. The present study was performed on a total of 20 permanent
teeth extracted at the Oral and Maxillofacial Surgery Clinic of the
Clinical Emergency County Hospital of Craiova, Romania. These teeth
did not exhibit carious lesions, attrition/abrasion, cracks, or
staining (when examined visually and using OCT).
The extracted teeth used in the present study were
rinsed with water and then disinfected with 10%
H2O2 for 10 min. Following the disinfection
process, each tooth sample was scaled and polished to remove
gingival tissue. To avoid desiccation, the samples were maintained
in deionized water until the brackets were bonded. The present
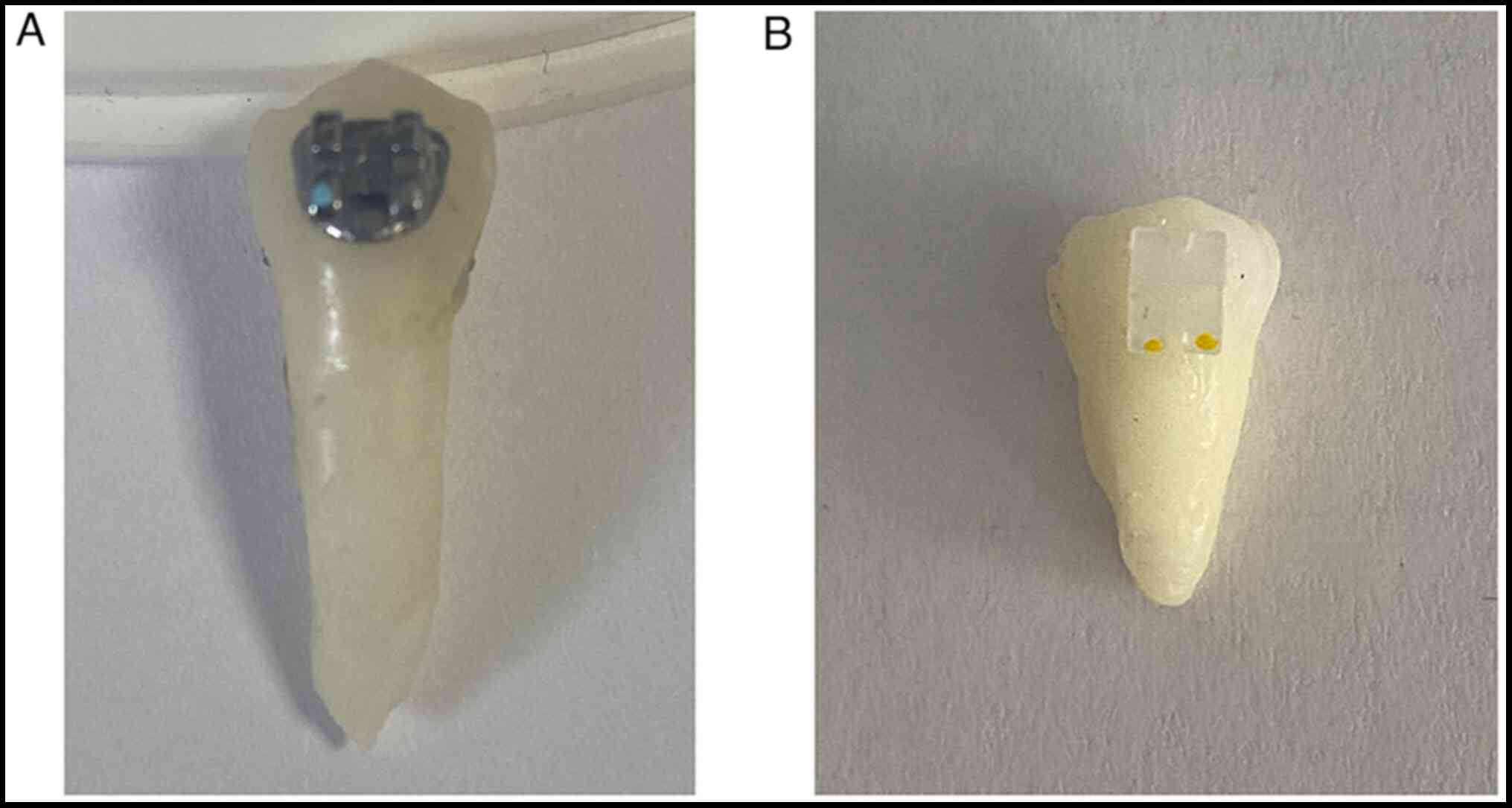
study used metallic brackets/Legend medium (GC Orthodontics, Inc.)
and ceramic brackets/Ceramic-1 (Changsha Denxy Technology Co.,
Ltd.), all with a similar mesh. The teeth were randomly divided
into four groups (n=5 per group) depending on the type of bonded
bracket and the pliers used for debonding.
Prior to the bonding procedure, the samples were
removed from the solution and dried using paper towels. The buccal
surface of each tooth was examined using the OCT system
manufactured by Thorlabs (OCS1300SS), powered by a swept laser
source with a central wavelength of 1,310 nm, a spectral bandwidth
of 100 nm and an average power of 12 mW. The device was used for 2D
and 3D scans, thus ruling out the possibility of tooth samples with
enamel damage.
The enamel surfaces were etched with
Trulock™ Etchant Gel (Rocky Mountain Orthodontics)
containing 37% phosphoric acid for 20 sec, and then rinsed with
water for 10 sec and air-dried. The bonding procedure was performed
using Trulock Light Activated Adhesive (Rocky Mountain
Orthodontics), following the manufacturer's instructions. The
adhesive was light-cured for 20 sec from the incisal/occlusal and
cervical sides of the bracket using a 3M™
Elipar™ DeepCure-L LED Curing Light (1,470
mW/cm2; 3M Science) (Fig.
1).
Following the bonding procedure, the tooth samples
were stored in deionized water for 24 h. The debonding procedure
was performed 24 h after bonding using two different pliers: A side
cutter (model T00552, Rocky Mountain Orthodontics) and anterior
bracket removal pliers (model 678-219, Hu-Friedy Mfg. Co., LLC).
All these procedures were performed by the same operator. Although
there are various methods regarding the use of these pliers, the
debonding phase was performed following a standardized
technique.
The side cutter was positioned diagonally at the
bracket base and at the incisal/occlusal and cervical level. The
bracket was removed by gently squeezing the pliers and performing
an additional clockwise rotational movement. The anterior bracket
removal pliers were applied by gripping under the bracket wings at
the bracket-enamel interface. By squeezing and tilting the pliers
downward, a rotational axis was generated at the lower edge of the
bracket, thus detaching it from the enamel surface.
Following the debonding procedure, the teeth were
fixed in dental silicone (Optosil Comfort Putty, Kulzer GmbH) and
positioned for examination using a stereomicroscope manufactured by
Nikon (SMZ745T), equipped with NIS-A AMEAS and NIS-A EDF software
(version 4.50) for image and data acquisition and processing.
Subsequently, the samples were also fixed in dental
silicone and positioned so that the OCT light beam could fall
perpendicularly on the debonded surfaces. Thus, the samples were
re-examined using the OCT system, and 2D and 3D images of the
surfaces involved were obtained.
The present study used a design that allowed the
visualization of the tooth surface at different angles in order to
detect enamel cracks, the amount of adhesive remaining and bracket
fragments resulting from the debonding procedure. At the same time,
healthy teeth surfaces were included as controls for the
experiment. Tooth surfaces imaged using the OCT system at widths of
10 mm with a distance of 10 mm and a depth of 3 mm were sampled.
The obtained images were processed using ImageJ software (version
1.8.0, National Institutes of Health), which is an open access
program.
Results
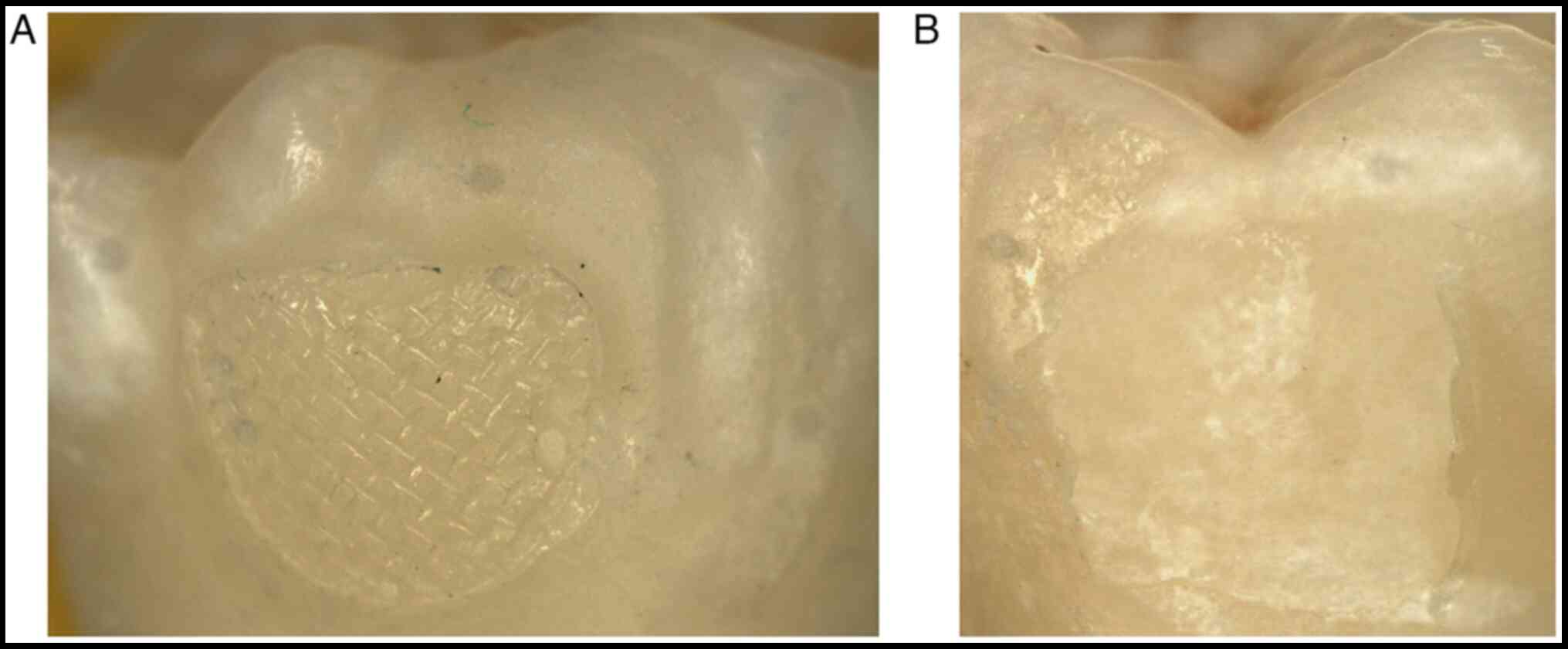
Following the OCT examination, 512 images were
obtained for each tooth surface subjected to the debonding
procedure. From these, the most representative images were
selected, both for the teeth bonded with metallic brackets and for
those bonded with ceramic brackets. Those images in which the OCT
image was well outlined to be relevant were considered, given that
the OCT beam did not always fall perpendicular due to the
convexities of the dental surfaces (Fig. 2).
As illustrated in Fig.
2A, the impression left by the sole of the metallic bracket on
the surface of the adhesive and small areas where the adhesive came
off with the bracket were noted. It was also noted that the
adhesive came off almost completely with the ceramic bracket and
some adhesive fragments were observed in the areas corresponding to
the periphery of the bracket (Fig.
2B).
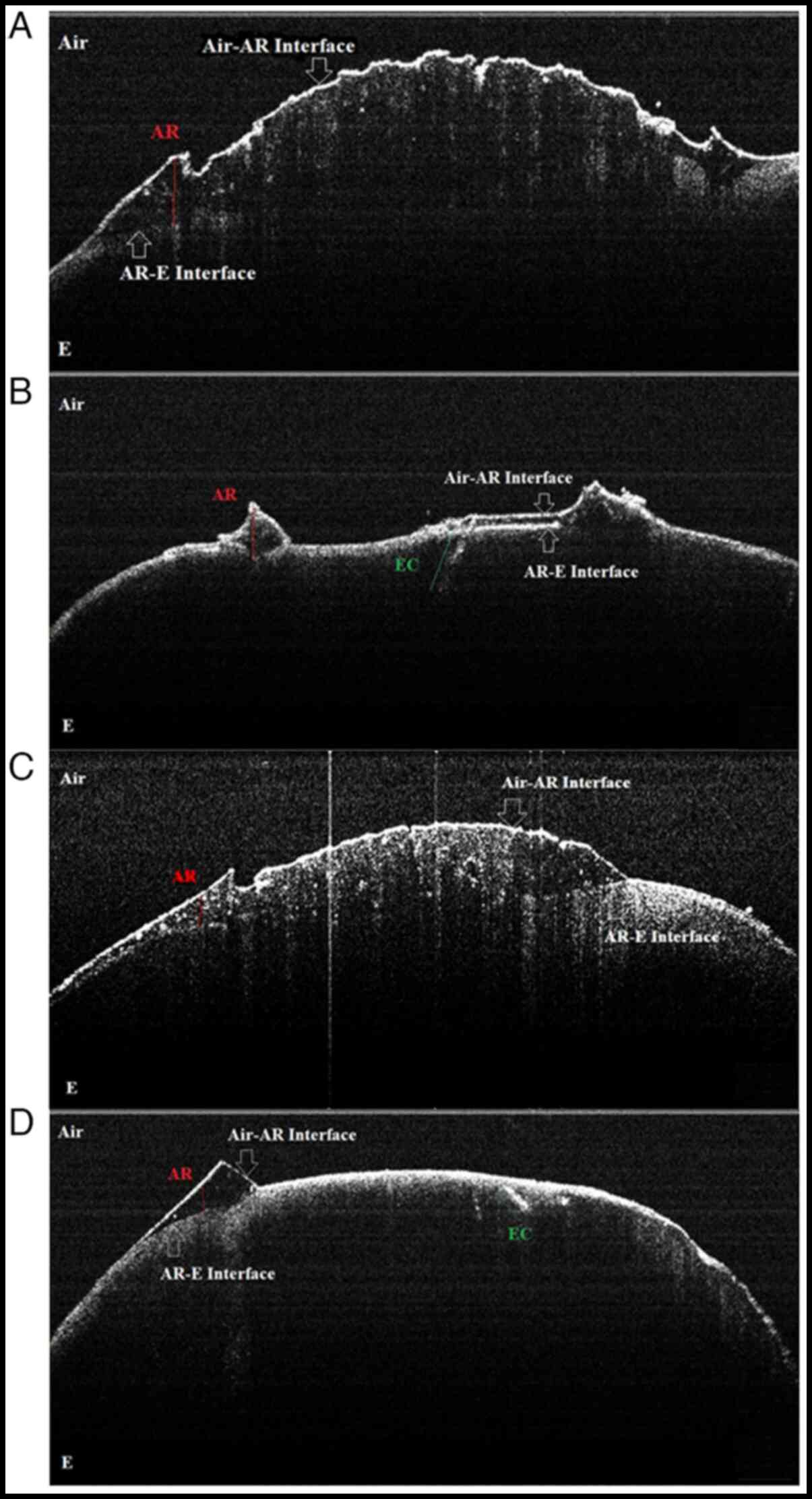
Following the processing of all the data obtained in
the study, it was noted that the metallic brackets generated a
larger amount of remaining adhesive on the enamel surfaces compared
with that on the ceramic surfaces (Fig.
3). It was observed that cracks appeared only at the tooth
surfaces bonded with ceramic brackets and that the type of pliers
used for debonding did not influence the incidence and extent of
enamel damage. In addition, the OCT images assisted in the
evaluation of the size and orientation of the enamel cracks.
As shown in Fig. 3A
and C, it was observed that a large
amount of the adhesive used for the bonding procedure remained on
the enamel surface after bracket debonding. Although the sole of
the metallic brackets has a mesh in order to increase mechanical
retention, the adhesive adhered more effectively to the enamel
surface. In the OCT images, the irregular surface of the adhesive
which remained after bracket debonding was observed. The debonding
of metallic brackets from dental surfaces does not cause cracks;
however, it generates larger amounts of adhesive remnant. This
increases the risk of damage to the enamel during conventional
adhesive removal techniques with tungsten carbide burs.
As shown in Fig. 3B
and D, cracks on the enamel surface
and small amounts of adhesive remnants were noted. The aspects that
were observed following the debonding technique highlighted the
strong adhering ability of the adhesive to the dental surfaces. As
regards the ceramic brackets, the adhesive adhered more effectively
to the mesh from their soles as compared to that of the metallic
ones. The debonding procedure generated marked detachment forces,
causing enamel cracks.
Following the debonding procedure, only fragments of
ceramic brackets remained on the enamel surface. It was found that
the side cutter generated fractures of the ceramic brackets more
frequently than the anterior bracket removal pliers. Both pliers
used in the present experiment generated variable amounts of
remaining adhesive on the enamel surface.
Discussion
OCT is a tomographic imaging procedure capable of
reproducing high-resolution sectional images of the internal
architecture of materials and tissues (1-2 mm depth). With the aid
of the OCT technique, images of both normal and pathological hard
dental structures can be examined, and the quality of various types
of dental treatments can be investigated (21,22).
This imaging technique has an increased sensitivity compared with
other investigative methods used for this purpose (23).
The majority of studies on the changes of hard
dental tissues associated with fixed orthodontic therapy have been
performed in vitro on teeth extracted from bovines or humans
using scanning electron microscopy, surface profilometry and laser
fluorescence (24-27).
These studies prompted the authors to conduct an in vitro
study on the structural changes caused by the bracket debonding
procedure. However, studies conducted using OCT technology are
limited. The resolutions (for air) of the OCT system used in the
present study were 12 µm for axial and 15 µm for lateral
resolutions. The system allowed for the analysis of a sample of
10x10x3 mm (length, width and depth, respectively) or
1,024x1,024x512 pixels in approximately 30 sec, using a
charge-coupled device-type detector (28,29).
As regards the etching of the dental surfaces in
order to bond the brackets, the present study used Trulock Etchant
Gel, which is effective on both dentin and enamel. This adhesive
system is mainly recommended to patients with poor oral hygiene
and, implicitly, with enamel demineralization. Over time, these
patients have posed real challenges for orthodontists, as the
quality of bracket adhesion on such enamel is poor (30). The viscosity of the gel prevents it
from leaking from tooth surfaces and can also be easily removed
without leaving residue.
For the bonding procedure, Trulock Light Activated
Adhesive was selected, as it is single-paste resin-based, thus
avoiding the deficiencies caused by conventional two-component
systems. The one-component adhesive reduces the risk of accidental
bracket debonding and significantly reduces the working time. This
adhesive system contains fluoride, which reduces the risk of
demineralization and even carious processes around the brackets.
These are used in patients with poor oral hygiene, with the fixed
orthodontic appliances promoting plaque retention (31).
The integration of fluoride in the adhesive systems
for bracket bonding has proven to be an extremely useful measure in
preventing dental demineralization following fixed orthodontic
treatment (32). The Trulock Light
Activated Adhesive is designed to bond metallic, ceramic and
plastic brackets. The etching technique (followed by the
infiltration of the adhesive resin into the surface layer of the
enamel during the bonding procedure) renders it impossible to
restore the initial status of the enamel following the completion
of orthodontic treatment (33).
Thus, bracket debonding is an orthodontic procedure
with an increased risk of damage to the enamel in the form of
scratches, cracks or tissue loss. To protect this structure,
orthodontists need to use procedures that prevent failures at the
enamel-adhesive interface, leaving as much adhesive on the tooth
surface as possible. It has been demonstrated that maintaining the
structural integrity of the enamel is dependent on the presence of
large amounts of remaining adhesive. Modern adhesive technologies
seem to be a favorable solution that facilitates orthodontic
treatment and yields promising results (34).
The present study used two types of orthodontic
pliers: A side cutter and an anterior bracket removal pliers. Both
pliers are made of high-quality stainless steel. The side cutter is
used for both cutting orthodontic wires and for removing brackets.
The anterior bracket removal pliers have a single use, to remove
brackets from the anterior zone. These pliers were selected for a
variety of reasons: The materials they are composed of, the joint
and handle construction and the design of the active parts. The
handles are designed to allow an optimal grip. The two arms are
joined by a sliding joint, resistant to corrosion, which allows the
two active parts to create a perfect alignment. The active parts
are narrow and composed of tungsten carbide to facilitate their
insertion at the junction between the tooth and the bracket sole.
Tungsten carbide is approximately twice as stiff as steel. This
property is an important feature of the active parts. These
qualities ensure the longevity of the pliers and facilitate the
process of bracket debonding. Given that the side cutter is often
used to cut orthodontic wires, its active parts are sharpened from
those of the anterior bracket removal. For this reason, when using
the side cutter for the debonding procedure, the risk of fracturing
the ceramic brackets is higher (35). Beginning from this premise, it was
decided that the bracket debonding procedure would be performed
using a standardized technique in the present study (36). Enamel cracks are difficult to
visualize and are often overlooked. They can subsequently lead to
the appearance of dental hypersensitivity and pain when chewing,
symptoms that dissipate when the stimulus is removed (37,38).
The demineralization of the adjacent enamel caused by fixed
appliances is an undesirable complication of orthodontic treatment,
particularly if it is not detected at an early stage and no
remedial action is taken (39).
Previous studies based on OCT imaging have analyzed
and compared the quality of the bonding procedure of ceramic and
polymeric brackets. The aim of these studies was to evaluate the
adhesive film between the bracket sole and the dental surface.
Unlike the present study, the OCT analysis of the samples was
performed following the bonding technique, observing the defects in
the adhesive structure. It was concluded that these gaps may also
be the consequence of a human error during the bonding procedure.
On the other hand, additional research is required to demonstrate
the effectiveness of the indirect bonding technique compared with
the direct one (40,41).
Another study performing the OCT analysis of the
tooth surfaces following bracket debonding concluded that the
removal of adhesive remnant increased the roughness of the enamel
in accordance with the technique used in this operation. Thus,
tungsten carbide burs generated the roughest surfaces, while the
use of Adhesive Residue Remover led to the smoothest surfaces
(42). It was further demonstrated
that the type of tooth on which the bracket is bonded plays an
important role (43). Similar to
the present study, these studies indicate the importance of OCT in
the field of fixed orthodontics (42,43).
A previous clinical study demonstrated that both
metallic and ceramic brackets have a similar failure rate (44). Although in vitro studies have
indicated that enamel cracks are potential gateways for
microorganisms, an infection of the endodontic system is unlikely
to occur if the dental pulp is healthy. The risk of pulp necrosis
generated by enamel cracks is 3.5% (45). Previous clinical studies have
demonstrated that if a tooth with enamel cracks and reversible
pulpitis is diagnosed at an early stage, it can be recovered by
applying a micro-prosthesis, with endodontic treatment being
necessary in only 20% of these cases in 6 months (46,47).
This finding indicates the importance of the early identification
of enamel cracks with the aid of OCT technology, which would
facilitate the diagnosis and early treatment of dental
hypersensitivity in current practice.
Studies have determined that maintaining the
structural integrity of the enamel is closely dependent on the
presence of large amounts of adhesive (19,48).
In the present study, both pliers used generated variable amounts
of adhesive remnants on the enamel surfaces. Thus, the type of
pliers did not affect the extent of the enamel damage. The results
of the present study are similar to those of other studies
(19,36). However, a previous study performed
on a small number of samples (n=6) demonstrated that the side
cutter led to bond failures at the enamel-adhesive interface, while
the anterior bracket removal pliers led to bond failures at the
bracket adhesive interface (49).
Ceramic brackets are extremely fragile, and thus a
small amount of energy may be sufficient to fracture them (50). From a clinical point of view, the
fracture of a ceramic bracket is undesirable, as the presence of
bracket fragments on the tooth surface hampers the polishing of the
enamel (51). The present study
found that the side cutters caused fractures of ceramic brackets
more frequently than the anterior bracket removal pliers.
Other studies have also demonstrated that enamel
cracks appeared only during the debonding of ceramic brackets,
revealing a greater risk of damage from this procedure compared
with the debonding of metallic brackets. This aspect can be
explained by the fact that the composite system used for the
bonding procedure adheres strongly to both surfaces (the enamel and
ceramic bracket mesh) (52,53).
Particular attention should be paid to the debonding
procedure. Following the bracket removal technique, there should be
no adhesive resin remaining on the enamel surface. This step needs
to be performed without causing enamel damage. This objective is as
important as the other objectives of the fixed orthodontic
treatment: The correction of the malocclusion and the re-education
of the functions of the dento-maxillary apparatus (mastication,
deglutition, respiratory function, speech and facial esthetics), as
enamel damage can endanger the vitality of the tooth.
In conclusion, the present study demonstrated that
the side cutter produced fractures of the ceramic brackets more
frequently than the anterior bracket removal pliers. By contrast,
the type of pliers used for the debonding procedures did not
influence the amount of adhesive remaining on the tooth surface.
After debonding, metallic brackets generated larger amounts of
adhesive remaining on the enamel. Thus, through the OCT analysis of
the enamel structure, the quality of the processes and materials
used for manufacturing brackets can be increased. In the future,
OCT examination may be used in vivo to facilitate
orthodontic procedures in order to restore the tooth surface to its
pre-treatment condition.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SMSP, MJT, FIM, AGN and ITD made substantial
contributions to the conception and design of the study. SMSP, EO,
AC, AIS, ITD and ESB made substantial contributions to the
acquisition, analysis and interpretation of the data for the study.
MJT, AC, ESB and ITD drafted the manuscript and revised it
critically for important intellectual content. All authors reviewed
the literature findings and critically revised the manuscript and
approved the current form of the article in order to be submitted
to the journal. MJT and ITD confirm the authenticity of all the raw
data. All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was conducted according to the
guidelines of the Declaration of Helsinki and approved by the
Ethical Committee of the University of Medicine and Pharmacy of
Craiova, Romania (decision reference no. 72/07.09.2020). Written
informed consent was obtained from all subjects involved in the
study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Shimada Y, Sadr A, Sumi Y and Tagami J:
Application of optical coherence tomography (OCT) for diagnosis of
caries, cracks and defects of restorations. Curr Oral Health Rep.
2:73–80. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Hee MR, Puliafito CA, Wong C, Duker JS,
Reichel E, Rutledge B, Schuman JS, Swanson EA and Fujimoto JG:
Quantitative assessment of macular edema with optical coherence
tomography. Arch Ophthalmol. 113:1019–1129. 1995.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Swanson EA, Izatt JA, Hee MR, Huang D, Lin
CP, Schuman JS, Puliafito CA and Fujimoto JG: In vivo retinal
imaging by optical coherence tomography. Opt Lett. 18:1864–1866.
1993.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Fercher AF, Hitzenberger CK, Drexler W,
Kamp G and Sattmann H: In vivo optical coherence tomography. Am J
Ophthalmol. 116:113–114. 1993.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Isenberg G and Sivak MV: Gastrointestinal
optical coherence tomography. Technol Gastrointest Endosc.
5:94–101. 2003.
|
|
6
|
Chen Y, Aguirre AD, Hsiung PL, Huang SW,
Mashimo H, Schmitt JM and Fujimoto JG: Effects of axial resolution
improvement on optical coherence tomography (OCT) imaging of
gastrointestinal tissues. Opt Express. 16:2469–2485.
2008.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhang J, Chen Z and Isenberg G:
Gastrointestinal optical coherence tomography: Clinical
applications, limitations, and research priorities. Gastrointest
Endosc Clin N Am. 19:243–259. 2009.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Welzel J: Optical coherence tomography in
dermatology: A review. Ski Res Technol. 7:1–9. 2001.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Zhang K, Huang Y, Pradilla G, Tyler B and
Kang JU: Real-time intraoperative full-range complex FD-OCT guided
cerebral blood vessel identification and brain tumor resection in
neurosurgery. In: Proceedings of the SPIE (International Society
for Optics and Photonics). Photonic Therapeutics and Diagnostics
VII, San Francisco, CA, pp1-8, 2011.
|
|
10
|
Srinivasan VJ, Radhakrishnan H, Jiang JY,
Barry S and Cable AE: Optical coherence microscopy for deep tissue
imaging of the cerebral cortex with intrinsic contrast. Opt
Express. 20:2220–2239. 2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Radhakrishnan H and Srinivasan VJ:
Compartment-resolved imaging of cortical functional hyperemia with
OCT angiography. Biomed Opt Express. 4:1255–1268. 2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Srinivasan VJ, Mandeville ET, Can A, Blasi
F, Climov M, Daneshmand A, Lee JH, Yu E, Radhakrishnan H, Lo EH, et
al: Multiparametric, Longitudinal optical coherence tomography
imaging reveals acute injury and chronic recovery in experimental
ischemic stroke. PLoS One. 8(e71478)2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Colston BW Jr, Everett MJ, Da Silva LB,
Otis LL, Stroeve P and Nathel H: Imaging of hard- and soft-tissue
structure in the oral cavity by optical coherence tomography. Appl
Opt. 37:3582–3585. 1998.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Braz AK, Aguiar CM and Gomes AS:
Evaluation of the integrity of dental sealants by optical coherence
tomography. Dent Mater. 27:e60–e64. 2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Garcez AS, Suzuki SS, Ribeiro MS, Mada EY,
Freitas AZ and Suzuki H: Biofilm retention by 3 methods of ligation
on orthodontic brackets: A microbiologic and optical coherence
tomography analysis. Am J Orthod Dentofac Orthop. 140:e193–e198.
2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Baek JH, Na J, Lee BH, Choi E and Son WS:
Optical approach to the periodontal ligament under orthodontic
tooth movement: A preliminary study with optical coherence
tomography. Am J Orthod Dentofac Orthop. 135:252–259.
2009.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Newman GV: Epoxy adhesives for orthodontic
attachments: Progress report. Am J Orthod. 51:901–912.
1965.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Oliver RG: A new instrument for debonding
clean-up. J Clin Orthod. 25:407–410. 1991.PubMed/NCBI
|
|
19
|
Bizheva K, Povazay B, Hermann B, Sattmann
H, Drexler W, Mei M, Holzwarth R, Hoelzenbein T, Wacheck V and
Pehamberger H: Compact, broad-bandwidth fiber laser for
sub-2-microm axial resolution optical coherence tomography in the
1300-nm wavelength region. Opt Lett. 28:707–709. 2003.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Hsieh YS, Ho YC, Lee SY, Chuang CC, Tsai
JC, Lin KF and Sun CW: Dental optical coherence tomography. Sensors
(Basel). 13:8928–8949. 2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Brady DJ: Optical Imaging and
Spectroscopy. In: Coherence imaging - 6.5 Optical coherence
tomography. Wiley & Sons, Inc., Hoboken NJ, pp238-242,
2009.
|
|
22
|
Drexler W and Fujimoto JG: Optical
Coherence Tomography. In: Dental OCT. Springer-Verlag, Berlin,
Heidelberg, pp1166-1168, 2008.
|
|
23
|
Vo-Dinh T: Optical coherence tomography
imaging. Chapter 13. In: Biomedical Photonics Handbook. CRC Press,
Boca Raton, London, New York, NY, Washington, DC, pp22-24,
2003.
|
|
24
|
Sectakof PA and Selnes JE: Iatrogenic
effects of ortodontic treatment. Ont Dent. 71:35–40.
1994.PubMed/NCBI
|
|
25
|
Geiger AM, Gorelick L, Gwinnett AJ and
Benson BJ: Reducing white spot lesions in orthodontic populations
with fluoride rinsing. Am J Orthod Dentofac Orthop. 101:403–407.
1992.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Geiger AM, Gorelick L, Gwinnett AJ and
Griswold PG: The effect of a fluoride program on white spot
formation during orthodontic treatment. Am J Orthod Dentofac
Orthop. 93:29–37. 1988.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Demito CF, Vivaldi-Rodrigues G, Ramos AL
and Bowman SJ: The efficacy of a fluoride varnish in reducing
enamel demineralization adjacent to orthodontic brackets: An in
vitro study. Orthod Craniofac Res. 7:205–210. 2004.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Osiac E, Bălşeanu TA, Mogoantă L, Gheonea
DI, Pirici I, Iancău M, Mitran SI, Albu CV, Cătălin B and Sfredel
V: Optical coherence tomography investigation of ischemic stroke
inside a rodent model. Rom J Morphol Embryol. 55:767–772.
2014.PubMed/NCBI
|
|
29
|
Osiac E, Săftoiu A, Gheonea DI, Mandrila I
and Angelescu R: Optical coherence tomography and Doppler optical
coherence tomography in the gastrointestinal tract. World J
Gastroenterol. 17:15–20. 2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Chhibber A, Agarwal S, Yadav S, Kuo CL and
Upadhyay M: Which orthodontic appliance is best for oral hygiene? A
randomized clinical trial. Am J Orthod Dentofac Orthop.
153:175–183. 2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Eissa OE, El Elshourbagy EA and Ghobashy
SA: In vivo effect of a fluoride releasing adhesive on inhibition
of enamel demineralization around orthodontic brackets. Tanta Dent
J. 10:86–96. 2013.
|
|
32
|
Höchli D, Hersberger-Zurfluh M,
Papageorgiou SN and Eliades T: Interventions for orthodontically
induced white spot lesions: A systematic review and meta-analysis.
Eur J Orthod. 39:122–133. 2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Fjeld M and Øgard B: Scanning electron
microscopic evaluation of enamel surfaces exposed to 3 orthodontic
bonding systems. Am J Orthod Dentofacial Orthop. 130:575–581.
2006.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Nawrocka A and Lukomska-Szymanska M: The
indirect bonding technique in orthodontics-a narrative literature
review. Materials (Basel). 13(986)2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Leão Filho JC, Braz AK, de Araujo RE,
Tanaka OM and Pithon MM: Enamel quality after debonding: Evaluation
by optical coherence tomography. Braz Dent J. 26:384–389.
2015.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Knösel M, Mattysek S, Jung K,
Sadat-Khonsari R, Kubein-Meesenburg D, Bauss O and Ziebolz D:
Impulse debracketing compared to conventional debonding. Angle
Orthod. 80:1036–1044. 2010.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Drisko C: Oral hygiene and periodontal
considerations in preventing and managing dentine hypersensitivity.
Int Dent J. 57 (Suppl):S399–S410. 2007.
|
|
38
|
Addy M: Dentine hypersensitivity: New
perspectives on an old problem. Int Dent J. 52 (Suppl 1):S367–S375.
2002.
|
|
39
|
Pretty IA, Pender N, Edgar WM and Higham
SM: The in vitro detection of early enamel de- and
re-mineralization adjacent to bonded orthodontic cleats using
quantitative light-induced fluorescence. Eur J Orthod. 25:217–223.
2003.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Sinescu C, Negrutiu ML, Hughes M, Bradu A,
Todea C, Rominu R, Dodenciu D, Laissuee PL and Podoleanu AG:
Investigation of bracket bonding for orthodontic treatments using
enface optical coherence tomography. Vol. 6991. SPIE Digital
Library, pp69911M-1-69911M-5, 2008. doi: 10.1117/12.780701.
|
|
41
|
Rominu RO, Sinescu C, Pop DM, Hughes M,
Bradu A, Rominu M and Podoleanu AG: En-face optical coherence
tomography and fluorescence in evaluation of orthodontic
interfaces. World Acad Sci Eng Technol. 56:641–644. 2009.
|
|
42
|
Janiszewska-Olszowska J, Tomkowski R,
Tandecka K, Stepien P, Szatkiewicz T, Sporniak-Tutak K and
Grocholewicz K: Effect of orthodontic debonding and residual
adhesive removal on 3D enamel microroughness. PeerJ.
4(e2558)2016.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Kuskonmaz C, De Stefani A, Artioli G,
Zanarini M, Bonetti GA, Bruno G and Gracco A: The use of the laser
confocal scanning microscopy to measure resin remnants on
customized lingual bracket. BMC Oral Health. 20(142)2020.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Ogiński T, Kawala B, Mikulewicz M and
Antoszewska-Smith J: A clinical comparison of failure rates of
metallic and ceramic brackets: A twelve-month study. Biomed Res
Int. 2020(9725101)2020.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Ravin JJ: Follow-up study of permanent
incisors with enamel cracks as result of an acute trauma. Scand J
Dent Res. 89:117–123. 1981.PubMed/NCBI
|
|
46
|
Bevenius J, Lindskog S and Hultenby K: The
micromorphology in vivo of the buccocervical region of premolar
teeth in young adults. A replica study by scanning electron
microscopy. Acta Odontol Scand. 52:323–334. 1994.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Daprile G, Gatto MR and Checchi L: The
evolution of buccal gingival recessions in a student population: A
5-year follow-up. J Periodontol. 78:611–614. 2007.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Zachrisson BU, Skogan O and Höymyhr S:
Enamel cracks in debonded, debanded, and orthodontically untreated
teeth. Am J Orthod. 77:307–319. 1980.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Zarrinnia K, Eid N and Kehoe M: The effect
of different debonding techniques on the enamel surface: An in
vitro qualitative study. Am J Orthod Dentofac Orthop. 108:284–293.
1995.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Bishara SE and Trulove TS: Comparisons of
different debonding techniques for ceramic brackets: An in vitro
study. Part I. Background and methods. Am J Orthod Dentofac Orthop.
98:145–153. 1990.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Karamouzos A, Athanasiou AE and
Papadopoulos MA: Clinical characteristics and properties of ceramic
brackets: A comprehensive review. Am J Orthod Dentofacial Orthop.
112:34–40. 1997.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Winchester LJ: Bond strengths of five
different ceramic brackets: An in vitro study. Eur J Orthod.
13:293–305. 1991.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Pinho M, Manso MC, Almeida RF, Martin C,
Carvalho Ó, Henriques B, Silva F, Pinhão Ferreira A and Souza JCM:
Bond strength of metallic or ceramic orthodontic brackets to
enamel, acrylic, or porcelain surfaces. Materials (Basel).
13(5197)2020.PubMed/NCBI View Article : Google Scholar
|