Introduction
Since the novel coronavirus-2019 disease (COVID-19)
first emerged in Wuhan, China, it has rapidly spread to other areas
of the country and then the world. It has now affected most
countries in the world, with the epicenter having shifted from Asia
to various parts of Europe and North America (1,2). The
virus that causes this disease was initially referred to as
2019-novel coronavirus (nCoV) by the Centre for Disease Control and
Prevention (CDC), but was later given the name severe acute
respiratory syndrome (SARS)-coronavirus 2 (CoV-2) (1).
The etiological agent of COVID-19, SARS-CoV-2, was
identified on January 3, 2020 and was confirmed to belong to the
genera of β-CoVs (3). Other viruses
in the same family of CoVs have previously been identified to be
the cause of SARS and Middle East Respiratory Syndrome (MERS)
epidemics in 2003 and 2012, respectively (4,5).
Soon after the identification of this virus,
researchers worldwide began trying to discover the transmission
pathways of this virus to humans, in addition to its pathogenicity
and evolutionary origin, to ascertain the causes of mortality and
the mechanism underlying severe cases of COVID-19 (6,7).
Human-to-human transmission was reported both in hospitals and
family settings, which was found to be characterized by 2-10-day
incubation times, and it was revealed to be spread through droplets
in the air and contaminated hands or surfaces (5,8-10).
Despite the adoption of extensive control measures worldwide, the
impact of the COVID-19 pandemic has been devastating, with several
categories of professions, particularly healthcare workers (HCWs),
being among the worst hit (11).
In past SARS and MERS CoV epidemics, HCWs were also
markedly affected. During the SARS epidemic, HCWs represented 21%
of all cases in the world (12). By
contrast, in other countries, including Canada, Hong Kong and
Singapore, that number reached >50% of all cases, with multiple
reported deaths (12). Recent data
from Italy revealed that 11.9% of all diagnosed COVID-19 cases
(27,439/230,414 diagnosed) occurred in HCWs (13). The infectivity of COVID-19 is
greater than that of influenza (R0 value, which the
basic reproduction number, which represents viral infectivity, of
0.9-2.1), with an estimated R0 value of 2.28-3.10
(14,15).
Despite intensive research efforts worldwide on the
treatment of the SARS-CoV-2 infection, little is known regarding
the causes of COVID-19-related mortality (16). The purpose of the present review was
to analyze the causes of mortality associated with SARS-CoV-2
infection in general, with particular focus on the result of
infection in a professional environment.
Materials and methods
PRISMA
This review was performed in accordance with the
PRISMA statement (17).
Literature search
The SCOPUS (release date: September 26 2018;
https://www.scopus.com), Medline (using PubMed as
the search engine; Release date: January 1996; https://pubmed.ncbi.nlm.nih.gov/), Embase
(version: 2020; https://www.elsevier.com/solutions/embase-biomedical-research)
and Web of Sciences databases (version: 2020; https://www.webofknowledge.com) were searched to
recognize the relevant literature available between January 1 and
May 15, 2020, to examine the possible transmission pathways and
causes of SARS-CoV-2 infection-related mortality.
The term ‘MeSH’ was used with the following entry
terms: ‘SARS-CoV-2’ or ‘2019-nCoV’ or ‘Covid-19’ or ‘Wuhan
coronavirus’ or ‘COVID19’ and ‘mortality’ and ‘HCWs’, ‘SARS-CoV-2’
or ‘2019-nCoV’ or ‘Covid-19’ or ‘Wuhan coronavirus’ or ‘COVID19’
and ‘comorbidity’ and/or ‘HCWs’. Subsequently, a survey of the
research manuscripts that were suitable for inclusion in this
review was performed, and the research papers of importance therein
were collected and reviewed.
Inclusion and exclusion criteria
The following inclusion criterion was adopted:
Studies that investigated the causes of mortality as a result of
SARS-CoV-2 infection. Research articles, clinical trial studies,
reports from international agencies and case studies were included.
No geographical restriction was applied. The following exclusion
criteria were used: i) Scientific papers not published in English;
ii) conference abstracts; iii) systematic reviews; and iv)
meta-analyses. In cases of duplicate studies, the article with more
detailed information was included.
Quality assessment and data
extraction
A total of two external reviewers (CL and GD)
retrieved the articles independently. The title, abstract and full
text of each potentially relevant study were reviewed. Any
disagreement on the eligibility of the studies was resolved by
debate or by consulting the third reviewer (FV). The following
information was extracted from all qualified papers: Authors, year
of publication, nationality of subjects and study
characteristics.
Results
Search results
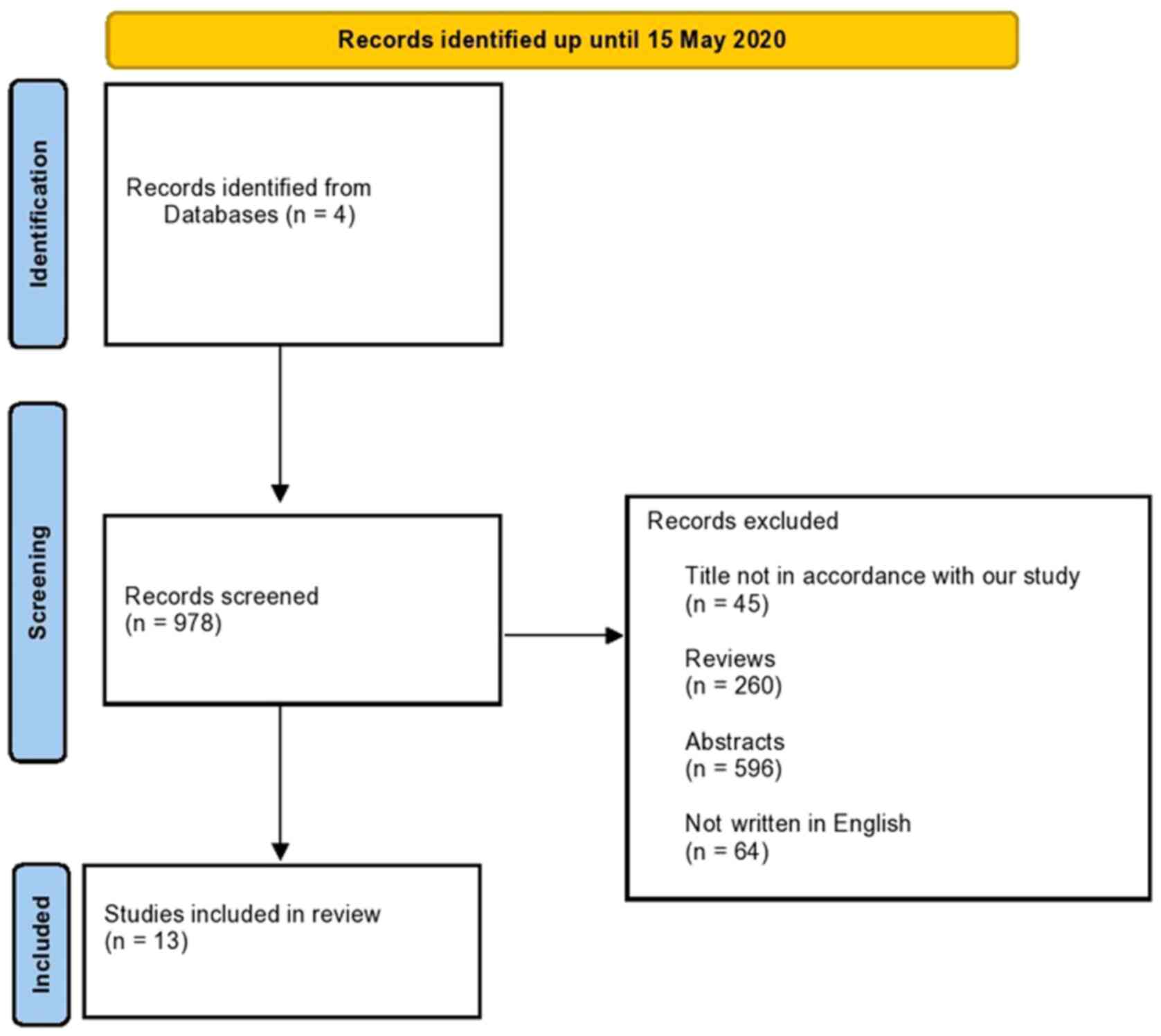
Following a search of the scientific literature by
the reviewers, a total of 978 documents were collected. A total of
260 (26%) were excluded due to them being reviews, 596 (61%) were
excluded due to them being only abstracts and 45 (5%) studies were
disqualified after a subsequent review of the title. A total of 64
(7%) of the papers were ruled out due to not being written in
English. At conclusion, 13 (1%) studies complied with the inclusion
criteria and were included in the present review (Fig. 1) (18-30).
The data mainly came from studies in Chinese and Italian
populations, since China and Italy were among the first countries
affected during the first pandemic phase.
Epidemiological analysis of mortality
data
Since the early stages of the COVID-19 outbreak, in
February, 2020, the case fatality rate (CFR; defined as the ratio
resulting from the number of individuals deceased divided by the
number of total recorded infections) in China has been 2-4%
(14). This is a much lower CFR
compared with that of SARS and MERS, which were ~10 and ~35%,
respectively, but higher than that of influenza (0.1%) (4,31).
The COVID-19 pandemic is rapidly developing. At the
time of writing the present review (June 2020), it has been ~6
months since the first case of COVID-19 was reported in Wuhan. So
far, according to a report from the World Health Organization,
COVID-19 has affected 4.5 million individuals worldwide, with
302,462 deaths as of May 15, 2020. Italy ranked fourth in the world
in terms of case number and second in terms of mortality during the
first 3 months of pandemic (16).
By May 15, 2020, Italy's CFR was ~13%, whilst that in China was
only 4% (32,33). Such a high figure is typified by the
observations in the Lombardy region, where ~50% of all Italian
infections have been recorded, with the CFR there being ~16%
(31). However, it should be noted
that CFR is generally an overestimated value of actual lethality,
which is measured as the infection fatality ratio (IFR). In
addition, the real number of cases of infection, including
asymptomatic and paucisymptomatic cases, are likely underestimated
due to them being easily overlooked as a result of limited testing
(34). IFR is the parameter that
measures the percentage of reduction over the overall infected
population, including the generally unknown number of recorded
cases that were not recorded (34).
Table I, Table II and Table III show the main results of the
eligible studies (18-30).
Based on this information, most patients with COVID-19 had good
prognoses, whilst a few were in a critical condition, particularly
the elderly and those with chronic underlying diseases (9). Statistical analyses performed
worldwide have confirmed that SARS-CoV-2 infection affects men and
women differently (9,18-21,23-26,28,29,32,35).
The fatality rate of confirmed cases in China is 4.7% in men,
compared with 2.8% in women (35).
These data are relevant with regards to HCWs, which are mainly
represented by women (90%) in the Hubei province in China (35). Therefore, any interpretation of the
differences in sex among age groups and countries must be made with
great caution (32). Italian data
also supported this trend (18);
the latest analysis conducted by the Italian National Institute of
Health (ISS) on a population of 18,641 patients (deceased and
tested positive for SARS-CoV-2) in Italy revealed that 6,339
patients were women (34% of the total), and of those who died after
being infected with SARS-CoV-2, the women were generally older
compared with the corresponding group of men who succumbed to
COVID-19 (mean age in women, 83 years; mean age in men, 79 years)
(18). To explain this, a number of
general hypotheses were made, including the following: i) Stronger
smoking habits among men; ii) higher attention to daily personal
hygiene among women; iii) more effective innate and adaptive immune
responses in women (36). In
addition, differences between men and women with regard to
mechanisms of infection, which can be associated with differences
in hormonal and genetic profiles, were also highlighted (37,38).
 | Table IMain results of infection that was
caused by or occurred in general population, workplace and
mortality. |
Table I
Main results of infection that was
caused by or occurred in general population, workplace and
mortality.
| Authors | Country | Study population,
N | Number of patients
who died | Sex,
male/female | Average age,
years | Workplace
infections, % | Case fatality
ratio, % | (Refs.) |
|---|
| Liu et al,
2020 | China | 56 HP (Elderly
patients, 18 Middle-aged patients, 38) | Elderly patients, 1
Middle-aged patients, 2 | Elderly patients,
12/6 Middle-aged patients, 19/19 | Elderly patients,
68 Middle-aged patients, 47 | Not detected | Elderly patients,
5.6 Middle-aged patients, 5.3 | (29) |
| Wang et al,
2020 | China | 138 HP | 6 | 75/63 | 56 | 29 | 4.3 | (25) |
| Wang et al,
2020 | China | 69 HP | 5 | 32/37 | 42 | Not detected | 7.5 | (27) |
| Chen et al,
2020 | China | 99 HP | 11 | 67/32 | 55.5 | Not detected | 11 | (19) |
| Guan et al,
2020 | China | 1,099 GP | 15 | 639/460 | 47 | Not detected | 1.4 | (20) |
| Yang et al,
2020 | China | 52 HP | 32 | 35/17 | 59.7 | 10 | 61.5 | (28) |
| Zhou et al,
2020 | China | 191 HP | 54 | 119/72 | 56 | Not detected | 28.3 | (21) |
| ISS report
2020 | Italy | Not reported | 6,801 | 4,789/2,012 | 78 | Not detected | 10 | (18) |
| Huang et al,
2020 | China | 41 HP | 6 | 30/11 | 49 | Not detected | 14.6 | (24) |
| Chen et al,
2020 | China | 274 HP | 113 | 83/30 | 68 | Not detected | | (26) |
| Cao et al,
2020 | China | 102 HP | 17 | 53/49 | 54 | 23.5 | 16 | (23) |
| Shi et al,
2020 | China | 416 HP | 57 | 205/211 | 64 | Not detected | 13.7 | (22) |
| Ruan et al,
2020 | China | 150 HP | 68 | 75/75 | 53 | Not detected | 45.3 | (30) |
 | Table IISummary of clinical manifestations,
hospitalization period, days of hospitalization in intensive care,
and causes of death and complications. |
Table II
Summary of clinical manifestations,
hospitalization period, days of hospitalization in intensive care,
and causes of death and complications.
| Authors | Country | Clinical
manifestations | Hospitalization
period, days | Intensive care
unit, Na | Causes of
death/complications | (Refs.) |
|---|
| Liu et al,
2020 | China | Elderly patients:
Cough, 33.3%; fever, 77%; fatigue, 11%; nasal congestion, 5.5%;
vomiting, 17%; dyspnea, 11% Middle-aged patients: Cough, 39%; fever
79%; fatigue, 7.9%; nasal congestion, 5%; vomiting, 18%; dyspnea,
5% | Not reported | Elderly patients, 5
Middle-aged patients, 4 | Elderly patients:
ARDS, 22%; HF, 16.7%; shock, 5.5%; SI, 22.2%; ARF, 19%; ALI, 19%
Middle-aged patients: ARDS, 5.2%; HF, 10.5%; shock, 5,2%; SI, 13%;
ARF, 6.5%; ALI, 6.5% | (29) |
| Wang et al,
2020 | China | Fever, 98.6%;
fatigue, 69.6%; cough, 59.4%; anorexia, 40%; myalgia, 34.8%;
dyspnea, 31.2%; diarrhea, 10%; nausea, 10%; headache, 9.4%;
vomiting, 3.6%; abdominal pain, 2%; dizziness, 9.4%; expectoration,
26.8% | Not reported | 36 | ARDS, 19.6%;
arrhythmia, 16.7%; HF, 7.2% | (25) |
| Wang et al,
2020 | China | Fever, 87%; cough,
55%; fatigue, 42%; myalgia, 30%; sputum, 29%; dyspnea, 29%; chest
pain, 20%; diarrhea, 14%; headache, 4% | Not reported | Not reported | Not reported | (27) |
| Chen et al,
2020 | China | Fever, 83%; cough,
82%; dyspnea, 31%; myalgia, 11%; headache, 8%; rhinorrhea, 4%;
chest pain, 2%; diarrhea, 4%; vomiting, 1% | Not reported | 11 | ARDS, 17%; SS, 4%;
ARF, 8%; ARI, 8%; ventilator-associated pneumonia, 1% | (19) |
| Guan et al,
2020 | China | Fever, 88%; cough,
68%; diarrhea, 3.8%; myalgia, 14.9%; nasal congestion, 4.8%;
conjunctival congestion, 0.8%; fatigue, 38%; vomiting, 5%; dyspnea,
18.7%; chills, 11.5%; sore throat, 14% | Not reported | 55 | ARDS, 3.37%; ARI,
79.1%; SS, 1%; ARF, 0.5% | (20) |
| Yang et al,
2020 | China | Fever, 98%; cough,
77%; dyspnea, 63.5%; myalgia, 11.5%; rhinorrhea, 6%; chest pain,
2%; headache, 6%; vomiting, 4%; malaise, 35%; arthralgia, 2% | Not reported | Not reported | ARDS, 81%; HF, 28%;
ARI, 37.5%; ALI, 28% | (28) |
| Zhou et al,
2020 | China | Fever, 94%; cough,
79%; sputum, 23%; myalgia, 15%; fatigue, 23%; diarrhea, 5%;
vomiting, 4% | 21 | 50 | ARDS, 31%; sepsis,
59%; HF, 40%; SI, 15%; ARI, 54%; ARF, 15% | (21) |
| ISS report
2020 | Italy | Fever, 76%;
dyspnea, 74%; cough, 39%; diarrhea, 6%; hemoptysis, 1% | 9 | Not reported | ARDS, 96.4%; ARF,
24.7%; SI, 10.4%; HF, 10.1% | (18) |
| Huang et al,
2020 | China | Fever, 98%; cough,
76%; myalgia, 44%; sputum, 28%; headache, 8%; hemoptysis, 5%;
diarrhea, 3%; dyspnea, 55% | Not reported | 13 | ARDS, 29%; HF, 12%;
SI, 10% | (24) |
| Chen et al,
2020 | China | Fever, 91%; cough,
68%; fatigue, 50%; anorexia, 24%; myalgia, 22%; dyspnea, 44%;
sputum, 30%; hemoptysis, 3%; diarrhea, 28%; nausea, 9%; vomiting,
6%; abdominal pain, 7%; headache, 11%; dizziness, 8% | 16 | Not reported | ARDS, 100%; HF,
68%; shock, 41%; ARF, 25%; ED, 40%; hyperkalemia, 37%; ARI, 51%;
hypoxic encephalopathy, 29%; sepsis, 100% | (26) |
| Cao et al,
2020 | China | Fever, 81.4%;
fatigue, 55%; cough, 49%; muscle ache, 34.3%; diarrhea, 10.8% | 17 | 18 | ARDS, 19.6%; shock,
9.8%; HF, 14.7%; ARF, 19.6%; ALI, 33.3%; multiple organ dysfunction
syndrome, 58.8% | (23) |
| Shi et al,
2020 | China | Fever, 80%; cough,
34.6%; dyspnea, 28%; fatigue, 13.2%; sputum, 5.5%; muscle ache,
4.6%; diarrhea, 3.8%; chest pain, 3.4%; sore throat, 3%;
rhinorrhea, 2.4%; headache, 2% | Not reported | Not reported | ARDS, 23.3%; ARF,
1.9%; coagulation disorders, 2.9%; electrolyte disorders, 7.2% | (22) |
| Ruan et al,
2020 | China | Not reported | Not reported | Not reported | ARDS, 53%; ARI 53%;
Myocardial damage, 33%; HF, 7% | (30) |
 | Table IIISummary of findings on
comorbidities. |
Table III
Summary of findings on
comorbidities.
| References | Country | Hypertension,
% | Diabetes, % | Chronic liver
disease, % | Chronic kidney
disease, % | Cardiovascular
disease, % | Chronic obstructive
pulmonary disease, % | Malignancy, % | Autoimmune disease,
% | (Refs.) |
|---|
| Liu et al,
2020 | China | Elderly patients,
28 Middle-aged patients, 13.2 | Elderly patients,
17 Middle-aged patients, 2.7 | Elderly patients,
55.5 Middle-aged patients, 4 | Not reported | Elderly patients,
17 Middle-aged patients, 4 | Not reported | Not reported | Not reported | (29) |
| Wang et al,
2020 | China | 31.2 | 10.1 | Not reported | Not reported | 14.5 | Not reported | 7.2 | Not reported | (25) |
| Wang et al,
2020 | China | 13 | 7 | Not reported | Not reported | 12 | 6 | 6 | Not reported | (27) |
| Chen et al,
2020 | China | Not reported | 12 | Not reported | Not reported | 40 | Not reported | 1 | Not reported | (19) |
| Guan et al,
2020 | China | 4.9 | 7.4 | Not reported | Not reported | 3.9 | 1.1 | 0.9 | Not reported | (20) |
| Yang et al,
2020 | China | Not reported | 17 | Not reported | Not reported | 23.5 | 8 | 4 | Not reported | (28) |
| Zhou et al,
2020 | China | 30 | 19 | Not reported | Not reported | 8 | 3 | 2 | Not reported | (21) |
| ISS report
2020 | Italy | 73 | 31.3 | Not reported | Not reported | 80 | Not reported | 17.3 | Not reported | (18) |
| Huang et al,
2020 | China | 15 | 20 | Not reported | Not reported | 15 | 2 | Not reported | Not reported | (24) |
| Chen et al,
2020 | China | 34 | 17 | Not reported | Not reported | 8 | 7 | 3 | 1 | (26) |
| Cao et al,
2020 | China | 27.5 | 10.8 | 2 | 3.9 | 10 | 9.8 | 3.9 | Not reported | (23) |
| Shi et al,
2020 | China | 30.5 | 14.4 | Not reported | Not reported | 20 | 2.9 | 2.2 | Not reported | (22) |
Advancing age, hypertension, high lactate
dehydrogenase levels, as well as men with severe heart trauma,
hyperglycemia and use of high-dose corticosteroids were previously
associated with a higher risk of mortality in general (39,40).
Patients with cardiovascular disease (CVD) who were infected with
the virus were also associated with an elevated risk of adverse
outcomes, such that the infection itself was found to be associated
with CVD complications (41-43).
Infection caused by or occurring in
the workplace and mortality
Following a review of the literature, only studies
that analyzed the relationship between infection and mortality in
HCWs could be found. To the best of our knowledge, no other working
sector appears to have been investigated in depth. Of the several
professional scenarios where individuals could be exposed to
SARS-CoV-2, only environments of HCWs appeared to be associated
with the highest risk of exposure (44-48).
As front-line caregivers for patients with COVID-19,
HCWs are considered to be in the high-risk population (49). Medical staff caring for these
patients face mental stress, physical exhaustion, separation from
families, stigma, and the emotional stress of losing their patients
and colleagues (50,51). Multiple HCWs have acquired
SARS-CoV-2 and some have died. In Italy, as of May 2020, 203 HCWs
had succumbed to COVID-19(33).
As of February 11, 2020, 3,019 HCWs were reported to
have been infected with SARS-CoV-2 in China. A total of 1,716 HCW
cases were confirmed by nucleic acid testing (52) and ≥6 HCWs have died (28). It was estimated that 3.8% patients
with COVID-19 were HCWs as reported by Zeng Yixin, vice minister of
China's National Health Commission during a news conference, on
February 14th, 2020(53). In
addition, hospital-associated transmission has been reported to be
a major route of spreading SARS-CoV-2(2).
HCWs are frequently at higher risks of being
infected during novel disease outbreaks, particularly before the
transmission dynamics have been fully ascertained (48,54,55).
Risks of SARS-CoV-2 infection may be higher among professionals who
work closely with patients, including dentists and ophthalmologists
(56,57). In addition, certain procedures, such
as non-invasive ventilation, high-flow nasal cannula and bag-mask
ventilation, are key treatments performed in non-mechanical
ventilation wards that may generate large volumes of aerosol
(58). HCW infection risks can be
lessened if proper precautions are taken in hospitals, such as
using personal protective equipment (PPE) (47,48,54,59,60).
To date, little is known regarding the route of
SARS-CoV-2 transmission in healthcare milieus. Heinzerling et
al (55) previously described
the first known cases of occupational SARS-CoV-2 transmission to
HCWs in Solano Hospital (Solano County, CA, USA). Among a cohort of
121 healthy HCWs who were exposed to patients COVID-19 positive
without protection, 43 of whom were symptomatic, but only three
developed confirmed COVID-19 despite multiple protected exposures
(55). HCWs who developed COVID-19
had a longer duration of exposure to the patient than other HCWs,
whose origin of SARS-CoV-2 infection was initially unknown
(55). In addition, exposure during
nebulizer treatments and biphasic positive airway pressure was also
more common among HCWs who developed COVID-19(55). These results emphasize the increased
COVID-19 transmission risk associated with prolonged, unprotected
patient contact and the importance of ensuring that HCWs exposed to
patients with confirmed/suspected COVID-19 are well protected
(50).
With regards to the USA, there is no comprehensive
analyses of mortality among HCWs. During March 1-May 31, 2020,
COVID-NET in the USA received reports of 28,972 hospitalized adult
patients. HCP status was documented for 6,760 of the sampled
patients, 438 of whom were HCPs, yielding a weighted estimate of
5.9% (95% CI=5.1-6.8%). A substantial proportion of HCP with
COVID-19 had indicators of severe disease: 27.5% were admitted to
an intensive care unit (ICU), 15.8% required invasive mechanical
ventilation and 4.2% died during hospitalization (61). This value included doctors, nurses
and paramedics, in addition to important healthcare support staff,
including hospital janitors, nursing home workers and
administrators (61).
In Italy, according to the National Institute for
Insurance against Accidents at Work data (updated to include data
up to May 15, 2020), 43,399 reports associated with COVID-19
infection were made, 54% of which occurred in March and very
quickly spread to Northwest Italy (62). Of these 43,399 COVID-19 reports,
almost all (99%) were associated with industry and services'
insurance management, with cases recorded in other sectors
including agriculture, navigation and state administration (<500
cases) (62). Of those reports,
72.8% were from the healthcare and social services sectors,
including hospitals, private clinics and assisted health centers,
compared with those in productive activities, such as the food
supply chain, involved in the pandemic (62).
With regards to lethal exitus in HCWs, a survey
(data available up to May 15, 2020) included 171 reports of deaths
for COVID-19, where 82.5% (n=141) of these were men and 17.5%
(n=30) were women (62). The mean
age of these patients was 59 years (for both sexes). The age range
data showed that 79.8% (n=121) of the overall cases of COVID-19
were patients aged 50-64 years. The >64-year age group was next
at 19.3% (n=33), then the 35-49-year age group at 8.2% (n=14) and
finally the <34-year age group at 1.7% (n=3) (50).
A previous territorial analysis revealed the
following distribution of mortality in Italy: 57.9% (n=99) occurred
in northwest Italy (Lombardy 43.9%), 14.0% (n=24) in northeast
Italy (Emilia-Romagna, 8.2%), 11.1% (n=19) in central Italy
(Marche, 4.1%), 15.2% (n=26) in southern Italy (Campania, 7,6%)
(n=9) and 1.8% (n=3) in the Italian island of Sicily (62). In detail, HCWs as healthcare
technicians (70% of whom are nurses) and physicians were the most
at risk of virus infection, where 15.5% of cases were codified,
followed by healthcare social workers (10.7%), administration
employees (8.3%) and social services workers (6.0%) (62).
Clinical manifestations
The complete clinical manifestation of COVID-19
infection includes respiratory, neurological, cardiovascular and
coagulative symptoms, which in certain cases can result in
mortality (Table II) (18-30,63-68).
The most common symptoms reported in the articles
examined in the current review were as follows: Fever (76-98.6%),
cough (34.6-82%), myalgia or weakness (11-44%), pneumonia and
complicated dyspnea (5-74%; Table
II) (18-21,24-30,69).
Less commonly reported symptoms included headache, diarrhea
(3-28%), hemoptysis, sore throat (3-14%), rhinorrhea (2.4-6%) and
phlegm-producing cough (Table II)
(18-21,24-30,68).
In addition, patients with COVID-19 tended to show higher leukocyte
numbers, prolonged prothrombin time (24), abnormal respiratory findings and
increased levels of plasma proinflammatory cytokines, including
IL-1, IL-6 and TNF (Table II)
(70).
According to several studies, significantly higher
blood levels of cytokines and chemokines were found in patients
with COVID-19, including interleukin (IL)-1β, IL-1RA, IL-6, IL-7,
IL-8, IL-9, IL-10, colony-stimulating factor (CSF), fibroblast
growth factor-2, granulocyte-macrophage CSF, monocyte
chemoattractant protein 1 (MCP1), IFN-γ, macrophage inflammatory
protein 1α (MIP1α), MIP1β, platelet-derived growth factor subunit
B, TNFα and vascular endothelial growth factor (23,25).
Some of the patients with severe COVID-19 who were admitted to the
ICU exhibited high levels of proinflammatory cytokines, including
IL-2, IL-7, IL-10, granulocyte-CSF, C-X-C motif chemokine ligand 1,
MCP1, MIP1α and TNFα, all of which are considered to enhance
disease severity (71,72).
High erythrocyte sedimentation rate and D-dimer
levels have also been detected (73). The main manifestations of severe
COVID-19 in the respiratory system were severe pneumonia and
detectable serum SARS-CoV-2 viral load, combined with the incidence
of ground-glass opacity in the lung and acute cardiac injury (ACI)
(24).
Bonetti et al (74) previously reported that several
laboratory abnormalities, including lymphopenia, increased values
of C reactive protein, lactate dehydrogenase, erythrocyte
sedimentation rate, accurately predicted the risk of mortality in a
cohort of 144 patients with COVID-19. A number of studies suggested
that a marked decrease in the total number of lymphocytes indicated
that SARS-CoV-2 can destroy immune cells to inhibit immune function
(74,75). Furthermore, damage to T lymphocytes
may be one of the important factors leading to disease exacerbation
in patients with COVID-19 (70,71).
The low absolute lymphocyte value could be used as a referencing
index for the clinical diagnosis of new SARS-CoV-2 infections
(75).
Comorbidities
Old age, obesity and smoking habits (76) may be associated with increased
mortality (Table III) (19). Populations with reduced immune
functions, including the elderly, patients with diabetes and HIV,
in addition to individuals with long-term use of immunosuppressive
drugs, are associated with increased risk of complications and
higher mortality rates in COVID-19 (Table III) (19). For example, patients with diabetes
are at higher risks of ketoacidosis during COVID-19, whereas
patients with chronic kidney disease frequently develop renal
dysfunction that necessitates kidney transplantation (20). Therefore, clinicians need to
thoroughly assess the comorbidities of patients on an individual
basis during diagnosis and the treatment of COVID-19(77).
Similar to patients that were affected by avian
origin influenza A, elderly men suffering from comorbidities and
acute respiratory distress syndrome (ARDS) have been reported to
have a higher mortality risk (75).
In all of the studies analyzed (Table
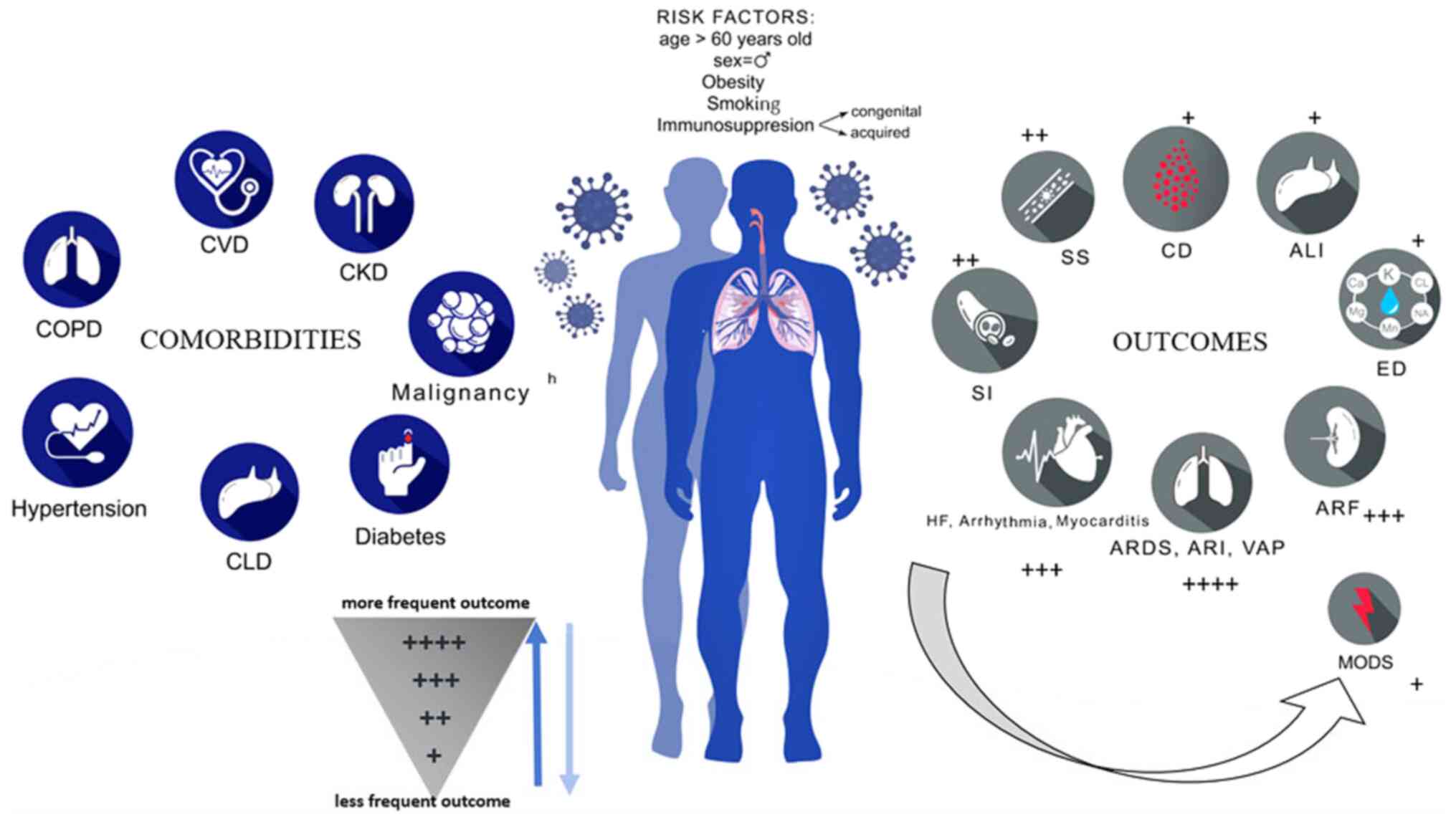
II), ARDS was reported as a major cause of mortality. Fig. 2 summarizes the main comorbidities of
COVID-19, including hypertension, COPD, cardiovascular disease,
diabetes and malignancies and outcomes in patients who died of
COVID-19, including ARDS, acute respiratory injury and heart
failure.
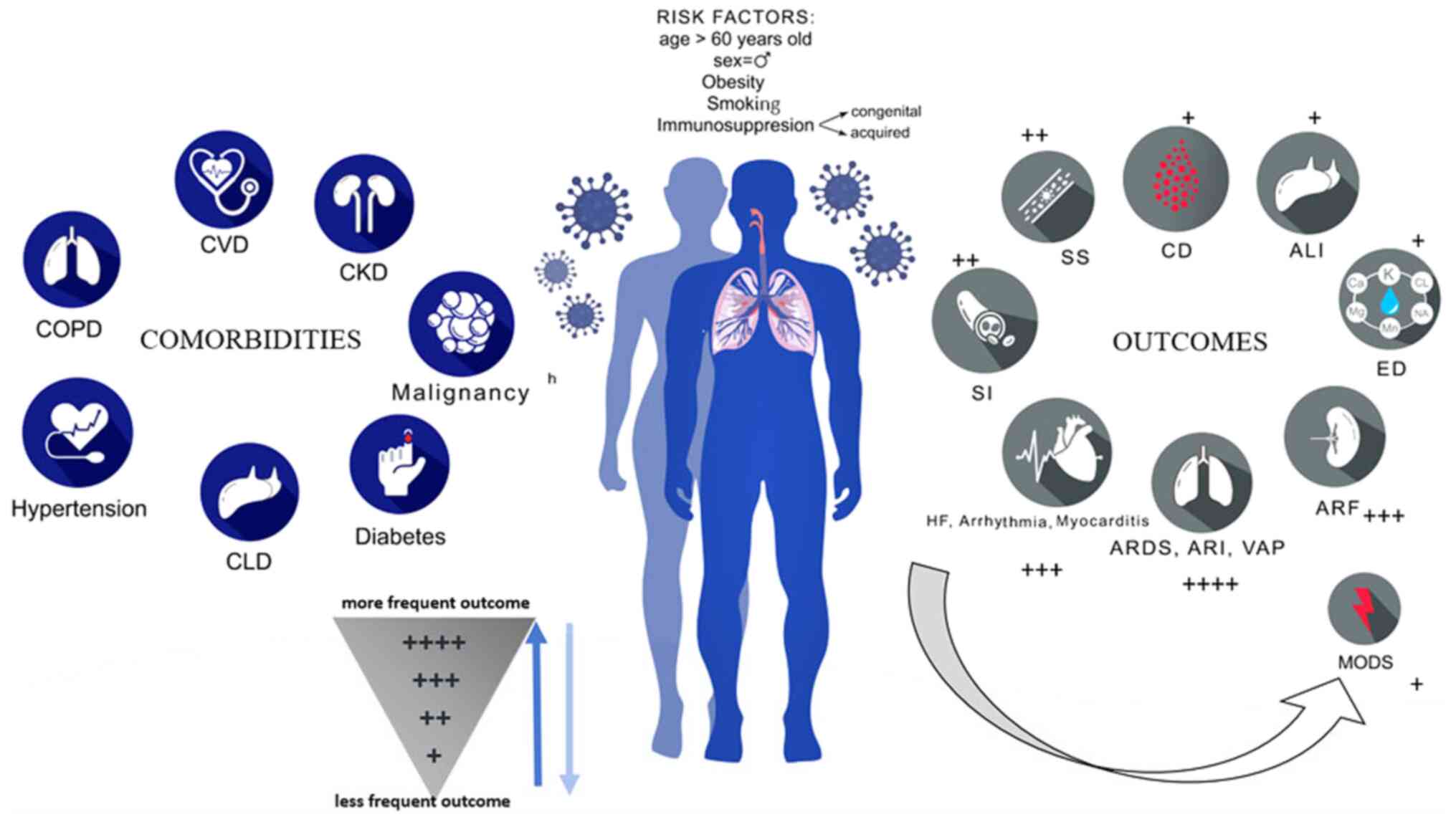 | Figure 2Comorbidities and outcomes of
patients who succumbed to COVID-19. ALI, acute liver injury; ARDS,
acute respiratory distress syndrome; ARF, acute renal failure; ARI,
acute respiratory injury; CD, coagulation disorders; CLD, chronic
liver disease; CKD, chronic kidney disease; COPD, chronic
obstructive pulmonary disease; CVD, cardiovascular disease; ED,
electrolyte disorders; HF, heart failure; MODS, multiple organ
dysfunction syndrome; SI, secondary infection; SS, septic shock;
VAP, ventilator-associated pneumonia. |
Patients with CVD have a greater risk of COVID-19.
Previous studies have revealed an association between CVD and SARS
or MERS in terms of disease severity and the risk of death
(76,77). In addition, a large number of
studies have reported an association between pre-existing CVDs and
the severity of COVID-19 (10,18,19,21-27,76-80).
A systematic analysis of 637 MERS-CoV cases showed
that hypertension and diabetes were prevalent in ~50% of patients,
whereas CVDs were present in 30% of cases (29). Diabetes was also identified as an
independent predictor of mortality and morbidity in patients with
SARS (72). A total of 12 studies
(18-29)
reported diabetes among the comorbidities of patients who succumbed
to COVID-19, whilst 10 studies (18,20-27,29)
previously reported hypertension as a risk factor (Table III).
With the spread of SARS-CoV-2 and the increase in
cases, an increasing number of infected individuals have exhibited
comorbidities such as diabetes, hypertension and CVD (41). Chen et al (19) previously reported a higher number of
men with SARS-CoV-2 infection compared with women. The reduced
susceptibility of women to all viral infections may account for the
important role of the X chromosome and sex hormones in innate and
adaptive immunity (19,81).
Hospitalization period
According to the Italian Report of ISS published on
March 26, 2020, among the Italian patients who succumbed to
COVID-19, the median hospitalization time from symptom onset to
death was 9 days; 4 days from symptom onset to hospitalization and
5 days from hospitalization to death. The time from hospitalization
to death was 2 days more in those who were moved to ICU compared
with those who were not (6 vs. 4 days) (82). According to Chen et al
(19), in deceased patients, the
median time from symptom onset to hospitalization was 10.0 days
(interquartile range, 7.0-13.0), which tended to be longer compared
with that in patients who recovered [9.0 (6.0-12.0) days]. The
median time from symptom onset to death was 16 (12.0-20.0) days,
whereas the median time from symptom onset to discharge for
patients who recovered was 26 (21.8-29.0) days. The median time
from hospitalization to death was 5 (3.0-9.3) days and the median
time from hospitalization to discharge was 16 (14.0-19.0) days
(65). According to a study by Cao
et al (23), the median time
from symptom onset and from SARS-CoV-2 exposure to death was 15 and
17 days, respectively.
Causes of mortality
All studies examined in the present review (Table II) reported ARDS (18-26,28-30)
and acute respiratory injury (ARI) (19-21,26,28,30)
as the main COVID-19-related complications followed by cardiac
complications, including arrhythmia, heart failure and myocardial
damage (Fig. 2) (18,21,23-26,29-30).
The high prevalence of arrhythmia may be partly
caused by metabolic dysfunction, hypoxia, neurohormonal or
inflammatory stress as a result of viral infection in patients with
or without prior CVD (28,83). Zou et al (8) reported that heart failure was observed
in 23% of patients with COVID-19 presentations. In particular,
heart failure was more commonly detected than acute renal failure
(ARF) in this cohort and was more common in patients who did not
survive hospitalization than in those who did (18-21,26,29).
With regard to ARDS, respiratory failure is characterized by the
rapid onset of widespread lung inflammation and subsequent
mortality (18,21,24,25).
The mortality rate of ARDS in all patients with COVID-19 was ~50%
and if ARDS reached the moderate/advanced stages, the mortality
rate reached as high as 70% (19,29).
Cardiovascular event risk factors following
pneumonia include old age, pre-existing CVD and severe pneumonia at
admission (84). Coronary heart
disease has also been found to be associated with poorer outcomes
in influenza and other viral respiratory infections (84).
Other common complications associated with COVID-19
include shock (64), ARF, acute
liver injury (ALI) and secondary infection (23,24,28,29).
Multiple organ dysfunction syndrome can either occur individually
at different times or concurrently (23,25,79).
Secondary infection, sepsis and subsequent septic shock have been
reported by seven previous studies (18-21,24,26,29).
According to Zhou et al (21), sepsis developed at a mean of 9 days
after illness onset in all patients with COVID-19. Coagulopathy
commonly occurs during sepsis and may be an indicator of worse
outcomes of severe COVID-19(20).
ARI and systemic coagulopathy can be listed as two of the
underlying causes of morbidity and mortality that characterize
SARS-CoV-2 infection (85).
Recent observations have suggested that respiratory
failure during COVID-19 is not followed by the development of ARDS
alone and that microvascular thrombotic processes may also serve a
role (86). These processes may
have significant consequences as far as the diagnostic and
therapeutic management of these patients is concerned. A strong
association has been found among the D-dimer levels, disease
progression and chest CT features, suggesting venous thrombosis
(21). Han et al (87) previously reported reduced
coagulation functions in patients with SARS-CoV-2 infection
compared with those in healthy individuals, including elevated
D-dimer, fibrin/fibrinogen degradation products and fibrinogen
levels. In addition, Zhou et al (21) and Tang et al (88) recently reported a positive
correlation between elevated D-dimer levels upon hospitalization
and in-hospital COVID-19 mortality, suggesting the presence of an
unknown pulmonary embolism and the possible role of CT pulmonary
angiography in the rapid identification of cases that will undergo
rapid clinical deterioration with COVID-19.
ARF was previously assessed as a complication in
five different studies and was found to have a higher incidence
rate in Italy compared with that elsewhere, where it was detected
in 24% of deceased patients (18,20,21,26,29).
In addition, ARF was revealed to be more common among patients with
more severe disease, particularly those admitted to the ICU and
could therefore be considered a negative prognostic factor of
survival (89).
It has been suggested that an insufficient systemic
inflammatory immune response during a cytokine storm may contribute
to the hypoperfusion-related damage of renal tubules (90). In addition to organ dysfunction as a
result of immune dysregulation, emerging evidence has suggested the
possibility of a direct cytopathic effect of SARS-CoV-2(91).
ALI as a COVID-19 complication was observed only by
three studies (23,28,29).
In the study by Yang et al (28), which detected in 28% (n=14) of the
examined patients, all of whom were admitted to hospital already in
a critical condition.
It was observed in some studies that poorer
clinical outcomes were associated with disease severity (29,29,63,67).
In addition, disease tended to progress faster in the elderly, with
a shorter median number of days from early symptom onset to death
recorded among people aged ≥65 years (67).
Cytokine release syndrome (CRS) is a systemic
inflammatory response that occurs in a large number of patients
with severe COVID-19, which is also an important cause of death
(92). IL-6 is the key molecule of
CRS (92). SARS-CoV-2 binds to
alveolar epithelial cells and then activates innate and adaptive
immune systems, resulting in the release of a large number of
cytokines, including IL-6(93).
During the first phase of the pandemic, the therapeutic use of an
IL-6 receptor antagonist (tocilizumab) in combination with
corticosteroids was recommended for the treatment of cytokine
storm, which reduced the dose and treatment period compared with
corticosteroid therapy alone (94).
However, after the studies were conducted, its use was eliminated
since it showed no clinical benefit (95-97).
Given the proposed role of these proinflammatory factors, increases
in vascular permeability can let a large amount of fluid and blood
cells into the alveoli, resulting in dyspnea and even respiratory
failure (98,99). The first gross examination report of
an autopsy of a patient who succumbed to COVID-19 revealed that the
bronzed aspect of both lungs and a large amount of gray-white
viscous liquid overflow could be observed following incision
(100).
Discussion
COVID-19-related contagion and mortality rates are
continuously growing worldwide, having spread from China to the
rest of the world, including South America (64). During the initial stages of the
pandemic, Italy, Spain and France were particularly affected in
Europe (101,102). As of May 2020, the USA is the
country with the most COVID-19 cases (>1,361,522 cases)
(102) and a 6% mortality rate. By
contrast, the mortality rate in Italy is ~13% (103). Latin America and the Caribbean are
also witnessing increasing infection rates, with >425,000 cases
(102). In addition, Brazil, Peru,
Chile and Mexico are countries that are on the list of the highest
numbers of infections in the Americas (102). In Brazil, the pandemic was growing
exponentially with an increase of 10,000 infections per day as of
May 2020 May (104).
COVID-19 was also analyzed as an outcome of
infection in the workplace. The analyzed data revealed that
healthcare and social services have been particularly affected
(105). In the USA, HCWs represent
10-20% of patients with COVID-19, a number similar to that observed
in other badly affected countries, such as Italy and Spain
(103). In Italy, ~17,000 HCWs
have been infected at the time of writing (May 2020) (106). Although a number of studies have
explored COVID-19 in HCWs worldwide (23,50,62,107),
to date, systematized mortality data are scarce (49).
The high number of infections among HCWs, mainly
during the early stages of the outbreak, could be attributed to a
lack of awareness regarding its presence in hospitals treating
patients with SARS-CoV-2 infection (54,108).
In addition, only a partial knowledge of the risks, lack of bespoke
preventive actions and possibly the inadequate availability of PPE
have been proposed to serve a role in the number of infections
(54,108).
The Italian healthcare system is a well-developed
healthcare system (109); however,
the country was unprepared to cope with the impact of
COVID-19(110). According to Chou
et al (110), a significant
diffusion route of SARS-CoV-2 is in-hospital transmission,
particularly through HCWs. This was largely underestimated at the
early stages of the pandemic, including by the HCWs themselves
(49,111).
In some hospitals in Europe, especially in Italy
and Spain, the same waiting rooms contained both patients who were
infected and those who were not (112). This provided a favorable milieu
for the virus to spread (111).
Incidentally, centralized ventilation systems also made a negative
contribution, since they did not contain high-efficiency
particulate air filters, which may have functioned to trap the
viral particles (93).
The guidelines developed during the first pandemic
phase for the prevention of SARS-CoV-2 infection recommend the use
of rapid diagnostic tests for the screening of patients and HCWs
prior to their admission to hospital, which has enabled the early
identification of asymptomatic cases (102,105). The currently available molecular
diagnostic methods have also improved. In addition, antibody-based
methods used to detect infections that went undetected in the
population, including those that are asymptomatic, were also
employed early but were found to be unsuitable for early disease
detection (59,113-115).
Furthermore, according to Li et al (112), HCWs were not well-prepared for
this sudden COVID-19 outbreak, particularly in departments of
infectious diseases.
During the first phase of the pandemic, little was
known regarding SARS-CoV-2 transmission in the health care sector.
Reports from Singapore, Illinois, USA and Hong Kong previously
described clusters of HCWs exposed to patients with COVID-19
without any documented HCW transmission (116,117). Most cases of HCW exposure to
COVID-19 occurred even when the HCWs were using precautions against
contact, droplet or airborne risks (93). In addition, as COVID-19 community
transmission increased, determining whether HCW infections develop
in workplaces or in the general population became increasingly
difficult (50).
The studies examined in the present review
confirmed that increased age was associated with increased risk of
mortality in patients with COVID-19 (18-30).
Although the mean age of patients tested positive for SARS-CoV-2
observed in China was lower than that in Italy, mean life duration
should be taken into consideration, as it is longer in Italy
compared with China (40,52).
According to Zhou et al (21), age-related defects in T- and B-cell
function, in addition to the excess production of type 2 cytokines,
may lead to the insufficient control of viral replication and more
prolonged proinflammatory reactions. This can potentially result in
poorer outcomes. Cardiac complications, including the induction or
aggravation of heart failure, arrhythmia and myocardial infarction
are common among patients with pneumonia (21).
Cardiac arrest was observed in ~3% of patients with
pneumonia (117). Cardiovascular
event risk factors following pneumonia include old age,
pre-existing CVD and high severity of pneumonia at admission
(21,116). Most deceased patients in all
studies had at least one comorbidity (18,20,21,22,24-28,30).
The most common pre-existing pathologies diagnosed prior to
infection with COVID-19 were hypertension, diabetes, ischemic
cardiopathy, atrial fibrillation and active cancer in the last 5
years (18,23,24,64,66-68,78,79).
Furthermore, the main complications causing lethal exitus in
patients were ARDS with ARI, cardiac failure, secondary infection
and septic shock, with ARF and ALI only appearing in a small
percentage of cases (18,20-22,24,27,28,30).
According to Liu et al (29), admission to the ICU with mechanical
and assisted ventilation was only required for elderly patients.
Furthermore, in a study performed by Huang et al (24), patients admitted in ICUs had higher
plasma levels of proinflammatory cytokines, such as IL-2, IL-7,
IL-10 and TNFα, compared with patients not admitted to the ICU. The
highest mortality rate was recorded in ICU cases (24).
According to Chen et al (19), patients with COVID-19 may also be at
risk of severe lung embolism. According to Magro et al
(85), severe COVID-19 may define a
type of microvascular damage syndrome mediated by the activation of
complement pathways and an associated pro-coagulant condition.
Although both the etiology and incidence of acute
pulmonary embolism under the setting of COVID-19 pneumonia remain
unclear, available biological and clinical data raised concerns
regarding unsuspected pulmonary embolism and warrants further
research into this specific issue (117). The International Society on
Thrombosis and Haemostasis advocates the use of laboratory tests,
including tests for D-dimers, prothrombin time and platelet count,
to identify patients who are at risk of an adverse outcome and
require hospitalization (118).
According to the ISS report that described the
characteristics of 6,801 patients with COVID-19 who died in Italy,
the mean patient age at death was 78 years, with women comprising
29.6% of all deaths and being older than men at the time of death.
The majority of patients with the infection died of ARDS, followed
by ARF, secondary infections and ALI (18). This potentially explains why the
median age of deceased Italian patients is much older than that of
patients in other countries, and may also contribute to the
increase in the mortality rate to ≤13% (119). Elderly age is associated with the
presence of comorbidities that can contribute to the mortality of
patients with COVID-19 (18,119).
However, these mortality rate estimates are based on the number of
casualties relative to the number of confirmed cases of infection
and do not represent the actual death rate. Patients who die on any
given day were infected much earlier and therefore the mortality
rate denominator should be the overall number of individuals
infected at the same time as those who died (120). However, the full denominator
remains unknown since asymptomatic cases or patients with mild
symptoms may not be tested and will not be confirmed as COVID-19
cases. Such cases therefore cannot be included in the assessment of
real mortality rates as actual estimates only pertain to clinically
apparent COVID-19 cases. These findings showed that the current
numbers may be underestimating the potential threat of COVID-19 in
symptomatic patients (120).
During the first pandemic phase in the world, no
autopsies have been performed on any patients who succumbed to
COVID-19. Therefore, in most cases, there was no official
verification of the causes of death (121), which has led to the loss of
information regarding the causes that resulted in lethal exitus
that could have provided useful information for treatment
strategies (122).
Due to the potential infection by SARS-CoV-2, tight
control is essential to monitor its potential host adaptation,
infectivity, viral evolution, transmissibility and pathogenicity,
to obtain an effective vaccine and accelerate herd immunity
(90,123,124).
Despite the short time elapsed since the COVID-19
outbreak, a large number of studies have been conducted and large
quantities of real-time information have been generated. This
enabled the present review to provide an accurate description of
the mortality causes. A limitation of the present study is that it
only focused on articles published in English during the early
stages of the outbreak, considering that this pandemic was
initiated in China. Although the data examined herein cannot be
used to represent the rest of the world in terms of COVID-19, it
will provide a foundation for further studies. Furthermore, in the
present study, the COVID-19-related mortality due to occupational
infection was only described during the first phase of the
pandemic. Therefore, no second-wave mortality data were reported.
The existing data on COVID-19-mediated mortality were mainly
centered on China and Italy, but not on other European countries.
Since COVID-19 case numbers have rapidly increased, particularly in
European countries, it is of importance to determine the
transmissibility and mortality rates of SARS-CoV-2 in these
countries to establish prevention and control procedures. Lastly,
the analysis of COVID-19 in the present study was also performed
with regards to mortality in HCWs. However, analysis on the
incidence, mode of transmission and clinical characteristics would
have been difficult due to incomplete data.
Following a thorough analysis of the studies in the
present review, it may be reasonable to question whether COVID-19
should be categorized as severe pneumonia. According to Pomara
et al (16), the only
medical method that can address this issue is autopsy. Despite the
decline in the frequency of postmortem examinations, autopsies are
a useful procedure for determining the cause of deaths. Physicians
are now considering whether COVID-19 has a systemic pathology that
involves the vascular system of other body regions instead of only
the lungs, including the heart, kidneys, liver, bowels, brain or
even the skin (24,117,125). Pomara et al (16) strongly recommended conducting total
autopsies on patients who succumbed to suspected or confirmed
COVID-19, particularly in the presence of other comorbidities.
COVID-19 is a public health and humanitarian crisis
that has put the healthcare systems of numerous countries under
pressure and has caused the death of thousands worldwide, including
hundreds of HCWs engaged in the frontline care of patients
(126). Additional studies are
required to further clarify the pathophysiology of COVID-19, which
appears to be more of a multi-organ disease than a type of
pneumonia. In any case, the presence of comorbidities definitely
remains a prognostic factor for predicting an unfavorable
outcome.
In conclusion, the COVID-19 pandemic is an ongoing
challenge and poses a threat to global health. Therefore, control
over the spread of the virus, fast diagnostics and research efforts
are required to understand this pathogen and develop effective
countermeasures.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
PS, FV and EV prepared and drafted the manuscript.
PS, VR, AT, GD and CL conceived and designed the study. PS, EV and
VR performed the literature search and analysis. GD, NM, AM and AT
reviewed and edited the manuscript. NM, EV, CL and VR supervised
and revised the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
World Health Organization. Coronavirus
disease (COVID-19) pandemic. Novel Coronavirus (2019-nCoV).
Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
Accessed February 7, 2020.
|
|
2
|
World Health Organization. WHO
Director-General's opening remarks at the media briefing on
COVID-19-11 March 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020.
Accessed March 13, 2020.
|
|
3
|
He F, Deng Y and Li W: Coronavirus Disease
2019 (COVID-19): What we know? J Med Virol. 92:719–725.
2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
de Wit E, van Doremalen N, Falzarano D and
Munster VJ: SARS and MERS: Recent insights into emerging
coronaviruses. Nat Rev Microbiol. 8:523–534. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Chan JF, Yuan S, Kok KH, To KK, Chu H,
Yang J, Xing F, Liu J, Yip CC, Poon RW, et al: A familial cluster
of pneumonia associated with the 2019 novel coronavirus indicating
person-to-person transmission: A study of a family cluster. Lancet.
395:514–523. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
She J, Jiang J, Ye L, Hu L, Bai C and Song
Y: 2019 novel coronavirus of pneumonia in Wuhan, China: Emerging
attack and management strategies. Clin Transl Med.
9(19)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhang H, Penninger JM, Li Y, Zhong N and
Slutsky AS: Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2
receptor: Molecular mechanisms and potential therapeutic target.
Intensive Care Med. 46:586–590. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zou L, Ruan F, Huang M, Liang L, Huang H,
Hong Z, Yu J, Kang M, Song Y, Xia J, et al: SARS-CoV-2 viral load
in upper respiratory specimens of infected patients. N Engl J Med.
382:1177–1179. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD,
Jin HJ, Tan KS, Wang DY and Yan Y: The origin, transmission and
clinical therapies on coronavirus disease 2019 (COVID-19)
outbreak-an update on the status. Mil Med Res. 7(11)2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Zhou P, Yang XL, Wang XG, Hu B, Zhang L,
Zhang W, Si HR, Zhu Y, Li B, Huang CL, et al: A pneumonia outbreak
associated with a new coronavirus of probable bat origin. Nature.
579:270–273. 2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ji Y, Ma Z, Peppelenbosch MP and Pan Q:
Potential association between COVID-19 mortality and health-care
resource availability. Lancet Glob Health. 8(e480)2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sepkowitz KA and Eisenberg L: Occupational
deaths among healthcare workers. Emerg Infect Dis. 11:1003–1008.
2005.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Integrated Surveillance of COVID-19 in
Italy (Ordinanza n. 640 del 27/02/2020) 25 May 2020 update.
Available from: https://www.epicentro.iss.it/en/coronavirus/bollettino/Infografica_25maggio%20ENG.pdf.
Accessed May 26, 2020.
|
|
14
|
Zhang S, Diao MY, Yu W, Pei L, Lin Z and
Chen D: Estimation of the reproductive number of novel coronavirus
(COVID-19) and the probable outbreak size on the Diamond Princess
cruise ship: A data-driven analysis. Int J Infect Dis. 93:201–204.
2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
D'arienzo M and Coniglio A: Assessment of
the SARS-CoV-2 basic reproduction number, R0, based on
the early phase of COVID-19 outbreak in Italy. Biosaf Health.
2:57–59. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Pomara C, Li Volti G and Cappello F:
COVID-19 deaths: Are we sure it is pneumonia? Please, autopsy,
autopsy, autopsy! J Clin Med. 9(1259)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Moher D, Liberati A, Tetzla J, Altman DG,
Altman D, Antes G, Atkins D, Barbour V, Barrowman N, Berlin JA, et
al: Preferred reporting items for systematic reviews and
meta-analyses: The PRISMA statement. Ann Intern Med. 151:264–269.
2009.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Istituto Superiore di Sanità (ISS). Report
2020. Characteristics of COVID-19 patients dying in Italy.
Available from: https://www.epicentro.iss.it/coronavirus/sars-cov-2-decessi-italia.
Accessed May 15, 2020.
|
|
19
|
Chen N, Zhou M, Dong X, Qu J, Gong F, Han
Y, Qiu Y, Wang J, Liu Y, Wei Y, et al: Epidemiological and clinical
characteristics of 99 cases of 2019 novel coronavirus pneumonia in
Wuhan, China: A descriptive study. Lancet. 395:507–513.
2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He
JX, Liu L, Shan H, Lei CL, Hui DSC, et al: Clinical characteristics
of coronavirus disease 2019 in China. N Engl J Med. 382:1708–1720.
2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z,
Xiang J, Wang Y, Song B, Gu X, et al: Clinical course and risk
factors for mortality of adult inpatients with COVID-19 in Wuhan,
China: A retrospective cohort study. Lancet. 395:1054–1062.
2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Shi S, Qin M, Shen B, Cai Y, Liu T, Yang
F, Gong W, Liu X, Liang J, Zhao Q, et al: Association of cardiac
injury with mortality in hospitalized patients with COVID-19 in
Wuhan, China. JAMA Cardiol. 25:802–810. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Cao J, Tu WJ, Cheng W, Yu L, Liu YK, Hu X
and Liu Q: Clinical features and short-term outcomes of 102
patients with coronavirus disease 2019 in Wuhan, China. Clin Infect
Dis. 71:748–755. 2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu
Y, Zhang L, Fan G, Xu J, Gu X, et al: Clinical features of patients
infected with 2019 novel coronavirus in Wuhan, China. Lancet.
395:497–506. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J,
Wang B, Xiang H, Cheng Z, Xiong Y, et al: Clinical characteristics
of 138 hospitalized patients with 2019 novel coronavirus-infected
pneumonia in Wuhan, China. JAMA. 323:1061–1069. 2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Chen T, Wu D, Chen H, Yan W, Yang D, Chen
G, Ma K, Xu D, Yu H, Wang H, et al: Clinical characteristics of 113
deceased patients with coronavirus disease 2019: Retrospective
study. BMJ. 368(m1091)2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Wang Z, Yang B, Li Q, Wen L and Zhang R:
Clinical features of 69 cases with coronavirus disease 2019 in
Wuhan, China. Clin Infect Dis. 71:769–777. 2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H,
Wu Y, Zhang L, Yu Z, Fang M, et al: Clinical course and outcomes of
critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China:
A single-centered, retrospective, observational study. Lancet
Respir Med. 8:475–481. 2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Liu K, Chen Y, Lin R and Han K: Clinical
features of COVID-19 in elderly patients: A comparison with young
and middle-aged patients. J Infect. 80:e14–e18. 2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Ruan Q, Yang K, Wang W, Jiang L and Song
J: Clinical predictors of mortality due to COVID-19 based on an
analysis of data of 150 patients from Wuhan, China. Intensive Care
Med. 46:846–848. 2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Fauci AS, Lane HC and Redfield RR:
Covid-19-navigating the uncharted. N Engl J Med. 382:1268–1269.
2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
World Health Organization. Coronavirus
disease (COVID-2019) situation reports 116. 2020. Available from:
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situationreports.
Accessed May 15, 2020.
|
|
33
|
Ceylan Z: Estimation of COVID-19
prevalence in Italy, Spain, and France. Sci Total Environ.
729(138817)2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
De Natale G, Ricciardi V, De Luca G, De
Natale D, Di Meglio G, Ferragamo A, Marchitelli V, Piccolo A, Scala
A, Somma R, et al: The COVID-19 infection in Italy: A statistical
study of an abnormally severe disease. J Clin Med.
9(1564)2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
The Novel Coronavirus Pneumonia Emergency
Response Epidemiology Team. The epidemiological characteristics of
an outbreak of 2019 novel coronavirus diseases (COVID-19)-China,
2000. China CDC Weekly. 2:113–122. 2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Cagnacci A and Xholli A: Age-related
difference in the rate of COVID-19 mortality in women versus men.
Am J Obstet Gynecol. 223:453–454. 2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Wenham C, Smith J and Morgan R: Gender and
COVID-19 Working Group. COVID-19: The gendered impacts of the
outbreak. Lancet. 395:846–848. 2020.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Channappanavar R, Fett C, Mack M, Ten Eyck
PP, Meyerholz DK and Perlman S: Sex-based differences in
susceptibility to severe acute respiratory syndrome coronavirus
infection. J Immunol. 198:4046–4053. 2017.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y,
Shi J, Zhou M, Wu B, Yang Z, et al: Risk factors for severity and
mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin
Immunol. 146:110–118. 2020.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Zhou P, Huang Z, Xiao Y, Huang X and Fan
XG: Protecting Chinese healthcare workers while combating the 2019
novel coronavirus. Infect Control Hosp Epidemiol. 41:745–746.
2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Li B, Yang J, Zhao F, Zhi L, Wang X, Liu
L, Bi Z and Zhao Y: Prevalence and impact of cardiovascular
metabolic diseases on COVID-19 in China. Clin Res Cardiol.
109:531–538. 2020.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Zheng YY, Ma YT, Zhang JY and Xie X:
COVID-19 and the cardiovascular system. Nat Rev Cardiol.
17:259–260. 2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Bansal M: Cardiovascular disease and
COVID-19. Diabetes. Metab Syndr. 3:247–250. 2020.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Cannizzaro E, Cirrincione L, Mazzucco W,
Scorciapino A, Catalano C, Ramaci T, Ledda C and Plescia F:
Night-time shift work and related stress responses: A study on
security guards. Int J Environ Res Public Health.
17(562)2020.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Occupational Safety & Health
Administration (OSHA). Guidance on preparing Workplaces for
Covid-19. Available from: www.osha.gov/Publications/OSHA3990.pdf. Accessed May
15, 2020.
|
|
46
|
Cannizzaro E, Cannizzaro C, Martorana D,
Moscadini S and Lo Coco D: Effects of shift work on cardiovascular
activity, serum cortisol and white blood cell count in a group of
italian fishermen. Euro Med Biomed J. 2012:109–113. 2012.
|
|
47
|
Rapisarda V, Nunnari G, Senia P, Vella F,
Vitale E, Murabito P, Salerno M and Ledda C: Hepatitis B
vaccination coverage among medical residents from Catania
University Hospital, Italy. Future Microbiol. 14:41–44.
2019.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Ledda C, Cinà D, Garozzo SF, Senia P,
Consoli A, Marconi A, Scialfa V, Nunnari G and Rapisarda V:
Tuberculosis screening among healthcare workers in Sicily, Italy.
Future Microbiol. 14:37–40. 2019.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Modenese A and Gobba F: Increased risk of
COVID-19-related deaths among general practitioners in Italy.
Healthcare (Basel). 8(155)2020.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Ramaci T, Barattucci M, Ledda C and
Rapisarda V: Social stigma during COVID-19 and its impact on HCWs
outcomes. Sustainability. 12(3834)2020.
|
|
51
|
Ramaci T, Rapisarda V, Bellini D, Mucci N,
De Giorgio A and Barattucci M: Mindfulness as a protective factor
for dissatisfaction in HCWs: The moderating role of mindful
attention between climate stress and job satisfaction. Int J
Environ Res Public Health. 17(3818)2020.PubMed/NCBI View Article : Google Scholar
|
|
52
|
The Novel Coronavirus Pneumonia Emergency
Response Epidemiology Team, Chinese center for disease control and
prevention. The epidemiological characteristics of an outbreak of
2019 novel coronavirus diseases (COVID-19) in China. Chin J
Epidemiol. 42:145–151. 2020.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Conference on COVID-19, by Zeng Yixin,
vice minister of China's National Health Commission. 1,700+ health
care workers have the new coronavirus. https://www.advisory.com/daily-briefing/2020/02/14/coronavirus.
Accessed March 28, 2020.
|
|
54
|
Rapisarda V, Ledda C and Maltezou HC:
Vaccination in healthcare workers: Risk assessment, planning,
strategy of intervention and legal implications. Future Microbiol.
14:1–3. 2019.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Heinzerling A, Stuckey MJ, Scheuer T, Xu
K, Perkins KM, Resseger H, Magill S, Verani JR, Jain S, Acosta M
and Epson E: Transmission of COVID-19 to health care personnel
during exposures to a hospitalized patient-Solano County,
California, February 2020. MMWR Morb Mortal Wkly Rep. 69:472–476.
2020.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Lai TH, Tang EW, Chau SK, Fung KS and Li
KK: Stepping up infection control measures in ophthalmology during
the novel coronavirus outbreak: An experience from Hong Kong.
Graefes Arch Clin Exp Ophthalmol. 8:1049–1055. 2020.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Lu CW, Liu XF and Jia ZF: 2019-nCoV
transmission through the ocular surface must not be ignored.
Lancet. 395(e39)2020.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Tran K, Cimon K, Severn M, Pessoa-Silva CL
and Conly J: Aerosol generating procedures and risk of transmission
of acute respiratory infections to healthcare workers: A systematic
review. PLoS One. 7(e35797)2012.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Ghinai I, McPherson TD, Hunter JC, Kirking
HL, Christiansen D, Joshi K, Rubin R, Morales-Estrada S, Black SR,
Pacilli M, et al: First known person-to-person transmission of
severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the
USA. Lancet. 395:1137–1144. 2020.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Cai SJ, Wu LL, Chen DF, Li YX, Liu YJ, Fan
YQ, Du SH, Huang H, Liu N, Cheng LL, et al: Analysis of
bronchoscope-guided tracheal intubation in 12 cases with
coronavirus disease 2019 under the personal protective equipment
with positive pressure protective hood. Zhonghua Jie He He Hu Xi Za
Zhi. 43:332–334. 2020.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
61
|
Center for disease Control and prevention.
Available from: www.cdc.gov.it. Accessed May 15,
2020.
|
|
62
|
Istituto nazionale Assicurazione Infortuni
sul Lavoro (INAIL). Scheda tecnica INAIL. I dati sulle denunce da
Covid. Available from: www.inail.it. Accessed May 15,
2020.
|
|
63
|
Center for disease control and prevention
(CDC). 2019 Novel Coronavirus, Wuhan, China. 2020. Available from:
https://www.cdc.gov/coronavirus/2019-nCoV/summary.html.
Accessed February 1, 2020.
|
|
64
|
Tsatsakis A, Calina D, Falzone L, Petrakis
D, Mitrut R, Siokas V, Pennisi M, Lanza G, Libra M, Doukas SG, et
al: SARS-CoV-2 pathophysiology and its clinical implications: An
integrative overview of the pharmacotherapeutic management of
COVID-19. Food Chem Toxicol. 146(111769)2020.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Pennisi M, Lanza G, Falzone L, Fisicaro F,
Ferri R and Bella R: SARS-CoV-2 and the nervous system: From
clinical features to molecular mechanisms. Int J Mol Sci.
21(5475)2020.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Kordzadeh-Kermani E, Khalili H and
Karimzadeh I: Pathogenesis, clinical manifestations and
complications of coronavirus disease 2019 (COVID-19). Future
Microbiol. 15:1287–1305. 2020.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Wang W, Tang J and Wei F: Updated
understanding of the outbreak of 2019 novel coronavirus (2019-nCoV)
in Wuhan, China. J Med Virol. 92:441–447. 2020.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Zhang JJ, Dong X, Cao YY, Yuan YD, Yang
YB, Yan YQ, Akdis CA and Gao YD: Clinical characteristics of 140
patients infected with SARS-CoV-2 in Wuhan, China. Allergy.
75:1730–1741. 2020.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX,
Wang QZ, Sun C, Sylvia S, Rozelle S, Raat H and Zhou H:
Epidemiology, causes, clinical manifestation and diagnosis,
prevention and control of coronavirus disease (COVID-19) during the
early outbreak period: A scoping review. Infect Dis Poverty.
9(29)2020.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Shi Y, Wang Y, Shao C, Huang J, Gan J,
Huang X, Bucci E, Piacentini M, Ippolito G and Melino G: COVID-19
infection: The perspectives on immune responses. Cell Death Differ.
27:1451–1454. 2020.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Zhu N, Zhang D, Wang W, Li X, Yang B, Song
J, Zhao X, Huan B, Shi W, Lu R, et al: A novel coronavirus from
patients with pneumonia in China, 2019. N Engl J Med. 382:727–733.
2020.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Costela-Ruiz VJ, Illescas-Montes R,
Puerta-Puerta JM, Ruiz C and Melguizo-Rodríguez L: SARS-CoV-2
infection: The role of cytokines in COVID-19 disease. Cytokine
Growth Factor Rev. 54:62–75. 2020.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Rothan HA and Byrareddy SN: The
epidemiology and pathogenesis of coronavirus disease (COVID-19)
outbreak. J Autoimmun. 109(102433)2020.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Bonetti G, Manelli F, Patroni A,
Bettinardi A, Borrelli G, Fiordalisi G, Marino A, Menolfi A,
Saggini S, Volpi R, et al: Laboratory predictors of death from
coronavirus disease 2019 (COVID-19) in the area of Valcamonica,
Italy. Clin Chem Lab Med. 58:1100–1105. 2020.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Liu WJ, Zhao M, Liu K, Xu K, Wong G, Tan W
and Gao GF: T-cell immunity of SARS-CoV: Implications for vaccine
development against MERS-CoV. Antiviral Res. 137:82–92.
2017.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Vardavas C and Nikitara K: COVID-19 and
smoking: A systematic review of the evidence. Tob Induc Dis.
18(20)2020.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Zhao Y, Cui C, Zhang K, Liu J, Xu J,
Nisenbaum E, Huang Y, Qin G, Chen B, Hoffer M, et al: COVID19: A
systematic approach to early identification and healthcare worker
protection. Front Public Health. 8(205)2020.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Gao HN, Lu HZ, Cao B, Du B, Shang H, Gan
JH, Lu SH, Yang YD, Fang Q, Shen YZ, et al: Clinical findings in
111 cases of influenza A (H7N9) virus infection. N Engl J Med.
368:2277–2285. 2013.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Yang JK, Feng Y, Yuan MY, Yuan SY, Fu HJ,
Wu BY, Sun GZ, Yang GR, Zhang XL, Wang L, et al: Plasma glucose
levels and diabetes are independent predictors for mortality and
morbidity in patients with SARS. Diabet Med. 23:623–628.
2006.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Badawi A and Ryoo SG: Prevalence of
comorbidities in the Middle East respiratory syndrome coronavirus
(MERS-CoV): A systematic review and meta-analysis. Int J Infect
Dis. 49:129–133. 2016.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Jaillon S, Berthenet K and Garlanda C:
Sexual dimorphism in innate immunity. Clin Rev Allergy Immunol.
56:308–321. 2019.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Istituto Superiore di Sanitá (ISS).
Epidemia COVID-19. Aggiornamento nazionale. Available from:
https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_26-marzo%202020.pdf.
Accessed March 28, 2020.
|
|
83
|
Chen C, Zhou Y and Wang DW: SARS-CoV-2: A
potential novel etiology of fulminant myocarditis. Herz.
45:230–232. 2020.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Blackburn R, Zhao H, Pebody R, Hayward A
and Warren-Gash C: Laboratory-confirmed respiratory infections as
predictors of hospital admission for myocardial infarction and
stroke: Time-series analysis of English data for 2004-2015. Clin
Infect Dis. 67:8–17. 2018.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Magro C, Mulvey JJ, Berlin D, Nuovo G,
Salvatore S, Harp J, Baxter-Stoltzfus A and Laurence J: Complement
associated microvascular injury and thrombosis in the pathogenesis
of severe COVID-19 infection: A report of five cases. Transl Res.
220:1–13. 2020.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Oudkerk M, Büller HR, Kuijpers D, van Es
N, Oudkerk SF, McLoud TC, Gommers D, van Dissel J, Ten Cate H and
van Beek EJR: Diagnosis, prevention, and treatment of
thromboembolic complications in COVID-19: Report of the national
institute for public health of the Netherlands. Radiology.
297:E216–E222. 2020.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Han H, Yang L, Liu R, Liu F, Wu KL, Li J,
Liu XH and Zhu CL: Prominent changes in blood coagulation of
patients with SARS-CoV-2 infection. Clin Chem Lab Med.
58:1116–1120. 2020.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Tang N, Li D, Wang X and Sun Z: Abnormal
coagulation parameters are associated with poor prognosis in
patients with novel coronavirus pneumonia. J Thromb Haemost.
18:844–847. 2020.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Cheng Y, Luo R, Wang K, Zhang M, Wang Z,
Dong L, Li J, Yao Y, Ge S and Xu G: Kidney disease is associated
with in-hospital death of patients with COVID-19. Kidney Int.
97:829–838. 2020.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Naicker S, Yang CW, Hwangm SJ, Liu BC,
Chen JH and Jha V: The novel coronavirus 2019 epidemic and kidneys.
Kidney Int. 97:824–828. 2020.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Durvasula R, Wellington T, McNamara E and
Watnick S: COVID-19 and kidney failure in the acute care setting:
Our experience from seattle. Am J Kidney Dis. 76:4–6.
2020.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Zhang C, Wu Z, Li JW, Zhao H and Wang GQ:
Cytokine release syndrome in severe COVID-19: Interleukin-6
receptor antagonist tocilizumab may be the key to reduce mortality.
Int J Antimicrob Agents. 55(105954)2020.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Tay MZ, Poh CM, Rénia L, MacAry PA and Ng
LFP: The trinity of COVID-19: Immunity, inflammation and
intervention. Nat Rev Immunol. 20:363–374. 2020.PubMed/NCBI View Article : Google Scholar : Luo P, Liu Y, Qiu
L, Liu X, Liu D and Li J: Tocilizumab treatment in COVID-19: A
single center experience. J Med Virol 92: 814-818, 2020.
|
|
94
|
Kooistra EJ, Waalders NJB, Grondman I,
Janssen NAF, de Nooijer AH, Netea MG, van de Veerdonk FL, Ewalds E,
van der Hoeven JG, Kox M, et al: Anakinra treatment in critically
ill COVID-19 patients: A prospective cohort study. Crit Care.
24(688)2020.PubMed/NCBI View Article : Google Scholar
|
|
95
|
Ucciferri C, Auricchio A, Di Nicola M,
Potere N, Abbate A, Cipollone F, Vecchiet J and Falasca K:
Canakinumab in a subgroup of patients with COVID-19. Lancet
Rheumatol. 2:e457–ee458. 2020.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Falzone L, Musso N, Gattuso G, Bongiorno
D, Palermo CI, Scalia G, Libra M and Stefani S: Sensitivity
assessment of droplet digital PCR for SARS-CoV-2 detection. Int J
Mol Med. 46:957–964. 2020.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Knudsen L and Ochs M: The micromechanics
of lung alveoli: Structure and function of surfactant and tissue
components. Histochem Cell Biol. 150:661–676. 2018.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Leiva-Juárez MM, Kolls JK and Evans SE:
Lung epithelial cells: Therapeutically inducible effectors of
antimicrobial defense. Mucosal Immunol. 11:21–34. 2018.PubMed/NCBI View Article : Google Scholar
|
|
99
|
Liu Q, Wang RS, Qu GQ, Wang YY, Liu P, Zhu
YZ, Fei G, Ren L, Zhou YW and Liu L: Gross examination report of a
COVID-19 death autopsy. Fa Yi Xue Za Zhi. 36:21–23. 2020.PubMed/NCBI View Article : Google Scholar : (In English,
Chinese).
|
|
100
|
Vella F, Senia P, Ceccarelli M, Vitale E,
Maltezou H, Taibi R, Lleshi A, Venanzi Rullo E, Pellicanò GF,
Rapisarda V, et al: Transmission mode associated with coronavirus
disease 2019: A review. Eur Rev Med Farmacol Sci. 24:7889–7904.
2020.PubMed/NCBI View Article : Google Scholar
|
|
101
|
World Health Organization (WHO).
Coronavirus disease 2019 (COVID-19). Situation report 116.
Available from: www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
Accessed May 15, 2020.
|
|
102
|
Center for Disease Control and Prevention
(CDC). A weekly surveillance summery of U.S. Covid-19 activity.
Available from: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/pdf/covidview-05-15-2020.pdf.
Accessed May 18, 2020.
|
|
103
|
Centro Studi Politica Internazionale
(CESPI). Covid-19. Diario settimanale sulla situazione nel mondo.
Available from: www.cespi.com. Accessed May 15,
2020.
|
|
104
|
Ramaci T, Barattucci M, Vella F, Senia P,
Cannizzaro E, Scorciapino A, Ledda C, De Giorgio A and Rapisarda V:
Straining at work and its relationship with personality profiles
and individual consequences in healthcare workers (HCWs). Int J
Environ Res Public Health. 17(610)2020.PubMed/NCBI View Article : Google Scholar
|
|
105
|
Bahl P, Doolan C, de Silva C, Chughtai AA,
Bourouiba L and MacIntyre CR: Airborne or droplet precautions for
health workers treating COVID-19? J Infect Dis: Apr 16, 2020 (Epub
ahead of print). doi: 10.1093/infdis/jiaa189.
|
|
106
|
Istituto Superiore di Sanità (ISS).
Integrated surveillance of COVID-19 in Italy. Available from:
https://www.epicentro.iss.it/en/coronavirus/bollettino/Infografica_17aprile%20ENG.pdf.
Accessed May 15, 2020.
|
|
107
|
Kamerow D: Covid-19: Don't forget the
impact on US family physicians. BMJ. 368(m1260)2020.PubMed/NCBI View Article : Google Scholar
|
|
108
|
Cirrincione L, Plescia F, Ledda C,
Rapisarda V, Martorana D, Moldovan RE, Theodoridou K and Cannizzaro
E: COVID-19 pandemic: Prevention and protection measures to be
adopted at the workplace. Sustainability. 12(3603)2020.
|
|
109
|
Nacoti M, Ciocca A, Giupponi A,
Brambillasca P, Lussana F, Pisano M, Goisis G, Bonacina D, Fazzi F,
Naspro R, et al: At the epicenter of the Covid-19 pandemic and
humanitarian crises in Italy: Changing perspectives on preparation
and mitigation. NEJM Catal: Mar 21, 2021 (Epub ahead of print).
doi: 10.1056/cat.20.0080.
|
|
110
|
Chou R, Dana T, Buckley DI, Selph S, Fu R
and Totten AM: Epidemiology of and risk factors for coronavirus
infection in health care workers: A living rapid review. Ann Intern
Med. 173:120–136. 2020.PubMed/NCBI View Article : Google Scholar
|
|
111
|
Coronavirus disease 2019 (COVID-19)
pandemic: Increased transmission in the EU/EEA and the UK-seventh
update. Available from: www.ecdc.europa.eu. Accessed March 25, 2020.
|
|
112
|
Li W, Yang Y, Liu ZH, Zhao YL, Zhang Q,
Zhang L, Cheung T and Xiang YT: Progression of mental health
services during the COVID-19 outbreak in China. Int J Biol Sci.
16:1732–1738. 2020.PubMed/NCBI View Article : Google Scholar
|
|
113
|
Augustine R, Das S, Hasan A, S A, Abdul
Salam S, Augustine P, Dalvi YB, Varghese R, Primavera R, Yassine
HM, et al: Rapid antibody-based COVID-19 mass surveillance:
Relevance, challenges, and prospects in a pandemic and
post-pandemic world. J Clin Med. 9(3372)2020.PubMed/NCBI View Article : Google Scholar
|
|
114
|
Skoll D, Miller JC and Saxon LA: COVID-19
testing and infection surveillance: Is a combined digital
contact-tracing and mass-testing solution feasible in the United
States? Cardiovasc Digit Health J. 1:149–159. 2020.PubMed/NCBI View Article : Google Scholar
|
|
115
|
Ucciferri C, Vecchiet J and Falasca K:
Role of monoclonal antibody drugs in the treatment of COVID-19.
World J Clin Cases. 8:4280–4285. 2020.PubMed/NCBI View Article : Google Scholar
|
|
116
|
Rotzinger DC, Beigelman-Aubry C, von
Garnier C and Qanadli SD: Pulmonary embolism in patients with
COVID-19: Time to change the paradigm of computed tomography.
Thromb Res. 190:58–59. 2020.PubMed/NCBI View Article : Google Scholar
|
|
117
|
Marrie TJ and Shariatzadeh MR:
Community-acquired pneumonia requiring admission to an intensive
care unit: A descriptive study. Medicine (Baltimore). 86:103–111.
2007.PubMed/NCBI View Article : Google Scholar
|
|
118
|
Thachil J, Tang N, Gando S, Falanga A,
Cattaneo M, Levi M, Clark C and Iba T: ISTH interim guidance on
recognition and management of coagulopathy in COVID-19. J Thromb
Haemost. 18:1023–1026. 2020.PubMed/NCBI View Article : Google Scholar
|
|
119
|
Italian National Statistics Institute
(ISTAT). Report February 13. Available from: www.istat.it.
Accessed April 20, 2020.
|
|
120
|
Baud D, Qi X, Nielsen-Saines K, Musso D,
Pomar L and Favre G: Real estimates of mortality following COVID-19
infection. Lancet Infect Dis. 20(773)2020.PubMed/NCBI View Article : Google Scholar
|
|
121
|
Salerno M, Sessa F, Piscopo A, Montana A,
Torrisi M, Patanè F, Murabito P, Volti GL and Pomara C: No
autopsies on COVID-19 deaths: A missed opportunity and the lockdown
of science. J Clin Med. 9(1472)2020.PubMed/NCBI View Article : Google Scholar
|
|
122
|
Barth RF, Xu X and Buja LM: A call to
action: The need for autopsies to determine the full extent of
organ involvement associated with COVID-19. Chest. 158:43–44.
2020.PubMed/NCBI View Article : Google Scholar
|
|
123
|
Costantino C, Cannizzaro E, Alba D,
Conforto A, Cimino L and Mazzucco W: SARS-CoV-2 pandemic in the
mediterranean area: Epidemiology and perspectives.
EuroMediterranean Biomed J. 15:102–106. 2020.
|
|
124
|
Costantino C, Ledda C, Genovese C,
Contrino E, Vitale E, Maida CM, Squeri R, Vitale F and Rapisarda V:
Immunization status against measles of health-care workers
operating at three sicilian university hospitals: An observational
study. Vaccines (Basel). 7(175)2019.PubMed/NCBI View Article : Google Scholar
|
|
125
|
Yamaoka-Tojo M: Endothelial glycocalyx
damage as a systemic inflammatory microvascular endotheliopathy in
COVID-19. Biomed J. 43:399–413. 2020.PubMed/NCBI View Article : Google Scholar
|
|
126
|
Hunter DJ: Covid-19 and the stiff upper
lip-the pandemic response in the United Kingdom. N Engl J Med.
382(e31)2020.PubMed/NCBI View Article : Google Scholar
|